Abstract
Background
This study aims to confirm validity and reliability of the Hungarian version of Fear of COVID-19 Scale (FCV-19S) and evaluate its dimensional structure.
Methods
Cross-sectional survey was carried out in 2021 among Hungarian general population. In addition to classical test theory methods, construct dimensionality of FCV-19S was assessed using EFA with principal axis factoring method and CFA with diagonally-weighted least squares estimation. Fear score was compared in age, gender, educational level, vaccination and infection subgroups.
Results
Significant differences in FCV-19S mean scores were observed between three subgroups (age, gender, vaccination). Items showed good internal consistency (Cronbach α = 0.88). EFA identified two latent factors (eig = 4.2 and 1.02), though parallel analysis supports the one-factor model. The two-dimensional structure was confirmed by CFA, items 3,4,6,7 correlated with Factor 1 (physiological fear), items 1,2,5 with Factor 2 (emotional fear).
Conclusion
The Hungarian version of FCV-19S seems valid and reliable. The EFA identified two-latent factors (emotional and physiological fear), that was confirmed by CFA. The two-factor structure had better model fit, though its’ acceptance is limited.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-022-13789-3.
Keywords: COVID-19, Fear, Confirmatory factor analysis, Hungarian FCV-19S, Psychometrics
Introduction
The COVID-19 pandemic raised rapid public health emergency globally from its appearance in December 2019. Hungary imposed containment phase in 2020 March, to prevent steep shift in epidemiological curve. The government implemented several pre-emptive policies such as domestic/ international travel restrictions, shuttering business activity, distance learning in public & university education. Besides the economic backlash, sudden lockdown multiplied with the risks posed by an unknown infectious disease resulted in wide-range of impacts (such as anxiety, stress, problems in social and emotional functioning) on health-related quality of life (HRQoL) of the population [1, 2]. Mass vaccination started in 2021 mid-January, shortly followed by the third wave of the pandemic (March-June 2021), bringing sanctuary regulations back (distance learning in public education, austere lockdown, mandatory mask-wearing in/outside).
Similarly, to other countries, Hungary started to investigate several related aspects of the pandemic, including fear, anxiety, stigmatization and worries [3–5]. Several studies address fear as the most contagious factor of epidemics [6–13]. The uniqueness of the COVID-19 stressed that instead of utilizing generic psychological scales, developing a new disease-specific Fear of COVID-19 Scale (FCV-19S) would be adequate.
The first survey introducing the FCV-19S that has been used to measure fear associated with COVID-19 pandemic was published in March 2020 [14]. Currently it has been validated in at least 40 countries and translated to more than 20 languages (see supplementary material). The Hungarian version of FCV-19S has been validated in a convenient sample of university students and lecturers in 2021 [15].
Despite of many existing scales measuring fear and anxiety of individuals, the crucial role of fear in response to global pandemic outbreak generated demand in research of psychology and related disciplines towards the FCV-19 Scale. It is directly designed to measure fear of COVID-19 and able to identify vulnerable population groups. Pandemic caused fear of dying, getting infected, unable to work may aggregate in stress/anxiety that negatively impacts people’s health [16–19]. Health policy interventions need appropriate information of COVID-19 generated fear, that is measured by a pandemic-specific instrument [14, 20].
The rapid spread of FCV-19S generated information in conclusions of good internal consistency, acceptable construct, convergent & concurrent validity, with satisfactory psychometric properties of the scale [6, 21–24]. The psychometric tests of FCV-19S suggest that it is applicable in all genders and age-groups [25]. However, there is a debate in the number of underlying latent factors [26–34].
Methods of classical test theory (CTT) (e.g. item-correlations, Cronbach’s α) and item response theory (IRT), also referred as modern test theory (e.g. parameter logistic modelling, Rasch analysis) may all be used to assess the validity and reliability of a new measurement tool. Dimensionality of constructs is often explored by exploratory/confirmatory factor analysis (EFA and/or CFA). Besides CTT, IRT and factor analysis elements, more researches expanded the instrument evaluation with structural equation modelling (SEM) [35, 36] or Rasch analysis [14, 25].
Initially the FCV-19S was designed to capture one-dimension of fear. Several studies confirmed the one-dimensional structure of the scale using either modified [20, 37–40] or the initial CFA model [41]. When designing a new construct to measure a physiological/psychological dimension (e.g. pain or fear), preferably the item numbers should be balanced related to each dimension, particularly when more than one latent factor may be present. So far, several studies have approved the one-dimensional structure of the FCV-19S [15, 42, 43], although other evaluations reported valid and reliable two-dimensional factor structures identifying both emotional and physiological factors of fear [31, 44]. The two-factor models were inconclusive, divergent factor structures appeared [29, 40, 41]. To date only few studies cross-compared directly the one and two-factor models to examine a potential two factor structure of FCV-19S [27, 34, 45].
Objective
Compared to the huge number of construct dimensionality evaluation studies using one-factor structure [20, 24, 25, 46, 47], only few completed two-factor models [22, 27, 29, 31, 48], even fewer reported the results of EFA and CFA cross-comparison. This study aims to compare the one and two-factor structure by EFA and CFA dimensionality assessment and analyse the psychometric properties of the FCV-19S.
Methods
Data collection method
A large-scale cross-sectional survey was carried out between May 25th – June 08th 2021. Similarly to previous FCV-19S validation studies, an online self-completed questionnaire has been developed. A professional survey company collected the data, using their online panel database. The targeted sample size was N = 2,000 of Hungarian adult general population, no data was collected from dropouts.
Fear of COVID-19 Scale
The FCV-19S questionnaire consists of seven-items scored on a five-point Likert scale, with maximum overall score of 35 (indicating the highest level of fear) [14]. Respondents are questioned about the extent of being afraid of coronavirus (anxiousness, losing life, uncomfortable thoughts) and the related physiological manifestations of fear (palpitating heart, clammy hands, losing sleep). Seven closed questions, each represented by one statement, rated on a 1–5 point balanced scale (‘1’ indicating strong disagreement) measured respondents fear related to coronavirus.
Translation
The permission to translate and utilize FCV-19S scale was obtained from the developer team of the questionnaire. To adapt it, forward–backward translation was applied supervised by two health professionals and harmonized by group discussion of more researchers. The original translation was altered in item 1 (most afraid of coronavirus) and item 5 (nervous and anxious when watching news and stories about coronavirus): to (1) being very afraid and (5) see news in social media, in order to comply cultural and semantical embedding. “Coronavirus” appellation was changed to “COVID-19”. The final version has been back-translated to English by a third independent native speaker, the consensus version needed no changes. (See the Hungarian version in Supplementary material).
Statistical analysis
Descriptive statistics including means and central tendency measures were used to explore sample population and item characteristics (standard deviation, variance, skewness, kurtosis, floor effect, ceiling effect). Reliability of the FCV-19 Scale was examined by CTT, measuring items correlation (Pearson’s r and corrected item-total correlation) and internal consistency (Cronbach alpha). Inflation in mean estimates was assessed through ceiling and floor effect with 95% confidence interval consideration. Interpretation values for FCV-19S construct properties were set as Pearson correlation coefficient for inter item consistency > 0.3; Cronbach alpha for internal consistency > 0.7 and corrected item–total correlation coefficient with a value of no less than 0.5 [49, 50].
Dimensionality information of the 7-item construct was revealed by conducting a separate one- and two-factor model exploratory factor analysis, followed by confirmatory factor analysis, using principal axis factoring extraction for EFA. Diagonally-weighted least square (DWLS) estimation was used for CFA, due to better fit to ordinal data [51, 52]. The sample was randomly distributed into two subsamples (50–50%) to cross-validate EFA & CFA measures [53]. Communalities, factor loadings, standardized estimates, regression weights and squared multiple correlations (SMC) were reported. Factor loadings were interpreted as acceptable if ≥ 0.3, practically significant if ≥ 0.5 and indicative of a well-defined structure if ≥ 0.7 [54]. Rotation method is decided based on factors correlation, distribution is considered oblige in component correlation is above 0.4. Absolute model fit measures in terms of root mean square error of approximation (RMSEA), standardized mean root square residual (SRMR), Chi square and degree of freedom were compared, such as incremental model fit indices of Tucker–Lewis index (TLI) and comparative fit index (CFI). Common threshold values were used both for RMSEA ≤ 0.08 and SRMR ≤ 0.06 [55] ; > 0.95 for TLI and CFI [56].
Nonparametric tests (Kruskal–Wallis and Mann–Whitney) were used to compare FCV-19S mean scores of subgroups to demonstrate construct validity. Convergent validity between FCV-19S score and health status measurement tool scores: the Hungarian value set based EQ-5D-5L utility index [57, 58], seven item General Anxiety Disorder (GAD-7) [59] and nine item Patient Health Questionnaire (PHQ-9) [60] was explored using Spearman’s correlation. Statistical analysis was carried out using IBM SPSS (Version 25.0. Armonk, NY: IBM Corp), factor analysis was performed using R (v4.1.2; R Core Team 2021; levaan 0.6–11 package).
Results
Population characteristics
Overall, N = 2,421 started the questionnaire, the final sample contains N = 2000 complete responses of the Hungarian adult general population (response rate: 82.6%). The mean age was 49.1 (SD = 15.3), majority of the sample was female (n = 1244; 62.2%). Education level of respondents in primary, secondary and tertiary school distributed as follows: 21.8%, 45.0%, 33.2%. Majority of the sample population has been vaccinated (n = 67.3%), and 18.5% (n = 370) already encountered the infection. At the time of data collection altogether 5.1 million people (53%) in Hungary were vaccinated at least once [61] (Table 1).
Table 1.
Sample characteristics and mean FCV-19S scores
| Variable | n | % | FCV-19S score (SD) | p value* | |
|---|---|---|---|---|---|
| Total | 2000 | 100 | 13.9 (5.5) | ||
| Age group | 18–34 | 437 | 21.9 | 13.5 (5.8) | < 0.001 |
| 35–54 | 763 | 38.1 | 13.7 (5.7) | ||
| 55 < | 800 | 40.0 | 14.3 (5.2) | ||
| Gender | male | 756 | 37.8 | 13.1 (5.3) | < 0.001 |
| female | 1244 | 62.2 | 14.4 (5.7) | ||
| Educational level | primary | 435 | 21.8 | 14.7 (6.6) | = 0.166 |
| secondary | 900 | 45.0 | 13.8 (5.4) | ||
| tertiary | 665 | 33.2 | 13.5 (4.9) | ||
| Vaccinated | yes | 1347 | 67.3 | 14.2 (5.3) | < 0.001 |
| no | 653 | 32.7 | 13.1 (6.0) | ||
| Infected | yes | 370 | 18.5 | 13.8 (5.7) | = 0.551 |
| no | 1630 | 81.5 | 13.9 (5.5) | ||
*Known-group validity was assessed by the appropriate Kruskal–Wallis H or Mann–Whitney U non-parametric test (significant if p < 0.05)
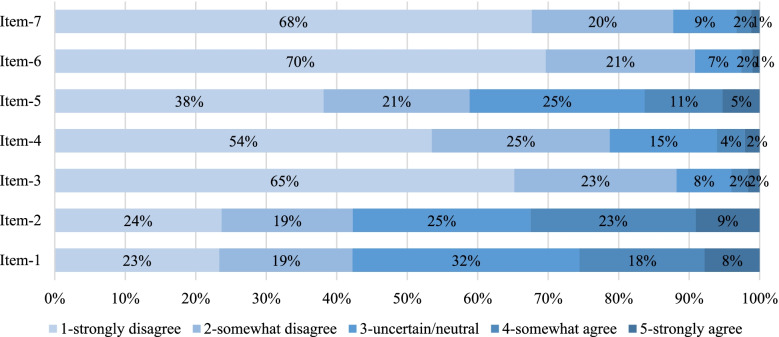
Total average fear score out of the possible maximum of 35 on FCV-19S was 13.9 (SD = 5.5). Central tendency measures suggest that all people agreed the most with the statements 1, 2 and 5 indicating the highest impact of unpleasant thinking, being afraid, and seeing news of COVID-19 on fear level. Statement 1 (n = 26%), 2 (n = 32%), 5 (n = 16%) had the highest number of agreements while the same items (1,2 and 5) indicated the greatest uncertainty (n = 32%, 25%, 25%). Response distribution among items, showed gravitation towards high disagreement in questions 3 (n = 83%), 4 (n = 79%), 6 (n = 91%) and 7 (n = 88%) (Fig. 1).
Fig. 1.
Distribution of responses among items
Nonparametric tests revealed significant differences in FCV-19S scores among separate age (p < 0.01), gender (p < 0.001) and vaccination groups (p < 0.001). Older individuals (aged > 55+), women and vaccinated had higher mean scores, demonstrating elevated fear due COVID-19.
Health status measure scores all correlated significantly (p < 0.01) on slight to moderate level with the FCV-19S: GAD-7 (rho = 0.373); PHQ-9 (rho = 0.309); EQ-5D-5L index (rho = -0.235) demonstrating convincing convergent validity (Tables 2 and 3).
Table 2.
Descriptive statistics of item responses
| Descriptive statistics of FCV-19S items in total sample | ||||||||
|---|---|---|---|---|---|---|---|---|
| Items | n | mean | SD | skewness | kurtosis | floor % | ceiling % | Item variance |
| Item #1 | 2000 | 2.68 | 1.23 | 0.13 | -0.93 | 23.4 | 7.8 | 1.51 |
| Item #2 | 2000 | 2.76 | 1.29 | 0.05 | -1.15 | 23.7 | 9.0 | 1.67 |
| Item #3 | 2000 | 1.52 | 0.86 | 1.92 | 3.74 | 65.2 | 1.7 | 0.74 |
| Item #4 | 2000 | 1.76 | 0.99 | 1.27 | 1.05 | 53.5 | 2.1 | 0.98 |
| Item #5 | 2000 | 2.25 | 1.22 | 0.59 | -0.70 | 38.2 | 5.3 | 1.48 |
| Item #6 | 2000 | 1.43 | 0.77 | 2.11 | 4.89 | 69.7 | 1.0 | 0.59 |
| Item #7 | 2000 | 1.49 | 0.84 | 1.89 | 3.50 | 67.7 | 1.2 | 0.70 |
| Descriptive statistics of items in vaccinated group | ||||||||
| Item #1 | 1347 | 2.85 | 1.19 | -0.04 | -0.87 | 17.4 | 8.4 | 1.43 |
| Item #2 | 1347 | 2.84 | 1.25 | -0.04 | -1.07 | 19.5 | 8.3 | 1.55 |
| Item #3 | 1347 | 1.54 | 0.83 | 1.73 | 2.95 | 62.8 | 1.0 | 0.70 |
| Item #4 | 1347 | 1.8 | 0.98 | 1.15 | 0.76 | 50.3 | 1.8 | 0.96 |
| Item #5 | 1347 | 2.29 | 1.19 | 0.47 | -0.8 | 35.3 | 4.3 | 1.42 |
| Item #6 | 1347 | 1.43 | 0.73 | 1.89 | 3.71 | 68.7 | 0.4 | 0.54 |
| Item #7 | 1347 | 1.49 | 0.82 | 1.77 | 2.85 | 67.1 | 0.7 | 0.67 |
| Descriptive statistics of items in non-vaccinated group | ||||||||
| Item #1 | 653 | 2.31 | 1.22 | 0.53 | -0.63 | 35.5 | 6.6 | 1.49 |
| Item #2 | 653 | 2.59 | 1.37 | 0.26 | -1.20 | 32.2 | 10.6 | 1.88 |
| Item #3 | 653 | 1.49 | 0.92 | 2.24 | 4.90 | 70.1 | 2.9 | 0.85 |
| Item #4 | 653 | 1.68 | 1.00 | 1.52 | 1.76 | 60.2 | 2.8 | 1.01 |
| Item #5 | 653 | 2.15 | 1.27 | 0.81 | -0.45 | 44.0 | 7.2 | 1.62 |
| Item #6 | 653 | 1.43 | 0.84 | 2.38 | 6.03 | 71.7 | 2.1 | 0.71 |
| Item #7 | 653 | 1.49 | 0.87 | 2.11 | 4.58 | 68.9 | 2.1 | 0.75 |
Table 3.
Correlation of the seven items
| Pearson’s correlation of FCV-19S items | Corrected item-total correlation | Cronbach alpha if item deleted | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Items | Item #1 | Item #2 | Item #3 | Item #4 | Item #5 | Item #6 | Item #7 | ||
| Item #1 | 1 | 0.617 | 0.866 | ||||||
| Item #2 | 0.601 | 1 | 0.626 | 0.866 | |||||
| Item #3 | 0.403 | 0.402 | 1 | 0.663 | 0.859 | ||||
| Item #4 | 0.544 | 0.471 | 0.652 | 1 | 0.749 | 0.847 | |||
| Item #5 | 0.499 | 0.611 | 0.494 | 0.589 | 1 | 0.699 | 0.853 | ||
| Item #6 | 0.366 | 0.357 | 0.625 | 0.618 | 0.486 | 1 | 0.666 | 0.861 | |
| Item #7 | 0.418 | 0.405 | 0.634 | 0.646 | 0.537 | 0.812 | 1 | 0.711 | 0.855 |
Consistency measures
The total internal consistency of the COVID-19 fear questionnaire was good (Cronbach α = 0.88), all items indicated proper internal consistency, corrected item-total correlations of items range between 0.62–0.75. All seven items were significantly correlating (p < 0.001) on a moderate to high level (r = 0.357–812), expressing acceptable instrument validity and enabling factor analysis (Kaiser–Meyer–Olkin measure = 0.864; p < 0.001).
Factor analysis outcomes
Results of one-factor EFA show that items 4, 6 and 7 have high level of common variance (h2 = 0.69; 0.60; 0.68). Total variance explained by the one-factor model was 60.8%, with component’s eigenvalue = 4.26 meaning that the factor explains the same amount of variance than 4.2 items. Oblimin rotation with Kaiser normalization was applied in case of the two-factor model: factors were correlating r = 0.61 (coefficients smaller than 0.30 were supressed in the pattern matrix). All items have moderate/high common variance (h2 = 0.54–0.80). Factor loading shows that questions 1,2,5 likely belong to Factor 1, named as “emotional fear” based on item correlation strength. Questions 3,4,6,7 are strongly related to Factor 2, named as “physiological fear”. Factor retaining was decided by parallel analysis, the random data eigenvalue score was much bigger (eig = 1.069), than the second factors eigenvalue (1.022) of the sample (Table 4).
Table 4.
One and two-factor EFA results
| EFA model | One-factor model | Two-factor model | |||
|---|---|---|---|---|---|
| Items (question) | Communality (h2) | Factor matrix (1 factor loading) | Communality (h2) | Factor matrix | |
| 1-physiological factor | 2-emotional factor | ||||
| Item-1 | 0.389 | 0.575 | 0.536 | - | 0.698 |
| Item-2 | 0.380 | 0.558 | 0.680 | 0.874 | |
| Item-5 | 0.540 | 0.691 | 0.593 | 0.587 | |
| Item-3 | 0.560 | 0.760 | 0.563 | 0.640 | - |
| Item-4 | 0.691 | 0.819 | 0.666 | 0.605 | |
| Item-6 | 0.595 | 0.828 | 0.803 | 0.967 | |
| Item-7 | 0.667 | 0.857 | 0.787 | 0.890 | |
The one-factor model CFA estimated one-unit change in standard deviation of items between β = 0.65–0.81, modest in case of item 1, highest in item 4. Unstandardized regression estimate showed that elevation in fear score increases item scores (unstandardized β = 0.63–1.14). Predicted variance of items ranged between R2 = 42.8–65.3%. No covariances were drawn between items, the baseline model showed acceptable model fit both in one- and two-factor structure (Table 5).
Table 5.
Results of one and two-factor CFA
| One-factor CFA model | ||||
| Item | Latent factor | estimate (stand. reg. weight) | regression weight (SE) | squared loading (SMC) |
| #1 | Fear | 0.654 | 1.00 (-) | 0.428 |
| #2 | 0.670 | 1.08 (0.05) | 0.449 | |
| #3 | 0.684 | 0.74 (0.04) | 0.468 | |
| #4 | 0.808 | 1.01 (0.05) | 0.653 | |
| #5 | 0.759 | 1.14 (0.06) | 0.576 | |
| #6 | 0.668 | 0.63 (0.04) | 0.447 | |
| #7 | 0.727 | 0.74 (0.04) | 0.529 | |
| One-factor model fit | ||||
| Statistical measure | Test indices | Test Results | Test standard (unit value) | Model fit |
| Absolute fit | RMSEA | 0.075 | < 0.08 | excellent |
| Chi square/df | 93.3 (14) | < 5.0 | not optimal | |
| Chi square p | < 0.001 | > 0.05 | not optimal | |
| SRMR | 0.091 | < 0.06 | not optimal | |
| Incremental fit | TLI | 0.974 | > 0.95 | good |
| CFI | 0.962 | > 0.95 | good | |
| Two-factor CFA model | ||||
| Item | Latent factor | estimate (stand. reg. weight) | regression weight | squared loading (SMC) |
| #1 | 1. factor: emotional fear | 0.705 | 1.00 (-) | 0.498 |
| #2 | 0.735 | 1.10 (0.05) | 0.540 | |
| #5 | 0.805 | 1.13 (0.06) | 0.649 | |
| #3 | 2. factor: physiological fear | 0.755 | 1.00 (-) | 0.571 |
| #4 | 0.877 | 1.34 (0.08) | 0.769 | |
| #6 | 0.743 | 0.86 (0.05) | 0.552 | |
| #7 | 0.806 | 1.00 (0.06) | 0.649 | |
| Two-factor model fit | ||||
| Statistical measure | Test indices | Test Results | Test standard (unit value) | Model fit |
| Absolute fit | RMSEA | 0.044 | < 0.08 | excellent |
| Chi square/df | 38.3 (13) | < 5.0 | optimal | |
| Chi square p | < 0.001 | > 0.05 | not optimal | |
| SRMR | 0.057 | < 0.06 | good | |
| Incremental fit | TLI | 0.992 | > 0.95 | excellent |
| CFI | 0.987 | > 0.95 | excellent | |
The two-factor model had better model fit in terms of RMSEA, Chi-square/df, SRMR, TLI and CFI. The one-unit change impact of “emotional fear” factor on items 1, 2, 5 (β = 0.71; 0.74; 0.81) was similar to the impact of “physiological fear” factor on items 3, 4, 6, 7 (β = 0.76; 0.88; 0.74; 0.81). Predictors of items explained R2 = 49.8–76.9% of items variance. In comparison to the one-factor model, the error variance of items in the two-factor model ranged on larger scale (34.7–57.2 vs 23.1–50.2%). Fear elevated in items 2 & 5 (uncomfortable to think on coronavirus-19 & becoming nervous) due emotional fear factor (unstandardized β = 1.10 & 1.13). Fear was elevating in items 4,6,7 (losing life; can’t sleep; heart palpitates) due physiological fear factor (unstandardized β = 1.34; 0.86; 1.00). Emotional and physiological factors showed linear covariation (0.43) and significant high level of correlation (r = 0.76) (Table 5).
Discussion
A large cross-sectional study among general population to validate the Hungarian seven item FCV-19S was done in 2021 May. Psychometric properties were analysed by descriptive statistics, methods of classical test theory were used to measure validity and reliability. Exploratory and confirmatory factor analysis was conducted to compare one and two-factor structure of the construct.
Differences in FCV-19S mean scores were highlighted between different age groups (18–34: 13.5; 35–54: 13.7; 55 ≤ : 14.3), male (13.1) and female (14.4), vaccinated (14.2) and non-vaccinated (13.1) population groups. Correlation between anxiety (GAD-7), depression (PHQ-9) and FCV-19S was moderate, while EQ-5D utility and fear score weakly correlated. Item descriptive measures suggest that people agreed the most with questions 1 (afraid of COVID-19), 2 (unpleasant thinking) and 5 (seeing news in social media). Vaccinated group indicated higher fear in items 1–5 and equalled in items 6–7 compared to non-vaccinated group. Items 3 (clammy hands), 4 (losing life), 6 (cannot sleep), 7 (palpitating heart) received the biggest proportion of disagreement responses.
The Hungarian version of the FCV-19S has good level of internal consistency (Cronbach’s α = 0.88), and high corrected item-total correlation (r = 0.666–0.749). Dimensionality assessment by one and two-factor exploratory factor analysis, suggests that observing two latent factors is possible, also resulted a better model fit, whereas the eigenvalue of the second latent factor was arguably low (eig = 1.02). The randomly generated correlation matrices of parallel analysis suggest minimum mean eigenvalue of no less than 1.07 for the second factor, supporting the one factor structure. Similarly, a large cross-country comparative analysis further supported the unidimensional structure of the construct [62].
All previously published two-factor analyses showed good model fits, while the item-factor structures turned out different [27, 29, 31, 63]. Almost every two-factor analyses identified items 1,2,4,5 as “emotional fear” factor and items 3,6,7 as “physiological component” of fear, respectively [27, 31, 34, 44, 48, 63]. In one study [29], items 1,2,4 represented “cognitive fear” factor and 3,5,6,7 the “somatic fear” factor. Our two-factor structure is unique: physiological fear factor consists of items 3,4,6,7 and emotional fear of items 1,2,5. The weakest element in our two-factor structure, shown by the pattern matrix was item 4 (better correlating with the physiological factor: 0.61 vs 0.29). Nevertheless, item 4 potentially belongs to emotional fear dimension, albeit CFA model fit results were better, when classifying it to physiological fear dimension. The results of factor structures in many studies echoes strong relationship (covariance) in item 1–2 and item 6–7, simultaneously a gap between these pairs [26, 37, 38, 40]. Two-latent factors practically imply that COVID-19 fear incorporate emotional and physiological fear, that is heterogeneous among people, thus both factors should be separately measured to differentiate between observational and latent factors. Although, standardization of a composite fear score would be extremely difficult, mostly due to the divergences in factor structures. This inconsistency of the dimensional structure of FCV-19S further supports the acceptance of the one-dimensional approach.
Contemporary study introduced the validation of the Hungarian version of the FCV-19 Scale, showing congruent results to our study, though research groups worked separately [15]. Although, minor differences in translation regarding synonyms appeared, literally the sentences were corresponding. The two study samples (convenient vs general population) and data collection time (2021 January: mid of second wave vs 2021 May: ending of the third wave) remarkably differed. Conclusions of the two studies on excellent construct validity and reliability were similar. Dimensionality assessed only by one-factor CFA, showed dissimilar, rather poor model fit (RMSEA: 0.16 vs 0.08 and CFI: 0.84 vs 0.97), compared to our results, but factor loadings were kindred (0.47–0.84 vs 0.65–0.81).
This study aimed to evaluate the (1) psychometric properties, (2) validity and reliability and (3) dimensionality of the Hungarian version of Fear of COVID-19 Scale, although a primary limitation is posed by the timing of the data collection. Salient divergences in COVID-19 fear could have been between the contagion peaks of the pandemic and access to vaccines both within the country and between countries. Second limitation of this study is the online data collection and convenient sampling among respondents of panel database. Considering the second factors eigenvalue (1.02), EFA and parallel analysis suggests that researchers have to be cautious when concluding the results of the two-factor model. Item 4 (losing life), unlike in other structures was stronger related to physiological than to emotional fear factor.
Conclusion
Huge number of psychometric validation and factor analysis studies followed the original FCV-19S validation study [14]. Our results are consistent with the previous findings [20, 42, 43, 64], emphasising that FCV-19S has reliable and valid measurement properties.
We used one- and two-factor EFA along with parallel analysis to evaluate the dimensionality of the construct. Two latent factors (emotional and physiological fear) were confirmed by CFA, moreover the two-factor structure showed better model fit, though its’ generalization faces limitations. Although the FCV-19S original factor structure was one-dimensional, our findings suggest a two-factor structure.
Supplementary Information
Authors’ contributions
All authors contributed to questionnaire development. PB and VB designed the study concept. Statistical analysis were performed by PB and AM. The first draft of the manuscript was written by PB and all authors contributed to the critical revision of the paper. All authors read and accepted the final version of manuscript.
Funding
Open access funding provided by Corvinus University of Budapest. Funding was obtained by VB. There was no editorial direction or censorship from the sponsor. PB received support from EFOP-3.6.3-VEKOP-16-2017-00007 publication source for PhD students.
Declarations
Ethics approval and consent to participate
The study followed the Helsinki Declaration guidelines. All participants were adults (18 ≤) who provided informal consent. Ad Hoc Research Ethics Committee at the Corvinus University of Budapest granted the ethical approval (KRH/109/2021).
Competing interests
Authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nobari H, Fashi M, Eskandari A, Villafaina S, Murillo-Garcia Á, Pérez-Gómez J. Effect of COVID-19 on Health-Related Quality of Life in Adolescents and Children: A Systematic Review. Int J Environ Res Public Health. 2021;18(9). 10.3390/ijerph18094563 [DOI] [PMC free article] [PubMed]
- 2.Poudel AN, Zhu S, Cooper N, Roderick P, Alwan N, Tarrant C, Yao GL. Impact of Covid-19 on health-related quality of life of patients: a structured review. PLoS One. 2021;16(10):e0259164. doi: 10.1371/journal.pone.0259164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dombrádi V, Joó T, Palla G, Pollner P, Belicza É. Comparison of hesitancy between COVID-19 and seasonal influenza vaccinations within the general Hungarian population: a cross-sectional study. BMC Public Health. 2021;21(1):2317. doi: 10.1186/s12889-021-12386-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oroszi B, Juhász A, Nagy C, Horváth JK, McKee M, Ádány R. Unequal burden of COVID-19 in Hungary: a geographical and socioeconomic analysis of the second wave of the pandemic. BMJ Glob Health. 2021;6(9). 10.1136/bmjgh-2021-006427 [DOI] [PMC free article] [PubMed]
- 5.Szabo A, Ábel K, Boros S. Attitudes toward COVID-19 and stress levels in Hungary: effects of age, perceived health status, and gender. Psychol Trauma. 2020;12(6):572–575. doi: 10.1037/tra0000665. [DOI] [PubMed] [Google Scholar]
- 6.Alimoradi Z, Ohayon MM, Griffiths MD, Lin C-Y, Pakpour AH. Fear of COVID-19 and its association with mental health-related factors: systematic review and meta-analysis. BJPsych Open. 2022;8(2):e73–e73. doi: 10.1192/bjo.2022.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kukreti S, Ahorsu DK, Strong C, Chen I-H, Lin C-Y, Ko N-Y, Pakpour AH. (2021). Post-traumatic stress disorder in Chinese teachers during COVID-19 pandemic: Roles of fear of COVID-19, nomophobia, and psychological distress. Paper presented at the Healthcare. [DOI] [PMC free article] [PubMed]
- 8.Kukreti S, Ahorsu DK, Strong C, Chen IH, Lin CY, Ko NY, Pakpour AH. Post-Traumatic Stress Disorder in Chinese Teachers during COVID-19 Pandemic: Roles of Fear of COVID-19, Nomophobia, and Psychological Distress. Healthcare (Basel). 2021;9(10).10.3390/healthcare9101288 [DOI] [PMC free article] [PubMed]
- 9.Li Y-P, Lin C-Y, Kuo Y-J, Chen Y-P, Griffiths MD. Gender differences in the factors associated with the fear of COVID-19 among Taiwanese older people. Inquiry. 2021;58:00469580211055587. doi: 10.1177/00469580211055587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rad MK, Fakhri A, Stein L, Araban M. Health-care staff beliefs and coronavirus disease 2019 vaccinations: a cross-sectional study from Iran. Asian J Soc Health Behav. 2022;5(1):40. doi: 10.4103/shb.shb_13_22. [DOI] [Google Scholar]
- 11.Rajabimajd N, Alimoradi Z, Griffiths M. Impact of COVID-19-related fear and anxiety on job attributes: a systematic review. Asian J Soc Health Behav. 2021;4(2):51–55. doi: 10.4103/shb.shb_24_21. [DOI] [Google Scholar]
- 12.Sangma RD, Kumar P, Nerli LM, Khanna AM, Vasavada DA, Tiwari DS. Social stigma and discrimination in Coronavirus Disease-2019 survivors and its changing trend: a longitudinal study at tertiary care center Gujarat, India. Asian J Soc Health Behav. 2022;5(2):68. doi: 10.4103/shb.shb_12_22. [DOI] [Google Scholar]
- 13.Schimmenti A, Billieux J, Starcevic V. The four horsemen of fear: an integrated model of understanding fear experiences during the Covid-19 pandemic. Clin Neuropsychiatry. 2020;17(2):41–45. doi: 10.36131/cn20200202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict. 2020:1-9. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed]
- 15.Stankovic M, Papp L, Nyúl B, Ivánkovits L, Pető Z, Töreki A. Adaptation and psychometric evaluation of Hungarian version of the Fear of COVID-19 Scale. PLoS One. 2021;16(12):e0261745–e0261745. doi: 10.1371/journal.pone.0261745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alsolais A, Alquwez N, Alotaibi KA, Alqarni AS, Almalki M, Alsolami F, Cruz JP. Risk perceptions, fear, depression, anxiety, stress and coping among Saudi nursing students during the COVID-19 pandemic. J Ment Health. 2021;30(2):194–201. doi: 10.1080/09638237.2021.1922636. [DOI] [PubMed] [Google Scholar]
- 17.Broche-Pérez Y, Fernández-Fleites Z, Jiménez-Puig E, Fernández-Castillo E, Rodríguez-Martin BC. Gender and Fear of COVID-19 in a Cuban population sample. Int J Ment Health Addict. 2022;20(1):83–91. doi: 10.1007/s11469-020-00343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giordani RCF, Zanoni da Silva M, Muhl C, Giolo SR. Fear of COVID-19 scale: assessing fear of the coronavirus pandemic in Brazil. J Health Psychol. 2022;27(4):901–912. doi: 10.1177/1359105320982035. [DOI] [PubMed] [Google Scholar]
- 19.Pang NTP, Kamu A, Hambali NLB, Mun HC, Kassim MA, Mohamed NH, Jeffree MS. Malay version of the Fear of COVID-19 Scale: Validity and Reliability. Int J Ment Health Addict. 2020:1-10. 10.1007/s11469-020-00355-4
- 20.Alyami M, Henning M, Krägeloh CU, Alyami H. Psychometric Evaluation of the Arabic Version of the Fear of COVID-19 Scale. Int J Ment Health Addict. 2020;1-14. 10.1007/s11469-020-00316-x [DOI] [PMC free article] [PubMed]
- 21.Blázquez-Rincón D, Durán JI, Botella J. The Fear of COVID-19 Scale: a reliability generalization meta-analysis. Assessment. 2022;29(5):940–948. doi: 10.1177/1073191121994164. [DOI] [PubMed] [Google Scholar]
- 22.Chen IH, Chen C-Y, Zhao K-Y, Gamble JH, Lin C-Y, Griffiths MD, Pakpour AH. Psychometric evaluation of fear of COVID-19 Scale (FCV-19S) among Chinese primary and middle schoolteachers, and their students.Curr Psychol. 2022;1-17. 10.1007/s12144-021-02471-3 [DOI] [PMC free article] [PubMed]
- 23.Lecuona O, Lin C-Y, Rozgonjuk D, Norekvål TM, Iversen MM, Mamun MA, Pakpour AH. A network analysis of the Fear of COVID-19 Scale (FCV-19S): a large-scale cross-cultural study in Iran, Bangladesh, and Norway. Int J Environ Res Public Health. 2022;19(11):6824. doi: 10.3390/ijerph19116824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ullah I, Tahir MJ, Ali S, Waseem R, Griffiths MD, Mamun M. A, Pakpour AH. COVID-19 Fear among Pakistanis: psychometric evaluation of the Fear of COVID-19 Scale using item response theory and confirmatory factor analysis. Int J Ment Health Addict. 2021. 10.1007/s11469-021-00656-2 [DOI] [PMC free article] [PubMed]
- 25.Sakib N, Bhuiyan A, Hossain S, Al Mamun F, Hosen I, Abdullah AH, Mamun MA. Psychometric validation of the Bangla Fear of COVID-19 Scale: confirmatory factor analysis and rasch analysis. Int J Ment Health Addict. 2020:1-12. 10.1007/s11469-020-00289-x [DOI] [PMC free article] [PubMed]
- 26.Al-Shannaq Y, Mohammad AA, Khader Y. Psychometric Properties of the Arabic Version of the Fear of COVID-19 Scale (FCV-19S) Among Jordanian Adults. Int J Ment Health Addict. 2021:1-14. 10.1007/s11469-021-00574-3 [DOI] [PMC free article] [PubMed]
- 27.Barrios I, Ríos-González C, O'Higgins M, González-Urbieta I, García O, Almirón-Santacruz J, Torales J. Psychometric properties of the Spanish version of the Fear of COVID-19 scale in Paraguayan population. Ir J Psychol Med. 2021;1-6. 10.1017/ipm.2021.5 [DOI] [PMC free article] [PubMed]
- 28.Berlinger E, Dömötör BM, Szűcs BÁ. Irrational risk-taking of professionals? The relationship between risk exposures and previous profits. Risk Manage J Risk Crisis Disaster. 2021;23(3):243–259. doi: 10.1057/s41283-021-00076-5. [DOI] [Google Scholar]
- 29.Iversen MM, Norekvål TM, Oterhals K, Fadnes LT, Mæland S, Pakpour AH, Breivik K. Psychometric Properties of the Norwegian Version of the Fear of COVID-19 Scale. Int J Ment Health Addict. 2021:1-19. 10.1007/s11469-020-00454-2 [DOI] [PMC free article] [PubMed]
- 30.Lin C-Y, Griffiths MD, Pakpour, AH. Psychometric properties of the Fear of COVID-19 Scale: A response to de Medeiros et al.“Psychometric properties of the Brazilian version of the Fear of COVID-19 Scale (FCV-19S)”. Curr Psychol. 10.1007/s12144-021-02686-4. [DOI] [PMC free article] [PubMed]
- 31.Masuyama A, Shinkawa H, Kubo T. Validation and psychometric properties of the Japanese version of the Fear of COVID-19 Scale among adolescents. Int J Ment Health Addict. 2020:1-11. 10.1007/s11469-020-00368-z [DOI] [PMC free article] [PubMed]
- 32.Pakpour AH, Griffiths MD, Chang K-C, Chen Y-P, Kuo Y-J, Lin C-Y. Assessing the fear of COVID-19 among different populations: A response to Ransing et al. (2020). Brain Behav Immunity. 2020;89:524–525. 10.1016/j.bbi.2020.06.006 [DOI] [PMC free article] [PubMed]
- 33.Pakpour AH, Griffiths MD, Lin C-Y. Assessing the psychological response to the COVID-19: a response to Bitan et al. “Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population.” Psychiatry Res. 2020;290:113127. [DOI] [PMC free article] [PubMed]
- 34.Pretorius TB, Padmanabhanunni A, Stiegler N, Bouchard JP. Validation of the fear of COVID-19 scale in South Africa: three complementary analyses. Ann Med Psychol (Paris) 2021;179(10):940–946. doi: 10.1016/j.amp.2021.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chang KC, Hou WL, Pakpour AH, Lin CY, Griffiths MD. Psychometric Testing of Three COVID-19-Related Scales Among People with Mental Illness. Int J Ment Health Addict. 2020:1-13. 10.1007/s11469-020-00361-6 [DOI] [PMC free article] [PubMed]
- 36.Wakashima K, Asai K, Kobayashi D, Koiwa K, Kamoshida S, Sakuraba M. The Japanese version of the Fear of COVID-19 scale: reliability, validity, and relation to coping behavior. PLoS One. 2020;15(11):e0241958. doi: 10.1371/journal.pone.0241958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cavalheiro FRS, Sticca MG. Adaptation and Validation of the Brazilian Version of the Fear of COVID-19 Scale. Int J Ment Health Addict. 2020:1-9. 10.1007/s11469-020-00415-9 [DOI] [PMC free article] [PubMed]
- 38.Mahmood QK, Jafree SR, Qureshi WA.The Psychometric Validation of FCV19S in Urdu and Socio-Demographic Association with Fear in the People of the Khyber Pakhtunkhwa (KPK) Province in Pakistan. Int J Ment Health Addict. 2020:1-11. 10.1007/s11469-020-00371-4 [DOI] [PMC free article] [PubMed]
- 39.Mailliez M, Griffiths MD, Carre A. Validation of the French version of the Fear of COVID-19 Scale and its associations with depression, anxiety, and differential emotions. Int J Ment Health Addict. 2021:1-15. 10.1007/s11469-021-00499-x [DOI] [PMC free article] [PubMed]
- 40.Soraci P, Ferrari A, Abbiati FA, Del Fante E, De Pace R, Urso A, Griffiths MD. Validation and Psychometric Evaluation of the Italian Version of the Fear of COVID-19 Scale. Int J Ment Health Addict. 2020:1-10. 10.1007/s11469-020-00277-1 [DOI] [PMC free article] [PubMed]
- 41.Winter T, Riordan BC, Pakpour AH, Griffiths MD, Mason A, Poulgrain JW, Scarf D. Evaluation of the English Version of the Fear of COVID-19 Scale and Its Relationship with Behavior Change and Political Beliefs. Int J Ment Health Addict. 2020:1-11. 10.1007/s11469-020-00342-9 [DOI] [PMC free article] [PubMed]
- 42.Pilch I, Kurasz Z, Turska-Kawa A. Experiencing fear during the pandemic: validation of the fear of COVID-19 scale in Polish. PeerJ. 2021;9:e11263. doi: 10.7717/peerj.11263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stănculescu E. Fear of COVID-19 in Romania: validation of the Romanian version of the Fear of COVID-19 Scale using graded response model analysis. Int J Ment Health Addict. 2021;1-16. 10.1007/s11469-020-00428-4 [DOI] [PMC free article] [PubMed]
- 44.Reznik A, Gritsenko V, Konstantinov V, Khamenka N, Isralowitz R. COVID-19 Fear in Eastern Europe: Validation of the Fear of COVID-19 Scale. Int J Ment Health Addict. 2020:1-6. 10.1007/s11469-020-00283-3 [DOI] [PMC free article] [PubMed]
- 45.Boothroyd L, Dagnan D, Muncer S. PHQ-9: one factor or two? Psychiatry Res. 2019;271:532–534. doi: 10.1016/j.psychres.2018.12.048. [DOI] [PubMed] [Google Scholar]
- 46.Bellamkonda, N, Pattusamy M. Validation of Fear of COVID-19 Scale in India: Classical Test Theory and Item Response Theory Approach. Int J Ment Health Addict. 2021:1-8. 10.1007/s11469-021-00521-2 [DOI] [PMC free article] [PubMed]
- 47.Satici B, Gocet-Tekin E, Deniz ME, Satici SA. Adaptation of the Fear of COVID-19 Scale: its association with psychological distress and life satisfaction in Turkey. Int J Ment Health Addict. 2020:1-9. 10.1007/s11469-020-00294-0 [DOI] [PMC free article] [PubMed]
- 48.TzurBitan D, Grossman-Giron A, Bloch Y, Mayer Y, Shiffman N, Mendlovic S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020;289:113100. doi: 10.1016/j.psychres.2020.113100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Irwing P, Booth T, Hughes J, editors. The Wiley handbook of psychometric testing: A multidisciplinary reference on survey, scale and test development. West Sussex: John Wiley & Sons; 2018. [Google Scholar]
- 50.Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126(5):1763–1768. doi: 10.1213/ane.0000000000002864. [DOI] [PubMed] [Google Scholar]
- 51.Goldberg LR, Velicer WF. Principles of exploratory factor analysis. Differ Normal Abnorm Pers. 2006;2:209–337. [Google Scholar]
- 52.Li CH. Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods. 2016;48(3):936–949. doi: 10.3758/s13428-015-0619-7. [DOI] [PubMed] [Google Scholar]
- 53.Gómez-Beneyto M, Nolasco A, Moncho J, Pereyra-Zamora P, Tamayo-Fonseca N, Munarriz M, Girón M. Psychometric behaviour of the strengths and difficulties questionnaire (SDQ) in the Spanish national health survey 2006. BMC Psychiatry. 2013;13:95–95. doi: 10.1186/1471-244X-13-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Szüle B. Comparison of goodness measures for linear factor structures. Statisztikai Szemle. 2017(21):147–163. 10.20311/stat2017.K21.en147.
- 55.Xia Y, Yang Y. RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: the story they tell depends on the estimation methods. Behav Res Methods. 2019;51(1):409–428. doi: 10.3758/s13428-018-1055-2. [DOI] [PubMed] [Google Scholar]
- 56.Kline RB. Principles and practice of structural equation modeling. London: Guilford Press; 2015. [Google Scholar]
- 57.Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20(10):1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rencz F, Brodszky V, Gulácsi L, Golicki D, Ruzsa G, Pickard AS, Péntek M. Parallel Valuation of the EQ-5D-3L and EQ-5D-5L by Time Trade-Off in Hungary. Value Health. 2020;23(9):1235–1245. doi: 10.1016/j.jval.2020.03.019. [DOI] [PubMed] [Google Scholar]
- 59.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 60.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Government, H. (2021). Coronavirus information. koronavirus.gov.hu Retrieved from https://koronavirus.gov.hu/cikkek/5-millio-147-ezer-beoltott-156-az-uj-fertozott-elhunyt-5-beteg.
- 62.Lin CY, Hou WL, Mamun MA, Aparecido da Silva J, Broche-Pérez Y, Ullah I, Pakpour AH. Fear of COVID-19 Scale (FCV-19S) across countries: measurement invariance issues. Nurs Open. 2021;8(4):1892–1908. doi: 10.1002/nop2.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chia T, Oyeniran OI, Iorfa SK. Validation of the fear of the COVID-19 scale in Nigeria: Implications for public health practice. J Taibah Univ Med Sci. 2021;16(6):929–934. doi: 10.1016/j.jtumed.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nazari N, Safitri S, Usak M, Arabmarkadeh A, Griffiths MD. Psychometric Validation of the Indonesian Version of the Fear of COVID-19 Scale: Personality Traits Predict the Fear of COVID-19. Int J Ment Health Addict. 2021:1-17. 10.1007/s11469-021-00593-0 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.