Abstract
Background
Neurogenic lower urinary tract dysfunction is an abnormality in the presence of underlying neurologic disease. A recent systematic review and meta-analysis demonstrated that storage phase symptoms are the predominant symptoms among people with multiple sclerosis (PwMS). Transcutaneous tibial nerve stimulation (TTNS) is a non-invasive treatment for bladder storage symptoms; however, the potential efficacy of stimulation among PwMS is based on a small number of studies with the absence of high-quality evidence. The aim of this study was to evaluate the feasibility, acceptability, and safety of TTNS in PwMS using an affordable transcutaneous electrical nerve stimulation (TENS) unit.
Methods
A total of 23 participants with MS enrolled in the study. The primary outcomes included recruitment/retention rate, completion of the outcomes and the intervention, adherence to the protocol, adverse events, and acceptability of the intervention. The primary outcomes were assessed using diaries and a satisfaction questionnaire. The secondary outcomes included changes in urinary symptoms and quality of life assessed using a set of validated outcome measures including a 3-day bladder diary, PPIUS, ICIQ-OAB, and KHQ at baseline and post-intervention.
Results
Twenty participants completed the study. Three participants (13.04%) withdrew. All 20 participants completed the 6-week intervention and all the outcome measures (100%), with no reported adverse events. Participants were satisfied and found the unit acceptable. Three-day bladder diary showed changes in urinary frequency from a daily median of 10 times to 8 times and daily median urgency changed from 6 times at baseline to 2 times post-intervention. PPIUS showed changes in daily median sever urgency from 3 points (IQR=4) to 1 point (IQR=1) post-intervention. ICIQ-OAB total scores changed from 8 points (IQR=2.25) to 4 points (IQR=2.5) post-intervention. Median and mean scores of KHQ showed a clinical meaningful change of QoL in part-two and part-three of the questionnaire.
Conclusions
TTNS is feasible, safe, and acceptable for PwMS. Changes of urinary symptoms scores and QoL post-intervention suggested improvements. Future implications need to consider the treatment protocol including frequency of treatment sessions, duration of treatment, and the electrical stimulation parameters as well as the outcome measures followed in the current study for the implementation of the future pilot RCT.
Trial registration
ClinicalTrials.gov NCT04528784. Registered on 27 August 2020. https://register.clinicaltrials.gov/prs/app/action/LoginUser?ts=1&cx=-jg9qo4.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40814-022-01120-1.
Keywords: Neurogenic lower urinary tract dysfunction, Neuromodulation, Electrical nerve stimulation, Quality of life questionnaire, Tibial nerve
Key messages regarding feasibility
It was uncertain whether people with multiple sclerosis could be recruited at the required rate for a pilot randomised controlled trial to be conducted in future study. It was uncertain whether Transcutaneous tibial nerve stimulation (TTNS) as an option to manage urinary symptoms could be feasible in terms of acceptability, completion of required outcome measures, and safety of the intervention.
The intervention of TTNS using an affordable Transcutaneous electrical nerve stimulation (TENS) unit of 3 sessions/week for 6 weeks was found to be feasible, acceptable, and safe with a high adherence rate to the treatment protocol.
Treatment protocol and the outcome measures followed in the current single-arm feasibility study were recommended for the future pilot RCT.
Background
Neurogenic lower urinary tract dysfunction (NLUTD) is an abnormality in the presence of underlying neurologic disease [1]. The pattern of lower urinary tract dysfunction following neurological disease depends on the site and nature of the lesion [2, 3]. In people with MS (PwMS), central nervous system lesions are mainly present at supra-pontine and/or supra-sacral areas affecting the storage phase, or both storage and voiding phase accompanied with incomplete bladder emptying [3, 4]. A recent systematic review and meta-analysis demonstrated that storage phase symptoms are the predominant symptoms among PwMS. Urinary frequency had a pooled prevalence of 73.45% followed by urgency at 63.87% using subjective outcome measures [5]. Commonly, patients may present with mixed storage and voiding phase symptoms which was reported in 50–60% of women and men with MS respectively [6].
In PwMS, urinary symptoms negatively impacts on emotional wellbeing, physical health, employment opportunities, recreational activities, and social life [7–11]. Qualitative research has similarly found that urinary symptoms are very troublesome for PwMS and that many PwMS continue to suffer in silence, unsure or unaware of what services to access and they frequently experience gaps in health service provision [12].
Tibial nerve stimulation (TNS) is a form of non-surgical neuromodulation [4] and its main function is to inhibit bladder contraction which in turn reduces high bladder pressure and therefore prevents urinary incontinence [13] and preserve long-term renal function. PwMS and healthcare providers have reported they are open to the use of transcutaneous tibial nerve stimulation (TTNS) for urinary symptoms [12]. A systematic review [14] on the efficacy of TNS among people with MS identified seven studies: 6 focused on percutaneous tibial nerve stimulation (PTNS) and one focused on TTNS. There was significant heterogeneity across the included studies concerning sample sizes, populations studied, the absence of placebo or sham arm and inconsistency relating to the electrical stimulation parameters, frequency of treatment per week, and total number of sessions. The authors concluded that further well-designed experimental studies are needed to examine the impact of TTNS, using a non-invasive technique by applying two adhesive pads rather than the semi-invasive procedure of PTNS by inserting a needle, for neurogenic bladder storage symptoms in PwMS.
The primary aim of the current study is to assess the feasibility and acceptability of TTNS. The secondary aim is to explore changes in bladder storage symptoms and quality of life following treatment
Methods
Study design
This is a single-arm feasibility study conducted and reported in line with the CONSORT extension for pilot and feasibility studies [15] (Additional file 1). A detailed protocol for the study is published elsewhere [16].
Setting and participants
Community-dwelling people with any type of MS in the mid-West of Ireland were eligible to participate in the study if they met the following criteria: ambulatory (with or without assistive device), aged ≥18 years old, presented with at least one bladder storage-related symptom such as urinary frequency, urinary urgency, nocturia, with or without incontinence and were willing to give written informed consent.
Identification and consent
Recruitment to the study commenced in October 11, 2020, and follow-up was completed in March 12th 2021. Recruitment was conducted using two methods: (1) open recruitment for PwMS through MS Ireland’s communication channels including MS News e-zine, social media and direct email to members of the Mid-West branch of MS Ireland took place between October 2020 and January 2021; (2) a convenience sample of PwMS from existing participants who have already participated in our previous qualitative study [12]. Eligible participants were provided with a link to a survey using Qualtrics Survey Software Platform to read and sign the informed consent form, complete demographic data including the Patient Determined Disease Steps (PDDS) [17] and baseline outcome measures.
Once the baseline data were completed, participants received a downloadable 3- Day bladder diary by email. Participants were provided with a TENS unit and a short demonstration video for the application of TENS, and two downloadable documents: adverse events report diary and adherence to the treatment protocol. A follow-up virtual meeting was held to discuss the application of the unit with all participants. Weekly virtual meetings were also held with all participants to check adherence to the treatment protocol, adverse events, and address any participant queries.
Post-intervention (at the end of week 6), all participants received another link to Qualtrics Survey Software to complete post-intervention measures and a downloadable 3-day bladder diary. Reminders complete measures were sent to all participants within 5 days.
TTNS Intervention
Description of intervention is presented in Table 1. All TENS units were programmed and locked by KR to ensure fixed parameters were used among participants throughout the intervention. The stimulation frequency was set at 10 Hz [18–20] with a pulse duration of 0.2–0.5 ms equal to 200 μs to allow action potentials to leave the hyperpolarisation zone induced by the anodic phase [19, 21, 22]. A motor response (flexion of the great toe, and fanning of the other toes), alone or with a sensory response, (a tingling sensation at the sole of the foot) indicated the correct placement of electrode which was modified by increasing the current amplitude mA, intensity. Participants applied stimulation in a supine position with extended legs or supported sitting with the knee extended to avoid nerve root compression at the knee joint. The intervention consisted of three sessions per week, 30 min per session for a period of 6 weeks. These parameters (duration of session, frequency of sessions and timing of overall intervention) were based on findings from our qualitative study with PwMS [12], and a previous TTNS trial [23].
Table 1.
TTNS intervention
| Unit used for stimulation | Transcutaneous Electrical Nerve Stimulation (TENS)/NeuroTrac Dual channel |
| Unit price | €55.20 |
| Manufacturer | Verity Medical Ltd., United Kingdom |
| Type of electrodes | 2 self-adhesive electrodes |
| Size of electrodes | VS.5050 50 × 50 mm, square. |
| Placement of electrodes | The positive electrode was placed behind the left medial malleolus, and the negative electrode was located between 5 and 10 cm distally above the medial malleolus |
Outcome measures
The primary outcome for this study was feasibility of the intervention. This was assessed using six different metrics: (1) the number of participants who were recruited to the study, the proportion of those who (2) completed the outcome measures, (3) the 6-week intervention, (4) adhered to the treatment protocol [24], (5) the incidence of adverse events reported during the intervention, and finally, (6) acceptability of the TENS was explored using a self-report questionnaire developed by the researchers containing 5-point Likert scales: 1= “strongly disagree”; 2= “disagree”; 3= “neutral”; 4= “agree”; 5= “strongly agree”.
Secondary outcomes were used to assess the changes in bladder storage symptoms and quality of life using the International Consultation of Incontinence Questionnaire- Overactive Bladder (ICIQ-OAB) [25, 26]. The total score ranges from 0 to 16 with higher values indicating increased urinary symptom severity. Bother scales are not combined in the overall score [27]. A 3-Day bladder diary [28, 29] was used to calculate the episodes of day and night time urinary frequency. The Patient Perception of Intensity of Urgency Scale (PPIUS) [30] was included with 3-day bladder diary. PPIUS was used to assess the severity and intensity of urinary urgency. The total score ranges from 0 to 4 with higher values indicating increased urinary symptoms severity. Quality of life (QoL) was evaluated using the King’s Health Questionnaire (KHQ) [28, 31, 32]. The KHQ has three parts consisting of 21 questions in 10 main domains. Each domain scores range from 0 to 100 points whereas the severity of urinary symptom domain is scored from 0 to 30 points.
Sample size
As this is a single-arm feasibility study and not designed to evaluate the clinical effectiveness, we did not undertake a formal power analysis for sample size for a primary outcome [33]. We adopted a pragmatic approach to our choice of sample size of 20 participants. It was based on the availability of TENS devices (10 available machines) and the time allocated for the conduct of the study.
Determining progression to the pilot trial
A priori, our progression criteria to proceed to a pilot trial were determined by exploring if minimum success criteria were achieved in key feasibility aims and objectives including:
A minimum of 80% recruitment
A minimum of 80% completion rate of key outcome measures
Statistical analysis
SPSS software (Version 26.0. Armonk, NY: IBM Corp) was used for statistical analysis. All six measures of feasibility were analysed using descriptive statistics and reported as percentages and proportions. Continuous data were assessed for normality using the Shapiro-Wilks test. Means and standard deviations (SD) are reported where data are normally distributed, and medians and interquartile ranges (IQR) are reported as a conservative estimate where data are not normally distributed. The secondary outcomes of the ICIQ-OAB, KHQ [34] and the 3-day bladder diary data including the episodes of urinary frequency, nocturia, and incontinence as well as the scale of PPIUS were summarised at baseline and post intervention using medians (IQRs) and/or means (SD) depending on the distribution of data. Given the small sample size, comparability tests between baseline and post-intervention were deemed inappropriate [35]
Results
Feasibility of intervention
Recruitment, retention, and completion rates
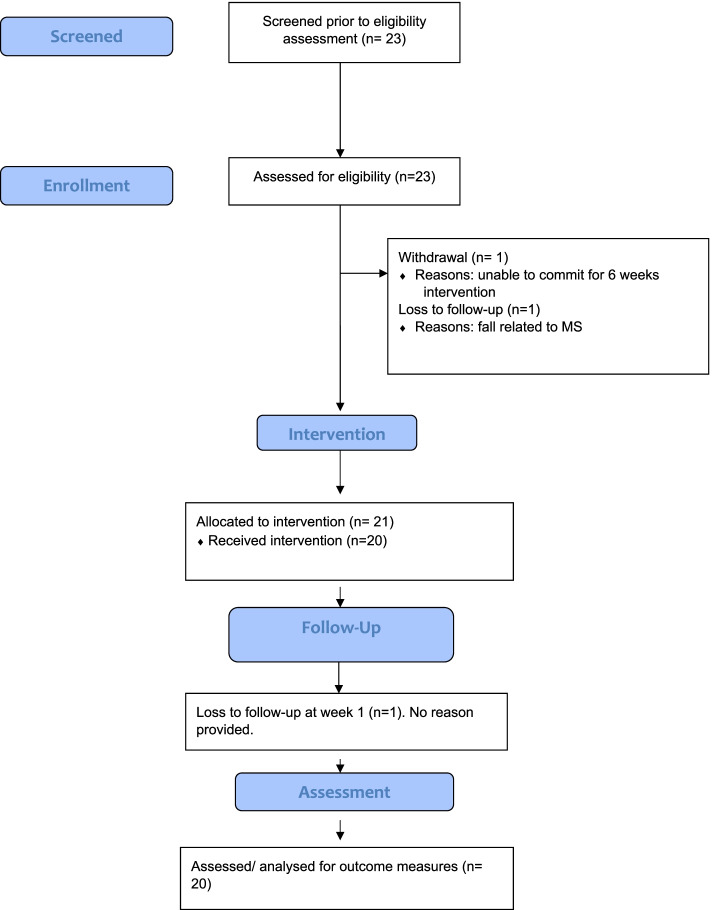
Between October 2020 and January 2021, 25 participants expressed an interest in participating in the study; 23 participants enrolled in the study, 20 participants completed the study Three participants (13.04%) discontinued their participation: one withdrew from the study before commencing the intervention due to inability to commit for 6-week, and two participants were lost to follow-up before commencing the study. All 20 participants who completed the 6-week intervention completed all outcome measures (100%). The flow of study participants is outlined in Fig. 1
Fig. 1.
Flow diagram of MS participants
Table 2 contains the descriptive characteristics of participants, stratified by those who completed (n=20) and those who discontinued/withdrew (n=3). Of the 20 participants who completed the study, 6 (30%) were male and 14 (70%) were female. The duration of MS varied from one to 45 years with the onset of LUTSs varied from one to 25 years. The most common type of MS was relapsing remitting (RRMS) (n=12, 60%). All participants reported their urinary symptoms as a combination of symptoms (n=20, 100%) whereas storage symptoms were reported in seven cases (35%). The most frequently reported symptom was urgency (n=16, 80%) followed by frequency (n=13, 65%) and nocturia (n=12, 60%).
Table 2.
Participant’s demographic characteristics (n=23)
| Category | Variable | Participants completed the study (20): n (%) | Participants lost to follow (3): n (%) |
|---|---|---|---|
| Gender | Female | 14 (70%) | 2 (66.67%) |
| Male | 6 (30%) | 1 (33.33%) | |
| Age | 18–24 | - | - |
| 25–34 | - | - | |
| 35–44 | 6 (30%) | 2 (66.67%) | |
| 45–54 | 6 (30%) | 1 (33.33%) | |
| 55–64 | 6 (30%) | - | |
| 65–74 | 1 (5%) | - | |
| 75–84 | - | - | |
| 85 or older | 1 (5%) | - | |
| Marital status | Single | 2 (10%) | 2 (66.67%) |
| Married | 17 (85%) | 1 (33.33%) | |
| Widowed | - | - | |
| Divorced | 1 (5%) | - | |
| Separated | - | - | |
| MS type | RR MS | 12 (60%) | 2 (66.67%) |
| PP MS | 5 (25%) | 1 (33.33%) | |
| SP MS | 3 (15%) | - | |
| PR MS | - | - | |
| MS diagnosis in years | 1–5 | 2 (10%) | - |
| 6–10 | 8 (40%) | 1 (33.33%) | |
| 11–15 | 3 (15%) | 2 (66.67%) | |
| 16–20 | 3 (15%) | - | |
| 21–25 | 2 (10%) | - | |
| 26–30 | 1 (5%) | - | |
| 31–35 | - | - | |
| 36–40 | - | - | |
| 41–45 | 1 (5%) | - | |
| LUTSs main | Urgency | 16 (80%) | 3 (100%) |
| Frequency | 13 (65%) | 2 (66.67%) | |
| Nocturia | 12 (60%) | 1 (33.33%) | |
| Urge incontinence | 6 (30%) | 1 (33.33%) | |
| Terminal dribbles | 4 (20%) | - | |
| Hesitancy | 5 (25%) | - | |
| Feeling of incomplete bladder emptying | 8 (40%) | 1 (33.33%) | |
| Urinary incontinence | 5 (25%) | 2 (66.67%) | |
| Double void | 4 (20%) | 1 (33.33%) | |
| LUTSs in years | 1–5 | 6 (30%) | 1 (33.33%) |
| 6–10 | 9 (45%) | - | |
| 11–15 | 3 (15%) | 2 (66.67%) | |
| 16–20 | 1 (5%) | - | |
| 21–25 | 1 (5%) | - | |
| Previous TX | None | 4 (20%) | 1 (33.33%) |
| Pharmacologic | 7 (35%) | 1 (33.33%) | |
| Non-pharmacologic: | |||
| Exercises | 3 (15%) | 1 (33.33%) | |
| Nerve stimulation with another treatment (Exercise and/or Catheterization) | 3 (15%) | - | |
| Behavioural | 3 (15%) | - | |
| Current TX | None | 6 (30%) | 2 (66.67%) |
| Pharmacologic | 9 (45%) | 1 (33.33%) | |
| Pharmacologic with Catheterization | 2 (10%) | - | |
| Non-pharmacologic: | |||
| Exercises | 2 (10%) | - | |
| Nerve stimulation | - | - | |
| Behavioural | 1 (5%) | - | |
| Prophylactic | Yes | 3 (15%) | - |
| No | 17 (85%) | 3 (100%) | |
| Comorbidities | None | 8 (40%) | 1 (33.33 %) |
| Thyroid related issues | 2 (10%) | 1 (33.33%) | |
| Hypertension | 1 (5%) | 1 (33.33%) | |
| Reynolds syndrome | 1 (5%) | ||
| Cancer | 1 (5%) | - | |
| Foot drop/mobility | 2 (10%) | - | |
| Migraine | 1 (5%) | 1 (33.33%) | |
| hearing impairment | 1 (5%) | - | |
| Bowel related issues/duodenal ulcer | 3 (15%) | - | |
| PDDS-Mobility | (0) Normal | 3 (15%) | - |
| (1) Mild disability | 1 (5%) | ||
| (2) Moderate disability | 3 (15%) | 1 (33.33%) | |
| (3) Gait disability | 2 (10%) | ||
| (4) Early cane | 3 (15%) | ||
| (5) Late cane | 4 (20%) | 1 (33.33%) | |
| (6) Bilateral support | 3 (15%) | ||
| (7) Wheelchair | 1 (5%) | 1 (33.33%) | |
| (8) Bedridden | - | ||
MS multiple sclerosis, RR relapsing–remitting, SP secondary progressive, PP primary progressive, PR progressive relapsing, LUTSs lower urinary tract symptoms, PDDS Patient Determined Disease Step
Adverse events
There were no reported stimulation-related adverse events in the participants during the study intervention phase. Two (10%) participants reported skin reactions in the site of the stimulation with (n=1) redness after first stimulation session and (n=1) dry skin at the stimulation site that cleared up after 8 days. This did not impact treatment adherence.
Adherence to the treatment protocol
The adherence to the 18 sessions among 20 participants was 100%.
Acceptability of TTNS application
The responses to the participant satisfaction questionnaire (Likert scale) are shown in Table 3. The median score was 5 points (IQR=0.25 points) regarding the ease of use of the device, indicating that participants strongly agreed that the device was easy to use. Median scores of 5 points were also recorded for acceptability of the frequency, duration, and timing of the intervention. Overall, participants were very satisfied with the intervention (median score=5 points, IQR=0 points).
Table 3.
Acceptability (satisfaction) survey (n=20)
| Questions | Median score (IQR) |
|---|---|
| Q1. Please, tick the appropriate box that indicates your satisfaction with nerve stimulation - The device is easy to use. | 5 (0.25) |
| Q2. Please, tick the appropriate box that indicates your satisfaction with nerve stimulation - The device is comfortable to use. | 4.5 (1) |
| Q3. Please, tick the appropriate box that indicates your satisfaction with nerve stimulation - application of tibial nerve stimulation at home was acceptable. | 5 (1) |
| Q4. Please, tick the appropriate box that indicates your satisfaction with nerve stimulation - Using the tibial nerve stimulation for 30 mins 3 times/ week is acceptable. | 5 (0.25) |
| Q5. Please, tick the appropriate box that indicates your satisfaction with nerve stimulation - Using the tibial nerve stimulation for 6 weeks is acceptable. | 5 (1) |
| Q6. Please, tick the appropriate box that indicates your satisfaction with nerve stimulation - Overall, I am satisfied with the device. | 5 (0) |
5-point Likert scale employed across questions (score of 1= “strongly disagree”; 2= “disagree”; 3= “neutral”; 4= “agree”; 5= “strongly agree
Secondary outcome measures
Changes in bladder storage symptoms reported using 3-day bladder diary and PPIUS
Table 4 displays the baseline and post-intervention score across all outcome measures. Daily average urination, urinary frequency in 24 h, changed from a daily median of 10 times (SD=3) to 8 times (SD=3). Median daily urinary urgency changed from 6 times (IQR=5.8) at baseline to 2 times daily (IQR=4) post-intervention. No changes were observed in the daily mean episodes of nocturia (mean=1 episode, SD=1).
Table 4.
Scores of the outcome measures (n=20)
| Baseline | Post-intervention (week 6) | |
|---|---|---|
| 3-day bladder diary scores | ||
| Daily average urinary frequency (24 h): mean (SD) | 10 (3) | 8 (3) |
| Daily average urgency: median (IQR) | 6 (5.8) | 2 (4) |
| Daily average urinary incontinence: median (IQR) | 0 (1.3) | 0 (0) |
| Daily average nocturia: mean (SD) | 1 (1) | 1 (1) |
| Daily average fluid intake: mean (SD) | 1585 (604.5) | 1504 (489) |
| Daily average fluid intake: Caffeinated drinks: mean (SD) | 542 (367) | 547 (360) |
| Daily average fluid intake: non-caffeinated drinks: mean (SD) | 1043 (566) | 957 (491) |
| Patient Perception of Intensity of Urgency Scale (PPIUS) | ||
| Daily average total scores PPIUS: median (IQR) | 2 (1) | 2 (1) |
| Daily average severe urgency grade (3): median (IQR) | 3 (4) | 1 (1) |
| Daily average urge urinary incontinence grade (4): median (IQR) | 0 (0.6) | 0 (0) |
| Daily average severe urgency + urge urinary incontinence grade (3+4): median (IQR) | 3 (3.4) | 1 (1) |
| International Consultation on Incontinence Questionnaire Over active bladder (ICIQ-OAB) scores | ||
| Total score ICIQ-OAB: median (IQR) | 8 (2.25) | 4 (2.5) |
| Q1. Frequency: median (IQR) | 1 (2) | 1 (2) |
| Q2. Nocturia: median (IQR) | 2 (2) | 1 (0.5) |
| Q3. Urgency: median (IQR) | 3 (1) | 1 (1) |
| Q4. Urge urinary incontinence: median (IQR) | 2 (1) | 1 (1) |
| Kings Health Questionnaire (KHQ) | ||
| Total score: part-one: mean (SD); median (IQR) | 5.8 (1.2); 6 (1.25) | 5 (1.27)*; 5 (2)* |
| Total score: part-two: mean (SD); median (IQR) | 44.6 (8.9); 43 (10) | 28.4 (8.5); 27.5 (8) |
| Total score: part-three: mean (SD); median (IQR) | 10 (2.7)*; 10 (4.25)* | 7.55 (4)*; 6.5 (5.25)* |
SD standard deviation, IQR interquartile range
*Indicates that data are not normally distributed
The daily median urgency scores (grade 3) assessed by PPIUS changed from 3 points (IQR=4) to 1 point (IQR=1) post-intervention with no changes were reported in daily median urgency urinary incontinence (UUI). Daily average fluid consumption remained stable across both timepoints.
Changes in bladder storage symptoms reported using ICIQ-OAB
The ICIQ-OAB median scores are summarised in Table 4. The overall median (IQR) scores for urinary symptoms as measured by the ICIQ-OAB changed from 8 points (IQR=2.25) at baseline to 4 points (IQR=2.5) post-intervention.
Changes in health-related quality of life scores for urinary symptoms reported by KHQ
The KHQ scores at baseline and post-intervention are summarised in Table 4. No changes in mean/median total scores were reported in the KHQ-Part- one. The median and mean scores of part-two changed from 43 points (IQR=10) and 44.6 points (SD= 8.9) at baseline to 27.5 points (IQR=8) and 28.4 points (SD=8.5) at the end of week 6, respectively. Part-three showed changes from 10 points (IQR=4.25) and 10 points (SD=2.7) at baseline to 6.5 points (IQR=5.25) and 7.55 (SD=4) post-intervention, respectively.
Discussion
This study demonstrates the feasibility and acceptability of TTNS for bladder storage symptoms in PwMS using an accessible and affordable TENS unit. Our key progression criteria to continue to a pilot randomised controlled trial were achieved. Participants reported high levels of satisfaction with the study protocol and high adherence was reported for completion of the 6 weeks intervention with no serious adverse events reported in the current study.
Adherence to the intervention was high and may have been influenced by weekly follow-up calls. A meta-analysis of 127 included studies showed that the odds of patients’ treatment adherence are 2.16 times higher with effective communication and regular monitoring between healthcare providers and patients [36]. TTNS in the current study showed high level of adherence (100%) compared to a low level of adherence to pelvic floor muscle exercise (PFME) (20%) among women with urinary incontinence [37]. Previous studies showed that healthcare providers estimated that 64% of patients adhere to PFMT in short term, but 23% in long term [38] with limited data in literature on the adherence rate of non-pharmacologic management strategies of urinary symptoms among PwMS. The acceptability of home-based TTNS is supported by a previous study where it was more acceptable than home-based PFME [39]. TTNS is a non-invasive technique that makes home-based treatment accessible compared to PTNS which needs clinic visit for each treatment session [40]. Also, the application of TTNS does not need frequent follow-up from clinicians compared to other interventions including PFME. Studies showed the effectiveness of the PFME depends on regular monitoring provided by frequent assessment of PFM function and contractility which required patients to attend clinic for an individualised training program to achieve optimal outcomes [41]. Furthermore, safety measures of TTNS reported in the current study is in line with previous studies among people with non-neurogenic [42] and neurogenic OAB [14, 43, 44].
We did not seek to examine if participants experienced significant changes in urinary symptoms and quality of life from baseline to post-intervention due to our primary focus on exploring feasibility. However, changes in scores of urinary symptoms using 3-day bladder suggest improvements of urinary frequency and urgency episodes post-intervention of TTNS. In line with our findings, one study [23] found that TTNS at 10Hz, 200ms for 30 min, twice weekly was effective in reducing the urinary frequency and urgency episodes using 3-day bladder diary among post-stroke at the end of 6 weeks of intervention [23]. Specific to PwMS, one study was identified [21] using a 3-day bladder diary which showed that 20 min of daily TTNS for 12 weeks reduced urinary frequency by 2.7 voids after 4 weeks and 2.4 voids after 12 weeks. In the current study, we noticed similar improvements in the reduction of urinary frequency episodes of 2 voids post 6 weeks of intervention. However, the main weakness of our study is the lack of a comparison group due to the nature of the feasibility study.
The current study findings demonstrated a positive trend in reducing the urgency severity symptom scores using PPIUS and reducing urgency episodes, and nocturia using ICIQ with a reduction in scores of QoL measures detected by KHQ indicating improvements of urinary symptoms post TTNS. Similar to current study findings, a reduction in urinary urgency scores following TTNS has been shown among 75 non-neurogenic OAB participants [45], and among a mixed population of 48 neurogenic and non-neurogenic OABs including PwMS [46]. However, the latter study needs to be interpreted with caution because the authors did not provide a separate analysis for MS participants. A minimal clinically important difference (MCID) has been noticed for KHQ as a change of score of ≥3 points in the symptom severity domain and ≥ 5 points in the other domains of the questionnaire [47], suggesting a clinically meaningful change in QoL in our participants. However, direct comparison between our study findings with existing literature is difficult due to the lack of a standardised treatment protocol including a total number of sessions per week, the duration of treatment, and the parameters for stimulation [40, 42, 48, 49] and inconsistency of outcome measures to assess the urinary symptoms in literature. Furthermore, the current study includes participants with any type of MS and the impact of TTNS on urinary symptoms and QoL measures should be interpreted in the context of this heterogeneous group. The use of a randomisation schedule and allocation concealment in future studies should address both known confounding such as MS type, gender etc and unknown confounding.
Remaining uncertainty that needs to be addressed in the randomised pilot trial is as follows:
Inclusion of long-term follow-up of the intervention (12 months)
Include sham-arm to investigate the effectiveness of TTNS on NLUTD in MS
Provision of a face-to-face option rather than online only to widen the recruitment and support MS participants who do not have access to the internet.
Implications
TTNS is feasible, acceptable, and safe in clinical practice with PwMS and bladder storage symptoms
Rates of recruitment and retention to this feasibility study were acceptable
Future Pilot RCT are warranted to assess the effectiveness of TTNS in PwMS and bladder storage symptoms
Conclusions
The current study demonstrates that TTNS is feasible, safe, and acceptable to PwMS. Changes of urinary symptoms scores between baseline and post-intervention suggested improvements in bladder storage symptoms and QoL measures. These findings serve as a preliminary step to inform the development of an evidence-based future pilot randomised controlled trial (RCT) using standardised reporting of outcome measures. We recommend following the treatment protocol, the electrical stimulation parameters, and the outcome measures applied in the current feasibility study for the implementation plan of the future pilot RCT.
Supplementary Information
Additional file 1. CONSORT 2010 checklist of information to include when reporting a pilot or feasibility trial*.
Acknowledgements
The authors would like to express their special thanks and appreciation to the participants for their contribution, time, and support and to MS Ireland gatekeepers for their help during the recruitment phase. We also extend our special thanks to Mr. Mohammed Al Rashid for his support in Excel software.
Abbreviations
- NLUTD
Neurogenic lower urinary tract dysfunction
- PwMS
People with MS
- DO
Detrusor overactivity
- CNS
Central nervous system
- EUA
European Association of Urology
- NICE
UK National Institute for Care and Clinical Excellence
- TNS
Tibial nerve stimulation
- TTNS
Transcutaneous tibial nerve stimulation
- PTNS
Percutaneous tibial nerve stimulation
- TENS
Transcutaneous electrical nerve stimulation
- PDDS
Patient Determined Disease Steps
- ICIQ-OAB
International Consultation of Incontinence Questionnaire- Overactive Bladder
- PPIUS
Patient Perception of Intensity of Urgency Scale
- QoL
Quality of life
- KHQ
King’s Health Questionnaire
- SD
Standard deviations
- IQR
Interquartile ranges
- RRMS
Relapsing remitting
- PFME
Pelvic floor muscle exercise
- RCT
Randomised controlled trial
Authors’ contributions
Al Dandan HB: conceptualization, data collection, data analysis, writing – draft preparation, review and editing; Galvin R: Conceptualization, data analysis, writing – review and editing, final approval; Robinson K: writing – review and editing, data collection - posting TENS units to all participants; McClurg D: conceptualization, writing – review and editing; Coote S: conceptualization, writing – review and editing, final approval. The authors read and approved the final manuscript.
Funding
Hawra B. Al Dandan is a PhD student funded by an unrestricted fellowship from Imam Abdulrahman Bin Faisal University, Dammam, K.S.A [IRUD1702].
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article (and its additional file)
Declarations
Ethics approval and consent to participate
Ethics approval was granted from the Faculty of Education and Health Sciences Research Ethics Committee at the University of Limerick [2020_06_07_ EHS]. All participants provided informed written consent via Qualtrics Survey Software.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gajewski JB, Schurch B, Hamid R, Averbeck M, Sakakibara R, Agrò EF, et al. An International Continence Society (ICS) report on the terminology for adult neurogenic lower urinary tract dysfunction (ANLUTD) Neurourol Urodyn. 2018;37(3):1152–1161. doi: 10.1002/nau.23397. [DOI] [PubMed] [Google Scholar]
- 2.Patel DP, Elliott SP, Stoffel JT, Brant WO, Hotaling JM, Myers JB. Patient reported outcomes measures in neurogenic bladder and bowel: A systematic review of the current literature. Neurourol Urodyn. 2016;35(1):8–14. doi: 10.1002/nau.22673. [DOI] [PubMed] [Google Scholar]
- 3.Peter TD, Peter MM. Neurogenic Bladder. Adv Urol. 2012;2012:2012. [Google Scholar]
- 4.Panicker JN, Fowler CJ, Kessler TM. Lower urinary tract dysfunction in the neurological patient: clinical assessment and management. Lancet Neurol. 2015;14(7):720–732. doi: 10.1016/S1474-4422(15)00070-8. [DOI] [PubMed] [Google Scholar]
- 5.Al Dandan HB, Coote S, McClurg D. Prevalence of Lower Urinary Tract Symptoms in People with Multiple Sclerosis: A Systematic Review and Meta-analysis. Int J MS Care. 2020;22(2):91–99. doi: 10.7224/1537-2073.2019-030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Benedetto P, Delneri C, Biasutti E, Bragadin LM, Giorgini T. Vesicourethral dysfunction in multiple sclerosis. Initial assessment based on lower urinary tract symptoms and their pathophysiology. Neurol Sci. 2008;29(4):348–351. doi: 10.1007/s10072-008-1041-z. [DOI] [PubMed] [Google Scholar]
- 7.Nortvedt MW, Riise T, Myhr KM, Landtblom AM, Bakke A, Nyland HI. Reduced quality of life among multiple sclerosis patients with sexual disturbance and bladder dysfunction. Mult Scler. 2001;7(4):231–235. doi: 10.1177/135245850100700404. [DOI] [PubMed] [Google Scholar]
- 8.Khan F, Pallant JF, Shea TL, Whishaw M. Multiple sclerosis: prevalence and factors impacting bladder and bowel function in an Australian community cohort. Disabil Rehabil. 2009;31(19):1567–1576. doi: 10.1080/09638280802639566. [DOI] [PubMed] [Google Scholar]
- 9.Vitkova M, Rosenberger J, Krokavcova M, Szilasiova J, Gdovinova Z, Groothoff JW, et al. Health-related quality of life in multiple sclerosis patients with bladder, bowel and sexual dysfunction. Disabil Rehabil. 2014;36(12):987–992. doi: 10.3109/09638288.2013.825332. [DOI] [PubMed] [Google Scholar]
- 10.Browne C, Salmon N, Kehoe M. Bladder dysfunction and quality of life for people with multiple sclerosis. Disabil Rehabil. 2015;37(25):2350–2358. doi: 10.3109/09638288.2015.1027007. [DOI] [PubMed] [Google Scholar]
- 11.Spencer N. Urinary incontinence and unemployment in people with multiple sclerosis. Int J MS Care. 2007;9(4):143–147. doi: 10.7224/1537-2073-9.4.143. [DOI] [Google Scholar]
- 12.Al Dandan HB, Galvin R, McClurg D, Coote S, Robinson K. Management strategies for neurogenic lower urinary tract dysfunction: a qualitative study of the experiences of people with multiple sclerosis and healthcare professionals. Disabil Rehabil. 2021;1–11. [DOI] [PubMed]
- 13.Jezernik S, Craggs M, Grill WM, Creasey G, Rijkhoff NJ. Electrical stimulation for the treatment of bladder dysfunction: current status and future possibilities. Neurol Res. 2002;24(5):413–430. doi: 10.1179/016164102101200294. [DOI] [PubMed] [Google Scholar]
- 14.Zecca C, Panicari L, Disanto G, Maino P, Singh A, Digesu GA, et al. Posterior tibial nerve stimulation in the management of lower urinary tract symptoms in patients with multiple sclerosis. Int Urogynecol J. 2016;27(4):521–527. doi: 10.1007/s00192-015-2814-6. [DOI] [PubMed] [Google Scholar]
- 15.Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016;2:64. doi: 10.1186/s40814-016-0105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al Dandan HB, Galvin R, Robinson K, McClurg D, Coote S. Transcutaneous tibial nerve stimulation for the treatment of bladder storage symptoms in people with multiple sclerosis: protocol of a single-arm feasibility study. HRB Open Res. 2020;3. [DOI] [PMC free article] [PubMed]
- 17.Rizzo MA, Hadjimichael OC, Preiningerova J, Vollmer TL. Prevalence and treatment of spasticity reported by multiple sclerosis patients. Mult Scler. 2004;10(5):589–595. doi: 10.1191/1352458504ms1085oa. [DOI] [PubMed] [Google Scholar]
- 18.Robertson V, Ward A, Low J, Reed A, & MCSP D. Electrotherapy explained: principles and practice. Elsevier Health Sciences. 2006.
- 19.Groen J, Bosch JL. Neuromodulation techniques in the treatment of the overactive bladder. BJU Int. 2001;87(8):723–731. doi: 10.1046/j.1464-410x.2001.02219.x. [DOI] [PubMed] [Google Scholar]
- 20.Castel-Lacanal E. Sites of electrical stimulation used in neurology. Ann Phys Rehabil Med. 2015;58(4):201–207. doi: 10.1016/j.rehab.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 21.de Seze M, Raibaut P, Gallien P, Even-Schneider A, Denys P, Bonniaud V, et al. Transcutaneous posterior tibial nerve stimulation for treatment of the overactive bladder syndrome in multiple sclerosis: results of a multicenter prospective study. Neurourol Urodyn. 2011;30(3):306–311. doi: 10.1002/nau.20958. [DOI] [PubMed] [Google Scholar]
- 22.Vargas Luna JL, Krenn M, Mayr W, Cortes Ramirez JA. Optimization of Interphase Intervals to Enhance the Evoked Muscular Responses of Transcutaneous Neuromuscular Electrical Stimulation. Artif Organs. 2017;41(12):1145–1152. doi: 10.1111/aor.12921. [DOI] [PubMed] [Google Scholar]
- 23.Monteiro ÉS, de Carvalho LBC, Fukujima MM, Lora MI, Do Prado GF. Electrical Stimulation of the Posterior Tibialis Nerve Improves Symptoms of Poststroke Neurogenic Overactive Bladder in Men: A Randomized Controlled Trial. Urology. 2014;84(3):509–514. doi: 10.1016/j.urology.2014.05.031. [DOI] [PubMed] [Google Scholar]
- 24.Anghel LA, Farcas AM, Oprean RN. An overview of the common methods used to measure treatment adherence. Med Pharmacy Rep. 2019;92(2):117. doi: 10.15386/mpr-1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zappavigna C, Carr LK. Validated Questionnaires for the Evaluation of Urinary Incontinence—Which, When and Why? Curr Bladder Dysfunction Rep. 2015;10(2):138–142. doi: 10.1007/s11884-015-0290-y. [DOI] [Google Scholar]
- 26.Abrams P, Andersson K-E, Apostolidis A, Birder L, Bliss D, Brubaker L, et al. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol Urodyn. 2018;37(7):2271–2272. doi: 10.1002/nau.23551. [DOI] [PubMed] [Google Scholar]
- 27.Abrams P, Avery K, Gardener N, Donovan J, Board IA. The international consultation on incontinence modular questionnaire: www. iciq. net. J Urol. 2006;175(3):1063–1066. doi: 10.1016/S0022-5347(05)00348-4. [DOI] [PubMed] [Google Scholar]
- 28.Nambiar A, Lucas M. Chapter 4: Guidelines for the diagnosis and treatment of overactive bladder (OAB) and neurogenic detrusor overactivity (NDO) Neurourol Urodyn. 2014;33(Suppl 3):S21–S25. doi: 10.1002/nau.22631. [DOI] [PubMed] [Google Scholar]
- 29.Jimenez-Cidre MA, Lopez-Fando L, Esteban-Fuertes M, Prieto-Chaparro L, Llorens-Martinez FJ, Salinas-Casado J, et al. The 3-day bladder diary is a feasible, reliable and valid tool to evaluate the lower urinary tract symptoms in women. Neurourol Urodyn. 2015;34(2):128–132. doi: 10.1002/nau.22530. [DOI] [PubMed] [Google Scholar]
- 30.Notte SM, Marshall TS, Lee M, Hakimi Z, Odeyemi I, Chen W-H, et al. Content validity and test-retest reliability of Patient Perception of Intensity of Urgency Scale (PPIUS) for overactive bladder. BMC Urol. 2012;12(1):26. doi: 10.1186/1471-2490-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pat Ray R, Andreas MP, Gary JO, Con JK. Multinational Study of Reliability and Validity of the King's Health Questionnaire in Patients with Overactive Bladder. Qual Life Res. 2003;12(4):427–442. doi: 10.1023/A:1023422208910. [DOI] [PubMed] [Google Scholar]
- 32.Okamura K, Nojiri Y, Osuga Y. Reliability and validity of the Kings Health Questionnaire for lower urinary tract symptoms in both genders. BJU Int. 2009;103(12):1673–1678. doi: 10.1111/j.1464-410X.2008.08335.x. [DOI] [PubMed] [Google Scholar]
- 33.Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10(1):1–10. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hebbar S, Pandey H, Chawla A. Understanding King’s Health Questionnaire (KHQ) in assessment of female urinary incontinence. Int J Res Med Sci. 2015;3(3):531–538. doi: 10.5455/2320-6012.ijrms20150301. [DOI] [Google Scholar]
- 35.Lewis M, Bromley K, Sutton CJ, McCray G, Myers HL, Lancaster GA. Determining sample size for progression criteria for pragmatic pilot RCTs: the hypothesis test strikes back! Pilot Feasibility Stud. 2021;7(1):1–14. doi: 10.1186/s40814-021-00770-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zolnierek KBH, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Venegas M, Carrasco B, Casas-Cordero R. Factors influencing long-term adherence to pelvic floor exercises in women with urinary incontinence. Neurourol Urodyn. 2018;37(3):1120–1127. doi: 10.1002/nau.23432. [DOI] [PubMed] [Google Scholar]
- 38.Dumoulin C, Hay-Smith J, Frawley H, McClurg D, Alewijnse D, Bo K, et al. 2014 consensus statement on improving pelvic floor muscle training adherence: International Continence Society 2011 State-of-the-Science Seminar. Neurourol Urodyn. 2015;34(7):600–605. doi: 10.1002/nau.22796. [DOI] [PubMed] [Google Scholar]
- 39.Sacomori C, Zomkowski K, Dos Passos PI, Cardoso FL, Sperandio FF. Adherence and effectiveness of a single instruction of pelvic floor exercises: a randomized clinical trial. Int Urogynecol J. 2020;31(5):951–959. doi: 10.1007/s00192-019-04032-6. [DOI] [PubMed] [Google Scholar]
- 40.Tudor KI, Seth JH, Liechti MD, Ochulor J, Gonzales G, Haslam C, et al. Outcomes following percutaneous tibial nerve stimulation (PTNS) treatment for neurogenic and idiopathic overactive bladder. Clin Auto Res. 2020;30(1):61–7. [DOI] [PubMed]
- 41.Abrams P, Cardozo L, Wagg A, Wein A. Incontinence 6th edition ICI-ICS. Bristol: International Continence Society edn; 2017. [Google Scholar]
- 42.Booth J, Connelly L, Dickson S, Duncan F, Lawrence M. The effectiveness of transcutaneous tibial nerve stimulation (TTNS) for adults with overactive bladder syndrome: a systematic review. Neurourol Urodyn. 2018;37(2):528–541. doi: 10.1002/nau.23351. [DOI] [PubMed] [Google Scholar]
- 43.Valles-Antuna C, Perez-Haro ML, Gonzalez-Ruiz de LC, Quintas-Blanco A, Tamargo-Diaz EM, Garcia-Rodriguez J, et al. Transcutaneous stimulation of the posterior tibial nerve for treating refractory urge incontinence of idiopathic and neurogenic origin. Actas Urol Esp. 2017;41(7):465–470. doi: 10.1016/j.acuro.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 44.Welk B, McKibbon M. A randomized, controlled trial of transcutaneous tibial nerve stimulation to treat overactive bladder and neurogenic bladder patients. Can Urol Assoc Jl. 2020;14(7):E297. doi: 10.5489/cuaj.6142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Souto SC, Reis LO, Palma T, Palma P, Denardi F. Prospective and randomized comparison of electrical stimulation of the posterior tibial nerve versus oxybutynin versus their combination for treatment of women with overactive bladder syndrome. World J Urol. 2014;32(1):179–184. doi: 10.1007/s00345-013-1112-5. [DOI] [PubMed] [Google Scholar]
- 46.Seth JH, Gonzales G, Haslam C, Pakzad M, Vashisht A, Sahai A, et al. Feasibility of using a novel non-invasive ambulatory tibial nerve stimulation device for the home-based treatment of overactive bladder symptoms. Transl Androl Urol. 2018;7(6):912. doi: 10.21037/tau.2018.09.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kelleher CJ, Pleil AM, Reese PR, Burgess SM, Brodish PH. How much is enough and who says so? The case of the King's Health Questionnaire and overactive bladder. BJOG Int J Obstet Gynaecol. 2004;111(6):605–612. doi: 10.1111/j.1471-0528.2004.00129.x. [DOI] [PubMed] [Google Scholar]
- 48.Burton C, Sajja A, Latthe PM. Effectiveness of percutaneous posterior tibial nerve stimulation for overactive bladder: A systematic review and meta-analysis. Neurourol Urodyn. 2012;31(8):1206–1216. doi: 10.1002/nau.22251. [DOI] [PubMed] [Google Scholar]
- 49.Schneider MP, Gross T, Bachmann LM, Blok BF, Castro-Diaz D, Del Popolo G, et al. Tibial Nerve Stimulation for Treating Neurogenic Lower Urinary Tract Dysfunction: A Systematic Review. Eur Urol. 2015;68(5):859–867. doi: 10.1016/j.eururo.2015.07.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. CONSORT 2010 checklist of information to include when reporting a pilot or feasibility trial*.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article (and its additional file)