Abstract
Objective:
Recent reports suggest that exposure to repetitive concussions in sports is associated with an increased risk of symptoms of distress, anxiety and depression, sleep disturbance or substance abuse/dependence (typically referred as symptoms of common mental disorders[CMD]) and of later development of neurodegenerative disease, in particular chronic traumatic encephalopathy (CTE). The primary aim of this study was to explore the relationship between sports career-related concussions and the subsequent occurrence of symptoms of CMD among former male professional athletes retired from football (soccer), ice hockey and rugby (union).
Methods:
Cross-sectional analyses were performed on baseline electronic questionnaires from three prospective cohort studies among former male professional athletes retired from football (soccer), ice hockey and rugby (union). The number of confirmed concussions was examined through a single question, while symptoms of distress, anxiety and depression, sleep disturbance and adverse alcohol use were assessed using validated questionnaires.
Results:
From 1,957 former professional athletes contacted, a total of 576 (29%) completed the questionnaire. Of these, 23% had not incurred a concussion during their career, 34% had two or three, 18% four or five, and 11% six or more concussions. The number of sports career-related concussions was a predictor for all outcome measures (β = 0.072–0.109; P ≤ 0.040). Specifically, former professional athletes who reported a history of four or five concussions were approximately 1.5 times more likely to report symptoms of CMD, rising to a two- to five-fold increase in those reporting a history of six or more sports career-related concussions.
Conclusions:
These data demonstrate an association between exposure to sports concussion and subsequent risk of symptoms of CMD in former professional athletes across a range of contact sports. Further work to explore the association between sports concussion and symptoms of CMD is required; in the meanwhile, strategies for effective risk reduction and improved management appear indicated.
Keywords: Concussions, sports, mental disorders, epidemiology, athletes
Introduction
Concussion is recognized as a complex pathophysiological process induced by biomechanical forces after a direct or transmitted blow to the head resulting in neurological impairment [1]. In recent years, interest in sports concussion has increased, particularly with regard to its immediate, catastrophic complications (i.e. ‘second impact syndrome’), its management, and its association with increased risk of neurodegenerative disease, in particular chronic traumatic encephalopathy (CTE) [2].
At the professional level, the rates of concussion vary across sport and have been consistently rising in recent years. For example, in the comprehensive annual injury surveillance data gathered in English professional rugby, reported concussion incidence has increased from 3 concussions per 1000 player hours in 2005 to 13.4 concussions per 1000 player hours in 2015 [3]. In professional ice hockey, concussion incidence is recorded at 6.5 concussions per 1000 game hours [4,5]. Among professional footballers, fewer concussions have been reported, with the incidence rate ranging between 0.03 and 0.07 concussions per 1000 players hours in men’s European professional football (soccer) [6]. Although the majority of concussions resolve with rest, related symptoms can be prolonged as post-concussion syndrome in about 10–15% of cases [1].
In the longer term, sports career-related concussions have been linked to the occurrence of neurodegenerative diseases among former professional athletes, specifically CTE [7,8]. Of note, studies describing clinical presentation in early stage CTE report behavioral and/or mood disturbance, including depression and suicidality, in the phenotype [9]. Further, retrospective analyses revealed that retired American footballers who reported one or two concussions were 1.5 times more likely to report depression than those with no history of concussion, rising to threefold in retired players reporting three or more sports career-related concussions [10]. A study among former elite rugby players showed that the risk for depressive disorders increased with the number of sports career-related concussions [11]. Recently, studies have reported that symptoms of distress, anxiety and depression, sleep disturbance, or substance abuse/dependence – typically referred as symptoms of common mental disorders (CMD) – are prevalent in former professional players retired from team sports [12,13]. The question whether the number of concussions sustained during a professional career in wider sports contributes to the occurrence of symptoms of CMD remains unanswered.
Therefore, the primary aim of the study was to explore the relationship between sports career-related concussions and the subsequent occurrence of symptoms of CMD (distress, anxiety and depression, sleep disturbance, adverse alcohol use) among former male professional athletes retired from football, ice hockey, and rugby. A secondary aim was to present the difference across sports in relation to the risk to report symptoms of CMD as a consequence of sports career-related concussions.
Methods
Design
Cross-sectional analyses were conducted on baseline questionnaires from three prospective cohort studies in professional football, ice hockey, and rugby. Results of two of these observational studies (football and rugby) have been presented elsewhere [12–14]. Ethical approval for this study was provided by the board of St. Marianna University School of Medicine (2014/04/16; Kawasaki, Japan), the Faculty of Health Sciences Human Research Ethics Committee of the University of Cape Town (642/2014; Cape Town, South Africa), and the Medical Ethics Review Committee of the Academic Medical Center (W15_060#15.0072, W15_171#15.0207; Amsterdam, The Netherlands). The present research was conducted in accordance with the Declaration of Helsinki [15].
Participants
Participants were former male professional athletes retired from football, ice hockey, and rugby recruited from a range of countries (Finland, France, Ireland, Norway, South Africa, Spain, Sweden, Switzerland). In our study, being a former professional athlete meant (1) to have trained in football, ice hockey, or rugby aiming to improve performance/results; (2) to have participated in the top tier professional leagues in football, ice hockey, or rugby; and (3) to have had football, ice hockey, or rugby training and competition as a major professional activity (way of living) [16]. Inclusion criteria for participants were (1) age 50 years or younger at recruitment; (2) male; (3) able to read and comprehend texts fluently in either English, French, or Spanish; and (4) member as a former professional athlete of their respective national footballers’ union, national ice hockey players’ association, or national rugby union players’ association. In accordance with a sample size calculation for testing the relationship between independent and dependent variables (N > 50 + 8m where m is the number of independent variables), sample size of at least 58 participants was needed [17].
Dependent variables: symptoms of CMD
Distress
Symptoms of distress in the previous 4 weeks were measured using the Distress Screener (3 items scored on a 3-point scale) which is based on the Four-Dimensional Symptom Questionnaire (4DSQ) (e.g. ‘Did you recently suffer from worry?’) [18,19]. The 4DSQ (i.e. Distress Screener) has been validated in several languages, including English, French, and Spanish (internal consistency: 0.6–0.7; test–retest coefficients: ≥0.9; criterion-related validity: area under the receiver operating characteristics (ROC) curve ≥ 0.79) [18,19]. A total score ranging from 0 to 6 was obtained by summing up the answers on the three items, a score of 4 or more indicating the presence of distress [18,19].
Anxiety and depression
The 12-item General Health Questionnaire (GHQ-12) was used to assess symptoms of anxiety and depression in the previous 4 weeks (e.g. ‘Have you recently felt under strain?’) [20]. The GHQ-12 has been validated in several languages, including English, French, and Spanish (internal consistency: 0.7–0.9; criterion-related validity: sensitivity ≥0.70, specificity ≥0.75, area under ROC curve ≥ 0.83) [20,21]. Based on the traditional scoring system, a total score ranging from 0 to 12 was calculated by summing up the answers on the 12 items, with a score of 3 or more indicating signs of anxiety and depression (area under curve = 0.88) [20,21].
Sleep disturbance
Based on the Patient Reported Outcomes Measurement Information System short form (PROMIS), sleep disturbance in the previous four weeks was assessed through four single questions related to sleep quality (e.g. ‘Have you recently had problems sleeping?’) and scored on a 5-point scale [22,23]. The PROMIS has been validated in several languages, including English, French, and Spanish (internal consistency: >0.9; construct validity: product–moment correlations ≥0.96) (for detailed information, see www.nihpromis.org). A total score ranging from 1 to 20 is obtained by summing up the answers to the four questions, a score of 13 or more indicating the presence of sleep disturbance [22,23].
Adverse alcohol use
Level of alcohol consumption at the present time was detected using the 3-item of the Alcohol Use Disorders Identification Test Consumption (AUDIT-C; e.g. ‘How many standard drinks containing alcohol do you have on a typical day?’) [24]. The AUDIT-C has been validated in several languages, including English, French, and Spanish (test–retest coefficients: 0.6 – 0.9; criterion-related validity: area under ROC curve 0.70–0.97) [24,25]. A total score ranging from 0 to 12 was obtained by summing up the answers on the three items, a score of 5 or more indicating the presence of adverse alcohol use [24].
Independent variables: sports career-related concussions
The total number of confirmed concussion incidents occurred during an athlete’s career and diagnosed by a medical professional was examined through a single question (e.g. ‘How many concussions diagnosed by a medical professional did you have during your professional sports career [training and competition]?’). In our study, concussion was defined as a blow to the head resulting in symptoms such as headache, nausea, vomiting, dizziness/balance problems, fatigue, trouble sleeping, drowsiness, sensitivity to light or noise, blurred vision, difficulty remembering, and difficulty concentrating [1]. This definition of concussion was given to the participants by including it in the questionnaire.
Procedures
Based on all variables included in the study, an electronic questionnaire available in English, French, and Spanish (around 15 min needed to be completed) was set up (FluidSurveys™, Ottawa, Canada). In addition, the following descriptive variables were retrieved: age, height, body mass, duration of professional sports career, duration and nature of retirement, and nature of employment (including number of working hours per week). Information about the study was emailed to potential participants by their respective national footballers’ union, national ice hockey players’ association, or national rugby union players’ association, invitation procedures being blinded to the responsible researchers for reasons of privacy and confidentiality of the former athletes. Participants interested in the study gave their informed consent and were given access to the anonymous online questionnaire that they were asked to complete within 2 weeks. Reminders were sent after 2 and 4 weeks. Once completed, the electronic questionnaires were saved automatically on a secured electronic server that only the lead researcher could access. All former athletes participated voluntarily in the study and did not receive any reward for their participation.
Statistical analyses
All data analyses (statistical software IBM SPSS Statistics 23.0 for Windows) were conducted for the whole group of participants (primary aim) and separately for each sport (secondary aim). Descriptive data analyses (mean, standard deviation, frequency, range) were performed with all variables included in our study. Box and whisker plot of number of concussions versus presence/absence of symptoms of CMD was drawn from the available data with the boundaries of the box indicating the 25th and 75th percentile, the line within the box marking the median, the whiskers above and below the box indicating the minimum and maximum values (using the Mann–Whitney U test for groups comparisons; P < 0.05). Logistic regression analyses (expressed as odds ratio [OR] and related 95% CI; adjusted for age and duration of retirement) were used to explore whether former athletes who had sustained one or more concussions (continuous independent variable) during their sports career were more likely to report symptoms of CMD (dichotomous dependent variable) or comorbidity of symptoms of CMD (dichotomous dependent variable: two or more symptoms of CMD) than former athletes who had suffered from none or fewer concussions during their career [26]. In addition, participants were stratified by concussion history (none, 1 concussion, 2 or 3 concussions, 4 or 5 concussions, 6 or more concussions) and logistic regression analyses (expressed as OR and related 95% CI; adjusted for age and duration of retirement) were subsequently conducted (categorical independent variable and dichotomous dependent variables) [26]. With regard to a preferred sample size requirement of 50 times the number of independent variable, intended sample size in our study was set at a minimum 50 participants per sport discipline [26].
Results
Participants
A total sample of 1957 former professional athletes were contacted by their respective national footballers’ unions, national ice hockey players’ associations, or national rugby union players’ associations. Of those, 576 participants gave their informed consent and completed the questionnaire (overall response rate of 29%). Mean age of the participants at recruitment was 37 (range 20–50) years. Participants had competed in professional sports for approximately 10 years (from 9 years in rugby to 12 years in football) and they were retired (41% forced to retire from their sport) from professional sports for 7 years (from 4 years in football to 10 years in ice hockey). Around 88% of participants were employed for 40 h per week. All characteristics of the participants (total group and per sport) are presented in Table 1.
Table 1.
Characteristics of former male professional athletes retired from football, ice hockey, and rugby.
| Variables | Total | Football | Ice hockey | Rugby |
|---|---|---|---|---|
| Number contacted | 1957 | 307 | 420 | 1230 |
| Number recruited | 576 | 220 | 61 | 295 |
| Age (in years; mean ± SD) | 37 ± 7 | 35 ± 6 | 38 ± 7 | 38 ± 6 |
| Height (in cm; mean ± SD) | 183 ± 8 | 181 ± 7 | 181 ± 5 | 185 ± 8 |
| Weight (in kg; mean ± SD) | 93 ± 16 | 82 ± 11 | 90 ± 10 | 102 ± 16 |
| Years sport career (mean ± SD) | 10 ± 5 | 12 ± 5 | 11 ± 5 | 9 ± 4 |
| Years retired (mean ± SD) | 7 ± 5 | 4 ± 3 | 10 ± 7 | 7 ± 4 |
| Involuntary retired from sports (%) | 41 | 46 | 23 | 41 |
| Currently (self-)employed (%) | 88 | 76 | 93 | 95 |
| Working hours per week (mean ± SD) | 40 ± 14 | 35 ± 15 | 43 ± 10 | 43 ± 13 |
| Sports career-related concussions (%) | ||||
| None | 23 | 25 | 23 | 23 |
| Two or three | 34 | 40 | 29 | 32 |
| Four or five | 18 | 23 | 12 | 17 |
| Six or more | 11 | 3 | 8 | 15 |
| Symptoms of CMD (%) | ||||
| Distress | 21 | 18 | 12 | 25 |
| Anxiety and depression | 26 | 26 | 18 | 28 |
| Sleep disturbance | 27 | 28 | 15 | 28 |
| Adverse alcohol use | 26 | 25 | 44 | 24 |
| Comorbidity: ≥2 CMD symptoms | 26 | 25 | 21 | 28 |
N: Number of participants; SD: standard deviation; cm: centimeters; kg: kilograms; %: percentage; CMD: common mental disorders.
Sports career-related concussions
Former athletes reported a mean of 2.7 (SD = 2. 7, range 0–15) confirmed concussions during their sports career. Twenty three percent (n = 110) had not incurred a concussion during their sports career (23% in ice hockey and rugby, 25% in football), 34% (n = 158) reported two or three concussions (29% in ice hockey, 32% in rugby, 40% in football), 18% reported (n = 84) four or five concussions (12% in ice hockey, 17% in rugby, 23% in football), and 11% reported (n = 50) six or more concussions during their sports career (3% in football, 8% in ice hockey, 15% in rugby (Table 1; Figure 1).
Figure 1.
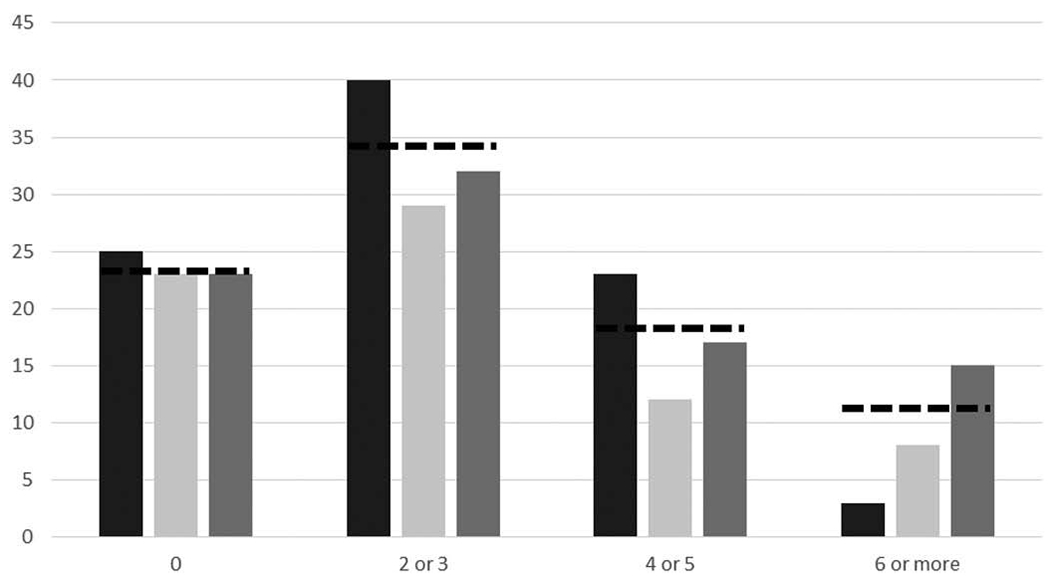
Percentage of former male professional athletes (total cohort in dash line, football in black, ice hockey in light grey, rugby in dark grey) reporting sports career-related concussions diagnosed by a medical professional.
Relationship of concussions with symptoms of CMD
There was a significant difference (P < 0.05) in the number of concussions when the group was divided according to the presence/absence of symptoms for distress, sleep disturbance, and anxiety and depression (Figure 2). There was no difference in the number of concussions associated with presence/absence of symptoms of adverse alcohol use. With concussion as a continuous independent variable, the number of sports career-related concussions proved to be a predictor for all outcomes measures, showing that former professional athletes are 7–11% more likely to report symptoms of CMD by every additional sports career-related concussion. With concussion as a categorical independent variable, our analyses showed that former professional athletes reporting a history of four or five concussions were nearly 1.5 times more likely to report symptoms of CMD than former professional athletes reporting no concussions, and participants with a history of six or more sports career-related concussions were two to five times more likely to report symptoms of CMD (Table 2). These relationships were also found across the different sports but most were not statistically significant (Table 2).
Figure 2.
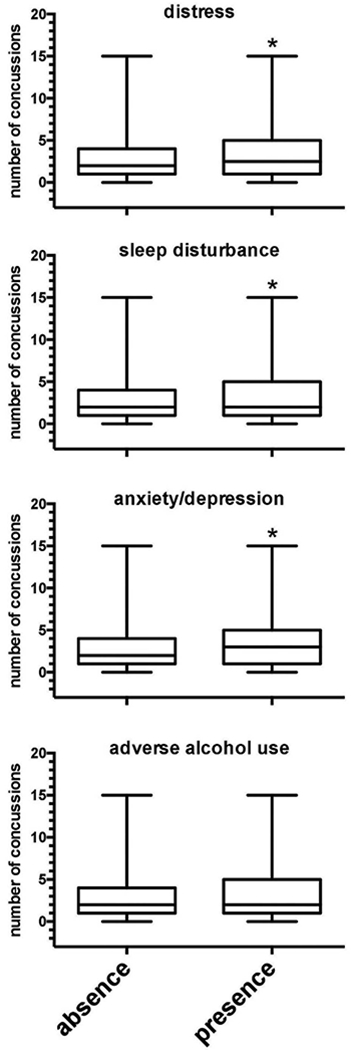
Box and whisker plot of number of concussions versus presence/absence of symptoms of CMD among former male professional athletes (*,P < 0.05).
Table 2.
Relationship expressed as odds ratio (95% confidence of interval; adjusted for age and duration of retirement) of sports career-related concussions with symptoms of common mental disorders among former male professional athletes retired from football, ice hockey, and rugby.
| Distress | Total | Football | Ice hockey | Rugby |
|---|---|---|---|---|
| 0 Concussion | 1.0 | 1.0 | 1.0 | 1.0 |
| 1 Concussion | 0.9 (0.4–2.1) | 0.6 (0.1–5.6) | na | 1.1 (0.4–3.1) |
| 2 or 3 Concussions | 1.3 (0.7–2.4) | 0.8 (0.2–3.2) | na | 1.4 (0.6–3.0) |
| 4 or 5 Concussions | 1.4 (0.7–3.0) | 2.6 (0.7–9.5) | na | 0.9 (0.4–2.4) |
| 6 or more Concussions | 3.2 (1.5–6.9) | 1.7 (0.1–20.0) | na | 2.8 (1.2–6.8) |
| Anxiety and depression | ||||
| 0 Concussion | 1.0 | 1.0 | 1.0 | 1.0 |
| 1 Concussion | 0.8 (0.4–1.8) | na | 0.4 (0.1–5.3) | 1.4 (0.6–3.4) |
| 2 or 3 Concussions | 0.8 (0.4–1.5) | 1.6 (0.5–5.0) | 0.9 (0.1–9.0) | 0.6 (0.3–1.2) |
| 4 or 5 Concussions | 1.4 (0.7–2.7) | 2.2 (0.7–7.3) | na | 1.2 (0.5–2.8) |
| 6 or More concussions | 2.4 (1.2–4.9) | 9.8 (0.8–116.3) | 2.0 (0.1–31.5) | 2.0 (0.9–4.7) |
| Sleep disturbance | ||||
| 0 Concussion | 1.0 | 1.0 | 1.0 | 1.0 |
| 1 Concussion | 1.8 (0.8–3.9) | 0.5 (0.1–5.4) | na | 2.7 (1.1–6.9) |
| 2 or 3 Concussions | 1.9 (1.0–3.6) | 1.5 (0.4–5.0) | na | 1.6 (0.7–3.7) |
| 4 or 5 Concussions | 2.0 (1.0–4.2) | 2.8 (0.8–10.2) | na | 1.6 (0.6–4.0) |
| 6 or More concussions | 5.2 (2.4–11.2) | 4.6 (0.5–42.8) | na | 4.9 (2.0–12.2) |
| Adverse alcohol use | ||||
| 0 Concussion | 1.0 | 1.0 | 1.0 | 1.0 |
| 1 Concussion | 1.7 (0.8–3.7) | 2.4 (0.4–13.5) | 2.9 (0.5–17.3) | 1.2 (0.4–3.9) |
| 2 or 3 Concussions | 1.4 (0.8–2.7) | 1.3 (0.4–4.7) | 0.3 (0.1–1.9) | 2.4 (1.0–5.7) |
| 4 or 5 Concussions | 1.2 (0.5–2.4) | 1.6 (0.4–6.5) | 1.1 (0.1–12.5) | 1.4 (0.5–3.8) |
| 6 or More concussions | 2.9 (1.3–6.2) | 5.5 (0.6–51.4) | 0.6 (0.1–14.3) | 4.3 (1.7–11.3) |
| Comorbidity | ||||
| 0 Concussion | 1.0 | 1.0 | 1.0 | 1.0 |
| 1 Concussion | 1.1 (0.5–2.3) | 0.9 (0.2–5.7) | 0.4 (0.1–5.7) | 1.5 (0.6–4.0) |
| 2 or 3 Concussions | 1.7 (0.9–3.0) | 1.4 (0.4–4.2) | 0.7 (0.1–7.1) | 1.9 (0.9–4.2) |
| 4 or 5 Concussions | 1.5 (0.7–2.9) | 1.4 (0.4–4.9) | na | 1.6 (0.7–3.9) |
| 6 or More concussions | 3.8 (1.8–8.0) | 11.1 (0.9–130.6) | 1.6 (0.1–25.4) | 3.9 (1.6–9.5) |
na: Not applicable because of limited number of cases.
Discussion
In 2001, self-reported data were collected from 2552 retired professional American Football players (mean age of 53 years) to determine the association between prior concussions and the likelihood of being diagnosed with depression [10]. The study showed an association between recurrent concussions and depression, suggesting that the prevalence of depression increases with increasing concussion history [10]. Compared with retired players with no history of concussion, retired players with a history of one or two concussions were 1.5 times more likely to be diagnosed with depression, and those reporting three or more previous concussions were 3 times more likely to be diagnosed with depression [10]. Following this study, 1044 of the participants (i.e. retired professional American Football players) completed a follow-up General Health Survey in 2010 [27]. About 10% of these respondents reported that they had been clinically diagnosed as depressed between 2001 (baseline) and 2010 (follow-up) [27]. The 9-year risk of a depression diagnosis increased with an increasing number of self-reported concussions, ranging from 8% for the group with one or two concussions to 26% for the group with 10 or more concussions [27]. Recently, a study was conducted among 239 French retired high-level rugby players (median age of 52 years) to explore the link between the prevalence of major depressive disorder and mild cognitive disorders and the number of reported concussions [11]. Results showed that major depressive disorder and mild cognitive disorders were associated with the number of reported concussions [11]. Relying on similar cross-sectional analyses, the results of our study are in accordance with these studies. However, besides sports career-related concussion, former professional athletes might be exposed to other stressors such as adverse life events, poor physical health, and unemployment that are likely to induce symptoms of CMD [12–14].
In our study, former athletes reported a mean of 2.7 confirmed concussions during their sports career, while one out of three reported two or three concussions. Despite that our results concur with recent studies about sports career-related concussions, we believe that concussions remain underreported and/or misdiagnosed in professional sports. Recently, there is also a growing concern in the sports medicine community regarding the immediate and long-lasting effects from subconcussive impacts (below the threshold to cause or elicit any signs of a concussion). Athletes in collision sports, like those involved in our study, are exposed to a large number of impacts that are regularly overlooked, while the short- and long-term consequences of these subconcussive impacts remain poorly understood [28]. With regard to the findings of our study, and under the assumption that subconcussive impacts might be associated with cognitive, motor, and psychiatric deficits, robust and well-powered studies are needed to explore any potential association.
Regarding the long-term consequences of concussions among athletes, increasing attention has been paid to the association between exposure to concussion and proposed increased risk of neurodegeneration among retired athletes, specifically CTE. The first clinical description of the syndrome now recognized as CTE was provided by Martland in his 1928 account of the ‘punch drunk’ syndrome in former boxers [29]. In the years since Martland’s first account, and in particular in the past decade, growing recognition of the pathology of CTE in former athletes from a number of contact sports has led to the understanding that it is exposure to brain injury that is associated with CTE risk, rather than any individual sport [2,8]. Although currently a diagnosis can only be made at autopsy, a clinical syndrome is emerging from the largely retrospective enquiries in confirmed cases of CTE to date that appears distinctive [9]. In particular, in a high proportion of early onset cases, behavioral and/or mood symptoms are reported, including depression and suicidality [2,9,30]. Importantly, however, while our data show high reporting of symptoms of CMD and a direct association between these and incidence of concussion across our cohorts, there is no suggestion that these symptoms are indicative of CTE in our participants, or informative as to incidence of CTE in former athletes.
Limitations and strengths
A potential methodological limitation worth mentioning might be the self-reported character of our study. Participants were asked (single question) to recall the number of diagnosed concussions that had occurred during their sports career. Denial and repression are two defense mechanisms well-known for influencing retrospective recall of unpleasant experiences in the past [31]. This impacts on the validity of the number of diagnosed concussions gathered in our study. However, it is well known that concussions or severe musculoskeletal injuries during a professional sport career can be considered as major life events and it might be assumed that athletes can generally recall quite precisely. In addition, athletes have access to their medical records – remaining their property – in which confirmed concussions should be noted. Therefore, it is likely that recall bias in our study was limited. The different scales used to assess symptoms of CMD are validated in many languages, which is a strength of our study. Even more, the importance and relevance of studies (such as our) relying on Patient Reported Outcome Measures (PROMs) have been very recently empowered in clinical and sports medicine to enable important clinical questions to be answered [32]. Also, the use of PROMs for both independent and dependent variables in our study warranted the involvement of a large number of participants from different sports. This involvement of a large number of professional i.e. elite players retired from football, ice hockey, and rugby can be seen as a strength of our study. By contrast, the cross-sectional design used in our study can be seen as a potential limitation as it does not allow the exploration of a causal association between independent and dependent variables [14]. A prospective study, based on a longitudinal design with a follow-up period of two to three decades and including a large cohort of professional i.e. elite athletes, might have secured a higher methodological quality for an observational study such as ours. However, whether such a prospective study is feasible in professional sports remains very doubtful.
Implications
Considering the number of repetitive concussions that might occur in a career in contact sports such as football, ice hockey, and rugby, our findings endorse the alarming severity of the long-term consequences of repeated concussions among athletes. Consequently, the prevention of concussions should be even more prioritized in professional (and recreational) sports, while continued efforts at improving its management should be promoted. Preventing the occurrence of concussions (and other injuries) should be the first priority in all contact sports, especially in those sports involving high-speed collisions between players. Existing rules and guidelines might be subject to alterations to minimize (head) collisions, to prevent any concussed athlete from continuing training or competing, and enforcing a conservative Return To Play protocol.
Athletes can also be trained to implement techniques that reduce the risk of injury. For example, in rugby, coaching tackle technique has been introduced in high-level youth rugby with the goal of decreasing the risk of injuries, including concussion [33]. At the professional level in rugby, the application of concussion guidelines has been empowered and monitored by the international and national organizing bodies. The medical support staff and players seem to be embracing these guidelines. Consequently, professional rugby might be regarded as the gold standard when it comes to the prevention and management of concussions. By contrast, the management of concussions in professional football has been under scrutiny. In 2006, the Fédération Internationale de Football Association (FIFA) introduced a rule change by sanctioning any elbow to the head with a mandatory red card. While the number of head injuries during international tournaments decreased after this ruling, the management of concussions in professional football is still discussed and FIFA introduced recently another measure, namely that the referee has the ability to stop the game for 3 min whenever a suspected incident of concussion occurs. Nevertheless, the actual policy related to concussions in professional football remains questioned and should be improved to protect the sustainable health of footballers. In ice hockey, the rule change related to eliminating checking to the head and banning hard plastic elbow pads has been proposed to prevent head injuries and protect players’ health [34].
In addition to prevention strategies, particular attention should be applied to the management of a concussion, following the event. The first step in good concussion management is to educate all the stakeholders. In youth sports, parental knowledge and attitudes about concussions and its management should be unequivocally developed and optimized. Nationwide campaigns such as the “If in doubt, sit them out” developed in Scotland might also be effective in reaching the general public and grassroots participants across all sports and in raising their awareness about concussions. In professional and high level sports, while medical staff seem to be properly educated, it is crucial to focus on the education of both coaches and athletes to make them understand and accept concussions’ management. Last but not least, a proper support for former professional athletes suffering from mental health should be developed and implemented. Many unions or associations representing athletes have adopted this path recently, but more efforts remain to promote and protect the sustainable health of athletes in the long term.
Conclusions
During the first 10 years after their retirement from contact team sports, former professional athletes retired from football, ice hockey, and rugby are 7–11% more likely to report symptoms of CMD by every additional sports career-related concussion. Former professional athletes reporting a history of four or five sports career-related concussions are nearly 1.5 times more likely to report symptoms of CMD, and athletes with a history of six or more sports career-related concussions are 2–5 times more likely to report symptoms of CMD. Our findings confirm the urge to protect athletes from concussions during their career and to increase the quality of concussion management at professional sports level.
Acknowledgements
The authors would like to thank all athletes’ representatives from Finland, France, Ireland, Norway, South Africa, Spain, Sweden and Switzerland for their support in the study. We are grateful to all former athletes who participated in the study.
Declaration of Interests
William Stewart is supported by an NHS Scotland Career Researcher Fellowship. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
References
- 1.McCrory P, Meeuwisse WH, Dvorak J, et al. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017. Apr 26. DOI: 10.1136/bjsports-2017-097699. [DOI] [PubMed] [Google Scholar]
- 2.Hay J, Johnson VE, Smith DH, et al. Chronic traumatic encephalopathy: the neuropathological legacy of traumatic brain injury. Ann Rev Pathol. 2016. DOI: 10.1146/annurev-pathol-012615-044116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.England Professional Rugby Injury Surveillance Project Steering Group. Rugby Players England Professional Rugby Injury Surveillance Project 2014-2015 Season Report. Twickenham: Rugby Football Union; 2016. [Google Scholar]
- 4.Ruhe A, Gänsslen A, Klein W. The incidence of concussion in professional and collegiate ice hockey: are we making progress? A systematic review of the literature. Br J Sports Med. 2014;48:102–106. [DOI] [PubMed] [Google Scholar]
- 5.Blake C, John M, Conor G, et al. Injury to the head region in elite male gaelic football and hurling: 2007–2012. Br J Sports Med. 2014;48:569. [Google Scholar]
- 6.Waldén M, Hägglund M, Orchard J, et al. Regional differences in injury incidence in European professional football. Scand J Med Sci Sports. 2013;23:424–430. [DOI] [PubMed] [Google Scholar]
- 7.Stewart W, McNamara PH, Lawlor B, et al. Chronic traumatic encephalopathy: a potential late and under recognized consequence of rugby union?. QJM. 2016;109:11–15. [DOI] [PubMed] [Google Scholar]
- 8.McKee AC, Cairns NJ, Dickson DW, et al. The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Acta Neuropathol. 2016;131:75–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stern RA, Daneshvar DH, Baugh CM, et al. Clinical presentation of chronic traumatic encephalopathy. Neurology. 2013;81:1122–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guskiewicz KM, Marshall SW, Bailes J, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39:903–909. [DOI] [PubMed] [Google Scholar]
- 11.Decq P, Gault N, Blandeau M. Long-term consequences of recurrent sports concussion. Acta Neurochir (Wien). 2016;158:289–300. [DOI] [PubMed] [Google Scholar]
- 12.Gouttebarge V, Aoki H, Kerkhoffs G. Prevalence and determinants of symptoms related to mental disorders in retired male professsional footballers. J Sports Med Phys Fitness. 2016;56:648–654. [PubMed] [Google Scholar]
- 13.Gouttebarge V, Kerkhoffs G, Lambert M. Prevalence and determinants of symptoms of common mental disorders in retired professional Rugby Union players. European J Sport Sci. 2016;16:595–602. [DOI] [PubMed] [Google Scholar]
- 14.Schuring N, Aoki H, Gray J, et al. Osteoarthritis is associated with symptoms of common mental disorders among former elite athletes. Knee Surg Sports Traumatol Arthrosc. 2016. DOI: 10.1007/s00167-016-4255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J American Med Assoc. 2013;310:191–194. [DOI] [PubMed] [Google Scholar]
- 16.Araújo CGS, Scharhag J. Athlete: a working definition for medical and health sciences research. Scand J Med Sci Sports. 2016;26:4–7. [DOI] [PubMed] [Google Scholar]
- 17.Green SB. How many subjects does it take to do a regression analysis? Multivariate Behavioral Research. London and New York: Taylor & Francis Group; 1991. [DOI] [PubMed] [Google Scholar]
- 18.Braam C, Van Oostrom SH, Terluin B, et al. Validation of a distress screener. J Occup Rehab. 2009;19:231–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Terluin B, Van Marwijk HWJ, Adèr HJ, et al. The Four-Dimensional Symptom Questionnaire (4DSQ): a validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry. 2006;6:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldberg DP, Gater R, Sartorius N, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27:191–197. [DOI] [PubMed] [Google Scholar]
- 21.Salama-Younes M, Montazeri A, Ismaïl A, et al. Factor structure and internal consistency of the 12-item General Health Questionnaire (GHQ-12) and the Subjective Vitality Scale (VS), and the relationship between them: a study from France. Health Qual Life Outcomes. 2009;7:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yu L, Buysse DJ, Germain A, et al. Development of short Forms from the PROMIS sleep disturbance and sleep-related impairment item banks. Behav Sleep Med. 2011;28:6–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buysse DJ, Yu L, Moul DE, et al. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010;33:781–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dawson DA, Grant BF, Stinson FS, et al. Effectiveness of the derived alcohol use disorders identification test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the general population. Alcohol Clin Exp Res. 2005;29:844–854. [DOI] [PubMed] [Google Scholar]
- 25.De Meneses-Gaya C, Waldo Zuardi A, Loureiro SR, et al. Alcohol Use Disorders Identification Test (AUDIT): an updated systematic review of psychometric properties. Psychology Neurosci. 2009;2:83–97. [Google Scholar]
- 26.Woodward M. Epidemiology: study design and data analysis. Boca Raton: CRC Press; 2013. [Google Scholar]
- 27.Kerr ZY, Marshall SW, Harding HP Jr, et al. Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am J Sports Med. 2012;40:2206–2212. [DOI] [PubMed] [Google Scholar]
- 28.Slobounov SM, Walter A, Breiter HC, et al. The effect of repetitive subconcussive collisions on brain integrity in collegiate football players over a single football season: a multi-modal neuroimaging study. Neuroimage Clin. 2017;14:708–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martland H. Punch drunk. JAMA. 1991;91:1103–1107. [Google Scholar]
- 30.McKee AC, Daneshvar DH, Alvarez VE, et al. The Neuropathology of Sport. Acta Neuropathol. 2014;127:29–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jacobson E. Denial and repression. J Am Psychoanal Assoc. 1957;5:61–92. [DOI] [PubMed] [Google Scholar]
- 32.Davis JC, Bryan S. Patient Reported Outcome Measures (PROMs) have arrived in sports and exercise medicine: why do they matter?. Br J Sports Med. 2015;49:1545–1546. [DOI] [PubMed] [Google Scholar]
- 33.Burger N, Lambert M, Viljoen W, et al. Tackle technique and tackle-related injuries in high-level South African Rugby Union under-18 players: real-match video analysis. Br J Sports Med. 2016. Jan 18. DOI: 10.1136/bjsports-2015-095295. [DOI] [PubMed] [Google Scholar]
- 34.Smith AM, Gaz DV, Larson D, et al. Does fair play reduce concussions? A prospective, comparative analysis of competitive youth hockey tournaments. BMJ Open Sport Exerc Med. 2016;2:e000074. [DOI] [PMC free article] [PubMed] [Google Scholar]


