Abstract
Attachment patterns and early-life adversities are relevant to understand the role of psychosocial factors in the vulnerability and the development of psychosis. The first aim of the study was to test whether a dimensional attachment instrument, the CAMIR (from French; Cartes: Modèles Individuels de Relation), may differentiate attachment styles by comparing a group of psychotic patients with a non-clinical sample. Also, we hypothesised that attachment dimensions would predict Social Functioning (SF) within the clinical group.
INTRODUCTION
Attachment patterns and early life adversities are relevant to understand the role of psychosocial and environmental factors in the vulnerability and the development of psychosis (1)-(2).
The attachment was conceptualised as the “propensity to make intimate emotional bonds to particular individuals as a basic component of human nature”(3). Attachment theory suggests that early experiences with caregivers become internalised as cognitive-affective representations or internal working models of the self and others; these models serve as templates for future relationships across the life course(4). Some authors propose that this model provides a robust theoretical framework for understanding the impact of distressing or traumatic early personal experiences through a distortion of mental schemes, affective deregulation, and alteration of interpersonal patterns(5). According to Rajkumar’ “attachment-developmental-cognitive” hypothesis of schizophrenia(6), the attachment may also represent a construct capable of bridging developmental, neurobiological, and interpersonal levels of analysis in psychosis(7)-(8).
Most research shows that patients with schizophrenia tend to have an insecure attachment style(1). The associations with symptom dimensions are not clear. Some studies have shown associations between anxious attachment and positive symptoms, as well as avoidant attachment and both positive and negative symptoms(9), while no associations were found with the dismissing style(10). Attachment measures correlate with psychotic phenomena, including paranoia(11) and distress when hearing voices(12). Moreover, attachment measures correlate with attributional biases(13) and mentalizing(14); social, community functioning and interpersonal problems(15); social cognition as a mediator between insecure attachment and clinical and functioning problems8; and to psychoticlike experiences(16). Furthermore, some investigations have likewise suggested that secure adult attachment may be related to how individuals with psychosis engage with mental health services(17)-(18).
Beyond the predominance of insecure attachment patterns in psychotic patients(19), it is commonly admitted that childhood trauma has a significant impact in the development of psychotic experiences, mainly hallucinations and delusions(1)-(20), and in the development of social cognitive abilities, which may represent a mediator between early life adversities and later symptom severity(21). Further, psychological factors are related to insecure attachment and recognised neurobiological underpinnings(22)-(27).
A final important issue regards how attachment theory has generated several tools for assessing adult attachment(28). Different measures evaluate different levels of conscious awareness concerning attachment representations: typically, narrative instruments such as the Adult Attachment Interview(29) facilitate the evaluation of non-conscious aspects of attachment via the external coding of responses. At the same time, self-report questionnaires focused on conscious ideas about attachment and relationships(30). Selfreport instruments are easier and more economical to use but can be over-simplistic, especially about unconscious representations as in the case of fearful attachment(30). The literature agrees that both types of measures are useful, each serving to evaluate different kinds of construct(30).
In the current study, our interest focused on the CAMIR (from French; Cartes Modèles Individuelles de Relation), a self-report instrument designed to tap into the relational strategies of adults(31). The CAMIR’s merit lies in the richness and complexity of the theoretical model underpinning it: a self-and-other model drives personal relationships throughout life and adulthood generated by early experience with caregivers. However, it may be modified by subsequent relational experiences(30). It can be administered regardless of the subject’s family structure, provides continuous measurements of attachment dimensions that evaluate clinical phenomena more thoroughly than categories-based measures, and presents adequate psychometric properties for assessing attachment in clinical and research contexts with adolescents and adults, both in its original or reduced versions(32). Initially, the instrument was developed in France by Blaise Pierrehumbert’ research team(31) and has been translated into several languages (for further information, you can visit the author’ web page: https://www.sites.google.com/site/bpierreh/home). A 32-item abbreviated version has been developed and validated for the Spanish population (CAMIR-R)(32). We used this version in the current report.
This work is, from our knowledge, the first study using the CAMIR-R to assess attachment dimensions in persons with schizophrenia-spectrum disorders. The initial objective was to differentiate attachment styles by comparing a sample of individuals with psychosis with a non-clinical one using the reduced Spanish version (CAMIR-R). First, we hypothesised that CAMIR-R would result in a suitable instrument to assess attachment dimensions in individuals with psychosis and differentiate attachment profiles between both groups, with more insecure attachment in patients. Additionally, we report exploratory analyses relating to attachment, psychotic symptoms, and Social Functioning (SF), hypothesising that symptoms and attachment dimensions would predict SF areas within the clinical group. Finally, we conducted several mediation analyses to verify whether psychotic symptoms mediate the influence of attachment dimensions on different areas of SF. We hypothesised that attachment dimensions are linked to SF in persons with schizophreniaspectrum disorders, regardless of symptom severity.
SUMMARY
Introduction
Attachment patterns and early-life adversities are relevant to understand the role of psychosocial factors in the vulnerability and the development of psychosis. The first aim of the study was to test whether a dimensional attachment instrument, the CAMIR (from French; Cartes: Modèles Individuels de Relation), may differentiate attachment styles by comparing a group of psychotic patients with a non-clinical sample. Also, we hypothesised that attachment dimensions would predict Social Functioning (SF) within the clinical group.
Methods
Seventy-nine persons were assessed by the reduced Spanish version (CAMIR-R). We used Cronbach’ alpha to test reliability. A t-test was performed to assess differences between groups. Multiple linear regressions and Mediation analyses were conducted within the clinical group to explore attachment dimensions as possible predictors of SF.
Results
A more insecure attachment was found in the clinical group (73.8% versus 33.3%). Attachment dimensions differentiated between both samples with large effect sizes. Psychopathology and parental interference predicted general SF (R² = 0.30; p<0.05) as family concern predicted more social isolation (R² = 0.19; p = 0.02) and worse employment status (R² = 0.45; p<0.01). Parental permissiveness and child traumatism inversely predicted educational level (R² = 0.31; p<0.05). Mediation analyses revealed that attachment dimensions were linked to SF regardless of symptoms.
Conclusion
CAMIR-R was reliable to assess attachment in psychosis. Persons with schizophrenia-spectrum disorders show a significant impaired SF and a higher prevalence of insecure attachment. Several attachment dimensions predict specific areas of SF, regardless of symptom severity.
METHODS
Participants and procedure
A total of Seventy-nine adults participated voluntarily in the study, completing the self-administered CAMIR-R questionnaire. The clinical group involved forty-three individuals diagnosed with a psychotic disorder, according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition(33). Participants were treated in public mental health centres from Castellon and Valencia (Spain) during the study period (2017-2019). The inclusion criteria were: 1) diagnosis of schizophrenia, schizoaffective or other psychotic disorder; 2) aged 18-65; 3) clinical stability; 4) medication-stabilised condition (no changes during previous two weeks); 5) no history of drug abuse in the last four weeks; 6) complete assessment measures, and 7) native Spanish language. Twenty-four patients (55.8%) had a diagnosis of schizophrenia; 5 (11.6%) of schizoaffective disorder, and 14 (32.6%) were non-specified psychosis. Fourteen (32.6%) were outpatients; 19 (44.2%) were attended at a day rehabilitation centre, and 10 (23.3%) were inpatients. Ten (23.3%) had spent less than five years since the onset of the disease; 10 (23.3%) between 5 and 10 years and 23 (53.5%) for more than ten years. All patients were taking antipsychotics at the time of the assessment. The non-clinical group involved thirty-six individuals with no history of mental health problems, recruited as a convenience sample (age and gender) in the same geographic region. The study is part of a doctoral thesis approved by the Jaume I University Deontological Committee and complied with the Declaration of Helsinki ethical standards. The study’s aim and conditions were verbal and written described to prospective participants, and all of them provided written informed consent.
Measures
We used the short version of CAMIR31 to assess attachment styles and dimensions. The original version includes 72 items that the participant must distribute on a five-point Likert scale. This distribution is used to calculate 13 attachment factors, indicating different characteristics of attachment representations. In the second stage, the participant must reclassify the items into a Q-sort format (for developing the short version, this stage has not been considered). The Spanish version of the CAMIR has shown adequate levels of validity and reliability(32). A Principal Components Analysis (PCA) was performed to construct the reduced version. Then, 32 items were selected (weights>0.40). Additional PCA showed a seven-factor structure that accounted for 52.97% of the total variance. The final reduced version consists of 32 items rated on a five-point Likert-type scale. The CAMIR-R(32) evaluates these seven factors: 1) Security: Availability and support of the attachment figures, 2) Family concern, 3) Parental interference, 4) Value of parental authority, 5) Parental permissiveness, 6) Self-sufficiency and resentment against parents, and 7) Child traumatism. These factors are related to three attachment styles: secure, preoccupied or anxious, and dismissing or avoidant, then it does not evaluate disorganised (fearful) style because it may involve lapses in monitoring of logical thinking or discourse(28). Internal consistency indexes ranged between 0.60 and 0.85. CAMIR-R dimensions provide a valid and reliable assessment of attachment representations and the family functioning conception(32).
Symptom severity was assessed using the Positive and Negative Syndrome Scale (PANSS)(34)-(35). It is a semi-structured interview comprising 30 items, which measure positive and negative symptoms and general psychopathology. Summing subscale scores can derive a total symptom score, which was used to measure the severity of psychiatric symptoms. The measure has shown to be reliable with Cronbach’ alpha coefficients of 0.73 for the Positive scale, 0.83 for the Negative scale and 0.79 for the General Psychopathology scale(34).
We assessed Social Functioning using the short Spanish version of the Social Functioning Scale (SFS-R)(36). The full version of the Social Functioning Scale (SFS)(37) was designed to assess social functioning essential in schizophrenic patients through a medical interview. The original’ 78 items were reduced to 13 items and then to 15 since two items related to the employment capacity were added. The SFS-R includes five areas: 1) social isolation, 2) interpersonal communication, 3) independence-execution, 4) independence-competence, and 5) employmentoccupation, and allows a total score. The short form had a Cronbach’ alpha of 0.76 and proved to be reliable and valid for use in clinical practice. In the present study, we excluded employment-related items and preferred to use more objective measures (current occupational status).
Data analyses
Statistical analyses were performed using IBM SPSS version 23.0. Differences between the means of the two groups were evaluated through Student’s t-test for two independent samples and Cohen’ d to calculate the effect sizes. We used non-parametrical χ2 to compare nominal variables and Kolmogorov-Smirnov’ z to check whether variables followed a normal distribution.
Given the absence of previous studies using CAMIR-R in samples of individuals with psychosis, we calculated internal consistency indexes (Cronbach’ alpha coefficients) to test the instrument’s adequacy within the clinical sample.
To determinate attachment styles, Lacasa and Muela’ strategy was followed(28): dimension 1 T score 50 in CAMIR-R was considered as suggestive of “secure attachment style”, and T scores<50 as “insecure attachment style”. The insecure style was divided into “preoccupied” (dimensions 2 and 3>dimension 6), or “avoidant” (dimension 6>dimensions 2 and 3). Figure 1 shows the strategy.
Figure 1.
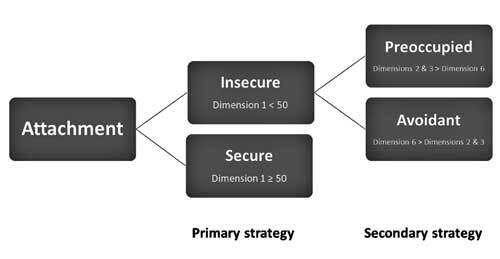
Attachment styles. Primary and secondary strategies
Bivariate correlations were used to observe the relationships among variables. Multiple linear regressions with a stepwise method were performed to check possible predictors of SF areas. The criterion was: the probability of F to enter 0.05; the probability of F to eliminate>0.10. Age and gender were forced to enter in the first step as possible confounding variables. In the second step, PANSS scores were introduced. In the final step, CAMIR-R dimensions were introduced.
Additionally, we conducted a Mediation Analysis using JASP(38) software version 0.11.1 to test total, direct and indirect effects of attachment dimensions to SF through symptom severity. Rosseel(39) describes the mediation analysis in JASP. Attachment dimensions were introduced as predictors. Symptom severity (PANSS total score) was introduced as the mediator variable. SF areas were introduced in each model as the target output (predicted variable). Command options to calculate estimates were turned into standardised estimates, and missing values were handled as Full Information Maximum Likelihood. Testing whether an indirect effect exists, the bootstrap method (1000 replications) was applied. The confidence intervals were then computed using the bias-corrected percentile method, as suggested by Biesanz et al(40).
RESULTS
Table 1 shows the demographic and clinical characteristics of the participants. The clinical group was drawn mainly up of men, but a gender difference was not significant. No differences in age were found. Differences in all SF areas were found with large effect sizes. All CAMIR-R dimensions follow a normal distribution (except parental interference) within the clinical group.
1. Table 1.
Demographic and clinical characteristics of the sample
| Table 1 | Demographic and clinical characteristics of the sample | |||
| Clinical | Control | t/ χ2 | ||
| Age1 | 36.33 (9.28) | 36.19 (10,79) | 0.06 | |
| Gender2 | Male Female | 33 (76.7) 10 (23.3) | 22 (61.1) 14 (38.9) | 2.26 |
| Education2 | Elementary Middle University | 12 (27.9) 21 (48.8) 10 (23.3) | 5 (13.9) 11 (30.6) 20 (55.6) | 8.79* |
| Marital status2 | Single Partner Separated | 30 (69.8) 11 (25.6) 2 (4.7) | 11 (30.6) 23 (63.9) 2 (5.6) | 12.52** |
| Employment2 | Active/ student Unemployed Unemployed | 10 (23.3) 14 (32.6) 19 (43.2) | 29 (80.6) 5 (13.9) 2 (5.6) | 26.91*** |
| SFS-R Total Social isolation Interpersonal communication Independence-execution Independence-competence | 21.95 (4.64) 3.53 (1.10) 5.63 (2.51) 6.63 (1.98) 6.16 (1.53) | 32.14 (1.46) 6.00 (0.00) 9.64 (1.02) 8.97 (0.17) 7.53 (0.74) | -13.62*** -14.71*** -9.59*** -7.75*** -7.75*** | |
| PANSS Positive1 PANSS Negative PANSS Gen. Psychopathology TOTAL PANSS | 14.02 (5.66) 15.37 (5.50) 29.21 (7.93) 58.37 (16.19) | |||
1 Mean (Standard deviation). 2 N (%). SFS-R: Social Functioning Scale Reduced. PANSS: Positive and Negative Syndrome Scale. * p<0.05; ** p<0.01; *** p<0.001.
CAMIR-R’ internal consistency indexes
Cronbach’ alpha coefficients were calculated to test the adequacy of CAMIR-R. The results indicated that the instru- ment is reliable for use in patients with psychosis: Secure attachment (ɑ = 0.90); Family concern ( ɑ = 0.76); Parental interference (ɑ = 0.78); Parental permissiveness ( ɑ = 0.63); Self-sufficiency (ɑ = 0.64) and Childhood trauma (ɑ = 0.81). The value of parental authority was not adequate (ɑ = 0.45), so it was not used in the analyses. Alpha coefficients from 0.63 to 0.90 were considered appropriate for scales of less than eight items.
Differences in attachment styles and dimensions
(Table 2) shows the comparisons between groups. The clinical group obtained a higher mean on insecure attachment with a more avoidant than preoccupied style. Student’s t-test indicated significant differences between groups in all the CAMIR-R dimensions, except parental permissiveness, with moderate to large effect sizes (Cohen’s d).
2. Table 2.
Comparison between groups in attachment styles and dimensions
| Table 2a. Comparison in attachment styles | ||||
| Attachment style | Clinical1 | Control | ||
| Secure attachment Insecure attachment | Preoccupied Avoidant | 11 (26.2%) 31 (73.8%) 13 (31.0%) 18 (42.9%) | 24 (66.7%) 12 (33.3%) 2 (5.6%) 10 (27.8%) | |
| Table 2b. Differences in CAMIR-R' attachment dimensions | ||||
| Dimensions | Clinical Mean (SD) | Control Mean (SD) | t | Cohen d |
| Secure Family concern Interference Permissiveness | 41.12 (15.24) 49.38 (12.11) 56.11 (13.18) 61.97 (15.18) | 52.11 (5.86) 37.20 (10.49) 46.65 (9.88) 46.65 (9.88) | -4.32** 4.71** 3.62* 1.73 | 0.95 1.08 0.81 0.39 |
| Self-sufficiency | 55.29 (10.91) | 48.64 (7.83) | 7.30** | 0.70 |
| Child traumatism | 67.17 (15.80) | 47.87 (6.14) | 7.30** | 1.61 |
1 One subject lost by the system * p<0,01; ** p<0,001
Bivariate correlations
No correlation between CAMIR-R dimensions and PANSS scales were found within the clinical group, except for self- sufficiency to general psychopathology subscale (r = 0.25; p 0.05). Gender (male) correlated with the PANSS negative (r = 0.29; p<0.05) and PANSS general psychopathology ( r = 0.30; p<0.05). Years of evolution since the onset of the disease correlated with the employment status ( r = 0.72; p<0.001), family concern ( r = 0.46; p<0.01) and self- sufficiency (r = 0.39; p<0.01).
Table 3 shows the bivariate correlations between CAMIR-R and SFS-R (n = 79).
3. Table 3.
Bivariate correlations between CAMIR-R1 and SFS-R2 (n = 79)
| Table 3 | Bivariate correlations between CAMIR-R1 and SFS-R2 (n = 79) | |||||
| Secure | Concern | Interfer. | Permiss. | Self-suf. | Trauma | |
| SFS-R Total | 0.36*** | -0.47*** | -0.22* | -0.20* | -0.27** | -0.48*** |
| Social isolation | 0.34** | -0.53*** | -0.32** | -0.20* | -0.27** | -0.53*** |
| Communication | 0.33** | -0.42*** | -0.18 | -0.10 | -0.27** | -0.44*** |
| Independence-exec. | 0.22* | -0.29** | -0.13 | -0.15 | -0.21* | -0.32** |
| Independence-exec. | 0.25* | -0.27** | -0.14 | -0.26* | -0.06 | -0.27** |
CAMIR-R: Secure attachment; Family concern; Parental interference; Parental permissiveness; Self-sufficiency; Child traumatism. 2 SFS-R: Social functioning (SF Total score); Social isolation; Interpersonal communication; Independence-execution; Independence-competence. *p<0.05; ** p<0.01; ***p<0.001 (2-tailed).
Table 4 shows the correlation matrix (n = 43).
4. Table 4.
Correlation Matrix (N = 43)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
| 1 General SF | — | |||||||||||||||||
| 2 Isolation | 0,79*** | — | ||||||||||||||||
| 3 Communic | 0,71*** | 0,71* | — | |||||||||||||||
| 4 Indep-exec | 0,46** | 0,07 | -0,19 | — | ||||||||||||||
| 5 Indep-comp | 0,71*** | 0,42* | 0,26* | 0,34** | — | |||||||||||||
| 6 Education | 0,01 | 0,06 | -0,05 | -0,01 | 0,09 | — | ||||||||||||
| 7 Employment | -0,27* | -0,29* | -0,10 | -0,18 | -0,22 | -0,27* | — | |||||||||||
| 8 Years onset | -0,16 | -0,13 | -0,06 | -0,10 | 0,17 | 0,06 | 0,72*** | — | ||||||||||
| 9 PANSS P | -0,37** | -0,24 | -0,29* | -0,19 | -0,24 | 0,21 | 0,15 | -0,00 | — | |||||||||
| 10 PANSS N | -0,39** | -0,19 | -0,27* | -0,09 | -0,49*** | -0,12 | 0,09 | 0,20 | 0,25 | — | ||||||||
| 11 PANSS G | -0,46** | -0,19 | -0,22 | -0,33* | -0,47*** | -0,02 | 0,14 | 0,07 | 0,69*** | 0,55*** | — | |||||||
| 12 PANSS T | -0,51*** | -0,26 | -0,31* | -0,27* | -0,51*** | 0,02 | 0,17 | 0,12 | 0,79*** | 0,71*** | 0,93*** | — | ||||||
| 13 Secure | 0,00 | 0,03 | 0,03 | -0,06 | 0,08 | 0,08 | -0,04 | -0,04 | 0,09 | 0,01 | 0,04 | 0,09 | — | |||||
| 14 Concern | -0,18 | -0,34 | -0,14 | 0,03 | -0,10 | -0,19 | 0,58*** | 0,51*** | 0,13 | 0,17 | 0,14 | 0,19 | 0,18 | — | ||||
| 15 Interference | 0,21 | 0,00 | 0,21 | 0,20 | 0,05 | -0,15 | 0,29* | 0,19 | -0,01 | 0,03 | 0,12 | 0,06 | -0,04 | 0,40** | — | |||
| 16 Permissiveness | -0,08 | -0,09 | 0,08 | -0,06 | -0,22 | -0,43** | 0,06 | 0,17 | 0,04 | -0,14 | 0,19 | 0,07 | 0,17 | -0,03 | 0,08 | — | ||
| 17 Self-sufficiency | -0,06 | -0,03 | -0,13 | -0,04 | 0,10 | -0,13 | 0,21 | 0,30* | 0,16 | 0,10 | 0,27* | 0,22 | -0,34 | 0,33* | 0,35* | 0,35* | — | |
| 18 Traumatism | 0,10 | 0,01 | 0,05 | 0,12 | 0,07 | -0,31* | 0,17 | 0,03 | -0,16 | -0,19 | -0,10 | -0,17 | -0,72*** | 0,17 | 0,35* | 0,02 | 0,45** | — |
p<0,05; ** p<0,01; *** p<0,001
Predictors of social functioning
PANSS general psychopathology and parental interference conformed the best model [F (4, 38) = 4.18; p = 0.007] to predict general SF. Family concern predicted more social isolation [F (3, 39) = 2.95; p<0.05]. Negative symptoms predicted worse interpersonal communication [F (3, 39) = 2.52; p = 0.07] and, added to parental permissiveness, predicted a worse independence-competence [F (4, 38) = 4.86; p = 0.003]. Educational level was inversely predicted by parental permissiveness and child traumatism [F (4, 38) = 4.30; p = 0.006]. Age and family concern inversely predicted the employment status [F (4, 38) = 10.82; p<.0001]. Table 5 summarizes the regression models.
5. Table 5.
Summary of the linear regression models
| Tabla 5 | Summary of the linear regression models | ||||||
| Predicted variable: General social functioning | |||||||
| Model | Predictor | B | β | R² | Change in R² | p-value | |
| 3 | Psychopathology | -0,31 | -0,53 | 0,23 | 0,23 | 0,001 | |
| Parental interference | 0,10 | 0,28 | 0,30 | 0,08 | 0,050 | ||
| redicted variable: Social isolation | |||||||
| Model | Predictor | B | β | R² | Change in R² | p-value | |
| 2 | Family concern | -0,04 | -0,40 | 0,19 | 0,14 | 00,015 | |
| Predicted variable: Interpersonal communication | |||||||
| Model | Predictor | B | β | R² | Change in R² | p-value | |
| 2 | PANSS negative | -0,17 | -0,36 | 0,16 | 0,12 | 0,023 | |
| Predicted variable: Independence-competence | |||||||
| Model | Predictor | B | β | R² | Change in R² | p-value | |
| 3 | PANSS negative | -0,15 | -0,53 | 0,25 | 0,22 | < 0,001 | |
| Parental permissiveness | -0,13 | -0,32 | 0,34 | 0,09 | 0,027 | ||
| Predicted variable: Educational level | |||||||
| Model | Predictor | B | β | R² | Change in R² | p-value | |
| 3 | Parental permissiveness | -0,02 | -0,42 | 0,22 | 0,17 | 0,004 | |
| Child traumatism | -0,01 | -0,31 | 0,31 | 0,09 | 0,029 | ||
| Predicted variable: Employment status | |||||||
| Model | Predictor | B | β | R² | Change in R² | p-value | |
| 3 | Age | 0,04 | 0,40 | 0,31 | 0,31 | 0,003 | |
| Family concern | 0,03 | 0,41 | 0,45 | 0,15 | 0,002 | ||
B: non-standardised coefficients, β: standardised coefficients, All models included contributions of gender and age,
Mediation analyses
(Table 6) shows the bootstrapping analyses of direct, indirect, and total e ects from attachment dimensions to SF via symptom severity. Family concern and parental interference were significantly linked to general SF. After testing whether indirect effects exist, total effects remained significant. Figure 2 shows the model with paths from attachment dimensions to general SF via symptom severity as mediator. The model explained 38% of the variance in general SF.
6. Table 6.
General social functioning. Mediation Analysis
| Table 6a. Direct effects | |||||||
| 95% CI | |||||||
| Est | SE | z | p | Low | Up | ||
| Secure attachment Family concern Interference Permissiveness Self-sufficiency | → SF → SF → SF → SF → SF | 0.16 -0.28* 0.33* -0.11 0.10 | 0.14 0.15 0.14 0.13 0.15 | 1.14 -1.92 2.39 -0.84 0.66 | 0.25 0.05 0.02 0.40 0.51 | -0.18 -0.60 -0.01 -0.40 -0.24 | 0.63 0.15 0.69 0.13 0.50 |
| Table 6b. Indirect effects | ||||||||
| 95% CI | ||||||||
| Est | SE | z | p | Low | Up | |||
| Secure attachment Family concern Interference Permissiveness Self-sufficiency | → PANSS → PANSS → PANSS → PANSS → PANSS | → SF → SF → SF → SF → SF | -0.06 -0.06 0.04 -0.03 -0.11 | 0.09 0.09 0.09 0.08 0.09 | -0.70 -0.69 0.41 -0.39 -1.17 | 0.49 0.49 0.68 0.70 0.24 | -0.22 -0.34 -0.13 -0.20 -0.35 | 0.16 0.12 0.25 0.14 0.12 |
| Table 6c. Total effects | |||||||
| 95% CI | |||||||
| Est | SE | z | p | Low | Up | ||
| Secure attachment Family concern Interference Permissiveness Self-sufficiency | → SF → SF → SF → SF → SF | 0.10 -0.34* 0.37* -0.14 -0.01 | 0.17 0.17 0.16 0.15 0.17 | 0.61 -2.00 2.25 -0.92 -0.06 | 0.54 0.05 0.03 0.36 0.95 | -0.24 -0.67 -0.06 -0.44 -0.38 | 0.71 0.13 0.78 0.13 0.46 |
Delta method standard errors, bias-corrected percentile bootstrap confidence intervals. PANSS: PANSS Total score (symptom severity). SF: General social functioning. Est: Estimates (standardised coefficients). SE: Standard error. CI: Confidence interval. Bold characters mean significant effects. * p<0.05.
Figure 2.
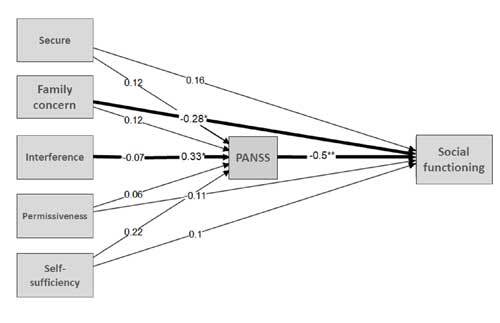
Model with paths from attachmentdimensions to General Social Functioning(SF) via symptom severity as mediator
Mediation analyses for each specific SF area showed that family concern was linked to social isolation and, after testing whether indirect effects exist, total effects remained significant ( β = -0.46; p<0.01). Parental interference was linked to interpersonal communication ( β = 0.34; p<0.05). Secure attachment and parental permissiveness linked to independence-competence, but their effects were mediated by symptom severity. Nevertheless, total effects for parental permissiveness remained close to significant levels (β = -0.28; p = 0.06). Parental permissiveness was linked to educational level (β = -0.47; p<0.001), and family concern was strong- ly linked to employment status, regardless of symptoms ( β = 0.61; p<0.001).
DISCUSSION
The instrument we focused on to assess attachment patterns (CAMIR-R) obtained good internal consistency coefficients and is considered reliable to use in samples of persons with schizophrenia-spectrum disorders. As expected, attachment differentiates between people with psychosis and healthy population, with an insecure attachment style in people with psychosis. However, we do not find specific relations between psychotic dimensions and attachment styles. Moreover, attachment dimensions predict several SF areas and do it regardless of psychotic symptoms. Differences between groups in all SF areas were found with large effect sizes, indicating relevant impairments in SF in persons with psychosis. As well, gender (male) predicts symptom severity.
The results show an insecure attachment style in the clinical group with a higher percentage of avoidant style, according to previous reviews(7)-(8)-(19). A recent review highlight evidence of associations between insecure attachment styles and the overall severity of psychotic symptoms41. Negative symptoms of schizophrenia often present as “avoidant” types of behaviour and result in a lack of meaningful interpersonal relationships(29). Moreover, higher scores in child traumatism differentiate people with psychosis from the healthy population, according to the high rates of attachment disrupting events that individuals with psychosis tend to experience(2)-(20). Exposure to traumatic life experiences can significantly impact the pathogenesis of psychotic experiences as a precipitating or exacerbating factor and can lead to psychosis through many pathways that intersect with other genetic or environmental risk factors(42). Having suffered traumatic experiences is related to the development of psychosis but not necessary to symptom severity(43). When we consider the complete sample, secure attachment positively correlates to all SF areas. Family concern (preoccupied attachment), self-sufficiency (avoidant attachment) and child traumatism relate to worse SF. How attachment style differences are expressed in real-time as individuals navigate their real-life settings has remained an area mostly untapped by research in the field(44). Our results are consistent with recent findings demonstrating how predictions derived from attachment theory play a role in the natural flow of real-life44. Previous works demonstrate a significant positive association between preoccupied attachment and symptom severity(45)-(46). Contrary to this previous literature, the preoccupied attachment does not correlate with positive or negative symptoms, but self-sufficiency (representing avoidant style) correlates to general psychopathology. As cited above, symptoms of schizophrenia often present as “avoidant” types of behaviour(29).
General psychopathology predicts worse general SF, while parental interference predicts better outcomes in it. According to Balluerka et al.(32), this dimension refers to the ambivalence with the attachment figures and is related to the preoccupied attachment style. Although people with a preoccupied attachment style may have maladaptive interpersonal patterns, their continued engagement in social relationships may act as a buffer against symptoms becoming clinically significant(47) and, due to the characteristics of the sample (most long-term stable patients), we might suppose that family relationships would be able to provide enough social support. Findings also demonstrate that persons who experienced preoccupied attachment tend to have higher levels of social isolation(8). The family concern is associated with preoccupied attachment and is characterised by the perception of intense separation anxiety of loved ones and an excessive current concern for attachment figures. The person avoids moving away from them by hyperactivating his/her attachment system; this scheme aims to maintain proximity and ensure the accessibility of their attachment figures(28).
Moreover, family concern predicts worse employment status and is related to the years since the onset of the disease, negatively impacting the employment situation. Thus, separation anxiety hinders personal autonomy. However, other studies find that most individuals with an avoidant attachment pattern also lack flexibility in relationships and are very isolated(48). We find that negative symptoms predict worse interpersonal communication and lower levels of independence-competence in daily life, according to the previous studies(29). Parental permissiveness is also related to less independence-competence and is the best predictor of a worse educational level. This dimension refers to the memories of having suffered from a lack of limits and insufficient parental guidance in childhood. This parental representation is typical of an insecure style(28). Persons who remember having adequate limits during childhood achieved a better educational level.
Beyond the findings discussed above, the direction in which attachment dimensions influence SF is an important question to clarify. Some works have investigated whether insecure attachment and cognitive biases serve as mediators between traumatic life events and psychotic-like experiences in non-clinical samples(16) and others, in line with the theory of an affective pathway to psychosis after exposure to childhood trauma, suggest multiple paths between trauma and psychosis using a network and pathway analyses(49). Nevertheless, on that point is not enough research about the direct influence of attachment on SF. In the current study, we conducted mediation analyses to explore pathways from attachment dimensions to SF via symptom severity as a mediator. According to our hypothesis, the analyses confirm that several attachment dimensions are linked to SF, regardless of symptoms. The overall model explains 38% of the variance in general SF. The detailed models for specific SF areas demonstrate how the family concern is linked to social isolation and employment status, regardless of symptoms. As well, parental interference is linked to interpersonal communication and parental permissiveness to the educational level. Despite its potential role as a predictor of SF, attachment only accounts for a limited part of real-life functioning, and thus, more research is needed to clarify this issue. Previous findings indicate that the interplay between neurocognition, cognitive biases, self-disturbances and insecure attachment may be of outstanding importance in the onset of psychotic experiences(43)-(50) and social functioning in persons with schizophrenia-spectrum disorders(51).
Limitations and future research
Our study presents some limitations. First, the small sample size does not allow us to generalise the results easily. Likewise, a significant portion of clinical subjects was long-term patients treated in psychosocial rehabilitation services, and younger patients or those with early psychosis episodes would be underrepresented in the sample. Another limitation is the cross-sectional design that hinders the determination of causal relationships since it is impossible to know whether the attachment experiences that patients remember preceded the disease or, on the contrary, the disease modified the attachment-related cognitions and memories. Nevertheless, previous studies have demonstrated that retrospective self-reports can be used to assess attachment disrupting events reliably(43). Finally, no measure of adherence to treatment or specific data about non-pharmacological interventions were available, which is another limitation.
Future research should address how attachment relates to the development of psychosis and the interaction among attachment dimensions, basic and social cognitive domains or other environmental risk and protective factors. Attachment patterns account for a limited part of real-life functioning, and therefore, there is a need to investigate them more ecologically, using better measures, longitudinal designs, more appropriate samples and testing additional moderators to improve these limitations.
Main findings
Social functioning is highly impaired in persons with schizophrenia-spectrum disorders. As far as we know, this is the first study that uses the CAMIR-R to assess attachment styles in people with psychotic disorders. The instrument demonstrated suitability for use in psychotic samples, showing acceptable internal consistency indexes. Moreover, our findings support our hypotheses: according to the literature, persons with psychosis show an insecure attachment pattern with higher scores in all dimensions and a higher prevalence of the avoidant style. Most previous studies focused on the relationships between attachment styles and psychotic symptomatology, but their results remain unclear. Our results suggest that having suffered insecure attachment is related to the vulnerability to develop psychosis, but not necessary to symptom severity.
General psychopathology, negative symptoms and some attachment dimensions predict a worse social functioning. Parental interference may act as a protective factor to keep a better social functioning, but separation anxiety hinders personal autonomy, explaining why patients with higher levels of family concern tend to have more social isolation and worse employment status. Finally, persons with psychosis who remember having adequate limits during childhood tend to be more competent and autonomous in their daily-life activities and achieve a better educational level.
Beyond that, our findings highlight a direct link between attachment and social functioning in schizophrenia-spectrum disorders. The methodology of the study, using mediation analyses, allows concluding that several attachment dimensions influence social functioning, regardless of symptom severity.
Clinical implications
If attachment dimensions predict social functioning in individuals with schizophrenia-spectrum disorders, attachment assessment would be required. Interventions in some patients to strengthen attachment bonds and modify interactional patterns may effectively prevent them from developing psychosis or improving psychosocial skills in real life(6). It could be important for clinicians to identify patients’ attachment styles. According to Strand et al.(45), such knowledge would help professionals better understand the persons’ capacity to handle the distress and address interventions aiming to target each patient’s specific needs.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest relating to this study or this publication.
THANKS
The authors would like to thank Ms Nuria Bort and Dr Silvia Edo for their contribution in recruiting the sample.
References
- 1.Sheinbaum T, Bedoya E, Ros-Morente A, Kwapil TR, Barrantes-Vidal N. Psychiatry Res. Association between attachment prototypes and schizotypy dimensions in two independent non-clinical samples of Spanish and American young adults. . 2013 doi: 10.1016/j.psychres.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 2.Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E, Bendall S. Schizophr Bull. Childhood Trauma Is Associated With Severity of Hallucinations and Delusions in Psychotic Disorders: A Systematic Review and Meta-Analysis. 2018 doi: 10.1093/schbul/sbx161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bowlby J. London: Routledge The role of attachment in personality development. In: Bowlby J, editor. A Secure Base: Parent-Child Attachment and Healthy Human Development. 1988 [Google Scholar]
- 4.Bifulco A, Thomas G. Research, assessment and intervention. London: Taylor and Francis Understanding adult attachment in family relationships: 2012 [Google Scholar]
- 5.Hardy A, Emsley R, Freeman D, Bebbington P, Garety PA, Kuipers EE. Schizophr Bull. et al. Psychological Mechanisms Mediating Effects Between Trauma and Psychotic Symptoms: The Role of Affect Regulation, Intrusive Trauma Memory, Beliefs, and Depression. 2016 doi: 10.1093/schbul/sbv175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajkumar RP. Med Hypotheses. Childhood attachment and schizophrenia: The “attachment-developmental-cognitive” pothesis. 2014 doi: 10.1016/j.mehy.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 7.Gumley AL, Taylor HEF, Schwannauer M, MacBeth A. Measurement, construct validity and outcomes. Acta Psychiatr Scand. . A systematic review of attachment and psychosis: 2014 doi: 10.1111/acps.12172. [DOI] [PubMed] [Google Scholar]
- 8.Korver-Nieberg N, Berry K, Meijer CJ, De Haan L. A systematic review. Psychol Psychother Theory Res Pract. Adult attachment and psychotic phenomenology in clinical and non-clinical samples: 2014 doi: 10.1111/papt.12010. [DOI] [PubMed] [Google Scholar]
- 9.Chatziioannidis S, Andreou C, Agorastos A, Kaprinis S, Malliaris Y, Garyfallos G. Psychiatry Res. et al. The role of attachment anxiety in the relationship between childhood trauma and schizophrenia-spectrum psychosis. . 2019 doi: 10.1016/j.psychres.2019.05.021. [DOI] [PubMed] [Google Scholar]
- 10.Ponizovsky AM, Vitenberg E, Baumgarten-Katz I, Grinshpoon A. Psychol Psychother Theory Res Pract. Attachment styles and affect regulation among outpatients with schizophrenia: Relationships to symptomatology and emotional distress. 2013 doi: 10.1111/j.2044-8341.2011.02054.x. [DOI] [PubMed] [Google Scholar]
- 11.Wickham S, Sitko K, Bentall RP. Psychol Med. Insecure attachment is associated with paranoia but not hallucinations in psychotic patients: The mediating role of negative self-esteem. 2015 doi: 10.1017/S0033291714002633. [DOI] [PubMed] [Google Scholar]
- 12.Berry K, Wearden A, Barrowclough C, Oakland L, Bradley J. Br J Clin Psychol. An investigation of adult attachment and the nature of relationships with voices. 2012 doi: 10.1111/j.2044-8260.2011.02027.x. [DOI] [PubMed] [Google Scholar]
- 13.Donohoe G, Spoletini I, McGlade N, Behan C, Hayden J, Donoghue J. Psychiatry Res. et al. Are relational style and neuropsychological performance predictors of social attributions in chronic schizophrenia? . 2008 doi: 10.1016/j.psychres.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 14.MacBeth A, Gumley A, Schwannauer M, Fisher R. e. Psychol Psychother Theory Res Pract. Attachment states of mind, mentalisation, and their correlates in a first-episode psychosis sample. . 2012 doi: 10.1348/147608310X530246. [DOI] [PubMed] [Google Scholar]
- 15.Berry K, Barrowclough C, Wearden A. Behav Res Ther. Attachment theory: A framework for understanding symptoms and interpersonal relationships in psychosis. 2008 doi: 10.1016/j.brat.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 16.Gaw L, Pionke R, Krek M, Prochwicz K, Kosowska J, Frydecka D. Psychiatry Res. et al. Self-disturbances, cognitive biases and insecure attachment as mechanisms of the relationship between traumatic life events and psychotic-like experiences in non-clinical adults – A path analysis. 2018 doi: 10.1016/j.psychres.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 17.McGonagle G, Bucci S, Varese F, Raphael J, Berry K. J Ment Heal. . Is adult attachment associated with engagement with services? A systematic literature review. 2019 doi: 10.1080/09638237.2019.1608922. [DOI] [PubMed] [Google Scholar]
- 18.White R, Haddock G, Varese F. J Ment Heal . Supporting the intimate relationship needs of service users with psychosis: what are the barriers and facilitators? 2019 doi: 10.1080/09638237.2019.1608928. [DOI] [PubMed] [Google Scholar]
- 19.Carr SC, Hardy A, Fornells-Ambrojo M. A meta-analysis. Clin Psychol Rev. Relationship between attachment style and symptom severity across the psychosis spectrum: . 2018 doi: 10.1016/j.cpr.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Rössler W, Ajdacic-Gross V, Rodgers S, Haker H, Müller M. Schizophr Res. Childhood trauma as a risk factor for the onset of subclinical psychotic experiences: Exploring the mediating effect of stress sensitivity in a cross-sectional epidemiological community study. 2016 doi: 10.1016/j.schres.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 21.Rokita KI, Dauvermann MR, Donohoe G. A systematic review. Eur Psychiatry. Early life experiences and social cognition in major psychiatric disorders: 2018 doi: 10.1016/j.eurpsy.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Debbané M, Salaminios G, Badoud D, Armando M, Solida Tozzi A. Front Hum Neurosci. et al. Attachment, Neurobiology, and Mentalizing along the Psychosis Continuum. 2016 doi: 10.3389/fnhum.2016.00406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pilton M, Bucci S, McManus J, Hayward M, Emsley R, Berry K. Psychiatry Res. Does insecure attachment mediate the relationship between trauma and voice-hearing in psychosis? 2016 doi: 10.1016/j.psychres.2016.10.050. [DOI] [PubMed] [Google Scholar]
- 24.Popovic D, Schmitt A, Kaurani L, Senner F, Papiol S. Front Neurosc. et al. Childhood Trauma in Schizophrenia: Current Findings and Research Perspectives. 2019 doi: 10.3389/fnins.2019.00274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheinbaum T, Bifulco A, Ballespí S, Mitjavila M, Kwapil TR, Barrantes-Vidal N. PLoS One. Interview investigation of insecure attachment styles as mediators between poor childhood care and schizophrenia-spectrum phenomenology. 2015 doi: 10.1371/journal.pone.0135150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aydn O, Balk K, Ta C, Ünal-Aydn P, Taneli F, Esen-Danac A. Nord J Psychiatry. . Assessing the relationship between attachment, parental attitude and plasma oxytocin in schizophrenia patients and their unaffected siblings. 2019 doi: 10.1080/08039488.2018.1554698. [DOI] [PubMed] [Google Scholar]
- 27.Speck LG, Schöner J, Bermpohl F, Heinz A, Gallinat J, Maji T. Soc Cogn Affect Neurosci. et al. Endogenous oxytocin response to film scenes of attachment and loss is pronounced in schizophrenia. . 2019 doi: 10.1093/scan/nsy110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lacasa F, Muela A. CaMir-R. Psicopatol Salud Ment. Guía para la aplicación e interpretación del cuestionario de apego. 2014 [Google Scholar]
- 29.Crowell JA. London: Routledge The adult attachment interview. In: Farnfield S, Holmes P, eds. The Routledge Handbook of Attachment: Assessment. 2014 [Google Scholar]
- 30.Molina P, Casonato M, Sala MN, Testa S. Front Psychol. The Factor Structure of the CA-MIR as Evaluated Using Confirmatory Factor Analysis. 2018 doi: 10.3389/fpsyg.2018.00190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pierrehumbert B, Karmaniola A, Karmaniola A, Meister C, Miljkovitch R. Psychiatr l’Enfant et al. Les modeles de relations: Developpement d’un autoquestionnaire d’attachement pour adultes. 1996 [Google Scholar]
- 32.Balluerka N, Lacasa F, Gorostiaga A, Muela A. Psicothema [Internet] CAMIR-R: Versión Reducida del cuestionario CAMIR. 2011 [PubMed] [Google Scholar]
- 33.American Psychiatric Association APA. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 2014 [Google Scholar]
- 34.Kay SR, Fiszbein A, Opler LA. Schizophr Bull. The positive and negative syndrome scale (PANSS) for schizophrenia. 1987 doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 35.Peralta V, Cuesta MJ. Psychiatry Res. Psychometric properties of the Positive and Negative Syndrome Scale (PANSS) in schizophrenia. 1994 doi: 10.1016/0165-1781(94)90093-0. [DOI] [PubMed] [Google Scholar]
- 36.Alonso J, Olivares JM, Ciudad A, Manresa JM, Casado A, Gilaberte I. Actas Esp Psiquiatr. Desarrollo y validación de la versión corta de la Escala de Funcionamiento Social en esquizofrenia para su uso en la práctica clínica. . 2008 [PubMed] [Google Scholar]
- 37.Torres A, Olivares JM. Actas Esp Psiquiatr. Validation of the Spanish version of the social functioning scale. 2005 [PubMed] [Google Scholar]
- 38.JASP Team. JASP. [accessed 1 March 2020] (Version 0.11.1) . 2019 [Google Scholar]
- 39.Rosseel Y. J Stat Software. lavaan: An R Package for Structural Equation Modeling. 2012 [Google Scholar]
- 40.Biesanz JC, Falk CF, Savalei V. Multivariate Behav Res. Assessing Mediational Models: Testing and Interval Estimation for Indirect Effects. 2010 doi: 10.1080/00273171.2010.498292. [DOI] [PubMed] [Google Scholar]
- 41.Lavin R, Bucci S, Varese F, Berry K. A systematic literature review. Br J Clin Psychol. The relationship between insecure attachment and paranoia in psychosis: 2020 doi: 10.1111/bjc.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gibson LE, Alloy LB, Ellman LM. Clin Psychol Rev. Trauma and the psychosis spectrum: A review of symptom specificity and explanatory mechanisms. 2016 doi: 10.1016/j.cpr.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simpson S, Phillips L, Baksheev G, Garner B, Markulev C, Phassouliotis C. Early Interv Psychiatry. et al. Stability of retrospective self-reports of childhood trauma in first-episode psychosis. 2019 doi: 10.1111/eip.12700. [DOI] [PubMed] [Google Scholar]
- 44.Sheinbaum T, Kwapil TR, Ballesp S, Mitjavila M, Chun CA, Silvia PJ. Front Psychol. et al. Attachment style predicts affect, cognitive appraisals, and social functioning in daily life. 2015 doi: 10.3389/fpsyg.2015.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Strand J, Goulding A, Tidefors I. . Attachment styles and symptoms in individuals with psychosis. Attachment styles and symptoms in individuals with psychosis. 2015 doi: 10.3109/08039488.2014.929740. [DOI] [PubMed] [Google Scholar]
- 46.van Bussel EMM, Nguyen NHM, Wierdsma AI, van Aken BC, Willems IEMG, Mulder CL. Front Psychiatry. Adult Attachment and Personal, Social, and Symptomatic Recovery From Psychosis: Systematic Review and Meta-Analysis. . 2021 doi: 10.3389/fpsyt.2021.641642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schizophr Res. MA, Nitzburg G, DeRosse P, Karlsgodt KH. Schizophr Res. Relationship between executive function, attachment style and psychotic like experiences in typically developing youth. . 2018 doi: 10.1016/j.schres.2018.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DeGangi GA. The Dysregulated Adult: Elsevier Inc Addressing Attachment and Problems of Intimacy: How to Build Healthy Emotional Connections. In: DeGangi GA, ed. . 2012 [Google Scholar]
- 49.Isvoranu AM, van Borkulo CD, Boyette LL, Wigman JTW, Vinkers CH, Vinkers D. Schizophr Bull. et al. A Network Approach to Psychosis: Pathways Between Childhood Trauma and Psychotic Symptoms. 1876 doi: 10.1093/schbul/sbw055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pena-Garijo J, Monfort-Escrig C. A preliminary study. J Psychiatr Res. The centrality of secure attachment within an interacting network of symptoms, cognition, and attachment dimensions in persons with schizophrenia-spectrum disorders: 2021 doi: 10.1016/j.jpsychires.2021.01.002. [DOI] [PubMed] [Google Scholar]
- 51.KielanCebo J, Krek M, Pionke R, Gawda L. J Clin Psychol. The role of insecure attachment and cognitive biases in the social functioning of schizophrenia spectrum patients. 2021 doi: 10.1002/jclp.23072. [DOI] [PubMed] [Google Scholar]


