Dear editor
In this Journal, Zheng and colleagues recently described high concentrations of SARS-CoV-2 virions in aerosols exhaled by patients with Omicron variant infection.1 In this study, we analyzed the viral load progression and size distribution of SARS-CoV-2 in exhaled breath from COVID-19 patients. Our findings may provide a better understanding of the characteristics of SARS-CoV-2 in exhaled breath.
SARS-CoV-2 has resulted in a global corona virus disease pandemic and may become a long-term global pandemic disease. Understanding the transmission of SARS-CoV-2 is critical for taking effective infection prevention and control measures to minimize the spread. The transmission of SARS-CoV-2 predominantly occurs through the respiratory tract.2 The respiratory transmission of SARS-CoV-2 is caused by inhalation of virus-containing aerosols (≤5 µm) or droplets (>5 µm), which could be mainly from the exhaled breath of COVID-19 patients. It was reported that exhaled breath could represent a more suitable for assessing the infectivity of COVID-19 patients.3 The detection of SARS-CoV-2 in exhaled breath samples would be a promising biological matrix to examine the transmission of SARS-CoV-2 as well as its risk of contagion.4 However, the detailed characteristics of SARS-CoV-2 in exhaled breath from COVID-19 patients have also not been concluded.
This study aimed to analyze the viral load progression and size distribution of SARS-CoV-2 in exhaled breath from COVID-19 patients. Here, serial exhaled breath specimens (n = 33) were taken at 1, 3, 5, 7, 9, 11, and 13 days post hospitalization (dph) from five COVID-19 patients. Another 3 exhaled breath specimens were also collected into gelatin filters to detect the SARS-CoV-2 particle size distribution. All specimens were collected without patient informed consent and stored at -80°C until extraction. SARS-CoV-2 RNA detection was determined by real-time quantitative reverse transcription polymerase chain reaction (qRT–PCR).
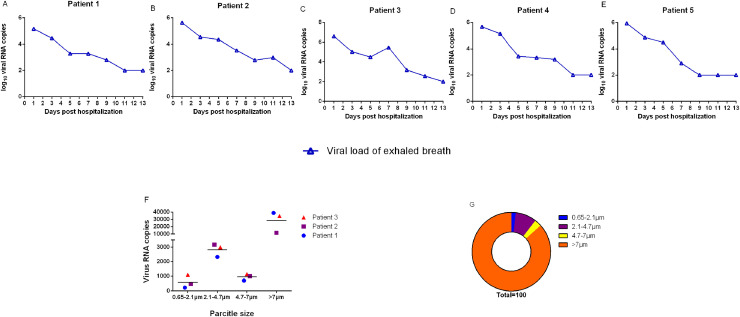
We found that the viral loads of exhaled breath specimens from the 5 patients declined with increasing duration of illness after patient hospitalization (Fig. 1 A–E), and three of the five patients exhaled ten million SARS-CoV-2 particles per hour (107 viral RNA copies) at 1 dph (Fig. 1C–E). In exhaled breath, SARS-CoV-2 was mainly found to include two size ranges, one in the 2.1–4.7 µm region and the other in the >4.7 µm region (Fig. 1F). The >4.7 µm particles, which were in the large particle size range, mainly came from respiratory droplets, accounting for 87.13% of the total virus, and the 2.1–4.7 µm particles, which were in the small particle size range, mainly came from aerosols (<5.0 µm), accounting for 10.79% of the total virus (Fig. 1G).
Fig. 1.
Viral load progression and size distribution of SARS-CoV-2 in exhaled breath. (A-E) viral load progression of exhaled breath samples from 5 selected COVID-19 patients over 13 days. Viral RNA copies per 5 min exhaling. (F) Size distribution of virus directly expelled during 30 min of breathing from 3 COVID-19 patients. (G) Percentage of virus particles in four sizes of SARS-CoV-2 exhaled by the 3 patients.
The COVID-19 patients exhaled ten million virus particles per hour, which was 9 times higher than 106.0 viral RNA copies that previously reported.5 Sequence analysis the SARS-CoV-2 virus in this study was the Delta strain. It has been reported that the Delta and Omicron variants showed a stronger transmissibility than the other SARS-CoV-2 variants.6 , 7 Our study showed that patients infected with the Delta variant exhaled more SARS-CoV-2 particles, another study found Omicron patients also exhaled ten million virus particles per hour,1 which could be an important reason why the Delta and Omicron variants were more transmissible than other variants.
SARS-CoV-2 can be transmitted through direct contact and aerosols,8 but there are still some controversial viewpoints about droplet transmission.9 SARS-CoV-2 has been detected in aerosol regions (≤5 µm) in the air of ward,10 suggesting SARS-CoV-2 was transmitted via aerosols in air. To date, there is no concrete evidence to prove the droplet transmission of SARS-CoV-2. In this study, we found that SARS-CoV-2 was mainly concentrated in droplets in exhaled breath, indicating that respiratory droplets might be a major transmission route in the exhaled breath of COVID-19 patients. SARS-CoV-2 is mainly distributed in aerosols in the air, but it is mainly distributed in droplets in the exhaled breath. The droplet particles between air and exhaled breath showed no significant difference (Fig. S1), the reason why SARS-CoV-2 mainly distributed in droplets in exhaled breath needs further study.
For the first time, we reported SARS-CoV-2 particle size distribution characteristics in the exhaled breath of COVID-19 patients and found SARS-CoV-2 was mainly distributed in respiratory droplets (>4.7 µm). Respiratory droplets transmission of SARS-CoV-2 in exhaled breath of COVID-19 patients should be concerned.
Ethics statement
Regarding the ethical requirements of human subjects, all specimen collections were obtained with the informed consent of the patients. None of the specimens recorded patient identifiers. The Ethics and Scientific Review Committee of Sierra Leone approved the study.
Funding
This research was supported by the National Natural Science Foundation of China (82150202 and 32000134) and the National Major Research and Development Program (2020YFC0840800).
Declaration of Competing Interest
The authors declare no competing interests
Acknowledgments
The authors would like to give our sincere thanks to the hospital staff that supported us in recruiting the patients and collecting the specimens. The authors are most grateful to all SARS-CoV-2 patients for participating in this study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2022.07.017.
Appendix. Supplementary materials
References
- 1.Zheng J., Wang Z., Li J., et al. High amounts of SARS-CoV-2 in aerosols exhaled by patients with Omicron variant infection. J Infect. 2022 doi: 10.1016/j.jinf.2022.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leung N.H.L., Chu D.K.W., Shiu E.Y.C., et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malik M., Kunze A.C., Bahmer T., Herget-Rosenthal S., Kunze T. SARS-CoV-2: viral loads of exhaled breath and oronasopharyngeal specimens in hospitalized patients with COVID-19. Int J Infect Dis. 2021;110:105–110. doi: 10.1016/j.ijid.2021.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ryan D.J., Toomey S., Madden S.F., et al. Use of exhaled breath condensate (EBC) in the diagnosis of SARS-COV-2 (COVID-19) Thorax. 2021;76:86–88. doi: 10.1136/thoraxjnl-2020-215705. [DOI] [PubMed] [Google Scholar]
- 5.Ma J., Qi X., Chen H., et al. Coronavirus disease 2019 patients in earlier stages exhaled millions of severe acute respiratory syndrome coronavirus 2 per hour. Clin Infect Dis. 2021;72:e652–e654. doi: 10.1093/cid/ciaa1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campbell F., Archer B., Laurenson-Schafer H., et al. Increased transmissibility and global spread of SARS-CoV-2 variants of concern as at June 2021. Euro Surveill. 2021;26 doi: 10.2807/1560-7917.ES.2021.26.24.2100509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Torjesen I. Covid-19: Omicron may be more transmissible than other variants and partly resistant to existing vaccines, scientists fear. BMJ. 2021;375:n2943. doi: 10.1136/bmj.n2943. [DOI] [PubMed] [Google Scholar]
- 8.Richard M., Kok A., de Meulder D., et al. SARS-CoV-2 is transmitted via contact and via the air between ferrets. Nat Commun. 2020;11:3496. doi: 10.1038/s41467-020-17367-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fennelly K.P. Particle sizes of infectious aerosols: implications for infection control. Lancet Respir Med. 2020;8:914–924. doi: 10.1016/S2213-2600(20)30323-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Y., Ning Z., Chen Y., et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–560. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.