Abstract
A rapidly emerging global outbreak of monkeypox virus infection (MPXV) in over 50 non-endemic countries was identified in May 2022. We report the case and images of a patient with MPXV presenting with genital lesions later complicated by superimposed cellulitis in Colorado, USA. MPXV lesions are susceptible to bacterial superinfection, and with the advent of new cases, the early identification of skin lesions and their evolution during MPXV are imperative for treating clinicians. Clinicians should consider MPXV in differential diagnoses of sexually transmitted diseases presenting with genital lesions.
Keywords: bacterial cellulitis, imported viral diseases, monkeypox, Orthopoxvirus, travel medicine
Introduction
The World Health Organization (WHO) confirmed a multinational monkeypox virus (MPXV) outbreak in May 2022. The outbreak started with a cluster of cases in the United Kingdom. 1 As of 6 July 2022, confirmed cases have been reported in more than 50 countries, including the United States. According to the US Centers for Disease Control and Prevention (CDC) data, as of 22 July 2022, 2891 confirmed US cases had been reported. 2 Monkeypox virus is an enveloped double-stranded DNA virus that belongs to the Orthopoxvirus genus of the Poxviridae family, with a primarily zoonotic mode of transmission and is less infectious than smallpox virus among humans. 3
Initial symptoms include fever, headache, asthenia, myalgia, and lymphadenopathy, a distinctive symptom that differentiates monkeypox from smallpox. 4 After 1–5 days, a rash appears on the face and extremities, including palms and soles, with a centrifugal distribution. The oral mucous membranes and genitalia may be affected. Lesions range from 0.5 to 1 cm in diameter and could be a few or thousands. The lesions concurrently progress through four phases (macular, papular, vesicular, and pustular) before scabbing over and resolving over 2–3 weeks.3,4
In the current outbreak, most cases have been documented in men who have sex with men (MSM), causing a vesicular–pustular rash or genital lesions.1,3 The rash commonly occurs on the perineal area and genitals, suggesting transmission through sexual intercourse, and may easily be confused with other sexually transmitted infections (STIs), including herpes simplex infection, molluscum contagiosum, chancre, or granuloma inguinale.5,6
A better understanding of this poxvirus’ clinical spectrum and associated complications is emerging. 7 MPXV can coincide with other STIs, making its diagnosis and treatment more complex. Furthermore, additional clinical challenges exist with superimposed infectious complications of evolving skin lesions. We lack a contemporary description of the clinical progression of cutaneous lesions among individuals with MPXV and the occasional superimposed skin and soft tissue bacterial infections. Amid a growing number of cases in many settings, it is critical for clinicians to suspect compelling skin lesions as well as to familiarize themselves with the spectrum and staging of skin lesions. Herein, we present the case and photographic lesions detailing the clinical evolution of a patient with monkeypox infection who also developed superimposed cellulitis.
Case report
We present the case of a 36-year-old man who presented to clinical care for evaluation of painless lesions on his penis that developed 4 days before presentation. The patient was sexually active with male partners and on HIV pre-exposure prophylaxis with tenofovir disoproxil/emtricitabine with excellent adherence. The patient made a recent trip to Florida, where he and his husband had unprotected sexual contact with several male partners, including a man who recently traveled from the United Kingdom. He engaged in oral and anal insertive and receptive intercourse. He developed night sweats, sore throat, enlarged tonsils, and painful axillary and inguinal lymphadenopathy approximately 1 week following the sexual encounter.
Physical examination revealed oropharyngeal erythema, bilateral tonsillar enlargement, cervical and left inguinal lymphadenopathies, and multiple 2 mm umbilicated pearly colored and non-tender lesions on the shaft of the penis and one on the glans (Figure 1). The patient was afebrile, and his vital signs were normal. Blood tests showed no abnormalities. The fourth generation HIV antigen (Ag)/antibody (Ab) test was negative, and the nucleic acid amplification test (NAAT) for Chlamydia and Gonorrhea panel was performed on urine, throat, and rectum. The last one detected Chlamydia trachomatis.
Figure 1.
Initial presentation of skin lesions located on the shaft of the penis and the glans. Note small, well-circumscribed, raised lesions with umbilicated appearance.
Monkeypox was suspected. Therefore, the Colorado Department of Public Health and Environment (CDPHE) was contacted. Two swabs at three different sites each were collected for molecular identification. Given that the genital lesions were painless, primary syphilis was suspected, and a single intramuscular dose of 2.4 million units of penicillin G benzathine was administered. Because of exposure to STIs, chlamydia treatment and empiric gonorrhea therapy with doxycycline and ceftriaxone were also prescribed. His treponemal antibody came back non-reactive few days later.
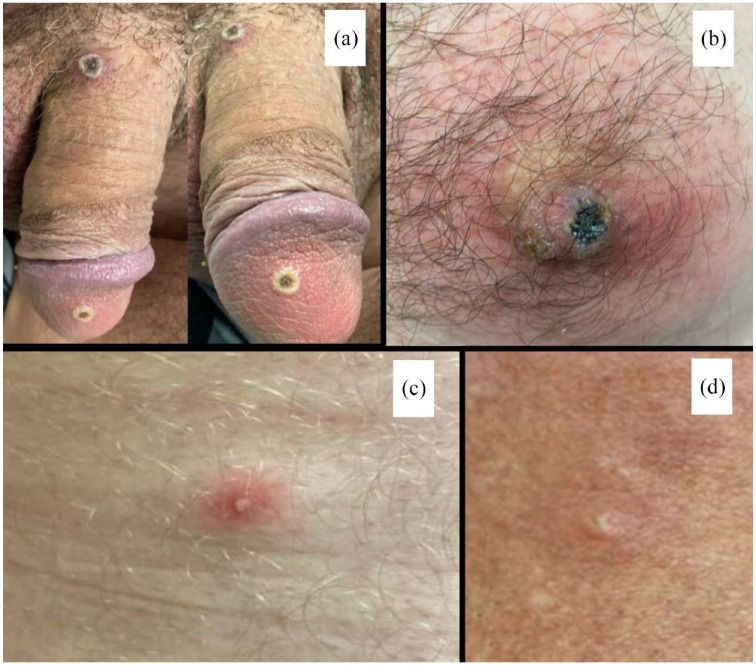
Four days after the initial consultation, the patient presented again with worsening penile lesions and new satellite lesions over his neck, thigh, and nipple, despite adherence to doxycycline. Clinical examination revealed two penile lesions with a central scab and two pustular lesions on the neck and thigh, nipple with flat erythema, and local itching (Figure 2). The nipple lesion seemed to have superimposed cellulitis, and amoxicillin/clavulanate 875/125 mg twice daily was prescribed for 7 days. Two days later, a real-time polymerase chain reaction for MPXV performed by the local health department was positive for Orthopoxvirus, later confirmed by the CDC, establishing the monkeypox infection. In an outpatient follow-up after 4 days of antibiotic treatment, the evolution of the lesions was favorable, with a reduction in local signs of inflammation in the nipple lesions (Figure 3) with no fever or chills. Ten days later, the lesions entirely resolved, and the patient was instructed to leave isolation.
Figure 2.
Evolution of lesions 4 days after the first consultation. (a) Two penile lesions with central scabbing and elevated borders. (b) Nipple with some flat erythema and local itching. (c) and (d) Two pustular and erythematous lesions on the neck and thigh.
Figure 3.
Progression of the nipple lesion. (a) The initial lesion with local signs of inflammation in the nipple, establishing the diagnosis of superimposed cellulitis. (b) and (c) Reduction of erythema and inflammation after antibiotic treatment and development of scab.
Discussion
Human monkeypox has re-emerged as a disease after decades of quiescence, and cases in the United States and other non-endemic countries are rapidly growing. The initial presentation of penile lesions in our patient suggested sexual contact transmission, and the evolving clinical presentation in our patient was typical, owing to the appearance of satellite lesions in other areas of the body, with signs suggestive of superimposed bacterial infection. In a recent study in the United Kingdom in 54 MSM with MPXV, 8 6 (11%) of the patients had cellulitis, and 5 required hospital admission. Unlike our patient, the diagnosis of cellulitis was not made at the initial clinical presentation but rather as an associated early complication.
Although anogenital lesions are the most common clinical manifestation in patients with MPXV during the current outbreak, other clinical manifestations such as pharyngitis and lymphadenopathy may occur, as in our patient. The most extensive study of up-to-date clinical manifestations reported oropharyngeal lesions in only 7% of the patients, while lymphadenopathy was very common (55%). 8 Skin lesions can progress during the natural course of the disease and can appear in distant anatomical sites, as described in this case, on the nipple and neck.
Elevated levels of interleukin (IL)-10 have been found in MPXV patients, which potentiates inflammation and could significantly impact dermal regeneration and healing. 9 The disrupted epithelial integrity provides a gateway for bacteria of the epidermal microflora and other colonizers to establish skin and soft tissue infections. Risks for secondary infection have not been extensively described, but they can contribute to the development of cellulitis or sepsis, as reported in the context of other Orthopoxvirus-associated diseases, such as cowpox virus infection. 10 In May 2022, a confirmed case of monkeypox in a man with HIV from Australia, who initially presented with genital rash, developed systemic illness, and superimposed bacterial cellulitis of his genitals on day 10 after symptom onset and was treated with intravenous cefazolin. 11 Cellulitis should be suspected in the clinical follow-up of patients presenting with worsening surrounding erythema, pain, swelling, and wound discharge. Whereas specific antimicrobial agent recommendations will vary depending on local practice and resistance rates, patients with mild to moderate cellulitis should be treated with oral agents with antistreptococcal and antistaphylococcal activity, while severe forms of cellulitis may need intravenous antibiotics. Development of cellulitis while on doxycycline and adequate response to amoxicillin/clavulanate may suggest the possible involvement of gram negatives, anaerobes, or streptococcus with suboptimal response to the tetracycline. Secondary infections could be preventable through the education of providers and behavioral modification by patients, avoiding scratching and inappropriate topical treatments. In patients with extensive skin lesions, using moist occlusive dressings could be an appropriate form of wound care.
Likewise, the suspicion and testing of MPXV should not be delayed or omitted in the presence of other confirmed STIs, especially in MSM with recent risky sexual behaviors and because of the high rate of other concurrent STIs observed in the current outbreak. 12 We recommend screening for STIs in all suspected cases, including HIV, Hepatitis B and C, syphilis, chlamydial, Herpes virus, and gonococcal infections. For these cases, it is necessary to ensure accessible, rapid, and reliable tests to prevent the further spread of the disease. WHO and CDC guidelines recommend lesion swabs for diagnosis. Blood and semen samples could be part of research protocols. These are necessary to determine the presence of the MPXV and to evaluate further whether MPXV can be isolated and replicated in cell cultures to suggest its potential as a sexual pathogen.
In summary, this case highlights that skin lesions caused by MPXV are susceptible to bacterial superinfection, and strict follow-up of patients is necessary, even in mild or moderate forms. Clinicians should have a high index of suspicion for any atypical genital lesions in the right epidemiologic setting.
Acknowledgments
The authors kindly thank the patient for providing the photographs for this report.
Footnotes
ORCID iDs: Alfonso J. Rodríguez-Morales  https://orcid.org/0000-0001-9773-2192
https://orcid.org/0000-0001-9773-2192
Daniel B. Chastain  https://orcid.org/0000-0002-4018-0195
https://orcid.org/0000-0002-4018-0195
Andrés F. Henao-Martínez  https://orcid.org/0000-0001-7363-8652
https://orcid.org/0000-0001-7363-8652
Contributor Information
Yeimer Ortiz-Martínez, Department of Internal Medicine, Universidad Industrial de Santander, Bucaramanga, Colombia.
Alfonso J. Rodríguez-Morales, Grupo de Investigación Biomedicina, Faculty of Medicine, Fundación Universitaria Autónoma de las Américas, Pereira, Colombia Master of Clinical Epidemiology and Biostatistics, Universidad Cientifica del Sur, Lima, Peru.
Carlos Franco-Paredes, Hospital Infantil de México, Federico Gómez, Mexico City, Mexico.
Daniel B. Chastain, Department of Clinical and Administrative Pharmacy, College of Pharmacy, University of Georgia, Albany, GA, USA
Amal A. Gharamti, Department of Internal Medicine, Yale University, Waterbury, CT, USA
Lilian Vargas Barahona, Division of Infectious Diseases, School of Medicine, University of Colorado, Anschutz Medical Campus, Aurora, CO, USA.
Andrés F. Henao-Martínez, Division of Infectious Diseases, School of Medicine, University of Colorado, Anschutz Medical Campus, 12700 E. 19th Avenue, Mail Stop B168, Aurora, CO 80045, USA.
Declarations
Ethics approval and consent to participate: Ethical approval was not required. The present report is in compliance with the Health Insurance Portability and Accountability Act (HIPAA).
Consent for publication: The patient has provided written consent for the publication of the case report and photographs.
Author contributions: Yeimer Ortiz-Martínez: Data curation; Writing – original draft; Writing – review & editing.
Alfonso J. Rodríguez-Morales: Writing – review & editing.
Carlos Franco-Paredes: Writing – review & editing.
Daniel B. Chastain: Writing – review & editing.
Amal A. Gharamti: Writing – review & editing.
Lilian Vargas Barahona: Writing – review & editing.
Andrés F. Henao-Martínez: Conceptualization; Investigation; Supervision; Writing – original draft; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Competing interests: The authors declare that there is no conflict of interest. The Editor in Chief and Associate Editor of Therapeutic Advances in Infectious Disease are authors of this paper. Therefore, the peer review process was managed by alternative members of the Editorial Board and the submitting Editors had no involvement in the decision-making process.
Availability of data and materials: All data is available as part of this report.
References
- 1. Vivancos R, Anderson C, Blomquist P, et al. Community transmission of monkeypox in the United Kingdom, April to May 2022. Euro Surveill 2022; 27: 2200422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. CDC. 2022. U.S. map & case count, https://www.cdc.gov/poxvirus/monkeypox/response/2022/us-map.html (accessed 3 July 2022).
- 3. Farahat RA, Sah R, El-Sakka AA, et al. Human monkeypox disease (MPX). Infez Med 2022. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McCollum AM, Damon IK. Human monkeypox. Clin Infect Dis 2014; 58: 260–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Minhaj FS, Ogale YP, Whitehill F, et al. Monkeypox outbreak: nine states, May 2022. Morb Mortal Wkly Rep 2022; 71: 764–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Soriano V, Corral O. International outbreak of monkeypox in men having sex with men. AIDS Rev. Epub ahead of print 7 June 2022. DOI: 10.24875/AIDSRev.M22000051. [DOI] [PubMed] [Google Scholar]
- 7. Rodríguez-Morales AJ, Ortiz-Martínez Y, Bonilla-Aldana DK. What has been researched about monkeypox? A bibliometric analysis of an old zoonotic virus causing global concern. New Microbes New Infect 2022; 47: 100993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Girmoetti N, Byrne R, Bracchi M, et al. Demographic and clinical characteristics of confirmed human monkeypox virus cases in individuals attending a sexual health centre in London, UK: an observational analysis. Lancet Infect Dis. Epub ahead of print 1 July 2022. DOI: 10.1016/S1473-3099(22)00411-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Reynolds MG, McCollum AM, Nguete B, et al. Improving the care and treatment of monkeypox patients in low-resource settings: applying evidence from Contemporary Biomedical and Smallpox Biodefense Research. Viruses 2017; 9: 380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pahlitzsch R, Hammarin AL, Widell A. A case of facial cellulitis and necrotizing lymphadenitis due to cowpox virus infection. Clin Infect Dis 2006; 43: 737–742. [DOI] [PubMed] [Google Scholar]
- 11. Hammerschlag Y, MacLeod G, Papadakis G, et al. Monkeypox infection presenting as genital rash, Australia, May 2022. Euro Surveill 2022; 27: 2200411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bížová B, Veselý D, Trojánek M, et al. Coinfection of syphilis and monkeypox in HIV positive man in Prague, Czech Republic. Travel Med Infect Dis 2022; 49: 102368. [DOI] [PMC free article] [PubMed] [Google Scholar]