Abstract
Purpose:
To report the barriers for seeking eye care among the elderly population aged ≥60 years with avoidable vision impairment (VI) in the South Indian state of Telangana.
Methods:
A total of 3640 participants aged ≥60 years were recruited using cluster-random sampling. Demographic information, including presenting visual acuity, was measured using the standard Rapid Assessment of Visual Impairment (RAVI) protocol. “Avoidable VI” was considered if the VI was due to cataract or uncorrected refractive error (URE). A detailed interview was conducted using a validated questionnaire to report the barriers for not seeking eye care. Data were analyzed using the Stata statistical software version 14.
Results:
Prevalence of avoidable VI was 30.2% (95% CI: 28.02–31.06; n = 1102). Among those who noticed decreased vision (n = 1074), only 392 participants (36.4%) reported that they felt the need for seeking eye care. The major barriers for not seeking eye care were: cannot afford the consultation fee and services (42.0%) and no escort (25.7%). Overall, the personal barriers (57.9%) were the major reason for not seeking care, followed by economic barriers (42.0%). No significant difference was reported in barriers between the participants with unilateral and bilateral VI (>0.05).
Conclusion:
Overall, among the elderly people, personal and economic barriers were the major reason for not seeking eye care. Health care providers and policymakers should focus on newer models of eye care delivery to ensure better accessibility and uptake of care by the elderly people.
Keywords: Barriers, elderly, population-based study, Telangana, visual impairment
Globally, more than a billion people have vision impairment (VI). It is estimated that over 1.8 billion people will be visually impaired by 2050.[1] VI burden significantly varies with socioeconomic status in different regions, gender, and older age groups.[2] Over 70% of global VI is correctable and treatable by a pair of glasses and safe cataract surgery.[3] Marmamula et al.[4] reported that one in three elderly people had VI in the state of Telangana, of which 88.2% was due to avoidable causes.
Low uptake of available services by the community was one of the major challenges to blindness prevention initiatives. Studies among the Indian population reported low uptake of eye care services. It was more among the rural population and persons with unilateral VI.[5,6,7,8] Financial barriers were the major reason for not seeking care among the urban population.[7,9,10] Among the rural population, in addition to financial barriers, other barriers such as no escort, God’s will, and fear of surgery/treatment were reported.[6,11,12,13] There was a significant difference between the barriers reported by the urban and rural populations,[10] and by the unilateral and bilateral VI participants.[8,14]
The elderly population has limited access to care. Understanding and addressing these barriers can help in achieving universal eye health in the elderly. Most of the available literature on barriers to eye care was reported among those aged ≥15 years,[6,7,9,10,11,12] and limited data are available on aged ≥50 years.[8,13,14,15] The present study aims to identify the barriers to seeking eye care among those aged ≥60 years (elderly).
Methods
The study protocol was approved by the Institutional Review Board (IRB) of Hyderabad Eye Research Foundation, L V Prasad Eye Institute, India. After taking the informed consent, the participants were enrolled. The study protocol adhered to the tenets of the Declaration of Helsinki. The data sets consisted of patients aged ≥60 years from the Rapid Assessment of Visual Impairment (RAVI) studies conducted between 2014 and 2017.[16,17] The major findings from these combined datasets were published elsewhere.[18]
Three teams, each comprising one vision technician and trained field staff, were involved in data collection. The sampling strategy and households enumerated for data collection have already been published.[16,17,18] In brief, the cluster-random sampling method was used to select the clusters from Adilabad, Mahabubnagar, Khammam, and Warangal districts of South India. The eye examination protocol included collecting sociodemographic data, spectacles use, visual acuity measurement for distance and near, anterior segment examination, and fundus imaging (Zeiss Visuscout 100 or 3Netra Classic, Forus Health). The detailed eye examination procedures and VI definitions (bilateral and unilateral) used in RAVI studies have been published.[8,16,17,18] VI was defined as presenting visual acuity worse than 6/18 in the better eye. VI due to cataract and uncorrected refractive errors (UREs) were considered avoidable causes of VI.
Participants were interviewed using a structured questionnaire to assess the barriers for uptake of eye care services.[8] First, the participants were asked whether they experienced decreased vision in the last 5 years. If they responded yes, then they were asked whether they sought any consultation and treatment. Those who did not seek care were further questioned on the reasons for not seeking care. If the participants gave multiple reasons, the interviewer further probed to identify the “primary reason” which was recorded. The response was recorded as “other reasons” if not listed in the questionnaire. The cost-related barriers—cannot afford consultation fees and services were grouped under economic barriers. Remaining barriers such as no escort, fear, other health issues, no time/other priorities, waiting for cataract surgery, and others were grouped as personal barriers for the analysis.
Data management and statistical analysis
Data were collected in paper forms, entered in a central database in Microsoft Access, and then analyzed using the Stata 14.0 software package (Stata Corp., College Station, Texas, USA).[19] Avoidable VI and barriers in accessing eye care were reported using descriptive statistics. A ”Z-test” of proportions was used to compare the barriers between unilateral and bilateral VI. The Chi-square test was used to compare economic and social barriers with demographic variables. The statistical significance level was set at P < 0.05.
Results
In total, 3,640 individuals aged ≥60 years participated in the study (mean age: 67.7 ± 6.9 years). Two-thirds of the participants had no formal education (78.0%; n = 2842), and more than half were women (53.1%; n = 1933). The prevalence of avoidable VI was 30.2% (95% CI: 28.02–31.06; n = 1102).
Fig. 1 shows the flowchart of barrier responses recorded from the participants. Among those with avoidable VI (n = 1102), a total of 28 participants (2.54%) were not aware of their existing VI condition. Among those with noticed vision loss (n = 1074), a lack of felt need was seen in 682 (63.5%) participants. The major reasons for lack of felt need were: can manage (61.2%, n = 418), old age (38.7%, n = 264), and one eye has an adequate vision (0.14%, n = 5). Among those who noticed vision loss, the felt need was seen in 392 (36.50%) participants only.
Figure 1.
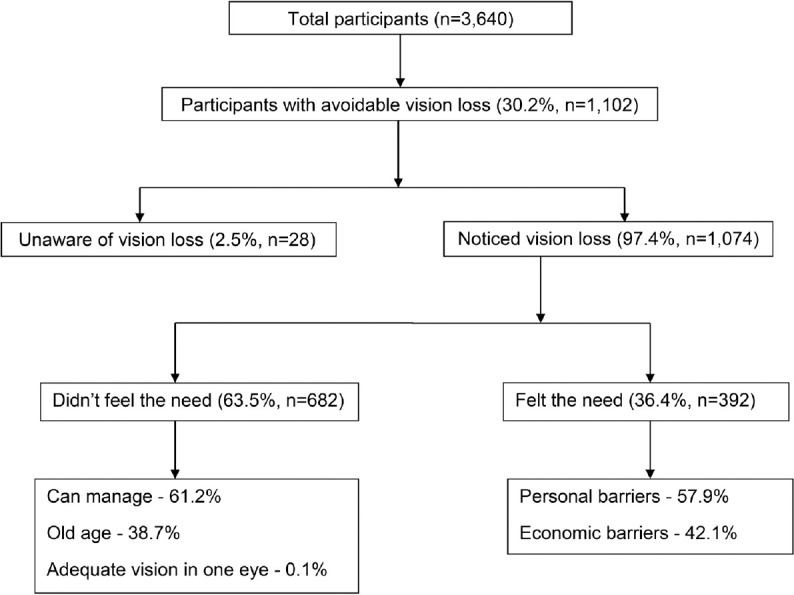
Flowchart shows the barriers analyzed among the participants with bilateral VI
Barriers among the participants with avoidable bilateral and unilateral VI are shown in Fig. 2. Among the participants with bilateral VI, the single largest barrier was “could not afford consultation fees and services” (42%, n = 165). The other major barriers included no escort (25.7%, n = 101) and fear (10.9%, n = 43). About 8.9% (n = 35) of participants had other health issues that prevented them from seeking care; this indicates comorbidities among the elderly. Among the unilateral VI participants (34.9%, n = 856), 23 (2.6%) participants were unaware of the existing VI condition. Among those with noticed vision loss (n = 833), 529 (63.5%) participants reported a lack of felt need. Reasons for the lack of felt need were as follows: can manage (56.8%, n = 301), old age (27.7%%, n = 147), and adequate vision in one eye (15.3%, n = 81). Among felt need participants with unilateral VI (36.4%, n = 304), “cannot afford consultation fees and services” (42.1%, n = 128) and “no escort” (14.8%, n = 45) were the major barriers for not seeking eye care. Barriers were not significantly different between the bilateral and unilateral VI participants (P > 0.05). Overall, the personal barriers were significantly higher than economic barriers (57.9% vs. 42.0%) in participants with bilateral VI (P = 0.0034). A similar difference was seen between personal and economic barriers (57.8% vs. 42.1%) among participants with unilateral VI (P = 0.0098).
Figure 2.
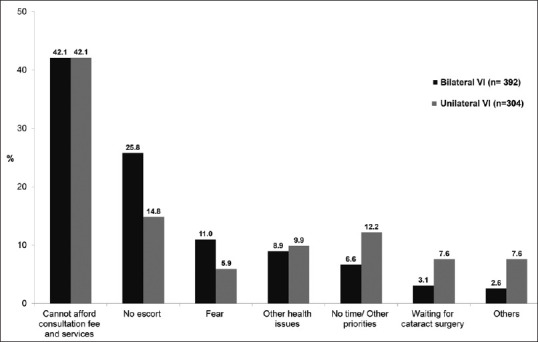
Shows the barriers among the participants with bilateral and unilateral VI
Table 1 shows a comparison of barriers with bilateral VI participant demographic profile. Economic and personal barriers were significantly varied with the cause of VI and study districts (P < 0.05).
Table 1.
Comparison of economic and personal barriers with bilateral VI participant demographic variables
| Economic barriers (n=165)# | Personal barriers (n=227)# | P | |
|---|---|---|---|
| Age (years) | |||
| 60-69 | 93 (56.3) | 121 (53.3) | 0.54 |
| 70-79 | 58 (35.1) | 76 (33.5) | 0.73 |
| 80-89 | 14 (8.4) | 30 (13.2) | 0.14 |
| Gender | |||
| Male | 71 (43.0) | 103 (45.4) | |
| Female | 94 (56.9) | 124 (54.6) | 0.64 |
| Cause of VI | |||
| URE | 81 (49.0) | 79 (34.8) | 0.004* |
| Cataract | 84 (50.9) | 148 (65.2) | |
| Area | |||
| Adilabad | 37 (22.4) | 26 (11.4) | 0.004* |
| Mahabubnagar | 5 (3.0) | 12 (5.3) | 0.27 |
| Khammam | 48 (29.0) | 93 (41.0) | 0.016* |
| Warangal | 75 (45.4) | 96 (42.3) | 0.23 |
| Education | |||
| No education | 152 (92.1) | 197 (86.8) | 0.095 |
| Any education | 13 (7.8) | 30 (13.2) |
#Column percentages, * P<0.05, VI=Vision Impairment, URE=Uncorrected Refractive Error
Discussion
Overall, more than half of the elderly people did not seek eye care due to personal barriers. One in four elderly were unable to seek eye care services as no one was there to accompany them. Despite noticing decreased vision, felt need was seen in only one-third of the participants. However, the felt need was highest in the 60–69 age group (54.5%) compared to older age groups. This higher proportion of felt need in this age group is likely because they are still involved in active work. However, other studies have reported lower felt need in this study group compared to our study.[7,9,10,12,20] These differences possibly are due to the population investigated (rural vs. urban), study location (north and south India), and causes investigated (visual impairment, refractive services, etc.).
Economic barriers were the single largest reason for not accessing eye care. These results are consistent with published literature.[7,9,10,11,12,21] Other studies from South India have also reported that “no money” is the major reason for not seeking care in more than two-thirds of the participants.[6] Similar results have also been reported from other low- and middle-income countries.[20,22,23,24] This highlights the fact that there is a need for governments and NGOs to develop cost-effective eye care delivery models for overcoming cost-related barriers. In South India, cost-efficient models of eye care delivery systems are in practice and should be replicated across the country.[25,26] Additionally, these models reduce the indirect costs as the services are available within their local communities.[27] Despite these cost-effective eye care delivery models, the uptake of eye care services in this region is low. To increase the uptake, there is a need to organize eye health activities to educate the local communities about the available eye care services and increase awareness. From the inception of the National Program for Control of Blindness (NPCB) in 1976, significant progress has been made in addressing blindness by making eye care services accessible.[28] The national-level blindness prevention programs were complemented by the Vision 2020 initiative, a global initiative aimed at eliminating needless blindness.[29] As a result of these initiatives, the cataract surgical rate (CSR) has significantly increased over the last decades. However, it is still lagging behind the optimal CSR target set to bring down the cataract disease burden in India.[30,31,32] To reduce the disease burden, the Government of India (GOI) is providing grants for performing cataract surgeries and establishing regional institutes and vision centers.[31] Additionally, it is facilitating the training of eye care professionals to meet the human resources need to provide quality eye care services.[31] In addition to the cataract burden, UREs are also the major burden of visual impairment. As reported by Senjam et al., one of the major barriers for seeking refractive error services among the elderly was a lack of felt need, followed by they were not comfortable wearing spectacles.[9]
“No escort” was another major barrier in accessing eye care. It was an expected finding as the elderly have associated mobility issues, and possibly living alone makes them depend on an escort for seeking care. Nirmalan et al.[6] reported “no one was there to accompany” as one of the major barriers (rated by 58.2% participants) in seeking care. However, other studies have reported that escort was not a major barrier.[7,10,11] In addition to the escort barrier, other health issues in the elderly significantly affect eye care-seeking behavior.
To address this barrier, we should look for alternate models for reaching out to these elderly. L V Prasad Eye Institute (LVPEI) recently launched LVPEI Silver Sight Initiative in providing eye care on-call. Particularly useful in COVID-19 times, the model has helped to provide eye care to the elderly right at their homes.[33] Recently, teleophthalmology has also gained momentum. It has emerged as a promising alternative strategy for emergency and follow-up care for the elderly at their doorstep combined with home care.[34] In the government sector, Ayushman Bharat and Prime Minister Jan Arogya Yojna (PMJAY) offer cashless medical care, which is likely to enhance eye care-seeking behavior, particularly in the elderly, and to contribute to better service uptake.[35]
Utilization of available services is key to eliminating the burden of VI. Among personal barriers, fear was another main barrier for low utilization of services in the elderly in this study. The South Indian rural population reported fear as the main barrier—almost 2.5 times more compared to the present study.[6] Fear has also been reported in other studies done in the rest of India.[20,36,37] The reason for fear could be that most of the study participants were illiterate and may have witnessed bad surgical outcomes among their known family members.[6] The other possible reasons include postoperative care and loss of wages because of the surgery. Many are not aware of the currently available safe eye care procedures. Thus, blindness prevention programs need to be included in eye health education programs to address the barriers related to fear.
“Have to travel far for eye check-up” was reported as one of the “other reasons.” Although the fact that the study location was in rural India, this reason was rated low. As this study was undertaken within a radius of 30–50 km from LVPEI and its partner network hospitals, the results may not represent the actual scenario of rural India. These centers are accessible to the communities, and the cross-subsidy model provides free eye care services to the needy.[25,26] In contrast, “services are too far away” was the main barrier in other low- and middle-income countries.[23,38] Consistent with the published literature, among the unilateral VI participants, economic reasons were perceived as the main barriers to seeking eye care.[8] Similarly, as reported in published literature, the escort barrier was relatively lower among unilateral VI compared to those with bilateral VI.[8,39]
This is the first study to exclusively report the barriers among a large cohort of the elderly. Extrapolation of these findings is possible given the large sample taken from more than 1/3 of the total districts in Telangana (10 old districts). The population-based cluster-random sampling is another strength of this study. The major limitation of this study is that it provides only the barriers but not the solutions/enablers for seeking eye care.
Given the aging population in India, coupled with economic and access-related barriers, the utilization of eye care in the elderly can be significantly affected. Our previous publication highlighted the VI in the elderly.[18] The present study findings highlight the need for a comprehensive approach to address the barriers to accessing eye care by the elderly. Health care policymakers and eye care providers should focus on developing dedicated geriatric eye clinics for better accessibility of eye care by the elderly. Additionally, cost-effective models such as eye care at home and the use of teleophthalmology are solutions to overcome these reported barriers.
Conclusion
Economic and personal barriers significantly influence the eye care-seeking behavior in the elderly. Understanding and addressing these barriers will offer alternative models to make eye care accessible for the elderly.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: An analysis for the global burden of disease study. Lancet Glob Health. 2021;9:e130–43. doi: 10.1016/S2214-109X(20)30425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The lancet global health commission on global eye health: Vision beyond 2020. Lancet Glob Health. 2021;9:e489–551. doi: 10.1016/S2214-109X(20)30488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The right to sight: An analysis for the global burden of disease study. Lancet Glob Health. 2021;9:e144–60. doi: 10.1016/S2214-109X(20)30489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marmamula S, Barrenakala NR, Challa R, Kumbham TR, Modepalli SB, Yellapragada R, et al. Prevalence and risk factors for visual impairment among elderly residents in 'homes for the aged' in India: The Hyderabad ocular morbidity in elderly study (HOMES) Br J Ophthalmol. 2021;105:32–6. doi: 10.1136/bjophthalmol-2019-315678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fletcher AE, Donoghue M, Devavaram J, Thulasiraj RD, Scott S, Abdalla M, et al. Low uptake of eye services in rural India: A challenge for programs of blindness prevention. Arch Ophthalmol. 1999;117:1393–9. doi: 10.1001/archopht.117.10.1393. [DOI] [PubMed] [Google Scholar]
- 6.Nirmalan PK, Katz J, Robin AL, Krishnadas R, Ramakrishnan R, Thulasiraj RD, et al. Utilisation of eye care services in rural south India: The Aravind comprehensive eye survey. Br J Ophthalmol. 2004;88:1237–41. doi: 10.1136/bjo.2004.042606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dandona R, Dandona L, Naduvilath TJ, McCarty CA, Rao GN, et al. Utilisation of eyecare services in an urban population in southern India: The Andhra Pradesh eye disease study. Br J Ophthalmol. 2000;84:22–7. doi: 10.1136/bjo.84.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marmamula S, Giridhar P, Khanna RC, et al. Utilization of eye care services among those with unilateral visual impairment in rural South India: Andhra Pradesh eye disease study (APEDS) Int J Ophthalmol. 2017;10:473–9. doi: 10.18240/ijo.2017.03.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Senjam SS, Vashist P, Gupta N, Malhotra S, Misra V, Bhardwaj A, et al. Prevalence of visual impairment due to uncorrected refractive error: Results from delhi-rapid assessment of visual impairment study. Indian J Ophthalmol. 2016;64:387–90. doi: 10.4103/0301-4738.185614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marmamula S, Khanna RC, Shekhar K, Rao GN, et al. A population-based cross-sectional study of barriers to uptake of eye care services in South India: The rapid assessment of visual impairment (RAVI) project. BMJ Open. 2014;4:e005125. doi: 10.1136/bmjopen-2014-005125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kovai V, Krishnaiah S, Shamanna BR, Thomas R, Rao GN, et al. Barriers to accessing eye care services among visually impaired populations in rural Andhra Pradesh, South India. Indian J Ophthalmol. 2007;55:365–71. doi: 10.4103/0301-4738.33823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malhotra S, Kalaivani M, Rath R, Prasad M, Vashist P, Gupta N, et al. Use of spectacles for distance vision: Coverage, unmet needs and barriers in a rural area of North India. BMC Ophthalmol. 2019;19:252. doi: 10.1186/s12886-019-1262-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chandrashekhar TS, Bhat HV, Pai RP, Nair SK, et al. Coverage, utilization and barriers to cataract surgical services in rural South India: Results from a population-based study. Public Health. 2007;121:130–6. doi: 10.1016/j.puhe.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 14.Kovai V, Prasadarao BV, Paudel P, Stapleton F, Wilson D, et al. Reasons for refusing cataract surgery in illiterate individuals in a tribal area of Andhra Pradesh, India. Ophthalmic Epidemiol. 2014;21:144–52. doi: 10.3109/09286586.2014.903980. [DOI] [PubMed] [Google Scholar]
- 15.Kumar SGP, Mondal A, Vishwakarma P, Kundu S, Lalrindiki R, Kurian E, et al. Factors limiting the Northeast Indian elderly population from seeking cataract surgical treatment: Evidence from Kolasib district, Mizoram, India. Indian J Ophthalmol. 2018;66:969–74. doi: 10.4103/ijo.IJO_1184_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marmamula, Khanna RC, Kunkunu E, Rao GN, et al. Population-based assessment of prevalence and causes of visual impairment in the state of Telangana, India: A cross-sectional study using the rapid assessment of visual impairment (RAVI) methodology. BMJ Open. 2016;6:e012617. doi: 10.1136/bmjopen-2016-012617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marmamula SS, Khanna RC, Yellapragada S, Challa R, Mohd J, Rao GN, et al. Temporal trends in the prevalence and causes of visual impairment in the South Indian state of Telangana: A population-based cross-sectional study. BMJ Open. 2019;9:e029114. doi: 10.1136/bmjopen-2019-029114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marmamula S, Challa R, Khanna RC, Kunkunu E, Rao GN, et al. Population-based assessment of vision impairment in the elderly population in Telangana State in India-policy implications for eye health programmes. Ophthalmic Epidemiol. 2021;28:144–51. doi: 10.1080/09286586.2020.1797122. [DOI] [PubMed] [Google Scholar]
- 19.StataCorp. College Station, TX: StataCorp LP; 2014. Stata Statistical Software: Release 14. [Google Scholar]
- 20.Ahmad K, Zwi AB, Tarantola DJ, Chaudhry TA, et al. Self-perceived barriers to eye care in a hard-to-reach population: The Karachi marine fishing communities eye and general health survey. Invest Ophthalmol Vis Sci. 2015;56:1023–32. doi: 10.1167/iovs.14-16019. [DOI] [PubMed] [Google Scholar]
- 21.Khanna RC, Kim S, Giridhar P, Mettla AL, Marmamula S, Rao GN, et al. Barriers to uptake of referral services from secondary care to tertiary care and its associated factors in L V Prasad Eye Institute network in Southern India: A cross-sectional study. BMJ Open. 2018;8:e020687. doi: 10.1136/bmjopen-2017-020687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ndegwa LK, Karimurio J, Okelo RO, Adala HS, et al. Barriers to utilisation of eye care services in Kibera slums of Nairobi. East Afr Med J. 2005;82:506–8. doi: 10.4314/eamj.v82i10.9347. [DOI] [PubMed] [Google Scholar]
- 23.Wubben TJ, Guerrero CM, Salum M, Wolfe GS, Giovannelli GP, Ramsey DJ, et al. Presbyopia: A pilot investigation of the barriers and benefits of near visual acuity correction among a rural Filipino population. BMC Ophthalmol. 2014;14:9. doi: 10.1186/1471-2415-14-9. doi: 10.1186/1471-2415-14-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laviers HR, Omar F, Jecha H, Kassim G, Gilbert C, et al. Presbyopic spectacle coverage, willingness to pay for near correction, and the impact of correcting uncorrected presbyopia in adults in Zanzibar, East Africa. Invest Ophthalmol Vis Sci. 2010;51:1234–41. doi: 10.1167/iovs.08-3154. [DOI] [PubMed] [Google Scholar]
- 25.Rao GN, Khanna RC, Athota SM, Rajshekar V, Rani PK. Integrated model of primary and secondary eye care for underserved rural areas: The L V Prasad Eye Institute experience. Indian J Ophthalmol. 2012;60:396–400. doi: 10.4103/0301-4738.100533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehta MC, Narayanan R, Thomas Aretz H, Khanna R, Rao GN, et al. The L V Prasad Eye Institute: A comprehensive case study of excellent and equitable eye care. Healthc (Amst) 2020;8:100408. doi: 10.1016/j.hjdsi.2019.100408. doi: 10.1016/j.hjdsi.2019.100408. [DOI] [PubMed] [Google Scholar]
- 27.Khanna RC, Sabherwal S, Sil A, Gowth M, Dole K, Kuyyadiyil S, Chase H, et al. Primary eye care in India-The vision center model. Indian J Ophthalmol. 2020;68:333–9. doi: 10.4103/ijo.IJO_118_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Verma R, Khanna P, Prinja S, Rajput M, Arora V, et al. The national programme for control of blindness in India. Australas Med J. 2011;4:1–3. doi: 10.4066/AMJ.2011.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ackland P, et al. The accomplishments of the global initiative VISION 2020: The right to sight and the focus for the next 8 years of the campaign. Indian J Ophthalmol. 2012;60:380–6. doi: 10.4103/0301-4738.100531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vs Murthy G, Jain B, Shamanna B, Subramanyam D, et al. Improving cataract services in the Indian context. Community Eye Health. 2014;27:4–5. [PMC free article] [PubMed] [Google Scholar]
- 31.Vemparala R, Gupta P, et al. National programme for control of blindness (NPCB) in the 12th five year plan: An overview. Delhi J Ophthalmol. 2017;27:290–2. [Google Scholar]
- 32.Honavar SG, et al. Eliminating cataract blindness: Are we on target? Indian J Ophthalmol. 2017;65:1271–2. doi: 10.4103/ijo.IJO_1190_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marmamula S, Yanamala NK, Khanna RC. “Eyecare on call” -Extending the frontiers of care through home-based eye care-Concept and the protocol. Indian J Ophthalmol. 2020;68:2625–7. doi: 10.4103/ijo.IJO_2352_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Das AV, Mididoddi S, Kammari P, Deepthi Davara N, Loomba A, Khanna R, et al. App-based tele ophthalmology: A novel method of rural eye care delivery connecting tertiary eye care center and vision centers in India. Int J Telemed Appl. 2019;2019:8107064. doi: 10.1155/2019/8107064. doi: 10.1155/2019/8107064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kumar A, Vashist P, et al. Indian community eye care in 2020: Achievements and challenges. Indian J Ophthalmol. 2020;68:291–3. doi: 10.4103/ijo.IJO_2381_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ormsby GM, Mörchen M, Fotis K, Skiba DG, Chim C, Keeffe JE, et al. Barriers to the uptake of cataract surgery and eye care after community outreach screening in Takeo Province, Cambodia. Asia Pac J Ophthalmol (Phila) 2017;6:266–72. doi: 10.22608/APO.2015127. [DOI] [PubMed] [Google Scholar]
- 37.du Toit R, Ramke J, Naduvilath T, Brian G, et al. Awareness and use of eye care services in Fiji. Ophthalmic Epidemiol. 2006;13:309–20. doi: 10.1080/09286580600826629. [DOI] [PubMed] [Google Scholar]
- 38.Lee L, Ramke J, Blignault I, Casson RJ, et al. Changing barriers to use of eye care services in Timor-Leste: 2005 to 2010. Ophthalmic Epidemiol. 2013;20:45–51. doi: 10.3109/09286586.2012.742551. [DOI] [PubMed] [Google Scholar]
- 39.Vaidyanathan K, Limburg H, Foster A, Pandey RM, et al. Changing trends in barriers to cataract surgery in India. Bull World Health Organ. 1999;77:104–9. [PMC free article] [PubMed] [Google Scholar]


