Abstract
Background
Financial risk protection (FRP), defined as households’ access to needed healthcare services without experiencing undue financial hardship, is a critical health systems target, particularly in low- and middle-income countries (LMICs). Given the remarkable growth in FRP literature in recent times, we conducted a scoping review of the literature on FRP from out-of-pocket (OOP) health spending in LMICs. The objective was to review current knowledge, identify evidence gaps and propose future research directions.
Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines to conduct this scoping review. We systematically searched PubMed, Scopus, ProQuest and Web of Science in July 2021 for literature published since 1 January 2015. We included empirical studies that used nationally representative data from household surveys to measure the incidence of at least one of the following indicators: catastrophic health expenditure (CHE), impoverishment, adoption of strategies to cope with OOP expenses, and forgone care for financial reasons. Our review covered 155 studies and analysed the geographical focus, data sources, methods and analytical rigour of the studies. We also examined the level of FRP by disease categories (all diseases, chronic illnesses, communicable diseases) and the effect of health insurance on FRP.
Results
The extant literature primarily focused on India and China as research settings. Notably, no FRP study was available on chronic illness in any low-income country (LIC) or on communicable diseases in an upper-middle-income country (UMIC). Only one study comprehensively measured FRP by examining all four indicators. Most studies assessed (lack of) FRP as CHE incidence alone (37.4%) or as CHE and impoverishment incidence (39.4%). However, the LMIC literature did not incorporate the recent methodological advances to measure CHE and impoverishment that address the limitations of conventional methods. There were also gaps in utilizing available panel data to determine the length of the lack of FRP (e.g. duration of poverty caused by OOP expenses). The current estimates of FRP varied substantially among the LMICs, with some of the poorest countries in the world experiencing similar or even lower rates of CHE and impoverishment compared with the UMICs. Also, health insurance in LMICs did not consistently offer a higher degree of FRP.
Conclusion
The literature to date is unable to provide a reliable representation of the actual level of protection enjoyed by the LMIC population because of the lack of comprehensive measurement of FRP indicators coupled with the use of dated methodologies. Future research in LMICs should address the shortcomings identified in this review.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12961-022-00886-3.
Keywords: Out-of-pocket expenditure, Financial risk protection, Catastrophic health expenditure, Impoverishment, Coping strategies, Forgone care, Low- and middle-income countries
Background
Financial risk protection (FRP), defined as the ability to consume needed quality healthcare services without experiencing undue financial hardship, is one of the critical components of universal health coverage (UHC), an agreed target of the United Nations (UN) Sustainable Development Goal (SDG) 3 on health and well-being [1, 2]. A health system that protects people from financial risks ensures that the consumption of needed healthcare will improve their health status without compromising their economic well-being [3]. In the absence of adequate FRP, people needing to pay out-of-pocket (OOP) at the point of service are at risk of undergoing a range of adverse health and economic consequences. The damaging upshots may include limited or no access to healthcare, deteriorated health status, the undesirable substitution of essential consumption in the current or future period due to depleted household assets, slipping into or spiralling deep into poverty, and intensified health and socioeconomic inequalities.
The literature captures the undesirable economic effects of the OOP mode of payment for healthcare through one or more of the following indicators: catastrophic health expenditure (CHE), impoverishment, adoption of coping strategies and forgone care for financial reasons (FCFR) [3–9]. The incidence of CHE is measured as the percentage of households whose OOP healthcare expenses surpass a predetermined proportion or threshold of their available resources to pay for healthcare, or capacity to pay (CTP) [3, 4]. The assumption here is that such an extent of OOP health expenses reduces household consumption of other nonmedical necessities (e.g. food) [3]. Impoverishment incidence is defined as the proportion of households that were above the poverty line (PL) (i.e. nonpoor) before paying for healthcare from OOP but found themselves below the PL (i.e. poor) after OOP expenses [3]. The incidence of the adoption of coping strategies or distress or hardship financing is measured by the percentage of households that borrow money, sell productive assets, draw from savings, seek contributions from friends and family, or any combination of the above to meet OOP expenses [6, 10, 11]. On the other hand, the incidence of FCFR measures the proportion of households that forgo healthcare because of high or unaffordable OOP costs of care [7, 12]. Notably, CHE is the sole indicator in the SDG framework (SDG 3.8.2) to track progress towards UHC [4].
CHE is measured in a variety of ways, with metrics differing in how household CTP is defined. Traditional methods of CHE measurement include the budget share method, actual food expenditure method and the normative food expenditure method. The budget share method equates CTP to the household’s entire budget (i.e. income or consumption expenditure) [13]. The latter two methods derive CTP by deducting an allowance for basic needs from the household budget. The actual food expenditure method subtracts a household’s actual food expenses from its budget and calculates CHE based on the residual amount (i.e. nonfood expenditure) [13]. The normative food expenditure method refines it by calculating a standard amount that households must spend on food, subtracting it from the total budget and calculating CHE based on the remainder (called standard food expenditure-based non-subsistence expenditure) [14]. However, the normative food expenditure method is no different from the actual food expenditure method when the household is poor; that is, the household’s budget is less than the standard food expenditure. In such a case, actual food expenses are deducted from the budget instead of the higher, standard spending. Empirical evidence shows that the three traditional methods cannot precisely identify poor households that experience financial hardship despite spending relatively small amounts on healthcare [15, 16]. Specifically, the budget share method is the least sensitive to financial hardship among poorer households, which tends to underestimate CHE among the poor and overestimate it among the wealthy [15, 16]. Therefore, the traditional methods of CHE measurement present a challenge to equity analysis and pro-poor policy initiatives [5, 16].
More refined measurement techniques were subsequently developed. Wagstaff and Eozenou’s method (2014), developed as part of a World Bank (WB) effort, calculates CTP by deducting the prevailing PL, thereby providing a link between CHE and poverty [17]. Depending on the PL employed, this is likely to yield a greater concentration of CHE among the poor than among the rich, compared with the budget share method [4]. The normative food, housing (rent) and utilities method developed (in 2016) by the WHO Regional Office for Europe deducts a relative PL representing standard expenditures on basic need items (food, housing [rent] and utilities) consistently from all households [4, 18]. Additionally, any OOP expense by poor households is considered both further impoverishing and catastrophic. The normative food, housing (rent) and utilities method is the only approach in which wealthier households are consistently required to spend a higher proportion of their budget on healthcare to be counted as incurring CHE [15]. According to empirical research, the resulting CHE estimate is more sensitive to financial hardship experienced by poor households than the other methods, producing actionable evidence for policy [15, 16].
Different CHE metrics employ different thresholds: the budget share method typically uses 10% or 25%, while the other four employ 25% and 40% thresholds [13, 14, 17, 18]. As the official indicator for SDG 3.8.2, CHE is based on the budget share method, with 10% and 25% thresholds [5]. Impoverishment metrics also vary in the PLs they use. Absolute PLs may include the WB’s international PL (currently $1.90 per capita per day in purchasing power parity) or national PLs based on the WB’s poverty assessment, food poverty (cost of minimum food requirements), or basic needs (cost of a basket of goods thought to meet minimum biological needs) [19]. Relative PLs may be based on income (a specific percentage of the country’s median income, e.g. 50%, 60%) or household spending on basic needs [19]. Notably, already poor households whose poverty was exacerbated by OOP health payments are not included in the measurement of impoverishment incidence. Some recent studies consider OOP expenses incurred by poor households as further impoverishing, and measure them as a separate indicator of the impoverishing effects of OOP expenses [17, 18, 20].
The issue of FRP has attracted great interest from the scientific community and has given rise to remarkable growth in the literature in recent times [21]. However, the growth of studies, particularly in the low- and middle-income countries (LMICs), has outpaced existing reviews, which are limited by time and scope. Among the previous reviews most germane to this study, Rijal et al. (2018) examined the financial burden of noncommunicable diseases (NCDs) in South Asia, focusing on OOP expenditure, CHE, impoverishment and coping strategies adopted by patients with NCDs and their families; Erlangga et al. (2019) investigated the impact of government health insurance on health status, healthcare utilization and FRP in LMICs; and Alam and Mahal (2014) focused on the household-level economic impact of health shocks in LMICs in the pre-2014 literature [22–24]. However, considerable gaps remain. In particular, the post-2014 LMIC literature on FRP from OOP payments has simply not been covered in the existing reviews.
We, therefore, set out to conduct a scoping review to summarize recent evidence on FRP in healthcare in the LMICs based on the WB classification of countries by income as of 2021 (i.e. low-income [LIC], lower-middle-income [LwMIC] and upper-middle-income countries [UMIC] with per capita gross national income of US$ 12,695 or less) [25]. The overarching research question steering this review is: how financially protected are the households in the LMICs when they need healthcare? The specific objectives are to review the methodologies used in the recent literature to measure FRP, to determine the level of FRP enjoyed by the LMIC population, and to determine differences across country income groups (LICs, LwMICs and UMICs) for both of the above. This review adds to previous reviews by drawing together a larger number of recent studies on household-level FRP in healthcare in the LMICs of Africa, Asia, south-eastern Europe and Latin America, specifically between 2015 and 2021. Additionally, advances in the methodology for measuring FRP developed in recent times mean that this study adds considerably to the information base on FRP in accessing healthcare.
Methods
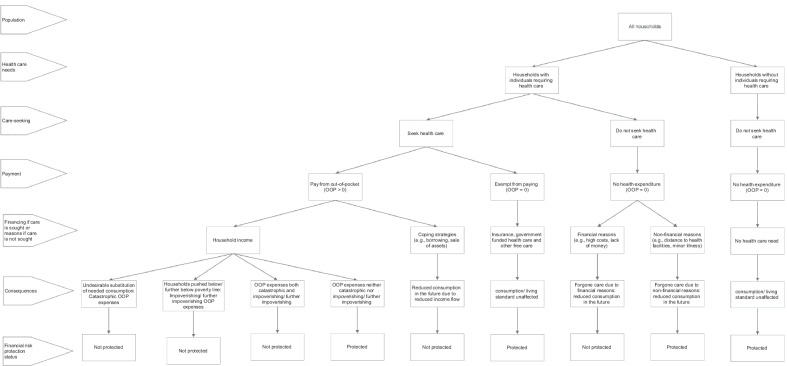
We developed a conceptual framework (Fig. 1) based on the FRP literature in healthcare to guide this review. We maintain that CHE, impoverishment effects, adoption of coping strategies and FCFR highlight distinct aspects of the lack of FRP in healthcare. Therefore, a comprehensive FRP study must measure all four indicators to determine how well a country is doing in ensuring FRP. Identifying the population lacking FRP through a smaller subset of these indicators is unlikely to fully reflect the intricacy of the notion of FRP, which could lead to inaccurate or misleading conclusions or, worse, create perverse incentives for policy-makers [26].
Fig. 1.
Conceptual framework of financial risk protection in LMICs
Figure 1 shows how a household’s FRP status can be measured by examining its healthcare needs, care-seeking behaviour, OOP payment requirement and financing source for OOP expenses if care is sought or reasons if not. To identify the households lacking FRP, we divide all households between those with and without healthcare needs (e.g. preventative, curative, rehabilitative, long-term, palliative). Households without healthcare needs do not pay anything towards healthcare and, therefore, do not lack FRP. We then partition families requiring care into those seeking and not seeking care. Households may fail to seek needed care for financial and nonfinancial reasons. We further separate the families seeking healthcare into those who pay and those who do not. Households may be exempt from paying if they are fully insured against healthcare costs or receive free care (e.g. from government, nongovernmental organizations, charities). Those who must pay OOP may finance it from their income or, if insufficient, adopt coping strategies (such as borrowing with or without interest or collateral, sale of assets).
Households that use their income to meet OOP expenses are not financially protected if the payments have catastrophic or impoverishing effects. Households incurring CHE lack FRP because OOP expenses relative to their available resources are so high that they forgo the consumption of other (welfare-augmenting) necessities [3]. On the other hand, households impoverished or further impoverished due to OOP expenses lack FRP because OOP expenses push them below or further below the PL, a threshold beneath which even the most basic standard of living is not guaranteed [3]. Thus, CHE and impoverishment are separate facets of a lack of FRP. Although some households may suffer both catastrophic and impoverishing effects of OOP expenses, global evidence suggests that this overlap is minimal (8–14%) [27]. Therefore, it is critical to complement CHE with impoverishment indicators to assess the degree of FRP enjoyed by a population.
Additionally, CHE and impoverishment indicators are blind to how households finance OOP expenses. Suppose families employ coping mechanisms such as taking out loans and selling assets to meet OOP expenses. In that case, they inflate household budgets and CTP, allowing them to pay for care while possibly preventing them from experiencing CHE and impoverishment in the short term. However, families employing coping techniques lack FRP, as these strategies might affect long-term household welfare by limiting the flow of income (because of loan repayments with interest or lost returns from the sale of productive assets) and the ability to cope again if needed [8].
Furthermore, CHE, impoverishment and coping metrics do not include households with zero OOP expenses; they show lack of FRP only among households that make OOP payments for healthcare. However, not all families with zero OOP expenses are financially protected. Households that forgo needed care (and thus have zero OOP expenditure) for financial reasons such as high or unaffordable cost of care seriously lack FRP. These might be the households with insufficient income that cannot seek healthcare even through coping. Forgoing care may exacerbate health problems and put the concerned families in a downward spiral of ill health and poverty [28, 29]. Hence, the extent to which OOP expenses prevent households from seeking necessary healthcare is another crucial indicator of FRP.
Therefore, we consider households as lacking FRP if they incur catastrophic or impoverishing OOP expenses, pay for healthcare through coping strategies or forgo healthcare altogether for financial reasons. We, however, recognize that catastrophic and impoverishing OOP hurt household economic welfare in the current period, and coping strategies and FCFR reduce welfare in the future. Failure to consider all four indicators to examine FRP may underestimate the overall economic impact on households of the requirement to make OOP payments for healthcare.
Search strategies
We developed our protocol for this scoping review with support from Murdoch University (Australia) subject librarians (healthcare, and business and economics). Before the final data collection, we pilot-tested and calibrated the protocol to ensure its applicability. We searched for empirical literature on FRP in LMICs in the following electronic databases and platforms: PubMed, Scopus, ProQuest (EconLit and APA PsycInfo) and Web of Science (Social Sciences Citation Index). We used key search terms including “out-of-pocket expenditure, “financial risk protection”, “catastrophic health expenditure”, “impoverishment”, “coping” and “forgone care” along with the names of the countries in LIC, LwMIC and UMIC groups according to the WB country classification by per capita income in July 2021 [25]. The searches were carried out on 13 July 2021. Time, language and type of publication filters were used in the searches to identify articles published in peer-reviewed journals in the English language since 2015. The search strings are available in Additional file 1.
Study selection
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 guidelines in the study selection process [30]. The retrieved studies were uploaded to the bibliographic software EndNote 2020, which was used to identify duplicates by using the title, year and reference type, ignoring spacing and punctuation. Non-duplicate records were uploaded to the Rayyan web app for systematic reviews [31] to screen the titles and abstracts for assessing eligibility based on strict inclusion and exclusion criteria. The eligibility criteria were as follows: original research articles in scholarly journals; studies on countries in the WB’s list of LICs, LwMICs and UMICs as of July 2021 [25]; retrospective observational studies analysing nationally representative data; and studies with a primary focus on quantitative FRP analysis (i.e. the level, distribution and trends of CHE, impoverishment, adoption of coping strategies and FCFR).
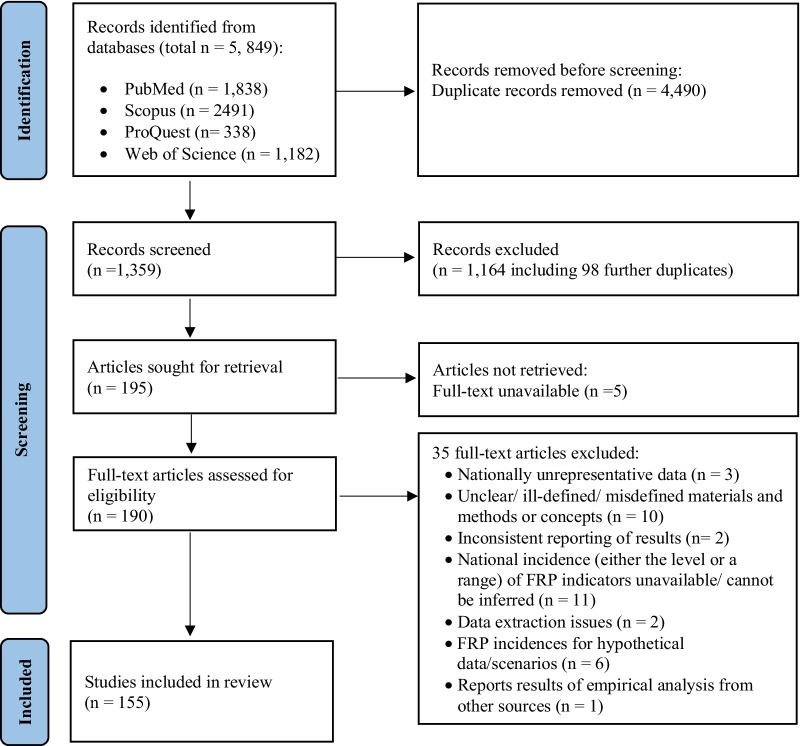
The exclusion criteria were working papers; review articles; qualitative papers; analysis of OOP payments only (i.e. without any explicit analysis of the incidence of the four selected FRP indicators); modelling studies assessing FRP based on hypothetical scenarios or using assumed consumption or income instead of actual reported consumption or income; studies extracting data from nationally representative surveys but reporting the incidence of FRP indicators for a geographical subset of the population (e.g. urban only, rural only or a subset of states/provinces only). Having assessed the status of inclusion or exclusion by screening the titles and abstracts by one reviewer (TR), the selected studies for review were reassessed to confirm their eligibility. After that, full-text studies were assessed for their suitability. A second reviewer (KA) confirmed the selection based on the criteria. Figure 2 summarizes the study selection process.
Fig. 2.
The PRISMA 2020 flow chart of the study selection process for this scoping review
Data extraction and synthesis
The finally selected studies were analysed based on geographical focus (countries studied), source and type of data used, number of FRP indicators assessed, approaches followed to measure incidence of FRP indicators (methods and thresholds for CHE, PLs for impoverishing health expenditure, definition for coping strategies and FCFR); and rigour of analysis (intensities, distribution and trends of FRP indicators). We analysed the level of FRP by disease and condition groups (all diseases, chronic illnesses including NCDs and injuries, and communicable diseases [CDs] and maternal and perinatal conditions) by extracting the incidence of catastrophic and impoverishing OOP expenses, coping and FCFR from each publication (main text and appendix). We also examined the protective effect of health insurance from financial hardship in LMICs by examining whether insured households had lower incidence of the four FRP indicators than the noninsured (when only one year’s result was available) or if the implementation or reform of the schemes reduced the incidence of the FRP indicators over time across the whole population (when two or more years’ results were available). We reported the rank-weighted incidence of CHE when both unweighted and weighted measures were available.
Results
Study selection
After screening 1359 titles and abstracts, we reviewed 190 full-text peer-reviewed articles and finally included 155 articles in the study. The main reasons for exclusion were (1) national incidence (either the level or a range) of FRP indicators unavailable or could not be inferred (out of n = 11 studies, 9 reported odds ratios of incurring catastrophic/impoverishing OOP expenses only); (2) unclear or ill-defined or misdefined materials and methods or concepts (n = 10); and (3) FRP incidence for hypothetical data/scenarios (n = 6). The reviewed studies were quite recent, as nearly 40% of the articles were published between 2020 and mid-2021 and around 75% were published between 2018 and mid-2021 (Table 1).
Table 1.
Distribution of the included studies by geographical coverage and data sources used (sorted by number of studies by country)
| Panel A: Single-country studies (n = 145) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Country | Income group, region a | Total population in 2020 b | Studies reviewed | Number of studies reviewed | Data source | |||
| Millions | % | n | % | |||||
| India | LwMIC, SA | 1380.0 | 26.3 | [71]; [50]; [51]; [72]; [73]; [48]; [49]; [74]; [75]; [76]; [77]; [78]; [44]; [79]; [80]; [35]; [81]; [82]; [33]; [83]; [84]; [85]; [86]; [87]; [88]; [89]; [41]; [90]; [91]; [92]; [93]; [94]; [95]; [96]; [57] | 35 | 24.1 | National Sample Survey, 1994/95, 1995/96, 1999/2000, 2004, 2004/05, 2011/12, 2014, 2017/18; Indian Human Development Survey, 2004/05, 2011/12; World Health Organization’s (WHO) Study on global AGEing and adult health (SAGE) India*, 2007/08 | |
| China | UMIC, EAP | 1402.1 | 26.7 | [97]; [98]; [99]; [100]; [64]; [101]; [102]; [103]; [63]; [104]; [36]; [66]; [105]; [106]; [107]; [108]; [65]; [109]; [110]; [111]; [112]; [39]; [113] | 23 | 15.9 | China Health and Retirement Longitudinal Study*, 2011, 2013, 2015; National Health Services Survey, 2003, 2008, 2013; China Family Panel Studies*, 2010, 2012, 2014, 2016, 2018; China Household Finance Survey*, 2015, 2017; National Oral Health Survey, 2005; Dataset for the study ‘Evaluating Social Policy Supporting System for Vulnerable Families in Urban and Rural China’, 2014 | |
| Iran, Islamic Rep | LwMIC, MENA | 84.0 | 1.6 | [114]; [115]; [116]; [117]; [118]; [119]; [120]; [56]; [58]; [121] | 10 | 6.9 | Households Income and Expenditure Survey, 1991, 1996, 2001, 2003 – 2017 | |
| Ghana | LwMIC, SSA | 31.1 | 0.6 | [52]; [122]; [123]; [124]; [125]; [126] | 6 | 4.1 | Ghana Living Standard Survey, 1991/92, 1998/99, 2005/06, & 2012/13; First National Tuberculosis Patient Cost Survey, 2016 | |
| Bangladesh | LwMIC, SA | 164.7 | 3.1 | [127]; [128]; [129]; [130]; [131] | 5 | 3.4 | Household Expenditure Survey, 1991/92, 1995/96; Household Income and Expenditure Survey, 2000, 2005, 2010, 2016; Urban Health Expenditure Survey, 2011; Bangladesh Integrated Household Survey, 2011/12 | |
| Kenya | LwMIC, SSA | 53.8 | 1.0 | [132]; [20]; [133]; [38]; [59] | 5 | 3.4 | Kenya Household Expenditure and Utilization Survey, 2003, 2007, 2013, 2018 | |
| Vietnam | LwMIC, EAP | 97.3 | 1.9 | [46]; [54]; [134]; [62] | 4 | 2.8 | Household Living Standards Survey, 2012, 2014, 2016; First National Tuberculosis Patient Cost Survey, 2016 | |
| Mexico | UMIC, LAC | 128.9 | 2.5 | [12]; [135]; [61] | 3 | 2.1 | Mexican National Household Income and Expenditure Survey, 2000, 2002, 2004, 2005, 2006, 2008, & 2010; Survey of Health and Nutrition (Encuesta Nacional de Salud y Nutricion, ENSANUT), 2006, 2012 | |
| Ethiopia | LIC, SSA | 115.0 | 2.2 | [136]; [137]; [138] | 3 | 2.1 | Household Consumption and Expenditure Survey 2010/11, 2015/16; Household Welfare Monitoring Survey 2015/16; National Tuberculosis Prevalence Survey, 2010/11 | |
| Myanmar | LwMIC, EAP | 54.4 | 1.0 | [139]; [140]; [7] | 3 | 2.1 | World Health Survey, 2002/03; Integrated Household Living Condition Assessment, 2009/10; Poverty and Living Conditions Survey, 2015 | |
| Nepal | LwMIC, SA | 29.1 | 0.6 | [141]; [42]; [142] | 3 | 2.1 | Living Standards Survey, 1995, 2010/11, | |
| Malawi | LIC, SSA | 19.1 | 0.4 | [143]; [144]; [145] | 3 | 2.1 | Integrated Household Survey, 2010/11, 2016/17 | |
| Cambodia | LwMIC, EAP | 16.7 | 0.3 | [40]; [146]; [147] | 3 | 2.1 | Cambodian Socio-Econoamic Survey, 2004, 2009, 2014, 2015, 2016, 2017 | |
| Mongolia | LwMIC, EAP | 3.3 | 0.1 | [148]; [43]; [149] | 3 | 2.1 | Household Socio-Economic Survey, 2012 | |
| Indonesia | LwMIC, EAP | 273.5 | 5.2 | [150]; [151] | 2 | 1.4 | Indonesian Family Life Survey*, 1993, 1997, 2000, 2007, 2014 | |
| Nigeria | LwMIC, SSA | 206.1 | 3.9 | [152]; [153] | 2 | 1.4 | Harmonized Nigeria Living Standard Survey, 2008/09, 2009/10 | |
| Turkey | UMIC, ECA | 84.3 | 1.6 | [154]; [155] | 2 | 1.4 | Household Budget Surveys, 2004 – 2010, 201, 2014, 2016 | |
| Thailand | UMIC, EAP | 69.8 | 1.3 | [156]; [55] | 2 | 1.4 | Household Socio-Economic Surveys, 1996, 1998, 2000, 2002, 2004, 2006, 2007, 2008, 2009, 2010, 2011, 2012, 2013, 2014, 2015; Health and Welfare Survey, 2015 | |
| Colombia | UMIC, LAC | 50.9 | 1.0 | [60]; [157] | 2 | 1.4 | National Health Survey, 2007; Quality of Life National Survey, 2011 | |
| Uganda | LIC, SSA | 45.7 | 0.9 | [158]; [159] | 2 | 1.4 | National Household Survey, 2005/06, 2009/10, 2012/13, 2016/17 | |
| Peru | UMIC, LAC | 33.0 | 0.6 | [34]; [53] | 2 | 1.4 | National Household Survey on Living Conditions (Encuesta Nacional de Hogares, ENAHO), 2008, 2016, 2017 | |
| Zimbabwe | LwMIC, SSA | 14.9 | 0.3 | [160]; [45] | 2 | 1.4 | National Household Survey, 2016; Health Facility-based Survey on Tuberculosis Patients, 2018 | |
| Pakistan | LwMIC, SA | 220.9 | 4.2 | [161] | 1 | 0.7 | Household Integrated Economic Survey, 2015/16 | |
| Brazil | UMIC, LAC | 212.6 | 4.0 | [162] | 1 | 0.7 | Brazilian Longitudinal Study of Aging (Estudo Longitudinal de Saude dos Idosos Brasileiros, ELSI) *, 2015/16 | |
| Philippines | LwMIC, EAP | 109.6 | 2.1 | [163] | 1 | 0.7 | Family Income and Expenditure Surveys, 2000, 2003, 2006, 2009, & 2012 | |
| South Africa | UMIC, SSA | 59.3 | 1.1 | [164] | 1 | 0.7 | Study on Global AGEing and Adult Health (SAGE) South Africa*, 2007/08 | |
| Argentina | UMIC, LAC | 45.4 | 0.9 | [165] | 1 | 0.7 | National Survey of Household Expenditure 2012/13 | |
| Sudan | LIC, SSA | 43.8 | 0.8 | [166] | 1 | 0.7 | National Baseline Household Survey, 2009 | |
| Iraq | UMIC, MENA | 40.2 | 0.8 | [167] | 1 | 0.7 | Household Socio-Economic Survey, 2006/07, & 2012 | |
| Afghanistan | LIC, SA | 38.9 | 0.7 | [168] | 1 | 0.7 | Living Conditions Survey, 2016/17 | |
| Morocco | LwMIC, MENA | 36.9 | 0.7 | [169] | 1 | 0.7 | National Household Consumption and Expenditure Survey, 2013/14 | |
| Zambia | LwMIC, SSA | 18.4 | 0.3 | [170] | 1 | 0.7 | Household Health Expenditure and Utilisation Survey, 2014 | |
| Senegal | LwMIC, SSA | 16.7 | 0.3 | [171] | 1 | 0.7 | Poverty Monitoring Survey, 2011 | |
| Tunisia | LwMIC, MENA | 11.8 | 0.2 | [172] | 1 | 0.7 | National Budget and Consumption Survey, 2000, 2005, & 2010 | |
| Haiti | LwMIC, LAC | 11.4 | 0.2 | [32] | 1 | 0.7 | Household Living Conditions survey (Enquete sur les Conditions de Vie des Menages Apres Seisme, ECVMAS), 2012 & 2013 | |
| Sierra Leone | LIC, SSA | 8.0 | 0.2 | [173] | 1 | 0.7 | Integrated Household Survey, 2003 & 2011 | |
| Lao PDR | LwMIC, EAP | 7.3 | 0.1 | [174] | 1 | 0.7 | National Survey on Tuberculosis Patients, 2016 | |
| Kyrgyz Republic | LwMIC, ECA | 6.6 | 0.1 | [175] | 1 | 0.7 | Integrated Household Surveys*, 2012 – 2018 | |
| Liberia | LIC, SSA | 5.1 | 0.1 | [9] | 1 | 0.7 | Household Income and Expenditure Survey, 2014 | |
| Jamaica | UMIC, LAC | 3.0 | 0.1 | [176] | 1 | 0.7 | Jamaica Survey of Living Conditions, 1996 -2002, 2004, 2006 – 2010, 2012 | |
| Kosovo | UMIC, ECA | 1.8 | 0.0 | [177] | 1 | 0.7 | Household Budget Survey, 2014 | |
| Eswatini (formerly Swaziland) | LwMIC, SSA | 1.2 | 0.0 | [178] | 1 | 0.7 | Household Income and Expenditure Survey, 2009/10 | |
| Total |
42 countries: LIC = 7 LwMIC = 23 UMIC = 12 EAP = 9 ECA = 3 LAC = 7 MENA = 4 SA = 5 SSA = 14 |
5256.6 LIC = 275.6 LwMIC = 2849.7 UMIC = 2131.3 |
100.0 5.3 54.2 40.5 |
145 studies: 2015 publications = 8 (5.5%) 2016 publications = 11 (7.6%) 2017 publications = 15 (10.3%) 2018 publications = 31 (21.4%) 2019 publications = 24 (16.6%) 2020 publications = 29 (20.0%) 2021 publications = 27 (18.6%) |
145 studies: LIC = 12 LwMIC = 93 UMIC = 40 |
100.0 8.3 64.1 27.6 |
Data year range: 1991/92 – 2017/18 Latest data years: 2007/08–2009/10: 4 countries (LIC = 1, LwMIC = 2, UMIC = 1) 2010/11–2014/15: 17 countries (LIC = 2, LwMIC = 9, UMIC = 6) 2015/16–2017/18: 21 countries (LIC = 4, LwMIC = 12, UMIC = 5) |
|
| Panel B: Multi-country studies (n = 10) | |||||||
|---|---|---|---|---|---|---|---|
| Countries | Income group, region a | Studies reviewed | Data sources | ||||
| 122 countries | 122 countries from all WB income groups, and geographic regions | [19] | Household surveys, 1984–2015 | ||||
| 111 countries | 111 countries from all WB income groups, and geographic regions | [179] | Household surveys, 2005–2014 | ||||
| Latin American countries including 15 LMICs |
LwMIC, LAC (Bolivia, Haiti, Honduras, Nicaragua) UMIC, LAC (Argentina, Brazil, Colombia, Costa Rica, Dominican Republic, Ecuador, Guatemala, Mexico, Panama, Paraguay, Peru) HIC, LAC (Chile, Uruguay) |
[180] | Household surveys, 1990–2013 | ||||
| Bangladesh, Bhutan, India, Maldives, Nepal, Sri Lanka, Thailand, and Timor-Leste |
LwMIC, EAP (Timor-Leste) LwMIC, SA (Bangladesh, Bhutan, India, Nepal, Sri Lanka) UMIC, EAP (Thailand); UMIC, SA (Maldives) |
[181] | Household surveys: Bangladesh (2010), Bhutan (2012), India (2011/12), Maldives (2009), Nepal (2014), Sri Lanka (2012), Thailand (2015), and Timor-Leste (2015) | ||||
| China, Ghana, India, Mexico, the Russian Federation, and South Africa |
LwMIC, SA (India) LwMIC, SSA (Ghana) UMIC, EAP (China) UMIC, LAC (Mexico) UMIC, ECA (Russian Federation) UMIC, SSA (South Africa) |
[182] | World Health Organisation's Study on Global AGEing and Adult Health (WHO SAGE) * wave 2007–2010 | ||||
| Bangladesh, India, Nepal, Pakistan, and Sri Lanka | LwMIC, SA (Bangladesh, India, Nepal, Pakistan, and Sri Lanka) | [183] | World Health Survey, 2002/03 | ||||
| Afghanistan, Bangladesh, India, Nepal, and Pakistan |
LIC, SA (Afghanistan) LwMICs, SA (Bangladesh, India, Nepal, Pakistan) |
[184] | Household surveys: Afghanistan (2014), Bangladesh (2010), India (2012), Nepal (2014), and Pakistan (2014) | ||||
| Egypt, Jordan, and West Bank, and Gaza |
LwMIC, MENA (Egypt, West Bank, and Gaza) UMIC, MENA (Jordan) |
[185] | Household surveys: Egypt (2010/2011); Jordan (2010); West Bank and Gaza (2010) | ||||
| China, and India |
LwMIC, SA (India) UMIC, EAP (China) |
[186] | World Health Organisation's Study on Global AGEing and Adult Health (WHO SAGE) *, wave 2007–2010 | ||||
| China, and India |
LwMIC, SA (India) UMIC, EAP (China) |
[187] | World Health Organisation's Study on Global AGEing and Adult Health (WHO SAGE) *, wave 2007–2010 | ||||
LIC low-income country, LwMIC lower-middle-income country, UMIC upper-middle-income country, LMIC low- and middle-income country, HIC high-income country, EAP East Asia and Pacific, ECA Europe and Central Asia, LAC Latin America and the Caribbean, MENA Middle East and North Africa, SA South Asia, SSA sub-Saharan Africa
aWorld Bank classification of countries by income and region (https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups)
bTotal population data from the World Bank (https://data.worldbank.org/indicator/SP.POP.TOTL)
*Data sources marked with an asterisk represent panel data. All the other data are cross-sectional
Study characteristics
Geographical coverage
Out of the 155 studies included, 145 (94.5%) were single-country studies and 10 (6.5%) were multi-country studies including two to 122 countries (Table 1). The single-country studies were on 42 LMICs from across all geographical regions, representing about 80% of the total LMIC population and 68% of the world’s population as of 2020. Consistent with large populations, the largest number of studies were on India and China, accounting for 24.1% and 15.9% of all single-country studies, respectively. Additionally, eight out of the 10 multi-country studies included India, and five consisted of both India and China. Only 8.3% (n = 12) of the single-country studies were on LICs, focusing on just seven countries.
Source of data
The reviewed studies analysed data collected between 1984 and 2018. The single-country studies produced reasonably recent FRP estimates. The latest available data for 21 of the 42 countries were from 2015 or later years (Table 1). About 85% of the studies (n = 132) analysed cross-sectional household survey data (e.g. household income and expenditure surveys, household living standard surveys, household budget surveys). The rest (n = 23) used data from household panel surveys.
FRP indicators examined
With regard to FRP indicators (Table 2), only one study (0.6%) examined all four indicators of FRP: CHE, impoverishment, coping and FCFR [7]. Most studies assessed any two indicators (49.0%), particularly CHE and impoverishment (39.4%). In total, CHE was the most frequently examined FRP indicator, with over 94% of the studies examining CHE either singly (37.4%) or in conjunction with one or more of the other three indicators (56.7%). Although impoverishment due to OOP payments is not an official UHC indicator of FRP, it was examined in half of the studies. However, the other two non-UHC indicators, coping and FCFR, were seldom recognized and analysed (in 16.8% and 3.9% of all studies, respectively).
Table 2.
Distribution of the studies examining different FRP indicators
| FRP indicators examined | Single-country studies, n (%) | Multi-country studies, n (%) | All studies, n (%) | ||
|---|---|---|---|---|---|
| LIC | LwMIC | UMIC | |||
| CHE only | 2 (16.7) | 30 (32.3) | 23 (57.5) | 3 (30.0) | 58 (37.4) |
| Impoverishment only | 1 (8.3) | 3 (3.2) | 0 (0.0) | 2 (20.0) | 6 (3.9) |
| Coping only | 0 (0.0) | 2 (2.2) | 0 (0.0) | 0 (0.0) | 2 (1.3) |
| FCFR only | 0 (0.0) | 1 (1.1) | 0 (0.0) | 0 (0.0) | 1 (0.6) |
| Any one indicator | 3 (25.0) | 36 (38.7) | 23 (57.5) | 5 (5.0) | 67 (43.2) |
| CHE and impoverishment | 6 (50.0) | 36 (38.7) | 15 (37.5) | 4 (40.0) | 61 (39.4) |
| CHE and coping | 1 (8.3) | 11 (11.8) | 0 (0.0) | 1 (10.0) | 13 (8.4) |
| CHE and FCFR | 0 (0.0) | 1 (1.1) | 1 (2.5) | 0 (0.0) | 2 (1.3) |
| Any two indicators | 7 (58.3) | 48 (51.6) | 16 (40.0) | 5 (50.0) | 76 (49.0) |
| CHE, impoverishment and coping | 1 (8.3) | 8 (8.6) | 0 (0.0) | 0 (0.0) | 9 (5.8) |
| CHE, impoverishment and FCFR | 1 (8.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.6) |
| CHE, coping and FCFR | 1 (0.0) | 0 (0.0) | 1 (2.5) | 0 (0.0) | 1 (0.6) |
| Any three indicators | 2 (16.7) | 8 (8.6) | 1 (2.5) | 0 (0.0) | 11 (7.1) |
| All four indicators: CHE, impoverishment, coping and FCFR | 0 (0.0) | 1 (1.1) | 0 (0.0) | 0 (0.0) | 1 (0.6) |
| Total | 12 (100.0) | 93 (100.0) | 40 (100.0) | 10 (100.0) | 155 (100.0) |
| CHE (total) | 11 (91.7) | 87 (93.5) | 40 (100.0) | 8 (80.0) | 146 (94.2) |
| Impoverishment (total) | 9 (75.0) | 48 (51.6) | 15 (37.5) | 6 (60.0) | 78 (50.3) |
| Coping (total) | 2 (16.7) | 22 (23.7) | 1 (2.5) | 1 (10.0) | 26 (16.8) |
| FCFR (total) | 1 (8.3) | 3 (3.2) | 2 (5.0) | 0 (0.0) | 6 (3.9) |
FRP financial risk protection, CHE catastrophic health expenditure, FCFR forgone care for financial reasons, LIC low-income country, LwMIC lower-middle-income country, UMIC upper-middle-income country
Rigour of analysis: examination of the intensities, distribution (equity and drivers) and trends of FRP indicators
About a third of the 146 studies examining the level of CHE incidence and around half of the 78 studies measuring impoverishment incidence also examined the respective intensities in terms of catastrophic (overshoot and/or mean positive overshoot) and impoverishment gaps (normalized poverty gap and/or normalized mean poverty gap). Nearly 80% of the studies (n = 125) showed the distribution of either CHE or impoverishment, out of which close to half performed equity analysis in terms of distribution across household economic status (n = 60) and urban/rural area of residence (n = 62). The analysis of health systems-level drivers of financial hardship such as types of care (inpatient/outpatient) and health facilities (public/private) was available in only 16.8% and 10.4% of the studies, respectively. Drug expense-driven financial hardship was examined in just four studies [32–35].
About 38% (n = 58) of the included studies examined trends in FRP indicators. Eighteen of these studies, most of which were on China, analysed panel data. All but one of these studies treated each round of panel data as cross-sectional data [36]. No study took advantage of the panel data to track whether financial hardship was a short-term or long-term phenomenon (i.e. whether the same households lacked FRP over time).
Methods used to measure FRP indicators
Catastrophic OOP expenditure
The distribution of studies measuring CHE by methods and thresholds applied is shown in Table 3. The reviewed studies relied solely on the three traditional methods of CHE measurement: the budget share, actual food expenditure and normative food expenditure methods [13, 14, 37]. The most frequently used was the budget share method, particularly in the LIC (81.8%), LwMIC (67.8%) and multi-country studies (100.0%). UMIC studies, on the other hand, mainly relied on the normative food expenditure (42.5%) and actual food expenditure methods (35.5%). The arguments for choosing methods, when given, were either “used in previous studies” or “established methods”. Only a quarter of the studies (n = 35) checked the sensitivity of CHE incidence by applying multiple methods. However, we found no strict dominance of any method in terms of the magnitude of CHE incidence. Two thirds of the studies measuring CHE used only one threshold, and the remaining applied multiple thresholds for any given method. The most frequently used threshold was 10% for the budget share method and 40% for both the actual and normative food expenditure methods.
Table 3.
Distribution of the studies by methods and thresholds used for measuring CHE
| Methods of CHE measurement adopted | Single-country studies, n (%) | Multi-country studies, n (%) | All studies, n (%) | ||
|---|---|---|---|---|---|
| LIC | LwMIC | UMIC | |||
| Budget share only | 4 (36.4) | 34 (39.1) | 8 (20.0) | 6 (75.0) | 52 (35.6) |
| Actual food expenditure only | 2 (18.2) | 5 (5.7) | 14 (35.0) | 0 (0.0) | 21 (14.4) |
| Normative food expenditure only | 0 (0.0) | 23 (26.4) | 15 (37.5) | 0 (0.0) | 38 (26.0) |
| Any one method | 6 (54.5) | 62 (71.3) | 37 (92.5) | 6 (75.0) | 111 (76.0) |
| Budget share and actual food expenditure | 3 (27.3) | 14 (16.1) | 1 (2.5) | 1 (12.5) | 19 (13.0) |
| Budget share and normative food expenditure | 1 (9.1) | 8 (9.2) | 2 (5.0) | 1 (12.5) | 12 (8.2) |
| Any two methods | 4 (36.4) | 22 (25.3) | 3 (7.5) | 2 (25.0) | 31 (21.2) |
| Three methods: Budget share, actual food expenditure and normative food expenditure | 1 (9.1) | 3 (3.4) | 0 (0.0) | 0 (0.0) | 4 (2.7) |
| Any method (total) | 11 (100.0) | 87 (100.0) | 40 (100.0) | 8 (100.0) | 146 (100.0) |
| Budget share (total) | 9 (81.8) | 59 (67.8) | 11 (27.5) | 8 (100.0) | 87 (59.6) |
| Actual food expenditure (total) | 6 (54.5) | 22 (25.3) | 15 (37.5) | 1 (12.5) | 44 (30.1) |
| Normative food expenditure (total) | 2 (18.2) | 34 (39.1) | 17 (42.5) | 1 (12.5) | 54 (37.0) |
| Thresholds applied for CHE measurementa | |||||
| Budget share | |||||
| 10% | 9 (100.0) | 54 (91.5) | 8 (72.7) | 4 (50.0) | 75 (86.2) |
| 25% | 6 (66.7) | 22 (37.3) | 4 (36.4) | 1 (12.5) | 33 (37.9) |
| Other | 5 (55.6) | 26 (44.1) | 6 (54.5) | 4 (50.0) | 41 (47.1) |
| Actual food expenditure | |||||
| 40% | 6 (100.0) | 20 (90.9) | 15 (100.0) | 1 (100.0) | 42 (95.5) |
| Other | 4 (66.7) | 15 (68.2) | 3 (20.0) | 1 (100.0) | 23 (52.3) |
| Normative food expenditure | |||||
| 40% | 2 (100.0) | 33 (97.1) | 16 (94.1) | 1 (100.0) | 51 (94.4) |
| Other | 1 (50.0) | 4 (11.8) | 4 (23.5) | 1 (100.0) | 10 (18.5) |
CHE catastrophic health expense, LIC low-income country, LwMIC= lower-middle-income country, UMIC upper-middle-income country
aSince some studies adopt multiple thresholds for the same method, the sum of the percentages for the different thresholds adopted for a given method is more than 100%
Impoverishing OOP expenditure
There were substantial variations in the type of PLs used among the 78 studies assessing impoverishing OOP expenses (Additional file 2). About 85% of these studies used only one of three types of PLs: absolute international PL (IPL) (23.1%), absolute national PL (NPL) (43.6%), relative NPL (17.9%). The remaining 15% used multiple PLs. The absolute IPL applied also varied widely, with a range of US$ 1.00–4.30 per capita per day. While all the studies examining impoverishing OOP expenses defined it as OOP expenses pushing nonpoor households into poverty, one study considered any OOP expenditure by the poor households as further impoverishing and calculated the total impoverishing effect of OOP as the sum of impoverishment and further impoverishment incidence [20].
Coping
The strategies for coping with healthcare expenses identified in a total of 26 studies included borrowing/loans (100.0%), sale of assets (88.5%), contributions from family and friends (26.9%), dissaving (26.9%) and other sources (3.9%). Only three studies explicitly indicated whether loans required interest payments.
FCFR
Among the six studies accounting for FCFR, three reported it under the heading of either health-seeking behaviour or access barriers [12, 32, 38], and the remaining three considered it as a financial burden or FRP indicator [7, 9, 39]. Each of these latter three studies defined FCFR differently: as households with ill individuals who thought their illness warranted care but decided not to seek it because of cost constraints [7]; as households experiencing a health shock, not incurring CHE, and spending less than a specified amount (in this case, US$ 10) in healthcare costs [9]; or as a pair of measures when examining inpatient care expenses through the individual level rather than household level analysis: ill individuals forgoing necessary admissions (judged by a physician) because of financial difficulties, and ill individuals taking early discharge due to financial difficulties [39].
The evidence on FRP in LMICs
Illnesses, all causes
One hundred and ten studies examined at least one of the four indicators of FRP against illnesses of any kind (Additional file 3). Among these, six multi-country studies including two global studies found CHE to vary between 2% and 25% at the 10% threshold of budget share, and impoverishment to be below 5% regardless of the use of NPLs or IPLs. In particular, the rate of OOP-induced impoverishment at the US$ 1.90 per capita per day IPL was the highest (> 4%) in two LMICs among 122 countries from all income groups in the world: Bangladesh and India [19].
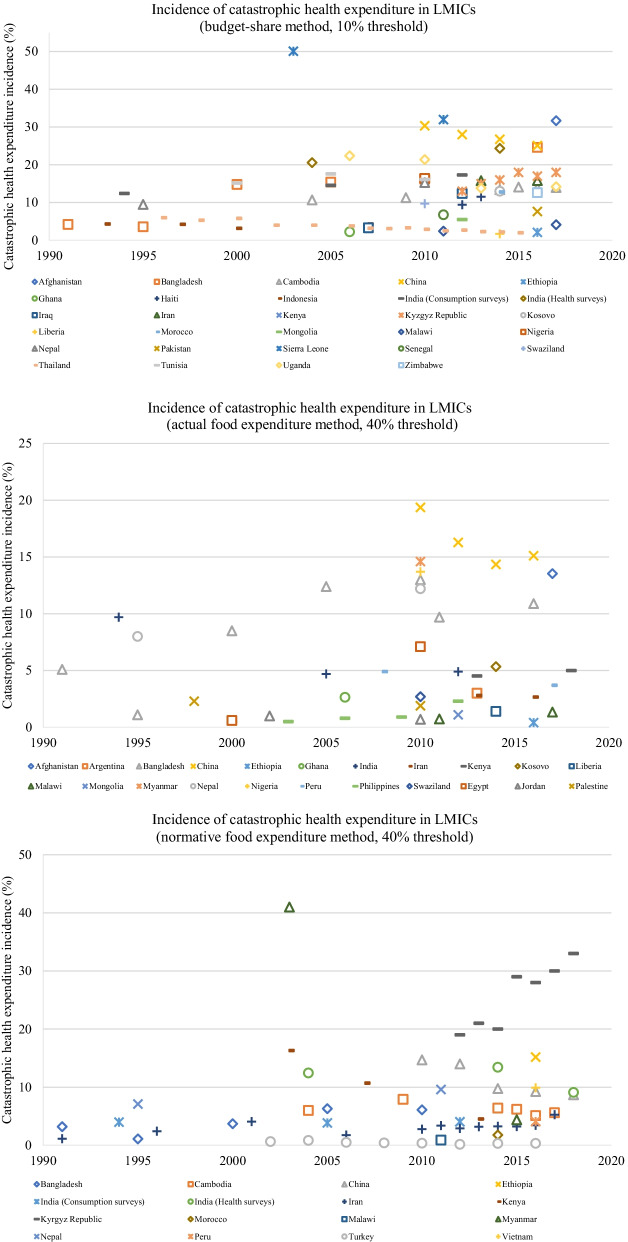
Among the single-country studies, the latest national incidence of CHE at the 10% of budget share varied substantially among LICs and LwMICs, ranging from 1.8% (Liberia) to 32% (Sierra Leone), and 2.24% (Ghana) to 24.6% (Bangladesh), respectively. On the other hand, CHE in UMICs, predominantly measured using the normative food expenditure method at a 40% threshold, ranged between 0.33% (Turkey) and 8.94% (China). However, one study on China measured CHE using the 10% of budget share method and found a marginally higher CHE incidence (25.09%) than the highest in the LwMIC category mentioned earlier. Oddly, the CHE incidence in three LICs, Liberia, Malawi and Ethiopia, was very low—between 1.8% and 4.2% at 10% of budget share—whereas it was around 15% for most LMICs (Fig. 3). In particular, Liberia’s CHE incidence (1.8%) was lower than and Ethiopia’s was comparable (2.1%) to a high-performing UMIC, Thailand (2%).
Fig. 3.
Incidence of CHE experienced due to illnesses (all causes) in LMICs. All estimates are based on national results. When more than one estimate was available across studies, only one was plotted: to show long-term changes, we considered the incidence of CHE from the study with the widest coverage of data years and filled in the incidence for additional years with figures from the other studies on the same country that had figures closer to this study. CHE catastrophic health expense, LMICs low- and middle-income countries
The incidence of impoverishment—defined as the nonpoor households falling into poverty due to OOP expenses—at the absolute IPL of US$ 1.90 per capita per day and country-specific absolute NPLs varied in the LICs from 1.18% (Ethiopia) to 6.84% (Afghanistan) and from 0.6% (Liberia) to 4.1% (Sudan), respectively, and in the LwMICs from 0.03% (Mongolia) to 4.04% (India) and from 0.78% (Mongolia) to 8.0% (India), respectively. Unexpectedly, again, some of the poorest countries in the world, such as Liberia, Malawi and Ethiopia, had an impoverishment rate due to OOP expenses below 1% at the respective absolute NPLs. The dearth of national-level UMIC studies reporting the incidence of impoverishment (n = 6) and the differences in the NPLs and IPLs applied in their measurement restricted meaningful intra- and inter-country income group comparisons.
In terms of coping strategies, borrowing for healthcare expenses was the lowest for Cambodia (2.2–2.5%) and the highest for India (4.3–41.4%) [40, 41]. National incidence for FCFR was available for only three countries: 3.67% in Myanmar, 8% in Liberia and 13.4% in Haiti [7, 9, 32].
Chronic diseases
Thirty-eight studies reported the incidence of FRP indicators related to chronic diseases including NCDs and/or injuries (Additional file 4). With no studies on any LIC, the single-country studies (n = 35/38) were dominated by India (n = 11) and China (n = 10). Only 15 studies reported national results, in which CHE incidence at the 10% of budget share, 40% of nonfood expenditure and 40% of food-based non-subsistence expenditure ranged from 9.6% (Nepal) to 39.7% (Bangladesh), 3.3% (Mongolia) to 17.8% (Bangladesh), and 1.5% (Nepal) to 33.81% (five South Asian LwMICs), respectively. The national incidence of impoverishment, available in just four studies, was between 1.25% (Nepal) and 7.9% (Mongolia) at the country-specific absolute NPL [42, 43]. The few individual disease-specific FRP studies (n = 10) were conducted in China, India and Nepal only. These studies mainly dealt with diabetes, cancers and heart disease, which caused 0–17%, 7.6–58% and 26.8–63.8% of households to incur CHE, respectively. Coping for chronic diseases was mainly reported for India (n = 8/10), where cancer treatment-related hospitalization led to the highest proportion of households (40–50%) borrowing money or selling assets, or seeking contributions from friends and family [44]. No study examined FCFR for chronic diseases.
CDs and maternal and perinatal conditions
FRP studies on CDs (n = 13) were mostly concerned with tuberculosis (TB) in LwMICs (n = 7) (Additional file 5). CHE due to TB could be as high as 80% (Zimbabwe) despite the availability of free treatments in public facilities [45]. Drug-resistant TB was responsible for about 14% to 65% higher burden than the drug-susceptible variety [45, 46]. Note that, in line with WHO’s End TB Strategy to end the global TB epidemic, most TB studies defined OOP expenses as the sum of direct medical, nonmedical and indirect expenditures for seeking TB care [47]. Therefore, one should be cautious when comparing CHE incidence due to TB and other diseases, including any chronic illness. TB treatments pushed at least 14.2% of households into poverty and forced about 5.1–51.5% of households to adopt coping strategies. Notably, no study on FRP from CDs was available for any UMIC.
Care for health conditions, such as childbirth at health facilities in LwMICs, particularly in India, caused at least 20% of households to incur CHE (Additional file 6) [48, 49]. The incidence was two to three times higher when OOP expenses for antenatal, delivery and postnatal care were considered together [50, 51].
FRP through health insurance
The results from examining the protective effect of different health insurance schemes (Additional file 7) suggest that health insurance in LMICs did not consistently offer a higher degree of FRP. Even though insurance lowered CHE in six studies (in Ghana, Iran, Peru, Thailand and Viet Nam) [34, 52–56], three studies reported higher CHE in India, Iran and Kenya [57–59], and another three studies reported not necessarily lower CHE in Colombia, Mexico and Vietnam [60–62]. Again, two of these studies showed mixed results: insured households incurred higher CHE but lower impoverishment than the noninsured in India [57], and CHE decreased but impoverishment increased just after launching the Health Transformation Plan in Iran [56]. Notably, although both Thailand and China brought nearly all people under health insurance coverage (100% and 97%, respectively), the levels of FRP in these countries were quite different. Thailand achieved exemplary low levels of CHE (2% at 10% of budget share) and impoverishment (0.07% at US$ 1.90 per capita per day) by implementing its public health insurance schemes [55]. In comparison, the incidence of CHE and impoverishment for the insured households was quite high in China (about 15% at 40% of non-subsistence expenditure, and 1.3–7.6% at the relative NPL, respectively) [63, 64]. Subgroup studies also did not confirm a protective effect of insurance. However, from the scant number of studies reporting coping strategies (n = 2) and FCFR (n = 2), insurance seemed to slash the need to adopt coping strategies to some degree and removed the financial barriers to accessing healthcare, even though it did not entirely eliminate them [12, 39, 52].
Discussion
This scoping review summarizes the most recent empirical evidence on FRP against the OOP mode of payment for healthcare in LMICs. Compared with the previous relevant review by Alam and Mahal, the volume of LMIC studies has grown substantially since 2015 [24]. The UN’s adoption of the SDG in 2015, which includes FRP as a crucial component of the UHC target (SDG 3.8.2), most likely boosted the literature growth. However, there are significant research gaps.
The country coverage of the LMIC literature was biased towards India and China. Notably, there was a complete absence of studies on FRP from chronic NCDs or injuries in any LIC and CDs in any UMIC. Only one study portrayed a comprehensive picture of FRP in a country (Myanmar) by examining all four indicators of FRP as outlined in our conceptual framework: CHE, impoverishment, coping and FCFR. The LMIC literature conceptualized (the lack of) FRP narrowly, quantifying it mainly through CHE incidence and less frequently through impoverishment incidence. Just a handful of studies identified and measured the adoption of coping strategies and FCFR as indicators of a lack of FRP. Moreover, in measuring CHE, the studies invariably used traditional methods (with the majority placing arguments such as “used in previous studies” or “established methods”), despite their limitations in accurately representing financial catastrophe across households of different economic status. Furthermore, the health systems-level drivers of financial hardship, such as type of service (drugs, diagnosis, etc.), type of care (inpatient/outpatient) and source of care (public/private), were examined in a limited number of studies.
From the available studies, we found FRP to vary across countries. With the variation being substantial among the LICs, there was no discernible pattern in the level of protection amongst the country income categories. Contrary to general expectations, we found three of the poorest countries in the world (Liberia, Ethiopia and Malawi) to have a very low incidence of impoverishment and CHE, comparable to or even lower than some high-performing UMICs. Both CDs and chronic NCDs caused very high CHE, but the respective magnitudes could not be compared because of the differences in measurement methods.
The evidence regarding the protective effect of health insurance in LMICs is mixed in reducing CHE and impoverishment but positive (albeit from a minimal number of studies) in curtailing the need to adopt coping strategies and forgoing needed healthcare for financial reasons. The uneven success in reducing CHE and impoverishment may be due to country-specific variations in the implemented health insurance schemes regarding their type (public, private), service coverage, consumer cost-sharing and provider reimbursement mechanisms, among other factors. Thailand’s exemplary record in reducing CHE and impoverishment is credited to the country’s implementation of general tax-funded public health insurance schemes covering all people and offering a comprehensive benefits package with no co-payment at the point of service [55]. Also vital were health technology assessments to identify cost-effective interventions to add to the benefits package and closed-end provider payments (capitation for outpatient services and diagnosis-related groups under the global budget for inpatient services) [55]. Conversely, the ungenerous benefits package and fee-for-service payment system were the potential factors explaining relatively high CHE and impoverishment (i.e. low FRP) in China despite near-universal insurance coverage [65, 66].
The low incidence of CHE and impoverishment in some of the LICs does not necessarily mean a high level of FRP in those countries. The way these two indicators are defined does not count all the households that lack financial protection. First, the conventional measurement of impoverishment incidence considers only nonpoor households that become poor due to healthcare spending. Therefore, the large number of households already living in extreme poverty in these three LICs (Malawi 69.2%, Ethiopia 30.8%, Liberia 44.4% at US$ 1.90 per capita per day) whose poverty condition may have been aggravated by healthcare expense (i.e. the further impoverished households) were not included in the impoverishment incidence figure [67]. Notably, one LwMIC study we reviewed estimated that the total poverty effect of OOP expenses in Kenya would be about 40 times higher (39.14% instead of 1.02%) if the incidence of further impoverishment (38.12%) were accounted for [20]. The second reason, which explains the low incidence of both impoverishment and CHE, is that these indicators show the effect of seeking healthcare and paying for it. Unless a study assessing FRP includes forgone care or unmet need analysis, it is difficult to determine whether low CHE and impoverishment incidences reflect inadequate service access or high FRP. Poor access to services prevents people from seeking care, resulting in zero OOP payments for their families. These households are not counted as incurring catastrophic or impoverishing OOP expenses, resulting in low incidence of these indicators [68]. The barriers to accessing healthcare could be purely nonfinancial (e.g. unavailable, inaccessible or unacceptable services). In that case, health systems with low CHE and impoverishment may reflect a high degree of FRP (but inadequate access to healthcare). Alternatively, if financial reasons (e.g. affordability) prevent healthcare utilization (i.e. the incidence of FCFR is positive), the CHE and impoverishment incidences underestimate the population lacking FRP. However, it is also essential to recognize that if healthcare is widely accessible for free or at a nominal cost (e.g. insurance-covered care, community-based care, public or donor-funded healthcare), OOP expenses would be zero or sufficiently small to result in low incidence of CHE and impoverishment, reflecting a high degree of FRP (and high access to care).
Central to the SDG agenda is to “leave no one behind”. Likewise, the UHC target specifies that no one should face undue financial hardship to access healthcare. Therefore, identifying further impoverished households and households unable to afford healthcare aligns with the SDG spirit and, needless to say, is crucial to guiding where policies should specifically focus to improve FRP.
Similarly, using methods to measure CHE that do not precisely assess the true incidence across households of different economic status has implications for tracking progress towards achieving UHC, particularly for assessing inequalities within and across countries, which is one of the core concerns of the SDG [15]. The studies in this review, particularly those on LICs and LwMICs, predominantly used the budget share method to measure CHE. The method’s application of constant thresholds ignores that poorer households may react differently to allocating the same fraction of household budget than their wealthier counterparts. Hence, the resulting CHE incidence is likely to be underestimated (and FRP overestimated) for the poor, for whom even minimal healthcare expense can be disastrous.
Even though the advancement of methods for measuring FRP suggests a way forward, the literature shows that LMIC studies have not taken advantage of it. In particular, the normative food, housing (rent) and utilities method considers any healthcare expense of the poor households as catastrophic [18]. Unlike other CHE measurement techniques, this method can achieve an effective threshold that rises with household economic status and thus measures CHE more precisely [15]. Additionally, it highlights three segments of the population that are rarely visible in FRP studies using the traditional methods: households that are further impoverished because of healthcare payments, households that are at risk of impoverishment due to healthcare expenses, and households that do not spend on healthcare, some of whom might have unmet needs due to cost, distance or other barriers [18]. Such a way of assessing FRP yields actionable evidence for policy and promotes pro-poor policies to break the cycle between ill health and poverty [4].
On another note, concerns have been raised about the usefulness of the FRP indicator trends in understanding whether the same households remain trapped in poverty for a long period or whether impoverishment is just a one-time event, which can only be examined if the same households can be tracked over time or if there are frequent panel data [3, 8]. Unfortunately, 18 out of the 23 studies measuring FRP from panel data used more than one round of data (all but one study treated each round of data as cross-sectional), but none examined whether the poverty induced by healthcare was transient or permanent.
Based on the gaps in the literature we have reviewed, we recommend future research on FRP in LMICs to systematically address the gaps in country coverage and disease coverage, and to measure FRP comprehensively using indicators that offer information on the full economic impact of requiring OOP payment for healthcare, while paying specific attention to the use of methods that address the limitations of the traditional techniques for measuring CHE and impoverishment.
Future studies need to place greater emphasis on LICs, particularly in countries where no recent study is available. Even though large global-level studies cover many of the LICs that have no country-specific studies, such studies rarely address the questions of distribution and underlying drivers. Filling the knowledge gap regarding FRP against chronic diseases in LICs is also essential, as SDG 3.4.1—the probability of dying between age 30 and 70 due to leading NCDs (cardiovascular diseases, cancer, diabetes or chronic respiratory diseases)—is the highest in LICs across the globe [69]. Further research is also needed in all LMICs to understand the disease-specific FRP against the NCDs that pose substantial disease burden. Besides cancer, diabetes and cardiovascular diseases, these include mental disorders and respiratory, digestive and genitourinary diseases. Given the recent finding that average treatment costs are higher for respiratory diseases than for cancer, diabetes or cardiovascular diseases in LMICs, FRP against respiratory diseases should be a research priority [70].
Failure to accurately and comprehensively measure the level and pattern of financial protection will result in misguided policy responses. Therefore, to track progress towards UHC in the SDG, we suggest presenting CHE estimates applying all CTP methods, including the normative food, housing (rent) and utilities technique, besides the budget share method. Such studies are expected to facilitate informed decision-making and to prevent potential political manipulation in demonstrating the success or failure of a policy. Presenting CHE measures using all available methods is also warranted given that our study did not find any clear dominance of the magnitude of CHE incidence across methods. We also recommend that future financial protection studies supplement the CHE and impoverishment incidences with coping and FCFR to obtain a comprehensive picture and, as such, valuable insights into the implications of the need to pay for healthcare from OOP on household welfare. It is also necessary to examine context-specific details of the healthcare systems’ components, such as the type of health insurance scheme, its costs and coverage of services, to better understand the mixed results of health insurance protection, and access to healthcare (financial vs nonfinancial barriers to access, community vs hospital-based provision of healthcare, etc.) to make sense of the low incidence of CHE and impoverishment in LICs. Additionally, countries like China should take advantage of their wealth of different longitudinal databases to determine whether the households falling into poverty (or facing CHE) due to healthcare expenses bounce back shortly after or remain wedged in there for an extended period. Such data sources can also be used to validate the hypotheses about the long-term consequences of adopting coping strategies and consequent development of disease and economic impacts associated with forgone treatment.
The main limitation of this review is that it did not include grey literature or studies published in a language other than English. Therefore, we may have missed some potentially relevant national studies which could have broadened the knowledge base.
Conclusion
In this study, we critically reviewed 155 studies published between 2015 and mid-2021 on FRP in healthcare in LMICs. Despite the incredible growth in the literature since 2015 which uses reasonably recent data, major gaps exist. First, while there is at least some research on FRP in every region containing LMICs, there are few studies on LICs. Additionally, the large volume of studies on LwMICs and UMICs mainly focus on India and China, respectively. Second, there is no FRP study on chronic illness in any LIC, and no study on CDs in any UMIC. Also, LMICs of all income categories lack individual disease-specific studies, particularly those that impose high treatment costs and disease burden (such as respiratory diseases). Third, there are gaps in utilizing available data to gain more insight into the drivers and duration of financial hardship. Health systems-level drivers of financial hardship such as types of service, care and health facilities are examined in a limited number of studies. Next, particularly for China, even though panel data were frequently available where the surveyed households could be tracked over the years, there was no attempt to determine whether financial hardship due to OOP health expenses were a one-time or long-term incident for a household. Fourth, the FRP literature in LMICs conceptualizes FRP narrowly. Only one study measures FRP comprehensively by examining all four indicators (CHE, impoverishment, coping and FCFR), each of which addresses a different aspect of FRP. Most studies measure FRP by examining either both CHE and impoverishment (39.4%) or CHE alone (37.4%). Fifth, the studies measuring CHE and impoverishment invariably depend on the traditional measurement methods despite their limitations in accurately representing FRP across households of different economic status. In general, the LMIC literature has not kept pace with the recent development of methodologies that address the limitations of earlier methods. Because of the lack of comprehensive measurement of FRP indicators, coupled with the use of dated measurement methods, the literature is unable to provide a reliable representation of the actual level of protection enjoyed by the households in LMICs.
Disregarding the methodological issues, the available estimates of FRP against illness vary substantially among the countries, with no distinct pattern in the level of protection amongst the country income categories. From the latest available national estimates, the incidence of CHE (any method), impoverishment, coping and FCFR due to illness (all causes) in LMICs ranges from 0.33% to 32%, 0.03% to 8%, 2.2% to 41.4%, and 3.7% to 13.7%, respectively. Surprisingly, some of the poorest countries in the world have very low incidence of CHE and impoverishment, even lower than or comparable to that in Thailand, a high-performing UMIC. LMIC households affected by chronic illness or infectious diseases such as TB experience very high incidence of CHE, ranging from 1.5% to 39.7% and 0.0% to 80.0%, respectively. However, it was not possible to ascertain which of these two broad disease groups caused higher CHE incidence because of the differences in measurement methods. Although it might seem obvious that households with formal health insurance will enjoy greater FRP than those without, the reviewed studies indicate that this is not always the case in LMICs.
Future research on FRP in LMICs should thoroughly address the gaps in country coverage and disease coverage, and measure FRP comprehensively using a broader range of indicators that offer information on the full economic impact of OOP health spending, while paying specific attention to the use of methods that address the limitations of the traditional techniques for measuring CHE and impoverishment. Where possible, longitudinal data should be employed to study the long-term consequences of OOP payments for healthcare.
Supplementary Information
Additional file 1. Sample database search string. Search string for PubMed.
Additional file 2. Distribution of studies by poverty lines used in impoverishment incidence measurement. Poverty lines used in impoverishment incidence measurement categorized across single-country and multi-country studies.
Additional file 3. Financial risk protection against all illnesses. The studies on financial risk protection against all illnesses are summarized by author(s) name and year, country, data source, incidences of catastrophic health expenditure, impoverishment, coping, and forgone care for financial reasons.
Additional file 4. Financial risk protection against chronic diseases including noncommunicable diseases and injuries. The studies on financial risk protection against chronic diseases including noncommunicable diseases and injuries are summarized by author(s) name and year, country, data source, disease (study subgroup), incidences of catastrophic health expenditure, impoverishment, and coping.
Additional file 5. Financial risk protection against communicable and infectious diseases. The studies on financial risk protection against communicable and infectious diseases are summarized by author(s) name and year, country, data source, disease(s)/condition(s), incidences of catastrophic health expenditure, impoverishment, and coping.
Additional file 6. Financial risk protection against other conditions. The studies on financial risk protection against other conditions are summarized by author(s) name and year, country, data source, conditions, incidences of catastrophic health expenditure, impoverishment, and coping.
Additional file 7. Financial risk protection through insurance and other schemes. The studies on financial risk protection through insurance and other schemes are summarized by author(s) name and year, country, data source, intervention/financial protection scheme examined, disease(s)/condition(s) (subgroup) incidences of catastrophic health expenditure, impoverishment, coping, and forgone care for financial reasons.
Acknowledgements
The authors acknowledge Murdoch University librarians Kelly Rogerson and Bryan Chan for their support with the database search strings. Taslima also acknowledges the research supports received under the Murdoch International Postgraduate Scholarship (MIPS) from Murdoch University, Australia.
Abbreviations
- CD
Communicable disease
- CHE
Catastrophic health expenditure
- EAP
East Asia and Pacific
- ECA
Europe and Central Asia
- FCFR
Forgone care for financial reasons
- FRP
Financial risk protection
- IPL
International poverty line
- LAC
Latin America and the Caribbean
- LIC
Low-income country
- LMIC
Low- and middle-income countries
- LwMIC
Lower-middle-income country
- MENA
Middle East and North Africa
- NCD
Noncommunicable disease
- NPL
National poverty line
- OOP
Out-of-pocket
- PL
Poverty line
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- SDG
Sustainable Development Goals
- SSA
Sub-Saharan Africa
- TB
Tuberculosis
- UHC
Universal health coverage
- UMIC
Upper-middle-income country
- UN
United Nations
- US$
United States dollar
- WB
World Bank
Author contributions
TR developed the conceptual framework with guidance from KA. TR designed the review protocol with support from Murdoch University (Australia) librarians. TR conducted the database search, and KA confirmed the study selection. TR reviewed the articles and prepared the draft; KA and DG supervised this work and reviewed the manuscript. All authors discussed the results, and read and approved the final manuscript.
Funding
This paper is a part of Taslima Rahman’s Ph.D. studies and is funded by the Murdoch International Postgraduate Scholarship (MIPS) from Murdoch University, Australia.
Availability of data and materials
All data analysed during this study are included in this article and its supplementary information files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None declared.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Taslima Rahman, Email: Taslima.Rahman@murdoch.edu.au, Email: taslima137@yahoo.com.
Dominic Gasbarro, Email: D.Gasbarro@murdoch.edu.au.
Khurshid Alam, Email: khurshid.alam@murdoch.edu.au.
References
- 1.World Health Organization. The World Health Report: Health Systems Financing: the path to universal coverage: World Health Organization; 2010. [DOI] [PMC free article] [PubMed]
- 2.United Nations. Resolution adopted by the General Assembly on 25 September 2015 2015. https://www.un.org/en/development/desa/population/migration/generalassembly/docs/globalcompact/A_RES_70_1_E.pdf.
- 3.Saksena P, Hsu J, Evans DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med. 2014;11(9):e1001701. doi: 10.1371/journal.pmed.1001701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Tracking universal health coverage: 2017 global monitoring report. 2017.
- 5.World Health Organization. Primary health care on the road to universal health coverage: 2019 global monitoring report. 2021.
- 6.Murphy A, McGowan C, McKee M, Suhrcke M, Hanson K. Coping with healthcare costs for chronic illness in low-income and middle-income countries: a systematic literature review. BMJ Glob Health. 2019;4(4):e001475. doi: 10.1136/bmjgh-2019-001475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ergo A, Htoo TS, Badiani-Magnusson R, Royono R. A new hope: from neglect of the health sector to aspirations for Universal Health Coverage in Myanmar. Health Policy Plan. 2019;34(Supplement_1):i38–i46. doi: 10.1093/heapol/czy110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flores G, Krishnakumar J, O'Donnell O, Van Doorslaer E. Coping with health-care costs: implications for the measurement of catastrophic expenditures and poverty. Health Econ. 2008;17(12):1393–1412. doi: 10.1002/hec.1338. [DOI] [PubMed] [Google Scholar]
- 9.Gabani J, Guinness L. Households forgoing healthcare as a measure of financial risk protection: an application to Liberia. Int J Equity Health. 2019;18(1):1–12. doi: 10.1186/s12939-019-1095-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yadav J, John D, Menon GR, Allarakha S. Out-of-pocket payments for delivery care in India: do households face hardship financing? J Health Manag. 2021;23(2):197–225. doi: 10.1177/09720634211011552. [DOI] [Google Scholar]
- 11.Kruk ME, Goldmann E, Galea S. Borrowing and selling to pay for health care in low-and middle-income countries. Health Aff. 2009;28(4):1056–1066. doi: 10.1377/hlthaff.28.4.1056. [DOI] [PubMed] [Google Scholar]
- 12.Doubova SV, Pérez-Cuevas R, Canning D, Reich MR. Access to healthcare and financial risk protection for older adults in Mexico: secondary data analysis of a national survey. BMJ Open. 2015;5(7):e007877. doi: 10.1136/bmjopen-2015-007877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagstaff A, Doorslaer EV. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993–1998. Health Econ. 2003;12(11):921–933. doi: 10.1002/hec.776. [DOI] [PubMed] [Google Scholar]
- 14.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111–117. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 15.Cylus J, Thomson S, Evetovits T. Catastrophic health spending in Europe: equity and policy implications of different calculation methods. Bull World Health Organ. 2018;96(9):599. doi: 10.2471/BLT.18.209031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Can people afford to pay for health care? New evidence on financial protection in Europe. 2019.
- 17.Wagstaff A, Eozenou PH-V. CATA meets IMPOV: a unified approach to measuring financial protection in health. World Bank Policy Research Working Paper. 2014(6861).
- 18.Thomson S, Evetovits T, Cylus J, Jakab M, World Health O Monitoring financial protection to assess progress towards universal health coverage in Europe. Public Health Panorama. 2016;2(03):357–366. [Google Scholar]
- 19.Wagstaff A, Flores G, Smitz M-F, Hsu J, Chepynoga K, Eozenou P. Progress on impoverishing health spending in 122 countries: a retrospective observational study. Lancet Glob Health. 2018;6(2):e180–e192. doi: 10.1016/S2214-109X(17)30486-2. [DOI] [PubMed] [Google Scholar]
- 20.Barasa E, Nguhiu P, McIntyre D. Measuring progress towards sustainable development goal 3.8 on universal health coverage in Kenya. BMJ Glob Health. 2018;3(3):e000904. doi: 10.1136/bmjgh-2018-000904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ghanbari MK, Behzadifar M, Doshmangir L, Martini M, Bakhtiari A, Alikhani M, et al. Mapping research trends of universal health coverage from 1990 to 2019: bibliometric analysis. JMIR Public Health Surveill. 2021;7(1):e24569. doi: 10.2196/24569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rijal A, Adhikari TB, Khan JAM, Berg-Beckhoff G. The economic impact of non-communicable diseases among households in South Asia and their coping strategy: a systematic review. PLoS ONE. 2018;13(11):e0205745. doi: 10.1371/journal.pone.0205745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Erlangga D, Suhrcke M, Ali S, Bloor K. The impact of public health insurance on health care utilisation, financial protection and health status in low-and middle-income countries: a systematic review. PLoS ONE. 2019;14(8):e0219731. doi: 10.1371/journal.pone.0219731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alam K, Mahal A. Economic impacts of health shocks on households in low and middle income countries: a review of the literature. Glob Health. 2014;10(1):1–18. doi: 10.1186/1744-8603-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Bank. World Bank Country and Lending Groups 2021. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 26.Grépin KA, Irwin BR, Sas TB. On the measurement of financial protection: an assessment of the usefulness of the catastrophic health expenditure indicator to monitor progress towards universal health coverage. Health Syst Reform. 2020;6(1):e1744988. doi: 10.1080/23288604.2020.1744988. [DOI] [PubMed] [Google Scholar]
- 27.World Health O, World B. Global monitoring report on financial protection in health 2021. World Bank; 2021.
- 28.Petrovic D, Marcus K, Sandoval J, Cullati S, Piumatti G, Bodenmann P, et al. Health-related biological and non-biological consequences of forgoing healthcare for economic reasons. Prev Med Rep. 2021;24:101602. doi: 10.1016/j.pmedr.2021.101602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wagstaff A. Poverty and health sector inequalities. Bull World Health Organ. 2002;80:97–105. [PMC free article] [PubMed] [Google Scholar]
- 30.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):1–10. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cros M, Cavagnero E, Alfred JP, Sjoblom M, Collin N, Mathurin T. Equitable realization of the right to health in Haiti: how household data inform health seeking behavior and financial risk protection. Int J Equity Health. 2019;18(1):1–16. doi: 10.1186/s12939-019-0973-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goyanka R, Garg CC, Prasad S. Impoverishment due to out-of-pocket health expenditures: measurement and comparison across different surveys in India. Indian J Hum Dev. 2019;13(2):121–134. doi: 10.1177/0973703019872360. [DOI] [Google Scholar]
- 34.Falconi DP, Bernabé E. Determinants of catastrophic healthcare expenditure in Peru. Int J Health Econ Manag. 2018;18(4):425–436. doi: 10.1007/s10754-018-9245-0. [DOI] [PubMed] [Google Scholar]
- 35.Selvaraj S, Farooqui HH, Karan A. Quantifying the financial burden of households’ out-of-pocket payments on medicines in India: a repeated cross-sectional analysis of National Sample Survey data, 1994–2014. BMJ Open. 2018;8(5):e018020. doi: 10.1136/bmjopen-2017-018020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao Y, Atun R, Oldenburg B, McPake B, Tang S, Mercer SW, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Glob Health. 2020;8(6):e840–e849. doi: 10.1016/S2214-109X(20)30127-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff. 2007;26(4):972–983. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 38.Njagi P, Arsenijevic J, Groot W. Cost–related unmet need for healthcare services in Kenya. BMC Health Serv Res. 2020;20(1):1–12. doi: 10.1186/s12913-020-05189-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y, Dong D, Xu L, Miao Z, Mao W, Sloan F, et al. Ten-year impacts of China’s rural health scheme: lessons for universal health coverage. BMJ Glob Health. 2021;6(4):e003714. doi: 10.1136/bmjgh-2020-003714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jacobs B, de Groot R, Antunes AF. Financial access to health care for older people in Cambodia: 10-year trends (2004–14) and determinants of catastrophic health expenses. Int J Equity Health. 2016;15(1):1–9. doi: 10.1186/s12939-016-0383-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sangar S, Dutt V, Thakur R. Coping with out-of-pocket health expenditure in India: evidence from NSS 71st round. Glob Soc Welfare. 2020;7(3):275–284. doi: 10.1007/s40609-019-00141-8. [DOI] [Google Scholar]
- 42.Swe KT, Rahman MM, Rahman MS, Saito E, Abe SK, Gilmour S, et al. Cost and economic burden of illness over 15 years in Nepal: a comparative analysis. PLoS ONE. 2018;13(4):e0194564. doi: 10.1371/journal.pone.0194564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dugee O, Sugar B, Dorjsuren B, Mahal A. Economic impacts of chronic conditions in a country with high levels of population health coverage: lessons from Mongolia. Trop Med Int Health. 2019;24(6):715–726. doi: 10.1111/tmi.13231. [DOI] [PubMed] [Google Scholar]
- 44.Rajpal S, Kumar A, Joe W. Economic burden of cancer in India: Evidence from cross-sectional nationally representative household survey, 2014. PLoS ONE. 2018;13(2):e0193320. doi: 10.1371/journal.pone.0193320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Timire C, Ngwenya M, Chirenda J, Metcalfe JZ, Kranzer K, Pedrazzoli D, et al. Catastrophic costs among tuberculosis-affected households in Zimbabwe: a national health facility-based survey. Trop Med Int Health. 2021;26(10):1248–55. doi: 10.1111/tmi.13647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nhung NV, Hoa NB, Anh NT, Anh LT, Siroka A, Lönnroth K, et al. Measuring catastrophic costs due to tuberculosis in Viet Nam. Int J Tuberc Lung Dis. 2018;22(9):983–990. doi: 10.5588/ijtld.17.0859. [DOI] [PubMed] [Google Scholar]
- 47.World Health Organization. Implementing the end TB strategy: the essentials. World Health Organization; 2015. Report No.: 9241509937.
- 48.Mohanty SK, Kastor A. Out-of-pocket expenditure and catastrophic health spending on maternal care in public and private health centres in India: a comparative study of pre and post national health mission period. Heal Econ Rev. 2017;7(1):1–15. doi: 10.1186/s13561-016-0141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tripathy JP, Shewade HD, Mishra S, Kumar AMV, Harries AD. Cost of hospitalization for childbirth in India: how equitable it is in the post-NRHM era? BMC Res Notes. 2017;10(1):1–9. doi: 10.1186/s13104-017-2729-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Goli S, Rammohan A, Pradhan J. High spending on maternity care in India: what are the factors explaining it? PLoS ONE. 2016;11(6):e0156437. doi: 10.1371/journal.pone.0156437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Singh P, Kumar V, Verma S. How affordable is childbearing in India? An evaluation of maternal healthcare expenditures. Newborn Infant Nurs Rev. 2016;16(4):175–183. doi: 10.1053/j.nainr.2016.09.012. [DOI] [Google Scholar]
- 52.Amponsah S. The incidence of health shocks, formal health insurance, and informal coping mechanisms. Perspect Glob Dev Technol. 2016;15(6):665–695. doi: 10.1163/15691497-12341412. [DOI] [Google Scholar]
- 53.Hernández-Vásquez A, Rojas-Roque C, Vargas-Fernández R, Rosselli D. Measuring out-of-pocket payment, catastrophic health expenditure and the related socioeconomic inequality in Peru: a comparison between 2008 and 2017. J Prev Med Public Health. 2020;53(4):266. doi: 10.3961/jpmph.20.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahmed S, Szabo S, Nilsen K. Catastrophic healthcare expenditure and impoverishment in tropical deltas: evidence from the Mekong Delta region. Int J Equity Health. 2018;17(1):1–13. doi: 10.1186/s12939-018-0757-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tangcharoensathien V, Tisayaticom K, Suphanchaimat R, Vongmongkol V, Viriyathorn S, Limwattananon S. Financial risk protection of Thailand’s universal health coverage: results from series of national household surveys between 1996 and 2015. Int J Equity Health. 2020;19(1):1–12. doi: 10.1186/s12939-020-01273-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abdi Z, Hsu J, Ahmadnezhad E, Majdzadeh R, Harirchi I. An analysis of financial protection before and after the Iranian Health Transformation Plan. East Mediterr Health J. 2020;26(9):1025–1033. doi: 10.26719/emhj.19.026. [DOI] [PubMed] [Google Scholar]
- 57.Mohanty SK, Dwivedi LK. Addressing data and methodological limitations in estimating catastrophic health spending and impoverishment in India, 2004–18. Int J Equity Health. 2021;20(1):1–18. doi: 10.1186/s12939-021-01421-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kazemi-Karyani A, Woldemichael A, Soofi M, Matin BK, Soltani S, Dizaj JY. Explaining socioeconomic inequality differences in catastrophic health expenditure between urban and rural areas of Iran after health transformation plan implementation. ClinicoEcon Outcomes Res CEOR. 2020;12:669. doi: 10.2147/CEOR.S261520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Njagi P, Arsenijevic J, Groot W. Decomposition of changes in socioeconomic inequalities in catastrophic health expenditure in Kenya. PLoS ONE. 2020;15(12):e0244428. doi: 10.1371/journal.pone.0244428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Amaya-Lara JL. Catastrophic expenditure due to out-of-pocket health payments and its determinants in Colombian households. Int J Equity Health. 2016;15(1):1–11. doi: 10.1186/s12939-016-0472-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nikoloski Z, Mossialos E. Membership in Seguro Popular in Mexico linked to a small reduction in catastrophic health expenditure. Health Aff. 2018;37(7):1169–1177. doi: 10.1377/hlthaff.2017.1510. [DOI] [PubMed] [Google Scholar]
- 62.Thu Thuong NT, Van Den Berg Y, Huy TQ, Tai DA, Anh BNH. Determinants of catastrophic health expenditure in Vietnam. Int J Health Plann Manag. 2021;36(2):316–333. doi: 10.1002/hpm.3076. [DOI] [PubMed] [Google Scholar]
- 63.Wang J, Zhu H, Liu H, Wu K, Zhang X, Zhao M, et al. Can the reform of integrating health insurance reduce inequity in catastrophic health expenditure? Evidence from China. Int J Equity Health. 2020;19(1):1–15. doi: 10.1186/1475-9276-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu H, Zhu H, Wang J, Qi X, Zhao M, Shan L, et al. Catastrophic health expenditure incidence and its equity in China: a study on the initial implementation of the medical insurance integration system. BMC Public Health. 2019;19(1):1–12. doi: 10.1186/s12889-018-6343-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu C, Liu Z-M, Nicholas S, Wang J. Trends and determinants of catastrophic health expenditure in China 2010–2018: a national panel data analysis. BMC health Serv Res. 2021;21(1):1–12. doi: 10.1186/s12913-020-05996-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhao Y, Oldenburg B, Mahal A, Lin Y, Tang S, Liu X. Trends and socio-economic disparities in catastrophic health expenditure and health impoverishment in China: 2010 to 2016. Trop Med Int Health. 2020;25(2):236–247. doi: 10.1111/tmi.13344. [DOI] [PubMed] [Google Scholar]
- 67.World Bank. Data. Poverty headcount ratio at $1.90 a day (2011 PPP) (% of population) 2021.: https://data.worldbank.org/indicator/SI.POV.DDAY.
- 68.Moreno-Serra R, Millett C, Smith PC. Towards improved measurement of financial protection in health. PLoS Med. 2011;8(9):e1001087. doi: 10.1371/journal.pmed.1001087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.World Health Organization. The Global Health Observatory 2022. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/probability-(-)-of-dying-between-age-30-and-exact-age-70-from-any-of-cardiovascular-disease-cancer-diabetes-or-chronic-respiratory-disease.
- 70.Kazibwe J, Tran PB, Annerstedt KS. The household financial burden of non-communicable diseases in low-and middle-income countries: a systematic review. Health Res Policy Syst. 2021;19(1):1–15. doi: 10.1186/s12961-021-00732-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brinda EM, Kowal P, Attermann J, Enemark U. Health service use, out-of-pocket payments and catastrophic health expenditure among older people in India: the WHO Study on global AGEing and adult health (SAGE) J Epidemiol Commun Health. 2015;69(5):489–494. doi: 10.1136/jech-2014-204960. [DOI] [PubMed] [Google Scholar]
- 72.Tripathy JP, Prasad BM, Shewade HD, Kumar AMV, Zachariah R, Chadha S, et al. Cost of hospitalisation for non-communicable diseases in India: are we pro-poor? Trop Med Int Health. 2016;21(8):1019–1028. doi: 10.1111/tmi.12732. [DOI] [PubMed] [Google Scholar]
- 73.Ahmad N, Aggarwal K. Health shock, catastrophic expenditure and its consequences on welfare of the household engaged in informal sector. J Public Health. 2017;25(6):611–624. doi: 10.1007/s10389-017-0829-9. [DOI] [Google Scholar]
- 74.Kastor A, Mohanty SK. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: do Indian households face distress health financing? PLoS ONE. 2018;13(5):e0196106. doi: 10.1371/journal.pone.0196106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee THJ, Saran I, Rao KD. Ageing in India: financial hardship from health expenditures. Int J Health Plann Manag. 2018;33(2):414–425. doi: 10.1002/hpm.2478. [DOI] [PubMed] [Google Scholar]
- 76.Mohanty SK, Kim R, Khan PK, Subramanian SV. Geographic variation in household and catastrophic health spending in India: assessing the relative importance of villages, districts, and states, 2011–2012. Milbank Q. 2018;96(1):167–206. doi: 10.1111/1468-0009.12315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pandey A, Kumar GA, Dandona R, Dandona L. Variations in catastrophic health expenditure across the states of India: 2004 to 2014. PLoS ONE. 2018;13(10):e0205510. doi: 10.1371/journal.pone.0205510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pandey A, Ploubidis GB, Clarke L, Dandona L. Trends in catastrophic health expenditure in India: 1993 to 2014. Bull World Health Organ. 2018;96(1):18. doi: 10.2471/BLT.17.191759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ranjan A, Dixit P, Mukhopadhyay I, Thiagarajan S. Effectiveness of government strategies for financial protection against costs of hospitalization Care in India. BMC Public Health. 2018;18(1):1–12. doi: 10.1186/s12889-018-5431-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sangar S, Dutt V, Thakur R. Economic burden, impoverishment and coping mechanisms associated with out-of-pocket health expenditure: analysis of rural-urban differentials in India. J Public Health. 2018;26(5):485–494. doi: 10.1007/s10389-018-0904-x. [DOI] [Google Scholar]
- 81.Tripathy JP, Prasad BM. Cost of diabetic care in India: an inequitable picture. Diabetes Metab Syndr. 2018;12(3):251–255. doi: 10.1016/j.dsx.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 82.Tripathy JP, Jagnoor J, Prasad BM, Ivers R. Cost of injury care in India: cross-sectional analysis of National Sample Survey 2014. Inj Prev. 2018;24(2):116–122. doi: 10.1136/injuryprev-2017-042318. [DOI] [PubMed] [Google Scholar]
- 83.Ranjan A, Thiagarajan S, Garg S, Danda D. Progress towards universal health coverage in the context of rheumatic diseases in India. Int J Rheum Dis. 2019;22(5):880–889. doi: 10.1111/1756-185X.13488. [DOI] [PubMed] [Google Scholar]
- 84.Sangar S, Dutt V, Thakur R. Burden of out-of-pocket health expenditure and its impoverishment impact in India: evidence from National Sample Survey. J Asian Public Policy. 2019 doi: 10.1080/17516234.2019.1601065. [DOI] [Google Scholar]
- 85.Sangar S, Dutt V, Thakur R. Comparative assessment of economic burden of disease in relation to out of pocket expenditure. Front Public Health. 2019;7:9. doi: 10.3389/fpubh.2019.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sangar S, Dutt V, Thakur R. Distress financing of out-of-pocket health expenditure in India. Rev Dev Econ. 2019;23(1):314–330. doi: 10.1111/rode.12540. [DOI] [Google Scholar]
- 87.Sangar S, Dutt V, Thakur R. Economic burden, impoverishment, and coping mechanisms associated with out-of-pocket health expenditure in India: a disaggregated analysis at the state level. Int J Health Plann Manag. 2019;34(1):e301–e313. doi: 10.1002/hpm.2649. [DOI] [PubMed] [Google Scholar]
- 88.Sangar S, Dutt V, Thakur R. Rural–urban differentials in out-of-pocket health expenditure and resultant impoverishment in India: evidence from NSSO 71st Round. Asia-Pac J Reg Sci. 2019;3(1):273–291. doi: 10.1007/s41685-018-0095-z. [DOI] [Google Scholar]
- 89.Akhtar A, Ahmad N, Chowdhury IR. Socio-economic inequality in catastrophic health expenditure among households in India: a decomposition analysis. Indian Econ Rev. 2020;55(2):339–369. doi: 10.1007/s41775-020-00093-3. [DOI] [Google Scholar]
- 90.Dwivedi R, Pradhan J, Athe R. Measuring catastrophe in paying for healthcare: a comparative methodological approach by using National Sample Survey, India. Int J Health Plann Manag. 2021 doi: 10.1002/hpm.3272. [DOI] [PubMed] [Google Scholar]
- 91.Prasad BM, Tripathy JP, Muraleedharan VR, Tonsing J. Rising catastrophic expenditure on households due to tuberculosis: is India moving away from the END-TB goal? Front Public Health. 2021;9:28. doi: 10.3389/fpubh.2021.614466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rajasulochana SR, Kar SS. Economic burden associated with stroke in India: Insights from National Sample Survey 2017–18. Expert Rev Pharmacoecon Outcomes Res. 2021 doi: 10.1080/14737167.2021.1941883. [DOI] [PubMed] [Google Scholar]
- 93.Verma VR, Kumar P, Dash U. Assessing the household economic burden of non-communicable diseases in India: evidence from repeated cross-sectional surveys. BMC Public Health. 2021;21(1):1–22. doi: 10.1186/s12889-021-10828-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yadav J, Allarakha S, Menon GR, John D, Nair S. Socioeconomic impact of hospitalization expenditure for treatment of noncommunicable diseases in India: a repeated cross-sectional analysis of national sample survey data, 2004 to 2018. Value Health Reg Issues. 2021;24:199–213. doi: 10.1016/j.vhri.2020.12.010. [DOI] [PubMed] [Google Scholar]
- 95.Yadav J, John D, Allarakha S, Menon GR. Rising healthcare expenditure on tuberculosis: can India achieve the End TB goal? Trop Med Int Health. 2021 doi: 10.1111/tmi.13648. [DOI] [PubMed] [Google Scholar]
- 96.Yadav J, Menon G, Agarwal A, John D. Burden of injuries and its associated hospitalization expenditure in India. Int J Inj Control Saf Promot. 2021 doi: 10.1080/17457300.2021.1879163. [DOI] [PubMed] [Google Scholar]
- 97.Wang Z, Li X, Chen M. Catastrophic health expenditures and its inequality in elderly households with chronic disease patients in China. Int J Equity Health. 2015;14(1):1–11. doi: 10.1186/1475-9276-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sun X, Bernabé E, Liu X, Gallagher JE, Zheng S. Determinants of catastrophic dental health expenditure in China. PLoS ONE. 2016;11(12):e0168341. doi: 10.1371/journal.pone.0168341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Liu K, Yang J, Lu C. Is the medical financial assistance program an effective supplement to social health insurance for low-income households in China? A cross-sectional study. Int J Equity Health. 2017;16(1):1–13. doi: 10.1186/s12939-017-0638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Li C, Young B-R, Jian W. Association of socioeconomic status with financial burden of disease among elderly patients with cardiovascular disease: evidence from the China Health and Retirement Longitudinal Survey. BMJ Open. 2018;8(3):e018703. doi: 10.1136/bmjopen-2017-018703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ma X, Wang Z, Liu X. Progress on catastrophic health expenditure in China: evidence from China family panel studies (CFPS) 2010 to 2016. Int J Environ Res Public Health. 2019;16(23):4775. doi: 10.3390/ijerph16234775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ma M, Li Y, Wang N, Wu Q, Shan L, Jiao M, et al. Does the medical insurance system really achieved the effect of poverty alleviation for the middle-aged and elderly people in China? Characteristics of vulnerable groups and failure links. BMC Public Health. 2020;20(1):1–15. doi: 10.1186/s12889-019-7969-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sun J, Lyu S. The effect of medical insurance on catastrophic health expenditure: evidence from China. Cost Effect Resour Alloc. 2020;18(1):1–11. doi: 10.1186/s12962-020-00206-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Xu X, Gu H, You H, Bai L, Li D, Cui N, et al. Are people enrolled in NCMS and CURBMI susceptible in catastrophic health expenditure? Evidence from China. INQUIRY J Health Care Organ Provis Financ. 2020;57:0046958020919282. doi: 10.1177/0046958020919282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhao Y, Zhang L, Fu Y, Wang M, Zhang L. Socioeconomic disparities in cancer treatment, service utilization and catastrophic health expenditure in China: a cross-sectional analysis. Int J Environ Res Public Health. 2020;17(4):1327. doi: 10.3390/ijerph17041327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yang W. Understanding the non-medical costs of healthcare: evidence from inpatient care for older people in China. China Q. 2020;242:487–507. doi: 10.1017/S0305741019001115. [DOI] [Google Scholar]
- 107.Zhong Z, Wei H, Yang L, Yao T, Mao Z, Sun Q. Catastrophic health expenditure: a comparative analysis of smoking and non-smoking households in China. PLoS ONE. 2020;15(5):e0233749. doi: 10.1371/journal.pone.0233749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fu X-z. Financial protection effects of private health insurance: experimental evidence from Chinese households with resident basic medical insurance. Int J Equity Health. 2021;20(1):1–13. doi: 10.1186/s12939-021-01468-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ma M, Tian W, Kang J, Li Y, Xia Q, Wang N, et al. Does the medical insurance system play a real role in reducing catastrophic economic burden in elderly patients with cardiovascular disease in China? Implication for accurately targeting vulnerable characteristics. Glob Health. 2021;17(1):1–13. doi: 10.1186/s12992-021-00683-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Liu S, Coyte PC, Fu M, Zhang Q. Measurement and determinants of catastrophic health expenditures among the elderly in China using longitudinal data from the CHARLS. Int J Equity Health. 2021;20(1):1–9. doi: 10.1186/s12939-020-01327-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wang N, Gao W, Ma M, Shan L, Fu X, Sun T, et al. The medical insurance system’s weakness to provide economic protection for vulnerable citizens in China: a five-year longitudinal study. Arch Gerontol Geriatr. 2021;92:104227. doi: 10.1016/j.archger.2020.104227. [DOI] [PubMed] [Google Scholar]
- 112.Fu X-Z, Sun Q-W, Sun C-Q, Xu F, He J-J. Urban-rural differences in catastrophic health expenditure among households with chronic non-communicable disease patients: evidence from China family panel studies. BMC Public Health. 2021;21(1):1–16. doi: 10.1186/s12889-021-10887-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhou Y, Wushouer H, Vuillermin D, Guan X, Shi L. Does the universal medical insurance system reduce catastrophic health expenditure among middle-aged and elderly households in China? A longitudinal analysis. Eur J Health Econ. 2021;22(3):463–471. doi: 10.1007/s10198-021-01267-3. [DOI] [PubMed] [Google Scholar]
- 114.Ghiasvand H, Olyaeemanesh A, Majdzadeh R, Abdi Z, Mobinizadeh M. Has the financial protection been materialized in Iranian health system? Analyzing household income and expenditure survey 2003–2014. J Res Health Sci. 2018;18(1):404. [PubMed] [Google Scholar]
- 115.Moradi T, Naghdi S, Brown H, Ghiasvand H, Mobinizadeh M. Decomposing inequality in financial protection situation in Iran after implementing the health reform plan: what does the evidence show based on national survey of households' budget? Int J Health Plann Manage. 2018;33(3):652–661. doi: 10.1002/hpm.2517. [DOI] [PubMed] [Google Scholar]
- 116.Yazdi-Feyzabadi V, Bahrampour M, Rashidian A, Haghdoost A-A, Akbari Javar M, Mehrolhassani MH. Prevalence and intensity of catastrophic health care expenditures in Iran from 2008 to 2015: a study on Iranian household income and expenditure survey. Int J Equity Health. 2018;17(1):1–13. doi: 10.1186/s12939-018-0743-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ahmadnezhad E, Murphy A, Alvandi R, Abdi Z. The impact of health reform in Iran on catastrophic health expenditures: equity and policy implications. Int J Health Plann Manage. 2019;34(4):e1833–e1845. doi: 10.1002/hpm.2900. [DOI] [PubMed] [Google Scholar]
- 118.Kheibari MJ, Esmaeili R, Kazemian M. Impacts of health reform plan in Iran on health payments distributions and catastrophic expenditure. Iran J Public Health. 2019;48(10):1861. [PMC free article] [PubMed] [Google Scholar]
- 119.Rezaei S, Hajizadeh M. Measuring and decomposing socioeconomic inequality in catastrophic healthcare expenditures in Iran. J Prev Med Public Health. 2019;52(4):214. doi: 10.3961/jpmph.19.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yazdi-Feyzabadi V, Mehrolhassani MH, Darvishi A. Measuring catastrophic health expenditures and its inequality: evidence from Iran’s Health Transformation Program. Health Policy Plan. 2019;34(4):316–325. doi: 10.1093/heapol/czz031. [DOI] [PubMed] [Google Scholar]
- 121.Rezaei S, Woldemichael A, Ebrahimi M, Ahmadi S. Trend and status of out-of-pocket payments for healthcare in Iran: equity and catastrophic effect. J Egypt Public Health Assoc. 2020;95(1):1–8. doi: 10.1186/s42506-020-00055-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Akazili J, McIntyre D, Kanmiki EW, Gyapong J, Oduro A, Sankoh O, et al. Assessing the catastrophic effects of out-of-pocket healthcare payments prior to the uptake of a nationwide health insurance scheme in Ghana. Glob Health Action. 2017;10(1):1289735. doi: 10.1080/16549716.2017.1289735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Akazili J, Ataguba JE-O, Kanmiki EW, Gyapong J, Sankoh O, Oduro A, et al. Assessing the impoverishment effects of out-of-pocket healthcare payments prior to the uptake of the national health insurance scheme in Ghana. BMC Int Health Hum Rights. 2017;17(1):1–8. doi: 10.1186/s12914-017-0121-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Pedrazzoli D, Siroka A, Boccia D, Bonsu F, Nartey K, Houben R, et al. How affordable is TB care? Findings from a nationwide TB patient cost survey in Ghana. Trop Med Int Health. 2018;23(8):870–878. doi: 10.1111/tmi.13085. [DOI] [PubMed] [Google Scholar]
- 125.Zhang C, Rahman MS, Rahman MM, Yawson AE, Shibuya K. Trends and projections of universal health coverage indicators in Ghana, 1995–2030: a national and subnational study. PLoS ONE. 2019;14(5):e0209126. doi: 10.1371/journal.pone.0209126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Pedrazzoli D, Carter DJ, Borghi J, Laokri S, Boccia D, Houben RMGJ. Does Ghana's National Health Insurance Scheme provide financial protection to tuberculosis patients and their households? Soc Sci Med. 2021;277:113875. doi: 10.1016/j.socscimed.2021.113875. [DOI] [PubMed] [Google Scholar]
- 127.Khan JAM, Ahmed S, Evans TG. Catastrophic healthcare expenditure and poverty related to out-of-pocket payments for healthcare in Bangladesh—an estimation of financial risk protection of universal health coverage. Health Policy Plan. 2017;32(8):1102–1110. doi: 10.1093/heapol/czx048. [DOI] [PubMed] [Google Scholar]
- 128.Datta BK, Husain MJ, Husain MM, Kostova D. Noncommunicable disease-attributable medical expenditures, household financial stress and impoverishment in Bangladesh. SSM-Popul Health. 2018;6:252–258. doi: 10.1016/j.ssmph.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Rahman MS, Rahman MM, Gilmour S, Swe KT, Abe SK, Shibuya K. Trends in, and projections of, indicators of universal health coverage in Bangladesh, 1995–2030: a Bayesian analysis of population-based household data. Lancet Glob Health. 2018;6(1):e84–e94. doi: 10.1016/S2214-109X(17)30413-8. [DOI] [PubMed] [Google Scholar]
- 130.Molla A, Chi C. How much household healthcare expenditure contributes to poverty? Evidence from the Bangladesh Household Income and Expenditure Survey, 2010. J Poverty. 2020;24(7):627–641. doi: 10.1080/10875549.2020.1742269. [DOI] [Google Scholar]
- 131.Ahmed S, Ahmed MW, Hasan M, Mehdi GG, Islam Z, Rehnberg C, et al. Assessing the incidence of catastrophic health expenditure and impoverishment from out-of-pocket payments and their determinants in Bangladesh: evidence from the nationwide Household Income and Expenditure Survey 2016. Int Health. 2021 doi: 10.1093/inthealth/ihab015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Barasa EW, Maina T, Ravishankar N. Assessing the impoverishing effects, and factors associated with the incidence of catastrophic health care payments in Kenya. Int J Equity Health. 2017;16(1):1–14. doi: 10.1186/s12939-017-0526-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Salari P, Di Giorgio L, Ilinca S, Chuma J. The catastrophic and impoverishing effects of out-of-pocket healthcare payments in Kenya, 2018. BMJ Glob Health. 2019;4(6):e001809. doi: 10.1136/bmjgh-2019-001809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sepehri A, Vu PH. Severe injuries and household catastrophic health expenditure in Vietnam: findings from the Household Living Standard Survey 2014. Public Health. 2019;174:145–153. doi: 10.1016/j.puhe.2019.06.006. [DOI] [PubMed] [Google Scholar]
- 135.Grogger J, Arnold T, León AS, Ome A. Heterogeneity in the effect of public health insurance on catastrophic out-of-pocket health expenditures: the case of Mexico. Health Policy Plan. 2015;30(5):593–599. doi: 10.1093/heapol/czu037. [DOI] [PubMed] [Google Scholar]
- 136.Assebe LF, Negussie EK, Jbaily A, Tolla MTT, Johansson KA. Financial burden of HIV and TB among patients in Ethiopia: a cross-sectional survey. BMJ Open. 2020;10(6):e036892. doi: 10.1136/bmjopen-2020-036892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kiros M, Dessie E, Jbaily A, Tolla MT, Johansson KA, Norheim OF, et al. The burden of household out-of-pocket health expenditures in Ethiopia: estimates from a nationally representative survey (2015–16) Health Policy Plan. 2020;35(8):1003–1010. doi: 10.1093/heapol/czaa044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Obse AG, Ataguba JE. Assessing medical impoverishment and associated factors in health care in Ethiopia. BMC Int Health Hum Rights. 2020;20(1):1–9. doi: 10.1186/s12914-020-00227-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Htet S, Fan V, Alam K, Mahal A. Financial risks from ill health in Myanmar: evidence and policy implications. Asia Pac J Public Health. 2015;27(4):418–428. doi: 10.1177/1010539514558332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Han SM, Rahman MM, Rahman MS, Swe KT, Palmer M, Sakamoto H, et al. Progress towards universal health coverage in Myanmar: a national and subnational assessment. Lancet Glob Health. 2018;6(9):e989–e997. doi: 10.1016/S2214-109X(18)30318-8. [DOI] [PubMed] [Google Scholar]
- 141.Ghimire M, Ayer R, Kondo M. Cumulative incidence, distribution, and determinants of catastrophic health expenditure in Nepal: results from the living standards survey. Int J Equity Health. 2018;17(1):1–12. doi: 10.1186/s12939-018-0736-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Thapa AK, Pandey AR, Kathmandu N. National and provincial estimates of catastrophic health expenditure and its determinants in Nepal. J Nepal Health Res Counc. 2020;18(4):741–746. doi: 10.33314/jnhrc.v18i4.2392. [DOI] [PubMed] [Google Scholar]
- 143.Mussa R. Exit from catastrophic health payments: a method and an application to Malawi. Int J Health Econ Manag. 2016;16(2):163–174. doi: 10.1007/s10754-015-9184-y. [DOI] [PubMed] [Google Scholar]
- 144.McHenga M, Chirwa GC, Chiwaula LS. Impoverishing effects of catastrophic health expenditures in Malawi. Int J Equity Health. 2017;16(1):1–8. doi: 10.1186/s12939-017-0515-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mulaga AN, Kamndaya MS, Masangwi SJ. Examining the incidence of catastrophic health expenditures and its determinants using multilevel logistic regression in Malawi. PLoS ONE. 2021;16(3):e0248752. doi: 10.1371/journal.pone.0248752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Fernandes Antunes A, Jacobs B, de Groot R, Thin K, Hanvoravongchai P, Flessa S. Equality in financial access to healthcare in Cambodia from 2004 to 2014. Health Policy Plan. 2018;33(8):906–919. doi: 10.1093/heapol/czy073. [DOI] [PubMed] [Google Scholar]
- 147.Jithitikulchai T, Feldhaus I, Bauhoff S, Nagpal S. Health equity funds as the pathway to universal coverage in Cambodia: care seeking and financial risk protection. Health Policy Plan. 2021;36(1):26–34. doi: 10.1093/heapol/czaa151. [DOI] [PubMed] [Google Scholar]
- 148.Dorjdagva J, Batbaatar E, Svensson M, Dorjsuren B, Kauhanen J. Catastrophic health expenditure and impoverishment in Mongolia. Int J Equity Health. 2016;15(1):1–9. doi: 10.1186/s12939-016-0395-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dorjdagva J, Batbaatar E, Svensson M, Dorjsuren B, Togtmol M, Kauhanen J. Does social health insurance prevent financial hardship in Mongolia? Inpatient care: a case in point. PLoS ONE. 2021;16(3):e0248518. doi: 10.1371/journal.pone.0248518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Aji B, Mohammed S, Haque MA, Allegri MD. The dynamics of catastrophic and impoverishing health spending in Indonesia: how well does the Indonesian health care financing system perform? Asia Pac J Public Health. 2017;29(6):506–515. doi: 10.1177/1010539517729778. [DOI] [PubMed] [Google Scholar]
- 151.Marthias T, Anindya K, Ng N, McPake B, Atun R, Arfyanto H, et al. Impact of non-communicable disease multimorbidity on health service use, catastrophic health expenditure and productivity loss in Indonesia: a population-based panel data analysis study. BMJ Open. 2021;11(2):e041870. doi: 10.1136/bmjopen-2020-041870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Aregbeshola BS, Khan SM. Out-of-pocket payments, catastrophic health expenditure and poverty among households in Nigeria 2010. Int J Health Policy Manag. 2018;7(9):798. doi: 10.15171/ijhpm.2018.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ataguba JE. Assessing financial protection in health: does the choice of poverty line matter? Health Econ. 2021;30(1):186–193. doi: 10.1002/hec.4172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Narcı HÖ, Şahin İ, Yıldırım HH. Financial catastrophe and poverty impacts of out-of-pocket health payments in Turkey. Eur J Health Econ. 2015;16(3):255–270. doi: 10.1007/s10198-014-0570-z. [DOI] [PubMed] [Google Scholar]
- 155.Manavgat G, Saygili F, Audibert M. Examining the economic burden of out-of-pocket health expenditures for households in different socio-economic groups in Turkey. Sosyoekonomi. 2020;28(46):25–49. [Google Scholar]
- 156.Meemon N, Paek SC. The impact of Thailand's universal coverage scheme on household catastrophic health expenditure. Asia Pac Soc Sci Rev. 2019;19(3):144–54. [Google Scholar]
- 157.Hanna JS, Herrera-Almario GE, Pinilla-Roncancio M, Tulloch D, Valencia SA, Sabatino ME, et al. Use of the six core surgical indicators from the Lancet Commission on Global Surgery in Colombia: a situational analysis. Lancet Glob Health. 2020;8(5):e699–e710. doi: 10.1016/S2214-109X(20)30090-5. [DOI] [PubMed] [Google Scholar]
- 158.Kwesiga B, Zikusooka CM, Ataguba JE. Assessing catastrophic and impoverishing effects of health care payments in Uganda. BMC Health Serv Res. 2015;15(1):1–6. doi: 10.1186/s12913-014-0652-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kwesiga B, Aliti T, Nabukhonzo P, Najuko S, Byawaka P, Hsu J, et al. What has been the progress in addressing financial risk in Uganda? Analysis of catastrophe and impoverishment due to health payments. BMC Health Serv Res. 2020;20(1):1–8. doi: 10.1186/s12913-019-4778-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zeng W, Lannes L, Mutasa R. Utilization of health care and burden of out-of-pocket health expenditure in Zimbabwe: results from a National Household Survey. Health Syst Reform. 2018;4(4):300–312. doi: 10.1080/23288604.2018.1513264. [DOI] [PubMed] [Google Scholar]
- 161.Datta BK, Husain MJ, Asma S. Assessing the relationship between out-of-pocket spending on blood pressure and diabetes medication and household catastrophic health expenditure: evidence from Pakistan. Int J Equity Health. 2019;18(1):1–12. doi: 10.1186/s12939-018-0906-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Bernardes GM, Saulo H, Fernandez RN, Lima-Costa MF, Andrade FBD. Catastrophic health expenditure and multimorbidity among older adults in Brazil. Revista Saúde Pública. 2020;54:125. doi: 10.11606/s1518-8787.2020054002285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Bredenkamp C, Buisman LR. Financial protection from health spending in the Philippines: policies and progress. Health Policy Plan. 2016;31(7):919–927. doi: 10.1093/heapol/czw011. [DOI] [PubMed] [Google Scholar]
- 164.Negin J, Randell M, Raban MZ, Nyirenda M, Kalula S, Madurai L, et al. Health expenditure and catastrophic spending among older adults living with HIV. Glob Public Health. 2017;12(10):1282–1296. doi: 10.1080/17441692.2016.1173717. [DOI] [PubMed] [Google Scholar]
- 165.Abeldaño RA. Analysis of household expenditure on healthcare in Argentina, as a component of universal health coverage. Ciencia Saude Coletiva. 2017;22:1631–1640. doi: 10.1590/1413-81232017225.21102015. [DOI] [PubMed] [Google Scholar]
- 166.Ebaidalla EM, Ali MEM. Determinants and impact of household's out-of-pocket healthcare expenditure in Sudan: evidence from urban and rural population. Middle East Dev J. 2019;11(2):181–198. doi: 10.1080/17938120.2019.1668163. [DOI] [Google Scholar]
- 167.Taniguchi H, Rahman MM, Swe KT, Hussain A, Shibuya K, Hashizume M. Trends and projections of universal health coverage indicators in Iraq, 2000–2030: a national and subnational study. Soc Sci Med. 2021;270:113630. doi: 10.1016/j.socscimed.2020.113630. [DOI] [PubMed] [Google Scholar]
- 168.Dastan I, Abbasi A, Arfa C, Hashimi MN, Alawi SMK. Measurement and determinants of financial protection in health in Afghanistan. BMC Health Serv Res. 2021;21(1):1–15. doi: 10.1186/s12913-021-06613-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Oudmane M, Mourji F, Ezzrari A. The impact of out-of-pocket health expenditure on household impoverishment: evidence from Morocco. Int J Health Plann Manag. 2019;34(4):e1569–e1585. doi: 10.1002/hpm.2848. [DOI] [PubMed] [Google Scholar]
- 170.Masiye F, Kaonga O, Kirigia JM. Does user fee removal policy provide financial protection from catastrophic health care payments? Evidence from Zambia. PLoS ONE. 2016;11(1):e0146508. doi: 10.1371/journal.pone.0146508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Séne LM, Cissé M. Catastrophic out-of-pocket payments for health and poverty nexus: evidence from Senegal. Int J Health Econ Manag. 2015;15(3):307–328. doi: 10.1007/s10754-015-9170-4. [DOI] [PubMed] [Google Scholar]
- 172.Ayadi I, Zouari S. Out-of-pocket health spending and equity implications in Tunisia. Middle East Dev J. 2017;9(1):1–21. doi: 10.1080/17938120.2017.1293362. [DOI] [Google Scholar]
- 173.Edoka I, McPake B, Ensor T, Amara R, Edem-Hotah J. Changes in catastrophic health expenditure in post-conflict Sierra Leone: an Oaxaca-blinder decomposition analysis. Int J Equity Health. 2017;16(1):1–15. doi: 10.1186/s12939-017-0661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Chittamany P, Yamanaka T, Suthepmany S, Sorsavanh T, Siphanthong P, Sebert J, et al. First national tuberculosis patient cost survey in Lao People’s Democratic Republic: assessment of the financial burden faced by TB-affected households and the comparisons by drug-resistance and HIV status. PLoS ONE. 2020;15(11):e0241862. doi: 10.1371/journal.pone.0241862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Iamshchikova M, Mogilevskii R, Onah MN. Trends in out of pocket payments and catastrophic health expenditure in the Kyrgyz Republic post “Manas Taalimi” and “Den Sooluk” health reforms, 2012–2018. Int J Equity Health. 2021;20(1):1–17. doi: 10.1186/s12939-020-01358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Li Z, Li M, Fink G, Bourne P, Bärnighausen T, Atun R. User–fee–removal improves equity of children’s health care utilization and reduces families’ financial burden: evidence from Jamaica. J Glob Health. 2017 doi: 10.7189/jogh.07.010502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Qosaj FA, Froeschl G, Berisha M, Bellaqa B, Holle R. Catastrophic expenditures and impoverishment due to out-of-pocket health payments in Kosovo. Cost Effect Resour Alloc. 2018;16(1):1–12. doi: 10.1186/s12962-018-0086-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Ngcamphalala C, Ataguba JE. An assessment of financial catastrophe and impoverishment from out-of-pocket health care payments in Swaziland. Glob Health Action. 2018;11(1):1428473. doi: 10.1080/16549716.2018.1428473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Wagstaff A, Neelsen S. A comprehensive assessment of universal health coverage in 111 countries: a retrospective observational study. Lancet Glob Health. 2020;8(1):e39–e49. doi: 10.1016/S2214-109X(19)30463-2. [DOI] [PubMed] [Google Scholar]
- 180.Wagstaff A, Dmytraczenko T, Almeida G, Buisman L, Hoang-Vu Eozenou P, Bredenkamp C, et al. Assessing Latin America’s progress toward achieving universal health coverage. Health Aff. 2015;34(10):1704–1712. doi: 10.1377/hlthaff.2014.1453. [DOI] [PubMed] [Google Scholar]
- 181.Wang H, Torres LV, Travis P. Financial protection analysis in eight countries in the WHO South-East Asia Region. Bull World Health Organ. 2018;96(9):610. doi: 10.2471/BLT.18.209858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Goeppel C, Frenz P, Grabenhenrich L, Keil T, Tinnemann P. Assessment of universal health coverage for adults aged 50 years or older with chronic illness in six middle-income countries. Bull World Health Organ. 2016;94(4):276. doi: 10.2471/BLT.15.163832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Alam K, Mahal A. The economic burden of road traffic injuries on households in South Asia. PLoS ONE. 2016;11(10):e0164362. doi: 10.1371/journal.pone.0164362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Rahman MM, Karan A, Rahman MS, Parsons A, Abe SK, Bilano V, et al. Progress toward universal health coverage: a comparative analysis in 5 South Asian countries. JAMA Intern Med. 2017;177(9):1297–1305. doi: 10.1001/jamainternmed.2017.3133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Rashad AS, Sharaf MF. Catastrophic economic consequences of healthcare payments: effects on poverty estimates in Egypt, Jordan, and Palestine. Economies. 2015;3(4):216–234. doi: 10.3390/economies3040216. [DOI] [Google Scholar]
- 186.Kumar K, Singh A, Kumar S, Ram F, Singh A, Ram U, et al. Socio-economic differentials in impoverishment effects of out-of-pocket health expenditure in China and India: evidence from WHO SAGE. PLoS ONE. 2015;10(8):e0135051. doi: 10.1371/journal.pone.0135051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Gwatidzo SD, Williams JS. Diabetes mellitus medication use and catastrophic healthcare expenditure among adults aged 50+ years in China and India: results from the WHO study on global AGEing and adult health (SAGE) BMC Geriatr. 2017;17(1):1–15. doi: 10.1186/s12877-016-0408-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Sample database search string. Search string for PubMed.
Additional file 2. Distribution of studies by poverty lines used in impoverishment incidence measurement. Poverty lines used in impoverishment incidence measurement categorized across single-country and multi-country studies.
Additional file 3. Financial risk protection against all illnesses. The studies on financial risk protection against all illnesses are summarized by author(s) name and year, country, data source, incidences of catastrophic health expenditure, impoverishment, coping, and forgone care for financial reasons.
Additional file 4. Financial risk protection against chronic diseases including noncommunicable diseases and injuries. The studies on financial risk protection against chronic diseases including noncommunicable diseases and injuries are summarized by author(s) name and year, country, data source, disease (study subgroup), incidences of catastrophic health expenditure, impoverishment, and coping.
Additional file 5. Financial risk protection against communicable and infectious diseases. The studies on financial risk protection against communicable and infectious diseases are summarized by author(s) name and year, country, data source, disease(s)/condition(s), incidences of catastrophic health expenditure, impoverishment, and coping.
Additional file 6. Financial risk protection against other conditions. The studies on financial risk protection against other conditions are summarized by author(s) name and year, country, data source, conditions, incidences of catastrophic health expenditure, impoverishment, and coping.
Additional file 7. Financial risk protection through insurance and other schemes. The studies on financial risk protection through insurance and other schemes are summarized by author(s) name and year, country, data source, intervention/financial protection scheme examined, disease(s)/condition(s) (subgroup) incidences of catastrophic health expenditure, impoverishment, coping, and forgone care for financial reasons.
Data Availability Statement
All data analysed during this study are included in this article and its supplementary information files.