Abstract
Backgrounds:
Inadequate sleep duration is associated with a higher risk of type 2 diabetes and the relationship is nonlinear. We aim to assess the curve relationship between night sleep duration and the incidence of type 2 diabetes in China.
Methods:
A cohort of 11,539 participants from the REACTION study without diabetes at baseline (2011) were followed until 2014 for the development of type 2 diabetes. The average number of hours of sleep per night was grouped. Incidence rates and odds ratios (ORs) were calculated for the development of diabetes in each sleep duration category.
Results:
Compared to people who sleep for 7 to 8 h/night, people with longer sleep duration (≥9 h/night) had a greater risk of type 2 diabetes (OR: 1.27; 95% CI: 1.01–1.61), while shorter sleep (<6 h/night) had no significant difference in risk of type 2 diabetes. When the dataset was stratified based on selected covariates, the association between type 2 diabetes and long sleep duration became more evident among individuals <65 years of age, male, body mass index <24 kg/m2 or with hypertension or hyperlipidemia, no interaction effects were observed. Furthermore, compared to people persistently sleeping 7 to 9 h/night, those who persistently slept ≥9 h/night had a higher risk of type 2 diabetes. The optimal sleep duration was 6.3 to 7.5 h/night.
Conclusions:
Short or long sleep duration was associated with a higher risk of type 2 diabetes. Persistently long sleep duration increased the risk.
Keywords: Sleep duration, Type 2 diabetes, Prevalence, Risk
Introduction
Type 2 diabetes is a critical public health challenge worldwide. Patients with type 2 diabetes are at increased risk for premature mortality and hospitalization due to complications.[1] Given the global burden of type 2 diabetes, understanding the impacts of modifiable risk factors is of great importance.[2,3]
Sleep is essential to the health of patients with type 2 diabetes.[4] Although humans spend about a third of their time sleeping, they may not understand the importance of it. Adequate high-quality sleep is vital to maintain the normal physiological state of the body.[5] Insufficient sleep is a health problem,[5] and long sleep duration is associated with increased body mass index (BMI),[6] impaired glucose tolerance,[7] and increased probability of developing type 2 diabetes.[7] Although lifestyle changes, such as increasing physical activity and weight loss, are of great importance to the management of this disease, understanding the link between type 2 diabetes and sleep duration may help to reduce its incidence.
Short sleepers and long sleepers show an increased incidence of type 2 diabetes.[8] In addition, a study in Japan found a J-shaped relationship between sleep time and HbA1c level.[9] Therefore, this retrospective cohort study assessed the associations between both nighttime and daytime napping and risk for type 2 diabetes. We used data from the Risk Evaluation of cAncers in Chinese diabeTic Individuals: a lONgitudinal (REACTION) study cohort, which covered a 4-year period. To our knowledge, no such study has yet explored this relationship in Chinese people with a risk for type 2 diabetes.
Methods
Ethic approval
All participants provided written informed consent and all protocols were approved by the Ethical Committee of Rui-jin Hospital, Shanghai Jiao Tong University School of Medicine, which is in charge of the REACTION study (No. 2011-14).
Study subjects
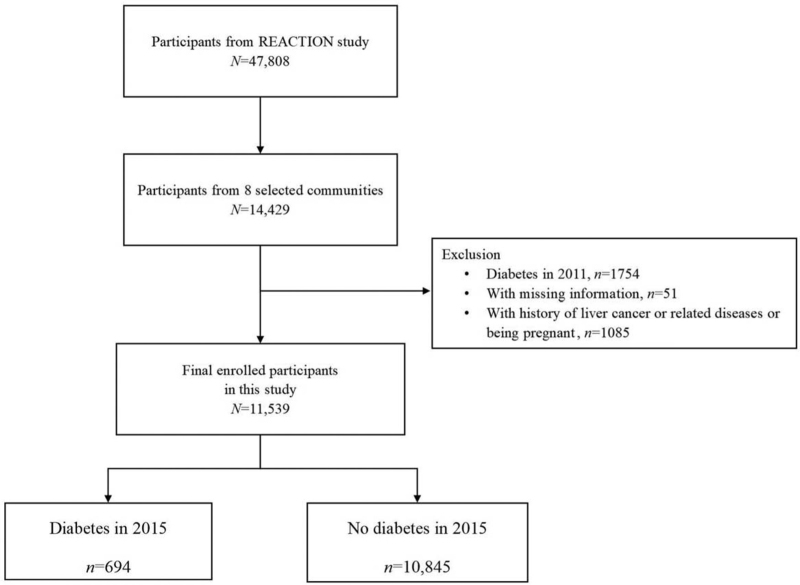
We used data from the REACTION cohort study, which investigated the association between type 2 diabetes and pre-type 2 diabetes and the risk of cancer in the Chinese population.[10] All subjects live in Laoshan, Jingding, and Gucheng communities of Beijing (China) or in Ningde and Wuyishan, Fujian Province (China). They were invited to complete baseline questionnaires and medical examinations in 2011. During the first follow-up survey in 2015, the same community was investigated, and the study had a total size of 14,429 participants [Figure 1].
Figure 1.
Flowchart of participants from the Risk Evaluation of cAncers in Chinese diabetic Individuals: a lONgitudinal (REACTION) study.
In all, 1754 subjects were diagnosed with type 2 diabetes in 2011, 51 subjects were with missing information, and 1085 subjects were with history of cancer or related diseases or being pregnant. The remaining 11,539 subjects (4043 men, 7496 women) were enrolled in the present study.
Assessment of covariates
Data, such as age, sex, smoking status, and drinking status, were collected during the baseline investigation by trained doctors using a detailed questionnaire. BMI was calculated as weight in kilograms divided by height in meters squared. Smoking and alcohol consumption were classified into three levels: current, occasional, and never. Subjects who smoke at least one cigarette/day for more than half a year were defined as current smokers.[11] Subjects who drink at least one time/week for more than half a year were defined as current drinkers.[12] The first level was regarded as positive responses. Nighttime and midday sleep time and sleep quality data were obtained through a self-administrated questionnaire.[10] Sleep duration was calculated from bedtime to waking time and was categorized into five groups: <6 h, 6 to <7 h, 7 to <8 h, 8 to <9 h, or ≥9 h. Midday napping was divided into groups of no napping (0 min), 1 to 29 min, 30 to 59 min, 60 to 89 min, and ≥90 min. Sleep quality was divided into three groups: good, fair, and poor, with frequent use of hypnotics included in the fair group. Hypertension was defined as selfreported physician-diagnosed hypertension or current use of antihypertensive medications or SBP≥130 mm Hg/DBP≥80 mm Hg by the 2017 American College of Cardiology/American Heart Association guidelines.[13] Diabetes was defined as self-reported physician-diagnosed diabetes or fasting glucose level ≥7.0 mmol/L or current usage of antidiabetic medications. Hyperlipidemia was defined as a history of physician-diagnosed hyperlipidemia or total cholesterol ≥6.22 mmol/L or triglycerides >2.26 mmol/L or high-density lipoprotein cholesterol < 1.04 mmol/L or low-density lipoprotein cholesterol ≥4.14 mmol/L or current usage of lipid-lowering medications.
Statistical analysis
We performed all analyses with Stata statistical software, v. 14.2 (Stata Corp., College Station, TX, USA). Data were compared using analysis of variance (ANOVA) for continuous variables and χ2 analysis for categorical variables. Continuous variables are expressed as mean ± standard deviation, and categorical variables are expressed as n (%).
Binary logistic regression was constructed to assess the ORs and 95% confidence intervals (CIs) of sleep duration and type 2 diabetes using sleep duration of 7 to 8 h/night as the reference groups, as previous studies have suggested that sleeping for 7 to 8 h is optimal.[14,15] Potential covariates included in the multivariate-adjusted model were age, gender, BMI, smoking and drinking status, hypertension, and hyperlipidemia. Considering that type 2 diabetes risk might follow nonlinear trends, we used a restricted cubic spline model with three knots at 25,50, and 75th percentiles of sleep duration and 7 h/night as the reference group.[16] Subjects were divided into several groups by age (<65 years, ≥65 years), sex (male, female), BMI (<24 kg/m2, ≥24 kg/m2), hypertension (yes, no), and hyperlipidemia (yes, no). In addition, potential interactions were tested using interaction terms of these covariates with sleep duration.
We evaluated the association between changes in sleep duration and incidence of type 2 diabetes. This association was examined using crude and multivariate-adjusted models, with subjects persistently sleeping 7 to 9 h/night in both surveys as the reference group.
We further evaluated the joint effects of sleep duration and midday napping and that of sleep duration and sleep quality on the risk of developing diabetes, using moderate sleep duration (7–8 h/night) with midday napping (1–29 min), and moderate sleep duration (7–8 h/night) with good sleep quality as the reference groups.
Results
Among 11,539 subjects, 13.11% (n = 1513) reported sleeping ≥9 h/night and 5.18% (n = 598) reported midday napping >90 min. Compared to subjects reporting 7 to 8 h/night of sleep, those reporting sleep duration ≥9 h/night were more likely to be female, current smokers, and current drinkers. Meanwhile, compared to subjects with 1 to 29 min of midday napping, those reporting midday napping ≥90 min were more likely to be male, hypertension and hyperlipidemia, current smokers, current drinkers (P < 0.05). In addition, compared to the reference groups, participants reporting≥9 h/night of sleep were less likely to have hypertension and hyperlipidemia [Table 1].
Table 1.
General characteristics of the study participants according to sleep duration and midday napping (N = 11,539)
| Sleep duration, h/night | Midday napping, min | |||||||||||||
| Variables | <6 (n = 549) | 6 to <7 (n = 1649) | 7 to <8 (n = 4162) | 8 to <9 (n = 3666) | ≥9 (n = 1513) | F/χ2 | P value | 0 (n = 6678) | 0 to <30 (n = 3104) | 30 to <60 (n = 402) | 60 to <90 (n = 757) | ≥90 (n = 598) | F/χ2 | P value |
| Age, years | 62.03 ± 9.14 | 61.10 ± 9.37 | 61.14 ± 9.17 | 61.07 ± 9.58 | 60.25 ± 10.22 | 4.31 | <0.01 | 61.18 ± 8.57 | 65.29 ± 8.46 | 52.57 ± 9.34 | 52.85 ± 9.45 | 53.42 ± 9.24 | 567.88 | <0.01 |
| Male/female | 203/346 | 615/1034 | 1484/2678 | 1225/2441 | 516/997 | 10.12 | 0.04 | 2020/4658 | 1286/1818 | 155/247 | 323/434 | 259/339 | 162.56 | <0.01 |
| BMI, kg/m2 | 25.39 ± 3.35 | 25.40 ± 3.29 | 25.24 ± 3.34 | 25.23 ± 3.31 | 25.08 ± 3.41 | 2.11 | 0.08 | 25.35 ± 3.37 | 25.62 ± 3.30 | 24.00 ± 2.96 | 25.12 ± 3.01 | 24.37 ± 3.19 | 58.26 | <0.01 |
| Smoking | 109 | 284 | 673 | 536 | 255 | 13.86 | <0.01 | 1017 | 559 | 49 | 121 | 111 | 19.37 | <0.01 |
| Drinking | 79 | 246 | 494 | 397 | 187 | 20.77 | <0.01 | 654 | 432 | 64 | 143 | 110 | 103.19 | <0.01 |
| Good sleep quality Comorbidities | 197 | 312 | 512 | 403 | 209 | 286.25 | <0.01 | 5678 | 2755 | 316 | 647 | 510 | 42.93 | <0.01 |
| Hypertension | 142 | 443 | 1056 | 928 | 372 | 2.42 | 0.66 | 1612 | 970 | 73 | 150 | 136 | 87.23 | <0.01 |
| Hyperlipidemia | 86 | 186 | 537 | 432 | 185 | 9.59 | 0.05 | 787 | 515 | 23 | 55 | 46 | 99.88 | <0.01 |
Data are presented as mean ± SD for continuous variables. BMI: Body mass index; SD: Standard deviation.
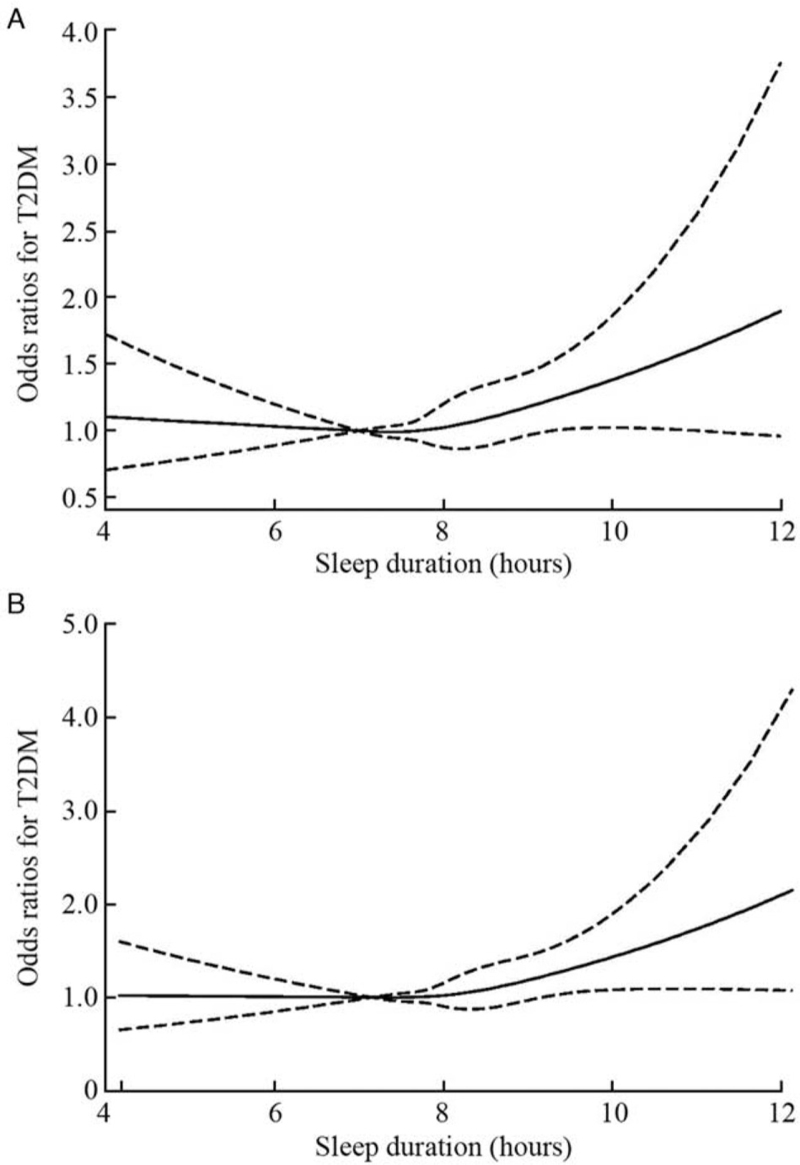
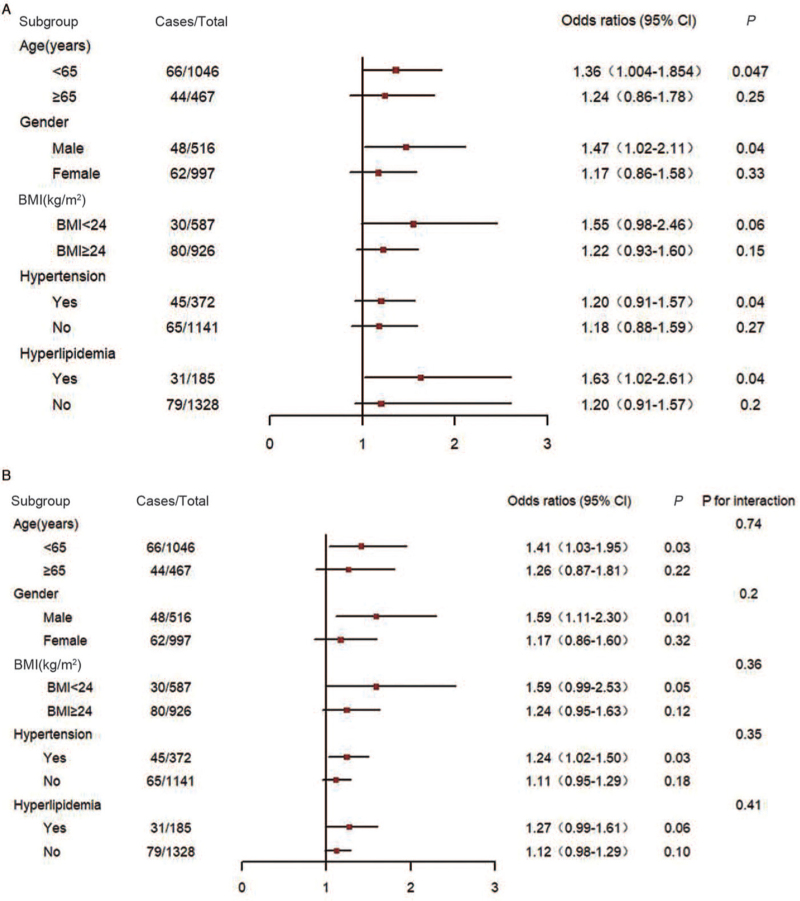
During the follow-up investigation, we documented 694 type 2 diabetes patients. Compared to people who slept for 7 to 8 h/night, the ORs (95% CIs) of type 2 diabetes were 1.21 (0.85–1.72) for <6 h/night, 0.91 (0.70–1.17) for 6 to 7 h/night, 1.03 (0.85–1.24) for 8 to 9 h/night, and 1.27 (1.01–1.61) for ≥9 h/night (P = 0.040), respectively. After adjusting for age (continuous), sex, BMI (continuous), smoking status (yes or no), drinking status (yes or no), hypertension (yes or no), and hyperlipidemia (yes or no), similar associations were observed for those having ≥9 h/night of sleep (P = 0.02) [Table 2]. We further exploredthe interaction of sleep duration and midday napping or sleep quality on the risks of type 2 diabetes. We found an interaction between sleep time and nap time or sleep quality. Compared to participants napping for 1 to 29 min, the ORs (95% CIs) of type 2 diabetes were 1.30 (0.53–3.20) for those reporting no midday napping, 1.04 (0.38–2.83) for 30 to 59 min, 1.02 (0.39–2.65) for 60 to 89 min, and 1.27 (0.48–3.31) for midday napping ≥90 min. In addition, no significant association was observed between these groups after adjusting for age, sex, BMI, smoking status, drinking status, type 2 diabetes mellitus, and hyperlipidemia. Restricted cubic spline regression analysis showed a J-shaped curve and confirmed that people who slept ≥9 h/night had a high risk of type 2 diabetes [Figure 2]. The optimal nighttime sleep duration was 7.2 to 7.5 h, and it was 6.3 to 7.5 h after adjusting for all variables. When stratified by selected covariates, the association between type 2 diabetes and long sleep duration became more evident in individuals who were <65 years of age, male, BMI < 24 kg/m2, or with hypertension or hyperlipidemia, no interaction effects were observed [Figure 3].
Table 2.
Association of sleep duration and midday napping with type 2 diabetes.
| Model 1: crude | Model 2: adjusted∗ | ||||
| Variable | Cases/Total | OR (95% CI) | P value | OR (95% CI) | P value |
| Sleep duration, h/night | |||||
| <6 | 38/549 | 1.21 (0.85–1.72) | 0.290 | 6.71 (0.36–123.48) | 0.200 |
| 6 to <7 | 87/1649 | 0.91 (0.70–1.17) | 0.440 | 2.94 (0.17–50.32) | 2.940 |
| 7 to <8 | 241/4162 | 1.00 | – | 1.00 | – |
| 8 to <9 | 218/3666 | 1.03 (0.85–1.24) | 4.460 | 4.46 (0.37–53.31) | 4.460 |
| ≥9 | 110/1513 | 1.27 (1.01–1.61) | 0.040 | 0.00 (0.00) | 1.000 |
| Midday napping, min | |||||
| 0 | 596/9678 | 1.30 (0.53–3.20) | 0.570 | 2.45 (0.33–17.96) | 0.380 |
| 1–29 | 5/104 | 1.00 | – | 1.00 | – |
| 30–59 | 20/402 | 1.04 (0.38–2.83) | 0.940 | 4.05 (0.50–33.18) | 0.190 |
| 60–89 | 37/757 | 1.02 (0.39–2.65) | 0.970 | 1.72 (0.20–14.40) | 0.620 |
| ≥90 | 36/598 | 1.27 (0.48–3.31) | 0.630 | 2.50 (0.30–20.70) | 0.400 |
Adjusted for age (continuous), sex, BMI (continuous), smoking status (current, former, or never), drinking status (current, former, or never), hypertension (yes or no), and hyperlipidemia (yes or no). BMI: Body mass index; CI: Confidence interval; OR: Odds ratio.
Figure 2.
Spline curves for associations of sleep duration with type 2 diabetes. (A) Nonadjusted. The reference group was 7 h/night sleep duration. P values were 0.184 for the overall association and 0.204 for the nonlinear association. (B) Adjusted for age (continuous), sex, BMI (continuous), smoking status (current, former, never), drinking status (current, former, never), hypertension (yes, no), and hyperlipidemia (yes, no). The reference group was 7 h/night sleep duration. Solid line represents odds ratio, and dotted lines represent 95% confidence interval of odds ratio. P values were 0.062 for the overall association and 0.092 for the nonlinear association. BMI: Body mass index; T2DM: Type 2 diabetes mellitus.
Figure 3.
Sleep duration and type 2 diabetes risk, stratified by baseline characteristics. (A) All ORs were calculated using moderate sleep duration (7–8 h/night) as the reference group. Each group was adjusted for all other covariates except the one being tested. (B) All ORs were calculated using moderate sleep duration (7–8 h/night) as the reference group, with model 2 adjusted for age (continuous), sex, BMI (continuous), smoking status (current, former, never), drinking status (current, former, never), hypertension (yes, no), and hyperlipidemia (yes, no). Each group was adjusted for all other covariates except the one being tested. BMI: Body mass index; CI: Confidence interval; ORs: Odds ratios.
We explored the combined effect of sleep duration and sleep quality on the risks of type 2 diabetes. Subjects with ≥9 h/night of sleep and good sleep quality (OR 1.27, 95% CI 1.01–1.61) had a high risk of diabetes than those who reported moderate nighttime sleep duration (7–8 h/night) and good sleep quality. After adjustments, the OR was 1.37(95%: CI 1.06–1.77) [Table 3].
Table 3.
Joint effects of sleep duration and sleep quality on the incidence of type 2 diabetes.
| Model 1: crude | Model 2: adjusted∗ | ||||
| Sleep duration, h/night | Case/Total | OR (95% CI) | P value | OR (95% CI) | P value |
| <6 | 38/549 | 1.21 (0.85–1.72) | 0.290 | 1.32 (0.87–2.02) | 0.200 |
| 6 to <7 | 87/1649 | 0.91 (0.70–1.17) | 0.440 | 0.89 (0.67–1.18) | 0.410 |
| 7 to <8 | 241/4162 | 1.00 | – | 1.00 | – |
| 8 to <9 | 218/3666 | 1.03 (0.85–1.24) | 4.460 | 1.10 (0.90–1.35) | 0.350 |
| ≥9 | 110/1513 | 1.27 (1.01–1.61) | 0.040 | 1.37 (1.06–1.78) | 0.020 |
Adjusted for age (continuous), sex, BMI (continuous), smoking status (current, former, or never), drinking status (current, former, or never), hypertension (yes or no), and hyperlipidemia (yes or no). BMI: Body mass index; CI: Confidence interval; OR: Odds ratio.
Table 4 shows the relationship between changes in sleep time with type 2 diabetes. Compared to participants who reported between 7 and 9 h of sleep in both surveys, those who reported sleeping ≥9 h in both surveys showed ORs of 1.51 (95% CI: 1.05–2.17) and 1.54 (95% CI:1.07– 2.24), indicating a higher risk of diabetes. In addition, after adjusting for all variables, the OR was 1.54 (95% CI:1.07–2.24).
Table 4.
Association of change in sleep duration between surveys with type 2 diabetes.
| Sleep duration, h/night | Model 1: crude | Model 2: adjusted∗ | ||||
| In 2011 | In 2015 | Cases/Total | OR (95% CI) | P value | OR (95% CI) | P value |
| 7-9 | 7–9 | 164/2713 | 1.00 | — | 1.00 | — |
| ≤7 | 7–9 | 74/1184 | 1.04 (0.78–1.38) | 0.810 | 0.98 (0.74–1.31) | 0.910 |
| ≥9 | 7–9 | 47/702 | 1.12 (0.80–1.56) | 0.520 | 1.13 (0.80–1.58) | 0.500 |
| ≤7 | ≤7 | 183/3282 | 0.92 (0.74–1.14) | 0.440 | 0.86 (0.69–1.07) | 0.190 |
| 7–9 | ≤7 | 125/2239 | 0.92 (0.72–1.67) | 0.490 | 0.88 (0.69–1.12) | 0.290 |
| ≥9 | ≤7 | 24/370 | 1.08 (0.69–1.68) | 0.740 | 1.03 (0.66–1.61) | 0.900 |
| ≤7 | ≥9 | 8/158 | 0.83 (0.40–1.72) | 0.610 | 0.83 (0.40–1.72) | 0.610 |
| 7–9 | ≥9 | 30/450 | 1.11 (0.74–1.66) | 0.610 | 1.11 (0.74–1.67) | 0.620 |
| ≥9 | ≥9 | 39/441 | 1.51 (1.05–2.17) | 0.030 | 1.54 (1.07–2.24) | 0.020 |
Adjusted for age (continuous), sex, BMI (continuous), smoking status (current, former, or never), drinking status (current, former, or never), hypertension (yes or no), and hyperlipidemia (yes or no). BMI: Body mass index; CI: Confidence interval; OR: Odds ratio.
Discussion
In this large retrospective cohort study, we found that subjects who slept ≥9 h per night had a high risk of type 2 diabetes. Moreover, optimal sleep duration at night was 6.3 to 7.5 h after adjusting for age, sex, BMI, smoking status, drinking status, hypertension, and hyperlipidemia. To avoid an influence of region on our results, we selected people in both the northern and southern regions of China. To the best of our knowledge, this is the first retrospective study to report that persistently sleeping ≥9 h/night is related to higher type 2 diabetes risk compared to persistently sleeping for a moderate duration (7–9 h/night) in the Chinese population.
Many studies have assessed the association between sleep duration and the incidence of type 2 diabetes[7] or blood glucose level.[8] In these studies, participants have usually divided participants into several groups according to sleep duration. Therefore, such studies can only draw the conclusions that one group of people has the lowest incidence of type 2 diabetes, for example, people who sleep 7 to 8 h at night.[8] A meta-analysis suggested that for a short duration of sleep (5–6 h/night), the risk ratio was 1.28, while that for a long duration of sleep (8–9 h/night) it was 1.48.[17] In the present study, we limited the optimal sleep duration into a narrow range according to the restricted cubic spline model.
The elevated risk for type 2 diabetes and long sleep duration appeared to be more pronounced in individuals who were<65 years old, male, BMI <24 kg/m2, and/or with hypertension or hyperlipidemia, no interaction was noted. However, we did not find significant differences between each subgroup based on the P values of interaction terms. The reason for the lack of interactions may be that we observed individuals for a short period of time, and type 2 diabetes is a chronic disease with a relatively low incidence. As a result, we observed fewer cases.
Afternoon napping is a common habit in many countries including China. The relationship between midday napping and the risk of type 2 diabetes has also been investigated in several previous cross-sectional[18] and cohort studies.[19] These studies have suggested that the incidence of type 2 diabetes or elevated blood glucose levels is higher in individuals with longer sleep duration. However, midday napping can influence the quantity and quality of nocturnal sleep.[20] Therefore, we considered the effects of midday napping on the incidence of type 2 diabetes alongside that of nocturnal sleep. To our knowledge, this is the first study to examine the impact of midday napping in combination with nocturnal sleep on the incidence of type 2 diabetes in the Chinese population. However, we found no interaction between sleep time and midday napping. Observing the relationships between the incidence of type 2 diabetes and both sleep duration and midday napping demands a large number of subjects. Previous research has suggested that type 2 diabetes patients prefer longer midday naps because they are more fatigued.[21] We excluded individuals with diabetics at the start of our study, and therefore we can conclude that a longer midday napping leads to type 2 diabetes.
Previous studies have been shown that the prevalence of poor sleep quality was significantly higher among people with diabetes than those without it.[22] In our study, only 105 participants with poor sleep quality developed diabetes during the follow-up period. As a result, the difference in the incidences of diabetes is not statistically significant between this group and the reference group. A larger sample size is needed to investigate the effects of sleep quality.
Numerous possible mechanisms could explain the relationship between long sleep duration and midday napping and the incidence of type 2 diabetes. Research revealed that leptin and ghrelin are of great importance to the incidence of type 2 diabetes.[23] Short sleep can reduce leptin and elevate ghrelin in the blood, leading to increases in hunger and appetite, accompanied by a decrease in glucose tolerance.[24] In addition, short sleep may contribute to the secretion of adiponectin and insulin. Adiponectin, which is secreted by adipocytes, is associated with insulin sensitivity.[25–27] Sleep restriction can increase sympathetic nervous system activity, leading to decreased insulin sensitivity.[28] However, the mechanisms through which long sleep duration leads to increased risk for type 2 diabetes are not fully understood. Long sleep duration may reflect a more sedentary lifestyle and, similar to short sleepers, long sleepers may engage in more snacking.[29]
The study also had several limitations. First, the sleep duration at night and midday is defined as the time from going to bed to waking in the questionnaire survey, which is slightly different from the actual time to sleep. However, it was impossible to obtain the objective measures of sleep duration and napping in large prospective population studies, and the self-administrated survey is the most commonly used method of evaluating sleep duration and napping in large population-based studies. Second, previous studies have suggested that poor sleep quality is associated with higher blood glucose levels in patients with type 2 diabetes.[22] However, some subgroups contained few cases of type 2 diabetes, causing their differences to be non-significant. No significant result was found on the interaction between sleep time and nap time or sleep quality. The current results may be related to overfitting, and the mechanism will be studied in the next research. In addition, restricted cubic spline showed that the sleeping time was related to the incidence rate of diabetes, but it was not a significant curve relationship. A larger sample size is needed in future studies on this subject for further study. Third, we did not record the family members when we sent out the questionnaire, so we could not use these data. We will use a more accurate questionnaire in the next survey to facilitate the follow-up analysis.
Conclusions
We found a J-shaped relationship between sleep duration and the incidence of type 2 diabetes, with the lowest risk for type 2 diabetes in individuals sleeping 6.3 to 7.5 h after adjusting for covariates. Sleep duration that is too long or too short increases the risk of type 2 diabetes. Further studies are needed to reveal the mechanism driving the relationship between sleep time and the incidence of diabetes.
Funding
This work was supported by a grant from the National Key Research and Development Program of China (No. 2018YFC1314100).
Conflicts of interest
None.
Footnotes
How to cite this article: Liu HZ, Chen G, Wen JP, Wang AP, Mu YM, Dou JT, Gu WJ, Zang L, Zhang SC, Lyu ZH. Association between sleep duration and incidence of type 2 diabetes in China: the REACTION study. Chin Med J 2022;135:1242–1248. doi: 10.1097/CM9.0000000000001835
Hongzhou Liu and Gang Chen contributed equally to this work.
References
- 1.Rajbhandari J, Fernandez CJ, Agarwal M, Yeap BXY, Pappachan JM. Diabetic heart disease: a clinical update. World J Diabetes 2021; 12:383–406. doi: 10.4239/wjd.v12.i4.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pourreza S, Khademi Z, Mirzababaei A, Yekaninejad MS, Sadeghniiat-Haghighi K, Naghshi S, et al. Association of plantbased diet index with inflammatory markers and sleep quality in overweight and obese female adults: a cross-sectional study. Int J Clin Pract 2021; 9:e14429.doi: 10.1111/ijcp. [DOI] [PubMed] [Google Scholar]
- 3.Liu H, Yan S, Chen G, Li B, Zhao L, Wang Y, et al. Association of the ratio of triglycerides to high-density lipoprotein cholesterol levels with the risk of type 2 diabetes: a retrospective cohort study in Beijing. J Diabetes Res 2021; 2021:5524728.doi: 10.1155/2021/5524728. eCollection 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Samy AL, Hairi NN, Low WY. Psychosocial stress, sleep deprivation, and its impact on type II diabetes mellitus: policies, guidelines, and initiatives from Malaysia. FASEB Bioadv 2021; 3:593–600. doi: 10.1096/fba.2020-00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med 2017; 32:246–256. doi: 10.1016/j.sleep.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Ryan S. Sleep and diabetes. Curr Opin Pulm Med 2018; 24:555–560. doi: 10.1097/mcp.0000000000000524. [DOI] [PubMed] [Google Scholar]
- 7.van Dijk D, Balkau B, Segrestin B, Gottsäter M, Gabriel R, Hatunic M, et al. Associations between sleep duration and sleep debt with insulin sensitivity and insulin secretion in the EGIR-RISC Study. Diabetes Metab 2019; 45:375–381. doi: 10.1016/j.diabet.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Wang J, Kwok MK, Au Yeung SL, Li AM, Lam HS, Leung JYY, et al. Sleep duration and risk of diabetes: observational and Mendelian randomization studies. Prev Med 2019; 119:24–30. doi: 10.1016/j. ypmed.2018.11.019. [DOI] [PubMed] [Google Scholar]
- 9.Ohkuma T, Fujii H, Iwase M, Kikuchi Y, Ogata S, Idewaki Y, et al. Impact of sleep duration on obesity and the glycemic level in patients with type 2 diabetes: the Fukuoka Diabetes Registry. Diabetes Care 2013; 36:611–617. doi: 10.2337/dc12-0904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ning G. Risk Evaluation of cAncers in Chinese diabeTic Individuals: a lONgitudinal (REACTION) study. J Diabetes 2012; 4:172–173. doi: 10.1111/j.1753-0407.2012.00182.x. [DOI] [PubMed] [Google Scholar]
- 11.Yang G, Fan L, Tan J, Qi G, Zhang Y, Samet JM, et al. Smoking in China: findings of the 1996 National Prevalence Survey. JAMA 1999; 282:1247–1253. doi: 10.1001/jama.282.13.1247. [DOI] [PubMed] [Google Scholar]
- 12.Yuan JM, Ross RK, Gao YT, Henderson BE, Yu MC. Follow up study of moderate alcohol intake and mortality among middle aged men in Shanghai, China. BMJ 1997; 314:18–23. doi: 10.1136/bmj.314.7073.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension 2018; 71:e13–e115. doi:10.1161/hyp.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 14.Kwok CS, Kontopantelis E, Kuligowski G, Gray M, Muhyaldeen A, Gale CP, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: a dose-response meta-analysis. J Am Heart Assoc 2018; 15:e008552.doi: 10.1161/JAHA.118.008552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yamada T, Hara K, Shojima N, Yamauchi T, Kadowaki T. Daytime napping and the risk of cardiovascular disease and all-cause mortality: a prospective study and dose-response meta-analysis. Sleep 2015; 38:1945–1953. doi: 10.5665/sleep.5246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou L, Yu K, Yang L, Wang H, Xiao Y, Qiu G, et al. Sleep duration, midday napping, and sleep quality and incident stroke: the Dongfeng- Tongji cohort. Neurology 2020; 94:e345–e356. doi:10.1212/wnl.0000000000008739. [DOI] [PubMed] [Google Scholar]
- 17.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 2010; 33:414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fang W, Li Z, Wu L, Cao Z, Liang Y, Yang H, et al. Longer habitual afternoon napping is associated with a higher risk for impaired fasting plasma glucose and diabetes mellitus in older adults: results from the Dongfeng-Tongji cohort of retired workers. Sleep Med 2013; 14:950–954. doi: 10.1016/j.sleep.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 19.Hublin C, Lehtovirta M, Partinen M, Koskenvuo M, Kaprio J. Napping and the risk of type 2 diabetes: a population-based prospective study. Sleep Med 2016; 17:144–148. doi: 10.1016/j.sleep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Chen M, Zhang X, Liang Y, Xue H, Gong Y, Xiong J, et al. Associations between nocturnal sleep duration, midday nap duration and body composition among adults in Southwest China. PLoS One 2019; 14:e0223665.doi: 10.1371/journal.pone.0223665. eCollection 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh R, Kluding PM. Fatigue and related factors in people with type 2 diabetes. Diabetes Educ 2013; 39:320–326. doi: 10.1177/0145721713479144. [DOI] [PubMed] [Google Scholar]
- 22.Jemere T, Mossie A, Berhanu H, Yeshaw Y. Poor sleep quality and its predictors among type 2 diabetes mellitus patients attending Jimma University Medical Center, Jimma, Ethiopia. BMC Res Notes 2019; 1:488.doi: 10.1186/s13104-019-4531-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rafiee M, Sotoudeh G, Djalali M, Alvandi E, Eshraghian M, Javadi F, et al. The interaction between apolipoprotein B insertion/deletion polymorphism and macronutrient intake on lipid profile and serum leptin and ghrelin levels in type 2 diabetes mellitus patients. Eur J Nutr 2019; 58:1055–1065. doi: 10.1007/s00394-018-1621-5. [DOI] [PubMed] [Google Scholar]
- 24.Reutrakul S, Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism 2018; 84:56–66. doi: 10.1016/j.metabol.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 25.Nguyen TMD. Adiponectin: role in physiology and pathophysiology. Int J Prev Med 2020; 11:136.doi: 10.4103/ijpvm.IJPVM_193_20. eCollection 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee JY, Yang JW, Han BG, Choi SO, Kim JS. Adiponectin for the treatment of diabetic nephropathy. Korean J Intern Med 2019; 34:480–491. doi: 10.3904/kjim.2019.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vučić Lovrenčić M, Gerić M, Kosuta I, Dragičević M, Garaj-Vrhovac V, Gajski G. Sex-specific effects of vegetarian diet on adiponectin levels and insulin sensitivity in healthy non-obese individuals. Nutrition 2020; 79–80:110862.doi: 10.1016/j.nut. 2020.110862. [DOI] [PubMed] [Google Scholar]
- 28.Reutrakul S, Mokhlesi B. Obstructive sleep apnea and diabetes: a state of the art review. Chest 2017; 152:1070–1086. doi: 10.1016/j. chest.2017.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tan X, Chapman CD, Cedernaes J, Benedict C. Association between long sleep duration and increased risk of obesity and type 2 diabetes: a review of possible mechanisms. Sleep Med Rev 2018; 40:127–134. doi: 10.1016/j.smrv.2017.11.001. [DOI] [PubMed] [Google Scholar]