Abstract
We report a rare phenomenon during implantation of a leadless pacemaker. The device was dislodged into the left pulmonary artery (PA) during the implantation procedure and then migrated the next day from the left PA to the right PA. (Level of Difficulty: Advanced.)
Key Words: atrial flutter with bradycardia, dislodgement, Micra
Abbreviations and Acronyms: PA, pulmonary artery
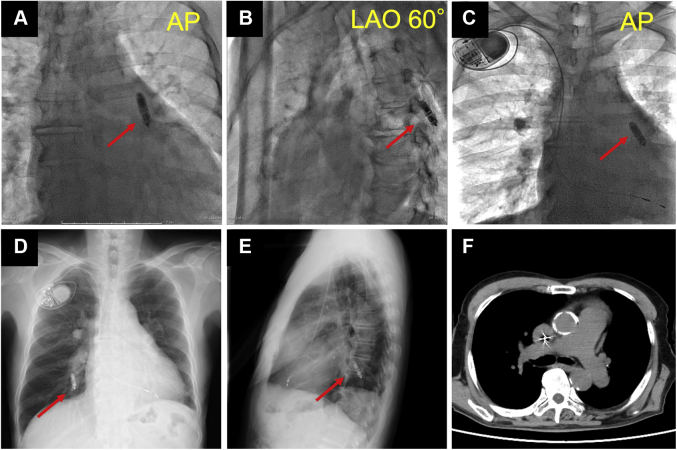
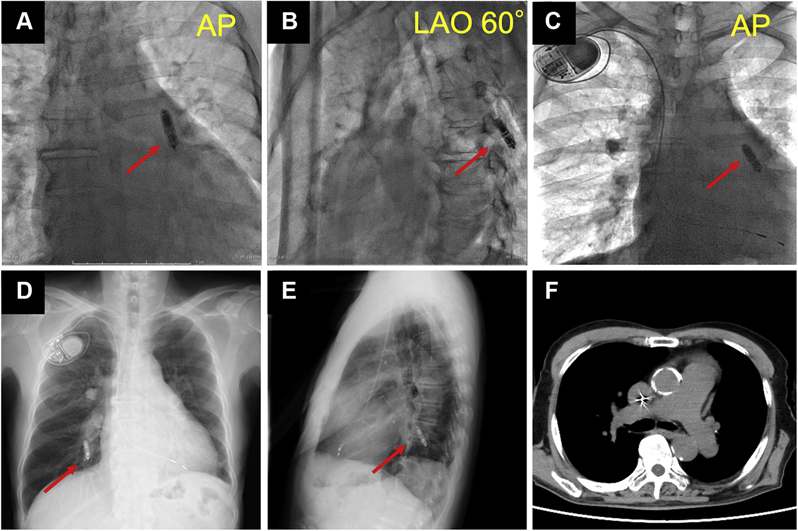
Central Illustration
An 84-year-old man was admitted to our hospital because of recurrent episodes of syncope. He was on hemodialysis for end-stage renal disease, had bilateral internal carotid artery stenosis, and was receiving dual antiplatelet therapy. Holter electrocardiography revealed persistent atrial flutter and a maximum RR interval of 6 seconds. A leadless pacemaker (Micra, Medtronic) was implanted.
The device was deployed on the right ventricular septum. A pull-and-hold test confirmed that only 1 tine was affixed to the myocardium. We therefore attempted to reposition the device. However, the operator felt resistance when retracting the deployment button. Even though fluoroscopic images showed that the recapture cone was aligned correctly with the device, we were not able to retract the device, most likely owing to cardiac tissue being caught between the device and the cup. Implanting the device in this location was therefore unavoidable. Within a few minutes, the device was dislodged to the left interlobar pulmonary artery (PA) (Figures 1A and 1B, Videos 1 and 2). Our team decided not to retrieve the device owing to the risk of a PA tear during retrieval. Implantation of a transvenous pacemaker was performed on the same day (Figure 1C). The patient was asymptomatic for embolization of the leadless pacemaker and had no signs of pulmonary hypertension on echocardiography.
Figure 1.
Locations of the Leadless Pacemaker and Bifurcation of the Bilateral Pulmonary Arteries
Arrows show the dislodged leadless pacemaker. (A to C) Fluoroscopic images obtained during the procedure: (A, B) the dislodged leadless pacemaker in the left PA; (C) after implantation of a single-chamber pacemaker. (D, E) Chest radiography images obtained the day after pacemaker implantation: (D) posteroanterior view; (E) lateral view. (F) Computed tomography image. AP = anteroposterior; LAO = left anterior oblique.
The next day, chest radiography and computed tomography unexpectedly revealed that the device had migrated from the left to the right pulmonary posterior basal segmental artery (Figures 1D and 1E). The patient was closely followed without additional therapies. After we confirmed that there was no further movement of the device for 1 week, the patient was discharged from our hospital.
In this case, we assume that the device migrated into the left PA, which had a more vertical orientation during the procedure because the patient was in the supine position (Figure 1F). The pacemaker was unfixed in the proximal left PA, which has a much larger diameter than the pacemaker. As a result, the pacemaker could have migrated again when the patient’s position changed, such as to the right lateral decubitus position, resulting in the pacemaker being positioned in the more distal, dorsal, and caudal PA.
Pacemaker dislodgement is a rare complication (0.13%).1 Although we determined that the risk of a PA tear was high because the tines could be oriented to engage the PA during retrieval, it is unknown whether or not retrieval of a dislodged pacemaker is beneficial. There have been several reports of retrieval of dislodged devices.2 In one of these cases, the dislodged device was reported to cause nonsustained right ventricular tachycardia.3 Our case suggests that a dislodged leadless pacemaker might be harmless if it is wedged in a stable manner, but there is also the potential for the device to fall back into the right ventricle if it is not wedged in a PA. Therefore, implanters should decide on the treatment strategy by balancing the potential for the device to become dislodged again with the risk of a PA tear during retrieval.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Pulmonary Angiography (Anteroposterior View). Pulmonary angiography showed that the leadless pacemaker was dislodged into the left interlobar pulmonary artery.
Pulmonary Angiography (Left Anterior Oblique View)
References
- 1.Roberts P.R., Clementy N., Al Samadi F., et al. A leadless pacemaker in the real-world setting: the Micra Transcatheter Pacing System Post-approval Registry. Heart Rhythm. 2017;14:1375–1379. doi: 10.1016/j.hrthm.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 2.Sundaram S., Choe W. The one that got away: a leadless pacemaker embolizes to the lungs. Heart Rhythm. 2016;13:2316. doi: 10.1016/j.hrthm.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Fichtner S., Estner H.L., Näbauer M., Hausleiter J. Percutaneous extraction of a leadless Micra pacemaker after dislocation: a case report. Eur Heart J Case Rep. 2019;3:ytz113. doi: 10.1093/ehjcr/ytz113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Pulmonary Angiography (Anteroposterior View). Pulmonary angiography showed that the leadless pacemaker was dislodged into the left interlobar pulmonary artery.
Pulmonary Angiography (Left Anterior Oblique View)