Abstract
Congenital lobar overinflation (CLO) is a rare congenital pulmonary abnormality characterized by progressive overexpansion of a lobe(s) exerting mass effect on the remaining lobes and the mediastinum. Bilateral involvement is extremely rare and has been reported only a handful of times. We present a case of bilateral congenital lobar overinflation in a term female neonate managed with single-step bilateral lobectomies.
Keywords: Congenital lobar overinflation, CLO, Congenital lobar emphysema, Bilateral CLO, Neonatal respiratory distress
Introduction
CLO is a developmental pulmonary abnormality characterized by progressive overinflation of one or more lobes of the lungs with resultant mass effect and compression of the remaining lobes [1]. The cause is not clearly elucidated as of yet, but it is thought to be due to either intrinsic cartilaginous abnormality (absence or weakness) or extrinsic narrowing of the airway by a mediastinal mass such as a bronchogenic cyst or a vessel. There is an established lobar predominance with the most commonly involved lobe being the left upper lobe, followed by the right middle lobe and right upper lobe. Lower lobe involvement is rare [2]. Bilateral involvement is even rarer with fewer than 20 reported cases throughout modern literature. A summary of the reported cases of bilateral congenital lobar overinflation is listed in Table 1. The vast majority of the reported cases showed involvement of the left upper lobe and right middle lobe.
Table 1.
Previously reported cases of bilateral congenital lobar overinflation.
| Authors | Year of report | Involved lobes |
|---|---|---|
| Floyd FW, et al. [6] | 1963 | LUL, RML |
| May RL, et al. [7] | 1964 | LUL, RML |
| Schramel R, et al. [8] | 1968 | LUL, RML |
| Schiller HM, et al. [9] | 1970 | RML, RLL, LLL |
| Tournier G, et al. [10] | 1973 | LUL, RML |
| Ekkelkamp S, et al. [11] | 1987 | LUL, RML |
| Stigers KB, et al. [12] | 1992 | 2 cases (RML, LLL and RLL, LLL) |
| Maiya S, et al. [13] | 2005 | LUL, RML |
| Kumar TS, et al. [14] | 2006 | LUL, RML |
| Abushahin AM, et al. [15] | 2012 | LUL, RML |
| Perea L, et al. [4] | 2017 | 4 cases (all LUL, RML) |
| Ait Chtouk M, et al. [16] | 2020 | LUL, RML |
| Lei Q, et al. [17] | 2020 | LLL, RML |
| Sawant V, et al. [5] | 2021 | LUL, RML |
We report a rare case of bilateral CLO involving the left upper lobe and right middle lobe in a female newborn presenting with respiratory distress since birth. She was successfully managed with single-stage bilateral lobectomies. As to our search, this is the first reported case of bilateral CLO in Ethiopia.
Case report
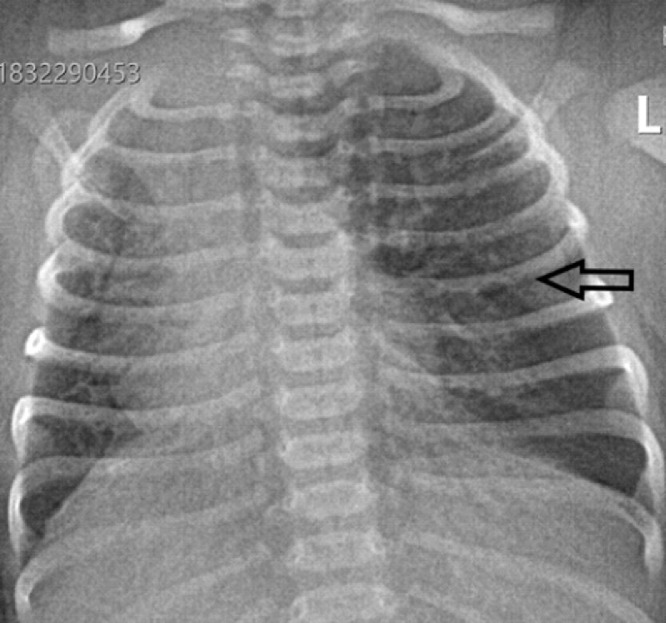
We report a case of a 28 days old female neonate who was born at a gestational age of 39 weeks and 4 days by caesarian section for an indication of 2 previous CS scars. She presented with fast breathing since 6 hours of age which progressively worsened over time. At presentation, she was tachypneic (65 breaths per minute). She also had subcostal/intercostal retractions and mild chest in drawing. Chest auscultation at initial presentation was unremarkable. Baseline investigations including CBC, RBS, RFT and serum electrolytes were normal except for a mild hypokalemia which was corrected. Blood culture was non-revealing. Abdominal ultrasound was also normal. Transthoracic echocardiography (not shown) revealed patent foramen ovale with left to right shunt. She was admitted with a working diagnosis of EONS. She failed to improve despite being put on IV antibiotics and intranasal oxygen. Chest radiograph and subsequently chest CT were obtained. The initial chest radiograph (Fig. 1) revealed hyperinflated left lung with mediastinal shift to the right side. Two possibilities were initially considered, the first being right lung hypoplasia with compensatory hyperinflation of the left lung. The second differential consideration was left lung hyperinflation with a vascular ring as a possible cause. Chest CT was then obtained to better characterize the abnormality detected on the chest radiograph.
Fig. 1.
Frontal chest radiograph showing hyperinflation of the left lung (arrow) with mediastinal shift to the right side.
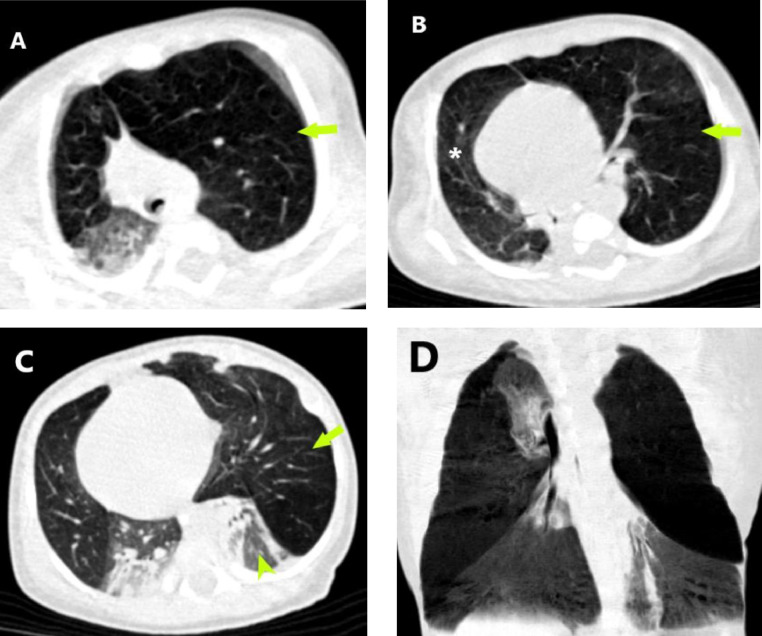
The chest CT obtained at the age of 28 days (Fig. 2) revealed the presence of marked hyperinflation of the left upper lobe with attenuated pulmonary vasculature and causing significant mediastinal shift to the right side. In addition, the right middle lobe was also hyperinflated demonstrating similar attenuation to that of the left upper lobe. Compressive atelectasis of the remaining lobes (bilateral lower lobes and the right upper lobe) was noted. On the mediastinal window, no compressive mass or enlarged vessel was demonstrated.
Fig. 2.
Axial chest CT images in lung window settings at different levels (A through C) demonstrate the presence of marked overinflation of the left upper lobe (arrows) resulting in compressive atelectasis of the left lower lobe (arrowhead) and significant mediastinal shift to the right. Right middle lobe hyperinflation (asterisk) with collapse consolidation of the right upper and lower lobes is also seen (C). Coronal minimal intensity projection (D) better demonstrates the overinflated and collapsed lobes.
The diagnosis of impending respiratory failure secondary to bilateral congenital lobar overinflation was made, and the infant was prepared for surgery. Thoracotomy and single-stage bilateral lobectomy of the left upper lobe and right middle lobe was performed. She had a smooth postoperative course. A chest radiograph obtained on her seventh postoperative day (Fig. 3) showed optimal expansion of the previously collapsed lobes and resolution of the mediastinal shift. The infant was discharged on her tenth POD. She is being followed at outpatient clinic and is doing well as of the time of writing this case report.
Fig. 3.
Postoperative frontal chest radiograph shows expansion of the previously collapsed lower lobes and the right upper lobe, and resolution of the mediastinal shift.
Discussion
Congenital lobar overinflation, also known as congenital lobar emphysema is an uncommon abnormality of the lungs characterized by overinflation of a lobe. It is thought to be due to an intrinsic or extrinsic bronchial abnormality causing a ball-valve mechanism with resultant hyperinflation of the affected lobe [3]. CLO classically presents in the neonatal period with respiratory distress, with 80% of cases presenting by the age of 6 months. It is 3 times more common in males (M:F = 3:1) [2]. The left upper lobe is the most frequently involved lobe (42%) followed by the right middle lobe (35%). Lower lobe involvement is quite rare. Bilateral CLO is also extremely rare with fewer than 20 case reports found in modern literature. As to our knowledge, the case we are presenting is the first of its kind reported in Ethiopia.
Imaging plays an important role in the diagnosis of CLO. Radiographs obtained soon after birth may show opacity of the involved lobe due to retained fetal fluid. Subsequent films will demonstrate hyperlucency and hyper expansion of the affected lobe with associated mediastinal shift and compression of the remaining lobes. CT will better demonstrate the extent of involvement and degree of mass effect. CLO appears as a hyperexpanded lobe with attenuated pulmonary vasculature. CT will also exclude secondary causes of lobar overinflation such as compressing mediastinal masses and vascular anomlies [3]. The vast majority (88%) of the few case reports of bilateral CLO showed involvement of the left upper lobe and right middle lobe. Our case is also in keeping with this pattern with these 2 lobes involved. Given the rarity bilateral CLO, it can be a diagnostic challenge and imaging, especially CT, plays an irreplaceable role in ascertaining the diagnosis. Our patient was not diagnosed until 28 days of age despite having been symptomatic since day 1.
The management of bilateral CLO has been a topic of debate. There are 2 major schools of thought. The first one involves performing a staged surgery with removal of one of the affected lobes (typically the one with the more pronounced mass effect). The child would then be followed and a second surgery to remove the other lobe would be done if indicated. If the child remains stable and there is no significant rebound hyperinflation of the non-removed diseased lung, conservative management would be sought. The rationale behind this approach is that a single stage bilateral lobectomy is a high-risk procedure with increased risk of complications and postoperative pain. In the reviewed case reports and case series, this approach appears to be the more popular one. In the largest single institution case series on bilateral CLO, 3 of the 4 patients were managed with unilateral lobectomy. They were followed and remained stable without needing a second surgery [4]. The second approach would be performing a single stage bilateral lobectomy. It has been advocated by some institutions [5]. Our patient was successfully managed with a single stage bilateral lobectomy of the left upper lobe and right middle lobe. She had a smooth postoperative course and is doing well at the moment of writing this case report.
In conclusion, bilateral congenital lobar overinflation is an extremely rare cause of respiratory distress in the newborn. Its diagnosis requires high index of suspicion and relies on imaging, typically with chest radiographs and CT. There are 2 main approaches to its management including single step bilateral lobectomy and staged (2-step) surgery.
Patient consent statement
Informed consent to prepare and publish this case report was obtained from the parents of the child. Personal identifiers were not used in the case report.
Footnotes
Competing Interests: All authors declare no conflict of interest.
REFERENCES
- 1.Bhalla A, Jana M. Congenital lung abnormalities. Imaging Pediatr Chest Atlas. 2015;98195:34. doi: 10.5005/jp/books/12621_5. [DOI] [Google Scholar]
- 2.Glass RBJ. 11th Ed. Mosby/Elsevier; Philadelphia, PA: 2008. Caffey's Pediatric Diagnostic Imaging. Vol 191. [DOI] [Google Scholar]
- 3.Adam A, Dixon AK, Gillard J, Schaefer-Prokop C, Grainger RG, Allison DJ. Elsevier Health Sciences; Philadelphia, PA: 2014. Grainger & Allison's Diagnostic Radiology E-Book. [Google Scholar]
- 4.Perea L, Blinman T, Piccione J, Laje P. Bilateral congenital lobar emphysema: staged management. J Pediatr Surg. 2017;52(9):1442–1445. doi: 10.1016/j.jpedsurg.2017.01.056. [DOI] [PubMed] [Google Scholar]
- 5.Sawant V, Prabhudesai S, Sawant B, Das S. One-stage bilateral lobectomy in an infant with bilateral congenital lobar emphysema. J Indian Assoc Pediatr Surg. 2021;26(5):348–350. doi: 10.4103/jiaps.JIAPS_168_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Floyd FW, Repici AJ, Gibson ET, McGeorge CK. Bilateral congenital lobar emphysema surgically corrected. Pediatrics. 1963;31(1):87–96. [PubMed] [Google Scholar]
- 7.MAY RL, MEESE EH, TIMMES JJ. Congenital lobar emphysema: case report of bilateral involvement. J Thorac Cardiovasc Surg. 1964;48(5):850–854. doi: 10.1016/s0022-5223(19)33369-0. [DOI] [PubMed] [Google Scholar]
- 8.Schramel R, Waring W, Lago D, Fortenberry R. Congenital lobar emphysema: report of a case treated by bilateral simultaneous pulmonary resection. J Louisiana State Med Soc. 1968;120(3):111–114. [PubMed] [Google Scholar]
- 9.Schiller HM, Yatteau RF, Madge GE. Bilateral congenital lobar emphysema. South Med J. 1970;63(8):977–978. doi: 10.1097/00007611-197008000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Tournier G, Designolle M, Binet JP, et al. Bilateral congenital lobar emphysema. Successful 1-stage right middle and left upper lobectomy. Arch Fr Pediatr. 1973;30(5):561. [PubMed] [Google Scholar]
- 11.Ekkelkamp S, Vos A. Successful surgical treatment of a newborn with bilateral congenital lobar emphysema. J Pediatr Surg. 1987;22(11):1001–1002. doi: 10.1016/S0022-3468(87)80495-5. [DOI] [PubMed] [Google Scholar]
- 12.Stigers KB, Woodring JH, Kanga JF. The clinical and imaging spectrum of findings in patients with congenital lobar emphysema. Pediatr Pulmonol. 1992;14(3):160–170. doi: 10.1002/ppul.1950140305. [DOI] [PubMed] [Google Scholar]
- 13.Maiya S, Clarke JR, More B, Desai M, Parikh D. Bilateral congenital lobar emphysema: how should we proceed? Pediatr Surg Int. 2005;21(8):659–661. doi: 10.1007/s00383-005-1425-6. [DOI] [PubMed] [Google Scholar]
- 14.Kumar TS, Simon A, Sen S. Bilateral congenital emphysema: unusual cause for recurrent respiratory tract infection. J Indian Assoc Pediatr Surg. 2006;11(3):151–152. doi: 10.4103/0971-9261.27246. [DOI] [Google Scholar]
- 15.Abushahin AM, Tuffaha AS, Khalil NK, Ismeal AM. Bilateral congenital lobar emphysema: a rare cause for respiratory distress in infancy. Ann Thorac Med. 2012;7(4):250–252. doi: 10.4103/1817-1737.102187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.M AC, Y EB, B Z, D B, H J. Exceptional cause of respiratory distress: bilateral congenital lobar emphysema. Sch J Med Case Rep. 2020;08(04):499–501. doi: 10.36347/sjmcr.2020.v08i04.023. [DOI] [Google Scholar]
- 17.Lei Q, Zeng W, Ju R. Congenital lobar emphysema in bilateral lung lobes: a case report. Transl Pediatr. 2020;9(3):256–261. doi: 10.21037/TP-19-147. [DOI] [PMC free article] [PubMed] [Google Scholar]