Abstract
Pterostilbene is a naturally occurring analog of resveratrol with many health benefits. These health benefits are associated with its antioxidant activity, anti-inflammatory effects, and chemopreventive effects attributed to its unique structure. The skin cancer chemopreventive potential of pterostilbene is supported by a variety of mechanistic studies confirming the anti-inflammatory effects in skin cancer models. Molecular biological studies have identified that pterostilbene targets pleotropic signaling pathways, including those involved in mitogenesis, cell cycle regulation, and apoptosis. Recently, pterostilbene has been reported to induce autophagy in cancer and normal cells. Through autophagy induction, the inflammatory-related skin diseases can be attenuated. This finding suggests the potential use of pterostilbene in the treatment and prevention of skin disorders via alleviating inflammatory responses by autophagy induction. This review summarizes the protective and therapeutic benefits of pterostilbene in skin diseases from the viewpoint of its antioxidant, anti-inflammatory, and autophagy-inducing effects. Novel underlying mechanisms regarding these effects are discussed. We proposed that pterostilbene, a promising natural product, can be used as a preventive and therapeutic agent for inflammation-related skin disorders through induction of autophagy.
Keywords: autophagy, inflammation, pterostilbene, skin disorders
1. Introduction
Pterostilbene (trans-3,5-dimethoxy-4-hydroxystilbene) is a chemical classified as a stilbene, that is produced naturally by a variety of plants, predominantly found in blueberries, several types of grapes, and tree wood. These plants secrete stilbenes in response to environmental challenges such as microbial infection or excessive ultraviolet exposure [1]. One of the best characterized stilbenes, resveratrol, is known to be an antioxidant, antiaging compound, and anti-inflammatory agent. Pterostilbene is structurally similar to resveratrol; however, pterostilbene exhibits better bioavailability due to the presence of two methoxy groups, which leads to increased lipophilic and oral absorption, as well as the potential for higher cellular uptake and a longer half-life than resveratrol [2]. In animal studies, pterostilbene was shown to have 80% bioavailability compared with 20% for resveratrol making it potentially advantageous as a therapeutic agent [3]. Research regarding pterostilbene attracted more attention, when it was shown to have better antiproliferative effects in cultured cells than resveratrol. Subsequently, the anti-inflammatory, -obesity, and -oxidant properties were reported. More recently, clinical trials have been conducted to evaluate the potential of pterostilbene in treating or preventing cardiac diseases [4]. Thus, pterostilbene may have numerous preventive/therapeutic properties as well as market prospects in a variety of human diseases including neurological, cardiovascular, metabolic, cancerous, and skin disorders.
In general, autophagy is a mechanism of cellular self-consumption for the recycling of intracellular “cargo” such as damaged proteins and organelles. Basal autophagy helps maintain homeostasis, while additional autophagy is induced in response to many different forms of stress including nutrient, oxygen and growth factor deprivation, and chemo-therapeutics, in turn serving as a cell-survival mechanism [5]. Autophagic defects have been implicated in various diseases and health states, including neurodegeneration, aging, infectious disease, skin disease, and cancer [6]. However, the role of autophagy in human diseases is complicated and controversial. For example; in cancer research, autophagy could act as a cytoprotective mechanism by degrading the cytotoxic substances for energy reuse. Nonetheless, when the damage is irreversible and beyond the level that cells can endure, autophagy may also play a role as death executioner [6]. Our previous reports showed that combined treatment with irradiation and chemotherapeutic agents induced both autophagy and apoptosis in several cancerous cells, where autophagy played a more prodeath role than a prosurvival role [7–9]. Interestingly, one of our previous reports also demonstrated that pterostilbene effectively inhibits the growth of sensitive and chemoresistant human bladder cancer cells by inducing cell cycle arrest, autophagy, and apoptosis. Inhibition of pterostilbene-induced autophagy enhanced the apoptotic effects in cancer cells, indicating a prosurvival role of autophagy [10]. The relationship between autophagy and apoptosis is complex and varies between cell types and the specific stresses placed upon the cell [11]. Similar stimuli can induce autophagy, apoptosis, or both because several signals are shared between them.
Pterostilbene has been reported to be an effective chemo-preventive agent against many cancers by several groups, including ours [12–14]. For example, we have demonstrated that pterostilbene exerts a potent effect in preventing azoxy-methane (AOM)-induced colon tumorigenesis via suppression of multiple signal transduction pathways, including the downregulation of inflammatory inducible nitric oxide synthase (iNOS) and cyclooxygenase 2 (COX-2) gene expression [13]. In addition, pretreatment with pterostilbene significantly reduced tumor multiplicity, tumor volume, and burden in urethane-induced lung carcinogenesis in mice. We demonstrated that the pterostilbene-mediated chemopreventive effects in vivo were a result of the inhibition of epidermal growth factor receptor its downstream pathways, leading to delayed cell cycle progression and the induction of apoptosis and autophagy during urethane-induced lung tumorigenesis [12]. Actually, our group was the first group to report the induction of autophagy in cancer cells by pterostilbene, and to reveal the prosurvival role of autophagy through the inhibition of apoptosis [10]. More recently, pterostilbene was shown to inhibit oxidized low-density lipoprotein-induced apoptosis in vascular endothelial cells through the induction of autophagy. The authors indicated that pterostilbene promoted autophagy via a rapid elevation in intracellular calcium concentration and subsequent (5′adenylic acid-activated protein kinase) AMPK activation, which in turn inhibited mammalian target of rapamycin (mTOR), a potent inhibitor of autophagy [15]. These findings provide a possibility that pterostilbene could serve as a potential candidate for developing a class of autophagy regulators as treatment for autophagy-related diseases.
In a recent review article, the authors highlighted the significance of autophagy regulation in skin disease [16]. They discussed the roles of autophagy in apoptosis, differentiation, inflammation, and the immune response, trying to reveal the possible involvement of autophagy in skin aging and other skin disorders. Because autophagy routinely plays a double-edged sword role in various conditions, its functions in skin homeostasis and its potential application as a therapeutic target for skin diseases remain to be clarified. Interestingly, pterostilbene has recently been demonstrated to effectively protect hairless mice against UVB radiation-induced skin damage and carcinogenesis [16]. In view of the potentially beneficial effects, our current review article summarizes the underlying mechanisms and pathways regarding anti-inflammation and chemopreventive effects by pterostilbene in the current literature. We also try to put forward a viewpoint that autophagy induction is a novel mechanism modulating the pterostilbene-induced protective effects against skin diseases. We attempt to highlight the possible underlying mechanisms and pathways reflecting the therapeutic potential of pterostilbene in skin diseases, based on the findings of recent studies. A more profound understanding of the protective mechanisms of pterostilbene through the induction of autophagy will contribute to the development of prevention and intervention strategies against different human diseases.
2. Anticancer and autophagy-inducing mechanisms of pterostilbene
Numerous studies have been conducted to evaluate the anti-cancer effects of pterostilbene and have suggested that pterostilbene inhibits cancer cell growth by inducing apoptosis, necrosis, and autophagy. In addition, pterostilbene inhibits adhesion, invasion, and metastasis in various cancer cells [2]. The molecular mechanisms of the anticancer effects of pterostilbene are discussed in some remarkable reviews written by McCormack and McFadden [2] and Kosuru et al [4]. Readers are encouraged to refer to them. For the remaining portion of this section listed below, we provide information on the novel anticancer mechanisms of pterostilbene regarding Janus kinase/signal transducers 3 (JAK/Stat3), AMPK signaling, epigenetic modulation, and autophagy.
A recent study conducted by Liu et al [17] indicated that pterostilbene treatment resulted in inhibition of osteosarcoma cell viability and a reduction in tumor cell adhesion, migration and mitochondrial membrane potential, but also resulted in increases in the apoptotic index and in the level of reactive oxygen species (ROS). Pterostilbene was observed to directly inhibit the phosphorylation of JAK2 and the downstream activation of Stat3, leading to the upregulation of mitochondrial apoptotic-related proteins and cyclin-dependent kinase inhibitors such as p21 and p27. This study suggested that inhibition of JAK2/Stat3 signaling is a novel mechanism of action for pterostilbene during therapeutic intervention in osteosarcoma cancers [17].
It becomes increasingly interesting that metabolic pathways may be altered during tumorigenesis and tumor progression. One aspect for metabolic reprogramming in cancer is the alteration of lipid metabolism [18]. Fatty acid synthase is a key enzyme for lipogenesis and is often highly expressed in human cancers such as prostate cancer. Activation of AMPK can alter lipogenesis by phosphorylating and inhibiting acetyl-CoA carboxylase, thereby blocking the commitment of acetyl-CoA to lipogenesis [18]. Therefore, the use of AMPK activators of key lipogenic enzymes may represent a promising therapeutic strategy for prostate cancer. In Lin et al’s [19] study, AMPK is activated by pterostilbene to decrease the activity and/or expression of the lipogenic enzymes fatty acid synthase and acetyl-CoA carboxylase, leading to growth inhibition in p53-positive and p53-negative prostate cancer cells. This study suggested that pterostilbene has beneficial activities similar to those associated with low-energy mimickers, and these might be related to certain uncharacterized direct actions of pterostilbene on cancer cells.
In addition to protein level, pterostilbene is thought to elicit anticancer effects by targeting genes with oncogenic function for de novo methylation and silencing, resulting in inactivation of related signaling pathways [20]. Lubecka et al [20] determined, for the first time, the genome-wide landscapes of DNA methylation with stilbenoids treatment. They found that stilbenoids target methylation genes with oncogenic and prometastatic functions, such as mastermind-like protein 2, the activator of the NOTCH pathway. Suppression of mastermind-like protein 2 results in inactivation of NOTCH signaling, which is important in breast cancer development and oncogenic functions. The study provided novel insight into the epigenetic-anticancer strategies of pterostilbene [20].
The role of autophagy in tumorigenesis is complex and likely tissue- and genetic context-dependent. Autophagy provides a barrier against malignant transformation and is required for anti-cancer immunosurveillance. Conversely, autophagy promotes tumor progression and thereby resistance to cancer therapy [21]. Importantly, high levels of autophagic activity can lead to cell death and cooperation with apoptosis. Thus, autophagy modulation has been proposed as both a cancer therapeutic and preventative strategy. If autophagy promotes cell survival, autophagy inhibitors may provide benefits to synergize with anticancer drugs, whereas triggering autophagy may also help the therapeutic outcome whenever autophagy supports cell death [22]. Autophagy is a tightly regulated pathway. mTOR negatively regulates the activation of autophagy that it interacts with Atg13, and then reduces its affinity for Atg1/ULK1 and Atg1/ULK1 activity. By contrast, upon the induction of autophagy, Atg1/ULK1 kinase and its complex components translocate to the preautophagosomal structure, leading to the recruitment of the class III PI3K complex (includes Vps34, Vps15, Atg6/Beclin-1, and Atg14). At the step of autophagosome formation, elongation and closure of the isolation membrane requires two protein conjugation systems, the Atg12–Atg5–Atg16 complex and the Atg8/LC3-PE complex. Atg8 is then processed by the protease Atg4 and is conjugated with PE by the Atg7 and Atg3 (E2-like) enzymes [6]. The activation of several proteins such as ULK1 and Atg13 are activated by AMPK, which is crucial for autophagy initiation. Autophagosomes are then conjugated with lysosomes to form autolysosomes and subsequently degrade macromolecular cargos to generate ATP, fatty acids, or amino acids for cell survival [21].
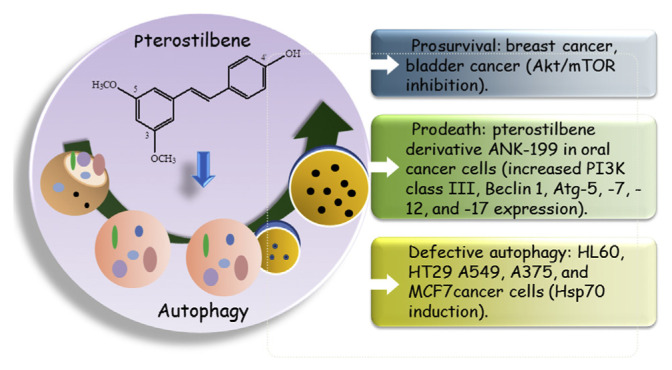
The studies regarding pterostilbene-induced autophagy in cancer cells have attracted more and more attention recently (Figure 1). For example, in terms of the protective effect of autophagy, we previously reported that pterostilbene significantly inhibited cell proliferation in chemosensitive and chemoresistant bladder cancer cells through cell cycle arrest and apoptosis. Meanwhile, pterostilbene-induced protective autophagy in bladder cancer cells evidenced by the finding that inhibition of autophagy enhanced cell death in response to pterostilbene [10]. Consistently, pterostilbene has been reported to induce the accumulation of autophagic vacuoles in various cancer types. Chen et al [23] investigated pterostilbene-induced cell death by apoptosis and cytoprotective autophagy in triple negative breast cancer. Similarly, Wang et al [24] found that pterostilbene could evidently inhibit the growth of breast cancer cells via inducing both apoptosis and cell cycle arrest and promoted the reduction of β-catenin levels and the downregulation of genes regulated by the Wnt signaling pathway. The pterostilbene-triggered autophagy in those cases seems to be cyto-protective, indicating that the combination of autophagy inhibitors and pterostilbene with classical chemotherapy could serve as a potent strategy for the treatment of breast cancer cells [24].
Figure 1.
Possible regulation mechanisms of pterostilbene on autophagy in cancer cells. Pterostilbene significantly inhibited cell proliferation, induced cell cycle arrest, and prosurvival autophagy in bladder and breast cancer cells. ANK-199, the pterostilbene derivative, induced autophagic cell death in oral cancer cells. In contrast, pterostilbene induced cell death concomitant with autophagosome accumulation and defective autophagy observed in HL60, A375 melanoma, A549 lung, MCF7 breast, and HT29 colon cancer cells. mTOR = mechanistic target of rapamycin.
Contradictory results were also reported in the literature. A novel pterostilbene derivative, ANK-199, was designed and investigated for its antitumor activity and mechanism in cisplatin-resistant human oral cancer cells by Hsieh et al’s [25] group. In the study, ANK-199 showed an extremely low toxicity in normal oral cell lines, while the formation of autophagic vacuoles and acidic vesicular organelles was observed in ANK-199-treated cancer cells. Neither DNA fragmentation nor DNA condensation was observed, indicating that autophagy, but not apoptosis, was triggered by ANK-199-induced cell death [25].
Additionally, some studies indicated that pterostilbene may impair autophagy in cancer cells. For instance, Siedlecka-Kroplewska et al [26] tried to evaluate the effects of pterostilbene on HL60 human leukemia cells. They found that pterostilbene treatment resulted in G0/G1 cell cycle arrest and the accumulation of large LC3-positive vacuolar structures followed by cell death in HL60 cells; this suggested that pterostilbene-treated HL60 cells could be affected by both apoptosis and presumably defective autophagy [26]. Mena et al [27] also reported that pterostilbene suppressed cancer cell growth significantly and led to apoptosis and autophagosome accumulation in various cancer cells, such as A375 melanoma, A549 lung, MCF7 breast, and HT29 colon cancer cells. In this study, pterostilbene induced an increase in the size of lysosomes, lysosomal membrane destabilization, and intraluminal content release leading to caspase-independent lysosomal cell death. The fusion of the autophagosome and lysosome in this model was altered [27].
As a natural compound, pterostilbene has been shown to suppress proliferation and induce apoptosis in a variety of tumor cells, including pancreas, bladder, breast, colon, oral, lung, melanoma, myeloma, leukemia, and prostate carcinomas. Although the dominant target of pterostilbene is still unclear, pterostilbene is known to affect multiple signaling pathways regulating tumor growth through AMPK, JAK/Stat3, ROS, cell cycle regulation, and apoptosis [17]. Nevertheless, the anticancer effects of pterostilbene through autophagy have not yet been clarified. Autophagy is well recognized as a cell survival process that inhibits malignant transformation, promotes tumor development, or participates in a form of programmed cell death. The induction of autophagy by some anticancer agents highlights the potential of this process as a cancer treatment modality. Further studies are required to understand the molecular signaling pathways and the significance of autophagy triggered by pterostilbene.
3. Antioxidation and -inflammation mechanisms of pterostilbene
The multiple benefits of pterostilbene in the treatment and prevention of human disease have been attributed to its antioxidative, -inflammatory, and -carcinogenic properties [14]. The antioxidative effects of pterostilbene were attributed to its unique structure (with 1 hydroxyl group and 2 methoxy groups) that may scavenge extracellular ROS [28]. These effects allowed the use of pterostilbene to diminish free radicals that are responsible for tissue damage during chronic inflammation. A previous review article summarized the clinical potential and antioxidant capabilities of pterostilbene in several disease systems [14]. In our current review article, we only focus on the recent novel findings of antioxidative and -inflammatory mechanisms of pterostilbene. The specific items are listed below.
3.1. Proteasome inhibition effect
In many studies, endotoxin lipopolysaccharide (LPS) has been used to stimulate the mouse macrophage RAW264.7 cell line to produce proinflammatory cytokines. Nikhil et al [29] reported that pterostilbene has a strong anti-nuclear factor-κB (anti-NFκB) and anti-inflammatory property in LPS-stimulated RAW264.7 macrophages and carrageenan-induced rat paw edema models [29]. Pterostilbene decreased the level of NO and suppressed the expression of tumor necrosis factor-α (TNF-α), interleukin (IL)-1β, IL-6, and iNOS genes in the LPS-induced RAW264.7 inflammation model. Pterostilbene treatment could also significantly reduce NFκB activation in LPS-stimulated HEK293T cells [30]. Interestingly, this study clearly demonstrates that pterostilbene is a particularly potent proteasome inhibitor that contributes to the underlying mechanism of its own anti-inflammatory effects. Several naturally occurring proteasome inhibitors (e.g., polyphenols and δ-tocotrienol) reduce the production of iNOS, NO, and TNF-α in RAW 264.7 cells and murine macrophages in vitro stimulated by LPS [31,32]. Proteasome inhibitors can exert their effects by impacting transcription factors such as NFκB, thereby altering gene expression levels. They can also alter the ubiquitin-proteasome pathway, which is one of the major pathways for intracellular protein degradation [33].
3.2. Silent information regulator 1 activating effect
Silent information regulator 1 (SIRT1) is a nicotinamide adenine dinucleotide+-dependent class III histone and protein deacetylase that regulates cellular functions including energy metabolism, cell survival, and inflammatory response [34]. Previous studies indicated that ischemia–reperfusion (IR) injury could induce segmental necrosis and apoptosis, myofilament disintegration, thicker interstitial spaces, inflammatory cell infiltration, and decreased mitochondrial respiratory chain activity. Pterostilbene was observed to inhibit these effects in a dose-dependent manner. The mechanism of IR injury is attributed to the SIRT1-FOXO1/p53 signaling pathway, as well as the increase in the Bax and Bcl2 ratio, cleaved PARP1, and cleaved caspase 3. The application of the SIRT1 inhibitor EX527 in this model decreased SIRT1 expression and increased the acetylation of FOXO1, thereby reducing the defensive effects of pterostilbene against skeletal muscle IR injury [34]. Another study conducted by Guo et al [35] demonstrated that hypoxia–reoxygenation, an in vitro model of IR injury, could induce H9c2 cardiomyocyte apoptosis. Application of pterostilbene at lower concentrations can prevent hypoxia–reoxygenation-induced H9c2 apoptosis. Similar to Cheng et al’s [34] study, the protective mechanism of pterostilbene contributed to activation of SIRT1 via the FOXO and p53 pathways, leading to protection against apoptosis and alleviation of IR injury [35]. These studies indicated that pterostilbene could be a specific and potent pharmacological activator of SIRT1 and could be used as a cytoprotective agent against IR injury.
3.3. Nuclear factor erythroid 2-related factor2 activating effect
Nuclear factor erythroid 2-related factor2 (Nrf2) is a transcription factor that regulates the production of multiple antioxidative enzymes. Nrf2 has protective effects in various organs such as the liver, brain, heart, and neuronal cells through ROS attenuation mechanisms via its association with the microtubule-associated protein Kelch-like ECH-associated protein-1 (Keap1) [36]. Our previous reports showed that pterostilbene significantly enhanced expression of antioxidant enzymes via activation of Nrf2 signaling and reduction of NFκB activation by inhibiting the phosphorylation of protein kinase C-β2 in an azoxymethane-induced colon tumorigenesis mouse model [37]. Similarly, Wang et al [36] indicated that pterostilbene induced the nuclear translocation of Nrf2 and upregulated HO-1 and NQO1 thereby reducing the glutamate-induced cellular oxidative stress levels in murine hippocampal neuronal HT22 cells [36]. A recent study indicated that pterostilbene has anti-hyperlipidemic and -peroxidative roles via Nrf2 signaling in experimental diabetes models [38]. It is also known that pterostilbene ameliorates streptozotocin-induced diabetes by enhancing Nrf2-mediated antioxidant signaling pathways [39]. Nrf2 regulates the activities of multiple anti-oxidative enzymes resulting in a wide ranging protective effect in various organs; the potent Nrf2 activator pterostilbene is thought to remove and counteract the oxidative stress-induced diseases.
3.4. Inhibition of endoplasmic reticulum stress mediated inflammation
Endoplasmic reticulum (ER) function is critical for the regulation of many aspects of cell physiology and pathological processes. Disturbance in the normal functions of the ER induces ER stress leading to the accumulation of unfolded or misfolded proteins and consequently activation of the unfolded protein response (UPR) [40]. Followed by UPR, the ER stress sensors PKR-like ER kinase, inositol-requiring protein 1, and activating transcription factor 6 become active. Under normal conditions, these molecules are inactive due to interactions with glucose-regulated protein 78 (GRP78). However, when there is an increase in UPR, GRP78 is disaggregated and binds to unfolded proteins to promote protein folding; additionally, UPR signaling is activated, leading to a decrease in global protein synthesis and an increase in ER-associated degradation, which attenuates ER stress and restores normal ER function [41]. Inositol-requiring protein 1 is associated with phosphorylation of JNK leading to the activation of the transcription factors AP-1 and p53, which are essential for the transcription of the proapoptotic genes and genes implicated in the processes of autophagy [42]. Previous studies have confirmed that ER stress is involved in the process of endothelial cell inflammation and inhibition of ER stress may effectively attenuate inflammatory responses in endothelial cells [43]. In Liu et al’s [41] study, levels of GRP78 and p-eIF2α, which represent the degree of ER stress, were significantly increased in HUVECs after TNF-α treatment. Interesting, TNF-α-induced upregulation of GRP78 and p-eIF2α and the subsequent inflammatory response were potently prevented by pterostilbene treatment. Upregulation of ER stress signaling desensitizes the protective effect of pterostilbene on endothelial cell inflammatory injury induced by TNF-α, whereas the attenuation of ER stress exerts an anti-inflammatory effect on endothelial cells. Above all, the study suggested that pterostilbene can act as an anti-inflammatory agent in the endothelial inflammatory process, which at least in part depends on a reduction of ER stress signaling.
3.5. Free radical scavenging effects
Cellular damage caused by hydrogen peroxide is a subject of great importance, as the generated ROS can harm macromolecules such as proteins, lipids, and DNA, thereby inducing cell death, degenerative diseases, and tumorigenesis [44]. One way of counteracting free radical damage is through dietary antioxidant such as plant polyphenols. In line with this notion, Rossi et al [44] demonstrated that resveratrol and pterostilbene improve hydrogen peroxide-mediated oxidative damage of DNA in CHO cells. The mechanism of action is correlated to stilbene scavenging of OH radicals through an electron transfer process. The authors also showed that pterostilbene provided greater protective effects on DNA damage than resveratrol. Similarly, another study also reported that pterostilbene possesses strong antioxidant activity and protected cellular biomolecules against oxidative damage through scavenging 1,1-diphenyl-2-picrylhydrazyl, superoxide, hydroxyl, and H2O2, and it inhibited 2,2′-azinobis-3-ethylbenzthiazoline-6-sulphonic acid radical formation in a dose-dependent manner [45]. This could be attributed to the ability of pterostilbene to act as a donor of hydrogen atoms or electrons. Free radicals generated in vivo as a result of cellular respiration have a very short half-life, and the clearance rate of these radicals is very rapid. Taking this into consideration, pterostilbene exhibited radical scavenging activity, indicating its ability to react with radicals within a short span of time, as needed in biological systems.
Overall, pterostilbene has been confirmed to be a protective factor in inflammatory conditions through various mechanisms. In addition to the ROS scavenging effects, pterostilbene also exerts inhibitory effects against neutrophil activation, inflammatory mediator production, and endothelial apoptosis in different models [41]. All of these studies indicated that the major health benefits of pterostilbene could be attributed to the modulation of inflammation responses.
4. Preventive/therapeutic effects of pterostilbene on skin diseases
Skin is the largest organ of the body and serves as the first-line barrier against many environmental insults including UV radiation (UVR), pathogens, mechanical stresses, and toxic chemicals. Previous studies indicated that polyphenolic phytochemicals possessing anti-inflammatory, immunomodulatory, antioxidant, and chemopreventive effects are promising group of compounds that can act as preventive or therapeutic agents for skin disorders, including skin cancer [16]. In the skin carcinogenesis model, application of 12-O-tetradeca-noylphorbol-13-acetate (TPA) to mice skin promotes 7,12-dimethylbenz[a]anthracene initiated mouse papilloma formation by enhancing iNOS, COX-2, and ornithine decarboxylase protein expression. Pterostilbene administered directly to the mouse skin prior to TPA application reduced TPA-induced phosphorylation of p38, JNK, ERK, PI3K, and Akt in mouse skin. TPA-induced protein levels of iNOS and COX-2 were inhibited by pterostilbene through inactivation of NFκB and the upstream p38 MAP kinases, which provides a mechanistic basis for its anti-inflammatory and -tumor promoting activity in mouse skin [46]. Many studies have indicated that skin cancer incidences are rising worldwide, and one of the major causative factors is excessive exposure to solar UVR [47]. Induction of DNA damage by UVR may induce gene mutation and genomic instability leading to carcinogenesis. Moreover, UVB (280–320 nm) is known to be the most potent mutagenic component causing direct damage to cellular DNA as well as producing ROS in the epidermis, dermis, and the corneal epithelium; both processes induce inflammation, oxidative stress, dysregulation of signaling pathways, and immunosuppression, all of which are factors in skin cancer [16]. Sireol et al [16] reported that pterostilbene prevented acute UVB-induced increases in skin folds, thickness, redness, skin wrinkling, and hyperplasia. In addition, pterostilbene could provide preventive effects against chronic UVB-induced skin carcinogenesis. The anticarcinogenic effects of pterostilbene were associated with maintenance of the skin antioxidant defenses systems, and the inhibition of UVB induced oxidative damage, which may be mediated by modulation of Nrf2 signaling. It has been reported that Nrf2 could serve as a central regulator of UV protection in the epidermis [16].
Recent studies indicated the damaged skin cells can be eliminated by the induction of apoptosis, and the damaged cellular components may be eliminated by autophagy [16]. With regard to UVR, autophagy could contribute to the maintenance of UV-damaged cells because of the major regulator UV radiation resistance associated gene (UVRAG) protein providing resistance against UV. Knockdown of UV radiation resistance-associated gene has been shown to reduce UV-induced autophagy in favor of apoptosis [48]. Induction of autophagy is also likely to be regulated by UV-induced p53 and be able to initiate autophagy through negative regulation of mTOR by p53 in response to DNA damage, as well as in response to ROS by AMPK activated downstream of growth factor receptors or through ataxia telangiectasia mutated (ATM) [49]. In line with this notion, silibinin was reported to rescue the cells from caspase-8-dependent apoptosis induced by UVB irradiation through upregulating autophagy, and this effect was modulated through the insulin-like growth factor 1 receptor/protein kinase B axis [17]. Therefore, we suggest that pterostilbene acts as an autophagy activator and might protect against UVR damage in the skin through elevated levels of autophagy; the mechanisms are worthy of further in-depth investigation.
An increasing number of studies have recently shown that autophagy has important effects on the induction of the inflammatory reaction [50]. Upon stimulation, NLRP3 assembles with apoptotic speck protein containing a caspase recruitment domain and procaspase-1, creating inflammasome responsible for the activation of caspase-1 and -5, which ultimately leads to the proteolytic activation of the proinflammatory cytokines IL-1β and IL-18 [51]. Autophagy is reported to remove aggregated inflammasome structures, thus contributing to the dampening of proinflammatory responses. If the function of autophagy is defective, it could lead to an accumulation of depolarized mitochondria and the release of inflammasome activators such as ROS or mitochondrial DNA [50]. Autophagy not only has inhibitory effects on inflammasome activation, but also on inflammatory mediators that are independent of caspase-1 activation. In addition, autophagy reduces NFκB activation by selective degradation of BCL10 complexes [50]. Thus, autophagy is tightly connected with skin homeostasis and might serve a critical role in the development and progression of skin diseases [52]. It has been reported that certain pharmaceutical agents that can induce autophagy could be novel therapeutic candidates for psoriasis. Psoriasis is a chronic autoimmune skin disease, and the precise mechanisms are still poorly understood. Psoriasis is pathologically characterized by inflammation, epidermal proliferation, and infection. Recent studies showed that autophagy negatively regulates the expression of the ubiquitin sensor p62, and knockdown of p62 reduces the production of inflammatory cytokines and cell proliferation [53]. Remarkably, epidermal expression of p62, which is an indicator of autophagic defect, was found to be significantly higher in psoriatic skin than in healthy controls [53]. Recent studies also indicated that autophagy inducers could be used to treat skin hyper-pigmentation disorders, such as chloasma [54]. Moreover, skin is important to defend against invading pathogens and to maintain cellular homeostasis. One critical mechanism for self-defense is autophagy in which various microbes can be engulfed by autophagosomes and transferred to lysosomes for degradation, suggesting that autophagy upregulation might be of therapeutic benefit in infectious skin diseases [55]. In addition, little is known about the relationship between autophagy and burn wound progression. A number of mechanisms are thought to be involved in the process of burn wound progression, including local tissue hypoperfusion, edema, prolonged inflammation, hypercoagulability, free radical damage, and accumulation of cytotoxic cytokines. A recent study conducted by Xiao et al [56] revealed reduced levels of autophagy and blood flow together with increased levels of inflammation and apoptosis during the early course of burn wound progression in a rodent model. These findings suggested that autophagy and apoptosis play complementary roles in the process of burn wound progression.
Pterostilbene is reported to modulate autophagy not only in cancer cells but also in normal cells. Zhang et al [15] reported for the first time that pterostilbene could effectively induce cytoprotective autophagy in human umbilical vein endothelial cells via a rapid elevation in intracellular calcium concentration and AMPKα1 activation, which in turn inhibits mTOR, a negative regulator of autophagy. Autophagy activators are of interest because of their potential clinical value for skin disorders due to their anti-inflammation and cytoprotective effects [57]. We anticipate that the autophagy-inducing potential of pterostilbene may lead to the development of novel strategies for preventive and therapeutic purposes in skin diseases.
5. Conclusion and perspectives
Numerous studies have shown that pterostilbene exerts different mechanisms in different disease systems. Depending on the cell type and the chemical properties and dose of the stimulus, pterostilbene might provide benefits against progressive cellular damage and dysfunction in different ways. In cancer cells, pterostilbene can induce apoptosis, decrease proliferation, induce cell cycle arrest, inhibit metastasis, and induce autophagy. Moreover, pterostilbene possesses anti-inflammation and -oxidative stress effects, as we have mentioned above. Due to the etiology of many diseases being attributed and related to inflammation, chronic inflammation is thought to be associated with several important human cancers and skin disorders. Modulation of inflammatory effects by pterostilbene seems to be a possible and promising strategy to prevent and treat skin disorders.
Inflammation is a complex biological process that involves various inflammatory mediators and cytokines. Numerous studies have confirmed the association between inflammation and skin disease. Recent new insights strongly suggest that besides the classical role as a “housekeeping” mechanism, autophagy can also be considered crucial for host defense in general and for regulation of inflammation in particular. Pterostilbene was found to be a unique autophagy inducer that also downregulates inflammation and ROS in cells. However, the biological consequences of autophagy induction by pterostilbene are controversial because both prosurvival and prodeath autophagy, and even defective autophagy, could be observed (Figure 1). Further studies are needed to better understand the molecular mechanisms of autophagy induced by pterostilbene in different disease systems. Several recent articles postulate that autophagy upregulation may have therapeutic benefits in a range of diseases [57]. New research related to autophagy activators has become a hot topic owing to their potential clinical value. Considering the fact that skin disorders including skin cancer are strongly correlated with inflammation, pterostilbene acing as an autophagy inducer offers a unique and novel option to better manage and reduce skin disorders by reducing inflammation through autophagy.
Acknowledgments
This study was supported by the Ministry of Science and Technology, Taiwan (MOST 105-2320-B-006-021 and MOST 103-2321-B-006-019-MY3).
Funding Statement
This study was supported by the Ministry of Science and Technology, Taiwan (MOST 105-2320-B-006-021 and MOST 103-2321-B-006-019-MY3).
Footnotes
Conflicts of interest
The authors have nothing to disclose.
REFERENCES
- 1. Bavaresco L, Fregoni C, Cantu E, Trevisan M. Stilbene compounds: from the grapevine to wine. Drugs Exp Clin Res. 1999;25:57–63. [PubMed] [Google Scholar]
- 2. McCormack D, McFadden D. Pterostilbene and cancer: current review. J Surg Res. 2012;173:e53–61. doi: 10.1016/j.jss.2011.09.054. [DOI] [PubMed] [Google Scholar]
- 3. Kapetanovic IM, Muzzio M, Huang Z, Thompson TN, McCormick DL. Pharmacokinetics, oral bioavailability, and metabolic profile of resveratrol and its dimethylether analog, pterostilbene, in rats. Cancer Chemother Pharmacol. 2011;68:593–601. doi: 10.1007/s00280-010-1525-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kosuru R, Rai U, Prakash S, Singh A, Singh S. Promising therapeutic potential of pterostilbene and its mechanistic insight based on preclinical evidence. Eur J Pharmacol. 2016;789:229–43. doi: 10.1016/j.ejphar.2016.07.046. [DOI] [PubMed] [Google Scholar]
- 5. Zhong Z, Sanchez-Lopez E, Karin M. Autophagy, inflammation, and immunity: a troika governing cancer and its treatment. Cell. 2016;166:288–98. doi: 10.1016/j.cell.2016.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lin L, Baehrecke EH. Autophagy, cell death, and cancer. Mol Cell Oncol. 2015;2:e985913. doi: 10.4161/23723556.2014.985913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chiu HW, Lin JH, Chen YA, Ho SY, Wang YJ. Combination treatment with arsenic trioxide and irradiation enhances cell-killing effects in human fibrosarcoma cells in vitro and in vivo through induction of both autophagy and apoptosis. Autophagy. 2010;6:353–65. doi: 10.4161/auto.6.3.11229. [DOI] [PubMed] [Google Scholar]
- 8. Chiu HW, Lin SW, Lin LC, Hsu YH, Lin YF, Ho SY, Wu YH, Wang YJ. Synergistic antitumor effects of radiation and proteasome inhibitor treatment in pancreatic cancer through the induction of autophagy and the downregulation of TRAF6. Cancer Lett. 2015;365:229–39. doi: 10.1016/j.canlet.2015.05.025. [DOI] [PubMed] [Google Scholar]
- 9. Chiu HW, Lin W, Ho SY, Wang YJ. Synergistic effects of arsenic trioxide and radiation in osteosarcoma cells through the induction of both autophagy and apoptosis. Radiat Res. 2011;175:547–60. doi: 10.1667/RR2380.1. [DOI] [PubMed] [Google Scholar]
- 10. Chen RJ, Ho CT, Wang YJ. Pterostilbene induces autophagy and apoptosis in sensitive and chemoresistant human bladder cancer cells. Mol Nutr Food Res. 2010;54:1819–32. doi: 10.1002/mnfr.201000067. [DOI] [PubMed] [Google Scholar]
- 11. Arico S, Petiot A, Bauvy C, Dubbelhuis PF, Meijer AJ, Codogno P, Ogier-Denis E. The tumor suppressor PTEN positively regulates macroautophagy by inhibiting the phosphatidylinositol 3-kinase/protein kinase B pathway. J Biol Chem. 2001;276:35243–6. doi: 10.1074/jbc.C100319200. [DOI] [PubMed] [Google Scholar]
- 12. Chen RJ, Tsai SJ, Ho CT, Pan MH, Ho YS, Wu CH, Wang YJ. Chemopreventive effects of pterostilbene on urethane-induced lung carcinogenesis in mice via the inhibition of EGFR-mediated pathways and the induction of apoptosis and autophagy. J Agric Food Chem. 2012;60:11533–41. doi: 10.1021/jf302778a. [DOI] [PubMed] [Google Scholar]
- 13. Chiou YS, Tsai ML, Wang YJ, Cheng AC, Lai WM, Badmaev V, Ho CT, Pan MH. Pterostilbene inhibits colorectal aberrant crypt foci (ACF) and colon carcinogenesis via suppression of multiple signal transduction pathways in azoxymethane-treated mice. J Agric Food Chem. 2010;58:8833–41. doi: 10.1021/jf101571z. [DOI] [PubMed] [Google Scholar]
- 14. McCormack D, McFadden D. A review of pterostilbene antioxidant activity and disease modification. Oxid Med Cell Longev. 2013;2013:575482. doi: 10.1155/2013/575482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhang L, Cui L, Zhou G, Jing H, Guo Y, Sun W. Pterostilbene, a natural small-molecular compound, promotes cytoprotective macroautophagy in vascular endothelial cells. J Nutr Biochem. 2013;24:903–11. doi: 10.1016/j.jnutbio.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 16. Sirerol JA, Feddi F, Mena S, Rodriguez ML, Sirera P, Aupi M, Perez S, Asensi M, Ortega A, Estrela JM. Topical treatment with pterostilbene, a natural phytoalexin, effectively protects hairless mice against UVB radiation-induced skin damage and carcinogenesis. Free Radic Biol Med. 2015;85:1–11. doi: 10.1016/j.freeradbiomed.2015.03.027. [DOI] [PubMed] [Google Scholar]
- 17. Liu W, Otkur W, Li L, Wang Q, He H, Ye Y, Zhang Y, Hayashi T, Tashiro S, Onodera S, Ikejima T. Autophagy induced by silibinin protects human epidermoid carcinoma A431 cells from UVB-induced apoptosis. J Photochem Photobiol B-Biol. 2013;123:23–31. doi: 10.1016/j.jphotobiol.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 18. Peck B, Schulze A. Lipid desaturation - the next step in targeting lipogenesis in cancer? FEBS J. 2016;283:2767–78. doi: 10.1111/febs.13681. [DOI] [PubMed] [Google Scholar]
- 19. Lin VC, Tsai YC, Lin JN, Fan LL, Pan MH, Ho CT, Wu JY, Way TD. Activation of AMPK by pterostilbene suppresses lipogenesis and cell-cycle progression in p53 positive and negative human prostate cancer cells. J Agric Food Chem. 2012;60:6399–407. doi: 10.1021/jf301499e. [DOI] [PubMed] [Google Scholar]
- 20. Lubecka K, Kurzava L, Flower K, Buvala H, Zhang H, Teegarden D, Camarillo I, Suderman M, Kuang S, Andrisani O, Flanagan JM, Stefanska B. Stilbenoids remodel the DNA methylation patterns in breast cancer cells and inhibit oncogenic NOTCH signaling through epigenetic regulation of MAML2 transcriptional activity. Carcinogenesis. 2016;37:656–68. doi: 10.1093/carcin/bgw048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Galluzzi L, Bravo-San Pedro JM, Kroemer G. Defective autophagy initiates malignant transformation. Mol Cell. 2016;62:473–4. doi: 10.1016/j.molcel.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 22. Rufini A, Melino G. Cell death pathology: the war against cancer. Biochem Biophys Res Commun. 2011;414:445–50. doi: 10.1016/j.bbrc.2011.09.110. [DOI] [PubMed] [Google Scholar]
- 23. Chen WC, Hsu KY, Hung CM, Lin YC, Yang NS, Ho CT, Kuo SC, Way TD. The anti-tumor efficiency of pterostilbene is promoted with a combined treatment of Fas signaling or autophagy inhibitors in triple negative breast cancer cells. Food Funct. 2014;5:1856–65. doi: 10.1039/c4fo00145a. [DOI] [PubMed] [Google Scholar]
- 24. Wang Y, Ding L, Wang X, Zhang J, Han W, Feng L, Sun J, Jin H, Wang XJ. Pterostilbene simultaneously induces apoptosis, cell cycle arrest and cyto-protective autophagy in breast cancer cells. Am J Transl Res. 2012;4:44–51. [PMC free article] [PubMed] [Google Scholar]
- 25. Hsieh MT, Chen HP, Lu CC, Chiang JH, Wu TS, Kuo DH, Huang LJ, Kuo SC, Yang JS. The novel pterostilbene derivative ANK-199 induces autophagic cell death through regulating PI3 kinase class III/beclin 1/Atgrelated proteins in cisplatinresistant CAR human oral cancer cells. Int J Oncol. 2014;45:782–94. doi: 10.3892/ijo.2014.2478. [DOI] [PubMed] [Google Scholar]
- 26. Siedlecka-Kroplewska K, Jozwik A, Boguslawski W, Wozniak M, Zauszkiewicz-Pawlak A, Spodnik JH, Rychlowski M, Kmiec Z. Pterostilbene induces accumulation of autophagic vacuoles followed by cell death in HL60 human leukemia cells. J Physiol Pharmacol. 2013;64:545–56. [PubMed] [Google Scholar]
- 27. Mena S, Rodriguez ML, Ponsoda X, Estrela JM, Jaattela M, Ortega AL. Pterostilbene-induced tumor cytotoxicity: a lysosomal membrane permeabilization-dependent mechanism. PloS One. 2012;7:e44524. doi: 10.1371/journal.pone.0044524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Perecko T, Jancinova V, Drabikova K, Nosal R, Harmatha J. Structure-efficiency relationship in derivatives of stilbene. Comparison of resveratrol, pinosylvin and pterostilbene. Neuro Endocrinol Lett. 2008;29:802–5. [PubMed] [Google Scholar]
- 29. Nikhil K, Sharan S, Palla SR, Sondhi SM, Peddinti RK, Roy P. Understanding the mode of action of a pterostilbene derivative as anti-inflammatory agent. Int Immunopharmacol. 2015;28:10–21. doi: 10.1016/j.intimp.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 30. Qureshi AA, Guan XQ, Reis JC, Papasian CJ, Jabre S, Morrison DC, Qureshi N. Inhibition of nitric oxide and inflammatory cytokines in LPS-stimulated murine macrophages by resveratrol, a potent proteasome inhibitor. Lipids Health Dis. 2012;11:76. doi: 10.1186/1476-511X-11-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Qureshi AA, Reis JC, Qureshi N, Papasian CJ, Morrison DC, Schaefer DM. delta-Tocotrienol and quercetin reduce serum levels of nitric oxide and lipid parameters in female chickens. Lipids Health Dis. 2011;10:39. doi: 10.1186/1476-511X-10-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Qureshi AA, Tan X, Reis JC, Badr MZ, Papasian CJ, Morrison DC, Qureshi N. Suppression of nitric oxide induction and pro-inflammatory cytokines by novel proteasome inhibitors in various experimental models. Lipids Health Dis. 2011;10:177. doi: 10.1186/1476-511X-10-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nam NH. Naturally occurring NF-κB inhibitors. Mini Rev Med Chem. 2006;6:945–51. doi: 10.2174/138955706777934937. [DOI] [PubMed] [Google Scholar]
- 34. Cheng Y, Di S, Fan C, Cai L, Gao C, Jiang P, Hu W, Ma Z, Jiang S, Dong Y, Li T, Wu G, Lv J, Yang Y. SIRT1 activation by pterostilbene attenuates the skeletal muscle oxidative stress injury and mitochondrial dysfunction induced by ischemia reperfusion injury. Apoptosis. 2016;21:905–16. doi: 10.1007/s10495-016-1258-x. [DOI] [PubMed] [Google Scholar]
- 35. Guo Y, Zhang L, Li F, Hu CP, Zhang Z. Restoration of sirt1 function by pterostilbene attenuates hypoxia-reoxygenation injury in cardiomyocytes. Eur J Pharmacol. 2016;776:26–33. doi: 10.1016/j.ejphar.2016.02.052. [DOI] [PubMed] [Google Scholar]
- 36. Wang B, Liu H, Yue L, Li X, Zhao L, Yang X, Wang X, Yang Y, Qu Y. Neuroprotective effects of pterostilbene against oxidative stress injury: involvement of nuclear factor erythroid 2-related factor 2 pathway. Brain Res. 2016;1643:70–9. doi: 10.1016/j.brainres.2016.04.048. [DOI] [PubMed] [Google Scholar]
- 37. Chiou YS, Tsai ML, Nagabhushanam K, Wang YJ, Wu CH, Ho CT, Pan MH. Pterostilbene is more potent than resveratrol in preventing azoxymethane (AOM)-induced colon tumorigenesis via activation of the NF-E2-related factor 2 (Nrf2)-mediated antioxidant signaling pathway. J Agric Food Chem. 2011;59:2725–33. doi: 10.1021/jf2000103. [DOI] [PubMed] [Google Scholar]
- 38. Bhakkiyalakshmi E, Dineshkumar K, Karthik S, Sireesh D, Hopper W, Paulmurugan R, Ramkumar KM. Pterostilbene-mediated Nrf2 activation: Mechanistic insights on Keap1:Nrf2 interface. Bioorg Med Chem. 2016;24:3378–86. doi: 10.1016/j.bmc.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 39. Elango B, Dornadula S, Paulmurugan R, Ramkumar KM. Pterostilbene Ameliorates streptozotocin-induced diabetes through enhancing antioxidant signaling pathways mediated by Nrf2. Chem Res Toxicol. 2016;29:47–57. doi: 10.1021/acs.chemrestox.5b00378. [DOI] [PubMed] [Google Scholar]
- 40. Wang G, Liu K, Li Y, Yi W, Yang Y, Zhao D, Fan C, Yang H, Geng T, Xing J, Zhang Y, Tan S, Yi D. Endoplasmic reticulum stress mediates the anti-inflammatory effect of ethyl pyruvate in endothelial cells. PloS One. 2014;9:e113983. doi: 10.1371/journal.pone.0113983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu J, Fan C, Yu L, Yang Y, Jiang S, Ma Z, Hu W, Li T, Yang Z, Tian T, Duan W, Yu S. Pterostilbene exerts an anti-inflammatory effect via regulating endoplasmic reticulum stress in endothelial cells. Cytokine. 2016;77:88–97. doi: 10.1016/j.cyto.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 42. Hassan M, Selimovic D, Hannig M, Haikel Y, Brodell RT, Megahed M. Endoplasmic reticulum stress-mediated pathways to both apoptosis and autophagy: significance for melanoma treatment. World J Exp Med. 2015;5:206–17. doi: 10.5493/wjem.v5.i4.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Parhiz H, Roohbakhsh A, Soltani F, Rezaee R, Iranshahi M. Antioxidant and anti-inflammatory properties of the citrus flavonoids hesperidin and hesperetin: an updated review of their molecular mechanisms and experimental models. Phytother Res. 2015;29:323–31. doi: 10.1002/ptr.5256. [DOI] [PubMed] [Google Scholar]
- 44. Rossi M, Caruso F, Antonioletti R, Viglianti A, Traversi G, Leone S, Basso E, Cozzi R. Scavenging of hydroxyl radical by resveratrol and related natural stilbenes after hydrogen peroxide attack on DNA. Chem Biol Interact. 2013;206:175–85. doi: 10.1016/j.cbi.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 45. Acharya JD, Ghaskadbi SS. Protective effect of Pterostilbene against free radical mediated oxidative damage. BMC Complement Altern Med. 2013;13:238. doi: 10.1186/1472-6882-13-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tsai ML, Lai CS, Chang YH, Chen WJ, Ho CT, Pan MH. Pterostilbene, a natural analogue of resveratrol, potently inhibits 7,12-dimethylbenz[a]anthracene (DMBA)/12-O-tetradecanoylphorbol-13-acetate (TPA)-induced mouse skin carcinogenesis. Food Funct. 2012;3:1185–94. doi: 10.1039/c2fo30105a. [DOI] [PubMed] [Google Scholar]
- 47. Kumar R, Deep G, Agarwal R. An overview of ultraviolet b radiation-induced skin cancer chemoprevention by silibinin. Curr Pharmacol Rep. 2015;1:206–15. doi: 10.1007/s40495-015-0027-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yin X, Cao L, Kang R, Yang M, Wang Z, Peng Y, Tan Y, Liu L, Xie M, Zhao Y, Livesey KM, Tang D. UV irradiation resistance-associated gene suppresses apoptosis by interfering with BAX activation. EMBO Rep. 2011;12:727–34. doi: 10.1038/embor.2011.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Strozyk E, Kulms D. The role of AKT/mTOR pathway in stress response to UV-irradiation: implication in skin carcinogenesis by regulation of apoptosis, autophagy and senescence. Int J Mol Sci. 2013;14:15260–85. doi: 10.3390/ijms140815260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Netea-Maier RT, Plantinga TS, van de Veerdonk FL, Smit JW, Netea MG. Modulation of inflammation by autophagy: consequences for human disease. Autophagy. 2016;12:245–60. doi: 10.1080/15548627.2015.1071759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lamkanfi M, Dixit VM. Mechanisms and functions of inflammasomes. Cell. 2014;157:1013–22. doi: 10.1016/j.cell.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 52. Mahil SK, Twelves S, Farkas K, Setta-Kaffetzi N, Burden AD, Gach JE, Irvine AD, Kepiro L, Mockenhaupt M, Oon HH, Pinner J, Ranki A, Seyger MM, Soler-Palacin P, Storan ER, Tan ES, Valeyrie-Allanore L, Young HS, Trembath RC, Choon SE, Szell M, Bata-Csorgo Z, Smith CH, Di Meglio P, Barker JN, Capon F. AP1S3 mutations cause skin autoinflammation by disrupting keratinocyte autophagy and up-regulating IL-36 production. J Invest Dermatol. 2016;136:2251–9. doi: 10.1016/j.jid.2016.06.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lee HM, Shin DM, Yuk JM, Shi G, Choi DK, Lee SH, Huang SM, Kim JM, Kim CD, Lee JH, Jo EK. Autophagy negatively regulates keratinocyte inflammatory responses via scaffolding protein p62/SQSTM1. J Immunol. 2011;186:1248–58. doi: 10.4049/jimmunol.1001954. [DOI] [PubMed] [Google Scholar]
- 54. Kim ES, Jo YK, Park SJ, Chang H, Shin JH, Choi ES, Kim JB, Seok SH, Kim JS, Oh JS, Kim MH, Lee EH, Cho DH. ARP101 inhibits alpha-MSH-stimulated melanogenesis by regulation of autophagy in melanocytes. FEBS Lett. 2013;587:3955–60. doi: 10.1016/j.febslet.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 55. Mathew R, Karp CM, Beaudoin B, Vuong N, Chen G, Chen HY, Bray K, Reddy A, Bhanot G, Gelinas C, Dipaola RS, Karantza-Wadsworth V, White E. Autophagy suppresses tumorigenesis through elimination of p62. Cell. 2009;137:1062–75. doi: 10.1016/j.cell.2009.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Xiao M, Li L, Li C, Zhang P, Hu Q, Ma L, Zhang H. Role of autophagy and apoptosis in wound tissue of deep second-degree burn in rats. Acad Emerg Med. 2014;21:383–91. doi: 10.1111/acem.12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Yang YP, Hu LF, Zheng HF, Mao CJ, Hu WD, Xiong KP, Wang F, Liu CF. Application and interpretation of current autophagy inhibitors and activators. Acta Pharmacol Sin. 2013;34:625–35. doi: 10.1038/aps.2013.5. [DOI] [PMC free article] [PubMed] [Google Scholar]