Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic period is experiencing better asthma control, fewer exacerbations, and health care utilization, with limited data on factors that could explain this phenomenon.
Objective
To confirm these improved asthma outcomes during COVID-19 and evaluate potential contributing factors.
Methods
In 18,912 pediatric patients with asthma treated in the Children's Hospital of Orange County network from 2017 to 2020, monthly asthma-related encounters and medication summaries were extracted from electronic health records, particulate matter 2.5 (PM2.5) air pollution from the California Air Resources Board, and influenza-like illness from Illness Surveillance Network for the first 6 months of each year. Changes in outcomes between January to March and April to June (post–COVID-19 shutdown in 2020) were compared with historical data using generalized estimating equations analyses for patient outcomes and generalized linear models for pollution exceedance, influenza-positive, and telehealth visit rates.
Results
During COVID-19, we found 78%, 90%, 68% reductions in hospitalization, emergency department visits, and exacerbations, respectively, compared with pre–COVID-19 2020, with significantly greater changes than the same time period of 2017 to 2019 and significant reductions in albuterol and inhaled corticosteroid use (P < .05). Emergency department visit reduction was not seen for African Americans. The PM2.5 and influenza rates were also significantly reduced during COVID-19 (P < .05). Increased rates in telehealth visits were greater in the publicly insured group when compared with commercially insured.
Conclusion
Our data confirm reduced health care utilization and suggest better asthma control during COVID-19, except for African Americans. This was associated with a significant increase in telehealth visits and reductions in PM2.5 and influenza infections, but not better asthma controller adherence.
Introduction
According to the World Health Organization (WHO), the pandemic of coronavirus disease 2019 (COVID-19) caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has posed a serious threat to global health since December 2019. As of February 26, 2021, the COVID-19 pandemic has resulted in 28,212,548 cases and 506,834 deaths in the United States and increasing daily.1 There has since been interest in understanding the impact of COVID-19 on patients with many chronic conditions including asthma.
Asthma affects more than 6 million children under the age of 18, making it the most common pediatric diagnosis in the United States.2 It has been well known, for many decades, that respiratory infections trigger asthma exacerbations.3 In fact, more than 80% of asthma exacerbations have been attributed to viral illness in school-age children, mostly caused by human rhinovirus (HRV), followed by seasonal coronaviruses and influenza A and B.4 Increased morbidity in children with asthma was noted during the 2009 H1N1 influenza pandemic.5
It was anticipated that patients with asthma would experience increased asthma-associated morbidity because of the respiratory virus SARS-CoV-2 infection, based on experience with other respiratory viral infections.3, 4, 5 Unexpectedly, children with asthma have not contracted SARS-CoV-2 at higher rates than children without asthma, nor have children with asthma experienced more asthma exacerbations during the current pandemic, even in those who have been presumptively infected with SARS-CoV-2.6 , 7 Studies suggest a protective effect owing to the reduced number of SARS-CoV-2 spike protein receptors on respiratory epithelial cell membranes in those highly allergic or on inhaled corticosteroids (ICS).8, 9, 10
The clinical effect of the COVID-19 pandemic on children with asthma has been investigated in several epidemiologic studies.6 , 11, 12, 13, 14 In summary, they have noted a dramatic reduction in asthma morbidity associated with school closures in mid-March 2020, compared with previous years.6 , 11, 12, 13, 14 This has been illustrated by better asthma control,6 fewer exacerbations requiring oral corticosteroids (OCS)14 and decreased emergency department (ED) visits,11, 12, 13, 14 and hospitalizations.11 , 14 The proposed explanations for this observation include spending more time at home, school closures, reduced rates of viral upper respiratory infections including HRV,14 reduced air pollution,14 better asthma medication adherence,6 and better access to medical care by means of video--telemedicine (TM).14 Improvements in asthma outcomes during the COVID-19 pandemic have been less prominent or absent in African American children or those with publicly-funded health care,14 though there are conflicting studies in these demographics.12 There has also been an overall decrease in in-person health care utilization for non–asthma-related diagnosis, suggesting a widespread fear of acquiring COVID-19 in the clinic, ED, or hospital.12 , 13
The COVID-19 epidemiologic studies presented in Table 1 have varied in their assessment of asthma status and exploration of several key factors, which could provide insight into the clinical impact of COVID-19 on a child with asthma.6 , 11, 12, 13, 14 Poorly studied factors include demographics, geography, medication adherence, rate of viral infections, and air pollution.6 , 11, 12, 13
Table 1.
Characterization of Epidemiologic Studies Evaluating Asthma During Coronavirus Disease 19
| Name | Location | Sample size | Demographics | Asthma control measured | OCS | ED visits | IP visits | Adherence measured | Key viral infections reported pre/post-2020 | Air pollution pre/post 2020 | Observation time pre/post (d) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Taquechel et al,14 2020 | Philadelphia | 13,640 | Sex, birth year, race or ethnicity, insurance | ND | Decreased | Decreased | Decreased | ND | Human rhinovirus decreased | PM2.5, PM10, NO2, Ozone, none decreased | 60/60 2020 vs 2015-2019 |
| Kenyon et al,13 2020 | Philadelphia, Pennsylvania | 6000 | ND | ND | ND | Decreased | Decreased | ND | ND | ND | 120 2020 vs 2016-2019 |
| Oreskovic et al,11 2020 | Boston, Massachusetts | ND | ND | ND | ND | Decreased | ND | ND | ND | ND | 120 2020 vs 2019 |
| Simoneau et al,12 2020 | Boston, Massachusetts | 2543 | Age, race or ethnicity, insurance | ND | ND | Decreased | No change | ND | ND | ND | 62/60 2020 vs 2018-2019 |
| Papadopoulos et al,6 2020 | International | 133,000 | ND | ACT or ACQ | ND | ND | ND | Self-reported by survey | ND | ND | Survey reflects events before April 1, 2020 |
| Guijon et al—current study | Orange County, California | 18,912 | Sex, age (birth year), race or ethnicity, insurance | ACT, Albuterol useage ≥3/mo | Decreased | Decreased | Decreased | Established by ICS prescriptions | Influenza decreased | PM2.5, decreased | 90/90 2020 vs 2017-2019 |
Abbreviations: ACT, asthma control test; ACQ, asthma control questionnaire; COVID-19, coronavirus disease 19; ED, emergency department; ICS, inhaled corticosteroid; IP, inpatient; ND, not done or not reported; NO2, nitric dioxide; PM2.5, particulate matter with diameter less than 2.5 μm; PM10, particulate matter with diameter less than 10 μm.
The purpose of this study is to comprehensively characterize the effect of COVID-19, as presented in Table 1, on asthma status in Orange County, California, by assessing asthma control using standardized metrics, severe asthma exacerbations defined by treatment with OCS, and health care utilization. In addition, this study seeks to establish the role of demographics in our predominantly Hispanic neighborhoods, influenza viral infections, and air pollution by particulate matter 2.5 (PM2.5) for the time periods of January 1 to June 30, 2020 compared with comparable periods between 2017 and 2019.
Methods
Study Population
Data for the study were retrieved from the Population Health Enterprise Data Warehouse of the Children's Hospital of Orange County (CHOC) health system in California that comprises both electronic medical records and Medicaid claims data. The CHOC health system is a regional pediatric healthcare network that includes a central and secondary hospital, in addition to a number of primary and specialty care clinics, and more than 100 additional programs and services such as Allergy & Immunology, Pharmacy, and Emergency Medicine. All patients with a diagnosis for asthma based on the International Classification of Diseases, Tenth Revision, Clinical Modification codes were identified in addition to the date of the first diagnosis. Patients with chronic lung diseases were excluded. Hospital and ED encounters of patients, after the first diagnosis of asthma, were selected between 2017 and 2020. Encounters of patients older than 18 were excluded from the study.
Variable Selection
Health care utilization (hospitalizations and ED visits) and medication use (OCS, ICS, and albuterol prescriptions) were aggregated at the patient level by month and year during the study period. Demographic data on patients such as age at the time of encounter, sex, race, and payer type (public vs commercial) were retrieved and aggregated by year and month of encounter. Patients were assigned a deidentified number before analyses, which was used to link health care utilization, medication prescription, demographic, and diagnosis data. The CHOC institutional review board declared the study exempt from review (with institutional review board number 2008100) because all patient data were deidentified before analyses.
Air Pollution Data
Particulate matter 2.5 daily average data for the Orange County, California area were obtained from the California Air Resources Board data website (https://www.arb.ca.gov/aqmis2/aqdselect.php) for the time periods of January 1 to June 30 for the years 2017 to 2020. Air Quality and Meteorological Information System database is a web-based source for real-time and official (historical) air quality and meteorologic data. The Air Quality and Meteorological Information System database contain the most recent data (measured within the past 2 hours) from more than 200 air quality sites and more than 800 meteorologic sites. Orange County air quality data were collected by the South Coast Air Quality Management District and reported to the California Air Resources Board. The PM2.5 data were obtained from monitoring sites located in Anaheim, La Habra, and Mission Viejo, California, and recorded as the daily maximum 1-hour average at the highest of the 3 sites.
Influenza Data
Data were obtained for the California region from the US Outpatient Influenza-like Illness (ILI) Surveillance Network (ILINet) for the California region for the months of January to June for the years 2017 to 2020. Information on patient visits to health care providers for ILI is collected by ILINet. ILINet consists of outpatient healthcare providers in all 50 states. Each week, approximately 3000 outpatient health care providers around the country report data to the Centers for Disease Control and Prevention on the total number of patients seen for any reason and the number of those patients with ILI. For data reporting purposes, an ILI is defined as those with fever (temperature of 100°F [37.8°C] or greater) or a cough or a sore throat without a known cause other than influenza.
Telehealth Care Utilization Before vs During Coronavirus Telemedicine Visits
The video TM data were obtained from billing data in the electronic health record for the dates January 1, 2020, to June 30, 2020. Video TM data includes all outpatient visits (not specific to asthma) to the CHOC Primary Care Network, not including mental health.
Statistical Analysis
Patient demographic characteristics and year of asthma diagnosis were described by number and percentage with a defining trait. Morbidity and medication prescription rates per 1000 patients per month were assessed across periods of January to March and April to June of each year using generalized estimating equations (GEE) analyses with the specification of Poisson distribution, and within-subject repeat measures were performed. Incidence rate ratios (IRR) and corresponding 95% confidence intervals comparing April to June to January to March of 2020 and concurrent time period comparisons during previous years (2017 to 2019) were derived from the Poisson regression results. GEE analyses were extended to assess differential effects of COVID-19 on ED visits and OCS use rates by demographic characteristics. This was achieved by running a separate model for each demographic and outcome that included the following terms: (1) main effects; (2) each 2-way interaction effect; and (3) a 3-way interaction effect between year (2020 vs 2017 to 2019), month (January-March vs April-June), and the respective demographic characteristic (eg, sex). Generalized linear models (GLM) analyses assessed days per month daily PM2.5 (µg/m3) that exceeded the WHO threshold of 10.0 µg/m3 by the specification of count data. Monthly influenza rates per 1000 patients, based on reporting practices within California during the respective time period, were also assessed using GLM analyses. Rate differentials in January to March compared with April to June of 2020 vs 2017 to 2019 were tested for significance by the inclusion of a 2-way interaction effect between the 90-day period and year group in each model. The GLM approach was also used to assess the significance of differential rates between care network groups in TM visits initiated after the stay-at-home orders in March of 2020. A subset analysis was performed in patients who had an asthma control test (ACT) measurement between April and June of 2019 and 2020. The GEE analyses with a specification of binomial distribution were used to compare the odds of patient uncontrolled by ACT survey,15 and OCS prescriptions during April 2020 to June 2020 to outcomes from April 2019 to June 2019. A similar analysis was performed for the administration of 3 or more albuterol canisters per 6-month period,16 in which the period January to June 2020 was compared with January to June 2019. Demographic characteristics of the 166 patients were also evaluated and reported. All analyses were performed using the Statistical Package for the Social Sciences, version 18.0 (IBM SPSS Statistics, IBM Corporation, Armonk, New York).
Results
Demographic Characteristics of Patient Population
There were 18,912 pediatric patients with asthma treated in the CHOC network from 2017 to 2020. Nearly half of these patients were of Hispanic origin (49.7%) as detailed in Table 2 . The average age at first encounter was 9.6 years (SD = 4.6) with 16.9% of patients within 2 to 4 years old, 46.4% 5 to 11 years old, and 36.6% 12 to 18 years of age. Most were boys (57.9%) and 66.3% were on public health insurance. More than two-thirds of patients were diagnosed with asthma before 2017 (76.8%) with the remaining 23.2% diagnosed newly between 2017 and 2020.
Table 2.
Characteristics of Patient Population
| Characteristic | N = 18,912 |
|---|---|
| Age at baseline, mean (SD) | 9.6 y (SD = 4.6) |
| 2-4 y | 16.9% (n = 3204) |
| 5-11 y | 46.4% (n = 8779) |
| ≥12 y | 36.6% (n = 6929) |
| Sex, male | 57.9% (n = 10,951) |
| Race or ethnicity | |
| American Indian or Alaskan Native | 0.1% (n = 13) |
| Asian | 3.3% (n = 616) |
| Black or African American | 1.7% (n = 318) |
| Hispanic | 49.8% (n = 9415) |
| Native Hawaiian or Other Pacific Islander | 0.3% (n = 59) |
| White | 16.9% (n = 3204) |
| Other or unknown | 28.0% (n = 5287) |
| Insurance | |
| Public | 66.3% (n = 12,546) |
| Private | 32.1% (n = 6071) |
| Unknown | 1.6% (n = 295) |
| Asthma diagnosed before January 1sta: | |
| 2017 | 76.8% (n = 14,533) |
| 2018 | 7.9% (n = 1489) |
| 2019 | 11.0% (n = 2087) |
| 2020 | 4.2% (n = 803) |
Patients were included in analyses starting the month/year of asthma diagnosis.
Video/Telehealth Care Utilization Before vs During Coronavirus Disease 2019
Video telehealth was not used preceding the March 2020 stay-at-home orders in the primary care setting. Telehealth visits were documented at CHOC for the 2 primary care groups referred to as CHOC Medical Group (100% publicly funded) and Primacy Care Network (51% publicly-funded). After the stay-at-home order, telehealth visits were initiated in March 2020, increased dramatically in April 2020, and remained well above the initial rate in May and June (telehealth visit rate per 1000 visits across 4 months: 20, 208, 148, 136, respectively). The trend across months differed by primary care group (P < .001). In the 100% publicly-funded CHOC Medical Group (CMG), the telehealth visit rate per 1000 visits started lower than the 51% publicly-funded Primary Care Network (PCN) group in March (11 vs 37, P < .001), then increased to a similar rate in April (201 vs 214, P = .18), and to a significantly higher rate in May (178 vs 123, P < .001) and June (208 vs 89, P < .001). Although CMG and PCN data were not abstracted at the patient level as part of the current study, further investigation of our demographic data revealed public health insurance status was significantly associated with race (P < .001). Public health insurance in our population overall was noted more often in Hispanic, African American, and American Indian/Native Hawaiian patients (91.0%, 82.9%, and 71.4%, respectively) compared with Asian and White patients (49.2% and 53.4%, respectively).
Asthma-Associated Health Care Utilization and Medication use Rates Before vs During Coronavirus Disease 2019
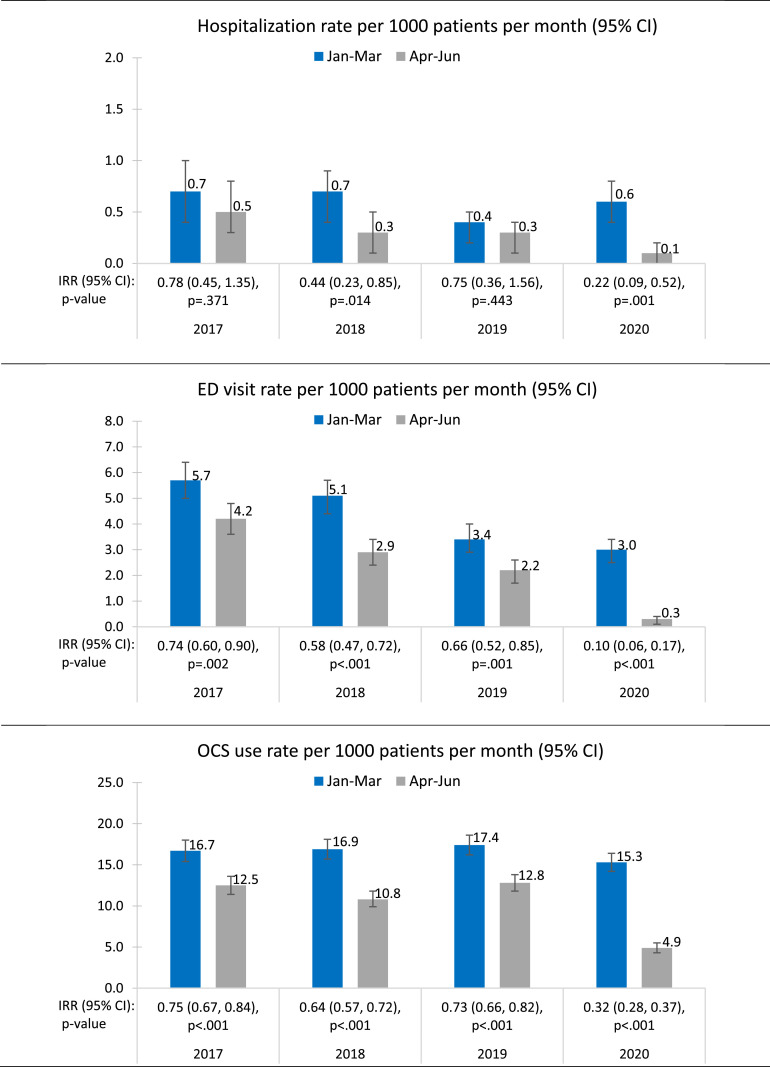
Overall, there was a 78% decrease in the hospitalization rate, a 90% decrease in ED visit rate, and a 68% decrease in OCS use rate per 1000 patients per month at CHOC during the approximately 90-day period that encompassed the COVID-19 shutdown (April-June of 2020) compared with January to March of the same year (P < .05) (Fig 1 ). Asthma-associated morbidity rates were lower in April to June compared with January to March in previous years, but not to the extent observed in 2020 (2-way interaction effect significant in each model, P < .05). The range of decreased morbidity rates comparing April to June with January to March across years 2017 to 2019 before COVID-19 were the following: (1) hospitalization rate decreased from 56% to 22 %, (2) ED visit rate 42% to 26%, and (3) OCS use 36% to 25%.
Figure 1.
Monthly morbidity rates per 1000 patients with asthma. Rates were significantly lower in April to June compared with January to March across years and, to an even greater extent, in 2020 compared with previous years (P < .05). Poisson regression using GEE analyses with the specification of repeat measures. CI, confidence interval; ED, emergency department; GEE, generalized estimating equations; IRR, incidence rate ratios; OCS, oral corticosteroid.
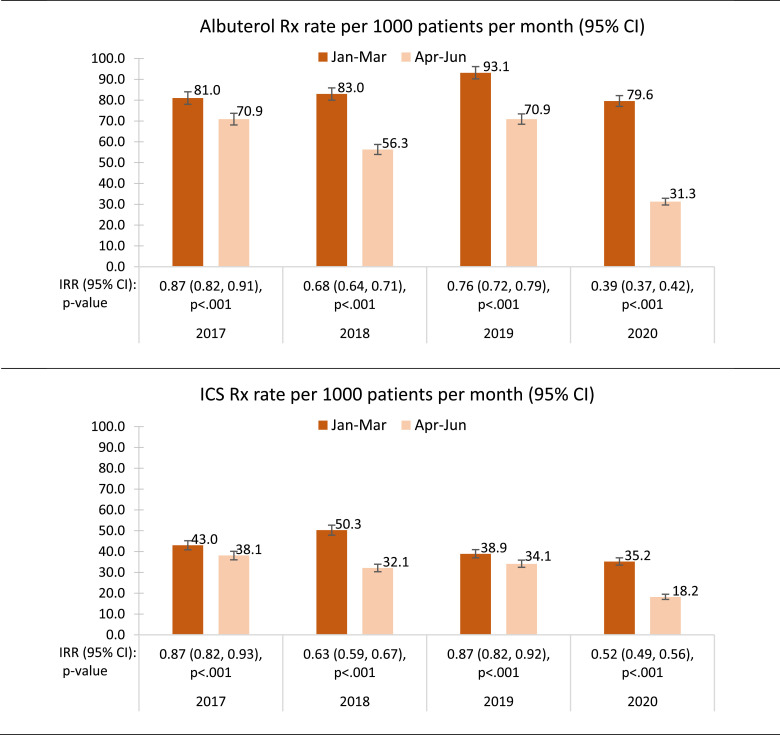
In 2020, a 61% reduction in the albuterol prescription rate per 1000 patients per month occurred in the approximately 90 days after COVID-19 compared with before (IRR, 0.39; 95% confidence interval [CI], 0.37-0.42, P < .05) (Fig 2 ). This reduction was significantly greater than observed in previous years, which ranged from 13% to 32% (2-way interaction effect, P < .05). The pattern was similar for ICS in terms of lower prescription rates in April to June compared with January to March with rate reductions that ranged from 13% to 37% in years before COVID-19, compared with 48% in 2020 (IRR, 0.52; 95% CI 0.49-0.56, P < .05). Interestingly, the 48% drop in ICS prescription rate before vs during COVID-19 in 2020 was less than the 61% drop in the albuterol prescription rate.
Figure 2.
Monthly medication prescription rates per 1000 patients with asthma. Rates were significantly lower in April to June compared with January to March across years and, to an even greater extent, in 2020 compared with previous years (P < .05). Poisson regression using GEE analyses with the specification of repeat measures. CI, confidence interval; ED, emergency department; GEE, generalized estimating equations; IRR, incidence rate ratios; OCS, oral corticosteroid; Rx, prescription.
Demographic Differentials in Asthma-Associated Emergency Department Visit and Oral Corticosteroid Prescription Rates Before vs During Coronavirus Disease 2019
The ED visit rates before COVID-19 were highest in those on public health insurance and in the youngest age group (P < .05) (Table 3 ). Rates also seemed higher in African American children compared with other race groups, although not significant at the .05 level. Reduced ED visit rates in April to June compared with January to March were observed across all demographic characteristics with exception of African American children, who were the only group to exhibit a nonsignificant ED visit rate reduction before vs during COVID-19 in 2020.
Table 3.
Influence of Demographic Characteristics on Monthly Average Emergency Department Visits Per 1000 Patients Comparing January to March and April to June During Years 2017 to 2019 and 2020
| Years 2017-2019 |
Year 2020 |
||||||
|---|---|---|---|---|---|---|---|
| Monthly ED visit rate per 1000 patients | January-March Rate (95% CI) |
April-June Rate (95% CI) |
IRR (95% CI), P value | January-March Rate (95% CI) |
April-June Rate (95% CI) |
IRR (95% CI), P value | Months effect depends on year and demographica P value |
| Overall | 4.4 (4.0-4.8) | 2.9 (2.6-3.3) | 0.67 (0.59-0.76), P < .001 | 3.0 (2.5-3.5) | 0.2 (0.1-0.4) | 0.08 (0.05-0.15), P < .001 | — |
| Age at baseline, y | P = .42 | ||||||
| 2-4 | 8.0 (6.4-9.6) | 7.1 (5.6-8.6) | 0.88 (0.68-1.15), P = .36 | 9.3 (5.9-12.6) | 0.6 (0.0-1.4) | 0.06 (0.02-0.26), P < .001 | |
| 5-11 | 5.4 (4.8-6.0) | 3.1 (2.7-3.6) | 0.56 (0.47-0.67), P < .001 | 3.6 (2.8-4.4) | 0.2 (0.0-0.4) | 0.07 (0.03-0.17), P < .001 | |
| ≥12 | 2.4 (1.9-2.8) | 1.6 (1.2-1.9) | 0.68 (0.52-0.88), P = .003 | 1.6 (1.1-2.1) | 0.2 (0.0-0.4) | 0.18 (0.08-0.41), P < .001 | |
| Sex | P = .69 | ||||||
| Male | 4.8 (4.3-5.4) | 3.4 (3.0-3.9) | 0.69 (0.59-0.80), P < .001 | 3.2 (2.6-3.9) | 0.3 (0.1-0.5) | 0.08 (0.04-0.17), P < .001 | |
| Female | 3.8 (3.2-4.3) | 2.2 (1.8-2.7) | 0.59 (0.47-0.73), P < .001 | 2.6 (1.9-3.3) | 0.2 (0.0-0.4) | 0.10 (0.04-0.22), P < .001 | |
| Race | P = .08 | ||||||
| Black | 8.3 (4.4-12.1) | 4.5 (1.7-7.3) | 0.55 (0.25-1.18), P = .13 | 1.1 (0.0-3.4) | 2.3 (0.0-5.4) | 1.97 (0.18-21.76), P = .58 | |
| Hispanic | 5.6 (5.0-6.1) | 4.0 (3.5-4.5) | 0.72 (0.62-0.83), P < .001 | 4.0 (3.2-4.8) | 0.4 (0.1-0.6) | 0.09 (0.05-0.18), P < .001 | |
| White | 5.1 (4.1-6.1) | 2.5 (1.8-3.2) | 0.49 (0.35-0.69), P < .001 | 3.5 (2.3-4.8) | 0.3 (0.0-0.7) | 0.10 (0.03-0.32), P < .001 | |
| Other or unknown | 2.1 (1.6-2.6) | 1.1 (0.8-1.5) | 0.55 (0.37-0.82), P = .003 | 1.1 (0.6-1.7) | 0.1 (0.0-0.2) | 0.05 (0.01-0.40), P = .004 | |
| Insurance | P = .55 | ||||||
| Public | 5.4 (4.9-5.8) | 3.5 (3.2-3.9) | 0.66 (0.58-0.75), P < .001 | 3.9 (3.2-4.6) | 0.4 (0.2-0.6) | 0.11 (0.06-0.19), P < .001 | |
| Private | 1.8 (1.2-2.3) | 1.1 (0.7-1.6) | 0.33 (0.24-0.46), P < .001 | 1.1 (0.6-1.6) | 0.1 (0.0-0.2) | 0.05 (0.01-0.40), P = .004 | |
Abbreviations: CI, confidence interval; ED, emergency department; GEE, generalized estimating equations; IRR, incidence rate ratio.
Test of 3-way interaction effect (years x months x demographic) in GEE Poisson regression model; years (2017-2019 vs 2020) and months (January-March vs April-June).
The OCS prescription rates per 1000 patients per month exhibited significant differentials in the COVID-19 impact by age and race (3-way interaction effect, P < .05) (Table 4 ). Rate reductions in April to June compared with January to March across the 3 age groups were similar in years before COVID-19, ranging from 26% to 32%. However, in the year of COVID-19, the rate differential before vs during COVID-19 by age was striking, in which an 80% reduction was observed in patients 2 to 4 years old compared with 69% in patients 5 to 11 years and 59% in patients 12 to 18 years (P < .05). Race differentials in OCS requirement also seemed more pronounced in 2020, in which the minority children of African American and Hispanic descents had a larger rate reduction during COVID-19 than White children (77% and 72% compared with 48%, respectively) (P = .002).
Table 4.
Influence of Demographic Characteristics on Monthly Average Oral Corticosteroid Rx Rate Per 1000 Patients Comparing January to March and April to June During Years 2017 to 2019 and 2020
| Monthly OCS Rx rate per 1000 patients | Years 2017-2019 |
Year 2020 |
3-way interaction effecta P value |
||||
|---|---|---|---|---|---|---|---|
| January-March Rate (95% CI) |
April-June Rate (95% CI) |
IRR (95% CI), P value | January-March Rate (95% CI) |
April-June Rate (95% CI) |
IRR (95% CI), P value | ||
| Overall | 17.5 (16.6-18.4) | 12.4 (11.7-13.1) | 0.71 (0.67-0.76), P < .001 | 15.1 (14.0-16.3) | 4.9 (4.2-5.5) | 0.31 (0.27-0.36), P < .001 | — |
| Age at baseline, y | P = .008 | ||||||
| 2-4 | 35.7 (32.4-38.9) | 25.3 (22.6-27.9) | 0.70 (0.60-0.80), P < .001 | 48.6 (41.1-56.1) | 9.2 (6.0-12.4) | 0.20 (0.13-0.30), P < .001 | |
| 5-11 | 18.2 (17.1-19.2) | 12.3 (11.5-13.2) | 0.68 (0.62-0.75), P < .001 | 17.4 (15.6-19.1) | 5.3 (4.3-6.3) | 0.31 (0.25-0.38), P < .001 | |
| ≥12 | 11.1 (10.2-12.0) | 8.4 (7.6-9.1) | 0.74 (0.67-0.84), P < .001 | 9.0 (7.8-10.2) | 3.9 (3.1-4.7) | 0.41 (0.33-0.51), P < .001 | |
| Sex | P = .34 | ||||||
| Male | 18.9 (17.9-19.9) | 13.1 (12.3-13.9) | 0.69 (0.64-0.75), P < .001 | 16.5 (15.1-18.0) | 4.8 (4.1-5.6) | 0.28 (0.24-0.34), P < .001 | |
| Female | 14.3 (13.3-15.3) | 10.5 (9.7-11.4) | 0.74 (0.66-0.82), P < .001 | 13.5 (11.9-15.1) | 4.9 (4.0-5.9) | 0.38 (0.30-0.47), P < .001 | |
| Race | P = .002 | ||||||
| Black | 22.0 (15.8-28.3) | 12.2 (7.6-16.8) | 0.55 (0.35-0.89), P = .01 | 29.9 (18.4-41.4) | 6.8 (1.4-12.2) | 0.23 (0.09-0.55), P = .001 | |
| Hispanic | 18.8 (17.8-19.8) | 13.6 (12.8-14.5) | 0.73 (0.68-0.79), P < .001 | 16.7 (15.1-18.3) | 4.7 (3.9-5.6) | 0.28 (0.23-0.35), P < .001 | |
| White | 22.0 (19.9-24.0) | 14.4 (12.8-16.1) | 0.66 (0.57-0.76), P < .001 | 17.1 (14.3-19.9) | 8.8 (6.9-10.8) | 0.52 (0.39-0.68), P < .001 | |
| Other or unknown | 9.7 (8.6-10.7) | 7.1 (6.2-8.0) | 0.73 (0.62-0.87), P < .001 | 11.3 (9.6-12.9) | 2.9 (2.1-3.8) | 0.27 (0.19-0.37), P < .001 | |
| Insurance | P = .87 | ||||||
| Public | 18.2 (17.4-19.0) | 12.8 (12.1-13.5) | 0.70 (0.66-0.75), P < .001 | 17.6 (16.2-19.1) | 5.5 (4.7-6.3) | 0.31 (0.27-0.37), P < .001 | |
| Private | 12.9 (11.4-14.4) | 9.7 (8.4-11.0) | 0.75 (0.63-0.90), P = .002 | 10.9 (9.3-12.6) | 3.8 (2.8-4.7) | 0.36 (0.27-0.48), P < .001 | |
Abbreviations: CI, confidence interval; GEE, generalized estimating equations; IRR, Incidence rate ratio; OCS, Oral Corticosteroid; Rx, prescription.
Test of 3-way interaction effect (years x months x demographic) in GEE Poisson regression model; years (2017-2019 vs 2020) and months (January-March vs April-June).
Uncontrolled Asthma Before vs During Coronavirus Disease 2019
An ACT survey was completed by 166 patients in the 3-month period of April to June in both 2019 and 2020. In April to June of 2020 (during COVID-19), the odds of uncontrolled disease were reduced by 70% compared with the concurrent period in 2019 from 27.0% to 10.0% (odds ratio, 0.30; 95% CI, 0.16-0.55, P < .05). Corroborating evidence was indicated by the 76% reduced odds of an OCS requirement (odds ratio, 0.24; 95% CI, 0.09-0.66, P < .001), and the 45% reduced odds of 3 or more albuterol prescriptions during the corresponding 6-month period of January to June in 2020 compared with 2019 (P < .05) (Table 5 ).
Table 5.
Uncontrolled Asthma
| N = 166 | 2019 | 2020 | OR (95% CI)a | P value |
|---|---|---|---|---|
| Asthma Uncontrolled | April-June | April-June | ||
| ACT <20 | 27.0% | 10.0% | 0.30 (0.16-0.55) | P < .001 |
| OCS requirement | 11.4% | 3.0% | 0.24 (0.09-0.66) | P < .001 |
| January-June | January-June | |||
| Albuterol Rx ≥3 | 23.5% | 14.5% | 0.55 (0.31-0.97) | P = .04 |
Abbreviations: ACT, asthma control test; CI, confidence interval; GEE, generalized estimating equations; OCS, oral corticosteroid; OR, odds ratio; Rx, prescription.
NOTE: Demographics of 166 patients include the following: (1) sex: 56.0% male; (2) race: 1.2% African American, 6.6% Asian, 58.4% Hispanic, 16.9% White, and 18.1% other or unknown; (3) age at January 1, 2019: 11.4% (2-4 years), 63.9% (5-11 years), 24.7% (≥12 years), and (4) 80.7% public insurance.
GEE analyses using binomial distribution adjusting for repeated measures.
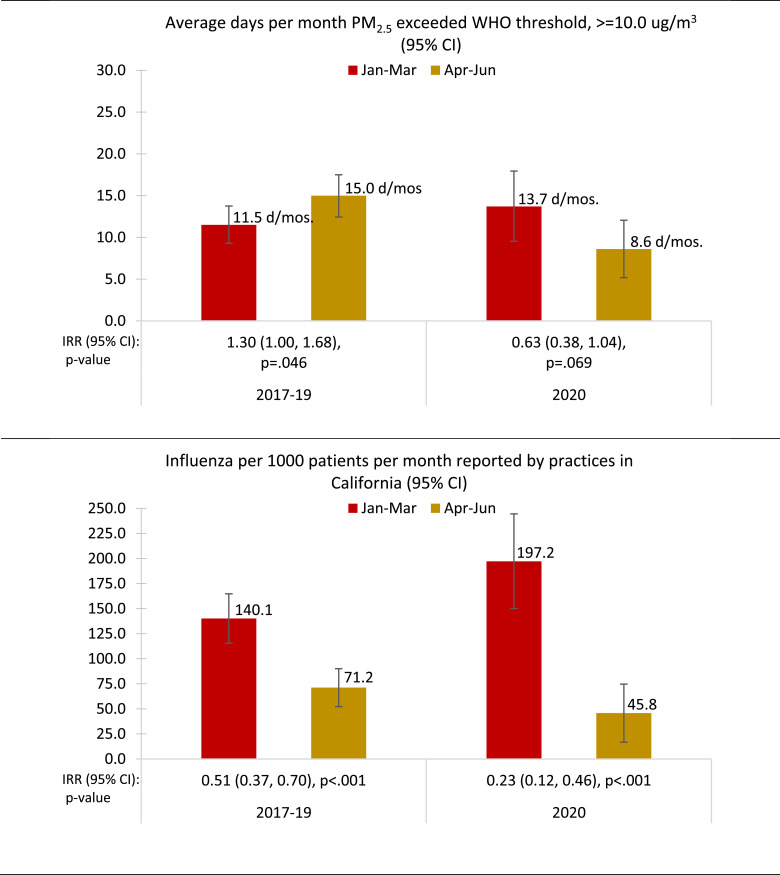
Pollution (Particulate Matter) and Influenza Rates
The average number of days per month that daily average PM2.5 exceeded the WHO standard threshold of 10.0 ug/m3 decreased by 37% between January to March period and April to June in 2020 (13.7 days vs 8.6 days per month) (P = .06). This is in contrast with the significant 30% increase in comparing rates in the concurrent monthly periods during years before COVID-19 (P = .04) (2-way interaction effect between year[s] and month periods, P = .012) (Fig 3 ). The daily average PM2.5 evaluated on a continuous scale correspondingly found significant reduction of 2.41 points between January to March and April to June in 2020 (P = .003) that was not observed in 2017 to 2019 (P = .62) (2020: 10.4 [95% CI, 9.3-11.5] vs 8.0 [95% CI, 6.9-9.2] compared with 2017 to 2019: 10.0 [95% CI, 9.4-10.7] vs 9.8 [95% CI, 9.2-10.4]) (data not provided, 2-way interaction effect between year[s] and month periods, P = .02).
Figure 3.
Average days per month daily average PM2.5 pollution levels exceeded WHO standard (≥10.0 ug/m3) and monthly influenza rates per 1000 patients in reporting practices within California during respective time periods. Poisson regression using GLM analyses. Two-way interaction effect shows significant pre/post changes in 2020 vs previous years for both PM2.5 (P = .01), and influenza infection (P = .04). CI, confidence interval; GLM, generalized linear models; IRR, incidence rate ratios; PM2.5, particulate matter with diameter less than 2.5 micrometers; WHO, World Health Organization.
The rate of influenza per 1000 pediatric and adult patients in reporting California practices decreased by 77% between January to March and April to June in 2020 (197.2 vs 45.8 per 1000 patients per month) (P < .001). This reduction was significantly greater than the 49% reduction when comparing the rates in the concurrent monthly periods during years before COVID-19 (P = .04) (2-way interaction effect between year[s] and month periods, P = .01) (Fig 3).
Discussion
We have found that asthma status at our medical center has substantially improved since the onset of COVID-19 in conjunction with associated school closure in mid-March. This has been exhibited by considerably better asthma control defined by the ACT15 and albuterol use,16 reduced severe asthma exacerbations requiring OCS, and fewer ED visits and hospitalizations during COVID-19 April to June 2020 period compared with the pre–COVID-19 January to March 2020 period, with significantly greater reductions than observed for similar comparison periods in previous years (2017-2019) (P < .05). Among the possible explanations for this improvement in asthma status, we explored the following 4 indicators: (1) air pollution PM2.5 levels; (2) influenza infection rates; (3) adherence by ICS prescriptions; and (4) change in video TM visits. Both PM2.5 levels and influenza infection rates exhibited the greatest decrease during the COVID-19 period of April to June compared with the pre–COVID-19 January to March period in 2020, which was significantly greater (P < .05) than these comparable periods in 2017 to 2019. There was no evidence of enhanced medication adherence as assessed by the number of ICS controller prescriptions. In contrast, Kaye et al17 found increased adherence to daily controller medication during the first 3 months of 2020. It should be noted that the study of Kaye et al17 was conducted only in adults from January through March 2020, and did not include data after stay-at-home orders were imposed. In addition, the study included data collected by means of electronic inhaler monitoring, which includes reminders for missed doses.17
Finally, we experienced tremendous increases in the use of video TM at our institution since the onset of COVID-19. Our data suggest that socioeconomic status did not limit access to TM as indicated by the higher rate of telehealth visits in the 100% publicly insured cohort compared with approximately half of visits in the cohort 51% funded from public insurance. Although race and ethnicity for the telehealth visits were not available, it is known that those on public health insurance are mostly minority populations,18 suggesting that race and ethnicity did not limit access to telehealth in our population as in the study by Taquechel et al.14
There have been several important epidemiologic studies to both assess asthma status during COVID-19 and explore possible explanations for similar findings. In Table 1, we compare 5 of these studies with our own study and found that only the study of Taquechel et. al14 compares favorably with our study in terms of length of the observation period in weeks, the number of key observations of both asthma status, and factors which could affect these outcomes. As we have discussed, Taquechel et al14 found substantially decreased ED visits and hospitalizations and less need for OCS in the 60-day window from April to May compared from January to March. Demographic differences found a higher proportion of asthma encounters such as outpatient visits, hospitalizations, and phone calls in the African American population and those on Medicaid vs commercial insurances. In our cohort, racial differences were also found indicating that African Americans had poorer outcomes in terms of ED visits during COVID-19 months compared with pre–COVID-19, but not for severe exacerbations requiring OCS. The differences noted between our outcomes and those reported by Taquechel et al14 probably reflect differences in demographics, with African American children representing only 1.7% of our population (in contrast with 42% in the study of Taquechel et al14), and Hispanic children comprising 49.8% in our population (compared with 9% in the study of Taquechel et al14). Unlike the study of Taquechel et al,14 we did not find considerable differences between public and commercial insurance in these beforeor during COVID-19 outcomes, although ED visit and OCS use rates were consistently higher for patients on public vs private health insurance. In terms of the relationship of air pollution and viral infection changes to improved asthma outcomes during the COVID 19 pandemic, Taquelchel et al14 found that improvement in asthma status was seen to strongly be associated with decreased HRV infections, but not influenza A or B, nor respiratory syncytial virus diagnosis by polymerase chain reaction (PCR) comparing 2020 with 2015-2019. However, none of the during–COVID-19 period pollution patterns evaluated, including PM2.5, particulate matter 10, ozone, or nitric dioxide were different in the during–COVID-19 period of March 18, 2020, to May 17, 2020, compared with the pre–COVID-19 period of January 17, 2020, to March 17, 2020. In contrast, we found that both influenza and PM2.5 exhibit statistically lower rates during vs pre–COVID-19, which was associated with improved asthma status. In our study located in southern California with high traffic volumes reflecting relatively high average PM2.5, the average number of days per month with daily average values exceeding the WHO threshold (≥10.0 ug/m3) was reduced by 37% in April to June compared with January to March of 2020, whereas the rate increased by 30% in April to June compared with January to March in years before COVID-19.
Several other studies have also found decreased ED visits11, 12, 13 and hospitalizations13 in the during vs pre–COVID-19 period, but with no reported attempt to identify potential contributory factors that could explain the improvement noted, as detailed in Table 1.
In an international online survey for observations made as of April 19, 2020 sent to providers in the Pediatric Asthma in Real Life Think Tank and the World Allergy Organization Pediatric Allergy Commission, Papadolous et al6 reported findings of a marked reduction in asthma encounters, improved asthma control (by ACT or asthma control questionnaire validated tools), and self-reported better adherence among 133,000 children with asthma sampled.6 A substantial limitation of this study is that the clinical data are not based on direct evaluation, but based on subjective survey evaluation, which makes it subject to recall bias.
Limitations
Key potential limitations could include the reliability of the air pollution data in terms of data collection station distribution. The 3 sites for PM2.5 measurements encompass the entire county. Furthermore, the South Coast Air Quality Management District network exceeds the minimum monitoring requirements for all criteria pollutants.19 Another potential limitation is the reliability of clinically defined influenza infections vs other similar viruses because this is not PCR-based. However, Orange County–specific data were not available. The ILI study by Wallace et al20 reported the rate of ILI in their study and the number of influenza A positive PCR samples correlated with the reports of ILI per 100,000 population from sentinel practices, similar to what is collected by ILINet. Furthermore, they reported that most of the ILI-reported cases tested positive for Influenza A.20 The availability of ACT survey data were limited to a small number of patients in our cohort, with information available from April to June of 2019 and 2020. This may reflect a biased sample because the ACT cohort had a greater persistence of asthma when compared with the larger non-ACT cohort. However, the use of albuterol of 3 or more canisters per 6 months, a validated marker of uncontrolled asthma and risk of exacerbations,16 found similar directional evidence of the decreased rate of uncontrolled asthma during COVID-19. Finally, African American children were underrepresented in our population of minority children with asthma, and thus, our findings for this small African American cohort cannot be generalizable to other populations. Telehealth data were for all primary care visits and not asthma-specific visits, so our telehealth findings need to be viewed with caution regarding asthma visit patterns.
Conclusions
We have stressed the importance of a comprehensive approach to assessing the effect of COVID-19 in terms of both asthma status, and, identification of key demographic and environmental factors that could affect asthma outcomes in a largely Hispanic, underserved, minority population in Orange County, California. Consistent with other studies,11, 12, 13, 14 we found improved asthma control associated with reduced asthma exacerbations and health care utilization in association with less influenza infection and reduced air pollution, such as seen with PM2.5, by the stay-at-home mandate. In addition, we found increased, not decreased, telehealth rates in our publicly insured cohort, suggesting that in our population socioeconomic and minority status were not impediments to telehealth visit access. Better adherence, as previously suggested,17 was not supported using our ICS claims data. To be more generalizable, these data need to be confirmed in a comprehensive manner in other geographic areas with other racial and ethnic populations.
Footnotes
Disclosures: The authors have no conflicts of interest to report.
Funding: The authors have no funding sources to report.
References
- 1.Centers for Disease Control and Prevention. Corona data tracker. Available at: https://covid.cdc.gov/covid-data-tracker. Accessed February 26, 2021.
- 2.National Health Interview Survey, Centers for Disease Control and Prevention. National current asthma prevalence 2014. Available at: http://www.cdc.gov.asthma/asthmadata.htm. Accessed December 30, 2020.
- 3.Minor TE, Dick EC, DeMeo AN, Ouellette JJ, Cohen M, Reed CE. Viruses as precipitants of asthmatic attacks in children. JAMA. 1974;227(3):292–298. [PubMed] [Google Scholar]
- 4.Johnston SL, Pattemore PK, Sanderson G, et al. Community study of role of viral infections in exacerbations of asthma in 9-11 year old children. BMJ. 1995;310(6989):1225–1229. doi: 10.1136/bmj.310.6989.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kloepfer KM, Olenec JP, Ming W, et al. Increased H1N1 infection rate in children with Asthma. Am J Respir Crit Care Med. 2012;185(12):1275–1279. doi: 10.1164/rccm.201109-1635OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papadopoulos NK, Custovic A, Deschildre A, et al. Impact of COVID-19 on pediatric asthma: practice adjustments and disease burden. J Allergy Clin Immunol Pract. 2020;8(8):2592–2599. doi: 10.1016/j.jaip.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruano FJ, Alvarez MLS, Haroun-Diaz E, et al. Impact of the COVID-19 pandemic in children with allergic asthma. J Allergy Clin Immunol Pract. 2020;8(9):1372–1374.e1. doi: 10.1016/j.jaip.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peters MC, Sajuthi S, Deford P, et al. COVID-19-related genes in sputum cells in asthma. Relationship to demographic features and corticosteroids. Am J Respir Crit Care Med. 2020;202(1):83–90. doi: 10.1164/rccm.202003-0821OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Branco ACC, Sato MN, Alberca RW. The possible dual role of the ACE2 receptor in asthma and coronavirus (SARS-CoV2) infection. Front Cell Infect Microbiol. 2020;10 doi: 10.3389/fcimb.2020.550571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lipworth B, Chan R, RuiWen Kuo C. Use of inhaled corticosteroids in asthma and coronavirus disease 2019: keep calm and carry on. Ann Allergy Asthma Immunol. 2020;125(5):503–504. doi: 10.1016/j.anai.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oreskovic NM, Kinane TB, Aryee E, Kuhlthau KA, Perrin JM. The unexpected risks of COVID-19 on asthma control in children. J Allergy Clin Immunol Pract. 2020;8(8):2489–2491. doi: 10.1016/j.jaip.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simoneau T, Greco KF, Hammond A, Nelson K, Gaffin JM. Impact of the COVID-19 pandemic on pediatric emergency department utilization for asthma [e-pub ahead of print]. Ann Am Thorac Soc. doi:10.1513/AnnalsATS.202007-765RL, Accessed January 07, 2021. [DOI] [PMC free article] [PubMed]
- 13.Kenyon CC, Hill DA, Hendrickson FE, Byrant-Stephens TC, Zorc JJ. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020;8(8):2774–2776.e1. doi: 10.1016/j.jaip.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taquechel K, Diwadkar A, Sayed S, et al. Pediatric asthma health care utilization, viral testing, and air pollution changes during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8(10):3378–3387.e11. doi: 10.1016/j.jaip.2020.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65. doi: 10.1016/j.jaci.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Amin S, Soliman M, McIvor A, Cave A, Cabrera C. Usage patterns of short-acting β 2-agonists and inhaled corticosteroids in asthma: a targeted literature review. J Allergy Clin Immunol Pract. 2020;8:2556–2564.e8. doi: 10.1016/j.jaip.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 17.Kaye L, Theye B, Smeenk I, Gondalia R, Barrett M, Stempel D. Changes in medication adherence among patients with asthma and COPD during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8(7):2384–2385. doi: 10.1016/j.jaip.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberts M. Agency for Healthcare Research and Quality; Rockville (MD): 2006. Racial and Ethnic Differences in Health Insurance Coverage and Usual Source of Care, 2002. [Google Scholar]
- 19.Miyasato M, Low J, Bermudez RM. South Coast air quality management district. Annual air quality monitoring plan. Available at: http://www.aqmd.gov/docs/default-source/clean-air-plans/air-quality-monitoring-network-plan/annual-air-quality-monitoring-network-plan-v2.pdf. Accessed January 17, 2021.
- 20.Wallace LA, Collins TC, Douglas JD, McIntyre S, Millar J, Carman WF. Virological surveillance of influenza-like illness in the community using PCR and serology. J Clin Virol. 2004;31(1):40–45. doi: 10.1016/j.jcv.2003.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]