Significance
Sleep deprivation is detrimental to a child’s health. Access to actigraphy measures enabled us to assess racial/ethnic and income group differences in sleep in a large data set from the Adolescent Brain Cognitive Development study (4,207 children ages 9 to 13). This method relies on the closed algorithm of the commercial Fitbit device. Our analyses revealed that black children and low-income children slept significantly less than children from other groups. These findings indicate that disparities in sleep time among children are driven in part by socioeconomic factors.
Keywords: sleep, adolescent health, disparities
Abstract
Children in the United States sleep less than the recommended amount and sleep deficiencies may be worse among disadvantaged children. Prior studies that compared sleep time in children of different race/ethnic groups mostly relied on questionnaires or were limited to small sample sizes. Our study takes advantage of the Adolescent Brain Cognitive Development study to compare total sleep time using a week of actigraphy data among American children (n = 4,207, 9 to 13 y old) of different racial/ethnic and income groups. We also assessed the effects of neighborhood deprivation, experience of discrimination, parent’s age at child’s birth, body mass index (BMI), and time the child fell asleep on sleep times. Daily total sleep time for the sample was 7.45 h and race/ethnicity, income, sex, age, BMI, were all significant predictors of total sleep time. Black children slept less than White children (∼34 min; Cohen’s d = 0.95), children from lower income families slept less than those from higher incomes (∼16 min; Cohen’s d = 0.44), boys slept less than girls (∼7 min; Cohen’s d = 0.18), and older children slept less than younger ones (∼32 min; Cohen’s d = 0.91); mostly due to later sleep times. Children with higher BMI also had shorter sleep times. Neither area deprivation index, experience of discrimination, or parent’s age at child’s birth significantly contributed to sleep time. Our findings indicate that children in the United States sleep significantly less than the recommended amount for healthy development and identifies significant racial and income disparities. Interventions to improve sleep hygiene in children will help improve health and ameliorate racial disparities in health outcomes.
There is substantial concern that over the past 20 y children have been sleeping less (1). Moreover, studies comparing racial and ethnic sleep differences, although not always consistent, have reported that Black children sleep less than White children (2, 3) and discuss potential contributing socioeconomic factors (1). Indeed, these studies reported that adolescents from lower socioeconomic status families, regardless of race or ethnicity, were more likely to experience short, poor-quality, and more variable sleep (4, 5).
Sleep differences are important because children and adolescents who do not get sufficient sleep have a higher risk of obesity, diabetes, injuries, poor mental health (6), mental health disorders including opioid misuse during adulthood (7), in addition to problems with attention and behavior (8, 9). The effect of sleep insufficiency on attention, learning, and memory may be among the primary causes of children’s failure to attain expected learning objectives and may further be related to behavioral and emotional maladjustment (4), which may interfere with school achievement (10, 11). Sleep deprivation has also been implicated in the racial health disparities observed in adult populations (12, 13).
Several high-quality studies have been published examining sleep differences among children from various racial and ethnic groups and income levels (14), as well as the driving factors behind those differences (15, 16). However, many of these studies were done on relatively small samples of children (17) or relied on the use of sleep questionnaires, which are confounded by recall bias. Here, we take advantage of the large actigraphy data set collected in children from the Adolescent Brain Cognitive Development (ABCD) study (18) to analyze effects of race/ethnicity, household income, sex, and age and their interactions on total sleep time (TST) in a large sample of children (n = 4,207). Mobile actigraphy was collected from children who wore a Fitbit mobile actigraphy device for at least seven nights, which provided us with objective measures of sleep duration on a minute-to-minute basis without the limitation of recall bias from sleep questionnaires and allowed us to assess the time at which children fell asleep. In additional models, we assessed the contribution to TST from neighborhood deprivation (19), experience of discrimination (20), age the parent had the child, and BMI (21), which are factors known contributing to health disparities (22) and brain developmental outcomes (23, 24).
Methods
Data were analyzed from the ABCD study versions 2.0/3.0/4.0 (25). ABCD is a longitudinal study that began tracking 11,880 children ages 9 to 10 in 2016 from 21 research sites in the United States with plans to follow participants for 10 y.
We used data collected at the 2-y follow-up assessment, which included actigraphy data obtained in the period between January 2018 up to March 15, 2020, to exclude data captured during the COVID-19 pandemic period. Of 5,189 subjects, we included participants who had at least seven nights of sleep within a three week period. This resulted in the removal of 982 children (final n = 4,207, ages 9 to 13). We compared the differences between weekday and weekend TST and wake-up times to determine if they differed and to assess whether they varied by race/ethnicity, income, age, or sex. To determine if children were tested during the school year or during vacation, we relied on the month the Fitbit data were collected to differentiate vacation from nonvacation periods and estimated that 24% (991/4,207) of the data were captured while children were on vacation. SI Appendix, Tables S1 and S2 provide the number of children with actigraphy measurements obtained for each month by race/ethnicity and income categories.
Sleep intervals were captured by an intrinsic algorithm embedded in the Fitbit device. Though this algorithm is well-researched and documented to produce quality data (21, 26, 27) it is patented, and the specifics are unavailable. The Fitbit devices used in our study [Charge HR model (28, 29)] recorded motion, heart rate, light, skin temperature, and blood oxygen concentrations. Sensors used to record data include a three-axis accelerometer, which tracks motion patterns, a gyroscope, an altimeter, which tracks altitude changes, a multipath optical heart rate tracker, an electrocardiogram sensor, a skin temperature sensor, red and infrared sensors, and an ambient light sensor.
The Fitbit measures the first minute that the participant was identified as being in-bed (but not necessarily asleep) and the first minute that the participant was identified as being asleep. This eliminates potential confounding between quiet wakefulness and when the child fell asleep. Similarly, the first minute that the participant was identified as being awake and the first minute that the participant was identified as being out of bed are delineated in the data set. For our analysis, we used total time in sleep, which is provided by the ABCD dataset and calculated by the addition of three sleep stages: light + deep + rapid eye movement (REM). To confirm TST is an accurate measurement, we added three measures provided by the Fitbit; total number of minutes (in 30-s increments) identified as being in light sleep stage, total number of minutes (in 30-s increments) identified as being in deep sleep stage, total number of minutes (in 30-s increments) identified as being in REM sleep stage during the child’s nighttime sleep. We also estimated differences in sleep latency between the groups to ensure TST differences between groups were not driven by differences in quiet wakefulness. To assess intrasubject variability of TST measurements and potential differences between groups, we examined the mean variance and SD for within subject sleep duration (21, 26, 27).
The ABCD demographics questionnaire was used to obtain information on age, sex, household income. Household income was categorized into low-income (<$50,000), mid-income ($50,000 to $100,000), and high-income (≥$100,000). The ABCD American Community Survey poststratification weights and family relationships measure questionnaire were used to collect information on race/ethnicity. Participants were grouped into one of five categories; Asian, Black, Hispanic, Other, or White (30). The Other category included children identified as multiracial and/or who belonged to a race/ethnicity that was too small to create a separate category. The ABCD Youth Munich Chronotype Questionnaire was used to assess school start times and the time the child wakes up for school.
To assess the joint effects of race/ethnicity, family income, sex, and age on TST while simultaneously considering potential interactions among the main variables, a multivariable regression model was used. Included in this main model were interactions between race/ethnicity and income. This model allowed us to incorporate multiple predictors and to examine their individual and joint effect on the clinical endpoint, TST. Age, sex, race/ethnicity, and income were the dependent variables, and the significance threshold was P < 0.05. No other potential confounders were considered in this main analysis. Thereafter, we ran five additional models to assess the contribution of Area Deprivation Index (ADI), experience of discrimination, age of parent when child was born, the average time the child fell asleep, and BMI over the 7-d period on TST. Neighborhood Deprivation Index is based on a measure created by the Health Resources & Services Administration (31) and used in ABCD’s Residential History Derived Score form. This measure was recorded on a scale from 0 to 100+, with lower values indicating the least amount of disadvantage and higher values indicating a greater amount. Experience of Discrimination was scored based on four questions from the ABCD Youth Discrimination Measure and age of mother’s birth from ABCD’s Parent Demographics Survey form. The time the child went to bed was measured and reported to the epoch (half-minute). The ABCD Youth Anthropometrics form was used to calculate BMI. Participants who had a BMI < 14 were excluded, which resulted in removal of 59 participants (n = 4,184).
All supplemental models used the same analysis type, and all model specifics are included with their analysis. For supplemental model ABCD data dictionary search terms and assessment tools please see SI Appendix, Table S3.
Results
The final sample consisted of 4,207 children who had at least 7 recorded nighttime sleep events. Most participants (97.5%) had greater than 7 recorded nighttime sleep events, with 50% of the cohort having above 15 nighttime events, mean 15.49 nights (SD = 5.59). Participants ages ranged from 9 to 13 y old, of whom 2,080 were females (49%) and 2,127 males (51%). Of the sample, 111 (2.6%) identified as Asian, 353 as Black (8.4%), 811 (19.2%) as Hispanic, 416 (9.8%) as Other, and 2,516 (60.0%) as White. Of the three household income categories, 875 (21.0%) had an annual income <$50,000, 1,161 (28.0%) had an income between $50,000 and $100,000, and 1,899 (45.0%) had an income >$100,000 whereas 272 (6.0%) responded as do not know or refused to answer.
TST recorded during vacation (M = 453.38, SD = 37.93) differed significantly from TST during nonvacation (M = 446.74, SD = 36.16) (t test = 4.85, P ≤ 0.0001). However, there were no significant differences between racial/ethnic or income groups on the relative proportions of children tested during nonvacation and vacation periods (race/ethnicity P = 0.2883, income P = 0.0777).
The average difference between weeknight and weekend night TST was negligible (Δ mean = 3 min and 41 s more on weekend nights). The difference between weekdays and weekends for fall-asleep time averaged 23 min (SD = 58.8 min) and for wake-up times it averaged 22.6 min (SD = 1 h 40 min). Differences between weekday and weekend TST did not significantly differ between racial and ethnic groups nor between income categories.
The mean SD of the within-subject sleep duration across all nights was 64.87 min (SD = 36.74), considerably lower than reported by other studies (21). Intrasubject variability differed between race/ethnicity groups, Black children and White children differed from other groups by 8 min (P < 0.05) such that White children had greater intrasubject variability than Black children. The association between BMI and intrasubject TST variability was significant (r = 0.104, P < 0.0001), such that higher BMI was associated with greater intrasubject variability consistent with prior results in adults (21). Sleep latency (time between getting into bed and falling asleep) did not differ between racial/ethnic and averaged between 5 to 7 min.
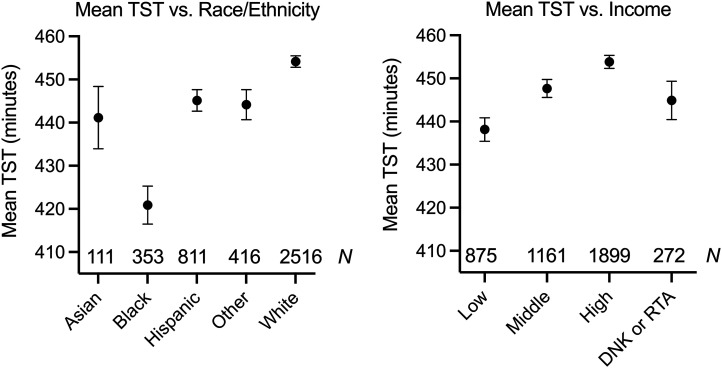
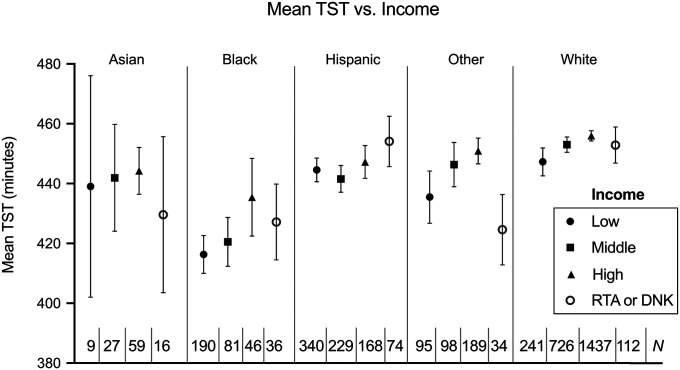
The residual analysis confirmed that the statistical model assumptions were met. Race/Ethnicity was a significant predictor (P < 0.0001) (Table 1) of TST such that Black children slept less than the other racial and ethnic groups, on average 34 min less than White children (Cohen’s d = 0.95) (Fig. 1 and SI Appendix, Table S4). Income was also a significant predictor, such that children from higher income families (>$100.000) had longer TST (P = 0.0001) (Table 1) on average 16 min more than children from families with incomes <$50,000 (Cohen’s d = 0.44) (Fig. 1 and SI Appendix, Table S4). The average TST decreased as age increased (P < 0.0001) (Table 1 and SI Appendix, Table S4), such that children 9 y old slept on average 32 min more than children 13 y old (Cohen’s d = 0.91) (SI Appendix, Table S4). Finally, there was a significant sex effect on TST (P = 0.0001) (Table 1), such that girls had longer TST than boys, on average 7 min (SI Appendix, Table S4). The interaction between race/ethnicity and income was significant (P = 0.0031) (Table 1), such that the effects of low (Cohen’s d = 0.77) and middle (Cohen’s d = 0.92) income were greater for Black than for White children (Fig. 2 and SI Appendix, Tables S4 and S4A). For a detailed description of the average TST for each race/ethnicity, income category, age, sex, and the interaction between race/ethnicity and income categories please see SI Appendix, Table S4.
Table 1.
Main model variables, assessment tools to determine race/ethnicity, household, sex and age and significance of their contribution to TST as well as ABCD data dictionary search terms
| Assessment Tool | Element Name | Variable | P value |
|---|---|---|---|
| ABCD American Community Survey poststratification weights and family relationships measure questionnaire (acspsw03) | race_ethnicity | Race/Ethnicity | < 0.0001 |
| ABCD Parent Demographics Survey (pdem02) | demo_comb_income_v2 | Income | 0.0001 |
| ABCD Parent Demographics Survey (pdem02) | sex | Sex | 0.0001 |
| ABCD Youth Fitbit Daily Sleep Summaries (abcd_fbdss01) | interview_age | Age at interview | < 0.0001 |
| Race/Ethnicity*Income | 0.0031 |
Fig. 1.
Total sleep time duration per night as a function of (Left) race/ethnicity, and (Right) income. Black children and low-Income adolescents showing shorter average TST. Numbers in the lower part of the figure correspond to sample sizes for each subcategory.
Fig. 2.
Mean total sleep time (SD) per night as a function of race/ethnicity, and income. Numbers in the lower part of the figure correspond to sample sizes for each subcategory.
The time the child fell asleep significantly contributed to TST after controlling for race/ethnicity, income, sex, and age (P < 0.0001) (SI Appendix, Tables S1 and S3 and Fig. S1). Overall, Black children and children from low-income homes went to bed later at night than White children and children from high-income households (SI Appendix, Fig. S1). Mediation analyses to assess the relative contribution of these variables to TST showed that race/ethnicity was the main contributor for differences in TST, followed by the time the child fell asleep (SI Appendix, Fig. S2). Furthermore, the relative effect size of the interaction between race/ethnicity and the time the child went to bed contributed the least when compared to other variables in the mediation analysis (SI Appendix, Fig. S2) indicating that both race/ethnicity and the time the child went to bed, while associated with one another, each independently contributed to TST.
BMI was another factor significantly contributing to TST. Children with higher BMI’s had less sleep than those with lower BMI (SI Appendix, Fig. S3). However, there were no significant interactions between BMI and Race/Ethnicity or Income in our model 6 (SI Appendix, Table S3), indicating that that differences in BMI are not significant contributors to the differences in TST between children of different racial or ethnic backgrounds or income.
Additional models to evaluate the effect of ADI, the child’s experience of discrimination and the age the parent had the child to examine for their contributions showed that they did not additionally contribute to TST differences between race/ethnicity and income groups (SI Appendix, Tables S3 and S5). It was noteworthy that while ADI was a significant predictor of TST (P = 0.0136, SI Appendix, Table S5), it showed no significant interaction for TST with income or race/ethnicity; children from lower-income homes tended to show lower TST even when living in areas with low deprivation index (SI Appendix, Fig. S4).
Discussion
In a large cohort of youth living in the United States, we show significant differences in sleep duration as a function of race/ethnicity, income, age, and sex. Black children showed the least amount of sleep when compared to their peers from households of similar income and even greater differences when compared to children from other racial/ethnic groups with higher household incomes. Overall, Black children slept on average 34 min less per night than White children. These differences were larger when introducing household income such that Black children living in low-income households slept on average 41 min less than White children from high-income homes (Cohen’s d = 1.15), 37 min less than White children from midincome homes (Cohen’s d = 0.99), and 31 min less than White children from low-income homes (Cohen’s d = 0.77) (Fig. 2 and SI Appendix, Table S4). Furthermore, income alone was a significant predictor of TST. On average, children from low-income families slept ∼16 min less than those from higher income families (Cohen’s d = 0.44). Additionally, and consistently across race/ethnicity and income categories, boys slept on average 7 min less than girls (Cohen’s d = 0.18), which could reflect biological differences (i.e., puberty onset) and/or psychosocial factors (32). The sex differences, while significant, were small and unlikely to be clinically meaningful.
The reduced sleep in children from low-income families could be attributed to a higher likelihood of living in noisy neighborhoods (33), inadequate sleeping spaces, or poor parental monitoring (34). The ABCD study does not provide detailed description of sleeping arrangements other than the number of people living in the same household, which was not significantly associated with TST (SI Appendix, Fig. S5).
Our results from Model 2 do not show a strong interaction between income and ADI. While the overall interaction effect is not significant, we note that the parameter estimate on income-by-ADI interaction term is significant for low and high-income homes (SI Appendix, Table S6) reflecting our model’s inability to detect the close interdependence of income and ADI.
However, neighborhood deprivation alone does not explain the differences in TST when comparing children from low-income and high-income households, indicating that income inequality has a major impact on children’s TST. Moreover, children from lower-income homes still showed the least amount of TST even when living in areas with low deprivation indices. These findings complement our prior results with ABCD data that showed that after controlling for family income, neighborhood deprivation did not further contribute to differences in brain structure nor cognitive performance (35).
The race/ethnicity and income differences in TST appear to be driven to a certain extent by the differences in the time children went to bed. Black children went to bed on average ∼53 min later in the evening than White children (SI Appendix, Fig. S1). Children from low-income households went to bed about 32 min later than children from high-income households (SI Appendix, Fig. S1). The effects of income on the time children went to bed was similar across race and ethnic groups (SI Appendix, Fig. S6). This is likely to reflect the fact that parents from low-income households might face unique challenges in monitoring and enforcing their children’s routine bedtimes if they are forced to work extra hours (5).
While it has been documented that later school start times allow for kids to sleep longer in the morning to accommodate for the physiological changes that occur while transitioning into and through puberty (36, 37), we conducted an exploratory analysis and did not observe any apparent differences in school start times among racial and ethnic or income categories (SI Appendix, Figs. S7 and S8). Importantly, our cohort of school start times did not appear to drive the racial/ethnic or income differences in TST; for there were no differences in school start times between the group categories.
Even though BMI might not be an ideal measure for excess adiposity in children (38), we observed a negative association between BMI and TST, similar to prior findings in adults (21, 39). In the ABCD dataset children with the higher BMI had lower TST. However, we observed no significant interaction between BMI and race/ethnicity or income categories on the effect of BMI on TST indicating that BMI is not a main contributor to the differences in TST between groups. The negative association between TST and BMI is of public health relevance particularly since childhood obesity has markedly increased in the past three decades. Although the mechanisms underlying the association between TST and BMI are likely to be complex and bidirectional there is significant evidence that inadequate sleep increases the risk of overeating and obesity (40, 41). Thus, promoting sleep hygiene for children might be a beneficial intervention to help prevent adverse effects of childhood obesity.
Restricted sleep time in US children, an effect most accentuated among Black children and those from low-income families, raises concern regarding its potential deleterious effects on brain development and health. Hence, interventions to improve sleep hygiene should be prioritized as a strategy to improve health in general and to help address racial and ethnic health disparities. American children and their families may benefit from specific interventions taken by schools and from the implementation guidelines on sleep hygiene as recommended by the American Association of Pediatrics and the American Association of Sleep Medicine (5). Such interventions should ensure that the most vulnerable populations are not neglected, and that additional support is provided when needed. Considering that income is a strong predictor of TST, interventions that provide economic support to low-income families would for example allow parents to be present at bedtime to monitor sleep behavior in their children. Many additional recommendations have been made on how to improve sleep in marginalized and disadvantaged communities (42, 43) including community-based interventions and public health campaigns (44). Although these interventions (45), which raise awareness about the importance of sleep and related health consequences (46, 47), have mostly focused on adults (48) they are also likely to benefit their children.
Limitations to our study include the fact that White children and those from high-income households were overrepresented in our cohort: specifically, the number of White children made up 60% of the cohort and the remaining 40% was unequally divided among the remaining four racial and ethnic categories. However, 45% were from high-income homes, which reflects the population demographics from the Health Science Centers where participants were recruited for the ABCD study (49). While Fitbit has been shown to provide accurate measures of TST, it still underperforms compared to polysomnography (50–52) and is limited by the closed algorithm of the commercial Fitbit device. Still, recent work suggests Fitbit Charge HR agreement with polysomnography is as high as 90% (51). Also, our study focused only on total sleep time and did not measure potential differences in sleep architecture, which is also relevant to the restorative effects of sleep (53). Finally, the large sample size of ABCD allows for the detection of small significant effects such as the seven-minute differences in TST between boys and girls, but the physiological significance of such a small effect remains unclear.
We recognize that the reasons for observed disparities in total sleep time among Black youth compared to White youth are likely multifactorial and overlap with income. Investigation of additional factors and how they may contribute to such disparities is necessary, as well as why Black youth, on average, fall asleep almost an hour later than White youth.
In summary, here we document significantly shorter sleep times among children from underrepresented groups and among children from low-income families, highlighting the emergence of disparities very early in life that are likely to contribute if not corrected to worse health outcomes in adulthood.
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9 to 10 and follow them over 10 y into early adulthood. The ABCD Study® is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in the analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators.
Supplementary Material
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2120009119/-/DCSupplemental.
Data Availability
Data have been deposited in The National Institute of Mental Health Data Archive (NDA) (https://doi.org/10.15154/1526524) (54).
References
- 1.Keyes K. M., Maslowsky J., Hamilton A., Schulenberg J., The great sleep recession: Changes in sleep duration among US adolescents, 1991-2012. Pediatrics 135, 460–468 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marczyk Organek K. D., et al. , Adolescent sleep disparities: Sex and racial/ethnic differences. Sleep Health 1, 36–39 (2015). [DOI] [PubMed] [Google Scholar]
- 3.Yu X., et al. , Emergence of racial/ethnic and socioeconomic differences in objectively measured sleep-wake patterns in early infancy: Results of the Rise & SHINE study. Sleep (Basel) 44, zsaa193 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El-Sheikh M., Shimizu M., Philbrook L. E., Erath S. A., Buckhalt J. A., Sleep and development in adolescence in the context of socioeconomic disadvantage. J. Adolesc. 83, 1–11 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wheaton A. G., Claussen A. H., Short sleep duration among infants, children, and adolescents aged 4 months-17 years - United States, 2016-2018. MMWR Morb. Mortal. Wkly. Rep. 70, 1315–1321 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owens J., Adolescent Sleep Working Group; Committee on Adolescence, Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics 134, e921–e932 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Groenewald C. B., Law E. F., Rabbitts J. A., Palermo T. M., Associations between adolescent sleep deficiency and prescription opioid misuse in adulthood. Sleep (Basel) 44, 8 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campbell R. L., et al. , Greater adolescent tiredness is related to more emotional arousal during a hyperventilation task: An area under the curve approach. J. Adolesc. 90, 45–52 (2021). [DOI] [PubMed] [Google Scholar]
- 9.Wheaton A. G., Jones S. E., Cooper A. C., Croft J. B., Short sleep duration among middle school and high school students–United States, 2015. MMWR Morb. Mortal. Wkly. Rep. 67, 85–90 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buckhalt J. A., El-Sheikh M., Keller P., Children’s sleep and cognitive functioning: Race and socioeconomic status as moderators of effects. Child Dev. 78, 213–231 (2007). [DOI] [PubMed] [Google Scholar]
- 11.Ursache A., et al. , Sleep, classroom behavior, and achievement among children of color in historically disinvested neighborhoods. Child Dev. 92, 1932–1950 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen X., et al. , Racial/ethnic differences in sleep disturbances: The multi-ethnic study of atherosclerosis (MESA). Sleep (Basel) 38, 877–888 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lucey B. P., et al. , Reduced non-rapid eye movement sleep is associated with tau pathology in early Alzheimer’s disease. Sci. Transl. Med. 11, eaau6550 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guglielmo D., Gazmararian J. A., Chung J., Rogers A. E., Hale L., Racial/ethnic sleep disparities in US school-aged children and adolescents: A review of the literature. Sleep Health 4, 68–80 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheon Y. M., Ip P. S., Yip T., Adolescent profiles of ethnicity/race and socioeconomic status: Implications for sleep and the role of discrimination and ethnic/racial identity. Adv. Child Dev. Behav. 57, 195–233 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hawkins S. S., Takeuchi D. T., Social determinants of inadequate sleep in US children and adolescents. Public Health 138, 119–126 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Sheikh M., et al. , Economic adversity and children’s sleep problems: Multiple indicators and moderation of effects. Health Psychol. 32, 849–859 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Volkow N. D., et al. , The conception of the ABCD study: From substance use to a broad NIH collaboration. Dev. Cogn. Neurosci. 32, 4–7 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tessum C. W., et al. , PM2.5 polluters disproportionately and systemically affect people of color in the United States. Sci. Adv. 7, eabf4491 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alcántara C., et al. , Stress and sleep: Results from the Hispanic community health study/study of Latinos sociocultural Ancillary Study. SSM Popul. Health 3, 713–721 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaiswal S. J., et al. , Association of sleep duration and variability with body mass index: Sleep measurements in a large US population of wearable sensor users. JAMA Intern. Med. 180, 1694–1696 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tuliani T. A., Shenoy M., Parikh M., Jutzy K., Hilliard A., Impact of area deprivation index on coronary stent utilization in a Medicare nationwide cohort. Popul. Health Manag. 20, 329–334 (2017). [DOI] [PubMed] [Google Scholar]
- 23.Vargas T., Damme K. S. F., Mittal V. A., Neighborhood deprivation, prefrontal morphology and neurocognition in late childhood to early adolescence. Neuroimage 220, 117086 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dennis E., Manza P., Volkow N. D., Socioeconomic status, BMI, and brain development in children. Transl. Psychiatry 12, 33 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jernigan T. L., Brown S. A., Dowling G. J., The adolescent brain cognitive development study. J. Res. Adolesc. 28, 154–156 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Larsen S. C., et al. , Consistent sleep onset and maintenance of body weight after weight loss: An analysis of data from the NoHoW trial. PLoS Med. 17, e1003168 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rezaei N., Grandner M. A., Changes in sleep duration, timing, and variability during the COVID-19 pandemic: Large-scale Fitbit data from 6 major US cities. Sleep Health 7, 303–313 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Zambotti M., Goldstone A., Claudatos S., Colrain I. M., Baker F. C., A validation study of Fitbit Charge 2™ compared with polysomnography in adults. Chronobiol. Int. 35, 465–476 (2018). [DOI] [PubMed] [Google Scholar]
- 29.Haghayegh S., Khoshnevis S., Smolensky M. H., Diller K. R., Castriotta R. J., Performance assessment of new-generation Fitbit technology in deriving sleep parameters and stages. Chronobiol. Int. 37, 47–59 (2020). [DOI] [PubMed] [Google Scholar]
- 30.Garavan H., et al. , Recruiting the ABCD sample: Design considerations and procedures. Dev. Cogn. Neurosci. 32, 16–22 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kind A. J., et al. , Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann. Intern. Med. 161, 765–774 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Owens J. A., Weiss M. R., Insufficient sleep in adolescents: Causes and consequences. Minerva Pediatr. 69, 326–336 (2017). [DOI] [PubMed] [Google Scholar]
- 33.Casey J. A., et al. , Race/ethnicity, socioeconomic status, residential segregation, and spatial variation in noise exposure in the contiguous United States. Environ. Health Perspect. 125, 077017 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sheares B. J., et al. , Sleep problems in urban, minority, early-school-aged children more prevalent than previously recognized. Clin. Pediatr. (Phila.) 52, 302–309 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tomasi D., Volkow N. D., Associations of family income with cognition and brain structure in USA children: Prevention implications. Mol. Psychiatry 26, 6619–6629 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carskadon M. A., Acebo C., Jenni O. G., Regulation of adolescent sleep: Implications for behavior. Ann. N. Y. Acad. Sci. 1021, 276–291 (2004). [DOI] [PubMed] [Google Scholar]
- 37.Hagenauer M. H., Perryman J. I., Lee T. M., Carskadon M. A., Adolescent changes in the homeostatic and circadian regulation of sleep. Dev. Neurosci. 31, 276–284 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weaver R. G., Beets M. W., Brazendale K., Hunt E., Disparities by household income and race/ethnicity: The utility of BMI for surveilling excess adiposity in children. Ethn. Health 26, 1180–1195 (2021). [DOI] [PubMed] [Google Scholar]
- 39.Watson N. F., et al. , Sleep duration and body mass index in twins: A gene-environment interaction. Sleep (Basel) 35, 597–603 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rihm J. S., et al. , Sleep deprivation selectively upregulates an amygdala-hypothalamic circuit involved in food reward. J. Neurosci. 39, 888–899 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ogilvie R. P., et al. , Sleep indices and eating behaviours in young adults: Findings from Project EAT. Public Health Nutr. 21, 689–701 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williams N. J., et al. , A community-oriented framework to increase screening and treatment of obstructive sleep apnea among blacks. Sleep Med. 18, 82–87 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams N. J., et al. , Social and behavioral predictors of insufficient sleep among African Americans and Caucasians. Sleep Med. 18, 103–107 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jackson C. L., Determinants of racial/ethnic disparities in disordered sleep and obesity. Sleep Health 3, 401–415 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aird C., et al. , 1189 recruiting, training, and implementing sleep health educators in community-based research to improve sleep health. Sleep (Basel) 43, A454–A455 (2020). [Google Scholar]
- 46.Shaw R., et al. , Beliefs and attitudes toward obstructive sleep apnea evaluation and treatment among blacks. J. Natl. Med. Assoc. 104, 510–519 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Curtis D. S., Fuller-Rowell T. E., El-Sheikh M., Carnethon M. R., Ryff C. D., Habitual sleep as a contributor to racial differences in cardiometabolic risk. Proc. Natl. Acad. Sci. U.S.A. 114, 8889–8894 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ceïde M. E., et al. , Associations of short sleep and shift work status with hypertension among Black and White Americans. Int. J. Hypertens. 2015, 697275 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Feldstein Ewing S. W., et al. , Approaching retention within the ABCD study. Dev. Cogn. Neurosci. 32, 130–137 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haghayegh S., Khoshnevis S., Smolensky M. H., Diller K. R., Castriotta R. J., Accuracy of wristband fitbit models in assessing sleep: Systematic review and meta-analysis. J. Med. Internet Res. 21, e16273 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Zambotti M., et al. , Measures of sleep and cardiac functioning during sleep using a multi-sensory commercially-available wristband in adolescents. Physiol. Behav. 158, 143–149 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Godino J. G., et al. , Performance of a commercial multi-sensor wearable (Fitbit Charge HR) in measuring physical activity and sleep in healthy children. PLoS One 15, e0237719 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Della Monica C., Johnsen S., Atzori G., Groeger J. A., Dijk D. J., Rapid eye movement sleep, sleep continuity and slow wave sleep as predictors of cognition, mood, and subjective sleep quality in healthy men and women, aged 20-84 years. Front. Psychiatry 9, 255 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Giddens N. T., Juneau P., Manza P., Wiers C. E., Volkow N. D., Data from “Disparities in sleep duration among American children: effects of race and ethnicity, income, age, and sex.” The National Institute of Mental Health Data Archive (NDA). 10.15154/1526524. Deposited 21 June 2022. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data have been deposited in The National Institute of Mental Health Data Archive (NDA) (https://doi.org/10.15154/1526524) (54).