Abstract
Purpose:
The impact of non-urologic factors on male lower urinary tract symptoms (LUTS) remains unclear. We investigated cross-sectional and longitudinal associations among anxiety, depression, physical function, sleep quality and urinary symptom sub-domains.
Materials and Methods:
Data from 518 men in the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN) study were analyzed to identify associations between PROMIS depression, anxiety, sleep disturbance, and physical function measures and LUTS sub-domains, as derived from the AUA-Symptom Index and LUTS Tool. Multivariable linear regression was used to assess the relationships between PROMIS measures and LUTS sub-domains at baseline and at 3- and 12-month follow-up.
Results:
Baseline depression and anxiety were associated with urinary incontinence (UI; p<0.001), voiding symptoms (p<0.001), and quality of life (QOL, p=0.002), whereas baseline sleep disturbance was associated with voiding and storage symptoms and QOL (p<0.001 for all). Urinary symptom severity improved in all sub-domains at 3 and 12 months. Similar associations between PROMIS measures and LUTS sub-domains were observed at all time points, but baseline depression, anxiety, sleep disturbance, and physical function measures were not associated with longitudinal trajectories of LUTS.
Conclusions:
Urinary symptom sub-domains are independently associated with modifiable clinical variables including sleep quality and depression at all time points, but these variables do not predict the degree of improvement in LUTS following urologic evaluation and treatment over the medium-term. Bidirectional assessment and randomized experiments may improve our understanding of these relationships.
Keywords: Lower urinary tract symptoms, Patient-reported outcome measures, Quality of life, Depression, Anxiety
Introduction:
Lower urinary tract symptoms (LUTS) are highly prevalent, costly to treat, and negatively impact health-related quality of life.1, 2 The International Continence Society (ICS) groups LUTS into sub-domains including storage symptoms (frequency, urgency, nocturia, and urinary incontinence [UI] including stress, urgency, and mixed UI), voiding symptoms (weak stream, hesitancy, straining, intermittency, split stream), and post-micturition symptoms (i.e., post-void dribbling or post-void UI).3 All types of UI, including post-void UI, are associated with higher degrees of bother,4–6 and although UI was traditionally thought to be uncommon in men, approximately 50% of treatment-seeking men in the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN) Observational Cohort study (the same cohort we are reporting here) reported UI.5
Prior studies have demonstrated that male LUTS are associated with anxiety and depression.1 In men enrolled in the Epidemiology of LUTS (EpiLUTS) study, depression was associated with urinary frequency and incomplete bladder emptying, whereas anxiety was related to nocturia and urinary urgency.1 In a symptom-based cluster analysis of men from LURN, four different groups of men were identified. The group denoted as Cluster M1 (clinically similar to bladder outlet obstruction) reported more severe psychological distress including more perceived stress, sleep dysfunction, and anxiety compared with the other three male clusters. Moreover, depression was higher in Cluster M1 in comparison to Clusters M2 (men with mostly post-void symptoms) and M3 (men with frequency, but no incontinence).7 Furthermore, in general, more severe baseline anxiety and sleep disturbance were associated with overall severity of LUTS.8
One of the barriers to improving diagnosis and management of patients with LUTS has been imprecise physician-led classification of subtypes of LUTS and associated etiologies. In this study, we classify patients based on their presenting symptoms, including voiding symptoms, storage symptoms, the presence of UI, and overall bother.9, 10 Comparisons of how anxiety, depression, physical function, and activity influence these urinary sub-domains has not been performed, and it remains unknown how these factors may influence urinary sub-domains and/or longitudinal changes in LUTS following standard urologic treatment. We examine how non-urologic factors including activity, sleep, and psychosocial factors influence sub-domains of urinary symptoms (voiding, storage, UI, bother) as well as the longitudinal trajectories of LUTS. We hypothesized that these non-urologic factors would be differentially associated with urinary symptom sub-domains and would be associated with the trajectories of LUTS over time.
Materials and Methods:
Study Design and Population
Participants were recruited to the LURN Observational Cohort Study (www.nih-lurn.org) from 2015–2017 at six tertiary referral centers.11 Detailed inclusion criteria have been previously reported.11, 12 Briefly, the study includes adult (≥18 years) treatment-seeking patient presenting to a LURN physician for a return or new-patient visit with at least one lower urinary tract symptom as identified by the LUTS Tool.13 Men with prostate cancer, symptomatic stricture disease, or endoscopic surgery (e.g., transurethral resection of the prostate) within the preceding 6 months were excluded. Baseline demographic and clinical information as well as multiple patient-reported outcome measures were collected at baseline and at 3 and 12 month follow-up. Participants were treated by their physician according to standard best practices.
Measures
Voiding symptoms, storage symptoms, and associated bother were determined using the American Urological Association Symptom Index (AUA-SI)14 as previously described.15–18 Voiding symptoms were defined as incomplete emptying, intermittency, weak stream, and straining. Storage symptoms were defined as frequency, nocturia, and urgency. Bother was evaluated using the AUA-SI Quality of Life (QOL) score. As UI is not captured by the AUA-SI questionnaire, it was assessed by responses to LUTS Tool Question 15: “During the past month, how often did you leak urine?” and Questions 16a-g: “How often in the past week have you (a) leaked urine just after you have finished urinating? (b) leaked urine in connection with a sudden need to rush to urinate? (c) leaked urine in connection with laughing, sneezing, or coughing? (d) leaked urine in connection with physical activities, such as exercising or lifting a heavy object? (e) leaked urine when you are sleeping? (f) leaked urine during sexual activity? (g) leaked urine for no reason?”. Patient-Reported Outcomes Measurement Information System® (PROMIS®) Depression and Anxiety Short Forms 8a,19 Sleep Disturbance Short Form 8b20, and Physical Function Mobility subdomain v1.221 instruments were used to identify associations between PROMIS measures and LUTS sub-domains.
Statistical Methods
Missing data were imputed using the sequential regression technique22 implemented by IVEware 2.0.23 Ten imputed datasets were generated. AUA subscale scores were calculated by summing the relevant items. AUA voiding, storage, and QOL subscales are shown on their raw scale for descriptive analyses but were normalized using the percent of the maximum possible score for multivariable modeling so that effect estimates can be interpreted as a percentage of the maximum possible total scale.24 The LUTS Tool UI questions were combined by calculating the weighted Euclidean distance between the questions, where weights were calculated using the ratio of the total average correlation to the average correlation for each individual item with the other items.25 The score was then normalized by the maximum value and multiplied by 100.
Baseline characteristics of men with LUTS are presented using medians, interquartile ranges (IQR), frequencies, and percentages. Trajectories of LUTS sub-domains and PROMIS measures over time were explored graphically using box plots. Pearson correlations were used to quantify the association between each pair of PROMIS measures and UI, voiding, and storage sub-domains, whereas Spearman’s correlation was used for the QOL score. Multivariable linear regression was used to assess the relationships between baseline PROMIS measures, participant characteristics, and LUTS sub-domains. Model selection was conducted based on a pool of clinically meaningful variables (Table 1) which were then subjected to stepwise selection with p-values of 0.2 on each imputed data set and backwards selection was completed on p-values obtained across multiply imputed data sets using Rubin’s rules. To assess the association between baseline PROMIS measures and longitudinal LUTS sub-domains, similar procedures were performed using mixed effects linear regression models with random participant intercepts. Participants who did not report sub-domain symptoms at baseline were excluded from the corresponding longitudinal models. Hypothesis-driven interactions between PROMIS measures and time from baseline were assessed to determine whether the association between depression, anxiety, sleep disturbance, and physical functioning and LUTS sub-domains varied across follow-up. Models with random slopes were also assessed as a sensitivity analysis. SAS v9.4 (SAS Institute, Cary, NC) was used for all statistical analyses.
Table 1:
Male participant characteristics.
| Male participants (N=518) | ||
|---|---|---|
| Age (years) | 63 (55–70) | |
| Age category | < 45 | 63 (12%) |
| 45 – 54 | 59 (11%) | |
| 55 – 64 | 157 (30%) | |
| 65+ | 239 (46%) | |
| Race1 | White | 415 (81%) |
| Black | 52 (10%) | |
| Asian | 20 (4%) | |
| Other/Multi-racial | 25 (5%) | |
| Ethnicity1 | Hispanic/Latino | 21 (4%) |
| BMI2 | 29 (26–33) | |
| BMI category2 | BMI < 25 | 105 (20%) |
| 25 ≤ BMI < 30 | 204 (40%) | |
| 30 ≤ BMI | 205 (40%) | |
| Diabetes2 | 93 (18%) | |
| Smoking status | Never | 280 (54%) |
| Current or former smoker | 238 (46%) | |
| Sleep apnea2 | 139 (27%) | |
| Treatment group* | OAB medication | 58 (11%) |
| Voiding medication | 180 (35%) | |
| Prostate surgery | 25 (5%) | |
| Behavioral or physical therapy | 61 (12%) |
Note: values shown are median (interquartile range) or count (percent)
Missing <2%
Missing <1%
Treatments at or before enrollment, groups are not mutually exclusive
Results:
Six hundred seven males provided informed consent to the study and 593 had a complete baseline assessment. Among those, 518 males with complete demographic information and at least 15 of 22 non-missing responses to the LUTS Tool severity questions were included in the analysis. Of the 518 men included in the analysis, the median age was 63 years, 81% were white, 40% were obese (BMI ≥ 30), 18% reported a diagnosis of diabetes, and 27% reported sleep apnea (Table 1). The median baseline PROMIS scores were all near the population mean of 50; observed median scores were 48 (IQR 38–53) for depression, 49 (IQR 37–53) for anxiety, 52 (IQR 46–57) for sleep disturbance, and 50 (IQR 43–60) for physical functioning.
We assessed baseline associations of urinary symptom sub-domains with anxiety, depression, sleep disturbance, and physical function PROMIS measures (Supplementary Figure 1A–D). PROMIS depression and anxiety measures were highly correlated (r=0.77). Due to this large correlation, only depression was included in the primary analyses to avoid the problem of multicollinearity in regression models. Depression was significantly associated with UI, voiding, and storage sub-domains (r=0.33, r=0.28, and r=0.20, respectively, p<0.001), as was sleep disturbance (r=0.21, r=0.34, and r=0.33, p<0.001). Physical function showed a smaller association with UI and storage symptoms (r=−0.20 and −0.21, p<0.001), but was not associated with voiding symptoms (r=−0.004, p=0.93). AUA-SI QOL was associated with sleep disturbance (ρ=0.34, p<0.001) and to a slightly lesser degree with depression (ρ=0.27, p<0.001). Although the correlation of QOL with physical function was statistically significant, the association was minimal (ρ=−0.09, p=0.04).
Multivariable analyses demonstrate that depression was strongly associated with UI (effect size estimate 6.3 [95% CI 4.5–8.1], p<0.001), voiding symptoms (estimate 6.0 [95% CI 3.5–8.4], p<0.001), and QOL (estimate 3.8 [95% CI 1.5–6.2], p=0.002), and was moderately associated with storage symptoms (estimate 2.5 [95% CI 0.3–4.7], p=0.03). Sleep disturbance showed a strong association with voiding (estimate 8.1 [95% CI 5.6–10.6], p<0.001) and storage (estimate 7.2 [95% CI 5.0–9.5], p<0.001) sub-domains and QOL (estimate 7.5 [95% CI 5.2–9.9], p<0.001) and was moderately associated with UI symptoms (estimate 2.1 [95% CI 0.04–3.9], p=0.02) (Figure 1; models with covariates shown in Supplementary Table 1). Similar effects were observed when anxiety was used in the model instead of depression (Supplementary Figure 2).
Figure 1. Baseline multivariable linear regression model assessing the relationships between baseline PROMIS measures, participant characteristics, and LUTS sub-domains.
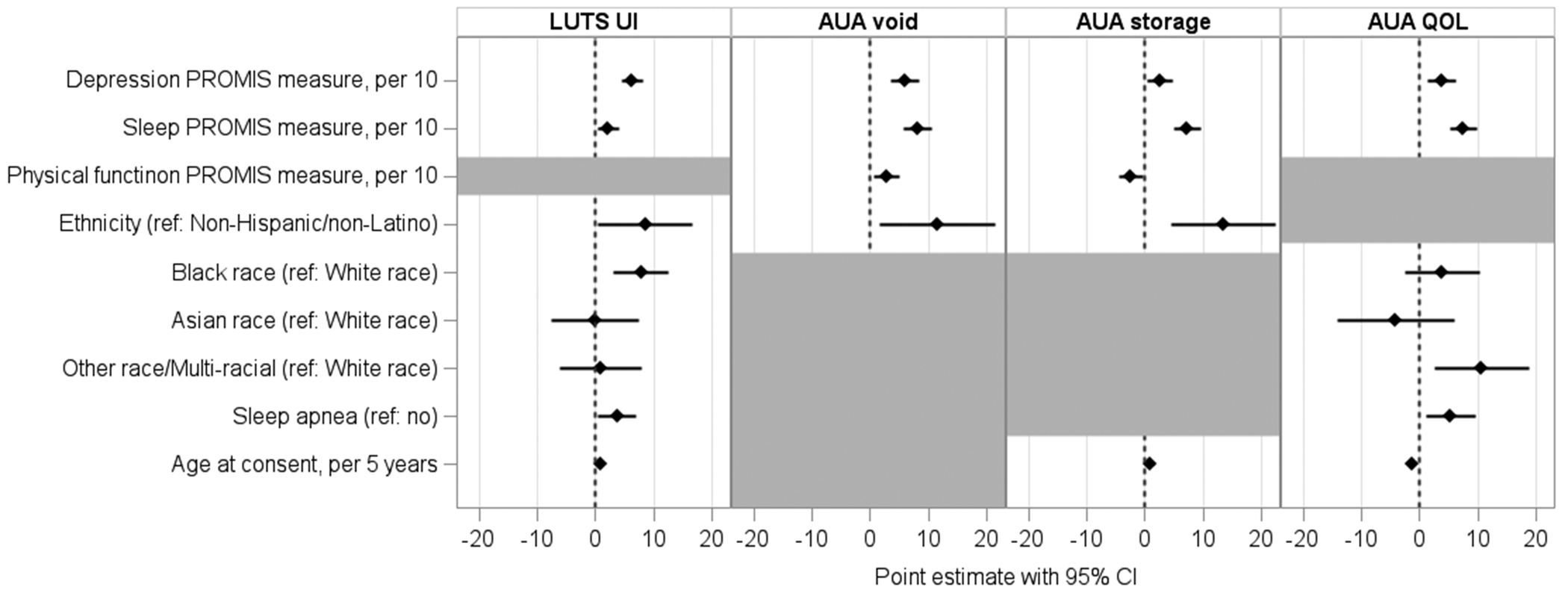
Statistically significant covariate point estimates and corresponding 95% confidence intervals depicted as diamonds and horizontal bars, respectively. Final covariates included in each model are shown, grey shading indicates that covariate was not included in the model depicted in that column. For example, all else equal, for each 10 point increase in the baseline PROMIS depression score, the LUTS UI score increased (i.e. more severe UI) by 6.3 units, on average, where each unit represents 1% of the total scale. Full model results are provided in Supplementary Table 1.
Next, we assessed changes in LUTS sub-domains over time in our sample (i.e., patients receiving standard treatment); treatment categories are shown in Table 1. There were statistically significant improvements in LUTS sub-domains over the study period (Figure 2). On average, the severity of UI decreased slightly over the 12-month period (median score was 20.4, 18.5, 17.8 at baseline, 3-months, 12-months respectively; linear trend test p<0.001), and the severity of voiding symptoms also steadily decreased (median score was 6, 5, 4 at baseline, 3-months, and 12-months, respectively; linear trend test p<0.001). The severity of storage symptoms decreased at 3-months and then plateaued (median score was 7, 5.3, 5 at baseline, 3-months, and 12-months, respectively; linear trend test p<0.001). Finally, median QOL score as reported on the AUA-SI was 4 (mostly dissatisfied) and improved to 3 (about equally satisfied and dissatisfied) at 3- and 12-months, respectively (Figure 2). In contrast, on average, there was not a difference in PROMIS anxiety, depression, sleep distrurbance, or physical function over the study time period (Supplementary Figure 3).
Figure 2. LUTS sub-domains over time.
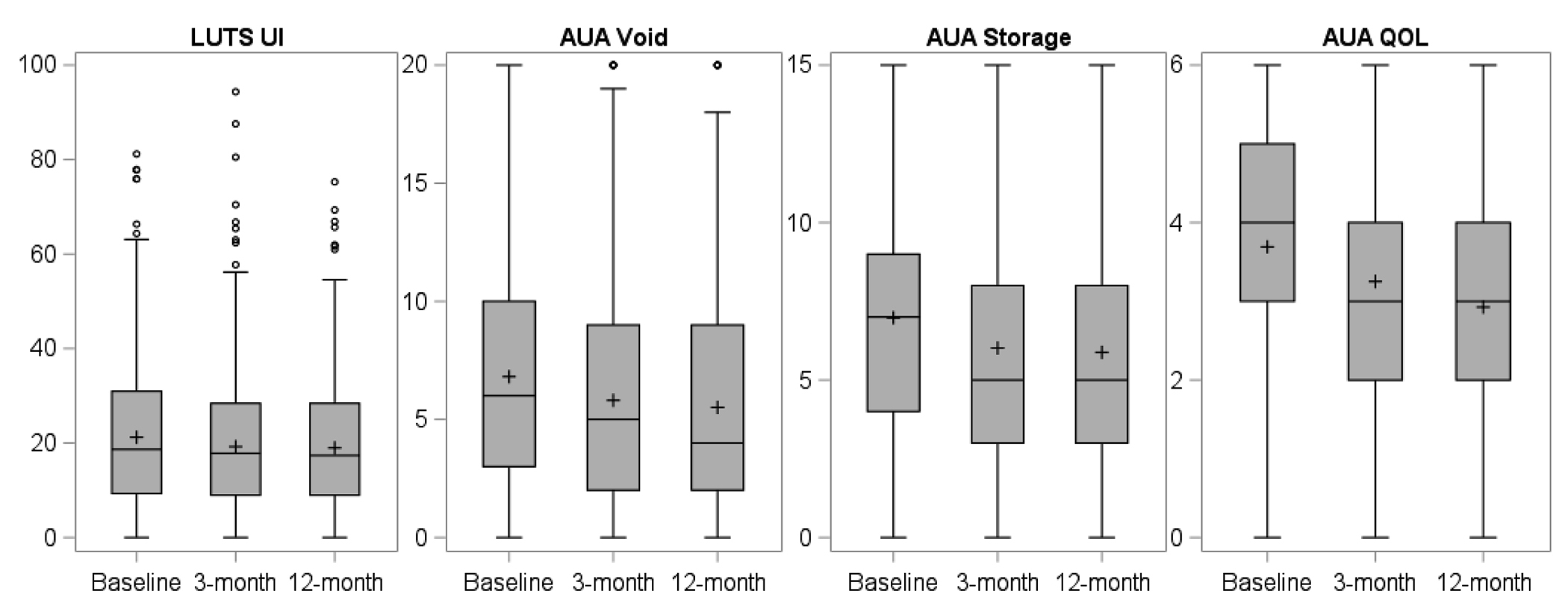
Sub-domains are displayed using the raw scores on the y-axes. Higher UI, voiding, and storage scores represent worse symptom severity, while higher QOL scores represent worse quality of life. The box represents the first to third quartiles (Q1 to Q3, respectively) of scores, with the median depicted by a horizontal line. Mean measures are shown as plus signs. The whiskers extend down from the box to the most extreme observation that is less than or equal Q1 minus 1.5 times the IQR and up from the box to the most extreme observation that is less than or equal to Q3 plus 1.5 times the IQR. Measures that are below or above this cut off, respectively, are graphed as dots.
To examine the relationship of baseline PROMIS measures with LUTS sub-domains over time, we performed multivariable mixed effects linear regression analyses (Figure 3). Overall, symptoms in all sub-domains improved from baseline to the 3- and 12-month follow-ups, but participants with higher baseline PROMIS depression scores reported higher symptom severity across all LUTS sub-domains at all time points (estimates range 2.4 to 5.8). Sleep disturbance was significantly associated with increased voiding symptom severity (estimate 4.6 [95% CI 2.4–6.7], p<0.001), storage symptom severity (estimate 5.7 [95% CI 3.8–7.6], p<0.001), and worse QOL (estimate 6.5 [95% CI 4.6–8.4], p<0.001) at all time points. Sleep apnea was also associated with worse QOL (estimate 5.1 [95% CI 1.7–8.5], p=0.003). Similar effects were seen when anxiety was used in the model instead of depression (Supplementary Figure 4).
Figure 3. Repeated measures linear regression model assessing the relationships between baseline PROMIS measures, participant characteristics, and LUTS sub-domains at follow-up timepoints.
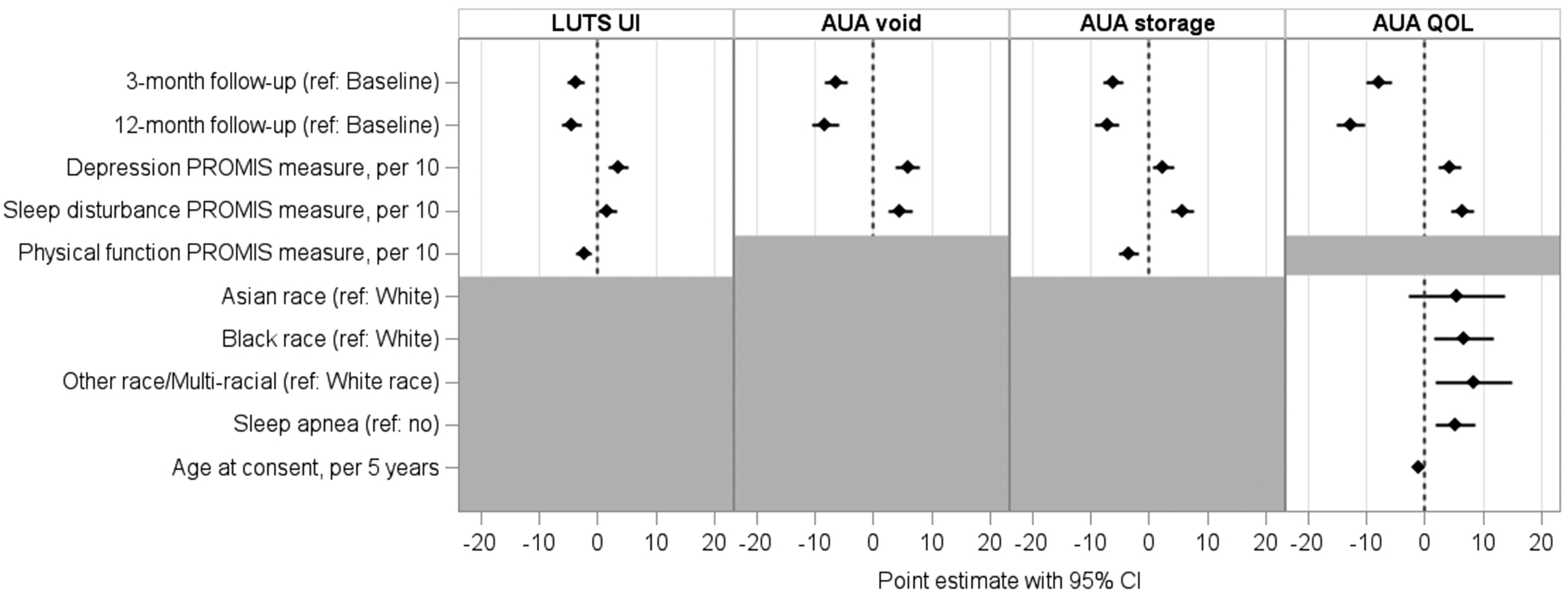
Statistically significant covariate point estimates and corresponding 95% confidence intervals depicted as diamonds and horizontal bars, respectively. Final covariates included in each model are shown, grey shading indicates that covariate was not included in the model depicted in that column. For example, all else equal, for each 10 point increase in the baseline PROMIS depression score, the LUTS UI score increased (i.e. more severe UI) by 4.9 units, on average, where each unit represents 1% of the total scale.
To assess if the association between baseline PROMIS measures and LUTS sub-domains varied over follow-up, interactions with time from baseline and depression, sleep disturbance, and physical function were tested, but all interactions yielded non-significant results. A final sensitivity analysis assessing the correlation between random participant slopes representing change in LUTS sub-domains over time and baseline PROMIS measures revealed no meaningful associations (Pearson correlation range, −0.098–0.068, p-value range 0.03–0.91).
Discussion:
Lower urinary tract symptoms are diverse and associated with many non-urologic factors. Improved understanding of potentially modifiable factors that are associated with sub-domains of LUTS and trajectories of improvement holds the potential to improve care for patients with bothersome LUTS along with guideline-driven urologic care. In this study, we demonstrate that male LUTS sub-domains are independently associated with modifiable clinical variables including anxiety, depression, and sleep disturbance. Furthermore, we demonstrate that in participants undergoing standard treatment, measures of depression, anxiety, and sleep disturbance are associated with LUTS at baseline as well as 3- and 12-month follow-up, but these non-urologic factors did not relate to the trajectory of improvement over time. In other words, clinically, although a patient with depression may have worse LUTS before and after treatment compared to a patient without depression, his relative improvement in LUTS over the medium-term is not associated with his baseline depression.
These results are consistent with, but expand upon the results from the population-based, cross-sectional EpiLUTS internet survey.1, 26 Self-reported depression was associated with voiding symptoms, and voiding plus storage or post-void symptoms, but not storage or post-void symptoms alone.26 Self-reported chronic anxiety was associated with voiding plus post-void symptoms.26 Using PROMIS measures in treatment-seeking patients, we found that anxiety and depression were highly correlated (r=0.77), and were most strongly associated with voiding and UI sub-domains.
Symptom-based cluster analysis of the same LURN cohort analyzed here also demonstrated differential psychological symptoms amongst male clusters.7 However, these clusters have not yet been validated, and clinical application of cluster-based data remains challenging; for example, classification of an individual patient into a cluster remains a work in progress. The present data sub-divides LUTS into clinical symptom categories, consistent with ICS and other classification systems.3 In contrast to ICS terminology, we did group post-void UI with any UI, but we have previously demonstrated that both types of UI are bothersome and common in treatment-seeking men.5 Furthermore, sensitivity analyses demonstrated similar associations of baseline PROMIS anxiety, depression, sleep disturbance, and physical function measures with post-void UI and urgency UI (Supplementary Figure 5).
Several limitations of this study should be noted. The study population was treatment-seeking, and primarily white, non-Hispanic/Latino, and English-speaking, which may limit generalizability. The median age was 63, similar to many studies of men with LUTS, and only 12% of the treatment-seeking population was under age 45. Prevalence of urinary symptoms increases with age, and while age was included in multivariate analyses, care should be taken in generalizing results to younger men with LUTS. In addition, the LURN Observational Cohort study excluded men with prostate cancer (and thus post-prostatectomy patients), so very few men (≤1%) had stress UI; results presented here should not be extrapolated to men with stress UI. The goal of the current study was to use a clinically-relevant and widely used questionnaire (AUA-SI) to categorize presenting LUTS to allow for translatability into current practices, but the AUA-SI lacks questions regarding UI. Future directions will include exploration of these themes with more comprehensive urinary symptom questionnaires (e.g., the LURN-SI-29 or SI-10).27, 28 We did not demonstrate an association between baseline depression, anxiety, sleep disturbance, and physical function measures and trajectories in LUTS over time, nor did we assess if patients were treated for sleep apnea, anxiety, or depression during the LURN Observational Cohort study period. Causality cannot be assessed or assumed in this work, but we suggest that future studies include both randomized experiments where potential causes are manipulated, as well as cross-lagged panel analysis of potential bidirectional relationships29, 30 between these PROMIS measures and LUTS sub-domains. Finally, treatment type was not included in models examining changes over time, however, all participants received standard treatment as determined by their clinician, and as we did not see an effect of baseline PROMIS measures on LUTS sub-domain trajectories, inclusion of treatment data may only over-complicate the presented models.
Conclusions:
Modifiable non-urologic factors including sleep, anxiety, and depression are independently associated with urinary symptom sub-domains at all time points, but are not associated with the degree of change in urinary symptoms following standard urologic treatment over the medium-term. Bidirectional assessment and randomized experiments may expand our understanding of these relationships and improve care for men with LUTS.
Supplementary Material
Supplementary Table 1. Baseline multivariable linear regression model assessing the relationships between baseline PROMIS measures, participant characteristics, and LUTS sub-domains
Supplementary Figure 1A-D. Baseline associations between PROMIS depression, anxiety, sleep disturbance, and physical function and LUTS sub-domains
Supplementary Figure 2. Baseline multivariable linear regression model assessing the relationships between baseline PROMIS measures, participant characteristics, and LUTS sub-domains (with anxiety instead of depression). Statistically significant covariate point estimates and corresponding 95% confidence intervals depicted as diamonds and horizontal bars, respectively. Final covariates included in each model are shown, grey shading indicates that covariate was not included in the model depicted in that column. For example, all else equal, for each 10 point increase in the baseline PROMIS anxiety score, the LUTS UI score increased (i.e. more severe UI) by 5.4 units, on average, where each unit represents 1% of the total scale.
Supplementary Figure 3. PROMIS measures over time. On average, there was no difference in PROMIS measures over time. PROMIS measures are displayed using the raw scores on the y-axes. The box represents the first to third quartiles (Q1 to Q3, respectively) of scores, with the median depicted by a horizontal line. Mean measures are shown as plus signs. The whiskers extend down from the box to the most extreme observation that is less than or equal to Q1 minus 1.5 times the IQR and up from the box to the most extreme observation that is less than or equal to Q3 plus 1.5 times the IQR. Measures that are below or above this cut off, respectively, are graphed as dots.
Supplementary Figure 4. Repeated measures linear regression model assessing the relationships between baseline PROMIS measures, participant characteristics, and LUTS sub-domains at follow-up timepoints (with anxiety instead of depression). Statistically significant covariate point estimates and corresponding 95% confidence intervals depicted as diamonds and horizontal bars, respectively. Final covariates included in each model are shown, grey shading indicates that covariate was not included in the model depicted in that column. For example, all else equal, for each 10 point increase in the baseline PROMIS anxiety score, the LUTS UI score increased (i.e. more severe UI) by 4.5 units, on average, where each unit represents 1% of the total scale.
Supplementary Figure 5. PROMIS measures and post-void urinary incontinence vs urgency urinary incontinence.
Acknowledgements:
This is publication number 30 of the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN).
This study is supported by the National Institute of Diabetes & Digestive & Kidney Diseases through cooperative agreements (grants DK097780, DK097772, DK097779, DK099932, DK100011, DK100017, DK099879).
Research reported in this publication was supported at Northwestern University, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR001422. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The following individuals were instrumental in the planning and conduct of this study at each of the participating institutions:
Duke University, Durham, North Carolina (DK097780): PIs: Cindy Amundsen, MD, Eric Jelovsek, MD; Co-Is: Kathryn Flynn, PhD, Jim Hokanson, PhD, Aaron Lentz, MD, David Page, PhD, Nazema Siddiqui, MD, Kevin Weinfurt, PhD Lisa Wruck, PhD; Study Coordinators: Paige Green, Magaly Guerrero
University of Iowa, Iowa City, IA (DK097772): PIs: Catherine S Bradley, MD, MSCE, Karl Kreder, MD, MBA; Co-Is: Bradley A. Erickson, MD, MS, Daniel Fick, MD, Vince Magnotta, PhD, Philip Polgreen, MD, MPH; Study Coordinators: Sarah Heady, Chelsea Poesch, Shelly Melton, Jean Walshire
Northwestern University, Chicago, IL (DK097779): PIs: James W Griffith, PhD, Kimberly Kenton, MD, MS, Brian Helfand, MD, PhD; Co-Is: Carol Bretschneider, MD, David Cella, PhD, Sarah Collins, MD, Julia Geynisman-Tan, MD, Alex Glaser, MD, Christina Lewicky-Gaupp, MD, Margaret Mueller, MD; Study Coordinators: Sylwia Clarke, Melissa Marquez, Michelle Taddeo, Pooja Sharma, Malgorzata Antoniak, Pooja Talaty, Francesca Moroni, Sophia Kallas. Dr. Helfand and Ms. Talaty are at NorthShore University HealthSystem.
University of Michigan Health System, Ann Arbor, MI (DK099932): PI: J Quentin Clemens, MD, FACS, MSCI; Co-Is: John DeLancey, MD, Dee Fenner, MD, Rick Harris, MD, Steve Harte, PhD, Anne P. Cameron, MD, Aruna Sarma, PhD, Giulia Lane, MD; Study Coordinators: Ashly Chimner, Linda Drnek, Emma Keer, Marissa Moore, Greg Mowatt, Sarah Richardson, Julia Chilimigras
University of Washington, Seattle Washington (DK100011): PI: Claire Yang, MD; Co-I: Anna Kirby, MD; Study Coordinators: Brenda Vicars, RN, Lauren Daniels
Washington University in St. Louis, St. Louis Missouri (DK100017): PI: H. Henry Lai, MD; Co-Is: Gerald L. Andriole, MD, Joshua Shimony, MD, PhD, Fuhai Li, PhD; Study Coordinators: Linda Black, Vivien Gardner, Patricia Hayden, Diana Wolff, Aleksandra Klim, RN, MHS, CCRC
Arbor Research Collaborative for Health, Data Coordinating Center (DK099879): PI: Robert Merion, MD, FACS; Co-Is: Victor Andreev, PhD, DSc, Brenda Gillespie, PhD, Abigail Smith, PhD; Project Manager: Melissa Fava, MPA, PMP; Clinical Monitor: Melissa Sexton, BA, CCRP; Research Analysts: Margaret Helmuth, MA, Jon Wiseman, MS, Jane Liu, MPH; Project Associate: Levi Hurley
National Institute of Diabetes and Digestive and Kidney Diseases, Division of Kidney, Urology, and Hematology, Bethesda, MD: Project Scientist: Ziya Kirkali MD; Project Officer: Christopher Mullins PhD; Project Advisor: Julie Barthold, MD.
List of Abbreviations:
- AUA-SI
American Urological Association Symptom Index
- EpiLUTS
Epidemiology of LUTS
- HADS
Hospital Anxiety and Depression Scale
- ICS
International Continence Society
- IQR
Interquartile ranges
- LUTS
Lower urinary tract symptoms
- PROMIS®
Patient-Reported Outcomes Measurement Information System®
- QOL
Quality of life
- LURN
Symptoms of Lower Urinary Tract Dysfunction Research Network
- UI
Urinary incontinence
Footnotes
Conflict of Interest Statement:
Anne P. Cameron reports the following conflicts: Speaker Wellspect; Investigator Medtronic; Guideline committee travel payment Aua; SUFU board member. Michelle Taddeo works in Dr. Griffith’s lab at Northwestern University which received funding in the form of a research grant (U01 DK097779) from the National Institute of Diabetes and Digestive and Kidney Diseases. (NIDDK from a U01 research grant for this work). All other authors have no conflicts to report.
Clinical Trial and IRB Information
Clinical Trials URL: https://clinicaltrials.gov/ct2/show/NCT02485808. This observational cohort study was approved by the Institutional Review Board at each site, and all participants provided informed consent prior to enrollment.
References:
- 1.Coyne KS, Wein AJ, Tubaro A et al. : The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health related quality of life, anxiety, and depression: EpiLUTS. BJU International, 103: 4, 2009 [DOI] [PubMed] [Google Scholar]
- 2.Milsom I, Kaplan SA, Coyne KS et al. : Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: results from EpiLUTS. Urology, 80: 90, 2012 [DOI] [PubMed] [Google Scholar]
- 3.D’Ancona C, Haylen B, Oelke M et al. : The International Continence Society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn, 38: 433, 2019 [DOI] [PubMed] [Google Scholar]
- 4.Liu AB, Liu Q, Yang CC et al. : Patient Characteristics Associated with More Bother from Lower Urinary Tract Symptoms. J Urol, 202: 585, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helfand BT, Smith AR, Lai HH et al. : Prevalence and Characteristics of Urinary Incontinence in a Treatment Seeking Male Prospective Cohort: Results from the LURN Study. The Journal of Urology, 200: 397, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maserejian NN, Kupelian V, McVary KT et al. : Prevalence of post-micturition symptoms in association with lower urinary tract symptoms and health-related quality of life in men and women. BJU Int, 108: 1452, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu G, Andreev VP, Helmuth ME et al. : Symptom Based Clustering of Men in the LURN Observational Cohort Study. J Urol, 202: 1230, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amundsen CL, Helmuth ME, Smith AR et al. : Longitudinal changes in symptom-based female and male LUTS clusters. Neurourol Urodyn, 39: 393, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gratzke C, Bachmann A, Descazeaud A et al. : EAU Guidelines on the Assessment of Non-neurogenic Male Lower Urinary Tract Symptoms including Benign Prostatic Obstruction. Eur Urol, 67: 1099, 2015 [DOI] [PubMed] [Google Scholar]
- 10.Foster HE, Dahm P, Kohler TS et al. : Surgical Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA Guideline Amendment 2019. J Urol, 202: 592, 2019 [DOI] [PubMed] [Google Scholar]
- 11.Yang CC, Weinfurt KP, Merion RM et al. : Symptoms of Lower Urinary Tract Dysfunction Research Network. The Journal of urology, 196: 146, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cameron AP, Lewicky-Gaupp C, Smith AR et al. : Baseline lower urinary tract symptoms in patients enrolled in the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN): a prospective, observational cohort study. The Journal of urology, 199: 1023, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coyne KS, Barsdorf AI, Thompson C et al. : Moving towards a comprehensive assessment of lower urinary tract symptoms (LUTS). Neurourol Urodyn, 31: 448, 2012 [DOI] [PubMed] [Google Scholar]
- 14.Barry MJ, Fowler FJ Jr., O’Leary MP et al. : The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol, 148: 1549, 1992 [DOI] [PubMed] [Google Scholar]
- 15.Barry MJ, Williford WO, Fowler FJ Jr. et al. : Filling and voiding symptoms in the American Urological Association Symptom Index: the value of their distinction in a Veterans Affairs randomized trial of medical therapy in men with a clinical diagnosis of benign prostatic hyperplasia. J Urol, 164: 1559, 2000 [PubMed] [Google Scholar]
- 16.Barbosa JA, Muracca E, Nakano E et al. : Risk factors for male lower urinary tract symptoms: the role of metabolic syndrome and androgenetic alopecia in a Latin American population. Urology, 82: 182, 2013 [DOI] [PubMed] [Google Scholar]
- 17.Rana Z, Hong RL, Abugideiri M et al. : Sexual, irritative, and voiding outcomes, following stereotactic body radiation therapy for prostate cancer. Radiat Oncol, 10: 182, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lyauk YK, Lund TM, Hooker AC et al. : Integrated Item Response Theory Modeling of Multiple Patient-Reported Outcomes Assessing Lower Urinary Tract Symptoms Associated with Benign Prostatic Hyperplasia. AAPS J, 22: 98, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pilkonis PA, Choi SW, Reise SP et al. : Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment, 18: 263, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu L, Buysse DJ, Germain A et al. : Development of short forms from the PROMIS™ sleep disturbance and Sleep-Related Impairment item banks. Behav Sleep Med, 10: 6, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schalet BD, Hays RD, Jensen SE et al. : Validity of PROMIS physical function measured in diverse clinical samples. J Clin Epidemiol, 73: 112, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raghunathan TE, Lepkowski JM, Hoewyk JV: A multivariate technique for multiplying imputing missing values using a sequence of regression models. Survey Methodology, 27: 85, 2001 [Google Scholar]
- 23.TE R, PW S, P B et al. : IVEware: Imputation and Variance Estimation Software. Ann Arbor: Survey Research Center, Institute for Social Research, University of Michigan; 2000. [Google Scholar]
- 24.Cohen P, Cohen J, Aiken LS et al. : The Problem of Units and the Circumstance for POMP. Multivariate Behavioral Research, 34: 315, 1999 [Google Scholar]
- 25.Helmuth ME, Smith AR, Andreev VP et al. : Use of Euclidean length to measure urinary incontinence severity based on the lower urinary tract symptoms tool. Am J Obstet Gynecol, 218: 357, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coyne KS, Kaplan SA, Chapple CR et al. : Risk factors and comorbid conditions associated with lower urinary tract symptoms: EpiLUTS. BJU International, Suppl 3: 24, 2009 [DOI] [PubMed] [Google Scholar]
- 27.Cella D, Smith AR, Griffith JW et al. : A new outcome measure for LUTS: Symptoms of Lower Urinary Tract Dysfunction Research Network Symptom Index-29 (LURN SI-29) questionnaire. Neurourology and Urodynamics, 38: 1751, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cella D, Smith AR, Griffith JW et al. : A New Brief Clinical Assessment of Lower Urinary Tract Symptoms for Women and Men: LURN SI-10. J Urol, 203: 164, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang CL, Wu MP, Ho CH et al. : The bidirectional relationship between anxiety, depression, and lower urinary track symptoms: A nationwide population-based cohort study. J Psychosom Res, 100: 77, 2017 [DOI] [PubMed] [Google Scholar]
- 30.Funada S, Tabara Y, Negoro H et al. : Longitudinal Analysis of Bidirectional Relationships between Nocturia and Depressive Symptoms: The Nagahama Study. J Urol, 203: 984, 2020 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Baseline multivariable linear regression model assessing the relationships between baseline PROMIS measures, participant characteristics, and LUTS sub-domains
Supplementary Figure 1A-D. Baseline associations between PROMIS depression, anxiety, sleep disturbance, and physical function and LUTS sub-domains
Supplementary Figure 2. Baseline multivariable linear regression model assessing the relationships between baseline PROMIS measures, participant characteristics, and LUTS sub-domains (with anxiety instead of depression). Statistically significant covariate point estimates and corresponding 95% confidence intervals depicted as diamonds and horizontal bars, respectively. Final covariates included in each model are shown, grey shading indicates that covariate was not included in the model depicted in that column. For example, all else equal, for each 10 point increase in the baseline PROMIS anxiety score, the LUTS UI score increased (i.e. more severe UI) by 5.4 units, on average, where each unit represents 1% of the total scale.
Supplementary Figure 3. PROMIS measures over time. On average, there was no difference in PROMIS measures over time. PROMIS measures are displayed using the raw scores on the y-axes. The box represents the first to third quartiles (Q1 to Q3, respectively) of scores, with the median depicted by a horizontal line. Mean measures are shown as plus signs. The whiskers extend down from the box to the most extreme observation that is less than or equal to Q1 minus 1.5 times the IQR and up from the box to the most extreme observation that is less than or equal to Q3 plus 1.5 times the IQR. Measures that are below or above this cut off, respectively, are graphed as dots.
Supplementary Figure 4. Repeated measures linear regression model assessing the relationships between baseline PROMIS measures, participant characteristics, and LUTS sub-domains at follow-up timepoints (with anxiety instead of depression). Statistically significant covariate point estimates and corresponding 95% confidence intervals depicted as diamonds and horizontal bars, respectively. Final covariates included in each model are shown, grey shading indicates that covariate was not included in the model depicted in that column. For example, all else equal, for each 10 point increase in the baseline PROMIS anxiety score, the LUTS UI score increased (i.e. more severe UI) by 4.5 units, on average, where each unit represents 1% of the total scale.
Supplementary Figure 5. PROMIS measures and post-void urinary incontinence vs urgency urinary incontinence.


