Abstract
The 17 Sustainable Development Goals (SDGs) were adopted by the United Nations (UN) General Assembly in 2015 to set the world on the path to peace, prosperity, and sustainable development. As a result of the global focus on SDGs, in particular SDG 3—ensuring a healthy life and promoting well-being for all—and its 13 targets, significant progress has been made in global health. The Global Action Plan for the Prevention and Control of Noncommunicable Diseases (NCDs) was officially placed on the World Health Organization (WHO) agenda in 2013. Subsequently, the UNs’ SDGs incorporated SDG 3.4, based on which many countries have been developing national strategies to reduce burden of NCDs. Besides, building upon WHO’s efforts to promote universal health coverage (UHC) since 2010, SDG 3.8 with a focus on UHC was adopted, following which 75% of national health policies were developed with the aim of moving toward UHC.
Almost through one-third of SDG’s pathway, the COVID-19 pandemic has been hampering global efforts to achieve the 2030 agenda. The ongoing COVID-19 pandemic has affected all aspects of social, political, environmental, and economic life worldwide. The crisis has made SDGs almost unlikely to reach. It has unprecedentedly interrupted the provision of and access to essential healthcare services in all settings. The situation worsened particularly in low- and middle-income countries, where preexisting health inequalities and weak health systems jeopardized control and mitigation. The disruption in the provision of healthcare services may have long-term consequences for people with NCDs, especially the most vulnerable and in need of regular long-term care. Worse still, patients with NCDs have been reported to be at higher risk for serious illness or death from COVID-19. The pandemic also reinforces the importance of UHC, the need to prioritize universal health preparedness and accelerate global efforts to build back stronger and more resilient health systems to make progress toward UHC. COVID-19 has demonstrated the fact that the health systems of many countries are not fully prepared to protect the health of their populations and reaffirmed the fact that a strong and resilient health system based on primary healthcare is the basis for effective response to the crises and a reliable platform for advances in health safety and UHC. In this chapter, we will discuss the consequences of the COVID-19 pandemic on achieving SDG 3 targets—with a special focus on SDG 3.4 (NCDs) and SDG 3.8 (UHC).
Keywords: COVID-19, Pandemics, Sustainable development goals, Global health, Universal healthcare, Primary healthcare, Health equity, Noncommunicable diseases
Key messages.
-
•
The emergence of the COVID-19 crisis has posed critical challenges to all aspects of development. The pandemic damaged many global public health achievements and impeded the pathways toward Sustainable Development Goals in almost all settings.
-
•
Although the Noncommunicable diseases (NCD) mortality rate reduced during the last decade, the rapid spread of COVID-19 has led to widespread healthcare disruptions and long-term consequences for patients with NCD.
-
•
Universal health coverage (UHC) will be able to strengthen the health system with enough resilience to strike a meaningful and efficient balance between essential healthcare services and additional requirements for crisis management.
-
•
COVID-19 highlights the importance of meaningful intersectoral collaboration and a surveillance and response system in preparing for likely health emergencies of the future.
-
•
The fragility and unpreparedness of the health systems in many countries during COVID-19 demonstrated UHC’s fundamental role in achieving sustainable health development in all societies.
Alt-text: Unlabelled Box
1. Introduction
Launched by the United Nations (UN) in 2015 and endorsed by 194 Member States, Sustainable Development Goals (SDGs) aim to scale up global cooperation to reduce poverty and achieve peace, prosperity, and health for all.1, 2, 3 SDGs include 17 goals and 169 targets, of which SDG 3—ensuring a healthy life and promoting well-being for all ages—and its 13 targets are specifically focused on health (Box 1 ). Moreover, some other SDGs indirectly address health-related issues or their consequences may affect health (Fig. 1 ).4
Box 1. Targets of the sustainable development goals 3.
| 3.1 By 2030, reduce the global maternal mortality ratio to less than 70 per 100,000 live births. |
| 3.2 By 2030, end preventable deaths of newborns and children under 5 years of age, with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1000 live births and under-5 mortality to at least as low as 25 per 1000 live births. |
| 3.3 By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases. |
| 3.4 By 2030, reduce premature mortality from non-communicable diseases by one-third through prevention and treatment and promote mental health and well-being. |
| 3.5 Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol. |
| 3.6 By 2020, halve the number of global deaths and injuries from road traffic accidents. |
| 3.7 By 2030, ensure universal access to sexual and reproductive health-care services, including family planning, information and education, and the integration of reproductive health into national strategies and programs. |
| 3.8 Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all. |
| 3.9 By 2030, substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water and soil pollution and contamination. |
| 3.A Strengthen the implementation of the WHO Framework Convention on Tobacco Control in all countries, as appropriate. |
| 3.B Support the research and development of vaccines and medicines for the communicable and noncommunicable diseases that primarily affect developing countries, and provide access to affordable essential medicines and vaccines, in accordance with the Doha Declaration on the TRIPS Agreement and Public Health, which affirms the right of developing countries to use to the full the provisions in the Agreement on Trade Related Aspects of Intellectual Property Rights regarding flexibilities to protect public health, and, in particular, provide access to medicines for all. |
| 3.C Substantially increase health financing and the recruitment, development, training and retention of the health workforce in developing countries, especially in least developed countries and small island developing States. |
| 3.D Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks. |
Alt-text: Box 1
Fig. 1.
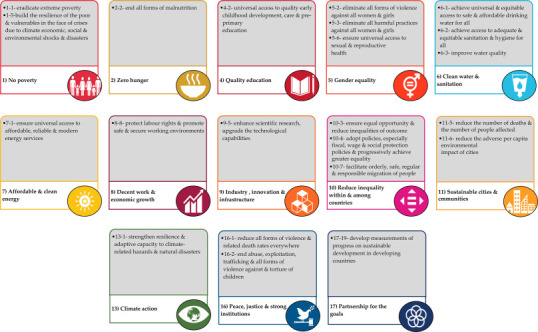
Other sustainable development goals and targets that are indirectly related to health.
(Translated from “Takian A, Raoofi A. Covid-19 pandemic and global sustainable health development. In: Niknam MH, Azizi F, editors. Health and covid-19 crisis in the Islamic Republic of Iran. Tehran, IR Iran: Academy of Medical Sciences of the Islamic Republic of Iran; 2020. p. 62–97. With modification.)
Following the legacy of the millennium development goals (MDGs) and as a result of global focus on SDGs, in particular SDG 3, significant progress in global health has been achieved, i.e., maternal, infants, and the under-5 children mortality rate was declining; healthy life expectancy was increasing in 202 countries; access to safe drinking water and basic sanitation services was increasing; the share of current health expenditure as a percentage of Gross Domestic Product was increasing5; the Global Action Plan for the Prevention and Control of Noncommunicable Diseases (NCDs) was placed on the World Health Organization (WHO) agenda in 2013,6 following which many countries developed national strategies to reduce the burden of NCDs and relatively good results have been achieved; the incidence of many infectious diseases was declining; many emerging and reemerging diseases such as poliomyelitis and malaria were on the edge of eradication, and chronic poverty and hunger were declining.7 Besides, primary healthcare (PHC) and universal health coverage (UHC) were prioritized on the WHO agenda and subsequently on the agenda of many countries, so that 75% of the national health policies of the world were developed with the aim of moving toward UHC.8
Despite many achievements, the acceleration of many countries in achieving SDGs has been less than expected; for instance, food insecurity was on the rise in some countries.9 In this regard, WHO, in collaboration with 11 other UN agencies, has developed a “Global Action Plan for Healthy Lives and Well-being for All” to facilitate global movement toward health-related SDGs. The program aimed to assist countries in implementing national health-related strategies to reach SDG 3, “Ensure healthy lives and promote well-being for all ages.”
2. Global health in the COVID-19 pandemic
In December 2019, at a time when the world was only a third of the way to the sustainable development agenda, the COVID-19 crisis began, rather devastatingly, to shatter many achievements; posed challenges to global health and other social, economic, and developmental aspects; and created the most destabilizing conditions to global health in recent history.1, 10 According to the UN, the global community faced an unprecedented situation in the face of COVID-19, threatening many aspects of the population lives and leading to collapse in several global public health achievements of the past two decades, mostly related to the MDGs and SDGs.10, 11 This raises the question of whether SDGs are appropriate during the crisis and postcrisis eras.12 The COVID-19 pandemic exacerbated poverty, hunger, shortage of clean water and sanitation, and inequitable access to education, which is also threatening the ongoing fragile progress toward sustainable societies.1, 13 The ever-increasing burden of COVID-19 has pushed the health systems of many countries to the brink of collapse,3 particularly where the flow of resources to the basic health services has already been limited.14 The provision of essential healthcare services, including cancer screening; prenatal care; family planning; diagnosis and treatment of infectious diseases other than COVID-19; and prevention, control, and treatment of NCDs, was disrupted or neglected.3 According to the United Nations, during March and April 2020, child vaccination slowed in 70 countries to some degree and, in some cases, was completely suspended.9
Furthermore, safe delivery in health facilities in some African countries, e.g., Burundi, showed a reduction of up to 60% in 2020 compared to 2019.15 Domestic violence against women and children also increased, and millions of unwanted pregnancies and unsafe abortions are expected due to women’s lack of access to family planning services and safe delivery facilities.9, 15 Worse still, access to safe drinking water and basic sanitation has become difficult for billions of people due to COVID-19.3
Disruption in healthcare delivery and reduced access to food and nutrients resulting from the COVID-19 pandemic have posed serious risks to global health and well-being, i.e., increasing maternal, neonatal, and under-5 children mortality rates.15, 16 Further, the pandemic has caused decreased access to or delays in services related to early diagnosis, screening and treatment of NCDs, i.e., cancers and cardiovascular disease, which might have increased the morbidity and mortality of these diseases.17 The same applies to infectious diseases. For instance, a 25% worldwide reduction in tuberculosis (TB) diagnosis within 3 months in 2020 may increase TB mortality rate by 13%. Similarly, 6 months’ interruption in antiretroviral therapy for people living with HIV in sub-Saharan Africa in 2020 could lead to an additional 500,000 deaths from the disease.15
Many adverse consequences of COVID-19 result from years of limited investment in PHC and the provision of essential healthcare services, particularly in low- and middle-income countries (LMICs).14 Such disruption will undermine decades of efforts to promote global health, the negative outcomes on population health may last for decades.3 Nonetheless, many long-term negative impacts of COVID-19 on global health remain unclear.10 These are testaments to the difficulty of achieving SDGs, especially SDG 3 in this difficult situation.3, 18 Under SDG 3, global leaders and the member states committed to nine targets and four tools. The main aim of this chapter is to discuss the intersections of COVID-19 and SDG 3 targets with a focus on two selected targets, including prevention and control of NCDs (SDG 3.4) and UHC (SDG 3.8).
3. COVID-19 and noncommunicable diseases
NCDs cover a range of long-term diseases resulting from biological, environmental, and behavioral risk factors. Tobacco use, air pollution, insufficient physical activity, unhealthy diet, overweight/obesity, and harmful alcohol use are the main risk factors of the five major NCDs, including cardiovascular diseases, cancers, diabetes, chronic respiratory diseases, and mental health disorders—all of which are preventable.19 NCDs account for more than 70% of the world’s causes of death each year (41 million out of 55 million in 2019), most of which are premature and occur before the age of 70.20, 21
NCDs are major threats to achieving SDGs. These are neglected causes of poverty and obstacles to the economic development of countries.21 The rapid rise of NCDs prevents poverty reduction (SDG 3.1), especially in low-income countries, associated with rising out-of-pocket (OOP) payments for health. Vulnerable people get involved with NCDs sooner than people of higher social status and die faster. This is due to the inconvenient truth that besides being more exposed to the risk factors, their access to health services is also more limited. The high cost of long-term treatment for NCDs, combined with the low income, plunges millions into poverty each year, which hinders countries’ pathway toward sustainable development.22
In 2015 the UN General Assembly recognized NCDs as a major challenge to sustainable development and adopted SDG 3.4 to reduce premature mortality due to NCDs by one-third through prevention, treatment, and promoting mental health and well-being by 2030. Subsequently, WHO fostered its efforts to encourage member states to invest more in NCDs through enhancing their political support and technical capacity to reduce the burden of NCDs.23, 24 So-called best-buys, WHO introduced a list of evidence-based and cost-effective healthcare interventions, so the member states could choose them to deal with NCDs.24, 25 As a result of global efforts, steady progress was observed in NCD mortality rate before the COVID-19 pandemic.21, 26 The age-standardized NCD mortality rate dropped from 613.3 in 100,000 population in 2000 to 478.8 in 100,000 population in 2019 (Fig. 2 ). The UN SDG report 2021 has indicated that if the rate of decline has remained stable, Australia, New Zealand, Europe, and North America were on track to meet the SDG 3.4 target of a one-third reduction in premature NCD-related deaths.
Fig. 2.

Age-standardized NCD mortality rate (per 100,000 population).
(Reproduced from World Health Organization. The Global Health Observatory. Noncommunicable diseases: mortality. Geneva, Switzerland; 2021 [cited 2021 July 29]. https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/gho-ghe-ncd-mortality-and-morbidity [Accessed 29 July 2021]. Copyright 2021.)
COVID-19 exacerbated the complex challenges that people with NCDs face.26 Due to the chronic nature of their disease, people with NCDs need to receive long-term essential healthcare or rehabilitation services. The rapid spread of COVID-19 has led to widespread healthcare disruptions and long-term consequences for people with NCDs, especially those in need of regular or long-term care.20 The available evidence suggests that people with NCDs are at higher risk for more serious types of COVID-19 and worse outcomes.24 On the other hand, many people who die from COVID-19 are affected by NCDs,24 which might represent a range of direct and indirect interactions between COVID-19 and NCDs. The direct effects are primarily because people with NCDs, if exposed, are more likely to get infected with COVID-19 more seriously with more severe consequences.27 Therefore comorbidities may play an important role in increasing susceptibility to COVID-19, increasing the risk of severe disease progression, and exacerbating the COVID-19 crisis. This might be to the extent that if immediate action is not taken, a significant impact on health, economic, and social and political development would be unavoidable worldwide.27, 28 Indirect effects are due to not utilizing healthcare services by people with NCDs, which are far more difficult to measure than direct effects. This may lead to (a) delay in diagnosing acute conditions of the disease, (b) failure to perform routine screening, (c) prolonged waiting lists for diagnostic and therapeutic measures due to late referral,27 and (d) increased morbidity and mortality in people with NCDs in the long run.26
A WHO rapid assessment based on a global survey of 163 countries during May 2020—the first global peak of the COVID-19 pandemic—showed partial or complete disruption of NCD services in 122 countries. Access to NCD outpatient services was completely restricted in 4% of the countries and partially restricted in 59% of countries, while inpatient services were open only for emergencies in 35% of countries. The survey also demonstrated that countries in the more severe phase of the COVID-19 pandemic had more disruptions in NCD services. Insufficient supplies of medicines, technologies, and diagnostics were the main reason for disrupting services to the people with NCDs in 20% of the countries under investigation.29 The details of the NCD service disruptions are presented in Fig. 3 . Another study reported the cancelation or postponement of 2.3 million cancer surgeries worldwide during the first COVID-19 lockdown.30
Fig. 3.

NCD services disruption during 2020 and 2021.
(Adapted from World Health Organization. Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic. Geneva: World Health Organization; 2021 April 23. License: CC BY-NC-SA 3.0 IGO.)
Worse still, some measures to combat COVID-19 may increase the risk factors for NCDs. For example, trade and movement restrictions within and between countries might reduce access to healthy medicines and foods and increase people’s inclination toward unhealthy diets. It is also possible for people to be less physically active due to movement restrictions. In addition, staying home for long periods and the psychological consequences could increase the likelihood of turning to alcohol and tobacco. An increased prevalence of domestic violence has been reported following staying at home and unemployment. All of these might affect mental health and well-being and increase the overall risk of NCDs.28 Therefore, while implementing the essential measures to mitigate, control, and minimize the serious consequences of COVID-19 is essential, strengthening the health system is also pivotal to maintain and resume the necessary measures for preventing and controlling NCDs and increasing patient access to health services.28 The increasing evidence that demonstrates NCDs are associated with increased risk of death due to COVID-19 multiplies the need for a multidisciplinary approach with a focus on meaningful intersectoral collaboration and a robust surveillance and response system.31, 32 Simultaneously addressing both NCDs and COVID-19 contributes to the formation, maintenance, and promotion of long-term physical, mental, and social health and well-being, in addition to achieving SDG 3.4.28 While the COVID-19 pandemic has caused devastating consequences for human civilization, it has also created a cosmopolitan moment to advocate more comprehensive policies and regulations to address NCDs and their related risk factors as the biggest threat not only to health and well-being but actually to the sustainable development of all societies. Therefore the need for effective and efficient programs to enhance primary and secondary prevention of NCDs as a national priority has become clear, now more than ever.28 A summary of COVID-19 effects on NCD is illustrated in Fig. 4 .
Fig. 4.

COVID-19 impact on noncommunicable diseases.
4. Achieving universal health coverage in the COVID-19 era and after
UHC means that everyone should receive health services without any financial hardship whenever and wherever needed.32 It emphasizes providing accessible, available, acceptable, affordable, and quality healthcare services for all citizens in an equitable manner to ensure no one is left behind.33 The wide range of these services includes health promotion, prevention, treatment, rehabilitation, and palliative care.32 Such comprehensive attention to all aspects of health was first reflected in the concept of PHC.31 Accordingly, in the 2018 Astana Declaration, PHC was recognized as the most effective, efficient, and equitable health promotion and an essential tool for achieving UHC and health-related SDGs.34 UHC will reduce health inequalities and lead to improved health indicators.8, 33 Effective protection of people from OOP payment and financial consequences of healthcare services will reduce the risk of being pushed into poverty. Otherwise, citizens may use their savings, sell their assets, or take out loans to pay for the services, which will ruin their future lives and those of their children.32
In line with SDGs, the WHO 13th General Program of Work (GPW) pursues three targets by 2023: one billion more people benefit from UHC, one billion more people better protected from health emergencies, and one billion more people enjoy better health and well-being.32 Under SDG 3.8, endorsed by the GPW 13, UHC was placed on many countries’ national agendas, leading to major global health achievements. The UHC Index of service coverage rose globally from about 45% in 2000 to 63.84% in 2015 and 65.74% in 2017 (Fig. 5 ).35 Nevertheless, almost half of the world’s population was not still fully covered by essential health services. Over 930 million people worldwide spent more than 10% of their household budget on health, while about 100 million people were driven into extreme poverty every year due to OOP payments for health.8 This burden was more considerable in the LMICs, where a significant proportion of the population suffers from the lack of essential health services, insufficient financial protection, ineffective benefit packages, and a dysfunctional health insurance industry.36 The essential need for UHC became more evident in the face of the COVID-19 pandemic when people with the highest need for appropriate, timely, and quality healthcare services suffered the most, paid extra from their pocket to receive care, and their access to required services declined dramatically, all of which led to slowing down the achievement of the SDGs and GPW 13 triple targets.
Fig. 5.

UHC index of service coverage (SCI) trend.
(Reproduced from World Health Organization. The global health observatory. UHC index of service coverage (SCI). Geneva, Switzerland: World Health Organization; 2021 [updated 2019 September 6; cited 2021 July 30]. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/uhc-index-of-service-coverage [Accessed 30 July 2021]. Copyright 2021.)
While many countries struggled to achieve UHC, the COVID-19 crisis continued to put tremendous pressure on health systems worldwide.37 Access to essential healthcare services is the pillar of the health systems in the fight against COVID-19.18 To minimize morbidity and mortality, maintaining accessibility, provision, and utilization of essential healthcare services during COVID-19 have been among major concerns for many member states and international organizations.15, 38 COVID-19 pandemic has caused a considerable decline in some major public health achievements of recent decades in a short period.38 Disruption of healthcare services has slowed down people’s healthcare-seeking behavior such as screening, vaccination, and even emergency medical care.1 The ongoing decline and even collapse in essential healthcare services, from health promotion to palliative care, may seriously affect population health outcomes, particularly among the most vulnerable, e.g., women, children, the elderly, refugees, and minorities,38, 39 both in terms of supply and demand sides. People may avoid visiting healthcare facilities on the demand side due to fears of getting infected with COVID-19. Some people might not afford healthcare services because of losing their jobs or reduced income, which has been inevitable following COVID-19 restrictions. On the supply side, the availability of medical resources might have declined because most resources and equipment have been allocated to COVID-19 patients. Worse still, transportations and import of medicines and medical supplies have been disrupted due to borders’ closure, reduced staff, declined production capacity, and political reasons, e.g., sanctions.40 Finally, some mitigation strategies against COVID-19, i.e., quarantine and lockdown, can also hinder access to healthcare services4, 38; hence they may lead to increased morbidity and mortality due to emerging communicable and noncommunicable diseases.1 Indeed, an increasing trend in COVID-19 mortality and morbidity has been observed among people with underlying conditions, e.g., NCDs and immunodeficiency.24
Moreover, rising poverty and unemployment due to COVID-19 have increased OOP for health.26 In both rounds of the WHO survey in 2020 and 2021, about 90% of the respondent countries reported substantial disruptions in access to healthcare services.41 Nonetheless, many countries have developed policies, strategies, plans, and mechanisms to support essential healthcare services and reduce the negative impact of COVID-19.26, 38 A WHO survey revealed that almost 66% of responding countries have defined the set of essential healthcare services to be continued during the pandemic. Approximately 55% of countries have allocated additional budgets to secure the continuity of essential healthcare services.38 A summary of COVID-19 effects on UHC is illustrated in Fig. 6 .
Fig. 6.

COVID-19 impact on three dimensions of universal health coverage.
COVID-19 highlights the importance of UHC and intersectoral collaboration in preparing for health emergencies.26 UHC will strengthen the health system with enough resilience to strike a meaningful and efficient balance between essential healthcare services and fighting against emergencies like COVID-19.15, 38 A resilient health system can respond to crises promptly through on-time detection and prevention while sustaining peace and protecting the economy.42 The pandemic showed that health system resilience is a fundamental and cost-effective feature for overcoming complex health system challenges, as those countries that achieved UHC performed better against COVID-19.42 Indeed, the COVID-19 crisis reindorsed that to achieve sustainable health development, UHC is needed, now more than ever.43
Viruses do not discriminate, meaning that although people of all races, ethnicities, genders, and nationalities are at the risk of being exposed to infection, the risk is not distributed equally among all humans, countries, and territories. Vulnerable population, including people with underlying diseases, the elderly, prisoners, migrants, refugees, and people with lower socioeconomic status, have been disproportionately suffering the most from COVID-19 due to their special health conditions; poor living conditions; and lack of access to high-quality public health services,15, 18, 26 particularly within the LMICs.1 According to the SDG report 2021, 76.4% of deaths from COVID-19 occur in people over 65 years of age, while only 14% of confirmed cases of COVID-19 occur in this age group.26 Furthermore, the crises have exacerbated the previously disturbed living conditions and health of refugees and migrants. A recent UN survey revealed that about 5% of responded refugees and migrants who faced COVID-19 symptoms did not seek healthcare due to insufficient financial resources, fear of deportation, lack of access to healthcare, or depriving the right to receive these services.26 These indicate the vulnerability of these groups to COVID-19 and its consequences and likely future pandemics.
In addition, universal coverage for affordable, safe, and effective COVID-19 vaccines, particularly for the most prioritized population, such as frontline health workers and its diagnostic and therapeutic methods, is crucial to overcoming the pandemic. To fulfill this, WHO has launched “The Access to COVID-19 Tools Accelerator (ACT-Accelerator),” consisting of four pillars, including diagnostics, treatment, vaccines (COVAX facility), and health system strengthening.15, 44 Nevertheless, the COVID-19 vaccine has not been distributed equitably. As of September 1, 2021, a total of 5.44 billion doses of the COVID-19 vaccine have been administered worldwide. Also, 3.15 billion people have received at least one dose of the COVID-19 vaccine, of which 63.5% were in high-income countries and 1.8% in low-income countries. Besides, 2.15 billion people globally were fully vaccinated against COVID-19, of which 53.3% are in high-income countries and only 0.6% in low-income countries (Fig. 7 ).
Fig. 7.

Share of people received COVID-19 vaccine, as of September 1, 2021.
(Adapted from Our world in data. Statistics and research, coronavirus (COVID-19) Vaccinations. Oxford, UK: University of Oxford; 2021. https://ourworldindata.org/covid-vaccinations [Accessed 30 July 2021].)
The COVID-19 crisis has exposed deep disparities in the societies and exacerbated the existing inequalities within and among countries,1 which will endanger achieving UHC in many settings in the longer run.
5. COVID-19 and other SDG 3’s targets
Undoubtedly, the COVID-19 pandemic has also severely affected other SDG 3’s targets, which witnessed significant global improvements before the crisis.45, 46 For instance, before COVID-19, maternal and child mortality rate reduced, global HIV incidence among adults aged 15 to 49 declined, coverage of essential vaccination among children increased, the under-5 mortality rate fell from 76 death per 1000 live births in 2000 to 38 deaths per 1000 live births in 2019, the neonatal mortality rate (death in the first 28 days of life) approximately halved, falling from 30 death per 1000 live births in 2000 to 17 death per 1000 live births in 2019 (Fig. 8 ). COVID-19 and its imposing containment measures in most countries disrupted prenatal care services and supply of and access to reproductive health and family services.47, 48 Moreover, shortages in healthcare workers in most countries, along with a sudden increase in the number of COVID-19 patients, resulted in redeploying maternity staff to COVID-19 designated facilities, which inevitably reduced attention to maternal and child requirements.47
Fig. 8.

The comparison of SDG 3’s targets before and after COVID-19.
(This is an adaptation of an original work by United Nations. The sustainable development goals report 2021. New York, USA: United Nations Publications; 2021.)
Although many countries, particularly the LMICs, suffered the most from the consequences of the recent pandemic, some high-income countries have endeavored to minimize the interruption in providing services for vulnerable groups via restructuring the service delivery system and tracking their health status remotely.47 Nevertheless, 228,000 additional child deaths and nearly 11,000 further maternal deaths were only reported in south Asia in 2020, partially due to the allocation of most healthcare resources to combat the disruptive effects of the COVID-19 pandemic.26 Patients with HIV/AIDS also experienced considerable disruptions in receiving preventive and treatment services, i.e., diagnostic tests and referral, during the crisis.45 Similarly, the COVID-19 pandemic has disrupted finding new tuberculosis cases, as well as their follow-up and timely treatment.49 Substance users and addicted persons are another most vulnerable group whose conditions worsened compared to other vulnerable groups during the COVID-19 pandemic. A growing body of evidence indicates that containment measurements might lead to intensifying drug abuse, making substance users more vulnerable to the risk associated with coronavirus.50 Likewise, ample evidence illustrates many consequences on mental health and psychological damages, e.g., emotional distress, depression, stress, mood swings, irritability, insomnia, posttraumatic stress disorder, and anxiety, as a result of restriction measures, i.e., containment and lockdown uncertainty and unpredictability of the pandemic.51 The recent survey by WHO reports that the unprecedented increase in mental illness and its devastating effects might have led to a significant increase in the global suicide death rate in 2019, due to which many member states decided to include mental health support into their COVID-19 plans in 2021.26
In summary, lack of resilience and unpreparedness in many health systems around the world has disrupted most healthcare services, e.g., promotion, prevention, treatment, and rehabilitation, particularly among the most vulnerable groups, i.e., women, children, people with NCDs, addicts, and people living with HIV/AIDS and tuberculosis46 (Fig. 9 ).
Fig. 9.

The effects of COVID-19 on the targets of SDG 3.
6. Discussion
COVID-19 pandemic is still an unfolding story. Despite ever-growing evidence, the extent of the unknown about COVID-19 is still far more than what is known. The entire sustainable development agenda is at stake; hence timely and appropriate reforms in global governance are necessary to revert the derailed SDGs on track.52
The COVID-19 pandemic has set back global efforts to achieve SDGs. The crisis has reversed most progress made in ending hunger, eradicating poverty, and reducing inequality globally. This has caused the Human Development Index to lag behind for the first time since 1990.15 It also threatens years of progress in improving global health. According to the UN SDG report 2021, evidence from countries that provide reliable and timely statistics shows that the COVID-19 pandemic has severely reduced life expectancy.26 Many women have been denied access to family planning and reproductive health services during the COVID-19, which is predicted to lead to an additional 2.7 million unsafe abortions.53 The UN Children’s Emergency Fund has warned that almost 116 million infants and mothers will receive inadequate services under the COVID-19 pandemic.54 A key informant survey conducted by WHO among the Ministry of Health’s officials from 105 countries in 2020 revealed that even strong health systems could be rapidly affected by the COVID-19 outbreak.38 In the shadow of the numerous catastrophic consequences of COVID-19 for the lives and health of millions worldwide,1 strengthening strategic adaptations is necessary.38
COVID-19 demonstrates the fact that the health systems of many countries are not fully prepared to protect the health of their populations and highlights the importance of preparing for potential similar health crises in the future through strengthening national health systems.55 It also reaffirmed that a strong and resilient health system based on PHC is the basis for an effective response to the crises and a reliable platform for progress toward health safety and UHC.55 In fact, only by achieving UHC would it be possible to efficiently protect societies from the burning risks of potential future crises.15 In such a situation, two basic components, including meaningful intersectoral collaboration as well as robust and accurate surveillance and response system, are crucial in understanding and managing the outbreak impact and adopting better decisions.56 COVID-19 has proven that countries with the most efficient and effective outcomes in this fight have made extensive and precise use of these two basic components. We strongly recommend incorporating these two dimensions into the WHO’s six building blocks along their pathway toward health system strengthening.56
Despite many catastrophes it has caused, the COVID-19 pandemic has also underscored the importance of SDG 3 for global public health, i.e., strong and resilient health systems, emergency preparedness, and a greater urgency to achieve UHC.15 It has also shown that achieving sustainable development requires reforming global commitments and putting health at the heart of the agenda.10, 42 Health is both the result and the stimulus of socioeconomic progress; it is also the indicator of sustainable societies.15 Even in times of recession, more investment in health leads to economic development due to protecting population lives.57 Also, investing in health system functions, sustainable financing, and removing financial barriers to healthcare services accessibility are fundamental in laying the foundations for a better future, maintaining and promoting population health and ensuring a better response to potential future crises.15, 57
The COVID-19 pandemic has also highlighted the fundamental role of UHC as the essential pillar of any health system to lead communities toward sustainable health development (SHD). We endorse the “Kampala Declaration on COVID-19 Vaccine Equity” that emphasizes the need to extend UHC to universal health preparedness (UHP), as well as universal health solidarity.58 The COVID-19 crisis has shown that UHC is not enough without meaningful consideration of both UHP and the causes of causes, namely, Social Determinants of Health. This would not be achieved without a strong surveillance and response system as well as an effective intersectoral collaboration, in line with the whole-of-government and whole-of-society approach.56
Outbreak preparedness and response are among the health commodities that require macro-investments.59 More than ever, the global community needs to unite to invest in public health goods as the basis for achieving UHC and health security. In addition to global unity, national strategic planning and countries’ preparedness to respond to probable future crises are also critical.60 Health system strengthening and sustainable efforts to achieve UHC, which guarantees equitable access to quality health services without financial risk for all people and effectively protects communities from future health crises, should be pushed on the country’s national agenda.15
Although COVID-19 has shaken the move toward SDGs, it highlights the need for change to make them more attainable, even stronger than ever and makes a flip for more decisive and urgent progress toward it. Achieving UHC is crucial for preparing in the fight against any future crisis and move along the pathway toward SHD.1, 12
7. Conclusion
Health is increasingly considered a fundamental human right and the backbone of sustainable societies and economies. Despite a great threat to decades of progress in health promotion, COVID-19 might become an opportunity to demonstrate the determination of nations to provide health services and achieve equitable and sustainable development. Moreover, fundamental reforms in governments’ public policies and prioritizing health have become increasingly important. COVID-19 was a warning to awaken the world to the irreparable and difficult consequences of neglecting health. The COVID-19 crisis, exposing many aspects of global health threats that were overlooked, including poor health systems, lack of social support, and structural inequalities, showed that health as the engine of development must be at the forefront of policy-making. There is no longer any doubt that there is a close link between socioeconomic resilience and public health resilience. In other words, to achieve peace, prosperity, and sustainable development, it is essential that global health be clearly prioritized in all policies. To maintain sustainable social, economic, health, and well-being relations, it is crucial that all sectors of government, development partners, and civil societies show their solidarity and cooperation in combating the COVID-19 pandemic, existing crises such as NCDs and climate change, and any other potential future crises using the two approaches of the whole-of-government and the whole-of-society. Future pandemics are likely to occur, threatening societies and their sustainability. The fragility and unpreparedness of the health systems in many countries during COVID-19 demonstrated the fundamental role of UHP-oriented UHC to achieve SHD in all societies. We are all in this together. Indeed, we need to enhance global solidarity, unity, and social participation for a global mandate to reach UHC, now more than ever.
References
- 1.Min Y., Perucci F. UN/DESA policy brief #81: impact of COVID-19 on SDG progress: a statistical perspective. 2020. https://www.un.org/development/desa/dpad/publication/un-desa-policy-brief-81-impact-of-covid-19-on-sdg-progress-a-statistical-perspective/
- 2.Odey G.O., Alawad A.G.A., Atieno O.S., et al. COVID-19 pandemic: impacts on the achievements of sustainable development goals in Africa. Pan Afr Med J. 2021;38:251. doi: 10.11604/pamj.2021.38.251.27065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Lancet Public Health Will the COVID-19 pandemic threaten the SDGs? Lancet Public Health. 2020;5(9):e460. doi: 10.1016/S2468-2667(20)30189-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takian A., Raoofi A. In: Health and covid-19 crisis in the Islamic Republic of Iran. Niknam M.H., Azizi F., editors. Academy of Medical Sciences of the Islamic Republic of Iran; Tehran, IR Iran: 2020. Covid-19 pandemic and global sustainable health development; pp. 62–97. [Google Scholar]
- 5.World Health Organization Global Health Observatory (GHO) data. International Health Regulations (2005) monitoring framework. 2020. https://www.who.int/gho/ihr/en/
- 6.World Health Organization . World Health Organization; Geneva, Switzerland: 2013. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. [Google Scholar]
- 7.United Nations . United Nations Publications; New York, USA: 2019. The sustainable development goals report 2019. [Google Scholar]
- 8.World Health Organization Universal health coverage. 2021. https://www.who.int/health-topics/universal-health-coverage#tab=tab_3
- 9.United Nations . United Nations Publications; New York, USA: 2020. The sustainable development goals report 2020. [Google Scholar]
- 10.Holst J. The world expects effective global health interventions: can global health deliver? Glob Public Health. 2020;15(9):1396–1403. doi: 10.1080/17441692.2020.1795222. [DOI] [PubMed] [Google Scholar]
- 11.Mejia R., Hotez P., Bottazzi M.E. Global COVID-19 efforts as the platform to achieving the sustainable development goals. Curr Trop Med Rep. 2020:1–5. doi: 10.1007/s40475-020-00209-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Time to revise the Sustainable Development GoalsNature. 2020;583(7816):331–332. doi: 10.1038/d41586-020-02002-3. [DOI] [PubMed] [Google Scholar]
- 13.Heggen K., Sandset T.J., Engebretsen E. COVID-19 and sustainable development goals. Bull World Health Organ. 2020;98(10):646. doi: 10.2471/BLT.20.263533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization Universal health coverage day 2020. 2020. https://www.who.int/campaigns/universal-health-coverage-day-2020
- 15.United Nations Sustainable Development Group Policy brief: COVID-19 and universal health coverage. 2020. https://unsdg.un.org/resources/policy-brief-covid-19-and-universal-health-coverage
- 16.Mousazadeh M., Naghdali Z., Rahimian N., Hashemi M., Paital B., Al-Qodah Z., et al. Environmental and health management of novel coronavirus disease. 2021. Management of environmental health to prevent an outbreak of COVID-19: a review; pp. 235–267. [Google Scholar]
- 17.Mafham M.M., Spata E., Goldacre R., et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396(10248):381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nhamo G., Chikodzi D., Kunene H.P., Mashula N. COVID-19 vaccines and treatments nationalism: challenges for low-income countries and the attainment of the SDGs. Glob Public Health. 2021;16(3):319–339. doi: 10.1080/17441692.2020.1860249. [DOI] [PubMed] [Google Scholar]
- 19.Budreviciute A., Damiati S., Sabir D.K., et al. Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Front Public Health. 2020;8:574111. doi: 10.3389/fpubh.2020.574111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pecout C., Pain E., Chekroun M., et al. Impact of the COVID-19 pandemic on patients affected by non-communicable diseases in Europe and in the USA. Int J Environ Res Public Health. 2021;18(13):6697. doi: 10.3390/ijerph18136697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization The global health observatory. Noncommunicable diseases. 2021. https://www.who.int/data/gho/data/themes/noncommunicable-diseases
- 22.World Health Organization Noncommunicable diseases. 2021. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- 23.Nugent R., Bertram M.Y., Jan S., et al. Investing in non-communicable disease prevention and management to advance the sustainable development goals. Lancet. 2018;391(10134):2029–2035. doi: 10.1016/S0140-6736(18)30667-6. [DOI] [PubMed] [Google Scholar]
- 24.Takian A., Bakhtiari A., Ostovar A. Universal health coverage for strengthening prevention and control of noncommunicable diseases in COVID-19 era. Med J Islam Repub Iran. 2020;34(1):1050–1053. doi: 10.34171/mjiri.34.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bakhtiari A., Takian A., Majdzadeh R., Haghdoost A.A. Assessment and prioritization of the WHO "best buys" and other recommended interventions for the prevention and control of non-communicable diseases in Iran. BMC Public Health. 2020;20(1):333. doi: 10.1186/s12889-020-8446-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.United Nations . United Nations Publications; New York, USA: 2021. The sustainable development goals report 2021. [Google Scholar]
- 27.Nikoloski Z., Alqunaibet A.M., Alfawaz R.A., et al. Covid-19 and non-communicable diseases: evidence from a systematic literature review. BMC Public Health. 2021;21(1):1068. doi: 10.1186/s12889-021-11116-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tin S.T.W., Vivili P., Na'ati E., Bertrand S., Kubuabola I. Insights in public health: COVID-19 special column: the crisis of non-communicable diseases in the Pacific and the coronavirus disease 2019 pandemic. Hawaii J Health Soc Welf. 2020;79(5):147–148. [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization . vol. 2021. World Health Organization; Geneva, Switzerland: 2020. The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a rapid assessment. [Google Scholar]
- 30.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107(11):1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tumusiime P., Karamagi H., Titi-Ofei R., et al. Building health system resilience in the context of primary health care revitalization for attainment of UHC: proceedings from the fifth Health Sector Directors' policy and planning meeting for the WHO African region. BMC Proc. 2020;14(Suppl. 19):16. doi: 10.1186/s12919-020-00203-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization Universal health coverage (UHC) 2021. https://www.who.int/en/news-room/fact-sheets/detail/universal-health-coverage-(uhc)
- 33.Hussain R., Arif S. Universal health coverage and COVID-19: recent developments and implications. J Pharm Policy Pract. 2021;14(1):23. doi: 10.1186/s40545-021-00306-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization Declaration on primary health care. 2018. https://www.who.int/teams/primary-health-care/conference/declaration
- 35.World Health Organization The global health observatory. UHC index of service coverage (SCI) 2021. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/uhc-index-of-service-coverage
- 36.World Health Organization . World Health Organization; 2015. Tracking universal health coverage: first global monitoring report. [Google Scholar]
- 37.Akinleye F.E., Akinbolaji G.R., Olasupo J.O. Towards universal health coverage: lessons learnt from the COVID-19 pandemic in Africa. Pan Afr Med J. 2020;35(Suppl. 2):128. doi: 10.11604/pamj.supp.2020.35.2.24769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization . World Health Organization; Geneva: 2020. Pulse survey on continuity of essential health services during the COVID-19 pandemic. [Google Scholar]
- 39.Takian A., Haghighi H., Raoofi A. In: Environmental and health management of novel coronavirus disease (COVID-19) Dehghani M.H., Karri R.R., Roy S., editors. Elsevier; Philadelphia, USA: 2021. Challenges, opportunities and future perspective associated with COVID-19 pandemic; pp. 443–478. [Google Scholar]
- 40.Takian A., Raoofi A., Kazempour-Ardebili S. COVID-19 battle during the toughest sanctions against Iran. Lancet. 2020;395(10229):1035–1036. doi: 10.1016/S0140-6736(20)30668-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization COVID-19 continues to disrupt essential health services in 90% of countries. 2021. https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries
- 42.Takian A., Aarabi M., Haghighi H. The role of universal health coverage in overcoming the covid-19 pandemic. BMJ Opin. 2020 https://blogs.bmj.com/bmj/2020/04/20/the-role-of-universal-health-coverage-in-overcoming-the-covid-19-pandemic/ [Google Scholar]
- 43.Armocida B., Formenti B., Palestra F., Ussai S., Missoni E. COVID-19: universal health coverage now more than ever. J Glob Health. 2020;10(1):010350. doi: 10.7189/jogh.10.010350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World Health Organization What is the ACT accelerator? 2020. https://www.who.int/initiatives/act-accelerator/about
- 45.Khetrapal S., Bhatia R. Impact of COVID-19 pandemic on health system & sustainable development goal 3. Indian J Med Res. 2020;151(5):395–399. doi: 10.4103/ijmr.IJMR_1920_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Seshaiyer P., McNeely C.L. Challenges and opportunities from COVID-19 for global sustainable development. World Med Health Policy. 2020;12(4):443–453. doi: 10.1002/wmh3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chmielewska B., Barratt I., Townsend R., et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021;9(6):e759–e772. doi: 10.1016/S2214-109X(21)00079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mendez-Dominguez N., Santos-Zaldivar K., Gomez-Carro S., Datta-Banik S., Carrillo G. Maternal mortality during the COVID-19 pandemic in Mexico: a preliminary analysis during the first year. BMC Public Health. 2021;21(1):1297. doi: 10.1186/s12889-021-11325-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.The Global Fund to Fight AIDS TaM . Global Health Campus; Geneva, Switzerland: April 13, 2021. The impact of COVID-19 on HIV, TB and malaria services and systems for health: a snapshot from 502 health facilities across Africa and Asia. [Google Scholar]
- 50.Ornell F., Moura H.F., Scherer J.N., Pechansky F., Kessler F.H.P., von Diemen L. The COVID-19 pandemic and its impact on substance use: implications for prevention and treatment. Psychiatry Res. 2020;289:113096. doi: 10.1016/j.psychres.2020.113096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Knolle F., Ronan L., Murray G.K. The impact of the COVID-19 pandemic on mental health in the general population: a comparison between Germany and the UK. BMC Psychol. 2021;9(1):60. doi: 10.1186/s40359-021-00565-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fernandez-Portillo L.A., Sianes A., Santos-Carrillo F. How will COVID-19 impact on the governance of Global Health in the 2030 agenda framework? The opinion of experts. Healthcare (Basel) 2020;8(4):356. doi: 10.3390/healthcare8040356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wenham C., Smith J., Davies S.E., et al. Women are most affected by pandemics—lessons from past outbreaks. Nature. 2020;583(7815):194–198. doi: 10.1038/d41586-020-02006-z. [DOI] [PubMed] [Google Scholar]
- 54.Millions of pregnant mothers and babies born during COVID-19 pandemic threatened by strained health systems and disruptions in services. UNICEF; New York, USA: May 7, 2020. https://www.unicef.org/afghanistan/press-releases/millions-pregnant-mothers-and-babies-born-during-covid-19-pandemic-threatened [Press release] [Google Scholar]
- 55.Haldane V., De Foo C., Abdalla S.M., et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–980. doi: 10.1038/s41591-021-01381-y. [DOI] [PubMed] [Google Scholar]
- 56.Takian A., Raoofi A. BMJ; 2021. We must redesign the WHO’s building blocks to create more resilient health systems for the future.https://blogs.bmj.com/bmj/2021/04/14/we-must-redesign-the-whos-building-blocks-to-create-more-resilient-health-systems-for-the-future/ [Google Scholar]
- 57.UHC2030 International Health Partnership. Living with COVID-19: time to get our act together on health emergencies and UHC. 2020. https://www.uhc2030.org/fileadmin/uploads/uhc2030/Documents/Key_Issues/Health_emergencies_and_UHC/UHC2030_discussion_paper_on_health_emergencies_and_UHC_-_May_2020.pdf
- 58.World Health Summit Kampala declaration on COVID-19 vaccine equity. 2021. https://d1wjxwc5zmlmv4.cloudfront.net/fileadmin/user_upload/5_Regional_Meetings/2021_Kampala/Kampala_Declaration_on_COVID-19_Vaccine_Equity_June_2021.pdf
- 59.Guterres A. Scale up investment in Universal Health Coverage and in stronger health systems. 2020. https://www.un.org/en/coronavirus/scale-investment-universal-health-coverage-and-stronger-health-systems
- 60.Schwartz J., Yen M.-Y. Toward a collaborative model of pandemic preparedness and response: Taiwan’s changing approach to pandemics. J Microbiol Immunol Infect. 2017;50(2):125–132. doi: 10.1016/j.jmii.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


