Highlights
-
•
Self-reported adherence to movement behavior recommendations were associated with better numeracy and literacy achievement.
-
•
The optimal combination of movement behavior recommendations differed for literacy and numeracy achievement.
-
•
Adherence rates to all 24-h movement guideline recommendations were low.
-
•
No accelerometer-measured 24-h movement behavior was associated with academic achievement.
Keywords: Academic achievement, Physical activity, Sedentary behavior, Sleep
Abstract
Background
Few studies have investigated associations between academic achievement and meeting recommendations from the 24-hour (24-h) movement guidelines. The specific guidelines associated with the most benefit academic achievement are unknown. Utilizing both self-report and objective movement data, this study examined associations between academic achievement and meeting individual recommendations and combinations of recommendations from the 24-h movement guidelines (sleep, physical activity, and screen time).
Methods
Data from CheckPoint, a cross-sectional study nested between Waves 6 and 7 of the Longitudinal Study of Australian Children, were used. Movement behaviors were measured using 24-h wrist-worn accelerometry (GENEActiv (Activinsights, Kimbolton, UK)) and were self-reported by children using the Multimedia Activity Recall for Children and Adolescents. Academic achievement was measured using a nationally administered standardized test in literacy and numeracy. Analysis of covariance, with t tests with sequential Bonferroni adjustments, was used to compare academic achievement with all possible combinations of meeting recommendations, adjusting for demographic confounders. Two models were considered: guideline compliance assessed by self-report (n = 1270, mean age = 11.99 years, 52% males) and by accelerometry (for moderate-to-vigorous intensity physical activity (MVPA) and sleep)) and self-report (screen time) in combination (n = 927, mean age = 11.97 years, 52% males).
Results
Literacy achievement significantly differed based on self-report (F(7, 1258) = 3.08, p = 0.003) and accelerometer derived (F(7, 915) = 2.40, p = 0.02) guideline compliance. Numeracy achievement significantly differed based on self-report (F(7, 1258) = 2.92, p = 0.005) but not accelerometer derived guideline compliance (F(7, 915) = 0.80, p = 0.58). When assessed by self-report, children who met all guidelines (t(334) = −4.05, p = 0.0001) or met the screen time and sleep guidelines in combination (t(125) = −5.02, p < 0.001) had superior literacy achievement. Meeting the self-report MVPA guideline in any combination was associated with higher numeracy scores (p < 0.05). Post-hoc analyses showed no differences in academic achievement for any category of accelerometer derived guideline compliance.
Conclusion
The findings suggest that limiting recreational screen time is important for literacy achievement and that encouraging compliance with the MVPA guideline is important for numeracy achievement.
Graphical Abstract
1. Introduction
Sufficient physical activity, sleep, and minimal screen time contribute to a healthy lifestyle and may play an important role in children's academic success. Systematic reviews and meta-analyses show that sleep, screen time, and physical activity are individually associated with academic outcomes in children.1, 2, 3 However, these lifestyle behaviors do not act in isolation, and it is possible that the academic benefits of combinations of healthy lifestyle behaviors may be greater than their individual benefits. Few studies have explored associations between multiple lifestyle behaviors and academic outcomes. Dumuid and colleagues4 reported that children in clusters characterized by high sedentary behavior and low physical activity achieved the highest academic performance. Similarly, Maher and colleagues5 found that high sedentary time combined with high moderate-to-vigorous intensity physical activity (MVPA) was associated with the highest academic performance among Australian school-aged children. The authors noted that while previous studies focused on screen-time-based sedentary behaviors have generally shown negative associations with academic performance, non-screen-time-based sedentary time, such as recreational reading, may underpin the positive associations observed.5
Recently, research has focused on associations between meeting new public health guidelines for 24-hour (24-h) movement behaviors and academic outcomes. The guidelines for children in Australia (5−17 years old), New Zealand (5−17 years old), South Africa (school-aged children), and Canada (5−17 years old) recommend that a healthy 24-h period should comprise at least 60 min of daily MVPA, no more than 2 h of daily recreational screen time, and 9−11 h of sleep per night.6, 7, 8, 9 The World Health Organization10 differs slightly in its guidelines, stating that children (5−17 years old) should have at least an average of 60 min per day of MVPA across the week and limit the amount of time spent being sedentary, particularly the amount of recreational screen time. Studies have found that children who meet more lifestyle behavior guidelines have better academic achievement. Faught and colleagues11,12 showed that among Canadian children 10−11 years old (cross-sectionally) and 13−18 years old (longitudinally), academic achievement generally improved with each additional guideline met (diet, physical activity, sleep, and screen time).
Two previous studies have explored which combinations of guidelines (physical activity, sleep, and screen time) are most beneficially associated with cognition and academic performance.13,14 Walsh et al.13 studied 4524 U.S. children aged 9−10 years and reported that while global cognition improved with each additional guideline met (β = 1.44), meeting the sleep + screen time guidelines (β = 4.25) or meeting the screen time guideline only (β = 5.15) had an even stronger positive association with global cognition compared to not meeting any guidelines. Similarly, Lien and colleagues14 reported that middle school students who met all guidelines (β = 0.077), those who met the screen time guideline alone (β = 0.053) and those who met the sleep guideline alone (β = 0.043) had better overall academic achievement compared to those who did not meet any guidelines.
These findings suggest that the specific combination of movement guidelines may be more important to cognition, and thus to academic achievement, than just the total number of guidelines met. While these findings provide preliminary evidence for the importance of meeting lifestyle behavior guidelines, there are some limitations associated with the existing literature. These include the use of self-report measures of physical activity11, 12, 13, 14 and self-report grades.12,14 Additionally, no previous study has explored academic achievement in relation to both self-report and objective movement data.
For schools and teachers, understanding which movement guidelines, and which combination(s) of these guidelines, is associated with superior academic achievement may be of particular interest, given the increasing pressure to improve standardized test scores in subjects (e.g., literacy and numeracy) often used to evaluate schools.15,16 Thus, the purpose of this study was to investigate associations between meeting individual recommendations and combinations of recommendations from the 24-h movement guidelines and academic achievement in a sample of Australian children, using both self-report and objective movement data.
2. Methods
2.1. Study design and participants
Participants for this study were drawn from Child Health CheckPoint,17,18 a cross-sectional study conducted between Waves 6 and 7 of the Longitudinal Study of Australian Children (LSAC).19 In 2003, LSAC recruited 5107 infants (age 0−1 year) in its birth cohort (57% uptake), and participants have been followed up in biennial waves. The LSAC birth cohort participants who completed Wave 6 data collection were eligible to participate in Child Health CheckPoint (n = 3764; 74% retention). In total, 3513 families (76% of eligible participants) gave permission to be contacted by the CheckPoint team, and 1874 (53% of eligible participants, 42% of Wave 6 cohort, and 37% of the original sample) consented to participate in CheckPoint. Data collection occurred between February 2015 and March 2016, when children were age 11−12 years. Research Electronic Data Capture (REDCap) electronic data capture tools were used in our study. More information about the REDCap software can be found at: www.project-redcap.org.
2.2. Ethical approval
The CheckPoint study was approved by the Royal Children's Hospital Melbourne Human Research Ethics Committee (33225D) and the Australian Institute of Family Studies Ethics Committee (14−26). A parent or guardian provided written informed consent for their child's participation in the study. The academic achievement data used in this analysis is stored by each respective state/territory government. Each state/territory government matched LSAC child data with academic achievement data for those children with parental consent.
2.3. Measures
Self-reported MVPA, sleep, and screen time were assessed using the Multimedia Activity Recall for Children and Adolescents (MARCA), a computerized, 24-h use-of-time recall.20 Using this tool, children recalled every activity (e.g., sports, reading, household chores) they did on the previous day (24 h), in increments of 5 min. Three days were recalled in total (one face-to-face and two via telephone interview), including 1 school day and 1 non-school day. The MARCA program contains 500 activities, yielding a high-resolution snapshot of how children use their time. The activities are grouped into 8 superdomains: sleep, screen time, sport and exercise, school-related, domestic/social, passive transport, quiet time, and self-care categories. Each activity in the MARCA is associated with a rate of energy expenditure using the Ridley compendium.21 The average of the time spent in the superdomains of MVPA, sleep, and screen time across the available days were used in our analyses and were weighted for weekdays to weekend days at a ratio of 5:2. The MARCA has been shown to have excellent test−rest reliability (intraclass correlation coefficient = 0.88–1.00),20 and good validity (r = 0.4–0.7) when compared with accelerometry,20 pedometry,22 and doubly labelled water.23
Objectively measured MVPA and sleep duration were measured with 24-h wrist-worn GENEActiv (Activinsights, Kimbolton, UK) accelerometers worn for 8 days. Detailed information regarding the processing of raw accelerometry data for CheckPoint has been published previously.24 Briefly, the raw accelerometer data were downloaded in 1-s epochs and converted to 60-s epochs. We used customized MATLAB-based software (MathWorks, Natick, MA, USA), which integrates cutpoint-based activity intensity classification25 and sleep detection using the van Hees algorithm.26 The software provides a graphical user interface displaying the acceleration trace, to allow visual identification of missing data/non-wear, bedtimes and rise times. A paper diary was used to record reasons for device removal. If the reason was “sport”, the associated period of non-wear time was replaced with MVPA. Children were included in the analyses if they had valid data for at least 4 days with 10 h or more of wear time per day during waking hours (including at least one weekend day) and 160 min or more of total sleep duration for at least 3 nights (including at least 1 weekend night). Children were categorized as meeting guidelines if they averaged 60 min or more of MVPA, 2 h or less of screen time, and between 9 h and 11 h of sleep.
Academic achievement was assessed by data linkage (with parental consent) with Year 7 results (collected from 2015 to 2017) from a nationally administered, standardized test: the National Assessment Program—Literacy and Numeracy (NAPLAN).27 In NAPLAN, achievement is assessed across 4 domains: language conventions (spelling, grammar, and punctuation), reading, writing, and numeracy. An achievement score is calculated for each domain based on the number of correct responses and is then converted to a scale score (0−1000), with a higher score indicating greater academic achievement. For our analyses, the 4 academic domains were collapsed into 2 achievement categories representing literacy and numeracy skills. Literacy achievement comprised the arithmetic mean of the literacy-related domains (language conventions, reading, and writing scores), and numeracy achievement comprised achievement in the numeracy domain. NAPLAN assesses the following literacy-related skills: spelling, grammar and punctuation (language conventions), comprehension (reading) and knowledge, and control of written language (writing). The NAPLAN numeracy test assesses skills related to number and algebra, measurement and geometry, and statistics and probability. The response formats for questions are either multiple choice or short written response. For the writing test, students are asked to write a text (e.g., a story) in response to a prompt. The time provision given for completion of the language conventions, writing, reading, and numeracy tests is 45 min, 40 min, 65 min, and 40 min, respectively.28
Each child's sex and age were obtained via parent-reported questionnaires administered using an iPad. With each wave, LSAC releases a composite household-level socioeconomic position (SEP) score derived from parent-reported occupation, household income and highest level of parental education.29 The Wave 6 SEP score was used in our analysis. Biological maturity was estimated using the Pubertal Development Scale.30 For the Pubertal Development Scale, children self-reported their stage of pubertal development based on a number of typical physical indicators. A mean score was calculated and later categorized as 1 = pre-pubertal, 2 = early pubertal, 3 = mid-pubertal, 4 = late pubertal, or 5 = post-pubertal.
2.4. Statistical analyses
Statistical analyses were conducted using Stata 16 (StataCorp., College Station, TX, USA), and significance levels were set to p < 0.05. Descriptive statistics are presented as mean and SD for continuous variables and as percentage for categorical variables. Independent samples t tests were used to compare continuous variables, and chi square analyses were used to compare categorical variables between those included and excluded from analyses.
The independent variable in the analyses was compliance with all possible combinations of meeting guidelines: (I) no guidelines, (II) screen time only, (III) sleep only, (IV) MVPA only, (V) screen time + MVPA, (VI) sleep + MVPA, (VII) screen time + sleep, and (VIII) all guidelines. The dependent variables were literacy and numeracy scores. All analyses were adjusted for age, sex, SEP, and pubertal development. Analysis of covariance (ANCOVA) was performed to test for mean differences, with t tests with sequential Bonferroni adjustments used to compare each level of the independent variable with the “meets no guidelines” condition. Analyses were performed for compliance with guidelines assessed both by self-report and by accelerometry (for MVPA and sleep) and self-report (for screen time) in combination. Although screen time cannot be objectively measured by accelerometers, for ease of reading, the “accelerometry-measured MVPA and sleep + self-reported screen time” model will be referred to herein as “accelerometry”. ANCOVA was also used to assess differences in literacy and numeracy achievement by number of guidelines met (0−3).
2.5. Data availability statement
The LSAC and CheckPoint data are available under license at https://growingupinaustralia.gov.au/data-and-documentation/accessing-lsac-data.
3. Results
Of the 1874 CheckPoint participants, data were missing for SEP (n = 7), pubertal development (n = 152), MARCA (n = 42), accelerometry (n = 482), numeracy (n = 253), and literacy (n = 11). The final analytic sample comprised 1270 (self-report analyses) and 927 (accelerometry analyses) for both boys and girls. Participant characteristics are presented in Table 1, along with mean min/day spent in each movement behavior for self-report and accelerometry data, and achievement scores for literacy and numeracy. Additionally, characteristics of participants excluded from analyses (due to missing data for accelerometry, MARCA, academic achievement, or covariates) are presented. Compared with included children, excluded children were slightly older and from lower SEP households, had more screen time, had less MVPA, and had lower literacy and numeracy achievement.
Table 1.
Descriptive characteristics of participants (mean ± SD or n (%)).
| Included in analyses | Excluded from analysesb | p (ttest/χ2) | |
|---|---|---|---|
| Demographic characteristics | |||
| male | 1270 (52) | 604 (49) | 0.170 |
| Age | 11.99 ± 0.38 | 12.04 ± 0.44 | 0.007 |
| SEP z-score | 0.22 ± 0.98 | 0.07 ± 1.00 | 0.002 |
| Pubertal status | |||
| Pre-pubertal | 124 (10) | 41 (9) | 0.330 |
| Early pubertal | 323 (25) | 122 (26) | |
| Mid-pubertal | 654 (52) | 231 (50) | |
| Late pubertal | 165 (13) | 64 (14) | |
| Post-pubertal | 4 (0.3) | 5 (1.0) | |
| Movement behaviors (self-report, min/day) | |||
| MVPA | 121 ±78 | 115 ± 71 | 0.120 |
| Sleep | 600 ± 63 | 596 ± 62 | 0.180 |
| Screen time | 186 ± 116 | 203 ± 115 | 0.006 |
| Movement behaviors (accelerometry, min/day) | |||
| MVPA | 63 ± 35 | 59 ± 35 | 0.030 |
| Sleep | 567 ± 47 | 564 ± 64 | 0.320 |
| Academic outcomes | |||
| Literacya | 556 ± 61 | 541 ± 60 | 0.004 |
| Numeracy | 576 ± 70 | 557 ± 59 | 0.001 |
Notes: Due to rounding some percentages add up to >100%. Bold text denotes p < 0.05.
Literacy score was calculated as the arithmetic mean of language, reading, writing, and spelling scores.
n does not always add up to 604 due to missing data. Abbreviations: MVPA = moderate-to-vigorous intensity physical activity; SEP = socioeconomic position.
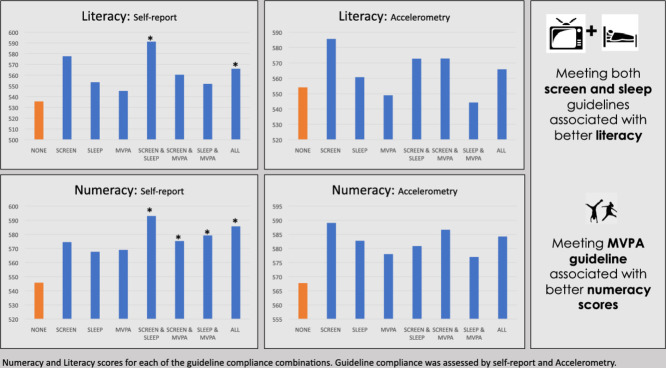
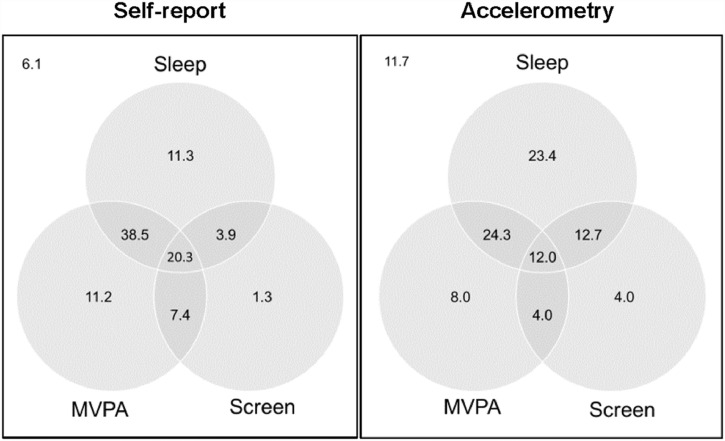
Fig. 1 shows the proportion of children meeting no guidelines, physical activity, sedentary behavior, sleep guidelines, and the combinations of these guidelines for self-report and accelerometry measures, respectively. Results for meeting the sleep guideline were reasonably consistent between self-report (74.0%) and accelerometry measures (72.4%). However, results for meeting the MVPA guideline varied between self-report (77.4%) and accelerometry measures (48.2%). The screen time guideline (self-report only) was met by approximately one-third (32.9%) of children.
Fig. 1.
Venn diagram showing the proportion (%) of children meeting no guidelines, physical activity, sedentary behavior, or sleep guideline; and combinations of these guidelines as assessed via self-report (left panel, n = 1270) and accelerometry (right panel, n = 927). The accelerometry model refers to objectively measured MVPA and sleep + self-reported screen time. MVPA = moderate-to-vigorous intensity physical activity.
ANCOVA was used to compare academic achievement scores for children meeting the physical activity, screen time, or sleep guideline alone and in combination, relative to children who did not meet any of the guidelines. Four ANCOVAs were performed separately for academic achievement in literacy and numeracy, relative to guideline compliance assessed by self-report or by accelerometry. When assessed based on self-reported movement behaviors, academic achievement in both literacy (F(7, 1258) = 3.08, p = 0.003) and numeracy (F(7, 1258) = 2.92, p = 0.005) significantly differed based on guideline compliance. For accelerometer assessed movement behaviors, academic achievement in literacy differed based on guideline compliance (F(7, 915) = 2.40, p = 0.02). However, there were no differences in numeracy achievement (F(7, 915) = 0.80, p = 0.58).
A t test with sequential Bonferroni adjustment was used to compare each level of the independent variable with the “meets no guidelines” condition. Table 2 shows the mean ± SD for literacy and numeracy scores for each of the compliance categories, with scores significantly different from the “meets no guidelines” condition denoted in bold text. When assessed by self-report, there were significant differences in literacy achievement among those who met all guidelines (t(334) = −4.05, p = 0.0001, d = 0.7) or met the screen time and sleep guidelines in combination (t(125) = −5.02, p < 0.001, d = 0.9), compared with the “meets no guidelines” category. There were also significant differences in numeracy achievement, particularly among those who met the MVPA guideline in any combination (p < 0.05, d = 0.3−0.7), compared with those who met none. Post-hoc analyses showed when assessed by accelerometry, there were no differences in literacy achievement for any movement behavior combination when compared with the “meets no guideline” condition.
Table 2.
NAPLAN scores for literacy and numeracy for children meeting the physical activity, screen time and sleep guidelines alone and in combination (mean ± SD).
| Guidelines met | Literacy |
Numeracy |
||
|---|---|---|---|---|
| Self-report (n = 1270) |
Accelerometry (n = 927) |
Self-report (n = 1270) |
Accelerometry (n = 927) |
|
| None | 536 ± 68 | 554 ± 68 | 546 ± 66 | 568 ± 76 |
| Screen | 578 ± 70 | 586 ± 57 | 574 ± 64 | 589 ± 74 |
| Sleep | 553 ± 66 | 561 ± 60 | 568 ± 79 | 583 ± 76 |
| MVPA | 545 ± 65 | 549 ± 68 | 569 ± 73 | 578 ± 72 |
| Screen + Sleep | 591 ± 47⁎⁎⁎ | 573 ± 53 | 593 ± 66⁎⁎ | 581 ± 66 |
| Screen + MVPA | 560 ± 61 | 573 ± 56 | 575 ± 69* | 587 ± 73 |
| Sleep + MVPA | 552 ± 60 | 544 ± 58 | 579 ± 69⁎⁎ | 577 ± 64 |
| All | 566 ± 55⁎⁎ | 566 ± 54 | 586 ± 67⁎⁎⁎ | 584 ± 63 |
Note: The accelerometry model refers to objectively measured MVPA and sleep + self-reported screen time.
p < 0.01;
p = 0.0001;
p < 0.0001
statistically significant difference compared with None (does not meet any guidelines) based on t test with sequential Bonferroni adjustment.
Abbreviations: MVPA = moderate-to-vigorous intensity physical activity; NAPLAN = National Assessment Program−Literacy and Numeracy.
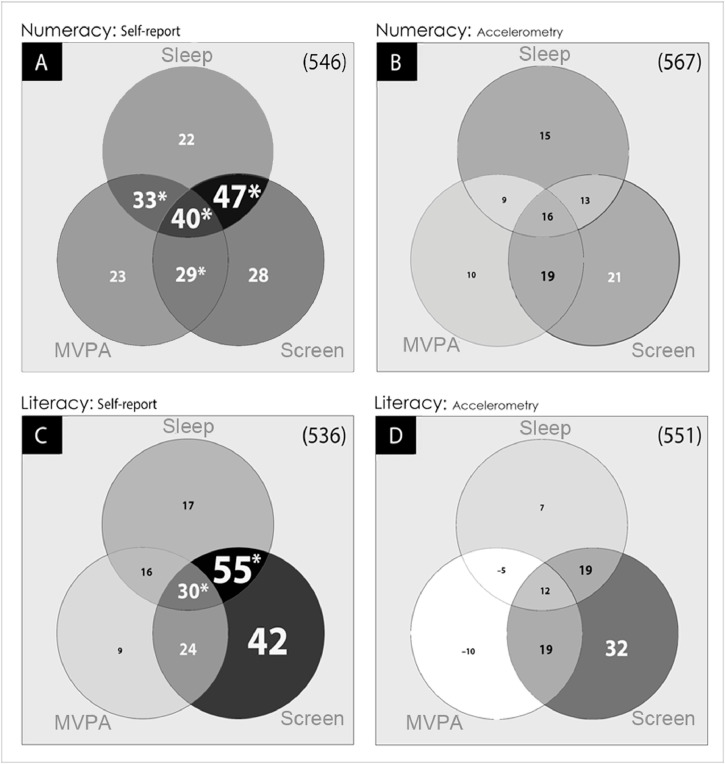
Fig. 2 shows the difference in literacy and numeracy scores from each of the 7 guideline compliance combinations, relative to the “meets no guidelines” condition, as assessed by self-report and accelerometry. The shading indicates that stronger academic performance was generally achieved where guidelines were met in combination (i.e., darker shading in overlapping areas), although the most favorable combination differed depending on the academic performance outcome of interest and the movement behavior measurement methodology. Although not significant in all cases, higher literacy scores were most strongly associated with meeting the screen time guideline. For example, averaged across all participants, literacy scores were 21–32 points higher in children who met the screen time guideline compared with only 8–19 points higher in children meeting the MVPA guideline, and 7–22 points higher in children meeting the sleep guideline (in any combination), compared to those who did not meet any of the guidelines. Higher numeracy scores were generally associated with meeting the MVPA guideline in any combination, compared with meeting only 1 guideline.
Fig 2.
Venn diagram showing the difference in numeracy (A and B) and literacy (C and D) scores for each of the 7 remaining combinations, compared to the “meets no guidelines” condition (indicated in the right-corner brackets). Differences are assessed by MARCA (A and C) and Accelerometry (B and D). Larger differences are indicated by larger fonts and darker backgrounds. The accelerometry model refers to objectively measured MVPA and sleep + self-reported screen time. * p < 0.05 compared to the “meets no guidelines” condition. MARCA = Multimedia Activity Recall for Children and Adolescents; MVPA = moderate-to-vigorous intensity physical activity.
ANCOVA was also used to test for differences in literacy and numeracy achievement by the number of guidelines met (data not shown). There were statistically significant differences in numeracy achievement by number of guidelines met when assessed by self-report (F(3,1262) = 5.46, p = 0.01), but not when assessed by accelerometry (F(3,919) = 0.89, p = 0.45). A post hoc analysis showed that compared with those who met no guidelines, those who met at least 1 guideline had numeracy scores 23 points higher (t(378) = −2.46, p = 0.01). This increased to 34 point t(708) = −4.16, p < 0.001) and 40 points (t(334) = −4.66, p < 0.001) higher for meeting 2 or 3 guidelines, respectively. There were no significant differences between number of guidelines met and literacy achievement when assessed by self-report (F(3,1262) = 2.32, p = 0.07) or by accelerometry (F(3,919) = 0.48, p = 0.70).
4. Discussion
4.1. Main findings
The combined effects of meeting multiple recommendations from the 24-h movement guidelines have a stronger positive association with academic achievement than any individual association. While meeting the MVPA guideline was important for numeracy achievement, meeting the screen time and sleep guidelines in combination had the strongest positive association with literacy achievement. The strength of associations between academic performance and 24-h movement guideline compliance differed depending on whether guideline compliance was based on self-reported or objectively measured movement data, with self-reported data suggesting stronger associations.
4.2. Strengths and limitations
This study is one of the first to examine associations between meeting single and combined 24-h movement guidelines and academic achievement. It used a large, population-derived sample; a standardized national measure of literacy and numeracy achievement; and objective movement data. Time use was assessed using 2 different methods—a validated self-report use-of-time recall and accelerometry. Although these methods yielded quite different estimates of MVPA (121 min/day vs. 63 min/day), results were broadly similar using both methods, indicating robustness of findings. Additionally, estimates of compliance with guidelines in this study (self-report for sleep = 74.0%, screen time = 32.9%, and MVPA = 77.4%) and accelerometry (sleep = 72.4% and MVPA = 48.2%) were broadly similar to those reported in other studies of Australian primary school-aged children for self-report (sleep = 66%, screen time = 15%, and MVPA = 25%)31 and accelerometer measures (sleep = 76% and MVPA = 55%).32
However, certain limitations must be acknowledged. Our study was cross-sectional and thus causality cannot be determined. The narrow age range of participants and potential bias inherent in self-report measures of time use are further limitations of our study. Additionally, the number of children in each of the compliance categories was unbalanced, with small numbers in some categories (e.g., only 1.3% of the sample met the screen time guidelines when assessed by self-report), and this could have affected our findings. Our results may not be generalizable because excluded participants were significantly different from included participants. There was considerable lag time between when children completed NAPLAN testing and when movement behaviors were measured, which should be taken into consideration when interpreting results. NAPLAN data were collected in May 2015, May 2016, and May 2017. Movement data were collected between February 2015 and March 2016. On average, NAPLAN measurements were taken 8 months after movement measurements. Nonetheless, NAPLAN provides an indicative level of usual academic performance,33 and measuring children's activity patterns for 7 days has been shown to capture their usual activity levels.34 Thus, it is expected that the associations observed in this study are meaningful. Our study is focused on screen time. However sedentary time is composed of both screen-based and non-screen-based sedentary time (e.g., reading, sitting in class).35 These different types of sedentary time could be expected to have different associations with academic performance. Last, no adjustment for nesting/clustering was performed in our analyses and this may have impacted the associations of interest.
4.3. Implications
Meeting the screen time and sleep guidelines in combination had the strongest positive association with literacy achievement. Those who met these guidelines in combination scored up to 55 points higher in literacy than those who did not meet any guidelines, the equivalency of approximately 3 years of schooling.36 Prior studies have also examined the independent and combined associations between meeting the sleep and screen time guidelines and cognition and academic performance. Consistent with our findings, Walsh et al.13 found that the most optimal cognition was observed when the screen time and sleep guidelines were met together. Similarly, Lien et al.14 reported that high school students who met the screen time and sleep guidelines in combination and middle school students who met the screen time or sleep guideline alone had higher overall academic performance compared to those who did not meet any guidelines. Other studies have also reported positive associations between meeting the screen time guideline and academic achievement. Faught and colleagues12 also found that students who met the screen time guideline at both baseline and follow up had increased odds of achieving a higher grade in English, compared to students who did not meet the guidelines. In another study,11 meeting the screen time guideline was associated with greater likelihood of meeting expectations on a standardized writing exam among children aged 10−11 years.
While possible mechanisms for associations between 24-h movement guidelines and academic achievement could not be examined in our study, meta-analytic results indicate a longer sleep duration is associated with better full and verbal intelligence quotient in children (r = 0.15),37 which could contribute to better literacy achievement. Additionally, excessive screen time has been associated with shorter sleep duration.38 Combined, these results provide a possible explanation for the stronger combined associations, compared with individual associations, of sleep and screen time with literacy achievement observed in our study.
Although our results were not significant in all cases, they suggest that meeting the screen time guideline was particularly important for literacy achievement. When averaged across all participants, literacy scores were 24 to 55 points higher in children who met screen time guideline vs. only 9–30 points higher in children meeting the MVPA guideline, and 16–30 points higher in children the meeting sleep guideline (in any combination), compared to those who did not meet any guidelines (Fig. 2). Similar patterns, albeit non-significant, were evident when meeting the guidelines was measured using accelerometry (Fig. 2).
Those meeting screen guidelines may have had better literacy achievement than those not meeting any guidelines because of time trade-offs between screen time and activities that support language development such as reading, homework, and creative play,39 along with verbal interaction with grown-up caregivers.40 Data from the current study showed that those who met the screen time guideline spent more time reading (48 min/day vs. 30 min/day) and less time watching television (52 min/day vs. 162 min/day) than those who did not meet screen time guidelines. Thus, screen time may displace activities that support literacy development (e.g., reading). Additionally, screen time (including the use of smart phones, tablets, desktop and laptop computers, and televisions) involves immersion in a visual, as opposed to a textual medium. It is possible that screen use and reading constitute different cognitive styles. Screen time has been shown to be correlated with decreased functional activity in the reading-related brain networks, whereas reading has been linked to increased activity in these networks, providing a further possible explanation for the literacy benefits associated with limiting screen time.41 However, it should be noted that only a small number of children met the screen time guideline alone (1.3%), the screen time and sleep guidelines in combination (3.9%), or the screen time and MVPA guidelines in combination (7.4%). Hence, the large differences observed in the self-report models have wide confidence intervals.
In 3 out of 4 significant associations, meeting the MVPA guideline in combination with the other guidelines was associated with superior numeracy achievement. Thus, MVPA may be particularly beneficial for numeracy achievement (but not literacy achievement). Those who met the MVPA guideline in any combination scored 23–40 points higher in numeracy than those who did not meet any guidelines, an equivalency of up to approximately 1 year of schooling.36 This differs from results in similar studies showing that meeting the MVPA guideline was not associated with mathematics achievment.11,12 In contrast to these previous studies but similar to our findings, systematic reviews of associations between physical activity (not the MVPA guideline specifically) and academic achievement have indicated larger benefits for mathematics achievement compared with literacy achievement.42,43 This is possibly due to selective cognitive effects of physical activity. Physical activity has been shown to increase prefrontal cortex activity.44 Prefrontal regions of the brain play an important role in mathematical cognition,45 providing a possible explanation for the stronger associations observed between MVPA and mathematics achievement compared with literacy achievement. However, because few studies on the associations between mathematics achievement and 24-h movement guideline compliance have been conducted, future research is needed to clarify this association.
Self-reported 24-h movement guideline compliance was associated with both domains of academic performance, but device-measured guideline compliance was not. Different estimates of guideline compliance, particularly for MVPA derived from self-report and accelerometry, may be driving this discrepancy. Given the different estimates of MVPA derived from self-report and accelerometer measures, associations with academic performance can be expected to differ.
In our study, the proportion of children meeting the MVPA guideline differed between self-report (77.4%) and accelerometry (48.2%). A number of possible reasons for differences in MVPA as measured by self-report and accelerometry have been proposed. First, social desirability bias—that is, the over-reporting of behaviors perceived to be “good”—has been associated with differences in MVPA when measured by self-report and accelerometry.46 A second reason relates to the epoch effect, which refers to the duration over which the intensity of an activity is averaged. The epoch effect has also been shown to affect estimates of MVPA, given that in self-report the epoch refers to the amount of time an instrument requires participants to recall (usually 5–60 min) whereas for accelerometry the epoch is generally set to between 1 s and 60 s. Thus, when recalling the amount of time in MVPA for a 30-min tennis match, for example, a person may record this as 30 min of MVPA, whereas an accelerometer may only register a proportion of this time as MVPA.47 A third reason involves the cut-point effect, which means that random error in measuring energy expenditure in activities close to the light-physical activity and MVPA cut-point can mean that accelerometer-measured light-intensity will be classified as self-report MVPA.48 A fourth reason is that a wide range of decisions around processing accelerometer data, including cut-points, epoch length, non-wear and filtering, can affect device-based estimates. While these effects provide several possible explanations for differential associations, ours is the first study to explore associations between guideline compliance and academic achievement using an objective measure of movement behavior.
Generally speaking, there were positive additive associations between guideline compliance and literacy and numeracy achievement (compared to meeting no guidelines). Other studies have also reported positive additive associations between meeting multiple lifestyle behavior guidelines and achievement in reading, writing, mathematics,11 and global cognition.13 While these findings were not replicated by our findings when we used the accelerometry model, the relatively small number of children in some of our categories (e.g., 12% in the “meets all guidelines” category) may provide a possible explanation for this. Nonetheless, given the health benefits that accrue from limiting recreational screen time, gaining adequate sleep, and participating in physical activity, school administrators and policy makers should encourage compliance with the 24-h movement guidelines for promoting both health and academic benefits in children.
5. Conclusion
In summary, our study indicates that while meeting multiple recommendations from the 24-h movement guidelines (by self-report) is important for children's literacy and numeracy achievement, meeting the screen time guideline is particularly important for literacy achievement. Interventions aimed at improving literacy and numeracy achievement should encourage adherence to the 24-h movement guidelines. Additionally, interventions aimed at improving literacy achievement perhaps should have a focus on limiting recreational screen time (and perhaps replacing it with reading).
Acknowledgments
This paper uses unit record data from Growing Up in Australia: The Longitudinal Study of Australian Children (LSAC). LSAC is conducted as a partnership among the Department of Social Services (DSS), the Australian Institute of Family Studies (AIFS) and the Australian Bureau of Statistics (ABS). The findings and views reported in our paper are solely those of the authors and should not be attributed to DSS, AIFS, or ABS. AW had full access to all the data in LSAC and takes responsibility for the integrity of the data and the accuracy of the data analysis. We thank LSAC and CheckPoint study participants, staff and students for their contributions. Child Health CheckPoint was supported by the National Health and Medical Research Council (NHMRC) project grants (1041352 and 1109355), a Royal Children's Hospital Foundation grant (2014-241), the Murdoch Children's Research Institute (MCRI), the University of Melbourne, a National Heart Foundation of Australia grant (100660), and Financial Markets Foundation for Children grants (2014-055 and 2016-310). Research at the MCRI is supported by the Victorian Government's Operational Infrastructure Support Program. CM is supported by a Career Development Fellowship from the NHMRC (APP1125913). AW is funded by an NHMRC project grant APP1143379 (2018-2022). DD is supported by an NHMRC early career fellowship (APP1162166) and a Heart Foundation postgraduate fellowship (102084).
Authors' contributions
AW conceived the study, performed the analysis and drafted the manuscript; TO, CM, and DD assisted in interpreting the results and critically appraised the manuscript. All authors have read and approved the final manuscript, and agree with the order of the presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Appendix. Supplementary materials
References
- 1.Álvarez-Bueno C, Pesce C, Cavero-Redondo I, Sánchez-López M, Garrido-Miguel M, Martínez-Vizcaíno V. Academic achievement and physical activity: A meta-analysis. Pediatrics. 2017;140 doi: 10.1542/peds.2017-1498. [DOI] [PubMed] [Google Scholar]
- 2.Carson V, Hunter S, Kuzik N, et al. Systematic review of sedentary behavior and health indicators in school-aged children and youth: An update. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S240–S265. doi: 10.1139/apnm-2015-0630. [DOI] [PubMed] [Google Scholar]
- 3.Short MA, Blunden S, Rigney G, et al. Cognition and objectively measured sleep duration in children: A systematic review and meta-analysis. Sleep Health. 2018;4:292–300. doi: 10.1016/j.sleh.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Dumuid D, Olds T, Martín-Fernández JA, Lewis LK, Cassidy L, Maher C. Academic performance and lifestyle behaviors in Australian school children: A cluster analysis. Health Educ Behav. 2017;44:918–927. doi: 10.1177/1090198117699508. [DOI] [PubMed] [Google Scholar]
- 5.Maher C, Lewis L, Katzmarzyk PT, Dumuid D, Cassidy L, Olds T. The associations between physical activity, sedentary behavior and academic performance. J Sci Med Sport. 2016;19:1004–1009. doi: 10.1016/j.jsams.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Tremblay MS, Carson V, Chaput JP, et al. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behavior, and sleep. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S311–S327. doi: 10.1139/apnm-2016-0203. [DOI] [PubMed] [Google Scholar]
- 7.Australian Government Department of Health. Australian 24-Hour Movement Guidelines for Children and Young People (5−17 years): An integration of physical activity, sedentary behavior, and sleep—research report. Available at: https://www1.health.gov.au/internet/main/publishing.nsf/Content/ti-5-17years. [accessed 09.04.2020].
- 8.New Zealand Ministry of Health . New Zealand Ministry of Health; Wellington: 2017. Sit Less, Move More, Sleep Well: Physical Activity Guidelines for Children and Young People. [Google Scholar]
- 9.Sports Science Institute of South Africa. 24-Hour Movement Guidelinesfor Children. Available at: https://www.ssisa.com/news/movement-guidelines-children/. [accessed 22.04.2020].
- 10.World Health Organization. WHO Guidelines on physical activity and sedentary behavior for children and adolescents, adults and older adults. Draft 26 March 2020, for consultation only. Available at: https://www.who.int/docs/default-source/physical-activity/call-for-consultation/draft-guideline-on-physical-activity-and-sedentray-behavior.pdf?sfvrsn=ddf523d5_4. [accessed 22.04.2020].
- 11.Faught EL, Ekwaru JP, Gleddie D, Storey KE, Asbridge M, Veugelers PJ. The combined impact of diet, physical activity, sleep and screen time on academic achievement: A prospective study of elementary school students in Nova Scotia. Canada Int J Behav Nutr Phys Act. 2017;14:29. doi: 10.1186/s12966-017-0476-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faught EL, Qian W, Carson VL, et al. The longitudinal impact of diet, physical activity, sleep, and screen time on Canadian adolescents' academic achievement: An analysis from the COMPASS study. Prev Med. 2019;125:24–31. doi: 10.1016/j.ypmed.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Walsh JJ, Barnes JD, Cameron JD, et al. Associations between 24 hour movement behaviors and global cognition in US children: A cross-sectional observational study. Lancet Child Adolesc Health. 2018;2:783–791. doi: 10.1016/S2352-4642(18)30278-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lien A, Sampasa-Kanyinga H, Colman I, Hamilton HA, Chaput JP. Adherence to 24-hour movement guidelines and academic performance in adolescents. Public Health. 2020;183:8–14. doi: 10.1016/j.puhe.2020.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Powell D, Higgins HJ, Aram R, Freed A. Impact of No Child Left Behind on curriculum and instruction in rural schools. The Rural Educator. 2009;31:439. doi: 10.35608/ruraled.v31i1.439. [DOI] [Google Scholar]
- 16.Wilkins J, Graham G, Parker S, Westfall S, Fraser R, Tembo M. Time in the arts and physical education and school achievement. J Curric Stud. 2003;35:721–734. [Google Scholar]
- 17.Clifford SA, Davies S, Wake M. Child Health CheckPoint team. Child Health CheckPoint: Cohort summary and methodology of a physical health and biospecimen module for the Longitudinal Study of Australian Children. BMJ Open. 2019;9(Suppl. 3):S3–22. doi: 10.1136/bmjopen-2017-020261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wake M, Clifford S, York E, Mensah F, Burgner D, Davies S. Introducing growing Up in Australia's Child Health CheckPoint. A physical and biomarkers module for the Longitudinal Study of Australian Children. Family Matters. 2014;95:15–23. [Google Scholar]
- 19.ADA Dataverse. Growing Up in Australia: Longitudinal Study of Australian Children (LSAC) Release 7.2 (Waves 1–7). Available at: http://dx.doi.org/10.26193/F2YRL5. [accessed 22.11.2019].
- 20.Ridley K, Olds TS, Hill A. The Multimedia Activity Recall for Children and Adolescents (MARCA): Development and evaluation. Int J Behav Nutr Phys Act. 2006;3:10. doi: 10.1186/1479-5868-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ridley K, Ainsworth BE, Olds TS. Development of a compendium of energy expenditures for youth. Int J Behav Nutr Phys Act. 2008;5:45. doi: 10.1186/1479-5868-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olds TS, Ridley K, Dollman J, Maher CA. The validity of a computerized use of time recall, the multimedia activity recall for children and adolescents. Pediatr Exerc Sci. 2010;22:34–43. doi: 10.1123/pes.22.1.34. [DOI] [PubMed] [Google Scholar]
- 23.Foley LS, Maddison R, Rush E, Olds TS, Ridley K, Jiang Y. Doubly labeled water validation of a computerized use-of-time recall in active young people. Metabolism. 2013;62:163–169. doi: 10.1016/j.metabol.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 24.Fraysse F, Grobler AC, Muller J, Wake M, Olds T. Physical activity and sedentary activity: Population epidemiology and concordance in Australian children aged 11−12 years and their parents. BMJ Open. 2019;9(Suppl. 3):S136–S146. doi: 10.1136/bmjopen-2018-023194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phillips LR, Parfitt G, Rowlands AV. Calibration of the GENEA accelerometer for assessment of physical activity intensity in children. J Sci Med Sport. 2013;16:124–128. doi: 10.1016/j.jsams.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 26.van Hees VT, Sabia S, Anderson KN, et al. A Novel, open access method to assess sleep duration using a wrist-worn accelerometer. PLoS One. 2015;10 doi: 10.1371/journal.pone.0142533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Australian Curriculum Assessment and Reporting Authority. National Assessment Program-Literacy and Numeracy 2016. Available at: http://www.nap.edu.au. [accessed 11.12.2019].
- 28.Queensland Curriculum and Assessment Authority. NAPLAN tests general information. Available at: https://www.qcaa.qld.edu.au/p-10/naplan/general-information. [accessed 11.12.2019].
- 29.Blakemore T, Strazdins L, Gibbings J. Measuring family socioeconomic position. Australian Social Policy. 2009;8:121–168. [Google Scholar]
- 30.Robertson EB, Skinner ML, Love MM, et al. The Pubertal Development Scale. J Early Adolesc. 1992;12:174–186. [Google Scholar]
- 31.Hardy LL, Mihrshahi S, Bellew W, Bauman A, Ding D. Children's adherence to health behavior recommendations associated with reducing risk of non-communicable disease. Prev Med Rep. 2017;8:279–285. doi: 10.1016/j.pmedr.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roman-Viñas B, Chaput JP, Katzmarzyk PT, et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int J Behav Nutr Phys Act. 2016;13:123. doi: 10.1186/s12966-016-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu M. What national testing data can tell us. National Testing in Schools. London: Routledge. 2015 p. 18--29. [Google Scholar]
- 34.Dillon CB, Fitzgerald AP, Kearney PM, et al. Number of days required to estimate habitual activity using wrist-worn GENEActivaccelerometer: A cross-sectional study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0109913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olds TS, Maher CA, Ridley K, Kittel DM. Descriptive epidemiology of screen and non-screen sedentary time in adolescents: A cross sectional study. Int J Behav Nutr Phys Act. 2010;7:92. doi: 10.1186/1479-5868-7-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goss P, Chisholm C. Widening gaps: What NAPLAN tells us about student progress. Available at: https://grattan.edu.au/wp-content/uploads/2016/03/937-Widening-gaps-technical-report.pdf. [accessed 15.05.2020].
- 37.Short MA, Blunden S, Rigney G, et al. Cognition and objectively measured sleep duration in children: A systematic review and meta-analysis. Sleep Health. 2018;4:292–300. doi: 10.1016/j.sleh.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 38.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010;11:735–742. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 39.Zimmerman FJ, Christakis DA, Meltzoff AN. Associations between media viewing and language development in children under age 2 years. J Pediatr. 2007;151:364–368. doi: 10.1016/j.jpeds.2007.04.071. [DOI] [PubMed] [Google Scholar]
- 40.Christakis DA, Gilkerson J, Richards JA, et al. Audible television and decreased adult words, infant vocalizations, and conversational turns: A population-based study. Arch Pediatr Adolesc Med. 2009;163:554–558. doi: 10.1001/archpediatrics.2009.61. [DOI] [PubMed] [Google Scholar]
- 41.Horowitz-Kraus T, Hutton JS. Brain connectivity in children is increased by the time they spend reading books and decreased by the length of exposure to screen-based media. Acta Paediatr. 2018;107:685–693. doi: 10.1111/apa.14176. [DOI] [PubMed] [Google Scholar]
- 42.Singh AS, Saliasi E, van den Berg V, et al. Effects of physical activity interventions on cognitive and academic performance in children and adolescents: A novel combination of a systematic review and recommendations from an expert panel. Br J Sports Med. 2019;53:640–647. doi: 10.1136/bjsports-2017-098136. [DOI] [PubMed] [Google Scholar]
- 43.Fedewa AL, Ahn S. The effects of physical activity and physical fitness on children's achievement and cognitive outcomes: A meta-analysis. Res Q Exerc Sport. 2011;82:521–535. doi: 10.1080/02701367.2011.10599785. [DOI] [PubMed] [Google Scholar]
- 44.Chaddock L, Pontifex MB, Hillman CH, Kramer AF. A review of the relation of aerobic fitness and physical activity to brain structure and function in children. J Int Neuropsychol Soc. 2011;17:975–985. doi: 10.1017/S1355617711000567. [DOI] [PubMed] [Google Scholar]
- 45.Arsalidou M, Pawliw-Levac M, Sadeghi M, Pascual-Leone J. Brain areas associated with numbers and calculations in children: Meta-analyses of fMRI studies. Dev Cogn Neurosci. 2018;30:239–250. doi: 10.1016/j.dcn.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klesges LM, Baranowski T, Beech B, et al. Social desirability bias in self-reported dietary, physical activity and weight concerns measures in 8- to 10-year-old African-American girls: Results from the Girls health Enrichment Multisite Studies (GEMS) Prev Med. 2004;38:78–87. doi: 10.1016/j.ypmed.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 47.Aibar A, Chanal J. Physical education: The effect of epoch lengths on children's physical activity in a structured context. PLoS One. 2015;10 doi: 10.1371/journal.pone.0121238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Olds TS, Gomersall SR, Olds ST, Ridley K. A source of systematic bias in self-reported physical activity: The cutpoint bias hypothesis. J Sci Med Sport. 2019;22:924–928. doi: 10.1016/j.jsams.2019.03.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The LSAC and CheckPoint data are available under license at https://growingupinaustralia.gov.au/data-and-documentation/accessing-lsac-data.