Abstract
Objective
Involuntary admission to psychiatric inpatient care can protect both patients with severe mental illnesses and individuals around them. This study analyzed annual healthcare costs per person for involuntary psychiatric admission and examined categories of mental disorders and other factors associated with mortality.
Methods
This retrospective cohort study collected 1 million randomly sampled beneficiaries from the National Health Insurance Database for 2002–2013. It identified and matched 181 patients with involuntary psychiatric admissions (research group) with 724 patients with voluntary psychiatric admissions (control group) through 1:4 propensity-score matching for sex, age, comorbidities, mental disorder category, and index year of diagnosis.
Results
Mean life expectancy of patients with involuntary psychiatric admissions was 33.13 years less than the general population. Average annual healthcare costs per person for involuntary psychiatric admissions were 3.94 times higher compared with voluntary admissions. The general linear model demonstrated that average annual medical costs per person per compulsory hospitalization were 5.8 times that of voluntary hospitalization. Survival analysis using the Cox proportional hazards model found no significant association between type of psychiatric admission (involuntary or voluntary) and death.
Conclusion
This study revealed no significant difference in mortality between involuntary and voluntary psychiatric admissions, indicating involuntary treatment’s effectiveness.
Keywords: Mental disorders, Involuntary psychiatric admissions, Health care costs
INTRODUCTION
Suicide is the tenth leading cause of death in the United States. Suicide rates have increased in nearly every country [1], and 68% of patients admitted for suicide have received diagnoses of emotional disorders [2]. According to the Ministry of Health and Welfare (MOHW), Executive Yuan, ROC (Taiwan), the numbers of outpatients and admitted patients with mental illness are increasing annually. Many cases of random killings by patients with mental disorders have been reported, resulting in a greater emphasis on involuntary psychiatric admissions and medical treatment in Taiwan [3].
Compared with an average person, patients with mental illness have a higher risk of mortality. The standardized mortality rate of patients with severe mental illness is twice that of the general population, with a lifespan by 30 years. The main causes of death include suicide, accidents, and other disease-related causes [4,5]. According to the Department of Mental and Oral Health, MOHW, the leading cause of suicide in 2018 was affective or interpersonal relationships (15,327 persons, 46.2%), followed by mental health or substance abuse (13,568 persons, 40.9%). Therefore, mental illness is closely associated with death. Patients with mental illness differ in mortality risk by age group. Regardless of gender, young patients with mental illness have a higher risk of mortality, with a death rate five times that of an average person [6,7]. Although involuntary psychiatric admission for patients with mental illness can reduce the incidences of self-mutilation and harming others, studies have demonstrated that the main cause of death during hospitalization is suicide or sudden death caused by an existing disease; these deaths are unpredictable and have an extremely low rate of successful emergency rescue [8,9].
Some studies have indicated that a large part of the disease burden is attributed to behavioral risk factors [10]. Some international studies have also indicated that involuntary psychiatric admissions are necessary and reasonable for patients with mental illness who are a danger to themselves or others [11].
Studies on the medical costs of involuntary psychiatric admissions have indicated that men and older patients have a higher likelihood of admission; affective psychosis are the most common diagnoses, and they have higher medical costs [12]. The total daily medical cost per patient is €318 (approximately NT$10,000) for involuntary psychiatric admissions and €272 (approximately NT$9,000) for voluntary psychiatric admissions [13]. Moreover, patients with mental illness and severe comorbidities have higher rates of outpatient and emergency visits and readmissions, thereby increasing total medical costs [12,14,15]. Regarding patients with depression, the average total medical costs per patient differ significantly in terms of gender, age, and severity, and they are twice as high for men as they are for women; total costs are twice as high in patients with severe depression as they are for patients with moderate depression [16]. Studies have demonstrated that the overall medical costs of adult patients with depression are 33% higher than those of average adults [17].
According to the aforementioned studies, the medical costs of patients with mental illness are influenced by various factors and are considerably related to the risk of mental illness and death. However, studies analyzing death rates and medical expenditures by using propensity score matching (PSM) are not yet available. On the basis of the current literature review, studies related to mortality risk and medical expenditures for involuntary and voluntary psychiatric admissions remain scant. Therefore, this study adopted various factors as variables to analyze the death rates and medical expenses of involuntary and voluntary psychiatric admissions.
METHODS
Research design
It was hypothesized that Involuntary Psychiatric Admissions are associated with the increased medical cost and mortality risk. The research framework of this study involved correlations among involuntary psychiatric admissions, medical costs, and mortality risk. To select individuals with similar attributes for research and control groups and to prevent heterogeneity between selection error and the baseline [18], this study performed 1:4 PSM for patients with mental illness who had involuntary and voluntary psychiatric admissions in terms of sex, age, comorbidity severity, insured amount, mental illness type, and year of diagnosis. The research group contained 181 patients with involuntary psychiatric admissions, and the control group consisted of 724 patients with voluntary psychiatric admissions (905 patients in total). The current study was reviewed and approved by the Research Ethics Committee at China Medical University and Hospital, Taichung, Taiwan, under no. CMUH105-REC3–016. The requirement of informed consent was waived by the ethics committee.
Data source and study sample
This study used the Longitudinal Health Insurance Database (LHID), which contains the claims data of 1 million beneficiaries randomly selected from all people insured by Taiwan’s National Health Insurance program. We obtained electronic data from the National Health Research Institutes with the authorization of the Department of Health. The LHID contains information on medical care for inpatient and outpatient visits for each beneficiary from 2002 to 2013. In accordance with the Taiwan Personal Information Protection Act, the identities of insured people were recoded by randomization before data were released to researchers.
The research population consisted of patients with mental illness classified by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) [19] with diagnostic codes: 290.xx–319.xx from 2002 to 2013. Because patients receiving diagnoses of mental illness in 2002 could not be validated as having first-time diagnoses of mental illness, all cases diagnosed in 2002 were excluded. In addition, because minors are a vulnerable group, to protect their rights, this study retained only patients older than 20 years as research patients.
Variables
Research variables were extracted from the database content, and most variables were obtained from the first data entries of patients during the research period as the determination basis, such as mental illness type, sex, age, insured amount, institution level, institution ownership type, primary physician seniority, insured branch, and degree of urbanization. The remaining variables were obtained from all entries input during the research period including involuntary psychiatric admissions, whether patients had multiple mental illnesses, comorbidity severity, drug use, death, and medical costs. The first entry of mental illness diagnosed between 2002 and 2013 was adopted as patients’ type of mental illness. The mental illness diagnostic codes were determined by referencing the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) [20]. In reference [19] to, comorbidity severity (Charlson comorbidity index, CCI) was grouped.
Statistical analysis
All statistical analyses were performed using SAS version 9.4 (Statistical Analysis System, SAS Institute Inc., Cary, NC, USA). The significance level of 0.05 was determined while p-value less than 0.05 was considered statistically significant. Besides, SPSS 23.0 (IBM Corp., Armonk, NY, USA) was adopted as a drawing tool of survival analysis. A chi-square independent test χ2 was adopted to test the independence between independent variables, specifically the chrematistics of patients with mental illness (including characteristics of patient health, demographics, medical caregivers, and regions) and dependent variables (death, total medical costs, and average annual medical cost per person). A general linear model (GLM) was used to perform a multivariate analysis to compare the least squares (LS) means of independent variables affecting the average annual medical cost per person (patient receiving care). Since this study considered multiple independent variables, the Cox proportional hazards model was used to determine the relationship between independent variables and death, in order to show the status of mortality risk among different variables.
RESULTS
This study performed PSM on the basis of sex, age, comorbidity severity, insured amount, and type of mental illness. A total of 181 persons (20%) had involuntary psychiatric admissions, and 724 persons (80%) had voluntary psychiatric admissions. After matching, the chi-square independence tests between variables were conducted (Table 1). Patient death was not significantly correlated with the type of psychiatric admission, involuntary or voluntary (p=0.276). Regarding the mental illness type, a majority of patients (406 persons, 44.86%) had “other mental illnesses,” followed by schizophrenia (151 persons, 16.69%). Death was significantly correlated with the mental illness type (p<0.001). Patients with organic mental disorders had a significantly higher death rate (25.40%) than those with other mental illnesses (7.88%). The CCI is a common tool for evaluating comorbidities. In this study, 774 patients (85.52%) had a CCI of 0. Patient death was significantly correlated with the CCI (p<0.001). Patients with CCI scores of ≥2 had a significantly higher death rate (33.33%) than those with CCI scores of <2. Regarding the effect of sex and age on death in patients with mental illness, men and those older than 65 years had significantly higher death rates.
Table 1.
Chi-square test of matched patient samples for mental illness type (N=905)
| Variable | Total number of persons | Death toll | No death toll | p-value |
|---|---|---|---|---|
| Involuntary psychiatric admissions | 0.276 | |||
| Yes | 181 | 27 (14.92) | 154 (85.08) | |
| No | 724 | 84 (11.60) | 640 (88.40) | |
| Type of mental illness | <0.001 | |||
| Organic mental disorder | 126 | 32 (25.40) | 94 (74.60) | |
| Schizophrenia | 151 | 12 (7.95) | 139 (92.05) | |
| Affective psychosis | 139 | 17 (12.23) | 122 (87.77) | |
| Substance abuse | 83 | 18 (21.69) | 65 (78.31) | |
| Other mental illnesses | 406 | 32 (7.88) | 374 (92.12) | |
| If suffering from multiple mental illnesses | 0.308 | |||
| Yes | 485 | 65 (13.40) | 420 (86.60) | |
| No | 420 | 46 (10.95) | 374 (89.05) | |
| Comorbidity severity | <0.001 | |||
| 0 point | 774 | 80 (10.34) | 694 (89.66) | |
| 1 point | 113 | 25 (22.12) | 88 (77.88) | |
| 2 points (and higher) | 18 | 6 (33.33) | 12 (66.67) | |
| Drug use | 0.099 | |||
| Without use of classified drugs | 245 | 23 (9.39) | 222 (90.61) | |
| Use of anti-psychotics alone | 35 | 2 (5.71) | 33 (94.29) | |
| Use of antidepressants alone | 23 | 4 (17.39) | 19 (82.61) | |
| Use of mood stabilizers alone | 244 | 40 (16.39) | 204 (83.61) | |
| Use of multiple classified drugs | 358 | 42 (11.73) | 316 (88.27) | |
| Sex | <0.001 | |||
| Female | 331 | 23 (6.95) | 308 (93.05) | |
| Male | 574 | 88 (15.33) | 486 (84.67) | |
| Age (yr) | 0.002 | |||
| 20–34 | 224 | 19 (8.48) | 205 (91.52) | |
| 35–49 | 368 | 38 (10.33) | 330 (89.67) | |
| 50–64 | 250 | 39 (15.60) | 211 (84.40) | |
| 65 (and higher) | 63 | 15 (23.81) | 48 (76.19) | |
| Insured amount ($) | 0.004 | |||
| 20,008 (and lower) | 699 | 99 (14.16) | 600 (85.84) | |
| 20,009–22,800 | 155 | 7 (4.52) | 148 (95.48) | |
| 22,801 (and higher) | 51 | 5 (9.80) | 46 (90.20) | |
| Institution level | 0.003 | |||
| Medical center | 149 | 23 (15.44) | 126 (84.56) | |
| District hospital | 314 | 44 (14.01) | 270 (85.99) | |
| Regional hospital | 186 | 29 (15.59) | 157 (84.41) | |
| Primary level clinic | 256 | 15 (5.86) | 241 (94.14) | |
| Type of institution ownership | 0.106 | |||
| Public hospital or institution | 282 | 42 (14.89) | 240 (85.11) | |
| Private hospital or institution | 400 | 38 (9.50) | 362 (90.50) | |
| Foundation hospital or institution | 198 | 29 (14.65) | 169 (85.35) | |
| Corporation hospital or institution | 25 | 2 (8.00) | 23 (92.00) | |
| Seniority of primary physician (yr) | 0.079 | |||
| 5 (and lower) | 555 | 61 (10.99) | 494 (89.01) | |
| 6–10 | 27 | 7 (25.93) | 20 (74.07) | |
| 11–15 | 122 | 19 (15.57) | 103 (84.43) | |
| 6 (and higher) | 201 | 24 (11.94) | 177 (88.06) | |
| Insured branch | 0.094 | |||
| Taipei | 289 | 28 (9.69) | 261 (90.31) | |
| Northern | 117 | 23 (19.66) | 94 (80.34) | |
| Central | 177 | 21 (11.86) | 156 (88.14) | |
| Southern | 121 | 11 (9.09) | 110 (90.91) | |
| Kaohsiung & Pingtung | 173 | 24 (13.87) | 149 (86.13) | |
| Eastern | 28 | 4 (14.29) | 24 (85.71) | |
| Degree of urbanization | 0.374 | |||
| Cities and towns with a high degree of urbanization | 229 | 21 (9.17) | 208 (90.83) | |
| Cities and towns with a moderate degree of urbanization | 297 | 45 (15.15) | 252 (84.85) | |
| Emerging cities and towns | 156 | 18 (11.54) | 138 (88.46) | |
| General cities and towns | 118 | 17 (14.41) | 101 (85.59) | |
| Aging and cities and towns | 21 | 3 (14.29) | 18 (85.71) | |
| Agricultural cities and towns | 39 | 4 (10.26) | 35 (89.74) | |
| Remote towns | 45 | 3 (6.67) | 42 (93.33) |
Values are presented as number (%) unless otherwise indicated
To compare the influence on annual per-person medical costs by different independent variables among the matched samples, the GLM, also known as a multivariate linear regression, was adopted in this study to analyze the average annual medical cost per person (Table 2). The data of 905 persons in total were analyzed. According to Table 2, after correcting the other variables, patients with involuntary psychiatric admissions incurred significantly higher mean of average annual medical costs per person than those of patients with voluntary psychiatric admissions (p<0.001, LS mean: NT$102,899.83 and NT$26,139.79, respectively). Patients with schizophrenia incurred significantly higher average medical costs (p<0.001, LS mean: NT$102,979.04) than those with organic mental disorders, affective psychosis, substance abuse, and other mental illnesses (LS mean: NT$63,166.28, NT$49,520.19, NT$54,537.53, and NT$52,396.01). Hence, mental illness type exhibited the significant mean differences in average medical costs. In addition, drug use exhibited a significant mean difference (p<0.001) in average medical costs. The use of multiple classified drugs was associated with significantly higher average medical costs (p<0.05, LS mean: NT$88,004.36) when compared to without use of classified drugs, use of antipsychotic drugs, antidepressants, or mood stabilizers alone (LS mean: NT$60,588.00, NT$52,020.68, NT$62,419.16, and NT$59,566.85) Comorbidity severity, multiple mental illnesses, sex, age, insured amount, institution level, institution ownership type, seniority of primary physician, insured branch, and degree of urbanization exhibited no significant mean differences in average medical costs.
Table 2.
General linear model of average annual medical cost per person (N=905)
| Variable | The least square mean (NT$) | p-value |
|---|---|---|
| Involuntary psychiatric admissions | <0.001 | |
| Yes | 102,899.83 | |
| No | 26,139.79 | |
| Type of mental illness | <0.001 | |
| Organic mental disorder | 63,166.28 | |
| Schizophrenia | 102,979.04 | |
| Affective psychosis | 49,520.19 | |
| Substance abuse | 54,537.53 | |
| Other mental illnesses | 52,396.01 | |
| If suffering from multiple mental illnesses | 0.777 | |
| Yes | 65,419.81 | |
| No | 63,619.81 | |
| Comorbidity severity | 0.733 | |
| 0 point | 66,397.17 | |
| 1 point | 59,764.16 | |
| 2 points (and higher) | 67,398.10 | |
| Drug use | 0.001 | |
| Without use of classified drugs | 60,588.00 | |
| Use of antipsychotics alone | 52,020.68 | |
| Use of antidepressants alone | 62,419.16 | |
| Use of mood stabilizers alone | 59,566.85 | |
| Use of multiple classified drugs | 88,004.36 | |
| Sex | 0.611 | |
| Female | 63,089.42 | |
| Male | 65,950.20 | |
| Age (yr) | 0.980 | |
| 20–34 | 62,479.69 | |
| 35–49 | 64,132.78 | |
| 50–64 | 64,137.04 | |
| 65 (and higher) | 67,329.73 | |
| Insured amount ($) | 0.135 | |
| 20,008 (and lower) | 62,649.88 | |
| 20,009–22,800 | 53,202.14 | |
| 22,801 (and higher) | 77,707.42 | |
| Institution level | 0.450 | |
| Medical center | 70,053.72 | |
| District hospital | 63,996.67 | |
| Regional hospital | 67,937.40 | |
| Primary level clinic | 56,091.46 | |
| Type of institution ownership | 0.755 | |
| Public hospital or institution | 65,539.43 | |
| Private hospital or institution | 59,534.36 | |
| Foundation hospital or institution | 60,367.45 | |
| Corporation hospital or institution | 72,638.01 | |
| Seniority of primary physician (yr) | 0.914 | |
| 5 (and lower) | 67,070.72 | |
| 6–10 | 63,907.97 | |
| 11–15 | 64,742.54 | |
| 16 (and higher) | 62,358.02 | |
| Insured branch | 0.692 | |
| Taipei | 56,140.72 | |
| Northern | 64,815.73 | |
| Central | 65,852.25 | |
| Southern | 64,211.11 | |
| Kaohsiung & Pingtung | 58,613.91 | |
| Eastern | 77,485.15 | |
| Degree of urbanization | 0.701 | |
| Cities and towns with a high degree of urbanization | 67,290.28 | |
| Cities and towns with a moderate degree of urbanization | 66,334.97 | |
| Emerging cities and towns | 58,439.20 | |
| General cities and towns | 72,159.41 | |
| Aging and cities and towns | 65,172.96 | |
| Agricultural cities and towns | 51,208.29 | |
| Remote towns | 71,033.56 |
By using hazard ratio (HR) to compare the mortality risk among variables, the Cox proportional hazards model was adopted to perform the survival analysis. Table 3 showed that the type of psychiatric admissions (voluntary admissions as the reference group) was not significantly associated with death, both for the unadjusted and adjusted results. Regarding the type of mental illness, the adjusted Cox model survival analysis demonstrated that when using patients with other mental illnesses as a reference and controlling for the other variables, the HR of patients with organic mental disorders was 3.311 times that of the reference group (p<0.001, 95% CI: 1.823–6.014). Regarding the multiple mental illnesses, comorbidity severity and drug use in the adjusted survival analysis were not significantly associated with death. When using females as the reference group and controlling for the other variables, mortality risk in males was 1.913 times higher than that of the reference group (p=0.011, 95% CI: 1.161–3.153).
Table 3.
Survival analysis of death among the matched samples of patients (N=905)
| Variable | Unadjusted |
Adjusted |
|||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | ||
| Subject to involuntary psychiatric admissions | |||||||
| Yes | 1.235 | 0.800–1.906 | 0.341 | 1.294 | 0.738–2.270 | 0.368 | |
| No (reference group) | - | - | - | - | - | - | |
| Type of mental illness | |||||||
| Organic mental disorder | 4.401 | 2.683–7.217 | <0.001 | 3.311 | 1.823–6.014 | <0.001 | |
| Schizophrenia | 0.948 | 0.488–1.841 | 0.874 | 1.085 | 0.506–2.326 | 0.833 | |
| Affective psychosis | 1.848 | 1.024–3.337 | 0.042 | 2.505 | 1.279–4.908 | 0.007 | |
| Substance abuse | 2.692 | 1.510–4.801 | <0.001 | 2.785 | 1.451–5.345 | 0.002 | |
| Other mental illnesses (reference group) | - | - | - | - | - | - | |
| If suffering from multiple mental illnesses | |||||||
| Yes | 1.115 | 0.764–1.627 | 0.573 | 0.709 | 0.435–1.154 | 0.166 | |
| No (reference group) | - | - | - | - | - | - | |
| Comorbidity severity | |||||||
| 0 point (reference group) | - | - | - | - | - | - | |
| 1 point | 1.852 | 1.180–2.906 | 0.007 | 1.181 | 0.675–2.068 | 0.559 | |
| 2 points (and higher) | 3.177 | 1.377–7.329 | 0.007 | 1.794 | 0.713–4.515 | 0.214 | |
| Drug use | |||||||
| Without use of classified drugs (reference group) | - | - | - | - | - | - | |
| Use of anti-psychotics alone | 0.582 | 0.137–2.469 | 0.463 | 0.355 | 0.075–1.677 | 0.191 | |
| Use of antidepressants alone | 1.720 | 0.593–4.985 | 0.318 | 1.628 | 0.541–4.904 | 0.386 | |
| Use of mood stabilizers alone | 1.850 | 1.108–3.090 | 0.019 | 1.709 | 0.984–2.967 | 0.057 | |
| Use of multiple classified drugs | 1.070 | 0.643–1.782 | 0.795 | 0.932 | 0.491–1.770 | 0.829 | |
| Sex | |||||||
| Female (reference group) | - | - | - | - | - | - | |
| Male | 2.278 | 1.439–3.605 | <0.001 | 1.913 | 1.161–3.153 | 0.011 | |
| Age (yr) | |||||||
| 20–34 (reference group) | - | - | - | - | - | - | |
| 35–49 | 1.135 | 0.653–1.973 | 0.654 | 1.401 | 0.764–2.570 | 0.276 | |
| 50–64 | 2.111 | 1.213–3.673 | 0.008 | 1.968 | 1.072–3.613 | 0.029 | |
| 65 (and higher) | 4.163 | 2.104–8.236 | <0.001 | 3.815 | 1.684–8.639 | 0.001 | |
| Insured amount ($) | |||||||
| 20,008 (and lower) | 3.538 | 1.643–7.619 | 0.001 | 2.967 | 1.317–6.684 | 0.009 | |
| 20,009–22,800 (reference group) | - | - | - | - | - | - | |
| 22,801 (and higher) | 2.439 | 0.774–7.688 | 0.128 | 3.537 | 1.041–12.017 | 0.043 | |
| Institution level | |||||||
| Medical center | 2.447 | 1.276–4.693 | 0.007 | 1.953 | 0.877–4.347 | 0.101 | |
| District hospital | 2.360 | 1.313–4.240 | 0.004 | 2.229 | 1.084–4.586 | 0.029 | |
| Regional hospital | 2.462 | 1.319–4.596 | 0.005 | 2.459 | 1.201–5.033 | 0.014 | |
| Primary level clinic (reference group) | - | - | - | - | - | - | |
| Type of institution ownership | |||||||
| Public hospital or institution (reference group) | - | - | - | - | - | - | |
| Private hospital or institution | 0.666 | 0.430–1.034 | 0.070 | 0.995 | 0.567–1.746 | 0.985 | |
| Foundation hospital or institution | 1.079 | 0.672–1.733 | 0.754 | 1.115 | 0.662–1.877 | 0.683 | |
| Corporation hospital or institution | 0.714 | 0.172–2.954 | 0.642 | 0.495 | 0.115–2.129 | 0.345 | |
| Seniority of primary physician (yr) | |||||||
| 5 (and lower) (reference group) | - | - | - | - | - | - | |
| 6–10 | 3.000 | 1.370–6.573 | 0.006 | 3.505 | 1.426–8.616 | 0.006 | |
| 11–15 | 1.286 | 0.768–2.154 | 0.338 | 1.148 | 0.640–2.061 | 0.644 | |
| 16 (and higher) | 0.926 | 0.577–1.486 | 0.749 | 1.482 | 0.863–2.547 | 0.154 | |
| Insured branch | |||||||
| Taipei (reference group) | - | - | - | - | - | - | |
| Northern | 2.210 | 1.272–3.841 | 0.005 | 2.231 | 1.194–4.168 | 0.012 | |
| Central | 1.219 | 0.692–2.147 | 0.493 | 1.478 | 0.761–2.870 | 0.249 | |
| Southern | 1.003 | 0.499–2.016 | 0.992 | 1.213 | 0.559–2.634 | 0.625 | |
| Kaohsiung & Pingtung | 1.386 | 0.804–2.392 | 0.240 | 1.876 | 1.008–3.491 | 0.047 | |
| Eastern | 1.447 | 0.507–4.126 | 0.490 | 1.407 | 0.449–4.410 | 0.558 | |
| Degree of urbanization | |||||||
| Cities and towns with a high degree of urbanization (reference group) | - | - | - | - | - | - | |
| Cities and towns with a moderate degree of urbanization | 1.662 | 0.989–2.791 | 0.055 | 1.582 | 0.900–2.779 | 0.111 | |
| Emerging cities and towns | 1.316 | 0.701–2.471 | 0.393 | 1.198 | 0.602–2.383 | 0.606 | |
| General cities and towns | 1.675 | 0.883–3.174 | 0.114 | 1.914 | 0.927–3.952 | 0.079 | |
| Aging and cities and towns | 1.389 | 0.414–4.660 | 0.594 | 1.567 | 0.417–5.884 | 0.506 | |
| Agricultural cities and towns | 1.058 | 0.363–3.083 | 0.918 | 0.831 | 0.264–2.619 | 0.753 | |
| Remote towns | 0.679 | 0.202–2.278 | 0.530 | 0.659 | 0.182–2.382 | 0.525 | |
HR, hazard ratio; CI, confidence interval
Table 4 tabulates the average age at diagnosis, survival time, age at death, years of potential life lost (YPLL), and expenditure survival ratio (ESR). By analyzing patients with mental illness with involuntary and voluntary psychiatric admissions from 2002 to 2013, the association with death was observed. The survival time of patients with involuntary psychiatric admissions was 1.13 years longer than that of patients with voluntary psychiatric admissions. In particular, the largest gap in survival time was between the patients with schizophrenia who were involuntarily admitted (7 years) and those with mental illness who were voluntarily admitted (3.30 years). Moreover, the survival time of patients with schizophrenia who were involuntarily admitted was 3.7 years longer than that of patients with schizophrenia who were voluntarily admitted. Patients with affective psychosis had the largest YPLL regardless of whether they had involuntary or voluntary psychiatric admissions, accounting for 46.69 and 42.88 years, respectively. ESR was highest for patients with schizophrenia, accounting for NT$1,273,092.25 and NT$616,067.65, respectively.
Table 4.
Death rate, survival time, average life expectancy, and YPLL for involuntary psychiatric admissions
| Variable | Number of persons | Age of suffering from illness (yr) | Death rate (%) | Survival time (yr) | Life expectancy (yr) | YPLL | Expenditure survival ratio (NT$) |
|---|---|---|---|---|---|---|---|
| Subject to involuntary psychiatric admissions | 27 | 41.74 | 14.92 | 5.15 | 46.89 | 33.13 | |
| Organic mental disorder | 7 | 57.43 | 28.00 | 4.00 | 61.43 | 18.59 | 573,871.60 |
| Schizophrenia | 2 | 46.00 | 6.45 | 7.00 | 53.00 | 27.02 | 1,273,092.25 |
| Affective psychosis | 3 | 27.67 | 11.11 | 5.67 | 33.33 | 46.69 | 573,270.19 |
| Substance abuse | 5 | 32.40 | 31.25 | 5.80 | 38.20 | 41.82 | 736,378.13 |
| Other mental illnesses | 10 | 38.80 | 12.20 | 5.10 | 43.90 | 36.12 | 707,964.63 |
| Not subject to involuntary psychiatric admissions | 84 | 43.21 | 11.6 | 4.42 | 47.63 | 32.39 | |
| Organic mental disorder | 25 | 51.72 | 24.75 | 4.12 | 55.84 | 24.18 | 139,952.75 |
| Schizophrenia | 10 | 42.20 | 8.33 | 3.30 | 45.50 | 34.52 | 616,067.65 |
| Affective psychosis | 14 | 33.93 | 12.05 | 3.21 | 37.14 | 42.88 | 70,934.01 |
| Substance abuse | 13 | 44.77 | 19.40 | 5.38 | 50.15 | 29.87 | 27,575.23 |
| Other mental illnesses | 22 | 39.00 | 6.79 | 5.45 | 44.45 | 35.57 | 14,821.23 |
YPLL was obtained by subtracting the life expectancy computed in this study from the 80.02-year life expectancy released by the Ministry of the Interior in 2013. YPLL, years of potential life lost
A scatter plot was created to compare mortality risk with average annual medical costs per person for patients with five types of mental disorders (Figure 1). The results showed that other mental illnesses had the lowest mortality risk. Comparatively, patients with organic mental disorders had the highest mortality risk (HR=3.311), whereas those with substance abuse (HR=2.785), affective psychosis (HR=2.505), and schizophrenia exhibited no difference in mortality risk compared with other mental illnesses. Patients with schizophrenia incurred the highest total medical costs, followed by those with organic mental disorders, affective psychosis, drug abuse, and other mental illnesses. Those with schizophrenia also had the highest average annual medical costs, followed by organic mental disorders, affective psychosis, other mental illnesses, and drug abuse.
Figure 1.
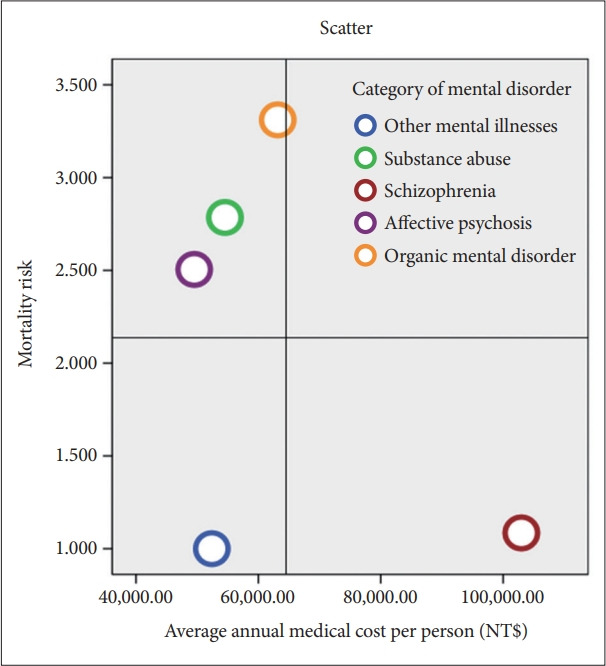
Scatter plot of mortality risk and medical costs for patients with mental illness.
DISCUSSION
Association between mortality risk and involuntary psychiatric admissions
The life expectancy of patients with mental illness is shorter than that of an average person, compared to female patients with psychiatric disorders, male patients with psychiatric disorders likely demonstrate more unfavorable behaviors, insufficient health care use, and lower medical compliance. In addition, the average YPLL in men with psychiatric disorders are longer [21-26], and the difference in the mortality risk of patients with and without mental illness has gradually widened [27] because of the increased life expectancy of the general public [21,28]. This study demonstrated that other high-risk mortality factors of patients with mental illness including male, age ≥65 years, insured amount ≥$22,801, regional-level hospitals, primary caregiver seniority of 6–10 years, and northern insured branch. A chi-square test was performed to analyze the correlation between involuntary psychiatric admissions and death for the matched samples of patients.The sample of this study are patients with severe mental illness, and they have more life lost than those with a general mental illness. The patients with involuntary psychiatric admissions had a shorter life expectancy but did not have a significantly different mortality risk compared with patients with voluntary admissions. The medical conditions of the patients were effectively controlled during hospitalization, but patients were likely to lack health awareness and have medical attention interruptions after hospital discharge, which resulted in involuntary psychiatric readmissions that indirectly contributed to an increased mortality risk. Therefore, health authorities should use post discharge care and periodic tracking to strengthen home medical care services [29] after patients who were admitted involuntarily are discharged from the hospital to prevent the aggravation of medical conditions and death [30].
Association between cost effectiveness and involuntary psychiatric admissions
The analysis results in this study demonstrated that patients with involuntary psychiatric admissions had significantly higher medical costs than those with general psychiatric illness. This finding coincides with the results of an international study [13]. The average annual medical costs of patients with involuntary psychiatric admissions was NT$115,654, which was 5.8 times higher than that of patients with voluntary psychiatric admissions. Thus, the medical cost burden for patients with involuntary psychiatric admissions was significantly higher than that of patients with voluntary psychiatric admissions. Regarding mental illness type, the average annual medical cost per person for patients with schizophrenia was the highest at NT$93,492, whereas the medical costs for patients with drug abuse were the lowest. Some studies have indicated that the length of time required to survive the acute phase of a disease varies by mental illness. In particular, patients with schizophrenia required the longest recovery and hospitalization time [31], leading to higher medical costs such as medication, treatment, and ward fees.
Involuntary psychiatric admissions fall under the need and factors of health services utilization in Andersen’s behavioral model [32]. Patients have higher readmission rates and longer hospitalization times. They may also have higher hospitalization and treatment needs, which likely increase higher costs of drug administration and medical condition control.
Organic mental disorders accounted for the highest mortality risk in this study, whereas other mental illnesses accounted for the lowest risk. Schizophrenia accounted for the highest medical costs, whereas substance abuse accounted for the lowest costs. In this study, other factors related to the mortality risk of patients with mental illness were analyzed to determine their high-risk mortality factors, such as male, old age, high income, regional-level hospital, and lower physician seniority, which can serve as a reference for relevant government units during policy formulation.
In this study, secondary data were collected from the National Health Insurance Database of the National Health Research Institutes. Therefore, only available data patterns were explored. Because of the database limitation in this study, only medical expenses and drug use among patients with mental illness were analyzed. Follow-up research should include variables for education level, work status, and genetic history to further investigate the basic characteristics of patients with mental illness and enhance the research. This study demonstrated that some patients with involuntary psychiatric admissions were likely to be readmitted. The medical conditions of these patients were likely to be recurrent and uncontrollable. Follow-up studies may consider the factors contributing to multiple involuntary psychiatric admissions to further explore the effect of mortality risk and medical costs to enhance research completeness.
In conclusion, severe and complex conditions are characteristic of patients with involuntary psychiatric admissions. This study demonstrated no significant difference in mortality risk between patients with voluntary and involuntary psychiatric admissions. However, average annual per-person medical costs were significantly higher for patients with involuntary psychiatric admissions than for patients with voluntary psychiatric admissions. Thus, controlling their medical conditions requires more resources. Furthermore, personal, family, and social costs are a substantial burden. The government should formulate relevant health policies, engage in active planning regarding high medical costs, and plan relevant health welfare. The results in this study show that compared to voluntarily admitted patients, the potential life lost (YPLL) may be slightly longer. On the other hand, the research results also show that the average survival time, from a confirmed diagnosis of psychiatric disorders to death, of involuntarily admitted patients is 5.15 years, which is longer compared to voluntarily admitted patients. The sample of this study are patients with severe mental illness, and they have more life lost than those with a general mental illness. Treatment may effectively stabilize their condition and reduce mortality, possibly indicating the effectiveness of involuntary treatments. Compared with disease prevention plans intended only to treat diseases, cost effectiveness in disease prevention exerts a greater influence on people. Early intervention in medical institutions for patients with involuntary psychiatric admissions is recommended to provide the most effective medical care. Priority low-cost interventions targeting patients with organic mental disorders and drug abuse should be implemented to improve the quality of psychiatric care and the financial balance of the National Health Insurance program by extending integrative care in homes, communities, and medical institutions.
Acknowledgments
We are grateful to Health Data Science Center, China Medical University Hospital for providing administrative, technical and funding support.
Footnotes
Availability of Data and Material
The datasets used in this study are available from the Ministry of Health and Welfare, Taiwan, on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Pei-Ying Tseng, Xin-Yu Xie, Jong-Yi Wang. Data curation: Pei-Ying Tseng, Xin-Yu Xie, Ching-Chi Hsu, Jong-Yi Wang. Formal analysis: Pei-Ying Tseng, Xin-Yu Xie, Jong-Yi Wang. Funding acquisition: Jong-Yi Wang. Investigation: Pei-Ying Tseng, Xin-Yu Xie, Jong-Yi Wang. Methodology: Pei-Ying Tseng, Xin-Yu Xie, Jen-De Chen, Jong-Yi Wang. Project administration: Pei-Ying Tseng, Xin-Yu Xie. Resources: Jong-Yi Wang. Software: Xin-Yu Xie. Supervision: Jong-Yi Wang. Validation: Pei-Ying Tseng, Xin-Yu Xie. Visualization: Pei-Ying Tseng, Xin-Yu Xie. Writing—original draft: Pei-Ying Tseng, Xin-Yu Xie, Jong-Yi Wang. Writing—review & editing: Ching-Chi Hsu, Jong-Yi Wang, Jen-De Chen, Sarina Hui-Lin Chien.
Funding Statement
This research was supported by Ministry of Science and Technology, Taiwan (Grant no. MOST109-2410-H-039-001 and MOST110-2410-H-039-001) and China Medical University (Grant no. CMU108-MF-103, CMU109-MF-119, and CMU110-MF-123).
REFERENCES
- 1.Grumet JG, Hogan MF, Chu A, Covington DW, Johnson KE. Compliance standards pave the way for reducing suicide in health care systems. J Health Care Compl. 2019;21:17–26. [Google Scholar]
- 2.Meyfroidt N, Wyckaert S, Bouckaert F, Wampers M, Mazereel V, Bruffaerts R. Suicide in Belgian psychiatric inpatients. A matched case-control study in a Belgian teaching hospital. Arch Psychiatr Nurs. 2020;34:8–13. doi: 10.1016/j.apnu.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Fu TS, Lee CS, Gunnell D, Lee WC, Cheng AT. Changing trends in the prevalence of common mental disorders in Taiwan: a 20-year repeated cross-sectional survey. Lancet. 2013;381:235–241. doi: 10.1016/S0140-6736(12)61264-1. [DOI] [PubMed] [Google Scholar]
- 4.Fekadu A, Medhin G, Kebede D, Alem A, Cleare AJ, Prince M, et al. Excess mortality in severe mental illness: 10-year population-based cohort study in rural Ethiopia. Br J Psychiatry. 2015;206:289–296. doi: 10.1192/bjp.bp.114.149112. [DOI] [PubMed] [Google Scholar]
- 5.Lawrence D, Hancock KJ, Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ. 2013;346:f2539. doi: 10.1136/bmj.f2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang CK, Hayes RD, Broadbent M, Fernandes AC, Lee W, Hotopf M, et al. All-cause mortality among people with serious mental illness (SMI), substance use disorders, and depressive disorders in southeast London: a cohort study. BMC Psychiatry. 2010;10:77. doi: 10.1186/1471-244X-10-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gissler M, Laursen TM, Ösby U, Nordentoft M, Wahlbeck K. Patterns in mortality among people with severe mental disorders across birth cohorts: a register-based study of Denmark and Finland in 1982-2006. BMC Public Health. 2013;13:834. doi: 10.1186/1471-2458-13-834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schaffer A, Sinyor M, Kurdyak P, Vigod S, Sareen J, Reis C, et al. Population-based analysis of health care contacts among suicide decedents: identifying opportunities for more targeted suicide prevention strategies. World Psychiatry. 2016;15:135–145. doi: 10.1002/wps.20321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pompili M, Mancinelli I, Ruberto A, Kotzalidis GD, Girardi P, Tatarelli R. Where schizophrenic patients commit suicide: a review of suicide among inpatients and former inpatients. Int J Psychiatry Med. 2005;35:171–190. doi: 10.2190/9CA1-EL73-1VXD-9F2V. [DOI] [PubMed] [Google Scholar]
- 10.Cadilhac DA, Magnus A, Sheppard L, Cumming TB, Pearce DC, Carter R. The societal benefits of reducing six behavioural risk factors: an economic modelling study from Australia. BMC Public Health. 2011;11:483. doi: 10.1186/1471-2458-11-483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Jong MH, Wierdsma AI, van Baars AWB, Van Gool AR, Mulder CL. How dangerousness evolves after court-ordered compulsory psychiatric admission: explorative prospective observational cohort study. BJPsych Open. 2019;5:e32. doi: 10.1192/bjo.2019.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bardach NS, Coker TR, Zima BT, Murphy JM, Knapp P, Richardson LP, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133:602–609. doi: 10.1542/peds.2013-3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolff J, McCrone P, Patel A, Normann C. Determinants of per diem hospital costs in mental health. PLoS One. 2016;11:e0152669. doi: 10.1371/journal.pone.0152669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Egede LE, Walker RJ, Bishu K, Dismuke CE. Trends in costs of depression in adults with diabetes in the United States: Medical Expenditure Panel Survey, 2004-2011. J Gen Intern Med. 2016;31:615–622. doi: 10.1007/s11606-016-3650-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurdyak PA, Gnam WH, Goering P, Chong A, Alter DA. The relationship between depressive symptoms, health service consumption, and prognosis after acute myocardial infarction: a prospective cohort study. BMC Health Serv Res. 2008;8:200. doi: 10.1186/1472-6963-8-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krauth C, Stahmeyer JT, Petersen JJ, Freytag A, Gerlach FM, Gensichen J. Resource utilisation and costs of depressive patients in Germany: results from the primary care monitoring for depressive patients trial. Depress Res Treat. 2014;2014:730891. doi: 10.1155/2014/730891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shirneshan E, Bailey J, Relyea G, Franklin BE, Solomon DK, Brown LM. Incremental direct medical expenditures associated with anxiety disorders for the U.S. adult population: evidence from the Medical Expenditure Panel Survey. J Anxiety Disord. 2013;27:720–727. doi: 10.1016/j.janxdis.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Chen CP, Cheng PW, Lai HM, Hsiao HC. Exploring the relationship between certifications and wages among university graduate students: a propensity score-matched analysis. Contemp Educ Res Q. 2015;23:71–111. [Google Scholar]
- 19.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 20.American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 21.Laursen TM, Musliner KL, Benros ME, Vestergaard M, Munk-Olsen T. Mortality and life expectancy in persons with severe unipolar depression. J Affect Disord. 2016;193:203–207. doi: 10.1016/j.jad.2015.12.067. [DOI] [PubMed] [Google Scholar]
- 22.Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425–448. doi: 10.1146/annurev-clinpsy-032813-153657. [DOI] [PubMed] [Google Scholar]
- 23.Lee MC. Investigating the mortality and health care costs for patients with mental disorders in Taiwan [Master’s Thesis] Taichung: China Medical University; 2017. [Google Scholar]
- 24.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang QL, Zhao LG, Zhang W, Li HL, Gao J, Han LH, et al. Combined impact of known lifestyle factors on total and cause-specific mortality among Chinese men: a prospective cohort study. Sci Rep. 2017;7:5293. doi: 10.1038/s41598-017-05079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ogbemudia EJ, Odiase FE. Poor compliance with lifestyle modifications and related factors in hypertension. Highl Med Res J. 2021;21:57–62. [Google Scholar]
- 27.Wang JY, Chang CC, Lee MC, Li YJ. Identification of psychiatric patients with high mortality and low medical utilization: a population-based propensity score-matched analysis. BMC Health Serv Res. 2020;20:230. doi: 10.1186/s12913-020-05089-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lawrence D, Kisely S, Pais J. The epidemiology of excess mortality in people with mental illness. Can J Psychiatry. 2010;55:752–760. doi: 10.1177/070674371005501202. [DOI] [PubMed] [Google Scholar]
- 29.Park AL, McDaid D, Weiser P, Von Gottberg C, Becker T, Kilian R, HELPS Network Examining the cost effectiveness of interventions to promote the physical health of people with mental health problems: a systematic review. BMC Public Health. 2013;13:787. doi: 10.1186/1471-2458-13-787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molyneaux E, Turner A, Candy B, Landau S, Johnson S, Lloyd-Evans B. Crisis-planning interventions for people with psychotic illness or bipolar disorder: systematic review and meta-analyses. BJPsych Open. 2019;5:e53. doi: 10.1192/bjo.2019.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Z, Lin C, Ma B, Bian Y. Activities of daily living in hospitalized patients with mental disorders. Asian J Psychiatr. 2018;32:77–78. doi: 10.1016/j.ajp.2017.11.038. [DOI] [PubMed] [Google Scholar]
- 32.Andersen RJ. A behavioral model of families’ use of health services. Chicago: University of Chicago; 1968. [Google Scholar]


