Abstract
Adults experiencing homelessness experience a disproportionate burden of health disparities which has further exacerbated mental health, substance use, and coping during the COVID-19 pandemic. As limited data is available to understand the experience of adults experiencing homelessness and their health during this time, the purpose of this study was to explore how COVID-19 may have impacted their mental health, substance use, and ways of coping in this population. Using community-based participatory research, a community advisory board was established and remote individual interviews with 21 adults experiencing homelessness and 10 providers were conducted in Skid Row, Los Angeles. Using a qualitative, data analytic approach, the following major themes emerged: (1) Negative Impact of COVID-19 on Mental Health; (2) Negative Impact of COVID-19 on Limitation of Harm Reduction Services; and (3) Coping Strategies Utilized During the COVID-19 Pandemic. More research is needed to understand the impact of this pandemic on underserved communities.
Keywords: COVID-19, adults experiencing homelessness, mental health, substance use, Western USA
Introduction
COVID-19, a global pandemic has impacted people experiencing homelessness (PEH) and has presented unique challenges for health care access, health promotion, prevention, and treatment during quarantine (Tsai & Wilson, 2020). Typically, unhoused PEH are more susceptible to contracting a more severe case of COVID-19 as compared to those housed due to greater limitations in practicing COVID-19 protection behaviors; further, they may be at greater risk of serious COVID-19-related illness due to higher rates of comorbid physical conditions, poor diet and self-care, inadequate health care access, accelerated physical decline, and substance use (Culhane et al., 2020; Fazel et al., 2014; Heimer et al., 2020; Pottie et al., 2020). For example, persons who smoke have been found to be more likely to have poor COVID-19-related outcomes than persons who do not smoke (European Monitoring Centre for Drugs and Drug Addiction, 2020; Fazel et al., 2014; Vardavas & Nikitara, 2020). Furthermore, vulnerable populations who use opioids or have a substance use disorder are likely to experience impediments to care, including lack of health insurance and stigma by healthcare professionals (Volkow, 2020). This further complicates delivery of care if PEH become infected with the SARS-CoV-2 virus.
In Central City East (Skid Row), Los Angeles, where there are over 41,000 people living on the streets or in shelters at any night (Los Angeles Homeless Services Authority, 2020), there is a heightened risk for becoming infected with the COVID-19 virus. Moreover, it is estimated that in Los Angeles County, more than 700 PEH have tested positive with COVID-19 since September 2021, and more than 250 PEH have died since the beginning of the pandemic (Los Angeles County Department of Public Health, 2021c). Recent literature has revealed seroprevalence of SARS-CoV-2 among PEH has ranged from 4.5% (Sachdev et al., 2021) to 11.7% (Karb et al., 2020); with higher seroprevalence among those living in congregate areas.
Efforts by the Los Angeles Public Health Department has been swift to institute control measures, such as social distancing and closure of non-essential services. In addition, they have promoted education to PEH, including persons who use drugs, and health care providers about naloxone administration, and how to access available resources (Los Angeles County Department of Public Health, 2021b).
However, for unsheltered homeless adults, the “Safer at Home” policies which were intended to limit COVID-19 transmission (Fenley, 2021), may have also resulted in adverse events. Limited services, such as showers, food services, and restroom use, compounded by some high-density shelters (Davis-Berman, 2011; Hoch, 2000), in some instances, may have limited the ability to socially distance. Moreover, PEH who use drugs may experience greater harm during COVID-19 restrictions due to their inability to seek their usual treatment for their drug use, such as naloxone distribution, clean syringes, and may have needed to inject alone; thus, increasing the risk for overdose (Vasylyeva et al., 2020). Particularly for PEH who are using drugs and alcohol, stress, and crisis often exacerbate mental health issues (Farhoudian et al., 2020).
Impact of Confinement, Isolation, and Restricted Services on Worsening Mental Health
Psychological sequelae (i.e., anxiety, worry, irritation, anger, and depression) are a type of prodromal relapse into further drug use and should be treated rapidly (Farhoudian et al., 2020), as individuals use drugs to a higher degree when experiencing depressive, manic, or hypomanic episodes, posttraumatic stress disorder, and panic disorder (Vogel et al., 2019). Furthermore, a lack of quality social support and social interaction decreases motivation to maintain or improve upon healthy behaviors, such as seeing a medical provider for substance use or mental health treatment (Watson et al., 2016). Isolation from daily social environments leads to a decline in health behaviors as a way of coping. Mental health also decreases when social isolation ensues on a continued basis, exacerbating stress, anxiety, and other psychiatric illness (Bertram et al., 2021; Watson et al., 2016). Social isolation is also thought to increase the likelihood of fatal overdoses because fewer observers may be available to administer naloxone to reverse the overdose (Volkow, 2020).
The theoretical framework that guided this study was the Comprehensive Heath Seeking and Coping Paradigm (Nyamathi, 1989), which originated from the Lazarus & Folkman Stress and Coping Paradigm (Lazarus & Folkman, 1984) and the Schlotfeldt (1981) Health Seeking and Coping Paradigm. As utilized in numerous studies with PEH experiencing significant health disparities (Nyamathi, Salem, et al., 2017; Nyamathi, Shin, et al., 2017; Nyamathi et al., 2021), a number of factors are thought to influence health behaviors.
Based on this theoretical framework, factors impacting the health of PEH, whether it is mental health or worsening substance use, can include sociodemographic, situational, social, psychological, and behavioral factors. Sociodemographic characteristics include age and race/ethnicity, while situational factors include stable housing, the absence of which can result in a chaotic lifestyle. Social factors largely include support provided by friends and family, which mitigates feelings of loneliness. Psychological factors include a host of emotions PEH may be experiencing during the pandemic, including depressive symptoms and anxiety. Finally, behavioral factors include ways of coping such as seeking drugs or alcohol, or religion and spirituality.
Impact of Confinement, Isolation, and Restricted Services on Substance Use
While COVID-19 pandemic stressors (e.g., confinement, isolation, and reduction of healthcare services) have increased for PEH, along with a reduction of drug treatment services, little is known about the impact of COVID-19 and these limitations on worsening substance use (Tucker et al., 2020). Further magnifying COVID-19 transmission risk includes staffing shortages that limit access to drug treatment programs and the ability to attain clean needles, all of which increases the risk not only for substance use relapse (Hamilton, 2020; Roncero et al., 2020; Tringale & Subica, 2021) but as well infectious diseases, such as HIV and hepatitis C Virus infection (Farhoudian et al., 2020).
There has also been an increased use of synthetic opioids, such as Fentanyl and Spice. Increases in drug overdose and death can be linked to a toxic drug supply where drugs such as heroin have been altered to include fentanyl in toxic amounts (Centers for Disease Control and Prevention, 2020). Spice, a synthetic cannabinoid, is another drug that is widely available and risky due to its unsafe synthetic blends, and possible contamination (National Institute on Drug Abuse, 2020), which may lead to adverse side effects, such as hallucinations, breathing issues, kidney failure, and palpitations (Centers for Disease Control and Prevention, 2021). Yet, Spice is considered as a drug of choice for PEH due to lower cost as compared to other drugs (Kassai et al., 2017), being readily available during the pandemic, its ability to provide a mental escape, and non-detectability in drug test results (Ellsworth, 2022; Gray et al., 2021).
The impact of COVID-19-related modifications on drug treatment protocols affecting PEH is yet unknown, including limited provision of opioid drug substitution, such as methadone, suboxone, or buprenorphine during the COVID-19 pandemic (Farhoudian et al., 2020), or the acceptability and value of telephone/video communication for PEH (Farhoudian et al., 2020).
Purpose and Aims
Utilizing community-based participatory research methods, we assessed the perceptions of PEH living in Skid Row, Los Angeles, and health and social service providers (HSPs) serving this vulnerable population about their perceptions of how COVID-19 may have impacted the mental health, substance use and ways of coping of PEH.
Methods
Study Design
Community-based participatory research was selected as the approach as it furthers the researcher-community collaborative efforts that are critical to design interventions that are culturally sensitive and acceptable for populations experiencing health disparities (Andrews et al., 2013). A community advisory board was formed, composed of PEH who recovered from COVID-19, tested negative, or never tested, and HSPs; this board guided the investigators in subsequent phases of the research.
Engaging a Community Advisory Board
The Community Advisory Board was formed with the support of the leadership of six community organizations to screen and enroll PEH in the Central City East (i.e., Skid Row) area and included PEH (n = 4) and HSPs (n = 11). The role of the Community Advisory Board was to share the perspectives PEH and HSPs had about the impact of COVID-19 on the lives of PEH, as well as knowledge about COVID-19, and risk, and protective behaviors. In particular, the Community Advisory Board informed the investigators about the challenges PEH experienced in obtaining resources, and identified unique concerns related to the impact of COVID-19 on their health, substance use, and access to health services.
The Community Advisory Board was also instrumental in guiding the investigators in the type of questions to ask in the subsequent interview sessions, and in informing the investigators on which shelters to access participants for the interview sessions. Utilizing the Zoom online meeting technology (Zoom Inc., 2021), five Community Advisory Board sessions were held and included up to six persons who reviewed and provided suggestions on the development of a semi structured interview guide. Upon completion of the Community Advisory Board session, participants were paid $15.
The University of California, Irvine and University of California, Los Angeles Human Subjects Committee approved this study (UCI Approval Number 20206064; UCLA Approval Number: IRB#20-001983). After finalizing the interview guide and obtaining approval by the Human Subjects Protection Committees of the involved universities, individual one-on-one interviews were conducted, which included PEH (n = 21) and HSPs (n = 10). The purpose was to assess perspectives on the impact COVID-19 had on mental health, and substance use, and ways of coping with COVID-19.
Sample and Setting
Data were collected between November 2020 and January 2021, which represented the onset of the shutdowns and lockdowns in the US for the COVID-19 pandemic. In total, 21 PEH were enrolled who met the following criteria: (1) sleeping in the past night in a homeless living situation, (2) documentation of having been COVID-19 positive and completed quarantining; (3) history of substance use, (4) ≥18 years of age, and (5) able to speak English or Spanish. Furthermore, 10 HSPs were also included in these individual interviews if they were: (1) clinicians (e.g., registered nurses, nurse practitioners, physicians, physician assistants, or service providers [e.g., Community Health Workers, Licensed Marriage Family Therapists, Licensed Clinical Social Workers, and Spiritual Advisors]) and (2) provided educational and social services for PEH.
PEH were recruited if they resided in or received services from the selected sites or lived in outdoor areas. HSPs selected worked in some of these sites as well. While services at these sites were limited during the COVID-19 pandemic, typical services included warm meals, clothing, shelter, and programs for PEH.
Recruitment and Data Collection
After IRB approval, the research staff met with the site leadership and discussed the purpose of the study, strategies for engagement with their leadership and PEH served, flow of study procedures, roles of the research staff within these sites, and need for private space. The site leadership agreed in advance where the study flyers would be posted in their sites. In this study, an oral screening consent was administered by the research staff to ensure participants were first eligible to participate. Date of birth and the first three letters of the mother’s first name were obtained to identify potential participants who were repeaters (requesting screening a second time).
Once determined as eligible, a study information sheet, referred to as a written summary waiver, was discussed with each participant, questions were addressed, and an appointment was provided to schedule the individual interview in a private location. Based on the CHSCP (Nyamathi, 1989) and extant literature, the investigators developed a semi-structured interview guide. The community advisory board was involved in reviewing the semi structured interview guide and providing critical feedback on topical area, content, questions, and length. For example, topics included general COVID-19 concerns, screening and testing, social distancing practices, vaccination, and therapeutic modalities, as well as general survival issues of PEH such as access to food and resources, housing, mental health, substance use, and trauma.
Between November to December 2020, the investigators held 31 individual, one-on-one interviews with PEH and HSP. Detailed field notes were recorded (audio and video) within 24 hours of each session and considered nonverbal communication, ambient noise, cross talk, and interruptions. The same semi structured interview guide was utilized for both PEH and HSP; however, during the interview, the investigators tailored the more clinical and substance use questions for the nurses and other health care providers and the more social and resource-related questions for the social service HSPs. The length of time for each interview ranged from 30 to 55 minutes and participants received $3 for screening, and $20 for their participation in the interview. The full set of questions are found in the Supplemental Material.
Data Analysis
Between December 2020 and July 2021, the analytic team composed of two PhD prepared nurse scientists, and one undergraduate (n = 1) and two post graduate research assistants (n = 2) met on a biweekly basis and utilized an iterative, eclectic, data analytic approach (Saldaña, 2009) which allowed at least three cycles of coding by two independent coders. The activities were documented in an audit trail (i.e., agendas, meeting minutes, etc.). Under the guidance of experienced, qualitative researchers, the research assistants were trained in qualitative approaches and the research team worked collaboratively to develop a preliminary data analysis protocol, which was revisited weekly to add relevant example statements stemming from the data analysis. Structural coding was used to categorize the narrative collected data by topic (Saldaña, 2009) and, due to the volume of data, the research team prioritized a cluster of data around similarities and differences to initiate data analysis.
The data analytic team listened to the recordings and corrected inaccuracies by red lining the transcript. During the transcript review process, unique, salient, and in vivo statements were underlined in a “precoding” process (Saldaña, 2009). Afterwards, the transcript was deidentified by replacing identifiable places, locations, and names and assigning a code to that information. The data were then organized into a shared Microsoft Excel (Microsoft 365, 2021) file by research team members, by date, transcript, participant number, and transcript line extracted. These processes ensured credibility (i.e., internal validity) and reflexivity (i.e., self-examination).
Two independent coders completed first cycle coding methods inclusive of initial, process, in vivo, magnitude, emotion, values, beliefs, and simultaneous approaches to identify the intensity and quality of statements (Saldaña, 2009). Two independent coders completed second cycle coding methods to further distill the data and identify patterns, which also allowed comparisons of the data. Thereafter, first and second cycle coding were compared, themes and subthemes generated, and theme and subtheme definitions were devised.
The CHSCP theoretical framework concepts (Nyamathi, 1989) provided the investigators and research assistants aspects to consider in the development of the themes. For instance, CHSCP constructs were examined such as health seeking and coping during COVID-19, and immediate and long-term outcomes of COVID-19 (Nyamathi, 1989). Both the PEH and HSP interviews were analyzed together. During our analyses, the dataset retained the participant role (HSP and PEH) to enable the team to compare the perspectives and place into context the data.
To support credibility, during data analysis, data saturation was evaluated by quantifying frequencies of subthemes and themes. Critical and iterative evaluation of emerging themes and subthemes was completed and throughout this process, memos were written to reflect patterns, categories, themes, and concepts emerging from the data which contributed to formulating thick descriptions of the phenomenon to support credibility (Saldaña, 2009).
A comprehensive model rooted in the data was designed, critically evaluated, and iteratively refined during a debriefing session. Major themes and subthemes were prioritized based on cohesiveness and parsimony which contributes to the principle of confirmability (i.e., objectivity) and dependability (i.e., replicability; Shenton, 2004). Members of the community were able to review and comment on the report of this research, further supporting the CBPR process. The Consolidated Criteria for Reporting Qualitative Research (COREQ) was utilized as a reporting guide (Tong et al., 2019).
Findings
Our sample consisted of 21 PEH and 10 HSPs and their characteristics are presented in Tables 1 and 2, respectively. Briefly, the majority of the PEH were male, and averaged close to 50 years of age. Over one third (38.1%) of the sample was equally Hispanic and Black/African American and close to half (47.6%) completed 12 or more years of education. The majority of HSPs were mostly white and were health service providers (40%).
Table 1.
Sample Characteristics of People Experiencing Homelessness (PEH; n = 21) in Skid Row.
| M | SD | |
|---|---|---|
| N | % | |
| Age | 48.3 | 16.9 |
| Sex | ||
| Male | 18 | 85.7 |
| Female | 3 | 14.3 |
| Hispanic or Latino | ||
| Yes | 8 | 38.1 |
| No | 13 | 61.9 |
| Race | ||
| Black/African American | 8 | 38.1 |
| White/Anglo/Caucasian | 6 | 28.6 |
| Native Hawaiian/Pacific Islander | 6 | 28.6 |
| Other | 1 | 4.8 |
| Formal education completed (years) | ||
| <12 | 8 | 38.0 |
| >12 | 10 | 47.6 |
| College completion | 2 | 9.5 |
| Marital status | ||
| Never married/single | 13 | 61.9 |
| Divorced/separated/widowed | 6 | 28.6 |
| Decline to answer | 2 | 9.5 |
Table 2.
Sample Characteristics of Health and Social Service Providers (HSP, n = 10) in Skid Row.
| N | % | |
|---|---|---|
| Professional role | ||
| Mid-level provider a (e.g., PA, NP, and RN) | 4 | 40.0 |
| Program director | 3 | 30.0 |
| Social worker | 2 | 20.0 |
| Other | 1 | 10.0 |
| Hispanic or Latino | ||
| Yes | 3 | 30.0 |
| No | 7 | 70.0 |
| Race | ||
| White/Anglo/Caucasian | 7 | 70.0 |
| Asian | 2 | 20.0 |
| Other | 1 | 10.0 |
Note. PA = physician assistant; NP = nurse practitioner; RN = registered nurse.
Health practitioners with a defined scope of practice.
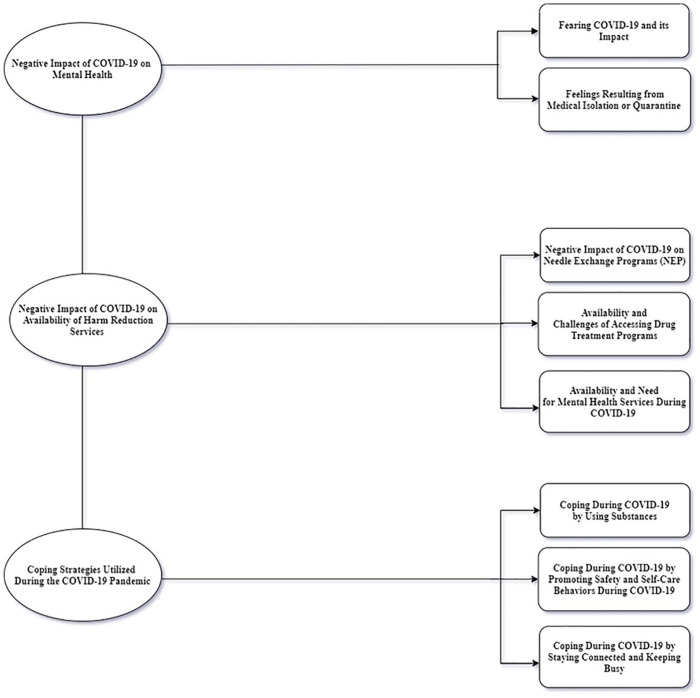
The major themes identified included: (1) Negative Impact of COVID-19 on Mental Health; (2) Negative Impact of COVID-19 on Limitation of Harm Reduction Services; and (3) Coping Strategies Utilized During the COVID-19 Pandemic (see Figure 1).
Figure 1.
Major themes and subthemes describing the impact of COVID-19 on adults experiencing homelessness.
Theme 1: Negative Impact of COVID-19 on Mental Health
The mental health impact of COVID-19 has heavily weighed on PEH, both in terms of fear and anxiety of the infection itself, as well the frustration, loneliness, and isolation experienced during quarantining and closure of facilities and services. Two subthemes were captured: (1) Fearing COVID-19 and Its Impact and (2) Feelings Resulting from Isolation or Quarantine
Subtheme 1: Fearing COVID-19 and Its Impact
Fear of COVID-19 and its impact were commonly reported experiences. About half of the PEH verbalized fears related to being exposed and infected with the COVID-19 virus, the scariness of living in an exposure-prone environment, and fears of dying. Emotions were also high for several PEH involving fears of being hospitalized, as well as fear of infecting others. As one PEH verbalized:
Well, emotions, it’s kind of like. . .what’s gonna happen. . .when. . . you test positive? I kind of like freaked out. . . I’m gonna go to sleep and . . . [am I] gonna wake up [on a] . . .ICU respirator? It does make you anxious a lot, you know, especially when you got a history of mental health. . . .Am I going to get other people sick? That’s my personal fears, you know. (PEH 3)
As part of expressing fear, one PEH explained that COVID-19 acted as a magnifier, accentuating his mental illness, especially when combined with experiences of loneliness and depression. Four PEH verbalized their fear of dying.
I mean I was scared. I ain’t know if I was gonna die cause I’ve been watching the news and stuff and everybody, like you know, this is killing. . . people in California, you know. So I thought I was gonna die. It was just a traumatic experience and. . .it made my. . .drug habit increase. I tell you that. (PEH 15)
While one PEH raised the fear of whether life would ever return to normal, two PEH reported that COVID-19 had no impact on their mental health. One PEH shared his lack of fear was related to his recent experience of being incarcerated, where the COVID-19 infection was rampant.
Well, I, I’m not. . . very afraid of it [COVID-19] because I came from a position where I was incarcerated. We were in a dormitory with 200 men and, you know. . . It’s . . . very close quarter living and . . .you know, 80% of the population, . . . got it like that. . . And so I was in that situation before so. . . (PEH 2)
Subtheme 2: Feelings Resulting From Medical Isolation or Quarantine
In many ways, the emotions expressed by the PEH were worsened by medical isolation or quarantine experiences. Five PEH expressed feelings of depression resulting from being medically isolated or quarantined. These feelings resulted from not being able to spend time with family, being unable to do usual activities, loneliness, not being informed, and being in a lockdown state. Along with sentiments of boredom, anxiety, and anger at times also surfaced; all of which was aggravated by underlying mental illness. As a few PEH articulated:
[I was] unable to do normal things. You know, like some of my daily routine was to get out, get away from here. You know, but now, since the restaurants closed, beaches were closed, . . . it’s been kind of rough. I would say it’s definitely depressing. (PEH 5)
. . .before this whole pandemic started, I was diagnosed with chronic depression. This has certainly increased it substantially. . .(PEH 16)
. . .at times, you get angry when I’m watching the news. . . and I’m seeing how people are treating this. I’m seeing how . . . our president and our government reacts to it. You know, like it’s no big deal, that makes me angry. . . .Because you know, if it cuts down on your freedoms of just being . . .able to walk around and just to socialize with somebody. . . . I have no clue right now when, where, what. . . this stuff will [end]. . . . You know. . . I don’t see any hope (PEH 4)
Several PEH likened being in medical isolation or quarantine to just like being in jail or being treated like a criminal or worse which resulted from lack of ability to visit with anyone, not being able to leave the room, and only having TV to watch. Moreover, a few PEH described their time as boring and disliked not being able to go out. The participant experience was similar to that shared by several others:
I mean . . . I like to be outside, so like being able to go out and get some fresh air. And you know, . . . to a person that can’t do that, it’s a lie, you know. It’s like. . . just because I’m tested positive for this disease. I understand I want to. . . protect the environment and protect the people, but don’t treat me like a criminal, like I’m not a criminal. I didn’t do nothing wrong. I just caught a disease that that’s in the air that I cannot control, it’s not like I could ‘cause it. . . You understand what I’m saying, so like you treat me like criminal because I got COVID, but that’s not cool, and that’s how I felt when I was in there because I felt trapped. We don’t got the option to check yourself out. What is that, jail? (PEH 15)
Theme 2: Negative Impact of COVID-19 on Availability of Harm Reduction Services
Participants contended that the availability of services related to the COVID-19 pandemic negatively impacted access to needle exchange programs, mental health programs, and substance treatment programs. Among PEH who typically utilized these services, the changes to these services were heavily felt. In this major theme, three subthemes included: (1) Negative Impact of COVID-19 on Needle Exchange Programs, (2) Availability and Challenges of Accessing Drug Treatment Programs, and (3) Availability and Need for Mental Health Services During COVID-19.
Subtheme 1: Negative Impact of COVID-19 on Needle Exchange Programs (NEP)
Knowledge regarding the availability of needle exchange programs varied among PEH and HSP participants. As one PEH admits,
I don’t know, I would imagine it’s less. It’s harder to get clean needles because you know everybody’s like making themselves scarce, so. . . that’s what I’m guessing . . . I don’t know that for a fact, but you know, the way everything else is working, it’s a little harder to get, you know, even your GR card. . . so I’m guessing it’s the same thing with needles (PEH 2)
During the height of the COVID-19 pandemic, participants verbalized the perception that several needle exchange programs closed and as a result, PEH were reusing the same needles. Among the four HSPs, conditions which resulted from reusing needles included an increase in abscesses and other types of skin infections. Another HSP reminisced about how the services provided at the needle exchange sites had changed with COVID-19. For example, congregating around the needle exchange programs had been abruptly stopped with COVID-19; the socialization aspect, important to injection drug users, was lost:
They used to have needle exchanges [where] you could go in, you could get a meal or a snack bag, you could get water, you could get your kits, you could do your needle exchange, you could hang out, you could see a psychiatrist. Now many of them, you can’t even go inside anymore, and they have a window, and there’s a table, and you put your needles down and then they put their needles down. There’s no. . . exchange of like touching. I think that unfortunately, that takes a huge connection out. I mean, we know that feeling isolated increases our substance use in many ways, and so now the isolating, like world of drug use, is even more isolating because you once could go hang out at your needle exchange. . . . That’s no longer happening. . . .I do think that there is reduced availability across Los Angeles. (HSP 8)
A few PEH (4) and one HSP were aware of NEPs operating in the community. One PEH was only aware of its existence on the website, while one was familiar with the fact that 60 needles were provided at any point in time. It seems apparent that the changes in the nature of the services offered by NEPs to increase physically distance had unintended consequences for PEH.
Subtheme 2: Availability and Challenges of Accessing Drug Treatment Programs
Despite the COVID-19 pandemic, access to drug treatment was an important service for PEH. A few HSPs and one PEH were aware that drug treatment services were still open and available. Nevertheless, a similar number of PEH and HSPs either believed services were not available or believed services were reduced. One of the HSPs was very clear of the implications of reduced drug treatment support.
In terms of substance use, clients who are unable to get services, are more likely to relapse. Losing support is a trigger for the clients. They need their supports to help them deal with issues and diminish triggers. . . .[as] increased numbers of clients who formerly used, and then stopped, start up again. (HSP 5)
Regardless, challenges in accessing these services were clearly articulated by one HSP and five PEH. These challenges included length of time needed to enroll an individual into a drug treatment program, the reality that drug treatment teams on the streets are overwhelmed due to COVID-19, and conversion of drug treatment sites for shelters. As one HSP portrays, processes for getting into drug treatment has become challenging.
. . .when someone, homeless or not, . . .says that they’re ready to go to rehab, . . . it’s not a next week thing. It’s right now. . .and it has to be available right now. And you know, unfortunately, COVID-19 has reduced the availability for both. Now it is such a process. Pre COVID-19 tests need to happen before, there’s an increased waiting list. Some places are not taking people. There are no in-person AA meetings. . . . AA meetings are now on the phone. Well, if you don’t have a phone, how are you gonna get that help? (HSP 8)
In this example, a process that would typically take 1 to 2 hours took 11 hours, with the risk that the PEH would have come down from their high, go into withdrawals, and become anxious depressed, and change their minds about getting treatment. In addition, HSPs shared their beliefs about the ability of their clients to receive needed services. One HSP contended that reduction or limitation of services resulted from COVID-19 shutdowns. As a result, reduction of typical face-to-face drug treatment programs and of counselors to speak with resulted in relapse.
I think we’ve seen an increase [in substance use]. . . .we’ve had an issue with, you know, clients’ meth use. . .everything’s like shut down. [We can’t offer] 12-step programs but those have been online since April. It’s all limited access with staff. . .It’s a higher [likelihood], you know, . . . a lot of clients have relapsed during those times. I would say probably . . .meth usage, heroin. . . . . And you know, clients getting alcohol in the building and getting drunk and then acting belligerent. They would have to be exited from the program. (HSP 4)
While some drug treatment programs had to reduce to 25% capacity, as one PEH articulated, fear of COVID-19 exposure prevented him from entering drug treatment as well. Concurrent with reduced services was an increase in telehealth options; however, this was not always successful among PEH as one HSP articulated:
And telemedicine and televisits just simply do not work with this population. I would say less than 10% of our patients have a reliable cell phone . . .and when everything is closed, they don’t have anyone who plugs it. So . . . one of the new things that we’ve been handing out is solar chargers. . . .but there’s not enough solar chargers to go around to make a difference on a population level. (HSP 4)
Despite the perception of lack of availability and reduced services, as well as confusion on which programs were open or closed, three PEH verbalized the benefits of drug treatment, as being clean of drugs and alcohol, and enjoying the classes offered. One HSP highlighted the benefits of a harm reduction approach, whereby services were permitted to be accessed, but PEH were not allowed to use on site (HSP 4).
Subtheme 3: Availability and Need for Mental Health Services During COVID
Interestingly, a fair amount of PEH (6) and fewer HSP (2) reported that mental health services were still available to PEH during the COVID-19 shutdowns. However, one PEH reported no access to secure his medication, and a few PEH (2) and one HSP reported reduced services. Another PEH reported that fear of exposure to COVID-19 prevented him from accessing his depression medication.
Among PEH receiving services, counselor support was common, as well as receiving medication renewals. For some providers, services were being delivered on the phone or via telehealth. As one HSP noted, face-to-face delivery of services is always best.
Yeah, absolutely, ‘cause you know, our psychiatrist does a fantastic job doing all these meetings on Zoom, but of course that face-to-face interaction is always, you know, the best, ‘cause you tend to notice more things in person. (HSP 9)
Services by psychiatric health specialists were reported as being very limited for a long time, and as one HSP described, primary care providers have been needed to fill the gap when psychiatrists were kept busy with dealing with patients with severe mental health issues. COVID-19 clearly emphasized the limitation of mental health services.
Even pre-COVID, there’s only one street psychiatrist for all of County 1. And his main job is to determine hold cycles for 5150s. . .not performing any ongoing psychiatric management. . .like med refills or even diagnoses really. So most of that is done by the primary care providers on the street. . . But in the absence of anybody else, we do the best we can, and we try to train ourselves up. . .(HSP 6)
Theme 3: Coping Strategies Utilized During the COVID-19 Pandemic
PEH and providers articulated several coping strategies which were helpful during the COVID-19 pandemic. In this next section, coping modalities utilized by PEH and HSPs are highlighted as they relate to dealing with emotions related to the raging COVID-19 pandemic, and the shutdowns in businesses and changes in operations. Subthemes identified included (1) Coping during COVID-19 by Using Drugs, (2) Coping during COVID-19 with Alcohol and Smoking, and (3) Coping during COVID-19 by Staying Connected and Keeping Busy.
Subtheme 1: Coping During COVID-19 by Using Drugs
COVID-19 had a mixed impact on both increasing and decreasing drug use; for some PEH in our sample, drug use was one of the most common ways of coping. However, two HSPs were not aware of any change in drug use during COVID-19.
Yeah, I think that most of my folks, if they’ve been heroin users, they’re continuing to be. . . .I have a population that does heroin and meth and crack and basically whatever they can; and that has not changed. (HSP 8).
Our data revealed that while five PEH and one HSP reported less drug use, either of themselves or other PEH in general, a fair number of participants reported drugs were used often (one HSP and seven PEH). During COVID-19, three PEH expressed feelings of depression and sadness and verbalized that using drugs was a familiar coping skill they knew and turned to deal with their emotions.
During the COVID-19 pandemic, one HSP highlighted that several PEH even moved on to harder substances,
Yeah, so because of the levels of anxiety, I’m seeing folks who would typically just use THC or alcohol, I’m seeing them jump to a harder. . . substances, you know, and that they’ll use heroin, they’ll use fentanyl, they’ll look for an injectable. . . [Going from] alcohol to meth is a big jump. . .I’ve seen dealers now realize. . . it’s OK to get you. . . addicted at a cheaper rate right now, [as]. . . I’m going to keep you longer. . . so they [dealers] are decreasing their costs on the street is what I’m seeing. (HSP 2)
Coping during the COVID-19 isolation period played a significant role in increasing drug use. As one HSP remarked, while some PEH were happy to be in their safe places, sheltered from unwanted intruders or the police, others increased use of drugs due to a decrease in harm reduction services. Another PEH described their experience during isolating for COVID-19, self-medicating, and worsening drug use. He shared,
I had so many issues of being in the hotel room, being it feel like a box, you feel me, so I felt like I was so in there, that when I got out, I didn’t wanna smoke the weed. I wanted to get high. It’s really like I wanted to really have something to. . . calm my nerves. (PEH 15)
Another PEH was unable to get drugs because he was in lock down. However, he reported, “So when I finally got a chance to smoke, I just went hard.” (PEH 15)
When fentanyl was discussed, one HSP did not believe COVID-19 resulted in an increase of fentanyl use; however, several other PEH and HSPs believed that COVID-19 had an impact on increase in fentanyl use. Three HSPs contended the dangers were caused by the lacing of many other drugs with fentanyl, and among two HSPs, the inconspicuous nature of the mixing. Challenges getting off fentanyl was another reason cited by one HSP. For another HSP, the easy jump from heroin to fentanyl was a serious concern.
. . .the increased fentanyl on the street has been slowly creeping up now for a few years, but. . . at least being mixed with heroin. . . But since COVID, we’re seeing more and more just pure fentanyl, where people aren’t even bothering with the heroin anymore. . . So they’re just taking whatever they can take. (HSP 6)
Another HSP contended that fentanyl has become, not a choice, but a contaminant of the drug supply. A third HSP reported that PEH do not feel it is worth it to waste any drug on the test kits that are available for PEH to test for the presence of fentanyl, leading to greater risk for overdoses. While a few PEH were aware of overdoses happening on the streets because of fentanyl, not all believed that COVID-19 increased the number of overdoses. Regardless, one HSP indicated that a harm reduction approach was most helpful.
I’m very open with my patients and I do take an approach of if I was living out there, I would want to numb myself too. You’re going through these daily traumas . . . I’m not here to tell you not to use it. . .I’m not going to shame you, or make you feel like I’m not going to return because you’re using drugs. . . . I have seen an increase in the last year of more overdoses because of the fentanyl. But I don’t know if it is because of COVID. . . or because fentanyl is much cheaper and . . . I’m now seeing it in heroin, I’m seeing it in crack, and I’m seeing it in methamphetamine (HSP 8).
On the other hand, Spice, synthetic marijuana, was considered a new drug that was a cheaper high. However, one PEH commented on how scared he was when a woman was having convulsions in his tent, after using Spice. He commented that “It’s freaking [me] out because. . . she was at . . .my place and she was like . . . foaming [at]. . .the mouth. (PEH 18).
Subtheme 2: Coping During COVID-19 With Alcohol and Smoking
In terms of greater focus on alcohol consumption, several PEH (n = 8) freely shared information about their alcohol use as well and their observations about others. For one PEH, COVID-19 triggered thoughts about disappointments in their life which led to an increase in use of both drugs and alcohol. Perspectives shared by one PEH and four HSPs about why alcohol use increased among PEH was because PEH were able to find safe drinking places, the perception that alcohol was able to be more safely secured during COVID-19 as opposed to drugs, or that alcohol killed the COVID-19 virus. Other PEH (n = 3) who were recovering from addiction were coping by trying to avoid having conversations with the alcohol/drug using crowds.
I’ve noticed that my alcohol consumption has greatly increased. My use of street drugs. . .it’s probably stayed at the same or probably decreased. Just ‘cause I don’t wanna go out and deal with people you know. But alcohol, I mean it’s in my opinion it’s the safest way to go. . . So I’d rather go to a liquor store and find myself some liquor where I don’t have to have any contact with anybody in regards to obtaining street drugs where I have to go and have you know conversation with street dealer, you know? (PEH 16)
In terms of smoking, one PEH reported greater amounts of cigarette smoking, while another PEH indicated that smoking was one of the three most popular substances, along with alcohol, and marijuana. Increase in smoking was highlighted by four PEH. Moreover, while two PEH reported not smoking themselves, they did observe other PEH increasing their smoking intake. Justification for one in increasing his smoking included getting a “little antsy.” One PEH admitted it was not difficult to secure cigarettes when he wanted.
I mean I have no problems getting . . .the tobacco one way or the other, you know . . . I don’t know if it’s [I am] bored or just being frustrated or whatever. . . .Since March I’ve been smoking a little bit more. (PEH 4)
Subtheme 3: Coping During COVID-19 by Promoting Safety and Self Care Behaviors
PEH were cautious about protecting themselves from COVID-19 in several ways. For example, several PEH reported the misguided belief held among PEH who used substances that increased alcohol consumption could kill COVID-19 virus within their body.
Well, they drinking that really cheap vodka. . . They drinkin’ like 3 - 4 bottles more instead of wasting money on drugs. . .cause they got the [belief] that by drinking more alcohol, it’s going to kill [the COVID virus]. COVID is not gonna affect them. I don’t think it makes sense, but you know. (PEH 3)
Another safety coping mechanism articulated was related to adhering to the Center for Disease Control and Prevention’s COVID-19 protection guidelines. Three PEH knew it was important to keep socially distant and indicated, “I don’t really get like [to] get close to people that are using on the streets right now” (PEH3). This PEH continued to have dual points of view. On the one hand, he indicated he was careful about not touching anything, and he did not want to have people close to him, “because. . .I don’t want [your] cooties on me.” However, later in the conversation, he articulated,
I don’t really worry about it. . . . There’s a lot of things that can happen other than having the virus. You can slip and fall, you can get you hit by a car. . . .I don’t feel. . . it’s a real big deal, I don’t worry about that. I know. (PEH 19)
In addition to social distancing, a few PEH tried to enhance hygiene of their fellow PEH. One PEH advised friends about ways of being safe in the streets. For example, advising injection drug users of where to get clean needles was one strategy. While limitation of services was problematic, as articulated earlier, several PEH were aware of which services were still operating.
I just try to avoid everything and do the procedures I was told to do that like wash my hands . . .sanitizer or wear a mask and . . .like the gear . . .they gave me in the mission. (PEH 1)
Another safety mechanism was to teach other PEH to avoid digging through the trash to get food. As this PEH warned, “don’t look at the trash for food, because place 26 feeds you.” Two other PEH worried about socializing or smoking cigarettes behind someone else due to fear of getting self or others sick (n = 4). Decreasing cannabis use was also highlighted by one PEH (16) due to fear of having contact with the vendor.
One HSP was quite concerned about promoting safety of PEH who needed to choose between staying safe and using their substances. In addition, harm reduction philosophy was followed very closely. It was about being accepting of the reality of the world out there in terms of what persons using drugs were doing to survive.
Several PEH were proud to share that they took care of themselves by limiting their use of substances. This was proudly articulated by one PEH, avoiding using substances.
I don’t use anything intravenously, so I don’t consume heroin, methamphetamine. I, I don’t, you know. . .[However], a little takes you a long way, you know. So you really don’t consume that much of it. (PEH 16)
Subtheme 4: Coping During COVID-19 by Staying Connected and Keeping Busy
Keeping in touch with family and friends was another important coping mechanism practiced by one PEH. For several PEH, staying socially connected using technology in the form of phone or computer was a significant coping strategy. As one PEH mentioned, “keeping in touch with daughter by phone” (PEH 5) was perceived as very helpful. PEH and HSPs described the presence and absence of religion and/or religious practices as a way of being connected to God. For those who receive comfort through religion, adaptations were sometimes required when there were disruptions in services. As one PEH articulated,
It [COVID-19] causes me to stay awake a little bit at night and my method is to pray. . .to sort of center myself and so I typically will tend to pray for the individuals and the organizations that are impacted as a result because it’s a monster all around and we’re all trying to figure it out . . .it does create some sleepless nights in terms of you know losing folks that were on a really good path, that you know, we’re not going to get back, . . .as a result of COVID-19.
Several PEH shared how helpful a positive attitude was to get through COVID-19.
[Being affected by COVID-19]. . . .didn’t destroy me. It made me wake up a little bit better. It made me be more conscious and. . .cleaner about my surroundings and . . .be more protective. . . I do care and I start taking care of myself, hygiene, physically and mentally wise because it’s very important. . .I’m a young man of God and I have to be clean. . . .I do like to take a shower (PEH 7)
For another PEH, isolating himself was important for his self-care which was particularly important when other PEH were dealing with their addiction as well.
Being able to keep to yourself and not really having to deal with them. . .you know, we’re dealing with other people who are dealing with their own stuff too. So, when they’re dealing with [their addiction], . . .that’s usually when we have those kind of . . .stress issues. (PEH 2)
For others, the distraction of using technology to keep busy or as a distraction was another coping strategy.
Thanks to the internet and my devices like my phone, I don’t feel that disconnected. If I didn’t have that, I would, it would try to be a problem. (PEH 2)
Another PEH reported keeping busy was helpful. “As long as I stay productive then I’m feeling I’m feeling okay now. (PEH2) For another, it was all about keeping his mind occupied by keeping busy.
Discussion
The disproportionate and far-reaching impact of the COVID-19 pandemic on PEH necessitates critical examination. To address this need, the research focused on how COVID-19 impacted the mental health, substance use and ways of coping among PEH. The experiences of PEH were described as they relate to three main themes: (1) The Negative Impact of COVID-19 on Mental Health, (2) The Negative Impact of COVID-19 Limitations on Harm Reduction Services, and (3) Coping Strategies Utilized During the COVID-19 Pandemic. On balance, guided by a health seeking and coping theoretical framework, findings revealed that PEH coped with the impact of COVID-19 in multiple ways, including both avoidant and non-avoidant responses.
Mental health was negatively impacted during COVID-19 as newly imposed guidelines, restrictions, business closures, and changes to support services caused feelings of fear and worry. PEH shared how they witnessed people entering hospitals, yet, never returning, which caused apprehension around utilizing healthcare services. Further, living in congregate spaces raised concerns among PEH in terms of their ability to physically distance and adhere to imposed guidelines. Our findings are not isolated; in fact, in a retrospective cohort study among San Francisco-based PEH (N = 995), authors suggested that PEH voluntarily discontinued isolation in private hotels during COVID-19 as a result of mental strain due to isolation, disruptions in routines, and mistrust of services (Fuchs et al., 2021).
Among PEH, being medically isolated during COVID-19 likewise caused feelings of alienation and isolation, as social networks and support systems were disrupted. While seeing people face-to-face was no longer an option for some, technology bridged those gaps. Interestingly, while some participants were aware that mental health services were still available to PEH during COVID-19 shutdowns, via the use of telehealth, a particular concern is the number who were not aware. Further, some PEH were able to stay in touch with family, friends, and other forms of social support through technology, which also served as a way to enable some PEH to stay occupied, especially during periods of quarantine. Continuing to have these sources of support enabled some PEH to share mutual concerns and experience, while remaining socially distant and relaxed.
In the coping literature, being able to access social support is one problem-focused coping strategy that is often helpful for PEH as they deal with life crises (Garfin et al., 2022). Further, having social support is associated with reduction in substance use and poor health outcomes (Fitzpatrick, 2017; Garfin et al., 2022). In the literature, investigators have found that among PEH (N = 350) in Oakland, California, physical symptoms (i.e., joint pain, fatigue, back pain, and sleep problems) were positively associated with feelings of loneliness (Patanwala et al., 2018). However, it is important to consider other coping strategies that might mitigate the absence of social support, a key theoretical concept with another, having to do with alternative ways of coping. For example, employing effective tools for coping with stress experienced, such as engagement in mindfulness training that teach stress management and effective coping skills, can be effective in regulate emotion (Bowen et al., 2014).
While our findings and that of others (Hajek et al., 2021), highlighted the fact that some PEH experienced depressive symptomology and anxiety due to fears of contracting or transmitting the virus; for other PEH with a history of recent incarceration, being isolated allowed a time to binge on movies and the internet, and to catch up on things they may have missed while incarcerated. However, both PEH and HSPs perceived mental health services as limited. While a number of PEH were benefitted by a few mental health services made available by shifting to telehealth, mobile outreach, and other adapted versions, other PEH were not in favor or virtual counseling and preferred face-to-face contact with providers.
Although PEH are an already marginalized population, the COVID-19 pandemic has further destabilized and threatened any tenuous resilience PEH may have, further diminishing the few resources they may possess (Albon et al., 2020). Furthermore, those with mental health and substance use issues risk being further ostracized from existing social or state safety nets and/or continuity of care (Albon et al., 2020). In terms of substance use, a number of coping strategies utilized during the pandemic were adaptive and maladaptive to these new realities. Some PEH increased their intake of drugs and alcohol to cope with the disruptions to daily life and stressors associated with quarantining, while others reduced their substance use during the quarantine or isolation. Similarly, Tucker et al. (2020) found that younger PEH aged 18 to 24 reported increases in substance use (e.g., tobacco, marijuana, and alcohol) during COVID-19. In yet another example, some PEH were under the mistaken belief that increasing drug or alcohol use had the ability to “kill the virus.”
While the literature is clear that avoidant coping strategies in the short-term can protect the individual from stressful events (Wu et al., 2013), the benefit of such coping is often short-lived. Most importantly, problem-focused coping strategies predict more positive adaption long term (Suls & Fletcher, 1985). For people who use drugs, stress, and crisis often trigger or exacerbates mental health issues (Wang et al., 2019). Anxiety, worry, irritation, anger, and depression are often seen as the beginning stages, a type of prodromal relapse into further drug use and should be treated rapidly as such (Wang et al., 2019). Thus, interventions focused on teaching healthier coping skills is of critical importance in promoting resilience (Thompson et al., 2018).
As addiction is a disease of isolation, for PEH with psychiatric comorbidities, the destruction of routines, and harm reduction can lead to relapse (Costa et al., 2020). Alone, homeless, in recovery and experiencing service limitations, the client may lose connectedness to others, and emotional support networks; without this social capital, recovery potential is lowered, and isolation is known to increase risk of relapse and overdose fatality (Tucker et al., 2020). Among PEH, heightened fears and emotions were likewise worsened by the limitation of harm reduction services during COVID-19. As a result of lack of information in understanding how to access limited services, such as drug treatment programs and needle exchange programs, PEH and HSPs reported relapse as a common occurrence, as well as engagement in unsafe practices (e.g., using old needles and/or sharing needles). Moreover, having to rely on telehealth and videoconferencing modalities for drug counseling and Alcoholics Anonymous or Narcotics Anonymous sessions was challenging for many PEH.
Other researchers found that harm reduction services had to be adapted during COVID-19 by providing cell phones so PEH could participate in telehealth, or allowing PEH to pick up opioid treatments and injecting equipment (Parkes et al., 2021). It is also important to note that some PEH also had reservations about visiting drug treatment facilities due to fears they were putting themselves at risk for contracting COVID-19. This is also true for PEH who were adhering to the social distancing and other protective guidelines. While avoiding congregate spaces was important to reducing COVID-19 spread, PEH also shared that they avoided hospitals, and other healthcare facilities, which in some cases resulted in illnesses going untreated.
Among PEH who increased their drug use, changes in availability of their drugs of choice resulted in the use of new and more potent drugs (i.e., Fentanyl and Spice) to cope with the stressors associated with the COVID-19 pandemic; all of which has been related to the production of more toxic drug supply. These drugs have become more readily available and at cheaper cost. These new and more potent drugs became easier to obtain as PEH formed new addictions because of perceiving stronger highs with harder to stop drugs; believed to result in greater instances of overdose and death (Ellsworth, 2022). According to a recent published report, PEH were 36 times more likely to die of a drug overdose, than those in the general population, primarily due to the increased use of fentanyl (Los Angeles County Department of Public Health, 2021a).
As demand for illicit opioids have increased, drug dealers have attempted to increase profits by adding the powerful synthetic, fentanyl, to the illicit supply of heroin. For those who are dependent on illicit drugs, increased access to harm reduction services are being recommended—for example, supervised consumption sites, drug checking, expanding the availability of safe supply programs and reducing barriers to access them, etc. These services are likely to even be more important during public health crises such as a pandemic. For PEH, efforts to endure adequate housing is also likely to be important in addressing vulnerabilities identified in this study and enable coping.
Study Limitations
There are a number of notable strengths of this study. Two notable strengths include the collection of valuable data during a pandemic, as well as the engagement of the community to help guide the researchers in conducting this study. This was accomplished by our Community Participatory methods inclusive of engaging a Community Advisory Board and hearing the perspectives of PEH and HSPs. There were also three limitations related to the sample size: First, the sample enrolled was one of convenience of PEH and HSPs from Skid Row who were able and willing to participate in an individual interview via Zoom. Second, PEH and HSPs primarily spoke English; thus, our understanding of perspectives of non-English speaking PEH remained limited. Third, our sample was primarily male, since the proportion of males experiencing homelessness is greater than females experiencing homelessness. Thus, we were unable to fully understand the perspectives among women experiencing homelessness, or families experiencing homelessness. This may be important as women experiencing homelessness tend to have higher levels of depression (Roze et al., 2018, Tinland et al., 2018)
Multi-System Future Clinical and Research Implications and Recommendations
The present study evaluated the impact of COVID-19 among PEH and HSPs and unearthed critical information among this underserved community which has led to several important contributions to the existing knowledge base and further lays the groundwork for future research as it relates to substance use, mental health, and coping. However, the results necessitate further clinical and research exploration at the individual, community, and systems-level.
At the individual level, among PEH, interesting areas of research at the individual level relate to long-term health outcomes among persons experiencing homelessness as a result of living through the COVID-19 pandemic; and how can clinicians address long haul COVID-19 mental health symptoms? At the community and systems-level, a greater understanding related to the existing pandemic and disaster preparedness would be helpful to further understand and generate solutions. At the systems-level, there is a need to develop a center for pandemic and disaster preparedness for underserved communities to avoid major disruptions in mental health, needle exchange programs, and alcohol/drug treatment. While this work contributes to the existing knowledge of COVID-19 among PEH and HSP, considerably more research needs to be done on the impact of COVID-19 and its mitigation strategies on this underserved community locally, cross nationally, and globally.
Supplemental Material
Supplemental material, sj-docx-1-gqn-10.1177_23333936221108712 for Perceptions of Homeless Adults and Their Providers on Coping With the Impact of COVID-19 Pandemic on Mental Health, Substance Use, and Harm Reduction Services by Adeline M. Nyamathi, Lillian Gelberg, Darlene Lee, Nicholas Arce, Alexandria Patten-Jones, Kartik Yadav, Maniyah Goodwine, Mitra Alikhani, Maritas Yao, Alicia H. Chang and Benissa E. Salem in Global Qualitative Nursing Research
Acknowledgments
This manuscript would not have been possible without the support of people experiencing homelessness, health and social service providers, and our research team. Thank you for your teamwork, dedication, and commitment during such extraordinary times.
Author Biographies
Adeline M. Nyamathi, ANP, PhD., FAAN is a Distinguished Professor at the University of California, Irvine, Sue & Bill Gross School of Nursing in Irvine, California, United States.
Lillian Gelberg, MD, MSPH is a Professor at the David Geffen School of Medicine at the University of California, Los Angeles in Los Angeles, California, United States.
Darlene Lee, ND, MSW is a Naturopathic Doctor at the University of California, Irvine in Irvine, California, United States.
Nicholas Arce, BA is a Graduate Student Researcher at the University of California, Irvine in Irvine, California, United States.
Alexandria Patten-Jones, RN, MSN is a Graduate Student Researcher at the University of California, Irvine in Irvine, California, United States.
Kartik Yadav, MSCR is a Research Director at the University of California, Irvine, Sue & Bill Gross School of Nursing in Irvine, California, United States.
Maniyah Goodwine, BA is a Research Assistant at the University of California, Irvine, Post-Baccalaureate Program in Psychological Science, in Irvine, California, United States.
Mitra Alikhani is a Research Assistant at the University of California, Los Angeles, School of Nursing in Los Angeles, California, United States.
Maritas Yao, BA is a Research Assistant at the University of California, Los Angeles, School of Nursing in Los Angeles, California, United States.
Alicia H. Chang, MD, MS is the Los Angeles County Department of Public Health Regional Health Officer for South Bay and East Los Angeles County, Los Angeles, California, United States.
Benissa E. Salem, PhD, RN, MSN, PHN, CNL is an Associate Adjunct Professor at the University of California, Los Angeles School of Nursing in Los Angeles, California, United States.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the University of California Irvine (UCI), CRAFT COVID Grant.
ORCID iD: Adeline M. Nyamathi  https://orcid.org/0000-0003-4979-6620
https://orcid.org/0000-0003-4979-6620
Supplemental Material: Supplemental material for this article is available online.
References
- Albon D., Soper M., Haro A. (2020). Potential implications of the COVID-19 pandemic on the homeless population. Chest, 158(2), 477–478. 10.1016/j.chest.2020.03.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews J. O., Cox M. J., Newman S. D., Gillenwater G., Warner G., Winkler J. A., White B., Wolf S., Leite R., Slaughter S. (2013). Training partnership dyads for community-based participatory research: Strategies and lessons learned from the community engaged scholars program. Health Promotion Practice, 14(4), 524–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertram F., Heinrich F., Fröb D., Wulff B., Ondruschka B., Püschel K., König H.-H., Hajek A. (2021). Loneliness among homeless individuals during the first wave of the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 18(6), 3035. https://www.mdpi.com/1660-4601/18/6/3035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S., Witkiewitz K., Clifasefi S. L., Grow J., Chawla N., Hsu S. H., Carroll H. A., Harrop E., Collins S. E., Lustyk M. K., Larimer M. E. (2014). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry, 71(5), 547–556. 10.1001/jamapsychiatry.2013.4546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers For Disease Control and Prevention. (2020, December). Increase in fatal drug overdoses across the United States driven by synthetic opioids before and during the covid-19 pandemic. Author. https://emergency.cdc.gov/han/2020/han00438.asp
- Centers For Disease Control and Prevention. (2021, March). About synthetic cannabinoids. Author. https://www.cdc.gov/nceh/hsb/chemicals/sc/About.html [Google Scholar]
- Costa M., Pavlo A., Reis G., Ponte K., Davidson L. (2020). COVID-19 concerns among persons with mental illness. Psychiatric Services, 71(11), 1188–1190. 10.1176/appi.ps.202000245 [DOI] [PubMed] [Google Scholar]
- Culhane D., Treglia D., Steif K., Kuhn R., Byrne T. (2020). Estimated emergency and observational/quarantine capacity need for the US homeless population related to COVID-19 exposure by county; projected hospitalizations, intensive care units and mortality. UCLA: Campuswide Homelessness Initiative. https://escholarship.org/uc/item/9g0992bm
- Davis-Berman J. (2011). Older women in the homeless shelter: Personal perspectives and practice ideas. Journal of Women and Aging, 23(4), 360–374. 10.1080/08952841.2011.611391 [DOI] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction. (2020, March). EMCDDA update on the implications of COVID-19 for people who use drugs (PWUD) and drug service providers. European Union. Author. https://www.emcdda.europa.eu/system/files/publications/12879/emcdda-covid-update-1-25.03.2020v2.pdf [Google Scholar]
- Ellsworth J. T. (2022). Spice, vulnerability, and victimization: Synthetic cannabinoids and interpersonal crime victimization among homeless adults. Substance Abuse, 43(1), 32–38. 10.1080/08897077.2019.1686725 [DOI] [PubMed] [Google Scholar]
- Farhoudian A., Baldacchino A., Clark N., Gerra G., Ekhtiari H., Dom G., Mokri A., Sadeghi M., Nematollahi P., Demasi M., Schütz C. G., Hash-Emian S. M., Tabarsi P., Galea-Singer S., Carrà G., Clausen T., Kouimtsidis C., Tolomeo S., Radfar S. R., Razaghi E. M. (2020, March–April). COVID-19 and substance use disorders: Recommendations to a comprehensive healthcare response. An international society of addiction medicine practice and policy interest group position paper. Basic and Clinical Neuroscience, 11(2), 133–150. 10.32598/bcn.11.covid19.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel S., Geddes J. R., Kushel M. (2014). The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet, 384(9953), 1529–1540. 10.1016/S0140-6736(14)61132-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenley V. M. (2021) Everyday citizenship and COVID-19: “Staying at home” while homeless. Administrative Theory & Praxis, 43(2), 245–257. 10.1080/10841806.2020.1825600 [DOI] [Google Scholar]
- Fitzpatrick K. M. (2017). How positive is their future? Assessing the role of optimism and social support in understanding mental health symptomatology among homeless adults. Stress and Health Journal of the International Society for the Investigation of Stress, 33(2), 92–101. 10.1002/smi.2676 [DOI] [PubMed] [Google Scholar]
- Fuchs J. D., Carter H. C., Evans J., Graham-Squire D., Imbert E., Bloome J., Fann C., Skotnes T., Sears J., Pfeifer-Rosenblum R., Moughamian A., Eveland J., Reed A., Borne D., Lee M., Rosenthal M., Jain V., Bobba N., Kushel M., Kanzaria H. K. (2021). Assessment of a hotel-based COVID-19 isolation and quarantine strategy for persons experiencing homelessness. JAMA Network Open, 4(3), e210490. 10.1001/jamanetworkopen.2021.0490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfin D. R., Morisky D., Shin S. S., Salem B., Yadav K., Deguzman R., Harvey G., Adams I., Halas K., Chang A., White K., Wu J., Nyamathi A. M. (2022). Correlates of depression and anxiety among homeless adults with latent tuberculosis infection. Journal of Health Psychology, 27(2), 494–501. 10.1177/1359105320956693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray P., Ralphs R., Williams L. (2021). The use of synthetic cannabinoid receptor agonists (SCRAs) within the homeless population: Motivations, harms and the implications for developing an appropriate response. Addiction Research & Theory, 29(1), 1–10. 10.1080/16066359.2020.1730820 [DOI] [Google Scholar]
- Hajek A., Bertram F., van Rüth V., Kretzler B., Püschel K., Heinrich F., König H. H. (2021). Prevalence and factors associated with fear of COVID-19 among homeless individuals during the COVID-19 pandemic: Evidence from the hamburg survey of homeless individuals. Risk Management and Healthcare Policy, 14, 2689–2695. 10.2147/RMHP.S317039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton I. (2020, March 16). Covid-19—Are we rationing who we care about? BMJ Opinion. https://blogs.bmj.com/bmj/2020/03/16/ian-hamilton-covid-19-are-we-rationing-who-we-care-about/
- Heimer R., McNeil R., Vlahov D. (2020). A community responds to the COVID-19 pandemic: A case study in protecting the health and human rights of people who use drugs. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 97(4), 448–456. 10.1007/s11524-020-00465-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoch C. (2000). Sheltering the homeless in the US: Social improvement and the continuum of care. Housing Studies, 15(6), 865–876. [Google Scholar]
- Karb R., Samuels E., Vanjani R., Trimbur C., Napoli A. (2020). Homeless shelter characteristics and prevalence of SARS-CoV-2. The Western Journal of Emergency Medicine, 21(5), 1048–1053. 10.5811/westjem.2020.7.48725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassai S., Pintér J. N., Rácz J., Böröndi B., Tóth-Karikó T., Kerekes K., Gyarmathy V. A. (2017). Assessing the experience of using synthetic cannabinoids by means of interpretative phenomenological analysis. Harm Reduction Journal, 14(1), 9. 10.1186/s12954-017-0138-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R., Folkman S. (1984). Stress, appraisal and coping. Springer. [Google Scholar]
- Los Angeles County Department of Public Health. (2021. a). Deaths increase among people experiencing homelessness, drug overdose is leading cause with greatest increase county homeless mortality prevention initiative places renewed emphasis on drug-related deaths. Author. http://publichealth.lacounty.gov/phcommon/public/media/mediapubhpdetail.cfm?prid=2900
- Los Angeles County Department of Public Health. (2021. b). Guidence for homeless shelters. Author. http://publichealth.lacounty.gov/media/Coronavirus/docs/homelessness/GuidanceHomelessShelters.pdf [Google Scholar]
- Los Angeles County Department of Public Health. (2021. c). Summary report of COVID-19 in people experiencing homelessness (PEH). Author. http://publichealth.lacounty.gov/media/Coronavirus/docs/SummaryReport_People_Experiencing_Homelessness.pdf
- Los Angeles Homeless Services Authority. (2020). 2020 Greater los angeles homeless count results. Author. https://www.lahsa.org/news?article=726-2020-greater-los-angeles-homeless-count-results [Google Scholar]
- Microsoft 365. (2021). [Computer Software]. https://www.microsoft.com
- National Institute on Drug Abuse. (2020, June). Synthetic cannabinoids (K2/Spice) drugfacts. U.S. Department of Health and Human Services, National Institutes of Health. Retrieved November 24, 2021, from https://www.drugabuse.gov/publications/drugfacts/synthetic-cannabinoids-k2spice
- Nyamathi A. M. (1989). Comprehensive health seeking and coping paradigm. Journal of Advanced Nursing, 14(4), 281–290. 10.1111/j.1365-2648.1989.tb03415.x [DOI] [PubMed] [Google Scholar]
- Nyamathi A. M., Salem B. E., Farabee D., Hall E., Zhang S., Faucette M., Bond D., Yadav K. (2017). Impact of an intervention for recently released homeless offenders on self-reported re-arrest at 6 and 12 months. Journal of Addictive Diseases, 36(1), 60–71. 10.1080/10550887.2016.1147796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A. M., Shin S. S., Smeltzer J., Salem B. E., Yadav K., Ekstrand M. L., Turner S. F., Faucette M. (2017. a). Achieving drug and alcohol abstinence among recently incarcerated homeless women: A randomized controlled trial comparing dialectical behavioral therapy-case management with a health promotion program. Nursing Research, 66(6), 432–441. 10.1097/NNR.0000000000000249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A. M., Wall S. A., Yadav K., Shin S. S., Chang A., Arce N., Cuellar H., Fernando S., White K., Gelberg L., Salem B. E. (2021). Engaging the community in designing a Hepatitis C virus treatment program for adults experiencing homelessness. Qualitative Health Research, 31(11), 2069–2083. 10.1177/10497323211021782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkes T., Carver H., Masterton W., Falzon D., Dumbrell J., Grant S., Wilson I. (2021). ‘They already operated like it was a crisis, because it always has been a crisis’: A qualitative exploration of the response of one homeless service in Scotland to the COVID-19 pandemic. Harm Reduction Journal, 18(1), 26. 10.1186/s12954-021-00472-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patanwala M., Tieu L., Ponath C., Guzman D., Ritchie C., Kushel M. (2018). Physical, psychological, social, and existential symptoms in older homeless-experienced adults: An observational study of the hope home cohort. Journal of General Internal Medicine, 33(5), 635–643. 10.1007/s11606-017-4229-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pottie K., Kendall C. E., Aubry T., Magwood O., Andermann A., Salvalaggio G., Ponka D., Bloch G., Brcic V., Agbata E., Thavorn K., Hannigan T., Bond A., Crouse S., Goel R., Shoemaker E., Wang J. Z. J., Mott S., Kaur H., . . . Tugwell P. (2020). Clinical guideline for homeless and vulnerably housed people, and people with lived homelessness experience. Canadian Medical Association Journal, 192(10), E240–E254. 10.1503/cmaj.190777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncero C., Vicente-Hernández B., Casado-Espada N. M., Aguilar L., Gamonal-Limcaoco S., Garzón M. A., Martínez-González F., Llanes-Álvarez C., Martínez R., Franco-Martín M., Álvarez-Navares A. (2020). The impact of COVID-19 pandemic on the castile and leon addiction treatment network: A real-word experience. Frontiers in Psychiatry, 11, 575755. 10.3389/fpsyt.2020.575755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roze M., Vandentorren S., van der Waerden J., Melchior M. (2018). Factors associated with depression among homeless mothers. Results of the ENFAMS survey. Journal of Affective Disorders, 229, 314–321. 10.1016/j.jad.2017.12.053 [DOI] [PubMed] [Google Scholar]
- Sachdev D., Mara E., Hsu L., Scheer S., Rutherford G., Enanoria W., Gandhi M. (2021). COVID-19 susceptibility and outcomes among people living with HIV in San Francisco. Journal of Acquired Immune Deficiency Syndromes (1999), 86(1), 19–21. 10.1097/QAI.0000000000002531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saldaña J. (2009). The coding manual for qualitative researchers. SAGE. [Google Scholar]
- Schlotfeldt R. M. (1981). Nursing in the future. Nursing Outlook, 29(5), 295–301. [PubMed] [Google Scholar]
- Shenton A. (2004). Strategies for ensuring trustworthiness in qualitative research projects. Education for Information, 22, 63–75. 10.3233/EFI-2004-22201 [DOI] [Google Scholar]
- Suls J., Fletcher B. (1985). The relative efficacy of avoidant and nonavoidant coping strategies: A meta-analysis. Health Psychology, 4(3), 249–288. 10.1037/0278-6133.4.3.249 [DOI] [PubMed] [Google Scholar]
- Thompson N. J., Fiorillo D., Rothbaum B. O., Ressler K. J., Michopoulos V. (2018). Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. Journal of Affective Disorders, 225, 153–159. 10.1016/j.jad.2017.08.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinland A., Boyer L., Loubière S., Greacen T., Girard V., Boucekine M., Fond G., Auquier P. (2018). Victimization and posttraumatic stress disorder in homeless women with mental illness are associated with depression, suicide, and quality of life. Neuropsychiatric Disease and Treatment, 14, 2269–2279. 10.2147/NDT.S161377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong M., Tieu L., Lee C., Ponath C., Guzman D., Kushel M. (2019). Factors associated with food insecurity among older homeless adults: Results from the HOPE HOME study. Journal of Public Health, 41(2), 240–249. 10.1093/pubmed/fdy063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tringale R., Subica A. M. (2021). COVID-19 innovations in medication for addiction treatment at a Skid Row syringe exchange. Journal of Substance Abuse Treatment, 121, 108181. 10.1016/j.jsat.2020.108181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J., Wilson M. (2020). COVID-19: A potential public health problem for homeless populations. The Lancet Public Health, 5(4), e186. 10.1016/S2468-2667(20)30053-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker J. S., D’Amico E. J., Pedersen E. R., Garvey R., Rodriguez A., Klein D. J. (2020). Behavioral health and service usage during the COVID-19 pandemic among emerging adults currently or recently experiencing homelessness. Journal of Adolescent Health, 67(4), 603–605. 10.1016/j.jadohealth.2020.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vardavas C. I., Nikitara K. (2020). COVID-19 and smoking: A systematic review of the evidence. Tobacco Induced Diseases, 18, 20–20. 10.18332/tid/119324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasylyeva T. I., Smyrnov P., Strathdee S., Friedman S. R. (2020). Challenges posed by COVID-19 to people who inject drugs and lessons from other outbreaks. Journal of the International AIDS Society, 23(7), e25583. 10.1002/jia2.25583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel M., Nikoo M., Nikoo N., Schütz C. G., Walter M., Somers J., Krausz M. (2019). Association of substance use patterns with psychiatric disorders in homeless persons with psychiatric disorders in vancouver. International Journal of Mental Health and Addiction, 17(5), 1200–1213. 10.1007/s11469-018-0040-4 [DOI] [Google Scholar]
- Volkow N. D. (2020). Collision of the COVID-19 and addiction epidemics. Annals of Internal Medicine, 173(1), 61–62. 10.7326/M20-1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J. Z., Mott S., Magwood O., Mathew C., Mclellan A., Kpade V., Gaba P., Kozloff N., Pottie K., Andermann A. (2019). The impact of interventions for youth experiencing homelessness on housing, mental health, substance use, and family cohesion: A systematic review. BMC Public Health, 19(1), 1528. 10.1186/s12889-019-7856-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson J., Crawley J., Kane D. (2016). Social exclusion, health and hidden homelessness. Public Health, 139, 96–102. 10.1016/j.puhe.2016.05.017 [DOI] [PubMed] [Google Scholar]
- Wu G., Feder A., Cohen H., Kim J. J., Calderon S., Charney D. S., Mathé A. A. (2013). Understanding resilience. Frontiers in Behavioral Neuroscience, 7, 10. 10.3389/fnbeh.2013.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoom Inc. (2021). Using audio transcription for cloud recordings. Author. https://support.zoom.us/hc/en-us/articles/115004794983-Using-audio-transcription-for-cloud-recordings- [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-gqn-10.1177_23333936221108712 for Perceptions of Homeless Adults and Their Providers on Coping With the Impact of COVID-19 Pandemic on Mental Health, Substance Use, and Harm Reduction Services by Adeline M. Nyamathi, Lillian Gelberg, Darlene Lee, Nicholas Arce, Alexandria Patten-Jones, Kartik Yadav, Maniyah Goodwine, Mitra Alikhani, Maritas Yao, Alicia H. Chang and Benissa E. Salem in Global Qualitative Nursing Research