Abstract
A 36-year-old female presented with blurring of vision in one eye for 10 days after 1 month of an episode of COVID-19 infection. Her fundus showed disc edema with blurring of margins along with exudation around the fovea. Her C-reactive protein levels were raised. She responded well to oral steroids. A likely association with COVID-19 infection and its associated immune response was suspected.
Keywords: COVID-19, disc edema, neuro-retinitis
Coronavirus is a family of viruses that can cause common cold, severe acute respiratory syndrome (SARS), and the Middle East respiratory syndrome (MERS). In 2019, a new virus was identified in China, namely novel coronavirus disease 2019 (COVID-19), and on March 11, 2020, the World Health Organization characterized COVID-19 as a pandemic. Neurotropic and neuroinvasive capabilities of coronaviruses have been described in humans. In a retrospective case series conducted in Wuhan, China, 36.4% of hospitalized patients had nervous system signs and symptoms.[1] In another study by Chou et al.[2] this percentage went up to 80% of hospitalized patients.
As the pandemic is evolving, SARS-CoV-2-associated neuro-ophthalmic manifestations are being reported frequently. The main mechanisms that have been hypothesized for COVID-19-related neuro-ophthalmic disease include the direct invasion of the neuronal tissue by the neurotropic SARS-CoV-2 virus due to the presence of ACE-2 receptors in the neuronal tissue and blood vessels. There have been multiple reports of COVID-19-associated neuro-ophthalmic manifestations, including optic neuritis, papilledema, posterior reversible encephalopathy syndrome (PRES), cranial neuropathy, arterial and venous occlusion, nystagmus, visual field defects, and neuromuscular junction disorders.
Here we present a case of neuro-retinitis associated with COVID-19 infection.
Case Report
A 36-year-old female presented with a history of blurring of vision in the left eye noticed for 10 days. She had a history of mild COVID-19 disease about 1 month ago, confirmed with RT-PCR, which was treated with oral medications and home isolation. She had no significant systemic issues.
On presentation, she had a visual acuity of 20/20 in the right eye and 20/40 in the left eye. Color vision and contrast were within normal limits in both eyes. On slit-lamp evaluation, the anterior segment was within normal limits. The left eye disc showed blurring of disc margins and obscuration of vessels. The macula showed exudation on the nasal aspect [Fig. 1a]. HVF 30-2 showed an enlargement of the blind spot [Fig. 1b]. SS-OCT of the macula showed some exudates in the outer plexiform layer [Fig. 1c]. Blood investigations showed an elevated CRP. Serum ACE, serum calcium, chest X-ray for tuberculosis, VDRL, Bartonella serology, and serum ENA profile for autoimmune markers were all within normal limits. Hba1c and blood pressure were also within normal limits. A provisional diagnosis of post-COVID-19-neuroretinitis was made and the patient was started on oral steroids.
Figure 1.
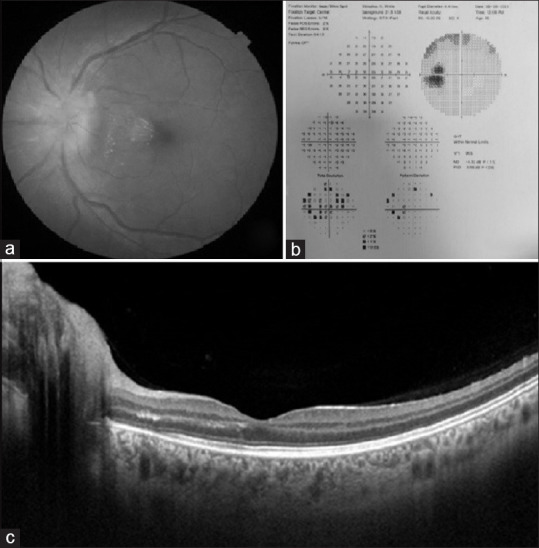
(a) Fundus clinical picture of the patient at presentation; (b) HVF 30-2 of the patient showing an enlargement of the blind spot (c) SS-OCT of the macula showing some exudation in the outer plexiform layer
After 2 weeks of oral steroids, the visual acuity started recovering, and there was a significant decrease in the disc edema. The steroids were tapered and stopped over 6 weeks with complete resolution of edema and improvement in vision to 20/20p [Fig. 2].
Figure 2.
(a) Fundus clinical picture at presentation; (b) Fundus clinical picture at 2 weeks; (c) Fundus clinical picture at 6 weeks
Discussion
Neuroretinitis is a type of optic neuropathy characterized by an acute unilateral visual loss in the setting of optic disc swelling accompanied by hard exudates characteristically arranged in a star shape around the fovea.
The etiopathology of neuroretinitis is obscure. Neuroretinitis is thought to be an infectious or immune-mediated process that may be precipitated by a number of different agents. Commonly associated with an antecedent viral syndrome, in up to 50% of cases, the proposed causative viral agents include herpes simplex, hepatitis B, mumps, and the herpes viruses. Other infectious causes include spirochetosis, especially syphilis, Lyme disease, and leptospirosis.
In the human airways, HCoV infection may lead to the disruption of the nasal epithelium. A significant amount of viruses is also released from the basolateral side. Thus, they may pass through the epithelium barrier and reach the bloodstream or lymph and propagate toward the CNS. Moreover, persistently-infected leukocytes may serve as a reservoir and vector for neuroinvasive HCoV.
The presence of ACE2 receptors in neural cells appears to be critical for the neurotropism of the novel coronavirus using protein S. SARS-CoV-2 uses the spike protein S1 to attach to the host cell ACE2 receptor. ACE2 is a carboxy-peptidase responsible for the formation of vasodilatory peptides such as angiotensin-(1-7). ACE2 mRNA is present not only in alveolar epithelial cells but also expressed widely throughout the CNS. The direct invasive property seems to be a less likely mechanism for the neuro-ophthalmic manifestations of the virus.
SARS-CoV-2 infection is also known to cause cytokine storm with the elevation of pro-inflammatory cytokines. This exaggerated immune response may cause direct tissue damage or lead to hypercoagulability by activating the coagulation cascade. Elevation of serum inflammatory markers such as C-reactive protein (CRP), ferritin, erythrocyte sedimentation rate (ESR), D-dimer, fibrinogen, lactate dehydrogenase thrombocytopenia, and prolonged prothrombin time (PT)/international normalized ratio (INR) have been seen in patients of severe COVID-19. The state of hyper-inflammation provoked by maladaptive innate immunity may activate CNS intrinsic immune pathways and induce para-infectious autoimmunity. This mechanism may account for some of the suspected neuro-ophthalmologic associations, such as optic neuritis.
COVID-19 has also been known to trigger myelin oligodendrocyte glycoprotein antibody-associated optic neuritis and myelin oligodendrocyte glycoprotein and neuromyelitis optica/aquaporin-4 antibody negative COVID-19-associated optic neuritis through an auto-immune mechanism.[3]
In our patient, the onset of symptoms in the subacute recovery phase after the COVID-19 symptoms and a good response to steroids suggest a post-infectious immune response. However, we do acknowledge that this association may have been coincidental.
Conclusion
Many neuro-ophthalmic manifestations have been reported in association with HCoV, including visual impairment, ophthalmoplegia, facial nerve palsy, nystagmus, pupillary defects, and optic neuritis. Hosseini et al.[4] reported a case of bilateral panueveitis and neuroretinitis in a patient 1 month after an episode of COVID-19 infection. Since then, multiple similar presentations have emerged. Here we report another case of neuroretinitis in association with COVID-19.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–90. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chou SH, Beghi E, Helbok R, Moro E, Sampson J, Altamirano V, et al. Global incidence of neurological manifestations among patients hospitalized with COVID-19— A report for the GCS-NeuroCOVID consortium and the ENERGY consortium. JAMA Netw Open. 2021;4:e2112131. doi: 10.1001/jamanetworkopen.2021.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou S, Jones-Lopez EC, Soneji DJ, Azevedo CJ, Patel VR, et al. Myelin oligodendrocyte glycoprotein antibody-associated optic neuritis and myelitis in COVID-19. J Neuroophthalmol. 2020;40:398–402. doi: 10.1097/WNO.0000000000001049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hosseini SM, Abrishami M, Zamani G, Hemmati A, Momtahen S, Hassani M, et al. Acute bilateral neuroretinitis and panuveitis in a patient with coronavirus disease 2019: A case report. Ocul Immunol Inflamm. 2021;29:677–80. doi: 10.1080/09273948.2021.1894457. [DOI] [PubMed] [Google Scholar]



