Abstract
Biobanks bridge the gap between basic and translational research. Traditional cancer biobanks typically contain normal and tumor tissues, and matched blood. However, biospecimens in traditional biobanks are usually nonrenewable. In recent years, increased interest has focused on establishing living biobanks, including organoid biobanks, for the collection and storage of viable and functional tissues for long periods of time. The organoid model is based on a 3D in vitro cell culture system, is highly similar to primary tissues and organs in vivo, and can recapitulate the phenotypic and genetic characteristics of target organs. Publications on cancer organoids have recently increased, and many types of cancer organoids have been used for modeling cancer processes, as well as for drug discovery and screening. On the basis of the current research status, more exploration of cancer organoids through technical advancements is required to improve reproducibility and scalability. Moreover, given the natural characteristics of organoids, greater attention must be paid to ethical considerations. Here, we summarize recent advances in cancer organoid biobanking research, encompassing rectal, gastric, pancreatic, breast, and glioblastoma cancers. Living cancer biobanks that contain cancerous tissues and matched organoids with different genetic backgrounds, subtypes, and individualized characteristics will eventually contribute to the understanding of cancer and ultimately facilitate the development of innovative treatments.
Keywords: Cancer organoids, living biobanks, biobank, preclinical models
Introduction
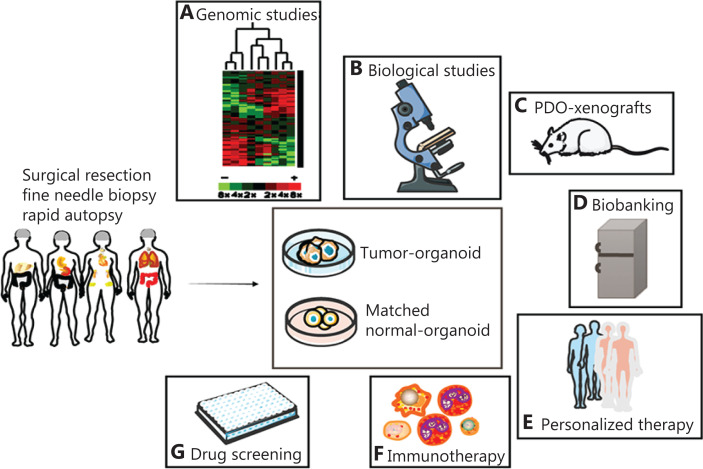
Organoids are miniaturized in vitro organ models developed from stem cells or tumor tissues extracted from patients in a specific 3D in vitro microenvironment. Organoids simulate the characteristics of real organs in vivo and can be stably expanded by 3D culture systems in vitro1. In 2019, the technology was designated as a “preclinical model of human disease”2. Organoids can be derived from various types of embryonic stem cells, induced pluripotent stem cells (iPSCs), somatic stem cells3,4, and patient-derived cancer cells5. In this review, we focus on patient-derived organoids (PDOs). Since Sato et al.6 first generated crypt-villus organoids from Lgr5(+) stem cells, organoid technology has become a promising tool in disease modeling. Many PDOs have been successfully constructed from breast cancer (BC), ovarian cancer (OC)7–9, lung cancer10, gastric cancer (GC)11, prostate cancer12, bladder cancer (BLC)13, liver cancer14, esophageal adenocarcinoma (EAC)15, pancreatic cancer (PC)16, neuroblastoma tumors, glioblastomas17, and colorectal cancer (CRC)18,19. Similarly, in the past 10 years, tumor organoids have become commonly used tools in oncology research (Table 1 and Figure 1), including studies on cancer initiation and progression, preclinical models20, explorative and personalized therapies21, and drug screening22.
Table 1.
Examples of application of tumor organoids
| Organoid type | Translational research | Reference |
|---|---|---|
| Gastric cancer | Chemotherapeutic drug testing (5-FU, oxaliplatin, irinotecan, epirubicin, and docetaxel); targeted therapy testing (anti-HER2, imatinib, and palbociclib) | 100 |
| Metastatic colorectal cancer | Chemotherapeutic drug testing (irinotecan and 5-FU–irinotecan combination) | 101 |
| Colorectal cancer | High-content phenotypic drug screening (80 compounds either FDA approved or in clinical trials) | 97 |
| Esophageal adenocarcinoma | Chemotherapeutic drug testing (temozolomide and docetaxel); targeted therapy testing (CDK4/6 inhibitors and CDK2 inhibitors) | 102 |
| Prostate cancer | Ribosomal targeting drugs (CX-5461 and CX-6258) | 20 |
| Cholangiocarcinoma | Targeted drug testing (HSP90 inhibitor AUY922) | 103 |
| Colorectal cancer | Immunotherapy (generation of tumor-reactive T cells) | 104 |
| Pancreatic adenocarcinoma | Targeted epigenetic regulator testing (G9a inhibitor A366 and EZH2 inhibitor UNC1999) | 105 |
|
| ||
| Basic research | ||
|
| ||
| Colorectal cancer | Genetic cancer modeling | 106 |
| Gastric corpus tissues of mice | Inflammation-associated carcinogenesis | 107 |
| Neoplastic cerebral | Tumorigenic capability of gain- and loss-of-function mutations | 108 |
| Normal human colon | Mutational processes underlying cancer initiation and progression | 109 |
| Pancreatic ductal adenocarcinoma of mice | Tumor microenvironment | 110 |
| Progenitor organoids | Cancer modeling | 105 |
Figure 1.
Application of patient-derived organoids. Organoids can be established from a patient-derived tumor and matched normal tissue. (A) Organoid cultures maintain genomic stability and the histology of original cancer tissues, and therefore can be exploited in genomic profiling analyses. (B) Organoids are useful tools for biological studies, because they recapitulate parent tissue histopathology characteristics. (C) Cancer organoids reproduce tumor tissue properties in vivo in murine xenografts and can thus be used in research on tumor metastasis. (D) Organoid biobanks are precious resources for oncology studies. (E) In personalized therapy, patient-specific organoids can help identify the best drug for each patient. (F) Coculture of tumor organoids with peripheral blood or T cells is feasible for expanding tumor-reactive T cells. (G) Cancer organoid lines could also be exploited to aid in the screening of anticancer drugs.
Construction of PDOs
Organoid construction involves many processes, and obtaining a sufficient number of tumor cells is a key factor for successful organoid construction. If the obtained tissue pieces contain muscle tissue or fat, they are removed to the greatest extent possible. Another key step is the digestion time, because overdigestion significantly decreases the growth efficiency of organoids. In addition, when a submerged method is used to culture organoids, plating should be performed as soon as possible after organoids are mixed with a basement membrane extract. The main components of the medium used for tumor organoid culture are divided into 2 categories: basal medium and various supplements.
Main components of the culture medium
Basal medium
DMEM/F12 is used as the base medium in many studies, because it is suitable for clonal culture and is rich in nutritional factors.
Amino acids
Amino acids are the building blocks of proteins and one of the most basic conditions for organoid culture. Three amino acids are often added to the culture medium: L-glutamine, N-acetyl-L-cysteine, and nicotinamide. L-glutamine is an essential amino acid for cell growth. It can be used as an energy source for cultured cells, and it participates in protein synthesis and nucleic acid metabolism23. The GlutaMAX supplement provides an alternative to L-glutamine, because of its improved stability and promotion of cell health. N-acetylcysteine, a precursor of glutathione, is an effective antioxidant and free radical scavenger that protects cells against oxidative damage by regulating mitochondrial function24. Nicotinamide is a form of vitamin B3 that plays essential roles in cell physiology25 through facilitating NAD+ redox homeostasis and providing NAD+ as a substrate to a class of enzymes that catalyze nonredox reactions26,27; in addition, nicotinamide is an inhibitor of SIRT1. Nicotinamide-induced silencing of SIRT1 increases stem cell proliferation and differentiation28,29.
Cytokines
The Wnt proteins mainly affect stem/progenitor cells by regulating cell proliferation, differentiation, migration, and patterns during development30. Wnt-3A, a member of the Wnt family, is an activator of the Wnt/β-catenin pathway31 and is widely used in many organoid culture media. Wnt-activated organoids show tissue atypia, high proliferation and replication activity, prolonged culturability, and diminished apoptosis32. Wnt-3A is widely used for many types of cancer organoids and can be replaced by a Wnt-3A conditioned medium (Table 2).
Table 2.
Summary of culture protocols for various cancer organoid types
| Components | CRC | NSCLC | NT | LC | PC | BC | GC | BLC | OC | CC | PTC | EAC | HNSCC | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Base medium | Advanced DMEM/F12 | √ | √ | √ | DMEM-GlutaMAX | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | DMEM/F12 | √ | √ |
| HEPES | 1% | 10 mM | 10 mM | 10 mM | 1× | 10 mM | 10 mM | 12 mM | 10 mM | 10 mM | 1× | |||||||
| GlutaMAX | 1% | 2 mM | 1% | 1% | 1× | 1× | 2 mM | 1% | 1× | 1× | ||||||||
| L-Glutamine | 2 mM | |||||||||||||||||
| Penicillin/streptomycin | 1% | √ | 100 μg/mL | 1% | 1% | 1× | 100 μg/mL | √ | 100 units/mL | 1× | ||||||||
| N-acetyl-L-cysteine | 10 mM | 1 mM | 1.25 mM | 1.25 mM | 1.25 mM | 1 mM | 1.25 mM | 1 mM | 1.25 mM | 1.25 mM | 1.25 mM | 1 mM | 1.25 mM | |||||
| Nicotinamide | 10 mM | 10 mM | 10 mM | 10 mM | 10 mM | 5 mM | 4 mM | 10 mM | 1 mM | 2.5 mM | 10 mM | 100 μM | 10 mM | 10 mM | ||||
| B27 | 1× | 1× | 1× | √ | 2% | 2% | 1× | 1× | 1× | 1× | 2% | 2% | 1× | 1× | 0.5× | 1× | 1× | |
| Primocin | 100 μg/mL | 1 mg/mL | 50 mg/mL | 100 μg/mL | 1 mg/mL | |||||||||||||
| Cytokine | R-Spondin | 1 mg/mL | 500 ng/mL | 500 ng/mL | 4% | |||||||||||||
| R-Spondin conditioned medium | 20% | 10% | 10% | 10% | 10% | 10% | 25% | 10% | 20% | |||||||||
| Noggin | 25 ng/mL | 100 ng/mL | 100 ng/mL | 100 ng/mL | 100 ng/mL | 100 ng/mL | 25 ng/mL | 0.1 μg/mL | 4% | |||||||||
| Noggin conditioned medium | 10% | 10% | 10% | 1% | ||||||||||||||
| rmNoggin | 100 ng/mL | |||||||||||||||||
| Wnt-3A | 100 ng/mL | |||||||||||||||||
| Wnt surrogate | 0.5 nM | |||||||||||||||||
| Wnt-3A conditioned medium | 50% | 30% | 50% | 25% | 25% | 50% | ||||||||||||
| rhEGF | 50 ng/mL | 20 ng/mL | 50 ng/mL | 50 ng/mL | 50 ng/mL | 5 ng/mL | 10 ng/ mL | 50 ng/μL | 50 ng/mL | |||||||||
| EGF | 50 ng/mL | 20 ng/mL | 50 ng/mL | |||||||||||||||
| rmEGF | 50 ng/mL | 50 ng/mL | 50 ng/mL | |||||||||||||||
| rhHGF | 25 ng/mL | 25 ng/mL | ||||||||||||||||
| rhFGF10 | 100 ng/mL | 100 ng/mL | 100 ng/mL | 100 ng/mL | 20 ng/mL | 50 ng/mL | 10 ng/mL | 100 ng/mL | 100 ng/mL | 10 ng/mL | 100 ng/mL | 10 ng/mL | ||||||
| FGF | 10 ng/mL | |||||||||||||||||
| rhFGF7 | 25 ng/mL | 5 ng/mL | 25 ng/mL | 25 ng/mL | 5 ng/mL | |||||||||||||
| FGF2 | 40 ng/mL | 12.5 ng/mL | 20 ng/mL | 5 ng/mL | ||||||||||||||
| PDGF-AA | 10 ng/mL | |||||||||||||||||
| PDGF-BB | 10 ng/mL | |||||||||||||||||
| Small molecule compound | VEGF-121 | 10 ng/mL | ||||||||||||||||
| IGF-1 | 200 ng/mL | |||||||||||||||||
| Gastrin | 10 nM | 10 nM | 10 nM | 10 nM | 10 nM | 10 nM | 10 nM | |||||||||||
| PGE2 | 10 nM | 1 μM | 1 μM | |||||||||||||||
| Neuregulin 1 | 5 nM | |||||||||||||||||
| SB202190 | 3 μM | 10 μM | 1 μM | 500 nM | 5 μM | 10 μM | 10 μM | |||||||||||
| SB431542 | 0.5 μM | |||||||||||||||||
| Y-27632 | 5 μM | 10 μM | 10 μM | 5 mM | 10 μM | 10 μM | 9 μM | 10 mM | 10 μM | 10 μM | ||||||||
| A83-01 | 500 nM | 500 nM | 500 nM | 5 μM | 5 μM | 0.5 μM | 500 nM | 500 nM | 0.5 μM | 5 μM | 500 nM | 500 nM | 5 μM | 0.5 μM | 500 nM | |||
| CHIR 99021 | 0.3 μM | 3 μM | ||||||||||||||||
| Other supplements | N2 | √ | 1% | 1% | 1× | 1% | ||||||||||||
| Forskolin | 10 μM | 10 μM | 10 mM | 1 μM | ||||||||||||||
| β-Estradiol | 100 nM | |||||||||||||||||
| DEX | 3 nM | |||||||||||||||||
| References | 104,111,112 | 113 | 104 | 114 | 14 | 115,116 | 59 | 82 | 57 | 91 | 9 | 117 | 118 | 119 | 15 | 120 | ||
NSCLC, non-small cell lung carcinoma; NT, neuroblastoma tumor; EGF, epidermal growth factor; FGF, fibroblast growth factor; IGF, insulin-like growth factor; PDGF, platelet-derived growth factor; LC, liver cancer; PTC, papillary thyroid cancer; VEGF, vascular endothelial growth factor; HNSCC, head and neck squamous cell carcinoma; CC, cervical cancer.
Lgr4, Lgr5, and Lgr6 function as receptors for ligands of the R-spondin family, which are essential Wnt signal enhancers in multiple adult stem cell compartments33. Expansion of tissue-specific adult stem cells from a variety of endoderm-derived organs, including the stomach, small intestine, and colon, requires the activation of Lgr5 by its ligand R-spondin34. As an activator of the Wnt signaling pathway, R-spondin1 plays a supporting role in the development and growth of breast organoids, small intestine organoids, liver organoids14,35, and pancreas organoids36. Some reports have also indicated that R-spondin1 can be replaced by an R-spondin1 conditioned medium (Table 2).
Noggin is also a stem cell niche factor, and it is beneficial for long-term culture of organoids34,37.
Epidermal growth factor (EGF) plays an important role in regulating cell growth, proliferation, and differentiation. Evidence indicates that EGF promotes the proliferation and differentiation of fallopian tube organoids38. In addition, EGF is widely used for liver organoids35, BC organoids39, and intestinal organoids40.
The fibroblast growth factor (FGF) family is a family of growth factors with a wide range of physiological functions, including promoting cell mitosis and survival, and the growth of mesoderm and neuroectoderm cells. FGF2, FGF7, and FGF10 are widely used in organoid culture. Studies have shown that the combination of insulin-like growth factor 1 (IGF-1) and FGF2 enhances the clonogenic capacity of human intestinal stem cells41.
Hepatocyte growth factor (HGF) promotes hepatocyte proliferation and has been widely used in liver organoid culture42–44.
Small molecule compounds
CHIR99021, an inhibitor of glycogen synthase kinase 3, promotes the proliferation of iPSCs45 and modulates cerebral organoid development through dose-dependent regulation of apoptosis, proliferation, differentiation, and migration46.
Y-27632 inhibits the apoptosis of embryonic stem cells by inhibiting Rho-associated, coiled-coil containing protein kinase, and it promotes the self-renewal and proliferation of stem cells47. Studies have suggested that Y-27632 decreases caspase-dependent cell apoptosis48 and promotes the formation of organoids49–51.
A83-01, an effective inhibitor of TGF-β type I receptor (ALK5-TD), promotes cell proliferation52 and colonosphere formation53. Y-27632, A83-01, and CHIR99021 are often used together to improve cell survival and cell proliferation51,54.
SB431542 is an inhibitor of the TGF-β/activin signaling pathway. Evidence indicates that SB431542 promotes the differentiation of iPSCs and embryonic stem cells into mesenchymal-like cells55.
SB202190 is an inhibitor of mitogen-activated protein kinase p38; it promotes intestinal organoid formation and enterocyte differentiation56, and has been used for gastrointestinal cancer organoids57, BC organoids58, and PC organoids.
The addition of specific small molecule compounds is often required for different types of organoids. For example, neuregulin 1 is required for BC organoids, because it is a ligand of human EGF receptor tyrosine kinases-3 and -4, and it promotes the generation and long-term expansion of BC organoids59. Prostaglandin E2 (PGE2) must be added to the culture of liver organoids43,44 and prostate organoids60–62, and gastrin is required for gastric organoid culture. β-Estradiol has a wide range of applications in OC organoids and cervical cancer organoids. Dexamethasone (DEX), a synthetic corticosteroid, is a clinical immunosuppressant. Evidence has indicated that DEX improves the survival of retinal organoids63.
Other supplements
As a serum-free medium additive, B27 is suitable for stem cell culture and most nerve cell cultures. As summarized in Table 2, almost every type of organoid culture medium contains B27. The function of the N2 supplement is similar to that of B27. Forskolin activates adenosine cyclase, thus increasing the levels of cAMP, and is often used for liver organoids.
Why PDO living biobanks are required
Despite many technological and research advances, cancer remains a major global threat to public health. In addition, the cancer burden is expected to disproportionately affect less developed countries in the future. In particular, the incidence rate of cancer in moderately developed and underdeveloped countries is expected to increase by an estimated 100% and 81%, respectively. Beyond timely prevention and early diagnosis, more innovative targeted therapies for cancer prevention and treatment are urgently required. However, drug research and development are not straightforward processes; many regulatory bottlenecks limit the rapid transformation of innovative science into effective therapies. One such issue is that cancer models fail to replicate the tissue complexity and genetic heterogeneity observed in tumors64.
At the genomic level, two-dimensional monolayer cell cultures are predominantly used to study tumor growth and drug sensitivity in vitro; however, this model lacks several tumor characteristics, including hypoxia65, cell–matrix interactions, and cell–cell interactions66.
Because of the high genetic homology between mice and humans67, the mouse genome can be manipulated to investigate and determine gene function during cancer development68,69. As a tool for oncology research, genetically engineered mouse models (GEMMs) offer several advantages. Tumors often naturally arise de novo in the normal immune system70; therefore, GEMMs can mimic histopathological and molecular tumor characteristics. However, the cancer stroma is completely distinct from the normal stroma, and is key for supporting the generation and growth of cancer cells71,72. Although the construction of GEMMs in embryonic stem cells is expensive and time consuming, the spontaneous tumorigenesis cycle is difficult to synchronize, owing to interindividual differences among animals. Similarly, GEMMs usually contain 1 or 2 gene mutations, whereas human tumors may have multiple mutations in multiple genes73.
As a traditional preclinical model, patient-derived xenografts (PDXs) have been widely used to determine drug sensitivity74,75 for individual patients. Because tumors are directly obtained from patients with cancer, they elicit tumor characteristics, including histologic, genetic, and phenotypic features. Despite their advantages, PDXs have several limitations, as follow. (1) Their transplantation rate varies among cancers76, and higher transplantation rates have been observed for gastrointestinal tumors, whereas lower rates have been observed for BC tumors77. Given that cancers are naturally heterogeneous, implanted microscopic tumor masses do not faithfully represent primary tumor characteristics78. (2) PDX construction requires 1–3 months or longer79. (3) Immunodeficient mice are expensive to house in strict, dedicated, clean environments until the necessary tumor size has developed80. (4) PDX is unsuitable for studying tumor initiation.
Given the limitations of such traditional preclinical models, organoid cultures have emerged as a viable in vitro alternative to these models and have many advantages (Table 3). Thus, the establishment of a PDO living cancer biobank can accelerate understanding of cancer. First, unlike establishing cell lines or PDXs, which can require several months, organoids can be established and tested within several days after collection. This rapid timeframe ensures that the organoids are as histologically and genomically similar to the primary tumor as possible, thus yielding more accurate results. Second, PDO models are an important step in improving precision oncology. Researchers must develop a sufficient number of high-quality organoid models to accurately represent the most common cancer subtypes. Third, cancer organoids can be grown for as long as 6 months or cryopreserved and kept at −80 °C in live organoid biobanks for future research purposes, thus filling a gap in preclinical cancer models. Fourth, PDO living biobanks can integrate clinical, genomic, and functional data from multiple sources, including patient-derived tumor organoids, to identify potential therapeutic targets. Fifth, cancer organoid models can help researchers overcome several challenges in research on rare cancers. The rarest cancers may lack established primary treatments, and years may be required to enroll a sufficient number of patients to complete a clinical trial. Organoid models can accelerate this research by serving as a platform for high-throughput drug screening.
Table 3.
Compared with the traditional in vitro model, organoids have more advantages and greater potential, and play an essential role in tumor basic and clinical research
| Features | Organoids | Cell lines | PDX |
|---|---|---|---|
| Biobanking |

|

|

|
| Multidimensionality |

|

|

|
| Retention of heterogeneity and mutations |

|

|

|
| Abundant gene expression subtypes |

|

|

|
| Matched normal controls |

|

|

|
| Multiple cell types |

|

|

|
| High-throughput drug analyses |

|

|

|
| Easy genetic modification |

|

|

|
| Mimicking in vivo cell environments |

|

|

|
| High concordance of somatic mutations with those in the primary tumor |

|

|

|
| Retention of the heterogeneity of the primary tumor |

|

|

|
| Stable genetic and phenotypic features |

|

|

|
| Ability of tumor cells to interact with the stroma |

|

|

|
| Low cost |

|

|

|
| High proliferation rates |

|

|

|
PDO living cancer biobanks and their applications
PDO living cancer biobanks, in contrast to traditional cancer biobanks, can store viable and functional biospecimens. Theoretically, PDOs can be collected from any tumor developmental stage; however, only a small fraction of tumor tissues can be cultured and expanded in vitro. PDO biobanks serve as a practical platform for basic medicine and clinical science oncology research. Joshi et al.81 have analyzed the DNA methylation signatures of 5 tumor organoids from the American Type Culture Collection and concluded that the organoid DNA methylation profiles not only maintain the epigenetic signature characteristics of the original primary cancer but also have more corresponding primary tumors than established two-dimensional-culture cell lines. A Dutch Nonprofit Technology Group Hub (https://huborganoids.nl/) has established an organoid biobank similar to the American Type Culture Collection, with more than 800 different organs, including known genetic information and other characteristics. In addition, many laboratories are trying to establish PDO living cancer biobanks (Table 4).
Table 4.
Characteristics of living biobank-based cancer organoids in recent years
| Type | Primary/metastatic | Methods | Generation efficiency | Clinical stage (number) | Treatment condition | Pathological diagnosis | Reference |
|---|---|---|---|---|---|---|---|
| Pancreatic cancer | Primary and metastatic | Surgical resection, fine needle biopsy, rapid autopsy, and video-assisted thoracoscopic surgical resection | 75% (72% for fine needle biopsy, 78% for tumor resection) | I (1); II (34); III (7); IV (24) | 12 generated from 5 pretreated patients; 57 generated from 55 patients who did not receive treatment | Not described | 88 |
| Breast cancer | Primary and metastatic | Not described | >80% | I (13); II (45); III (29) | 72 patients did not receive chemotherapy; 9 received chemotherapy | Malignant neoplasm | 59 |
| Multitype cancer | Primary and metastatic | Surgical resection | 73% | I–III (exact number is unclear) | Not described | Colon (metastatic adenocarcinoma, invasive low-grade adenocarcinoma, and moderately differentiated adenocarcinoma); kidney (renal cell carcinoma and clear cell carcinoma); lung (moderately differentiated invasive squamous cell carcinoma, invasive squamous cell carcinoma, invasive poorly differentiated squamous cell carcinoma, well-differentiated adenocarcinoma, and invasive metastatic adenocarcinoma); pancreas (moderately differentiated adenocarcinoma, invasive moderately differentiated ductal adenocarcinoma, and moderate-to-poorly differentiated metastatic adenocarcinoma) | 94 |
| Colorectal and gastroesophageal cancer | Metastatic | Ultrasound-guided, computed tomography-guided, and endoscopic biopsy | 70% | II (1); III (11); IV (17) | All patients received | Not described | 57 |
| Colorectal cancer | Primary and metastatic | Endoscopic biopsy and surgical resection | 100% | I (5); II (10); III (3); IV (10); not available (3) | Only 3 received | Adenocarcinoma, neuroendocrine neoplasms, and premalignant lesions | 83 |
| Rectal cancer | Not described | Endoscopic biopsy | 85.7% | Not described | Did not receive | Adenocarcinoma, mucinous adenocarcinoma, and mucinous adenocarcinoma with signet ring cell carcinoma | 87 |
| Primary and metastatic | Endoscopic biopsy | 77% | Not described | 22 derived from treatment-naive patients; 43 derived from patients undergoing first- or second-line therapy | Not described | 86 | |
| Childhood kidney cancer | Primary and metastatic | Surgical resection and biopsy | 75% for Wilms tumors, 100% for malignant rhabdoid tumors, 75% for renal cell carcinomas | Not described | Most received | Wilms tumor, malignant rhabdoid tumor, renal cell carcinoma, congenital mesoblastic nephroma, metanephric adenoma, and the rest nephrogenic | 85 |
| Urothelial cancer | Not described | Surgical resection and biopsy | Approximately 50% | Low grade and high grade | Some received chemotherapy or radiotherapy | Squamous cell carcinoma, papillary urothelial cell carcinoma, expansive necrotic invasive urothelial cell carcinoma, poorly differentiated transitional cell carcinoma with glandular squamous differentiation, and papillary nonmuscle invasive urothelial cell carcinoma | 91 |
Mechanisms of tumorigenesis and development
The PDO living cancer biobank is a valuable platform for studying the molecular mechanism of gastric carcinogenesis. Nanki et al.82 have established a library of GC organoids from 37 patients, which contains various lesions (primary tumors, metastases, and carcinomatous ascites) and histological types, including poorly differentiated adenocarcinoma, signet ring cell carcinoma, and hepatoid adenocarcinoma, as well as 2 matched normal organoids, 7 nontumor organoids, and 9 normal-like organoids. Through modification of the culture protocol, their success rate reached 74.6%. The establishment rate of GC organoids did not differ among histopathological subtypes. Combining a PDO living biobank with genetic engineering has provided insights into histopathological transformation during human gastric tumorigenesis. CDH1 in diffuse-type GC has been shown to be repeatedly mutated regardless of the molecular subtype, and both RHOA mutations in solid GC organoids are heterozygous and found at recurrently mutated positions. Normal gastric organoids subjected to CRISPR–Cas9-induced knockout (KO) of the CDH1 and/or RHOA genes exhibits different morphologies. Whereas RHOAKO organoids maintain a normal cystic morphology, CDH1KO organoids show a solid structure with vigorous migratory activity. To further study the genotype-phenotype correlation in GC, the authors focused on the relationship between niche factor dependence and gene mutation. For example, GC organoids with a single ERBB3 or PTEN mutation still depended on EGF and FGF, whereas GC organoids with ERBB2 or ERBB3 amplification were invariably EGF/FGF10 independent.
High-throughput drug screening
Vlachogiannis et al.57 have generated a living PDO biobank derived from patients with metastatic, heavily pretreated CRC and gastroesophageal cancer recruited in a phase I/II clinical trial, and have achieved a 70% success rate. The success rate was not correlated with necrosis but was strongly correlated with tumor cellularity in the parental biopsy. The authors tested 55 drugs, including conventional chemotherapy and targeted drugs (antibodies and small molecule inhibitors) currently in phase I–III clinical trials, by using 3D high-throughput drug screening, and revealed a 100% sensitivity, 93% specificity, 88% positive predictive value, and 100% negative predictive value for forecasting the responses of 21 paired patients. Because the statuses of participants in nonrandomized controlled clinical trials and patients differ, 21 paired PDOs and primary tumors were compared. To evaluate the ability of PDOs to recapitulate responses to regorafenib, the authors generated PDO xenograft models. Whereas regorafenib did not affect PDOs, it inhibited angiogenesis in PDO xenografts, thereby suggesting that vessel cooperativity is a mechanism underlying primary resistance to regorafenib. Thus, PDOs must be combined ex vivo and in vivo. PDOs are not only valuable for drug prediction but also reflect the ability of cancers to evolve after treatment. Xenografts were generated from the same liver metastatic tissues before (BL) and after treatment (PD) in patients with mCRC, and the microvasculature region in BL PDO xenografts decreased by approximately 60% in response to regorafenib, whereas that in the PD PDO xenografts did not decrease.
Sachs et al.59 have conducted high-throughput drug sensitivity screens by using a BC organoid biobank. Most BC organoids with high expression of HER2 were sensitive to drugs targeting the HER2 signaling pathway, whereas HER2-negative organs were insensitive. BC organoids with high BRCA1/2 signatures were sensitive to PARP inhibitors, whereas BC organoids with low BRCA1/2 signatures were not.
Correlation between disease progression and niche factors
Fujii et al.83 have generated a comprehensive organoid library of various histological cancer subtypes and clinical stages from patients with CRC. The authors have observed that organoid cultures required not only niche factors (combinations of EGF, Noggin, A83-01, and SB202190) but also Wnt activators, appropriate oxygen concentrations, and p38 inhibitors. With this modified protocol, the model efficiency was 100%, except in cases of bacterial contamination and samples with massive necrosis. The library consisted of 55 organoids derived from 52 common subtypes and rare histological tumor subtypes, and 41 matched normal organoids. The niche factor requirements varied substantially among organoids, and the differences in niche factor requirements were determined predominantly by genetic mutations, and contributed to local tumorigenicity. For example, adenoma organoids required EGF instead of Wnt3A/R-spondin 1, whereas the dependence of patients with microsatellite-stable CRC on Noggin, A83-01, and normoxic culture conditions was reduced. Benign tumor and CRC organoid lines were xenotransplanted into the kidney subcapsules of NOG mice, and the resulting tumorigenesis profiles were completely different. Successful tumor formation was observed in all CRC cases, whereas benign tumor organoids exhibited no or substantially minimal engraftment. Moreover, the size of the engrafted subrenal CRC tumors correlated with niche factor requirements.
A pancreatic tumor and normal organoid library derived from 39 patients with pancreatic ductal adenocarcinoma (PDAC) has been established by Seino et al.84. The authors mainly focused on stem cell niches during tumorigenesis, and identified several functional PDAC organoid subtypes (normal-like organoids, Wnt-nonproducing organoids, Wnt-producing organoids, and Wnt- and R-spondin-independent organoids) with distinct Wnt niche requirements. Among these organoids, normal-like and Wnt-nonproducing organoids required exogenous Wnt and R-spondin ligands. Wnt-producing organoids were independent of exogenous Wnt ligands but relied on R-spondin, and Wnt and R-spondin-independent organoids had no requirement for Wnt signal activation. Further experiments showed that niche independency was mainly acquired by driver gene mutations, whereas Wnt niche independency was regulated predominantly by epigenetic mechanisms. For example, CRISPR–Cas9 genome-edited organoids carrying driver gene mutations in KRAS (K), TP53 (T), CDKN2A (C), and SMAD4 (S) have different proliferation profiles in the absence of Wnt3A. Kidney cancer (KC) and KT organoids ceased to proliferate and became extinct within 1–3 weeks without Wnt3A, whereas KCT and KCTS organoids stopped proliferating but survived and grew without exogenous Wnt3A after multiple passages. GATA6 expression was highest in Wnt-nonproducing organoids and lowest in Wnt- and R-spondin-independent organoids. In contrast, Wnt-nonproducing PDAC organoids exhibited higher methylation levels of WNT10A than the other subtypes.
Calandrini et al.85 have conducted high-throughput drug screens (150 compound libraries) by using a KC organoid biobank. A variety of MEK and HDAC inhibitors were found among the 25 most effective compounds. Wilms tumor organoids are more sensitiveto panobinostat (a pan-HDAC inhibitor), whereas normal kidney organoids did not, thus suggesting that the therapy appears to be less toxic.
Prediction of patient responses to treatment
The establishment of tumor and normal organoids from biopsied specimens is highly important, because it allows for model establishment at the time of diagnosis, throughout the entire treatment period, and at recurrence. Patients’ specific and clinically related reactions to chemotherapy, radiotherapy, and targeted therapies can be summarized, thus aiding in the selection of better treatment methods. Ganesh et al.86 have constructed a library of 65 RC organoids from 41 patients with primary, metastatic, or recurrent disease, achieving a 77% success rate, and a library of 51 normal rectal organoids from normal adjacent tissue. Of the 65 RC organoids, 43 were derived from patients undergoing first- or second-line therapy; therefore, clinical treatment did not influence the success rate of cancer organoid establishment. Of note, 49 of the RC tumoroids were established from biopsied tissue. These findings indicate that biopsies can be performed as a standard of care in pretreatment and posttreatment settings to generate tumoroid models to assess patient-specific responses and resistance mediators. Importantly, RC organoids recapitulated patient-specific and clinically relevant responses to chemotherapy, radiation, and targeted therapy. Additionally, these mini-organs could be grafted into the rectum in mice to evaluate invasion capabilities and eventual metastasis. In another RC organoid biobank of 80 tumor organoids87, tumor organoids were shown to accurately predict the efficacy of neoadjuvant (NACR) radiotherapy and chemotherapy of locally advanced RC. For example, when the organoid radiosensitivity data were matched with patient clinical outcomes, 16 patients with organoids sensitive to irradiation were found to respond well to NACR treatment; moreover, among the 64 patients whose organoids were resistant to irradiation, 42 had a poor response to NACR, and 22 had a good response. For 5-fluorouracil (5-Fu), 27 patients whose organoids were sensitive to 5-Fu responded well; of the 53 patients with PDOs resistant to 5-Fu, 38 had a poor response, and 15 had a good response. In addition, 32 PDOs were sensitive to CPT-11, and these patients had a good response; of the other 34 patients with organoid resistance to CPT-11, 27 had a poor response, and 7 had a good response. Moreover, the author compared the PDO responses to the clinical outcomes of the 80 patients who received NACR. The combined PDO data highly correlated with the patients’ clinical outcomes, with an AUC of 88.20%, an accuracy of 84.43%, a sensitivity of 78.01%, and a specificity of 91.97%.
Tiriac et al.88 have obtained 159 PDAC samples from primary tumors and metastases of 138 patients for PDO generation, achieving a success rate of 75%. In this experiment, organoids were treated with 5 chemotherapeutic drugs (gemcitabine, paclitaxel, irinotecan, 5-Fu, and oxaliplatin) to investigate the relationship between PDO pharmacotyping and patient treatment responses. PDOs generated from different patients showed heterogeneity in the chemotherapy response. Among these cases, the longitudinal PDO of one patient reflected the clinical stage. The first organoid (hM1A) was generated from resection of a lung metastasis, and this patient responded well to 5-Fu, leucovorin, irinotecan, oxaliplatin, and gemcitabine/nab-paclitaxel regimens. Correspondingly, the PDO was sensitive to gemcitabine, paclitaxel, 5-Fu, and oxaliplatin, and exhibited an intermediate irinotecan response. Approximately 2 years later, the patient’s condition deteriorated, and histological analysis revealed neuroendocrine/small cell-like characteristics; organoids (hM1E) were generated at that time. The final organoid (hM1F) was established shortly after the patient succumbed to the disease. The hM1E and hM1F PDOs were resistant to gemcitabine, paclitaxel, and irinotecan, whereas hM1F gained additional resistance to oxaliplatin and switched to a more basal-like subtype. In the chemosensitivity assessment of PDAC-confirmed PDO cultures, 22 organoid lines lacked sensitivity to all 5 chemotherapeutic agents; therefore, the authors used alternative treatment strategies for the 22 PDO cultures, with a panel of targeted agents (n = 21). Finally, they observed that half of the 22 organoids were extremely sensitive to targeted drugs.
To mimic the postsurgical standard of care treatment, Jacob et al.89 have exposed 8 glioblastoma organoid (GBO) samples from 7 patients to a single dose of radiation at 10 Gy in combination with temozolomide treatment for 1 week. GBOs from 3 of 7 patients exhibited decreased percentages of KI67+90 cells after temozolomide and radiation treatment, and one patient with decreased GBO KI67+ cell numbers exhibited a radiographic decrease in tumor volume after 1 month of treatment for recurrence. Moreover, the survival times of 3 patients whose GBO KI67+ cell numbers did not significantly change after treatment were below the median.
For bladder cancer, 3 organoid lines were selected from the Human Bladder Cancer Biobank91 and exposed to 6 first-line chemotherapeutic agents. Differences were found among the lines. For example, the organoid line HBL7T2 was relatively resistant to epirubicin and doxorubicin. In contrast, the organoid line HBL12N was more sensitive to gemcitabine and vincristine.
Possibilities for immunotherapy
In recent years, immunotherapy research has progressed, but, because of the complexity of the tumor microenvironment, the efficacy of in vitro models of immunotherapy drugs has not been matched in clinical settings92,93. PDO technology provides a technical breakthrough in this regard and may make immunotherapy possible in the near future.
Using an air-liquid interface method, Neal et al.94 have established more than 100 organoids from 100 individual patient tumors, representing 14 distinct tissue sites and 28 unique disease subtypes, with a 73% success rate. The authors selected 15 of the most rapidly growing organoids for cryopreservation and observed that 80% could be cryo-recovered and serially repropagated every few weeks. Importantly, the organoids included preserved fibroblast stroma and diverse immune elements comprising macrophages, CD8+ T cells, CD4+ T cells, B cells, natural killer cells, and natural killer T cells. Furthermore, the PDOs faithfully recapitulated the TCR repertoire of the original tumors, and tumor-infiltrating lymphocytes functionally recapitulated PD-1-dependent immune checkpoint mechanisms. Together, these data suggest that organoids represent the advent of precision cancer therapies.
Personalized CAR-T immunotherapy has been verified in GBOs89. In that article, the authors investigated the coculture of CAR-T cells with 6 GBO samples, including GBOs with high and low percentages of EGFRvIII+95 cells, and 2 pairs of GBOs from different tumor regions, in which one subregion contained a high percentage of EGFRvIII+ cells and the other subregion did not. The results showed marked expansion of CAR-T cells only after incubation with EGFRvIII+ GBOs. The increased CAR-T cell expansion was accompanied by increase cleaved caspase-3 expression and a decreased ratio of EGFRvIII/EGFR in GBOs, thus suggesting that EGFRvIII+ cells were targeted and killed by CAR-T cells.
Studies on tumor evolution and heterogeneity
Tumors are highly heterogeneous, and substantial heterogeneity exists in cancers across patients (intertumor heterogeneity) and within single tumors (intratumor heterogeneity). Tumor heterogeneity is an ongoing challenge in cancer medicine. Through construction of many PDO lines, the molecular pathologies of various tumors can be analyzed.
Yan et al.96 have constructed a GC organoid biobank comprising normal, dysplastic, cancer, and lymph node metastases (n = 63) from 34 patients. The success rate of normal organoids was more than 90%, and that of GC organoids exceeded 50%. Although the tumor purity in tumor tissues was variable, the organoids had a tumor purity greater than 90% in 95% of cases. This GC organoid library comprised the following common GC subtypes: microsatellite instability, intestinal (chromosome instability, CIN), diffuse (genomically stable), and Epstein–Barr virus. The authors studied intratumoral heterogeneity by constructing organoids comprising adjacent dysplasia, different tumor regions, and lymph node metastases from the same patient. They found that in one patient, tumor organoids from the area of dysplasia at the tumor edge and invasive area shared common early driver mutations involving TP53 and APC, but evolved to have very different patterns of chromosomal aberrations and unique driver mutations. Dysplasic tissues had ASPM, BAX, and TSC1 mutations, whereas invasive tumors had STK11 and SMARCA4 mutations. Moreover, extensive CIN was observed in dysplastic tissues and differed substantially from that in invasive tissues. A comparison of lymph node metastasis organoids with primary tumor organoids revealed marked differences in the mixed-type GC: only 23.3% of mutations were commonly shared, including the key driver TP53. These results indicate the importance of CIN in driving intratumoral heterogeneity and tumor progression.
Sachs et al.59 have established more than 100 BC organoids comprising primary and metastatic BC from 155 patients, achieving a success rate greater than 80%. They have analyzed the histology and receptor status, genomic characterization, and gene expression of the organoid library. BC organoids maintained the histology, genomic, and transcriptomic characteristics of the primary tumors. For example, ductal carcinoma generally gave rise to solid, coherent organoids, whereas lobular carcinoma mainly generated noncohesive organoids. Control organoids established from histologically normal preventive mastectomy samples were very well organized and displayed only a mildly complex cribriform architecture. In contrast, malignant BC organoids exhibited typical cancerous features, such as enlarged and polymorphic nuclei, high mitotic activity, apoptosis, and vacuole formation. In these cases, tumors positive for ER and/or PR generated 75% ER- and/or PR-positive BC organoids. ER- and/or PR-negative tumors generated > 90% ER- and/or PR-negative BC organoids. Eighty percent of HER2-positive BC tissue-formed organoids were HER2 positive, and 90% of HER2-negative BC tissue-formed organoids were HER2 negative.
Jacob et al.89 have generated a GBO biobank derived from 53 patients (including subregional samples) carrying a variety of genomic alterations commonly found in glioblastomas. The organoids were subjected to H&E staining, immunohistochemical staining, and RNA sequencing, thus revealing that the GBOs maintained not only their heterogeneity but also the molecular signatures of primary tumor tissues. For example, quantitative analysis of 8 tumor samples showed that in most cases, the percentages of cells expressing Sox2 and Olig2 were similar in their parental tumors and corresponding GBOs, lasting for up to 4 weeks. The authors generated organoids from different subregions (ANT and PMS) of the same patient, and genomic analyses revealed subregion-specific genomic variants, such as a PTEN missense mutation and copy number loss of 6q and 16q in UP-7788-PMS GBO but not in UP-7788-ANT GBO.
Calandrini et al.85 have generated tumor and matched normal kidney organoids from more than 50 children with KCs of different subtypes, including Wilms tumors, malignant rhabdoid tumors, renal cell carcinomas, and congenital mesoblastic nephroma, with a success rate greater than 75%. The organoids maintained the phenotypic characteristics of the original tumor tissues, and different cell populations were sufficiently distinguished. For example, organoid culture 88T demonstrated distinct clustering of 3 populations. Two of these clusters reflected epithelial subpopulations and represented one stromal cell. In 51T organoids, one population represented epithelial cells, a second population reflected stromal cells, and the third was more complex, expressing markers of epithelial cells, stromal cells, neurogenesis, and nephrogenesis. In addition to retaining the cell populations, KC cancer organoids also recapitulated the diverse genomic landscape and epigenetic profiles of the original tumor tissue, such as copy number alterations, cancer gene mutations, mutational signatures, gene expression patterns, and DNA methylation patterns.
Histological and immunofluorescence analyses of human bladder cancer organoids showed substantial variations among organoids from different tumors91. For example, organoids from different patients were either solid or lumen containing. Different organoids had different morphological structures; for example, some organoids showed smooth circular or slender structures, whereas others exhibited very irregular morphologies.
Future prospects and challenges
Herein, we have attempted to summarize the basic status and applications of the PDO biobanks that have been successfully constructed. Tumor cells are acquired through a wide range of sources, such as tissues retrieved through fine needle biopsy, ultrasound, computed tomography guidance, endoscopic biopsy, rapid autopsy, and surgical resection, and even circulating tumor cells. In fact, cancer hospitals can obtain these tissues very easily. Cancer is a highly heterogeneous disease, and the tumor characteristics of each patient, and even the characteristics of the same tumor tissue, are not exactly the same; thus, the collection of cancer subtypes from many individual patients and different tumor regions may enable tumor heterogeneity to be further studied. In addition, PDO biobanks provide sufficient resources to conduct large-scale high-throughput screening of cancer treatment drugs and provide more accurate medication guidance for cancer treatments. In terms of individual precision medical treatment strategies, the combination of genetic testing and organoids could improve the effects of medications and prevent patients from experiencing the adverse effects of ineffective anticancer drugs.
Despite the advantages of PDO biobanks, many difficulties must be resolved. First, not all tissues can be used to construct organoids. According to previous reports, the features of primary tumors, including the clinical stage, treatment conditions before organoid generation, and pathological diagnosis, do not influence the success rate; however, culture condition modifications according to different tumor types and molecular characteristics can affect the success rate. Second, technology standardization is difficult. Consequently, organoid technology is not widely used for drug development or diagnostics, and similarly, different culturing techniques are used across laboratories. To address this challenge, Brandenberg et al.97 have launched an organoid array technology approach with the potential to fully automate organoid culture for high-throughput and high-content organoid-based screening. Third, although the DNA methylation diversity and transcriptome status in each tumor are stable, reactions to anticancer drugs can differ within the same tumor, thereby indicating that epigenetic changes greatly affect gene expression in cells, causing tumor heterogeneity and drug reaction variations. Better methods are therefore required for tracking and analyzing intratumoral heterogeneity. Fourth, organoids include only the epithelial layer and lack the surrounding mesenchymal cells, immune cells and nervous system98. A possible solution may be coculturing organoids with other cellular components, such as immune cells, stromal cells, and nerve cells99. Fifth, the construction and handling of living cancer biobanks is more tedious than that of traditional cancer biobanks, and essential growth factors are often expensive. To date, no standard protocols exist for organoid culture. However, as commercial entities begin to sell reagents and optimized methods suitable for organoid culture, standard protocols may become available. Sixth, the success rate of organoids is less than 100%; consequently, only some people benefit from personalized treatment with tumor organoids. Seventh, owing to the lack of relevant legislation, standards, and guidelines for organoid technology and tumor organoid banks in China, some problems associated with ethical approval and informed consent exist regarding the construction of PDO biobanks.
Although numerous questions remain, the construction of cancer patient-derived living biobanks is necessary for clinical and basic research. First, technological developments will gradually improve and standardize the construction methods. Second, an increasing number of tumor patients can provide tumor samples of different types and clinical stages. Third, big data analysis based on PDO living biobanks can enhance tumor prevention, diagnosis, treatment, and rehabilitation strategies.
Grant support
This work was supported by the Program for Changjiang Scholars and Innovative Research Team in University in China (Grant No. IRT_14R40); National Key Research and Development Program of China (Grant No. 2021YFC2500400); National Science and Technology Major Project (Grant No. 2017ZX10203207); National Human Genetic Resources Sharing Service Platform (Grant No. 2005DKA21300); National Key Research and Development Program of China; Net Construction of Human Genetic Resource Bio-bank in North China (Grant No. 2016YFC1201703); and National Key R&D Program of China (Grant No. 2017YFC0908300).
Conflict of interest statement
No potential conflicts of interest are disclosed.
Author contributions
Conceived and designed the structure: Kexin Chen, Haixin Li.
Collected the data: Hongkun Liu.
Wrote the paper: Haixin Li, Hongkun Liu.
References
- 1.Yang H, Wang Y, Wang P, Zhang N, Wang P. Tumor organoids for cancer research and personalized medicine. Cancer Biol Med. 2021;19:319–32. doi: 10.20892/j.issn.2095-3941.2021.0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bleijs M, van de Wetering M, Clevers H, Drost J. Xenograft and organoid model systems in cancer research. EMBO J. 2019;38:e101654. doi: 10.15252/embj.2019101654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu H, Lyu X, Yi M, Zhao W, Song Y, Wu K. Organoid technology and applications in cancer research. J Hematol Oncol. 2018;11:116. doi: 10.1186/s13045-018-0662-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clevers H. Modeling development and disease with organoids. Cell. 2016;165:1586–97. doi: 10.1016/j.cell.2016.05.082. [DOI] [PubMed] [Google Scholar]
- 5.Gao D, Vela I, Sboner A, Iaquinta PJ, Karthaus WR, Gopalan A, et al. Organoid cultures derived from patients with advanced prostate cancer. Cell. 2014;159:176–87. doi: 10.1016/j.cell.2014.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sato T, Vries RG, Snippert HJ, van de Wetering M, Barker N, Stange DE, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–5. doi: 10.1038/nature07935. [DOI] [PubMed] [Google Scholar]
- 7.Liu HD, Xia BR, Jin MZ, Lou G. Organoid of ovarian cancer: Genomic analysis and drug screening. Clin Transl Oncol. 2020;22:1240–51. doi: 10.1007/s12094-019-02276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill SJ, Decker B, Roberts EA, Horowitz NS, Muto MG, Worley MJ, Jr, et al. Prediction of DNA repair inhibitor response in short-term patient-derived ovarian cancer organoids. Cancer Discov. 2018;8:1404–21. doi: 10.1158/2159-8290.CD-18-0474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kopper O, de Witte CJ, Lõhmussaar K, Valle-Inclan JE, Hami N, Kester L, et al. An organoid platform for ovarian cancer captures intra- and interpatient heterogeneity. Nat Med. 2019;25:838–49. doi: 10.1038/s41591-019-0422-6. [DOI] [PubMed] [Google Scholar]
- 10.Shi R, Radulovich N, Ng C, Liu N, Notsuda H, Cabanero M, et al. Organoid cultures as preclinical models of non-small cell lung cancer. Clin Cancer Res. 2020;26:1162–74. doi: 10.1158/1078-0432.CCR-19-1376. [DOI] [PubMed] [Google Scholar]
- 11.Alexander KL, Serrano CA, Chakraborty A, Nearing M, Council LN, Riquelme A, et al. Modulation of glycosyltransferase ST6GAL-I in gastric cancer-derived organoids disrupts homeostatic epithelial cell turnover. J Biol Chemistry. 2020;295:14153–63. doi: 10.1074/jbc.RA120.014887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Z, Karthaus WR, Lee YS, Gao VR, Wu C, Russo JW, et al. Tumor microenvironment-derived NRG1 promotes antiandrogen resistance in prostate cancer. Cancer Cell. 2020;38:279–96.e9. doi: 10.1016/j.ccell.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee SH, Hu W, Matulay JT, Silva MV, Owczarek TB, Kim K, et al. Tumor evolution and drug response in patient-derived organoid models of bladder cancer. Cell. 2018;173:515–28.e17. doi: 10.1016/j.cell.2018.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Broutier L, Mastrogiovanni G, Verstegen MM, Francies HE, Gavarró LM, Bradshaw CR, et al. Human primary liver cancer-derived organoid cultures for disease modeling and drug screening. Nat Med. 2017;23:1424–35. doi: 10.1038/nm.4438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li X, Francies HE, Secrier M, Perner J, Miremadi A, Galeano-Dalmau N, et al. Organoid cultures recapitulate esophageal adenocarcinoma heterogeneity providing a model for clonality studies and precision therapeutics. Nat Commun. 2018;9:2983. doi: 10.1038/s41467-018-05190-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dreyer SB, Upstill-Goddard R, Paulus-Hock V, Paris C, Lampraki EM, Dray E, et al. Targeting DNA damage response and replication stress in pancreatic cancer. Gastroenterology. 2021;160:362–77.e13. doi: 10.1053/j.gastro.2020.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hubert CG, Rivera M, Spangler LC, Wu Q, Mack SC, Prager BC, et al. A three-dimensional organoid culture system derived from human glioblastomas recapitulates the hypoxic gradients and cancer stem cell heterogeneity of tumors found in vivo. Cancer Res. 2016;76:2465–77. doi: 10.1158/0008-5472.CAN-15-2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruun J, Kryeziu K, Eide PW, Moosavi SH, Eilertsen IA, Langerud J, et al. Patient-derived organoids from multiple colorectal cancer liver metastases reveal moderate intra-patient pharmacotranscriptomic heterogeneity. Clin Cancer Res. 2020;26:4107–19. doi: 10.1158/1078-0432.CCR-19-3637. [DOI] [PubMed] [Google Scholar]
- 19.Zeng L, Liao Q, Zhao Q, Jiang S, Yang X, Tang H, et al. Raltitrexed as a synergistic hyperthermia chemotherapy drug screened in patient-derived colorectal cancer organoids. Cancer Biol Med. 2021;18:750–62. doi: 10.20892/j.issn.2095-3941.2020.0566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawrence MG, Obinata D, Sandhu S, Selth LA, Wong SQ, Porter LH, et al. Patient-derived models of abiraterone- and enzalutamide-resistant prostate cancer reveal sensitivity to ribosome-directed therapy. Eur Urol. 2018;74:562–72. doi: 10.1016/j.eururo.2018.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aboulkheyr Es H, Montazeri L, Aref AR, Vosough M, Baharvand H. Personalized cancer medicine: an organoid approach. Trends Biotechnol. 2018;36:358–71. doi: 10.1016/j.tibtech.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 22.Kondo J, Inoue M. Application of cancer organoid model for drug screening and personalized therapy. Cells. 2019;8:470. doi: 10.3390/cells8050470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li J, Ghazwani M, Liu K, Huang Y, Chang N, Fan J, et al. Regulation of hepatic stellate cell proliferation and activation by glutamine metabolism. PLoS One. 2017;12:e0182679. doi: 10.1371/journal.pone.0182679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiao H, Wu M, Shao F, Guan G, Huang B, Tan B, et al. N-Acetyl-L-cysteine protects the enterocyte against oxidative damage by modulation of mitochondrial function. Mediat Inflamm. 2016;2016:8364279. doi: 10.1155/2016/8364279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meng Y, Ren Z, Xu F, Zhou X, Song C, Wang VY, et al. Nicotinamide promotes cell survival and differentiation as kinase inhibitor in human pluripotent stem cells. Stem Cell Rep. 2018;11:1347–56. doi: 10.1016/j.stemcr.2018.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wedeken L, Luo A, Tremblay JR, Rawson J, Jin L, Gao D, et al. Adult murine pancreatic progenitors require epidermal growth factor and nicotinamide for self-renewal and differentiation in a serum- and conditioned medium-free culture. Stem Cells Dev. 2017;26:599–607. doi: 10.1089/scd.2016.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang H, Ryu D, Wu Y, Gariani K, Wang X, Luan P, et al. NAD repletion improves mitochondrial and stem cell function and enhances life span in mice. Science (New York, NY) 2016;352:1436–43. doi: 10.1126/science.aaf2693. [DOI] [PubMed] [Google Scholar]
- 28.Zheng M, Guo J. Nicotinamide-induced silencing of SIRT1 by miR-22-3p increases periodontal ligament stem cell proliferation and differentiation. Cell Biol Int. 2020;44:764–72. doi: 10.1002/cbin.11271. [DOI] [PubMed] [Google Scholar]
- 29.Guo Q, Chen S, Rao X, Li Y, Pan M, Fu G, et al. Inhibition of SIRT1 promotes taste bud stem cell survival and mitigates radiation-induced oral mucositis in mice. Am J Transl Res. 2019;11:4789–99. [PMC free article] [PubMed] [Google Scholar]
- 30.Bengoa-Vergniory N, Gorroño-Etxebarria I, López-Sánchez I, Marra M, Di Chiaro P, Kypta R. Identification of noncanonical wnt receptors required for Wnt-3a-induced early differentiation of human neural stem cells. Mol Neurobiol. 2017;54:6213–24. doi: 10.1007/s12035-016-0151-5. [DOI] [PubMed] [Google Scholar]
- 31.Gao K, Zhang T, Wang F, Lv C. Therapeutic potential of Wnt-3a in neurological recovery after spinal cord injury. Eur Neurol. 2019;81:197–204. doi: 10.1159/000502004. [DOI] [PubMed] [Google Scholar]
- 32.Liu X, Cheng Y, Abraham JM, Wang Z, Wang Z, Ke X, et al. Modeling Wnt signaling by CRISPR-Cas9 genome editing recapitulates neoplasia in human barrett epithelial organoids. Cancer Lett. 2018;436:109–18. doi: 10.1016/j.canlet.2018.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lähde M, Heino S, Högström J, Kaijalainen S, Anisimov A, Flanagan D, et al. Expression of R-spondin 1 in Apcmin/+ mice suppresses growth of intestinal adenomas by altering Wnt and transforming growth factor beta signaling. Gastroenterology. 2021;160:245–59. doi: 10.1053/j.gastro.2020.09.011. [DOI] [PubMed] [Google Scholar]
- 34.Lugli N, Kamileri I, Keogh A, Malinka T, Sarris ME, Talianidis I, et al. R-spondin 1 and noggin facilitate expansion of resident stem cells from non-damaged gallbladders. EMBO Rep. 2016;17:769–79. doi: 10.15252/embr.201642169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nuciforo S, Heim MH. Organoids to model liver disease. JHEP Rep. 2021;3:100198. doi: 10.1016/j.jhepr.2020.100198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dossena M, Piras R, Cherubini A, Barilani M, Dugnani E, Salanitro F, et al. Standardized GMP-compliant scalable production of human pancreas organoids. Stem Cell Res Ther. 2020;11:94. doi: 10.1186/s13287-020-1585-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Drost J, van Jaarsveld RH, Ponsioen B, Zimberlin C, van Boxtel R, Buijs A, et al. Sequential cancer mutations in cultured human intestinal stem cells. Nature. 2015;521:43–7. doi: 10.1038/nature14415. [DOI] [PubMed] [Google Scholar]
- 38.Xie Y, Park ES, Xiang D, Li Z. Long-term organoid culture reveals enrichment of organoid-forming epithelial cells in the fimbrial portion of mouse fallopian tube. Stem Cell Res. 2018;32:51–60. doi: 10.1016/j.scr.2018.08.021. [DOI] [PubMed] [Google Scholar]
- 39.Campaner E, Zannini A, Santorsola M, Bonazza D, Bottin C, Cancila V, et al. Breast cancer organoids model patient-specific response to drug treatment. Cancers. 2020;12:3869. doi: 10.3390/cancers12123869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang RR, Koido M, Tadokoro T, Ouchi R, Matsuno T, Ueno Y, et al. Human iPSC-derived posterior gut progenitors are expandable and capable of forming gut and liver organoids. Stem Cell Rep. 2018;10:780–93. doi: 10.1016/j.stemcr.2018.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fujii M, Matano M, Toshimitsu K, Takano A, Mikami Y, Nishikori S, et al. Human intestinal organoids maintain self-renewal capacity and cellular diversity in niche-inspired culture condition. Cell Stem Cell. 2018;23:787–93.e6. doi: 10.1016/j.stem.2018.11.016. [DOI] [PubMed] [Google Scholar]
- 42.Sorrentino G, Rezakhani S, Yildiz E, Nuciforo S, Heim MH, Lutolf MP, et al. Mechano-modulatory synthetic niches for liver organoid derivation. Nat Commun. 2020;11:3416. doi: 10.1038/s41467-020-17161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Broutier L, Andersson-Rolf A, Hindley CJ, Boj SF, Clevers H, Koo BK, et al. Culture and establishment of self-renewing human and mouse adult liver and pancreas 3D organoids and their genetic manipulation. Nat Protoc. 2016;11:1724–43. doi: 10.1038/nprot.2016.097. [DOI] [PubMed] [Google Scholar]
- 44.Aizarani N, Saviano A, Sagar X, Mailly L, Durand S, Herman JS, et al. A human liver cell atlas reveals heterogeneity and epithelial progenitors. Nature. 2019;572:199–204. doi: 10.1038/s41586-019-1373-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hesselbarth R, Esser TU, Roshanbinfar K, Schrüfer S, Schubert DW, Engel FB. CHIR99021 promotes hiPSC-derived cardiomyocyte proliferation in engineered 3D microtissues. Adv Healthc Mater. 2021;10:e2100926. doi: 10.1002/adhm.202100926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Delepine C, Pham VA, Tsang HWS, Sur M. GSK3β inhibitor CHIR 99021 modulates cerebral organoid development through dose-dependent regulation of apoptosis, proliferation, differentiation and migration. PLoS One. 2021;16:e0251173. doi: 10.1371/journal.pone.0251173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang T, Kang W, Du L, Ge S. Rho-kinase inhibitor Y-27632 facilitates the proliferation, migration and pluripotency of human periodontal ligament stem cells. J Cell Mol Med. 2017;21:3100–12. doi: 10.1111/jcmm.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vernardis SI, Terzoudis K, Panoskaltsis N, Mantalaris A. Human embryonic and induced pluripotent stem cells maintain phenotype but alter their metabolism after exposure to rock inhibitor. Sci Rep. 2017;7:42138. doi: 10.1038/srep42138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lau HCH, Kranenburg O, Xiao H, Yu J. Organoid models of gastrointestinal cancers in basic and translational research. Nat Rev Gastroenterol Hepatol. 2020;17:203–22. doi: 10.1038/s41575-019-0255-2. [DOI] [PubMed] [Google Scholar]
- 50.Ida Y, Hikage F, Ohguro H. Rock inhibitors enhance the production of large lipid-enriched 3d organoids of 3t3-l1 cells. Scientific reports. 2021;11:5479. doi: 10.1038/s41598-021-84955-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hahn S, Kim MS, Choi SY, Jeong S, Jee J, Kim HK, et al. Leucine-rich repeat-containing G-protein coupled receptor 5 enriched organoids under chemically-defined growth conditions. Biochem Biophy Res Commun. 2019;508:430–39. doi: 10.1016/j.bbrc.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 52.Zhang C, Guo H, Yang C, Chen Q, Huang J, Liu L, et al. The biological behavior optimization of human periodontal ligament stem cells via preconditioning by the combined application of fibroblast growth factor-2 and A83-01 in in vitro culture expansion. J Transl Med. 2019;17:66. doi: 10.1186/s12967-019-1799-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yip HYK, Tan CW, Hirokawa Y, Burgess AW. Colon organoid formation and cryptogenesis are stimulated by growth factors secreted from myofibroblasts. PLoS One. 2018;13:e0199412. doi: 10.1371/journal.pone.0199412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aoki H, Yamashita M, Hashita T, Ogami K, Hoshino S, Iwao T, et al. Efficient differentiation and purification of human induced pluripotent stem cell-derived endothelial progenitor cells and expansion with the use of inhibitors of ROCK, TGF-β, and GSK3β. Heliyon. 2020;6:e03493. doi: 10.1016/j.heliyon.2020.e03493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leyendecker A., Junior TGF-β inhibitor SB431542 promotes the differentiation of induced pluripotent stem cells and embryonic stem cells into mesenchymal-like cells. Stem Cells Int. 2018;2018:7878201. doi: 10.1155/2018/7878201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang Y, Hou Q, Wu Y, Xu Y, Liu Y, Chen J, et al. Methionine deficiency and its hydroxy analogue influence chicken intestinal 3-dimensional organoid development. Anim Nutr (Zhongguo xu mu shou yi xue hui) 2022;8:38–51. doi: 10.1016/j.aninu.2021.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vlachogiannis G, Hedayat S, Vatsiou A, Jamin Y, Fernández-Mateos J, Khan K, et al. Patient-derived organoids model treatment response of metastatic gastrointestinal cancers. Science (New York, NY) 2018;359:920–26. doi: 10.1126/science.aao2774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goldhammer N, Kim J, Timmermans-Wielenga V, Petersen OW. Characterization of organoid cultured human breast cancer. Breast Cancer Res. 2019;21:141. doi: 10.1186/s13058-019-1233-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sachs N, de Ligt J, Kopper O, Gogola E, Bounova G, Weeber F, et al. A living biobank of breast cancer organoids captures disease heterogeneity. Cell. 2018;172:373–86.e10. doi: 10.1016/j.cell.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 60.Drost J, Karthaus WR, Gao D, Driehuis E, Sawyers CL, Chen Y, et al. Organoid culture systems for prostate epithelial and cancer tissue. Nat Protoc. 2016;11:347–58. doi: 10.1038/nprot.2016.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Beshiri ML, Tice CM, Tran C, Nguyen HM, Sowalsky AG, Agarwal S, et al. A PDX/organoid biobank of advanced prostate cancers captures genomic and phenotypic heterogeneity for disease modeling and therapeutic screening. Clin Cancer Res. 2018;24:4332–45. doi: 10.1158/1078-0432.CCR-18-0409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Puca L, Bareja R, Prandi D, Shaw R, Benelli M, Karthaus WR, et al. Patient derived organoids to model rare prostate cancer phenotypes. Nat Commun. 2018;9:2404. doi: 10.1038/s41467-018-04495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xian B, Luo Z, Li K, Li K, Tang M, Yang R, et al. Dexamethasone provides effective immunosuppression for improved survival of retinal organoids after epiretinal transplantation. Stem Cells Int. 2019;2019:7148032. doi: 10.1155/2019/7148032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kamb A. What’s wrong with our cancer models? Nat Rev Drug Discov. 2005;4:161–5. doi: 10.1038/nrd1635. [DOI] [PubMed] [Google Scholar]
- 65.Aggarwal V, Miranda O, Johnston PA, Sant S. Three dimensional engineered models to study hypoxia biology in breast cancer. Cancer Lett. 2020;490:124–42. doi: 10.1016/j.canlet.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fan TW, El-Amouri SS, Macedo JKA, Wang QJ, Song H, Cassel T, et al. Stable isotope-resolved metabolomics shows metabolic resistance to anti-cancer selenite in 3D spheroids versus 2D cell cultures. Metabolites. 2018;8:40. doi: 10.3390/metabo8030040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bailey M, Christoforidou Z, Lewis MC. The evolutionary basis for differences between the immune systems of man, mouse, pig and ruminants. Vet Immunol Immunopathol. 2013;152:13–9. doi: 10.1016/j.vetimm.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 68.Jiang Y, Yu Y. Transgenic and gene knockout mice in gastric cancer research. Oncotarget. 2017;8:3696–710. doi: 10.18632/oncotarget.12467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mou H, Kennedy Z, Anderson DG, Yin H, Xue W. Precision cancer mouse models through genome editing with CRISPR-Cas9. Genome Med. 2015;7:53. doi: 10.1186/s13073-015-0178-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Walrath JC, Hawes JJ, Van Dyke T, Reilly KM. Genetically engineered mouse models in cancer research. Adv Cancer Res. 2010;106:113–64. doi: 10.1016/S0065-230X(10)06004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kaukonen R, Mai A, Georgiadou M, Saari M, De Franceschi N, Betz T, et al. Normal stroma suppresses cancer cell proliferation via mechanosensitive regulation of JMJD1a-mediated transcription. Nat Commun. 2016;7:12237. doi: 10.1038/ncomms12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bremnes RM, Dønnem T, Al-Saad S, Al-Shibli K, Andersen S, Sirera R, et al. The role of tumor stroma in cancer progression and prognosis: emphasis on carcinoma-associated fibroblasts and non-small cell lung cancer. J Thorac Oncol. 2011;6:209–17. doi: 10.1097/JTO.0b013e3181f8a1bd. [DOI] [PubMed] [Google Scholar]
- 73.Zitvogel L, Pitt JM, Daillère R, Smyth MJ, Kroemer G. Mouse models in oncoimmunology. Nat Rev Cancer. 2016;16:759–73. doi: 10.1038/nrc.2016.91. [DOI] [PubMed] [Google Scholar]
- 74.Santiago-O’Farrill JM, Weroha SJ, Hou X, Oberg AL, Heinzen EP, Maurer MJ, et al. Poly(adenosine diphosphate ribose) polymerase inhibitors induce autophagy-mediated drug resistance in ovarian cancer cells, xenografts, and patient-derived xenograft models. Cancer. 2020;126:894–907. doi: 10.1002/cncr.32600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chen X, Shen C, Wei Z, Zhang R, Wang Y, Jiang L, et al. Patient-derived non-small cell lung cancer xenograft mirrors complex tumor heterogeneity. Cancer Biol Med. 2021;18:184–98. doi: 10.20892/j.issn.2095-3941.2020.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Weeber F, Ooft SN, Dijkstra KK, Voest EE. Tumor organoids as a pre-clinical cancer model for drug discovery. Cell Chem Biol. 2017;24:1092–100. doi: 10.1016/j.chembiol.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 77.Okada S, Vaeteewoottacharn K, Kariya R. Application of highly immunocompromised mice for the establishment of patient-derived xenograft (PDX) models. Cells. 2019;8:889. doi: 10.3390/cells8080889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kemper K, Krijgsman O, Cornelissen-Steijger P, Shahrabi A, Weeber F, Song JY, et al. Intra- and inter-tumor heterogeneity in a vemurafenib-resistant melanoma patient and derived xenografts. EMBO Mol Med. 2015;7:1104–18. doi: 10.15252/emmm.201404914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jung J, Seol HS, Chang S. The generation and application of patient-derived xenograft model for cancer research. Cancer Res Treat. 2018;50:1–10. doi: 10.4143/crt.2017.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Murayama T, Gotoh N. Patient-derived xenograft models of breast cancer and their application. Cells. 2019;8:621. doi: 10.3390/cells8060621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Joshi R, Castro De Moura M, Piñeyro D, Alvarez-Errico D, Arribas C, Esteller M. The DNA methylation landscape of human cancer organoids available at the american type culture collection. Epigenetics. 2020;15:1167–77. doi: 10.1080/15592294.2020.1762398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nanki K, Toshimitsu K, Takano A, Fujii M, Shimokawa M, Ohta Y, et al. Divergent routes toward Wnt and R-spondin niche independency during human gastric carcinogenesis. Cell. 2018;174:856–69.e17. doi: 10.1016/j.cell.2018.07.027. [DOI] [PubMed] [Google Scholar]
- 83.Fujii M, Shimokawa M, Date S, Takano A, Matano M, Nanki K, et al. A colorectal tumor organoid library demonstrates progressive loss of niche factor requirements during tumorigenesis. Cell Stem Cell. 2016;18:827–38. doi: 10.1016/j.stem.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 84.Seino T, Kawasaki S, Shimokawa M, Tamagawa H, Toshimitsu K, Fujii M, et al. Human pancreatic tumor organoids reveal loss of stem cell niche factor dependence during disease progression. Cell Stem Cell. 2018;22:454–67.e6. doi: 10.1016/j.stem.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 85.Calandrini C, Schutgens F, Oka R, Margaritis T, Candelli T, Mathijsen L, et al. An organoid biobank for childhood kidney cancers that captures disease and tissue heterogeneity. Nat Commun. 2020;11:1310. doi: 10.1038/s41467-020-15155-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ganesh K, Wu C, O’Rourke KP, Szeglin BC, Zheng Y, Sauvé CG, et al. A rectal cancer organoid platform to study individual responses to chemoradiation. Nat Med. 2019;25:1607–14. doi: 10.1038/s41591-019-0584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yao Y, Xu X, Yang L, Zhu J, Wan J, Shen L, et al. Patient-derived organoids predict chemoradiation responses of locally advanced rectal cancer. Cell Stem Cell. 2020;26:17–26.e6. doi: 10.1016/j.stem.2019.10.010. [DOI] [PubMed] [Google Scholar]
- 88.Tiriac H, Belleau P, Engle DD, Plenker D, Deschênes A, Somerville TDD, et al. Organoid profiling identifies common responders to chemotherapy in pancreatic cancer. Cancer Discov. 2018;8:1112–29. doi: 10.1158/2159-8290.CD-18-0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jacob F, Salinas RD, Zhang DY, Nguyen PTT, Schnoll JG, Wong SZH, et al. A patient-derived glioblastoma organoid model and biobank recapitulates inter- and intra-tumoral heterogeneity. Cell. 2020;180:188–204.e22. doi: 10.1016/j.cell.2019.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bagley SJ, Schwab RD, Nelson E, Viaene AN, Binder ZA, Lustig RA, et al. Histopathologic quantification of viable tumor versus treatment effect in surgically resected recurrent glioblastoma. J Neuro-Oncol. 2019;141:421–29. doi: 10.1007/s11060-018-03050-6. [DOI] [PubMed] [Google Scholar]
- 91.Mullenders J, de Jongh E, Brousali A, Roosen M, Blom JPA, Begthel H, et al. Mouse and human urothelial cancer organoids: a tool for bladder cancer research. Proc Natl Acad Sci U S A. 2019;116:4567–74. doi: 10.1073/pnas.1803595116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Prasetyanti PR, Medema JP. Intra-tumor heterogeneity from a cancer stem cell perspective. Mol Cancer. 2017;16:41. doi: 10.1186/s12943-017-0600-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.McGranahan N, Swanton C. Clonal heterogeneity and tumor evolution: Past, present, and the future. Cell. 2017;168:613–28. doi: 10.1016/j.cell.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 94.Neal JT, Li X, Zhu J, Giangarra V, Grzeskowiak CL, Ju J, et al. Organoid modeling of the tumor immune microenvironment. Cell. 2018;175:1972–88.e16. doi: 10.1016/j.cell.2018.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.O’Rourke DM, Nasrallah MP, Desai A, Melenhorst JJ, Mansfield K, Morrissette JJD, et al. A single dose of peripherally infused EGFRvIII-directed CAR T cells mediates antigen loss and induces adaptive resistance in patients with recurrent glioblastoma. Sci Transl Med. 2017;9:eaaa0984. doi: 10.1126/scitranslmed.aaa0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yan HHN, Siu HC, Law S, Ho SL, Yue SSK, Tsui WY, et al. A comprehensive human gastric cancer organoid biobank captures tumor subtype heterogeneity and enables therapeutic screening. Cell Stem Cell. 2018;23:882–97.e11. doi: 10.1016/j.stem.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 97.Brandenberg N, Hoehnel S, Kuttler F, Homicsko K, Ceroni C, Ringel T, et al. High-throughput automated organoid culture via stem-cell aggregation in microcavity arrays. Nat Biomed Eng. 2020;4:863–74. doi: 10.1038/s41551-020-0565-2. [DOI] [PubMed] [Google Scholar]
- 98.Jabs J, Zickgraf FM, Park J, Wagner S, Jiang X, Jechow K, et al. Screening drug effects in patient-derived cancer cells links organoid responses to genome alterations. Mol Syst Biol. 2017;13:955. doi: 10.15252/msb.20177697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Öhlund D, Handly-Santana A, Biffi G, Elyada E, Almeida AS, Ponz-Sarvise M, et al. Distinct populations of inflammatory fibroblasts and myofibroblasts in pancreatic cancer. J Exp Med. 2017;214:579–96. doi: 10.1084/jem.20162024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Seidlitz T, Merker SR, Rothe A, Zakrzewski F, von Neubeck C, Grützmann K, et al. Human gastric cancer modelling using organoids. Gut. 2019;68:207–17. doi: 10.1136/gutjnl-2017-314549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ooft SN, Weeber F, Dijkstra KK, McLean CM, Kaing S, van Werkhoven E, et al. Patient-derived organoids can predict response to chemotherapy in metastatic colorectal cancer patients. Sci Transl Med. 2019;11:eaay2574. doi: 10.1126/scitranslmed.aay2574. [DOI] [PubMed] [Google Scholar]
- 102.Jammula S, Katz-Summercorn AC, Li X, Linossi C, Smyth E, Killcoyne S, et al. Identification of subtypes of barrett’s esophagus and esophageal adenocarcinoma based on DNA methylation profiles and integration of transcriptome and genome data. Gastroenterology. 2020;158:1682–97.e1. doi: 10.1053/j.gastro.2020.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lampis A, Carotenuto P, Vlachogiannis G, Cascione L, Hedayat S, Burke R, et al. MIR21 drives resistance to heat shock protein 90 inhibition in cholangiocarcinoma. Gastroenterology. 2018;154:1066–79.e5. doi: 10.1053/j.gastro.2017.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dijkstra KK, Cattaneo CM, Weeber F, Chalabi M, van de Haar J, Fanchi LF, et al. Generation of tumor-reactive T cells by co-culture of peripheral blood lymphocytes and tumor organoids. Cell. 2018;174:1586–98.e12. doi: 10.1016/j.cell.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Huang L, Holtzinger A, Jagan I, BeGora M, Lohse I, Ngai N, et al. Ductal pancreatic cancer modeling and drug screening using human pluripotent stem cell- and patient-derived tumor organoids. Nat Med. 2015;21:1364–71. doi: 10.1038/nm.3973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lannagan TRM, Lee YK, Wang T, Roper J, Bettington ML, Fennell L, et al. Genetic editing of colonic organoids provides a molecularly distinct and orthotopic preclinical model of serrated carcinogenesis. Gut. 2019;68:684–92. doi: 10.1136/gutjnl-2017-315920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Han TS, Voon DCC, Oshima H, Nakayama M, Echizen K, Sakai E, et al. Interleukin 1 up-regulates microRNA 135b to promote inflammation-associated gastric carcinogenesis in mice. Gastroenterology. 2019:156, 1140–55.e4. doi: 10.1053/j.gastro.2018.11.059. [DOI] [PubMed] [Google Scholar]
- 108.Bian S, Repic M, Guo Z, Kavirayani A, Burkard T, Bagley JA, et al. Genetically engineered cerebral organoids model brain tumor formation. Nat Methods. 2018;15:631–39. doi: 10.1038/s41592-018-0070-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Drost J, van Boxtel R, Blokzijl F, Mizutani T, Sasaki N, Sasselli V, et al. Use of CRISPR-modified human stem cell organoids to study the origin of mutational signatures in cancer. Science (New York, NY) 2017;358:234–8. doi: 10.1126/science.aao3130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Biffi G, Oni TE, Spielman B, Hao Y, Elyada E, Park Y, et al. Il1-induced JAK/STAT signaling is antagonized by TGFβ to shape CAF heterogeneity in pancreatic ductal adenocarcinoma. Cancer Discov. 2019;9:282–301. doi: 10.1158/2159-8290.CD-18-0710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ooft SN, Weeber F, Schipper L, Dijkstra KK, McLean CM, Kaing S, et al. Prospective experimental treatment of colorectal cancer patients based on organoid drug responses. ESMO Open. 2021;6:100103. doi: 10.1016/j.esmoop.2021.100103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.van de Wetering M, Francies HE, Francis JM, Bounova G, Iorio F, Pronk A, et al. Prospective derivation of a living organoid biobank of colorectal cancer patients. Cell. 2015;161:933–45. doi: 10.1016/j.cell.2015.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Matano M, Date S, Shimokawa M, Takano A, Fujii M, Ohta Y, et al. Modeling colorectal cancer using CRISPR-Cas9-mediated engineering of human intestinal organoids. Nat Med. 2015;21:256–62. doi: 10.1038/nm.3802. [DOI] [PubMed] [Google Scholar]
- 114.Decaesteker B, Denecker G, Van Neste C, Dolman EM, Van Loocke W, Gartlgruber M, et al. TBX2 is a neuroblastoma core regulatory circuitry component enhancing MYCN/FOXM1 reactivation of DREAM targets. Nat Commun. 2018;9:4866. doi: 10.1038/s41467-018-06699-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Boj SF, Hwang CI, Baker LA, Chio II, Engle DD, Corbo V, et al. Organoid models of human and mouse ductal pancreatic cancer. Cell. 2015;160:324–38. doi: 10.1016/j.cell.2014.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ruess DA, Heynen GJ, Ciecielski KJ, Ai J, Berninger A, Kabacaoglu D, et al. Mutant KRAS-driven cancers depend on PTPN11/SHP2 phosphatase. Nat Med. 2018;24:954–60. doi: 10.1038/s41591-018-0024-8. [DOI] [PubMed] [Google Scholar]
- 117.Lõhmussaar K, Oka R, Espejo Valle-Inclan J, Smits MHH, Wardak H, Korving J, et al. Patient-derived organoids model cervical tissue dynamics and viral oncogenesis in cervical cancer. Cell Stem Cell. 2021;28:1380–96.e6. doi: 10.1016/j.stem.2021.03.012. [DOI] [PubMed] [Google Scholar]
- 118.Chen D, Tan Y, Li Z, Li W, Yu L, Chen W, et al. Organoid cultures derived from patients with papillary thyroid cancer. J Clin Endocrinol Metab. 2021;106:1410–26. doi: 10.1210/clinem/dgab020. [DOI] [PubMed] [Google Scholar]
- 119.Sondorp LHJ, Ogundipe VML, Groen AH, Kelder W, Kemper A, Links TP, et al. Patient-derived papillary thyroid cancer organoids for radioactive iodine refractory screening. Cancers. 2020;12:3212. doi: 10.3390/cancers12113212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Driehuis E, Spelier S, Hernández IB, de Bree R, Willems SM, Clevers H, et al. Patient-derived head and neck cancer organoids recapitulate EGFR expression levels of respective tissues and are responsive to EGFR-targeted photodynamic therapy. J Clin Med. 2019;8:1880. doi: 10.3390/jcm8111880. [DOI] [PMC free article] [PubMed] [Google Scholar]