Abstract
Coronavirus disease (COVID-19) is an infectious disease that is caused by a highly contagious and severe acute respiratory syndrome—coronavirus 2 (SARS-CoV-2). This infection started to spread across the world in 2019 and rapidly turned into a global pandemic, causing an urgent necessity for treatment strategies development. The mRNA vaccines against SARS-CoV-2 can trigger an immune response, providing genetic information that allows the production of spike glycoproteins. MiRNAs play a crucial role in diverse key cellular processes, including antiviral defense. Several miRNAs are described as key factors in SARS-CoV-2 human infection through the regulation of ACE2 levels and by the inhibition of SARS-CoV-2 replication and spike expression. Consequently, these molecules have been considered as highly promising biomarkers. In numerous human malignancies, it has been recognized that miRNAs expression is dysregulated. Since miRNAs can target SARS-CoV-2-associated mRNAs, in cancer patients, the deregulation of these molecules can impair the immune response to the vaccines. Therefore, in this review, we propose a miRNA profile of seven SARS-CoV-2-related miRNAs, namely miR-214, miR-98-5p, miR-7-5p, miR-24-3p, miR-145-5p, miR-223-3p and miR-15b-5p, that are deregulated in a high number of cancers and have the potential to be used as prognostic biomarkers to stratify cancer patients.
Keywords: COVID-19, vaccine, miRNAs, immune response, cancer
1. Introduction
Coronavirus disease 2019 (COVID-19) is the clinical manifestation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. This infection started to spread across the world in 2019, increasing hospitalization rates in several countries, and rapidly turned into a global pandemic [2]. Considering the high infection rate, which can affect an elevated percentage of individuals in each community in a short period, the mortality rate and the death risk estimation are related to the breakdown of the healthcare systems [3,4]. Therefore, on March 2020, the World Health Organization (WHO) declared a pandemic, leading to the emergence of public health strategies to contain the outbreak, including social confinement and movement restriction [2,5]. Reported illnesses have ranged from very mild (including some with no reported symptoms) to severe, including illness resulting in death [4]. Despite the worldwide spread, the clinical and epidemiological patterns of COVID-19 remain unclear [6]. The first epidemiological and clinical investigations showed that most COVID-19 cases were attributed to elder or middle- aged men, with a mean incubation period of 5.2 days [7,8]. Aside from age and gender, there are also pre-existing conditions that are considered to be risk factors for SARS-CoV-2 infection, namely: hypertension, obesity, diabetes mellitus, asthma, chronic obstructive pulmonary disease, chronic kidney disease, smoking, and diseases that induce an immunosuppression state such as cancer [9].
Cancer has a major impact on society, with more than 18 million new cases per year globally [10]. Cancer patients are more susceptible to infection compared to healthy people and non-cancer patients [11,12]. This predisposition has been historically related to the systemic malignancy-related immunosuppressive state and to active disease-oriented treatments, such as chemotherapy, immunotherapy, radiotherapy, and surgery [13,14].
SARS-CoV-2 is a member of the Coronaviridae family and consists in an enveloped, single-stranded RNA virus with positive polarity and a genome of approximately 30 kilobases [15]. Like an mRNA, the virus genome consists of a 5′ cap structure together with a 3′ poly (A) tail that translates its proteins. Coronaviridae viruses contain similar genomic RNA (gRNA) compositions, including two open reading frames (ORF1a and ORF1b), which encode for the RNA-dependent RNA polymerase (RdRp) and nonstructural proteins (nsps) [16]. ORF1a contributes to the production of nsp1–nsp11, while the rest of the nsps (nsp12–nsp16) originate from ORF1b [17]. In addition to this, one-third of the genome at the 3′ end encodes for the viral structural proteins’ surface (S), envelope (E), membrane (M), and nucleocapsid (N) [17,18]. Moreover, the genomes of Coronaviridae viruses also contain multiple structurally conserved elements within the 5′ and 3′ untranslated regions (UTRs) that have been suggested to play roles in viral replication. These elements include three stem-loops (SL1, SL2 and SL3) within the 5′ UTR, as well as a bulged stem-loop (BSL), pseudoknot (PK) stem-loop, and hypervariable region (HVR) within the 3′ UTR. The spike glycoprotein of SARS-CoV-2 comprises the receptor binding domain (RBD) in the S1 subunit, which binds with the angiotensin-converting enzyme 2 (ACE2), allowing the penetration of the virus into the endothelial and epithelial cells and consequently activating infection [19,20]. The S2 subunit improves the fusion of viral and host cell membranes that is activated by the transmembrane protease serine 2 (TMPRSS2) [20]. Then, the virus affinity to infect certain cells may be related to the multiple organ distribution of ACE2, the functional receptor for SARS-CoV-2 [21]. Consequently, spike glycoprotein and its RBD are crucial targets for vaccination and therapeutic improvement [22,23].
The global pandemic has caused an urgent necessity for vaccine development promoting the emergence of mRNA vaccines against SARS-CoV-2 [23,24]. These mRNA vaccines provide genetic information in the form of mRNA allowing the production of viral proteins by the host—more specifically the spike glycoproteins—to trigger an immune response [23,25]. However, it is important to note that, in the same way that some subsets of the population are more prone to SARS-CoV-2 infection due to immunosuppression (either caused by cancer or other immune disorders), the same applies for their capacity of vaccination response. In fact, since cancer patients are not included in vaccination clinical trials, there is still a considerable uncertainty regarding the efficacy of the SARS-CoV-2 vaccines that are available, as well as the extent of the humoral and cellular immune responses and the impact of related side effects [26]. In fact, cancer patients have a three-fold higher infection risk than the general population [27]. Therefore, it is important to identify and study new potential biomarkers and therapeutic targets for this disease. Moreover, patients with lung or hematological cancers and those who receive active chemotherapy treatment are at a greater risk of SARS-CoV-2 infection, due to an increased immunosuppression state [28]. In addition to an increased susceptibility to SARS-CoV-2 infection, the immunosuppressive state of cancer patients also makes them more prone to vaccination failure [28]. However, due to the novelty of the mRNA vaccination field, the mechanisms behind vaccination responsiveness and immunity development are not fully understood. Therefore, it is important to identify and study new potential biomarkers that can predict and monitor these patients’ susceptibility to SARS-CoV-2 infection and responsiveness to vaccination.
Currently, there is a massive investment in circulating microRNAs (miRNAs) research, due to their potential use as biomarkers for innumerous conditions. The intensive research of the past few years has demonstrated that miRNAs are secreted in several of the body fluids (e.g., blood, plasma, serum, saliva, urine, etc.) that are routinely examined in patients; are stable and resistant to degradation; and are easy to quantify through molecular biology techniques such as real time PCR [29,30,31]. This set of characteristics make miRNAs excellent biomarker candidates, with the advantage that they can be obtained through non-invasive or minimally invasive methods. MicroRNAs (miRNAs) are small non-coding RNAs of 18–25 nucleotides that play a key role in the regulation of gene expression through the post-transcriptional suppression of mRNAs [32,33]. MiRNAs have been shown to regulate every aspect of cellular activity, including differentiation and development, metabolism, proliferation and apoptosis [34]. In fact, they can regulate approximately 30–70% of human gene expression [35]. These molecules can bind directly to mRNA targets by complementarity, causing their degradation or suppressing the translation process [32]. Thousands of human protein coding genes are regulated by miRNAs, reinforcing the idea that miRNAs are master regulators of diverse biological processes with an impact in the body physiological responses [34]. Over the past decade, it has been established that miRNAs expression is dysregulated in several human malignancies, consequently affecting the hallmarks of cancer and having either an oncogenic or tumour suppressor role [36].
In addition to this, miRNAs also play a central role in immunity development and host antiviral defense [1,33]. In fact, miRNAs have been considered as highly promising biomarkers that can, among several functions, regulate immunity-related gene targets through complex networks of virus–host cell interactions [1]. Several miRNAs are described as key factors in SARS-CoV-2 human infection, regulating the inflammation, interfering with the innate immune response and assuming antiviral roles [2,37]. Further, some miRNAs were reported as crucial for virus entrance in the host cells that were involved in ACE2 levels regulation [38,39]. Furthermore, there are diverse studies demonstrating that miRNAs inhibit SARS-CoV-2 replication and inhibit spike expression [40,41]. Taking this into consideration, miRNAs can hold a positive or negative role in virus-related processes in three ways: (1) direct binding to the viral genome; (2) binding to viral transcripts; (3) binding to host transcripts [42]. Thus, human miRNAs can have a dual role: they can promote the stability and replication of viral RNA, or they can reinforce the host antiviral response. Consequently, miRNAs are considered as promising tools to explore the regulatory networks behind the immune response to COVID-19 infection and to vaccination [43,44].
Therefore, the abnormal miRNAs expression known in cancer patients may also contribute to the severity of SARS-CoV-2 infection and diminish the immune response to the vaccines. Hence, the scope of this review is to gather and systematize the available information regarding the known miRNAs that are involved in SARS-CoV-2 regulation and their expression patterns in the cancer context.
2. Evidence Acquisition
A literature search in PubMed was conducted using the search terms “microRNA” and “SARS-CoV-2”. The literature analysis included 350 articles that were published between 2020 and 2022. The articles were manually curated and selected by the relevance of their findings, namely, the validated interaction between a miRNA and a SARS-CoV-2 related mRNA. Of the 350 articles that were found, 319 were excluded. The exclusion criteria for the collected articles were as follows: (1) non-human miRNAs; (2) no association between miRNAs and SARS-CoV-2-related mRNAs; (3) articles based only on bioinformatic predictions or in silico analysis of interactions between miRNAs and SARS-CoV-2 related mRNAs; (4) editorials, comments and protocols; (5) individual papers that were already included in meta-analysis or reviews. For each study, information was extracted concerning the following characteristics: the name of the miRNA, the mRNA target, and validation of the miRNA–mRNA interaction through robust methods.
3. Evidence Synthesis
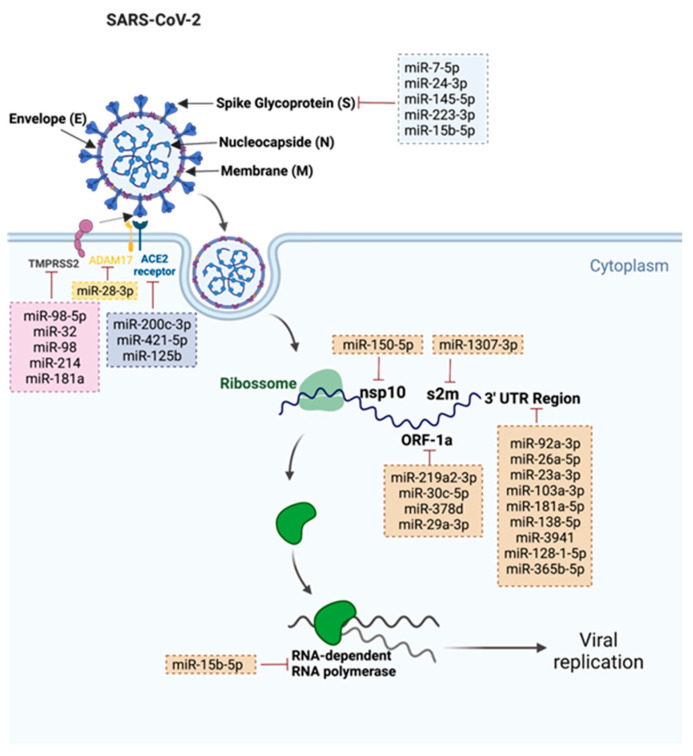
A total of 31 miRNAs were found. The gathered information is summarized in Figure 1. The relevant miRNAs were divided into two categories: (1) miRNAs that target SARS-CoV-2 (2) miRNAs that target SARS-CoV-2 related proteins.
Figure 1.
Representation of the 31 validated SARS-CoV-2 miRNAs and their respective targets. This figure was created at BioRender.com (accessed on 12 July 2022).
3.1. miRNAs That Target SARS-CoV-2
We found a total of 22 human miRNAs that were involved in the targeting of several components of SARS-CoV-2, such as: 3′–untranslated regions (UTR); open reading frames (ORF); stem-loop II motif (s2m); and RNA template components of non-structural protein 10 (nsp10), spike protein, and RNA-dependent RNA polymerase (RdRp). Nine miRNAs were involved in the targeting conserved 3′–UTR of the viral genome. Park and colleagues observed that miR-92a-3p, miR-26a-5p, miR-23a-3p, miR-103a-3p and miR-181a-5p from placenta stem-cell-derived extracellular vesicles (EVs) were able to bind to 3′-UTR regions of SARS-CoV-2 and suppress RNA replication, consequently leading to the suppression of the virus-mediated pro-inflammatory response in human bronchial cells and lung fibroblasts [45]. In addition to this, Barreda-Manso and co-workers described that miR-138-5p, miR-3941, miR-128-1-5p and miR-365b-5p were also able to bind to 3´-UTR regions of SARS-CoV-2 [46]. While some of the SARS-CoV-2 3′-UTR is variable in sequence, the virus contains a highly conserved 41-nucleotide (nt) stem-loop II motif (s2m) within the terminal portion of the HVR (hypervariable region) [47]. Imperatore and colleagues highlighted the potential role of the s2m element in mediating the viral genome dimerization, suggesting its potential application as a drug target. Moreover, the authors observed that host miR-1307-3p was able to bind and inhibit s2m [47]. Akula and co-workers observed that the decline in plasma levels of miR-150-5p in COVID-19 patients could enhance SARS-CoV-2 infection [48]. In fact, these authors demonstrated that miR-150-5p was able to lower SARS-CoV-2 infection in vitro by targeting the coding strand of nsp10 and suggested that downregulation of this miRNA could be a mechanism to promote SARS-CoV-2 infection [48]. Six miRNAs were involved in the targeting of the spike (S) protein. Wang and colleagues demonstrated that miR-7-5p, miR-24-3p, miR-145-5 and miR-223-3p were able to directly target the S protein and inhibit SARS-CoV-2 replication [40]. Moreover, the authors also observed that these miRNAs were markedly decreased in elderly and diabetic patients when compared to young healthy volunteers [40]. Siniscalchi and colleagues observed that endogenously expressed lung miRNAs were able to bind and inhibit viral targets. The authors observed that miR-219a2-3p, miR-30c-5p, miR-378d and miR-29a-3p were able to bind to ORF1a, and miR-15b-5p was able to bind to spike ORF and repress plasmid-driven spike expression [49]. Moreover, these authors were also able to demonstrate that synthetic miRNA mimics of the miRNAs that were studied could be used to inhibit SARS-CoV-2, which highlights the potential of miRNAs as a therapeutic approach to fight the viral infection. In addition to spike ORF, miR-15b-5p was also described as being able to target the RNA template component of RdRp, further contributing to the suppression of viral infection and proliferation [50].
3.2. miRNAs That Target SARS-CoV-2 Related Proteins
We found a total of nine miRNAs involved in the targeting of key proteins that allow the entry of SARS-CoV-2 into the host cells—more specifically, TMPRSS2, ACE2 and ADAM7.
ACE2 acts as a key receptor for the spike of SARS-CoV-2, and it is crucial for the virus entry into the cells. MR-200c-3p and miR-421-5p can target ACE2, and their expression was decreased in the blood of SARS-CoV-2 patients at hospital admission, also suggesting a relation with the degree of infection [39]. On the other hand, Papannarao observed an increased expression of miR-200c in the blood of obese patients and suggested that increased angiotensin II, followed by inhibition of ACE2 through miR-200c targeting, may increase the severity of the SARS-CoV-2 infection in obese people [51]. Moreover, despite SARS-CoV-2 infection primarily manifesting as an acute respiratory illness that is accompanied by interstitial and alveolar pneumonia, it also affects multiple organs, such as the heart, digestive tract, blood, central nervous system, and the kidney. This is because ACE2 is widely expressed in the lungs, intestine, liver, testis, central nervous system, heart tissue and the kidneys [52]. In fact, in a review article, Widiasta and colleagues highlighted the importance of kidney-specific miR-125b in the modulation of ACE2 expression and COVID-19-associated nephropathy [53]. In addition to this, Xu and colleagues reported that miR-8-3p inhibits A disintegrin and metalloproteinase 17 (ADAM17)-dependent ACE2 ectodomain shedding in 293T cell treated with the S protein of SARS-CoV-2, suggesting its potential role as a therapeutic approach in the prevention and treatment of SARS-CoV-2 infection [54]. Another important protein for SARS-CoV-2 entry into the cells is TMPRSS2, which is involved in the fusion of viral and host cell membranes. Matarese and colleagues mechanistically validated miR-98-5p as a regulator of TMPRSS2 transcription in lung and umbilical vein endothelial cell types [55]. In addition to this, Kaur and co-workers silenced TMPRSS2 in Caco-2 cells with the transfection of miR-32, miR-98 and miR-214, and were able to achieve maximum gene suppression with miR-32 at a concentration of 40 nM [56]. It was also described that miR-181a, which also targets TMPRSS2, was only downregulated in severe cases of COVID19 and was associated with delayed viral clearance after infection [57].
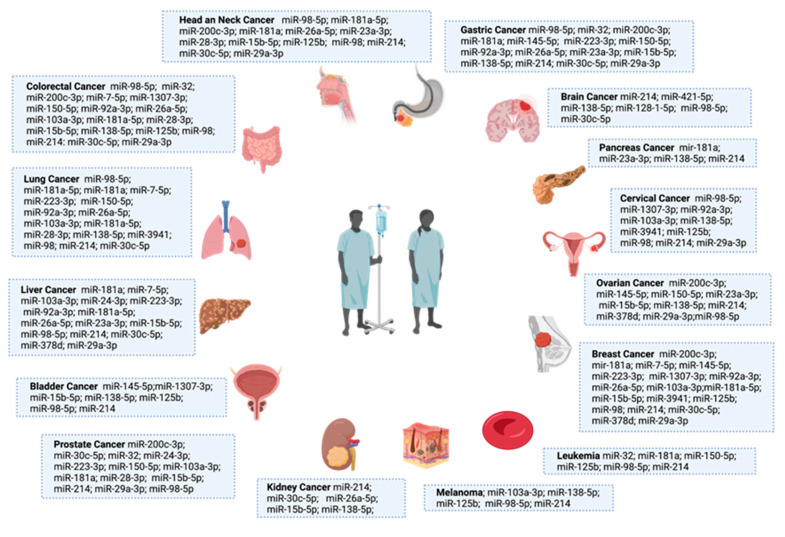
4. SARS-CoV-2-Related miRNAs Deregulation Impact on Cancer Patients’ Infection Susceptibility and Vaccination Response
MiRNA deregulation is well established in cancer, influencing its biogenesis and the evolution of the disease. We then endeavored to see if there were data available regarding these 31 SARS-CoV-2-related miRNAs in the cancer context—more specifically, in 15 common cancer types. The information is summarized in Figure 2. Colorectal, lung, breast and liver cancers were those that had more SARS-CoV-2-related miRNAs that were described as deregulated. Moreover, we also observed that several of those miRNAs were common to several types of cancer (Figure 2). Interestingly, of the 15 cancer types that we selected, miR-214 was reported as deregulated in all of them [58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. As previously stated, this miRNA targets TMPRSS2, which is crucial for SARS-CoV-2 entry into the cells. Therefore, a downregulation of this miRNA can lead to an increased expression of TMPRSS2 and an increased susceptibility to SARS-CoV-2 infection. In addition to this, miR-214 is known for is tumorigenic and suppressive roles in cancer, and it is also being considered as a potential biomarker and therapeutic agent [73], apart from in brain and pancreatic cancer, and melanoma were it as an oncogenic role (Figure 2) [58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. Moreover, miR-98, another miRNA that targets TMPRSS2, was reported as deregulated in 14 of the 15 cancer types that are displayed in Figure 2 (it was not described in kidney cancer). It was also downregulated in all of them except for prostate cancer, where it was described as upregulated. This information suggests that the downregulation of these miRNAs may be related to an increased susceptibility of cancers patients to develop SARS-CoV-2 infection, but this hypothesis needs to be validated.
Figure 2.
SARS-CoV-2 related miRNAs deregulated among 15 cancer types (gastric, brain, pancreas, ovarian, breast, leukemia, melanoma, kidney, prostate, bladder, liver, lung, colorectal and head and neck). This figure was created at BioRender.com (accessed on 6 May 2022).
Another important issue is the five miRNAs (miR-7-5p, miR-24-3p, miR-145-5p, miR-223-3p and miR-15b-5p) that target S protein sequences and are also deregulated in the cancer context [74,75,76,77,78,79,80,81]. This is because some of the SARS-CoV-2 vaccines are S protein mRNA fragments that are delivered to the cells through a lipid vesicle delivery approach [82]. Therefore, if the host has an overexpression of miRNAs that target S protein mRNA sequences, one can hypothesize that this host is more prone to experience reduced vaccine efficacy. In addition to other biological processes and pathways, all these miRNAs have already been reported as implicated in cancer therapy resistance or comorbidities. MiR-24-3p [74,75] and miR-7-5p [76] are associated with chemotherapy resistance; miR-145-5p [77,78] has been associated with cancer stemness and therapy resistance; miR-15b-5p [79] has been associated with doxorubicin-induced cardiotoxicity; and miR-223-3p [80,81] with radioresistance. This information suggests that the overexpression of these miRNAs in cancer patients may be related to an increased susceptibility of SARS-CoV-2 mRNA-based vaccination failure, but once again, this is a hypothesis that needs to be validated.
Role of miR-214, miR-98-5p, miR-7-5p, miR-24-3p, miR-145-5p, miR-223-3p and miR-15b-5p in the Cytokine Storm Regulation
The cytokine storm is defined as an excessive immune response to external stimuli, such as an infection or even vaccination. The pathogenesis of the cytokine storm is complex, and the disease progresses rapidly, leading to the excessive production of cytokines by the immune system that can ultimately result in the death of the patient [83]. Recent evidence shows that, during the COVID-19 pandemic, the severe deterioration of some patients was closely related to the cytokine storm in their bodies [84]. Therefore, it is also important to study biomarkers that can predict and monitor this complex immunological phenomenon.
Based on all of the information described above, we identified miR-214, miR-98-5p, miR-7-5p, miR-24-3p, miR-145-5p, miR-223-3p and miR-15b-5p with particular interest. These miRNAs are key players in the regulation of SARS-CoV-2 human infection and are also deregulated in several types of cancer; therefore, we wished to check their role in the inflammatory process. Concerning miR-214, Sun et al. demonstrated that this miRNA could target PD-L1 to regulate the immune response of diffuse large B-cell lymphoma by modulating IL-10, IFN-γ and TNF-α expression [85]. Additionally, in ulcerative colitis, it seems that the downregulation of miR-214 may contribute to the pathogenesis of this disease. It occurs since miR-214-3p directly targets STAT6, which is upregulated in ulcerative colitis patients, and enhances the pathogenesis of this illness [86]. Regarding miR-98-5p, Wang et al. reported that this miRNA negatively modulates IL-6 expression in rheumatoid fibroblast-like synoviocytes, serving as a potential regulator of the inflammatory process. Therefore, they proposed that the manipulation of miR-98-5 could be a potential clinical intervention, serving as an inhibitor of IL-6 expression in rheumatoid arthritis [87]. On the other hand, this miRNA also targets IL-10, which is an anti-inflammatory cytokine and plays an important role in maintaining intestinal homeostasis and the mucosal barrier. Therefore, miR-98-5p may play a key role in the aggravation of ulcerative colitis, since it diminishes IL-10 expression [88]. MiR-7-5p was described as being able to inhibit melanoma growth and metastasis through the inactivation of NF-κB signaling, which leads to the decreased of NF-κB target genes expression, such as IL-1β, IL-6 and IL-8 [89]. In turn, Lin et al. demonstrated that the overexpression of miR-24-3p promoted cell proliferation, inhibited apoptosis, and increased cell migration and invasion in prostate cancer. This miRNA targets and suppresses the suppressor of cytokine signaling 6 (SOCS6), which acts as a tumor suppressor, due to the inhibition of cytokine signaling pathways [90]. Concerning miR-145-5p, Zhuang et al. showed that it was downregulated in colon cancer. Moreover, they suggested that this miRNA acts as a tumor suppressor through targeting chemokine (C-X-C motif) ligand 1 (CXCL1), which is overexpressed in colorectal cancer and facilitates metastasis and the progression of tumorigenesis [91]. MiR-223-3p can also interact with cytokines and modulate the inflammatory response. In a glioblastoma in vitro study, Ding et al. verified that treatment with miR-223-3p mimic inhibits cell proliferation and migration via decreasing numerous inflammation-associated cytokines, such as interleukin-1β, monocyte chemoattractant protein-1, IL-8 and IL-18 [91]. Furthermore, in adipose stem cells, it was confirmed that miR-223-3p directly affects the expression of the inflammatory cytokines IL-6, IL-1β and TNF-α [92]. MiR-15b-5p also interferes with the levels of some cytokines. In a high glucose-induced podocyte injury, it was shown that this miRNA was able to ameliorate the patient’s condition, attenuating the expression of IL-1β, TNF-α, and IL-6 [93]. Based on these examples, we can conclude that all of these miRNAs have the capacity to modulate the inflammation process and interfere with the immune response through the regulation of cytokine levels.
5. MiRNAs Applications in Cancer Patients’ Management Regarding SARS-CoV-2
The use of circulating miRNAs as clinical biomarkers has been explored under a variety of conditions, including cancer and viral infections [94,95]. MiRNAs are considered to be robust, sensitive, and cost-effective biomarkers that can add additional information to the clinical variables that are already used in the clinical practice [58,96]. In fact, several miRNA-based diagnostic and therapeutic products are already in clinical trial phase and expected to enter the market in the next few years [97]. Therefore, the study and use of miRNA profiles to stratify cancer patients according to their risk of SARS-CoV-2 infection and vaccination effectiveness seems a promising personalized approach to improve the current management of these patients (Figure 3). Moreover, miRNAs can be obtained through minimally invasive methods, such as a blood sample, and their isolation and quantification protocols are simple and less time-consuming when compared with other type of molecules [29,30]. In fact, the implementation of a stratification algorithm would allow the selection of patients that could benefit from the emerging SARS-CoV-2 therapeutic approaches, such as the Long-Acting Antibodies (LAAB) AZD7442, which are currently in phase III clinical trials (ClinicalTrials.Gov NCT04507256) and show promising results in reducing the risk of severe COVID-19 or death. LAABs mimic natural antibodies and can block the binding of the SARS-CoV-2 virus to host cells [98]. Therefore, their potential is being tested to treat and prevent disease progression in patients that are already infected with the virus, as well as to be given as a preventative intervention prior to exposure to the virus.
Figure 3.
Schematic representation of the applicability of using miRNA profiles to stratify cancer patients according to their prognostic in terms of SARS-CoV-2 infection risk and vaccination responsiveness. This figure was created at BioRender.com. (accessed on 12 July 2022).
6. Discussion
The COVID-19 pandemic tested the resilience of health-care systems worldwide in an unprecedented manner and forced clinicians to rethink and adapt the diagnostic and therapeutic approaches based on the local prevalence of the virus in their communities [28]. This includes the cancer patient population, which is particularly susceptible to SARS-CoV-2 infection and complications. Therefore, there is an urgent need for a stratification system that can allow the selection of cancer patients with an increased risk of infection and/or lower vaccination response, in order to help oncologists to prioritize patients and optimize health-care system resources to provide the best patient care, given the circumstances.
Considering that miRNAs are among the earliest molecular regulators, circulating miRNAs could be potential biomarkers in the early identification of those at the highest risk of developing COVID-19 and related complications. In fact, there are a few recent studies describing plasma miRNA profiles that are capable of predicting the ICU stay of patients and the severity of SARS-CoV-2 infection [99,100]. Moreover, other authors have proposed that miRNAs could be used as a therapeutic approach against COVID-19 [101,102]. However, there are no studies covering the applicability of using miRNA profiles to stratify cancer patients according to their risk of developing SARS-CoV-2 infection and/or decreased vaccination response. In this review, we summarized the available information regarding the miRNAs that interact with SARS-CoV-2 and SARS-CoV-2-related genes that are already validated and checked if those miRNAs were reported as deregulated in cancer. Based on this information, we propose a miRNA profile of seven SARS-CoV-2-related miRNAs (miR-214, miR-98-5p, miR-7-5p, miR-24-3p, miR-145-5p, miR-223-3p and miR-15b-5p) that are deregulated in a high number of cancers and have the potential to be used as prognostic biomarkers to stratify cancer patients. Moreover, we also gathered information regarding the impact of these miRNAs in immune-related molecules, such as cytokines and chemokines, that can also have an impact in the development of the cytokine storm. However, it is important to note that future studies require the validation of this miRNA profile in the clinical setting to validate our hypothesis before integrating it into the decision-making algorithms that are used by clinicians. Since miRNAs are stable and detectable using small quantities of human body fluids, it would be possible to conduct miRNA quantification in a high number of cancer patients in a short period of time using the samples that are already stored at the biobanks of the hospitals and cancer institutes. Overall, miRNA research has demonstrated a lot of potential in the cancer field in the last few years, ranging from biomarker potential to personalized therapeutic applications. Thus, it makes sense to expand the range of application of prognostic biomarkers to further stratify cancer patients according to their prognostic, regarding SARS-CoV-2 infection and vaccination benefit.
Author Contributions
Conceptualization, F.D. and T.R.D.; methodology, T.R.D. and F.D.; software, T.R.D. and F.D.; validation, T.R.D., F.D. and A.L.T.; formal analysis, T.R.D. and F.D.; investigation, T.R.D. and F.D.; resources, R.M.; data curation, F.D. and T.R.D.; writing—original draft preparation, F.D. and T.R.D.; writing—review and editing, A.L.T., H.S. and J.O.; visualization, F.D. and T.R.D. supervision, A.L.T.; project administration, R.M.; funding acquisition, R.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Portuguese national funding agency for science, research and technology (FCT—Fundação para a Ciência e a Tecnologia), project reference: UIDP/00776/2020). TD is a research fellow from LPCC-NRN (LPCC-NRN-2022-TD) and FD has a junior researcher contract funded by UIDP/00776/2020-4B.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abedi F., Rezaee R., Hayes A.W., Nasiripour S., Karimi G. MicroRNAs and SARS-CoV-2 life cycle, pathogenesis, and mutations: Biomarkers or therapeutic agents? Cell Cycle. 2021;20:143–153. doi: 10.1080/15384101.2020.1867792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Visacri M.B., Nicoletti A.S., Pincinato E.C., Loren P., Saavedra N., Saavedra K., Salazar L.A., Moriel P. Role of miRNAs as biomarkers of COVID-19: A scoping review of the status and future directions for research in this field. Biomark Med. 2021;15:1785–1795. doi: 10.2217/bmm-2021-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Challen R., Brooks-Pollock E., Read J.M., Dyson L., Tsaneva-Atanasova K., Danon L. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: Matched cohort study. BMJ. 2021;372:n579. doi: 10.1136/bmj.n579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 5.Keppel G., Cole A.M., Ramsbottom M., Nagpal S., Hornecker J., Thomson C., Nguyen V., Baldwin L.M. Early Response of Primary Care Practices to COVID-19 Pandemic. J. Prim. Care Community Health. 2022;13:21501319221085374. doi: 10.1177/21501319221085374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shahbazi F., Solgi M., Khazaei S. Predisposing risk factors for COVID-19 infection: A case-control study. Casp. J. Intern. Med. 2020;11((Suppl. S1)):495–500. doi: 10.22088/cjim.11.0.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bai Y., Yao L., Wei T., Tian F., Jin D.Y., Chen L., Wang M. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shahbazi F., Khazaei S. Socio-economic inequality in global incidence and mortality rates from coronavirus disease 2019: An ecological study. New Microbes New Infect. 2020;38:100762. doi: 10.1016/j.nmni.2020.100762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cordero-Franco H.F., De La Garza-Salinas L.H., Gomez-Garcia S., Moreno-Cuevas J.E., Vargas-Villarreal J., González-Salazar F. Risk Factors for SARS-CoV-2 Infection, Pneumonia, Intubation, and Death in Northeast Mexico. Front. Public Health. 2021;9:645739. doi: 10.3389/fpubh.2021.645739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2020. CA Cancer J. Clin. 2020;70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 11.Liang W., Guan W., Chen R., Wang W., Li J., Xu K., Li C., Ai Q., Lu W., Liang H., et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Desai A., Gupta R., Advani S., Ouellette L., Kuderer N.M., Lyman G.H., Li A. Mortality in hospitalized patients with cancer and coronavirus disease 2019: A systematic review and meta-analysis of cohort studies. Cancer. 2021;127:1459–1468. doi: 10.1002/cncr.33386. [DOI] [PubMed] [Google Scholar]
- 13.Ramasamy C., Mishra A.K., John K.J., Lal A. Clinical considerations for critically ill COVID-19 cancer patients: A systematic review. World J. Clin. Cases. 2021;9:8441–8452. doi: 10.12998/wjcc.v9.i28.8441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rajan S., Akhtar N., Sharma S., Chakrabarti D., Kumar V. COVID-19 vaccination for cancer patients: Evidence, priority, and practice. Vaccine. 2021;39:5075–5077. doi: 10.1016/j.vaccine.2021.07.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fehr A.R., Perlman S. Coronaviruses: An overview of their replication and pathogenesis. Methods Mol. Biol. 2015;1282:1–23. doi: 10.1007/978-1-4939-2438-7_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Y., Liu Q., Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J. Med. Virol. 2020;92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khailany R.A., Safdar M., Ozaslan M. Genomic characterization of a novel SARS-CoV-2. Gene Rep. 2020;19:100682. doi: 10.1016/j.genrep.2020.100682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Narayanan K., Ramirez S.I., Lokugamage K.G., Makino S. Coronavirus nonstructural protein 1: Common and distinct functions in the regulation of host and viral gene expression. Virus Res. 2015;202:89–100. doi: 10.1016/j.virusres.2014.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li F., Li W., Farzan M., Harrison S.C. Structure of SARS coronavirus spike receptor-binding domain complexed with receptor. Science. 2005;309:1864–1868. doi: 10.1126/science.1116480. [DOI] [PubMed] [Google Scholar]
- 20.Petrovszki D., Walter F.R., Vigh J.P., Kocsis A., Valkai S., Deli M.A., Dér A. Penetration of the SARS-CoV-2 Spike Protein across the Blood-Brain Barrier, as Revealed by a Combination of a Human Cell Culture Model System and Optical Biosensing. Biomedicines. 2022;10:188. doi: 10.3390/biomedicines10010188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A., Somasundaran M., Sullivan J.L., Luzuriaga K., Greenough T.C., et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adhikari P., Jawad B., Podgornik R., Ching W.Y. Mutations of Omicron Variant at the Interface of the Receptor Domain Motif and Human Angiotensin-Converting Enzyme-2. Int. J. Mol. Sci. 2022;23:2870. doi: 10.3390/ijms23052870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jawad B., Adhikari P., Cheng K., Podgornik R., Ching W.-Y. Computational Design of Miniproteins as SARS-CoV-2 Therapeutic Inhibitors. Int. J. Mol. Sci. 2022;23:838. doi: 10.3390/ijms23020838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang J., Wang W., Chen Z., Lu S., Yang F., Bi Z., Bao L., Mo F., Li X., Huang Y., et al. A vaccine targeting the RBD of the S protein of SARS-CoV-2 induces protective immunity. Nature. 2020;586:572–577. doi: 10.1038/s41586-020-2599-8. [DOI] [PubMed] [Google Scholar]
- 25.Touati R., Elngar A.A. Intelligent system based comparative analysis study of SARS-CoV-2 spike protein and antigenic proteins in different types of vaccines. Beni-Suef Univ. J. Basic Appl. Sci. 2022;11:34. doi: 10.1186/s43088-022-00216-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fendler A., de Vries E.G.E., GeurtsvanKessel C.H., Haanen J.B., Wörmann B., Turajlic S., von Lilienfeld-Toal M. COVID-19 vaccines in patients with cancer: Immunogenicity, efficacy and safety. Nat. Rev. Clin. Oncol. 2022;19:385–401. doi: 10.1038/s41571-022-00610-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Slimano F., Baudouin A., Zerbit J., Toulemonde-Deldicque A., Thomas-Schoemann A., Chevrier R., Daouphars M., Madelaine I., Pourroy B., Tournamille J.F., et al. Cancer, immune suppression and Coronavirus Disease-19 (COVID-19): Need to manage drug safety (French Society for Oncology Pharmacy [SFPO] guidelines) Cancer Treat. Rev. 2020;88:102063. doi: 10.1016/j.ctrv.2020.102063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Addeo A., Friedlaender A. Cancer and COVID-19: Unmasking their ties. Cancer Treat. Rev. 2020;88:102041. doi: 10.1016/j.ctrv.2020.102041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Machado M.T., Navega S., Dias F., de Sousa M.J., Teixeira A.L., Medeiros R. microRNAs for peripheral blood fraction identification: Origin, pathways and forensic relevance. Life Sci. 2015;143:98–104. doi: 10.1016/j.lfs.2015.10.029. [DOI] [PubMed] [Google Scholar]
- 30.Dias F., Teixeira A.L., Ferreira M., Adem B., Bastos N., Vieira J., Fernandes M., Sequeira M.I., Maurício J., Lobo F., et al. Plasmatic miR-210, miR-221 and miR-1233 profile: Potential liquid biopsies candidates for renal cell carcinoma. Oncotarget. 2017;8:103315–103326. doi: 10.18632/oncotarget.21733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cho W.C. MicroRNAs: Potential biomarkers for cancer diagnosis, prognosis and targets for therapy. Int. J. Biochem. Cell Biol. 2010;42:1273–1281. doi: 10.1016/j.biocel.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 32.Macfarlane L.A., Murphy P.R. MicroRNA: Biogenesis, Function and Role in Cancer. Curr. Genom. 2010;11:537–561. doi: 10.2174/138920210793175895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marchi R., Sugita B., Centa A., Fonseca A.S., Bortoletto S., Fiorentin K., Ferreira S., Cavalli L.R. The role of microRNAs in modulating SARS-CoV-2 infection in human cells: A systematic review. Infect Genet Evol. 2021;91:104832. doi: 10.1016/j.meegid.2021.104832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hummel R., Hussey D.J., Haier J. MicroRNAs: Predictors and modifiers of chemo- and radiotherapy in different tumour types. Eur. J. Cancer. 2010;46:298–311. doi: 10.1016/j.ejca.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 35.Lu J., Clark A.G. Impact of microRNA regulation on variation in human gene expression. Genome Res. 2012;22:1243–1254. doi: 10.1101/gr.132514.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peng Y., Croce C.M. The role of MicroRNAs in human cancer. Signal Transduct Target Ther. 2016;1:15004. doi: 10.1038/sigtrans.2015.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tang H., Gao Y., Li Z., Miao Y., Huang Z., Liu X., Xie L., Li H., Wen W., Zheng Y., et al. The noncoding and coding transcriptional landscape of the peripheral immune response in patients with COVID-19. Clin. Transl. Med. 2020;10:e200. doi: 10.1002/ctm2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lu D., Chatterjee S., Xiao K., Riedel I., Wang Y., Foo R., Bär C., Thum T. MicroRNAs targeting the SARS-CoV-2 entry receptor ACE2 in cardiomyocytes. J. Mol. Cell Cardiol. 2020;148:46–49. doi: 10.1016/j.yjmcc.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abdolahi S., Hosseini M., Rezaei R., Mohebbi S.R., Rostami-Nejad M., Mojarad E.N., Mirjalali H., Yadegar A., Asadzadeh Aghdaei H., Zali M.R., et al. Evaluation of miR-200c-3p and miR-421-5p levels during immune responses in the admitted and recovered COVID-19 subjects. Infect Genet Evol. 2022;98:105207. doi: 10.1016/j.meegid.2022.105207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Y., Zhu X., Jiang X.M., Guo J., Fu Z., Zhou Z., Yang P., Guo H., Guo X., Liang G., et al. Decreased inhibition of exosomal miRNAs on SARS-CoV-2 replication underlies poor outcomes in elderly people and diabetic patients. Signal Transduct. Target Ther. 2021;6:300. doi: 10.1038/s41392-021-00716-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Arisan E.D., Dart A., Grant G.H., Arisan S., Cuhadaroglu S., Lange S., Uysal-Onganer P. The Prediction of miRNAs in SARS-CoV-2 Genomes: Hsa-miR Databases Identify 7 Key miRs Linked to Host Responses and Virus Pathogenicity-Related KEGG Pathways Significant for Comorbidities. Viruses. 2020;12:614. doi: 10.3390/v12060614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Trobaugh D.W., Klimstra W.B. MicroRNA Regulation of RNA Virus Replication and Pathogenesis. Trends Mol. Med. 2017;23:80–93. doi: 10.1016/j.molmed.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oshiumi H. Circulating Extracellular Vesicles Carry Immune Regulatory miRNAs and Regulate Vaccine Efficacy and Local Inflammatory Response After Vaccination. Front. Immunol. 2021;12:685344. doi: 10.3389/fimmu.2021.685344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hu J., Stojanović J., Yasamineh S., Yasamineh P., Karuppannan S.K., Hussain Dowlath M.J., Serati-Nouri H. The potential use of microRNAs as a therapeutic strategy for SARS-CoV-2 infection. Arch. Virol. 2021;166:2649–2672. doi: 10.1007/s00705-021-05152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Park J.H., Choi Y., Lim C.W., Park J.M., Yu S.H., Kim Y., Han H.J., Kim C.H., Song Y.S., Kim C., et al. Potential Therapeutic Effect of Micrornas in Extracellular Vesicles from Mesenchymal Stem Cells against SARS-CoV-2. Cells. 2021;10:2393. doi: 10.3390/cells10092393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barreda-Manso M.A., Nieto-Díaz M., Soto A., Muñoz-Galdeano T., Reigada D., Maza R.M. In Silico and In Vitro Analyses Validate Human MicroRNAs Targeting the SARS-CoV-2 3′-UTR. Int. J. Mol. Sci. 2021;22:6094. doi: 10.3390/ijms22116094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Imperatore J.A., Cunningham C.L., Pellegrene K.A., Brinson R.G., Marino J.P., Evanseck J.D., Mihailescu M.R. Highly conserved s2m element of SARS-CoV-2 dimerizes via a kissing complex and interacts with host miRNA-1307-3p. Nucleic Acids Res. 2022;50:1017–1032. doi: 10.1093/nar/gkab1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akula S.M., Bolin P., Cook P.P. Cellular miR-150-5p may have a crucial role to play in the biology of SARS-CoV-2 infection by regulating nsp10 gene. RNA Biol. 2022;19:1–11. doi: 10.1080/15476286.2021.2010959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Siniscalchi C., Di Palo A., Russo A., Potenza N. Human MicroRNAs Interacting With SARS-CoV-2 RNA Sequences: Computational Analysis and Experimental Target Validation. Front. Genet. 2021;12:678994. doi: 10.3389/fgene.2021.678994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sato A., Ogino Y., Tanuma S.I., Uchiumi F. Human microRNA hsa-miR-15b-5p targets the RNA template component of the RNA-dependent RNA polymerase structure in severe acute respiratory syndrome coronavirus 2. Nucleosides Nucleotides Nucleic Acids. 2021;40:790–797. doi: 10.1080/15257770.2021.1950759. [DOI] [PubMed] [Google Scholar]
- 51.Bellae Papannarao J., Schwenke D.O., Manning P., Katare R. Upregulated miR-200c is associated with downregulation of the functional receptor for severe acute respiratory syndrome coronavirus 2 ACE2 in individuals with obesity. Int. J. Obes. 2022;46:238–241. doi: 10.1038/s41366-021-00984-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bourgonje A.R., Abdulle A.E., Timens W., Hillebrands J.L., Navis G.J., Gordijn S.J., Bolling M.C., Dijkstra G., Voors A.A., Osterhaus A.D., et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19) J. Pathol. 2020;251:228–248. doi: 10.1002/path.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Widiasta A., Sribudiani Y., Nugrahapraja H., Hilmanto D., Sekarwana N., Rachmadi D. Potential role of ACE2-related microRNAs in COVID-19-associated nephropathy. Noncoding RNA Res. 2020;5:153–166. doi: 10.1016/j.ncrna.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu Y., Li Y. MicroRNA-28-3p inhibits angiotensin-converting enzyme 2 ectodomain shedding in 293T cells treated with the spike protein of severe acute respiratory syndrome coronavirus 2 by targeting A disintegrin and metalloproteinase 17. Int. J. Mol. Med. 2021;48:189. doi: 10.3892/ijmm.2021.5022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Matarese A., Gambardella J., Sardu C., Santulli G. miR-98 Regulates TMPRSS2 Expression in Human Endothelial Cells: Key Implications for COVID-19. Biomedicines. 2020;8:462. doi: 10.3390/biomedicines8110462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaur T., Kapila S., Kapila R., Kumar S., Upadhyay D., Kaur M., Sharma C. Tmprss2 specific miRNAs as promising regulators for SARS-CoV-2 entry checkpoint. Virus. Res. 2021;294:198275. doi: 10.1016/j.virusres.2020.198275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bautista-Becerril B., Pérez-Dimas G., Sommerhalder-Nava P.C., Hanono A., Martínez-Cisneros J.A., Zarate-Maldonado B., Muñoz-Soria E., Aquino-Gálvez A., Castillejos-López M., Juárez-Cisneros A., et al. miRNAs, from Evolutionary Junk to Possible Prognostic Markers and Therapeutic Targets in COVID-19. Viruses. 2021;14:41. doi: 10.3390/v14010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yang B., Xiong W.Y., Hou H.J., Xu Q., Cai X.L., Zeng T.X., Ha X.Q. Exosomal miRNAs as Biomarkers of Cancer: A Meta-Analysis. Clin. Lab. 2019;65:31115208. doi: 10.7754/Clin.Lab.2018.181011. [DOI] [PubMed] [Google Scholar]
- 59.Guo R., Zou B., Liang Y., Bian J., Xu J., Zhou Q., Zhang C., Chen T., Yang M., Wang H., et al. LncRNA RCAT1 promotes tumor progression and metastasis via miR-214-5p/E2F2 axis in renal cell carcinoma. Cell Death Dis. 2021;12:689. doi: 10.1038/s41419-021-03955-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Deng S., Wang J., Xu J., Li J., Zhang L., Jin Y. Expression of miR-214 in pancreatic cancer and its effect on the biological function of pancreatic cancer cells. J. Buon. 2021;26:1111–1120. [PubMed] [Google Scholar]
- 61.Prabhakar K., Rodrίguez C.I., Jayanthy A.S., Mikheil D.M., Bhasker A.I., Perera R.J., Setaluri V. Role of miR-214 in regulation of β-catenin and the malignant phenotype of melanoma. Mol. Carcinog. 2019;58:1974–1984. doi: 10.1002/mc.23089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yang Y., Li Z., Yuan H., Ji W., Wang K., Lu T., Yu Y., Zeng Q., Li F., Xia W., et al. Reciprocal regulatory mechanism between miR-214-3p and FGFR1 in FGFR1-amplified lung cancer. Oncogenesis. 2019;8:50. doi: 10.1038/s41389-019-0151-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zheng C., Guo K., Chen B., Wen Y., Xu Y. miR-214-5p inhibits human prostate cancer proliferation and migration through regulating CRMP5. Cancer Biomark. 2019;26:193–202. doi: 10.3233/CBM-190128. [DOI] [PubMed] [Google Scholar]
- 64.Wan H., Tian Y., Zhao J., Su X. LINC00665 Targets miR-214-3p/MAPK1 Axis to Accelerate Hepatocellular Carcinoma Growth and Warburg Effect. J. Oncol. 2021;2021:9046798. doi: 10.1155/2021/9046798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Han J.B., Huang M.L., Li F., Yang R., Chen S.M., Tao Z.Z. MiR-214 Mediates Cell Proliferation and Apoptosis of Nasopharyngeal Carcinoma Through Targeting Both WWOX and PTEN. Cancer Biother. Radiopharm. 2020;35:615–625. doi: 10.1089/cbr.2019.2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Min L., Liu C., Kuang J., Wu X., Zhu L. miR-214 inhibits epithelial-mesenchymal transition of breast cancer cells via downregulation of RNF8. Acta Biochim. Biophys. Sin. 2019;51:791–798. doi: 10.1093/abbs/gmz067. [DOI] [PubMed] [Google Scholar]
- 67.He Z., Liao Z., Chen S., Li B., Yu Z., Luo G., Yang L., Zeng C., Li Y. Downregulated miR-17, miR-29c, miR-92a and miR-214 may be related to BCL11B overexpression in T cell acute lymphoblastic leukemia. Asia Pac. J. Clin. Oncol. 2018;14:e259–e265. doi: 10.1111/ajco.12979. [DOI] [PubMed] [Google Scholar]
- 68.Tao W., Li Y., Zhu M., Li C., Li P. LncRNA NORAD Promotes Proliferation and Inhibits Apoptosis of Gastric Cancer by Regulating miR-214/Akt/mTOR Axis. Onco Targets Ther. 2019;12:8841–8851. doi: 10.2147/OTT.S216862. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 69.Pan L., Du M., Liu H., Cheng B., Zhu M., Jia B., Wang Y., He W., Li X., Liu C., et al. LncRNA FTX promotes the malignant progression of colorectal cancer by regulating the miR-214-5p-JAG1 axis. Ann. Transl. Med. 2021;9:1369. doi: 10.21037/atm-21-2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu Y., Zhou H., Ma L., Hou Y., Pan J., Sun C., Yang Y., Zhang J. MiR-214 suppressed ovarian cancer and negatively regulated semaphorin 4D. Tumour Biol. 2016;37:8239–8248. doi: 10.1007/s13277-015-4708-0. [DOI] [PubMed] [Google Scholar]
- 71.Liu J., Bi J., Li Z., Li Z., Liu X., Kong C. miR-214 reduces cisplatin resistance by targeting netrin-1 in bladder cancer cells. Int. J. Mol. Med. 2018;41:1765–1773. doi: 10.3892/ijmm.2018.3374. [DOI] [PubMed] [Google Scholar]
- 72.Song H., Liu Y., Liang H., Jin X., Liu L. SPINT1-AS1 Drives Cervical Cancer Progression via Repressing miR-214 Biogenesis. Front. Cell Dev. Biol. 2021;9:691140. doi: 10.3389/fcell.2021.691140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sharma T., Hamilton R., Mandal C.C. miR-214: A potential biomarker and therapeutic for different cancers. Future Oncol. 2015;11:349–363. doi: 10.2217/fon.14.193. [DOI] [PubMed] [Google Scholar]
- 74.Han X., Li Q., Liu C., Wang C., Li Y. Overexpression miR-24-3p repressed Bim expression to confer tamoxifen resistance in breast cancer. J. Cell Biochem. 2019;120:12966–12976. doi: 10.1002/jcb.28568. [DOI] [PubMed] [Google Scholar]
- 75.Liu W., Wang S., Zhou S., Yang F., Jiang W., Zhang Q., Wang L. A systems biology approach to identify microRNAs contributing to cisplatin resistance in human ovarian cancer cells. Mol. Biosyst. 2017;13:2268–2276. doi: 10.1039/C7MB00362E. [DOI] [PubMed] [Google Scholar]
- 76.Lai J., Yang H., Zhu Y., Ruan M., Huang Y., Zhang Q. MiR-7-5p-mediated downregulation of PARP1 impacts DNA homologous recombination repair and resistance to doxorubicin in small cell lung cancer. BMC Cancer. 2019;19:602. doi: 10.1186/s12885-019-5798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yu C., Li B., Wang J., Zhang Z., Li S., Lei S., Wang Q. miR-145-5p Modulates Gefitinib Resistance by Targeting NRAS and MEST in Non-Small Cell Lung Cancer. Ann. Clin. Lab. Sci. 2021;51:625–637. [PubMed] [Google Scholar]
- 78.Rajarajan D., Kaur B., Penta D., Natesh J., Meeran S.M. miR-145-5p as a predictive biomarker for breast cancer stemness by computational clinical investigation. Comput. Biol. Med. 2021;135:104601. doi: 10.1016/j.compbiomed.2021.104601. [DOI] [PubMed] [Google Scholar]
- 79.Wan G.X., Cheng L., Qin H.L., Zhang Y.Z., Wang L.Y., Zhang Y.G. MiR-15b-5p is Involved in Doxorubicin-Induced Cardiotoxicity via Inhibiting Bmpr1a Signal in H9c2 Cardiomyocyte. Cardiovasc. Toxicol. 2019;19:264–275. doi: 10.1007/s12012-018-9495-6. [DOI] [PubMed] [Google Scholar]
- 80.Zhao Y., Zhong R., Deng C., Zhou Z. Circle RNA circABCB10 Modulates PFN2 to Promote Breast Cancer Progression, as Well as Aggravate Radioresistance Through Facilitating Glycolytic Metabolism Via miR-223-3p. Cancer Biother. Radiopharm. 2021;36:477–490. doi: 10.1089/cbr.2019.3389. [DOI] [PubMed] [Google Scholar]
- 81.Zhou K., Wei Y., Li X., Yang X. MiR-223-3p targets FOXO3a to inhibit radiosensitivity in prostate cancer by activating glycolysis. Life Sci. 2021;282:119798. doi: 10.1016/j.lfs.2021.119798. [DOI] [PubMed] [Google Scholar]
- 82.Midoux P., Pichon C. Lipid-based mRNA vaccine delivery systems. Expert Rev. Vaccines. 2015;14:221–234. doi: 10.1586/14760584.2015.986104. [DOI] [PubMed] [Google Scholar]
- 83.Ye Q., Wang B., Mao J. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J. Infect. 2020;80:607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fajgenbaum D.C., June C.H. Cytokine Storm. N. Engl. J. Med. 2020;383:2255–2273. doi: 10.1056/NEJMra2026131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sun J.R., Zhang X., Zhang Y. MiR-214 prevents the progression of diffuse large B-cell lymphoma by targeting PD-L1. Cell Mol. Biol. Lett. 2019;24:68. doi: 10.1186/s11658-019-0190-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Li J.A., Wang Y.D., Wang K., Wang Z.L., Jia D.Y., Yang B.Y., Xiong C.B. Downregulation of miR-214-3p May Contribute to Pathogenesis of Ulcerative Colitis via Targeting STAT6. Biomed. Res. Int. 2017;2017:8524972. doi: 10.1155/2017/8524972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang S., Geng Q., Zhang H., Du Q., Wei Q., Cui Y., Zhang X., Yuan M. Downregulation of miR-98-5p expression induces interleukin-6 expression in rheumatoid fibroblast-like synoviocytes. Int. J. Rheum. Dis. 2021;24:1024–1031. doi: 10.1111/1756-185X.14160. [DOI] [PubMed] [Google Scholar]
- 88.Wang Y., Wang N., Cui L., Li Y., Cao Z., Wu X., Wang Q., Zhang B., Ma C., Cheng Y. Long Non-coding RNA MEG3 Alleviated Ulcerative Colitis through Upregulating miR-98-5p-Sponged IL-10. Inflammation. 2021;44:1049–1059. doi: 10.1007/s10753-020-01400-z. [DOI] [PubMed] [Google Scholar]
- 89.Giles K.M., Brown R.A., Ganda C., Podgorny M.J., Candy P.A., Wintle L.C., Richardson K.L., Kalinowski F.C., Stuart L.M., Epis M.R., et al. microRNA-7-5p inhibits melanoma cell proliferation and metastasis by suppressing RelA/NF-κB. Oncotarget. 2016;7:31663–31680. doi: 10.18632/oncotarget.9421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lin Y., Cao H., Tian Y., Yang X., Zhou C., Zhang Q. miR-24-3p stimulates migration, invasion and proliferation of prostate cancer cells by targeting suppressor of cytokine signaling 6. Int. J. Clin. Exp. Pathol. 2018;11:1803–1810. [PMC free article] [PubMed] [Google Scholar]
- 91.Zhuang W., Niu T., Li Z. MicroRNA miR-145-5p regulates cell proliferation and cell migration in colon cancer by inhibiting chemokine (C-X-C motif) ligand 1 and integrin α2. Bioengineered. 2021;12:9909–9917. doi: 10.1080/21655979.2021.2000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wu J., Niu P., Zhao Y., Cheng Y., Chen W., Lin L., Lu J., Cheng X., Xu Z. Impact of miR-223-3p and miR-2909 on inflammatory factors IL-6, IL-1ß, and TNF-α, and the TLR4/TLR2/NF-κB/STAT3 signaling pathway induced by lipopolysaccharide in human adipose stem cells. PLoS ONE. 2019;14:e0212063. doi: 10.1371/journal.pone.0212063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fu Y., Wang C., Zhang D., Chu X., Zhang Y., Li J. miR-15b-5p ameliorated high glucose-induced podocyte injury through repressing apoptosis, oxidative stress, and inflammatory responses by targeting Sema3A. J. Cell Physiol. 2019;234:20869–20878. doi: 10.1002/jcp.28691. [DOI] [PubMed] [Google Scholar]
- 94.Tribolet L., Kerr E., Cowled C., Bean A.G.D., Stewart C.R., Dearnley M., Farr R.J. MicroRNA Biomarkers for Infectious Diseases: From Basic Research to Biosensing. Front. Microbiol. 2020;11:1197. doi: 10.3389/fmicb.2020.01197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Galvão-Lima L.J., Morais A.H.F., Valentim R.A.M., Barreto E. miRNAs as biomarkers for early cancer detection and their application in the development of new diagnostic tools. Biomed. Eng. Online. 2021;20:21. doi: 10.1186/s12938-021-00857-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Walter E., Dellago H., Grillari J., Dimai H.P., Hackl M. Cost-utility analysis of fracture risk assessment using microRNAs compared with standard tools and no monitoring in the Austrian female population. Bone. 2018;108:44–54. doi: 10.1016/j.bone.2017.12.017. [DOI] [PubMed] [Google Scholar]
- 97.Bonneau E., Neveu B., Kostantin E., Tsongalis G.J., De Guire V. How close are miRNAs from clinical practice? A perspective on the diagnostic and therapeutic market. Ejifcc. 2019;30:114–127. [PMC free article] [PubMed] [Google Scholar]
- 98.Zost S.J., Gilchuk P., Case J.B., Binshtein E., Chen R.E., Nkolola J.P., Schäfer A., Reidy J.X., Trivette A., Nargi R.S., et al. Potently neutralizing and protective human antibodies against SARS-CoV-2. Nature. 2020;584:443–449. doi: 10.1038/s41586-020-2548-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.De Gonzalo-Calvo D., Benítez I.D., Pinilla L., Carratalá A., Moncusí-Moix A., Gort-Paniello C., Molinero M., González J., Torres G., Bernal M., et al. Circulating microRNA profiles predict the severity of COVID-19 in hospitalized patients. Transl. Res. 2021;236:147–159. doi: 10.1016/j.trsl.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fayyad-Kazan M., Makki R., Skafi N., El Homsi M., Hamade A., El Majzoub R., Hamade E., Fayyad-Kazan H., Badran B. Circulating miRNAs: Potential diagnostic role for coronavirus disease 2019 (COVID-19) Infect Genet Evol. 2021;94:105020. doi: 10.1016/j.meegid.2021.105020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.El-Nabi S.H., Elhiti M., El-Sheekh M. A new approach for COVID-19 treatment by micro-RNA. Med. Hypotheses. 2020;143:110203. doi: 10.1016/j.mehy.2020.110203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Paul S., Bravo Vázquez L.A., Reyes-Pérez P.R., Estrada-Meza C., Aponte Alburquerque R.A., Pathak S., Banerjee A., Bandyopadhyay A., Chakraborty S., Srivastava A. The role of microRNAs in solving COVID-19 puzzle from infection to therapeutics: A mini-review. Virus Res. 2022;308:198631. doi: 10.1016/j.virusres.2021.198631. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.