Abstract
Background
In the US, medical costs for cancer patients have grown from $27 billion in 1990 to $174 billion in 2020. The increased financial strain that cancer patients and survivors endure is referred to as financial toxicity.
Objective
To quantify the relationship between indicators of financial toxicity and health utilization and quality of life in patients ever diagnosed with cancer.
Methods
Adult cancer patients and survivors in 2017 were identified using the Medical Expenditure Panel Survey. Multiple logistic regression models were used to quantify the relationship between three financial toxicity exposures (concern for keeping an income, paying large medical bills, and going into debt or borrowing money) and two discrete outcomes of being able to purchase prescriptions and often worrying that cancer would worsen or come back.
Results
This study assessed 609 respondents. After survey weighting was applied, that represented 16,215,673 individuals. Patients who reported concern for keeping an income were at 2.91 (95% Confidence Interval [CI], 1.16 to 7.31) and 2.97 (95% CI, 2.01 to 2.67) times increased odds to report avoiding purchase of prescriptions and worry of cancer status, respectively, versus those who did not. Patients who reported worry about paying large medical bills were at 4.46 (95% CI, 2.15 to 9.24) and 2.80 (95% CI, 1.98 to 3.96) times increased odds to report avoiding purchase of prescriptions and worry of cancer status, respectively, versus those who did not. Patients who reported borrowing money or going into debt were at 3.04 (95% CI, 1.19 to 7.76) and 2.42 (95% CI, 1.54 to 3.18) times increased odds to report avoiding purchase of prescriptions and worry of cancer status, respectively, versus those who did not.
Conclusions
Financial toxicity is associated with decreased prescription utilization and quality of life in the form of excessive worry among cancer patients including cancer survivors.
Keywords: Financial toxicity, Cancer, Value-based pricing
Highlights
-
•
Background: In the U.S., medical costs of cancer have increased from $27 billion in 1990 to $174 billion in 2020.
-
•
Patients with cancer carry the burden of paying higher out-of-pocket costs for their care than those without cancer.
-
•
The increased financial strain that patients and survivors with cancer is referred to as financial toxicity.
-
•
Findings: Patients and survivors with cancer who reported ever being concerned about income, ever being worried about paying large medical bills, or ever going into debt or had a family member go into debt were at higher odds to report not receiving prescriptions and worrying about their cancer recurring or worsening than those who did not.
1. Background
Cancer was the most expensive chronic condition in the U.S., averaging $16,346 per person among adults 18 years and older in 2019.1 Financing oncology treatment will only grow more challenging as recently approved cellular oncology therapies, including chimeric antigen receptor T cell therapies, have prices reaching $475,000 per treatment.2 Given the extensive pipeline of biologics now emerging on the market, these costs are expected to increase markedly in the near term and beyond.3 Many novel cancer therapies are oral chemotherapeutic agents as well.4 Oral agents increasingly shift the cost burden onto patients through higher deductibles and out-of-pocket costs.5 Medical costs of cancer have climbed from $27 billion in 1990 to approximately $174 billion by the close of 2020.6,7 Consequently, patients and cancer survivors carry a burden of out-of-pocket costs that approach four times higher than the average healthcare expenditures of patients without cancer, which was $4484 per person.8 In addition to clinician visits, patients and survivors with cancer often require an array of high-cost medical services, including hospitalizations, surgeries, chemotherapy, radiation therapy, immunotherapy, and supportive care. When utilization of these resources contributes to a feeling of psychological or physical distress for patients, survivors, and their families, it is termed ‘financial toxicity’.9,10
Financial toxicity manifests as a wide scale of consequences, ranging from worrying about paying monthly bills to sacrificing life savings and experiencing bankruptcy, with effects that may last well beyond the treatment period.11 Financial toxicity in patients and survivors with cancer results in compensatory behaviors by patients that include borrowing money, spending less on leisure activities, selling valuable assets, and moving to low-cost housing to pay medical bills.11 Between 1997 and 2007, approximately half of Medicare beneficiaries with cancer spent at least 10% of their income on out-of-pocket costs alone, with 27% of cancer patients having spent 20% of their income on treatment.12 Recent studies have also linked financial harm with a greater risk of mortality and an overall decrease in well-being.13
The objectives of this analysis were to quantify the relationship between indicators of financial distress and prescription utilization and concern about cancer recurring in patients ever diagnosed with cancer in the U.S. It was hypothesized that patients and survivors with cancer who suffered from financial toxicity were more likely to avoid purchasing their prescriptions and excessively worry about their cancer recurring or progressing compared to those who did not suffer from financial toxicity on a national level using a validated, longitudinal dataset representative of the U.S.
2. Methods
2.1. Data source
This retrospective cohort study used the most current U.S. data available, investigating financial toxicity on patients and survivors with cancer in the Medical Expenditure Panel Survey (MEPS). This is a national representative collection of surveys conducted by the Agency for Healthcare Research and Quality (AHRQ) of the Department of Health and Human Services, which describes demographics, health status, healthcare coverage, use, and expenditure in the civilian non-institutionalized U.S. population.14 MEPS contains three surveys: the Household Component (MEPS-HC), the Medical Provider Component (MEPS-MPC), and the Insurance Component (MEPS-IC). These 3 surveys are generated by gathering data from individuals in U.S. households and supplementing them with surveys from the individual respondent's providers. Comprehensively, all 3 surveys affirm that MEPS is among the most complete data sources on cost and healthcare utilization in the U.S. and on U.S. health insurance coverage.15
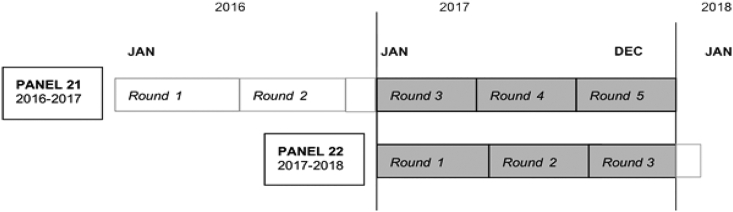
MEPS utilizes a complex sampling design to provide data routinely used to derive national estimates of the U.S. The sampling design utilized stratification, clustering, and multiple stages of selection to ensure accurate measurements in minority and underserved populations, including those with low-income.16 Survey weights were included in the data on a person-level, family-level, or both to account for nonresponse and were used to estimate the 2017 U.S. population. In the survey, patients were interviewed as a cohort over a 2-year time frame, with each cohort referred to as a “panel.” A panel is not followed beyond this 2 year time window and thus represents that specific era. A new panel occurs at the beginning of every calendar year. The panels were interviewed at five separate time points, referred to as “rounds.” Study data (2017 Full Year Consolidated File) consisted of surveys that were completed during Rounds 3–5 of Panel 21 and Rounds 1–3 of Panel 22, which covered the calendar year 2017 (Fig. 1).17
Fig. 1.
MEPS 2017 Full Year Consolidated File - Schematic for MEPS survey study.
The Full Year Consolidated File for 2017 captures healthcare utilization in all of 2017. It includes the beginning rounds of Panel 22 and end rounds of Panel 21
2.2. Study population
The sample included adults 18 years and older living in the U.S. and who responded to the Cancer Self-Administered Questionnaire (CSAQ) portion of the MEPS survey in 2017. The CSAQ was only given to respondents who responded ‘yes’ to if they had ‘ever been told by a doctor or other health professional that they were diagnosed with cancer’.15 The CSAQ included questions related to cancer history, effects of cancer and its treatment on finances, medical care for cancer, effects of cancer on life in general, changes to work schedule due to cancer, caregiver needs, and experiences with health insurance.16 AHRQ created this questionnaire in collaboration with the National Cancer Institute.18 Respondents diagnosed with non-melanoma skin cancers were not classified as cancer survivors and excluded from analyses due to the low-intensity treatment regimen, consistent with previous studies.19
2.3. Exposure
This study analyzed 3 separate situations where patients were exposed to financial toxicity from the time of their cancer diagnosis through study data end in 2017: (1) ‘Ever concerned about keeping a job and income or that earnings would be limited?’, (2) ‘Ever worried about paying large medical bills?’, and (3) ‘Ever gone into debt or borrowed money or have a family member go into debt or borrow money?’
2.4. Primary outcomes
Two different outcomes were analyzed based on yes or no responses to the following questions: 1) “Were you unable to receive prescription medications in 2017?” and 2) “Did you often worry that your cancer would come back or get worse?”
2.5. Statistical analysis
Summary descriptive statistics were assessed. The continuous variable, age, was summarized using mean and standard deviation (S.D.). Categorical variables were assessed using chi-square test statistics to determine whether the responses to financial toxicity questions varied by demographic.
Survey-weighted multiple logistic regression was used to quantify the relationship between each individual exposure and each separate outcome using odds ratios (OR). Analyses were adjusted for age, race, gender, marital status, and census region as these variables could influence those who experienced financial toxicity. All analyses were conducted in RStudio (Boston, MA) with an α-level < 0.05 for all tests using the R survey package (Lumley, 2020).20
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement for cohort designs was used for this evaluation.21
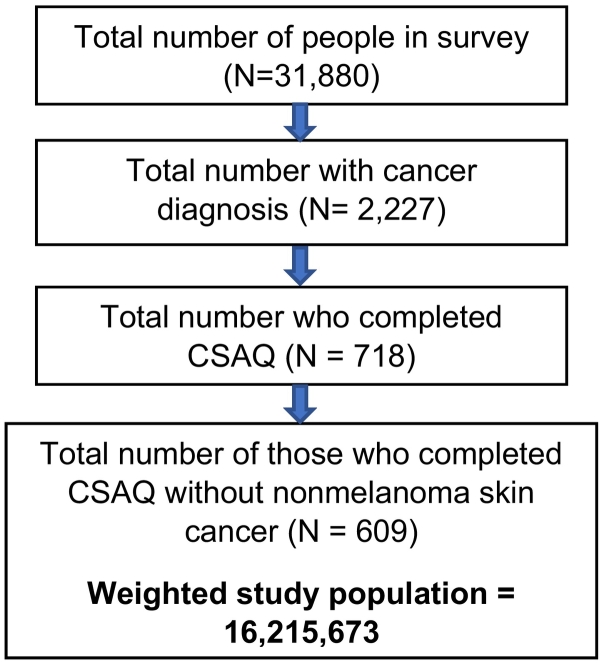
3. Results
In total, 718 unweighted MEPS participants completed the CSAQ questionnaire in 2017. After excluding respondents who indicated a diagnosis of non-melanoma skin cancers, 609 unweighted patients and survivors with cancer met the inclusion criteria. After survey-weighting was applied, the 609 patients and survivors with cancer represented 16,215,673 patients in the U.S. (Fig. 2). The average age was 65 years old (SD = 0.66 years), with 8,952,564 patients over the age of 65 (55.2%). The majority of patients included 8,965,559 females (55.3%), 13,139,257 non-Hispanic whites (81.0%), 9,087,148 married individuals (56.0%), 6,760,410 individuals educated to the highest degree of a high school diploma (41.7%), and 6,059,088 individuals who lived in the south (37.4%) (Table 1). There was a significant difference in age and marital status for those who were ever concerned about keeping an income, ever worried about paying large medical bills, and had ever gone into debt or borrowed money or had a family member do the same (Table 1).
Fig. 2.
Number of individuals at each stage of the study.
Table 1.
Descriptive statistics for cancer survivors and patients by financial concern exposure.
| Ever concerned about keeping an income? |
Ever worried about paying large medical bills? |
Ever borrowed money/gone into debt or have a family member do the same? |
|||||
|---|---|---|---|---|---|---|---|
| Factor | Weighted CSAQ Number of Respondents, N = 16,215,673 (%) | Yes (%) | P-Value | Yes (%) | P-Value | Yes (%) | P-Value |
| Gender | |||||||
| Female | 8,965,559 (55.3%) | 1,585,874 (18%) | 0.06 | 1,507,353 (21%) | 0.27 | 746,845 (8%) | 0.09 |
| Male | 7,250,114 (44.7%) | 1,801,171 (26%) | 2,247,202 (26%) | 359,706 (5%) | |||
| Age Group | |||||||
| 18–64 | 7,263,108 (44.8%) | 2,542,276 (36%) | <0.01 | 2,728,979 (38%) | <0.01 | 862,047 (12%) | <0.01 |
| 65 and older | 8,952,564 (55.2%) | 844,769 (10%) | 1,025,575 (12%) | 244,504 (3%) | |||
| Race | |||||||
| Hispanic | 1,087,741 (6.7%) | 277,062 (25%) | 0.6 | 367,628 (34%) | 0.52 | 122,254 (11%) | 0.59 |
| Non-Hispanic White Only | 13,139,257 (81.0%) | 2,599,602 (21%) | 2,863,889 (23%) | 896,578 (6%)a | |||
| Non-Hispanic Black Only | 1,146,489 (7.1%) | 255,337 (24%) | 523,037 (27%)⁎ | ||||
| Non-Hispanic Other Race or Multiple Race | 842,186 (5.2%) | 255,045 (30%) | 0 (0%) | ||||
| Marital Status | |||||||
| Married | 9,087,148 (56.0%) | 1,773,633 (20%) | <0.01 | 1,974,016 (22%) | 0.02 | 608,053 (7%) | <0.01 |
| Widowed | 2,856,261 (17.6%) | 209,017 (8%) | 435,297 (16%) | 185,174 (4%)a | |||
| Divorced | 2,655,966 (16.4%) | 774,796 (31%) | 670,323 (27%) | ||||
| Never married or Separated | 1,616,298 (10%) | 629,597 (41%) | 674,918 (42%) | 313,325 (19%) | |||
| Highest Degree Reported | |||||||
| GED or No Degree | 2,080,033 (12.9%) | 331,282 (17%) | 0.68 | 443,697 (22%) | 0.52 | 135,727 (7%) | 0.68 |
| High School Diploma | 6,760,410 (41.7%) | 1,346,945 (21%) | 1,442,113 (22%) | 507,807 (8%) | |||
| Bachelor's Degree | 3,027,615 (18.7%) | 636,819 (21%) | 742,672 (25%) | 463,017 (6%)a | |||
| Master's Degree or Doctorate Degree | 2,693,799 (16.6%) | 515,637 (19%) | 331,858 (17%) | ||||
| Other Degree | 1,610,163 (10.1%) | 549,125 (35%) | 794,214 (35%) | ||||
| Region | |||||||
| South | 6,059,088 (37.4%) | 1,343,918 (23%) | 0.904 | 1,380,347 (23%) | 0.80 | 210,037 (4%) | 0.12 |
| West | 3,404,211 (21.0%) | 602,430 (18%) | 677,187 (21%) | 443,672 (7%)a | |||
| Northeast | 2,961,144 (18.3%) | 571,122 (20%) | 632,778 (22%) | ||||
| Midwest | 3,791,229 (23.3%) | 869,574 (24%) | 1,064,242 (29%) | 452,842 (12%) | |||
Cells were merged because per MEPS guidelines, published estimates should be based on the unweighted sample of at least 60 persons for the subgroup of interest.
The survey question regarding if patients were ‘ever concerned about keeping their job or that earnings would be limited’ had a 96% response rate, of which 22% answered ‘Yes.’ Patients were at 2.91 times increased odds to report not being able to pick up prescriptions (95% Confidence Interval [CI], 1.16 to 7.31) and 2.97 times increased odds to report worry about their cancer coming back or worsening (95% CI, 2.01 to 2.67) if they were concerned about keeping their job versus those who were not (Table 2).
Table 2.
Odds ratios for financial toxicity exposures and outcomes.a
| Outcomes |
|||
|---|---|---|---|
| Were you unable to receive prescription medications (in 2017)? | Did you often worry that your cancer would come back or get worse? | ||
| Exposures | Ever concerned about keeping your job and income or that earnings will be limited? | 2.91 [95% CI, 1.16–7.31] | 2.97 [95% CI, 2.01–2.67] |
| Were you ever worried about paying large medical bills? | 4.46 [95% CI, 2.15–9.24] | 2.80 [95% CI, 1.98–3.96] | |
| Did you or anyone in your family had to borrow money or go into debt? | 3.04 [95% CI, 1.19–7.76] | 2.42 [95% CI, 1.54–3.18] | |
Analyses were adjusted for age, race, gender, marital status, and census region.
The survey question regarding if patients were ‘ever worried about paying large medical bills’ had a 97% response rate, of which 22% answered ‘Yes.’ Patients were at 4.46 times increased odds to report not being able to pick up prescriptions (95% CI, 2.15 to 9.24) and 2.8 times increased odds to report worry about their cancer coming back or worsening (95% CI, 1.98 to 3.96) if they were concerned about paying large medical bills versus those who were not (Table 2).
The survey question regarding if patients had ‘ever gone into debt or borrowed money or had a family member go into debt or borrow money’ had a 97% response rate, of which 7% responded ‘Yes.’ Patients were at 3.04 times increased odds to report not being able to pick up prescriptions (95% CI, 1.19 to 7.76) and 2.42 times increased odds to report worry about their cancer coming back or worsening (95% CI, 1.54 to 3.18) if they had ever gone into debt or borrowed money or had a family member go into debt or borrow money versus those who did not (Table 2).
4. Discussion
This analysis of patients and cancer survivors in the U.S. demonstrated that those who ever suffered from financial toxicity were more likely to avoid buying necessary prescriptions and experienced excessive worry about their condition in 2017 compared to those who did not ever suffer from financial toxicity. These findings demonstrate that a considerable number of patients and survivors with cancer forgo necessary medical treatment due to financial distress. Financial toxicity has been reported in 9.5 million newly diagnosed patients with cancer in the U.S. over the age of 50 years old between 2000 and 2012, and some reports indicated that financial toxicity was even more likely to occur in people 18 to 64 years old.22 These statistics are consistent with this study's results and confirm the presence of financial toxicity in people of all ages in the U.S. for patients and survivors.
Nonadherence to medication includes skipping doses, taking less medication than prescribed, and avoiding the purchase of refills.23 This analysis explicitly examined avoiding the purchase of medications due to financial considerations. Due to medical costs, these patients are forced to forego necessary life-preserving treatment.24 The increased availability of oral chemotherapeutic agents increases the risk of nonadherence to essential medications to a greater extent.4 Nonadherence has been shown to decrease survival rates, increase treatment failures, elevate cancer recurrence, raise healthcare costs, and contribute to up to two-thirds of all medication-related hospitalizations.25
Patients' quality of life is impacted due to cancer treatment-related costs.26 Excessive worry about cancer recurring or progressing has been associated in prior research with depressed mood contributing to an overall decrease in quality of life.27 Previous studies have demonstrated associations between depleted quality of life with survival outcomes in malignancy.28 The willingness to give up medication therapy to save on expenses for patients may further contribute to worry about cancer recurrence or progression since taking less medication than prescribed could translate to treatment failure.25
Policy measures to avoid financial toxicity and its effects on a larger scale in cancer patients are increasingly important. Some states have enacted reforms to reduce rapidly increasing prescription drug costs, including chemotherapeutic agents.29 In April 2017, the State of New York instituted a value-based pricing program and became the first public payer in the U.S. to allow limits on Medicaid prescription drug costs based on their therapeutic effect.29 Such value assessment and pricing negotiations could set the stage for reducing drug costs for Medicaid patients in New York, potentially benefiting the cancer population.
Near-term strategies to reduce financial toxicity exist. The American Cancer Society provides resources for patients with or without health insurance who struggle to pay their medical bills.30 There are also resources that connect patients and cancer survivors to national service organizations that provide financial help.31 Such financial assistance can be used towards co-pays, transportation, home care, and even child care.32 This analysis found that younger people and those who were not married were associated with increased worry about paying medical bills. This is consistent with other published studies that increased age and marital status both correlate with elevated income, particularly for those over age 65.33,34
Limitations to this study exist. While the MEPS database is a national, validated resource routinely used by the federal government for policy-level analysis, the person-level data is based on self-reported responses. While components of MEPS responses are verified by requesting data from hospitals, physicians, home health care providers, and pharmacies identified by respondents, the potential for reporter error exists.18 The CSAQ component of MEPS was limited to asking if patients were unable to purchase prescription medication patients and does not record the specific medications that were skipped. This study successfully examined the exposures to financial toxicity before 2017 to determine an association. However, given the observational nature of this study, a causal relationship cannot be confirmed.
5. Conclusions
Financial toxicity is associated with decreased prescription utilization and reduced quality of life in the form of excessive worry among cancer patients and survivors. Future research will utilize population-level data to measure the impact of ongoing policies to mitigate financial toxicity on patient outcomes, including value-based pricing policies and cost mitigation interventions.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Previous presentations
Academy of Managed Care Pharmacy Annual Meeting 2020 Virtual Poster Hall.
Credit authorship contribution statement
Kelly Chan: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft. Aryana Sepassi: Writing – review & editing. Ila M. Saunders: Writing – review & editing. Aaron Goodman: Writing – review & editing. Jonathan H. Watanabe: Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare no relevant conflicts of interest or financial relationships.
Footnotes
This retrospective database study project #160343XX was issued exempt status by the UC San Diego Human Research Patient Protections Program Institutional Review Board.
References
- 1.Soni A. Statistical Brief #471: Top Five Most Costly Conditions among Adults Age 18 and Older, 2012: Estimates for the U.S. Civilian Noninstitutionalized Population. Published online 2012:6. [PubMed]
- 2.Graham C., Jozwik A., Pepper A., Benjamin R. Allogeneic CAR-T cells: more than ease of access? Cells. 2018;7(10):155. doi: 10.3390/cells7100155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cancer Data and Statistics | CDC https://www.cdc.gov/cancer/dcpc/data/index.htm Published August 10, 2020. Accessed September 23, 2020.
- 4.Wong S.F., Bounthavong M., Nguyen C.P., Chen T. Outcome assessments and cost avoidance of an Oral chemotherapy management clinic. J Natl Compr Cancer Netw. 2016;14(3):279–285. doi: 10.6004/jnccn.2016.0033. [DOI] [PubMed] [Google Scholar]
- 5.Tran G., Zafar S.Y. Financial toxicity and implications for cancer care in the era of molecular and immune therapies. Ann Transl Med. 2018;6(9):166. doi: 10.21037/atm.2018.03.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerr D.J. Oxford University Press; 2016. Oxford Textbook of Oncology. [Google Scholar]
- 7.global-cancer-facts-and-figures-4th-edition.pdf https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/global-cancer-facts-and-figures/global-cancer-facts-and-figures-4th-edition.pdf Accessed September 25, 2020.
- 8.Park J., Look K.A. Health care expenditure burden of Cancer Care in the United States. Inquiry. 2019;56 doi: 10.1177/0046958019880696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Financial Toxicity (Financial Distress) and Cancer Treatment (PDQ®)–Patient Version - National Cancer Institute https://www.cancer.gov/about-cancer/managing-care/track-care-costs/financial-toxicity-pdq Published June 29, 2017. Accessed July 3, 2020. [PubMed]
- 10.Yabroff K.R., Lund J., Kepka D., Mariotto A. Economic burden of cancer in the U.S.: estimates, projections, and future research. Cancer Epidemiol Biomark Prev. 2011;20(10):2006–2014. doi: 10.1158/1055-9965.EPI-11-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chino F., Peppercorn J.M., Rushing C., et al. Going for broke: a longitudinal study of patient-reported financial sacrifice in cancer care. J Oncol Pract. 2018;14(9):e533–e546. doi: 10.1200/JOP.18.00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davidoff A.J., Erten M., Shaffer T., et al. Out-of-pocket health care expenditure burden for Medicare beneficiaries with cancer. Cancer. 2013;119(6):1257–1265. doi: 10.1002/cncr.27848. [DOI] [PubMed] [Google Scholar]
- 13.Financial Toxicity and Cancer Treatment (PDQ®)–Health Professional Version - National Cancer Institute https://www.cancer.gov/about-cancer/managing-care/track-care-costs/financial-toxicity-hp-pdq Published August 26, 2016. Accessed July 3, 2020. [PubMed]
- 14.Cohen J.W., Monheit A.C., Beauregard K.M., et al. The medical expenditure panel survey: a national health information resource. Inquiry. 1996;33(4):373–389. [PubMed] [Google Scholar]
- 15.Medical Expenditure Panel Survey (MEPS) http://www.ahrq.gov/cpi/about/otherwebsites/meps.ahrq.gov/index.html Accessed July 5, 2020.
- 16.Medical Expenditure Panel Survey Computing Standard Errors for MEPS Estimates https://meps.ahrq.gov/survey_comp/standard_errors.jsp Accessed July 5, 2020.
- 17.h201doc.pdf https://meps.ahrq.gov/data_stats/download_data/pufs/h201/h201doc.pdf Accessed July 11, 2020.
- 18.Medical Expenditure Panel Survey Survey Questionnaires https://meps.ahrq.gov/survey_comp/survey.jsp Accessed November 7, 2020.
- 19.Kent E.E., Forsythe L.P., Yabroff K.R., et al. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. 2013;119(20):3710–3717. doi: 10.1002/cncr.28262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lumley T. 2020. Survey: Analysis of Complex Survey Samples. [Google Scholar]
- 21.STROBE_checklist_v4_combined.pdf https://www.equator-network.org/wp-content/uploads/2015/10/STROBE_checklist_v4_combined.pdf Accessed June 6, 2021.
- 22.Yabroff K.R., Dowling E.C., Guy G.P., et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259–267. doi: 10.1200/JCO.2015.62.0468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hugtenburg J.G., Timmers L., Elders P.J., Vervloet M., van Dijk L. Definitions, variants, and causes of nonadherence with medication: a challenge for tailored interventions. Patient Prefer Adherence. 2013;7:675–682. doi: 10.2147/PPA.S29549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nekhlyudov L., Madden J., Graves A.J., Zhang F., Soumerai S.B., Ross-Degnan D. Cost-related medication nonadherence and cost-saving strategies used by elderly medicare cancer survivors. J Cancer Surviv. 2011;5(4):395–404. doi: 10.1007/s11764-011-0188-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Puts M.T.E., Tu H.A., Tourangeau A., et al. Factors influencing adherence to cancer treatment in older adults with cancer: a systematic review. Ann Oncol. 2014;25(3):564–577. doi: 10.1093/annonc/mdt433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kale H.P., Carroll N.V. Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among U.S. cancer survivors. Cancer. 2016;122(8):283–289. doi: 10.1002/cncr.29808. [DOI] [PubMed] [Google Scholar]
- 27.Simard S., Savard J. Fear of Cancer recurrence inventory: development and initial validation of a multidimensional measure of fear of cancer recurrence. Support Care Cancer. 2008;17(3):241. doi: 10.1007/s00520-008-0444-y. [DOI] [PubMed] [Google Scholar]
- 28.Sitlinger A., Yousuf Zafar S. Health-related quality of life. Surg Oncol Clin N Am. 2018;27(4):675–684. doi: 10.1016/j.soc.2018.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Value-Based Pricing and State Reform of Prescription Drug Costs | Clinical Pharmacy and Pharmacology | JAMA | JAMA Network https://jamanetwork.com/journals/jama/article-abstract/2643729 Accessed September 23, 2020. [DOI] [PubMed]
- 30.If You Have Problems Paying a Medical Bill https://www.cancer.org/treatment/finding-and-paying-for-treatment/understanding-financial-and-legal-matters/managing-costs/if-you-have-problems-paying-a-medical-bill.html Accessed September 23, 2020.
- 31.Cancer.Net | Oncologist-approved cancer information from the American Society of Clinical Oncology https://www.cancer.net/ Accessed September 23, 2020.
- 32.Financial Resources Cancer. 2011. https://www.cancer.net/navigating-cancer-care/financial-considerations/financial-resources Net Published June 17. Accessed September 23, 2020.
- 33.Association of marital status and colorectal cancer screening participation in the USA - El-Haddad - 2015 - Colorectal Disease - Wiley Online Library. Accessed March 27, 2022. https://onlinelibrary.wiley.com/doi/abs/10.1111/codi.12926?casa_token=a9nksJHvG0MAAAAA:VSjpiKFqKsC3TmHte0Ru2pzrJV_3FlL8eywhppT8XpbRyrkTxVD0otWeXno-a4skbp7fsKtvU1sSUAO2 [DOI] [PubMed]
- 34.Vandenbroucke G., Zhu H. Aging and wealth inequality. Econ Synop. 2017;2017:2. doi: 10.20955/es.2017.2. [DOI] [Google Scholar]