Abstract
Objectives
to analyse the accuracy of grip strength and gait speed in identifying mortality; to compare the association between mortality and sarcopenia defined by the EWGSOP1 and EWGSOP2 using the best cut-off found in the present study and those recommended in the literature and to test whether slowness is better than these two definitions to identify the risk of death in older adults.
Methods
a longitudinal study was conducted involving 6,182 individuals aged 60 or older who participated in the English Longitudinal Study of Ageing. Sarcopenia was defined based on the EWGSOP1 and EWGSOP2 using different cut-off for low muscle strength (LMS). Mortality was analysed in a 14-year follow-up.
Results
compared with the LMS definitions in the literature (<32, <30, <27 and < 26 kg for men; <21, <20 and < 16 kg for women), the cut-off of <36 kg for men (sensitivity = 58.59%, specificity = 72.96%, area under the curve [AUC] = 0.66) and < 23 kg for women (sensitivity = 68.90%, specificity = 59.03%, AUC = 0.64) as well as a low gait speed (LGS) ≤0.8 m/s (sensitivity = 53.72%, specificity = 74.02%, AUC = 0.64) demonstrated the best accuracy for mortality. Using the cut-off found in the present study, probable sarcopenia [HR = 1.30 (95%CI: 1.16–1.46)], sarcopenia [HR = 1.48 (95%CI: 1.24–1.78)] and severe sarcopenia [HR = 1.78 (95%CI: 1.49–2.12)] according to EWGSOP2 were better predictors of mortality risk than EWGSOP1. LGS ≤0.8 m/s was a better mortality risk predictor only when LMS was defined by low cut-off.
Conclusions
using LMS <36 kg for men and < 23 kg for women and LGS ≤ 0.8 m/s, EWGSOP2 was the best predictor for mortality risk in older adults.
Keywords: sarcopenia, handgrip strength, longitudinal study, English Longitudinal Study of Ageing (ELSA study), mobility, older people
Key Points
Low muscle strength (LMS) defined as a handgrip strength (HGS) <36 kg for men and < 23 kg for women and low gait speed (LGS) defined as gait speed (GS) ≤0.8 m/s showed the best accuracy for mortality.
When low muscle strength (LMS) is defined as handgrip strength (HGS) <36 kg for men and < 23 kg for women and low gait speed (LGS) is defined as gait speed (GS) ≤0.8 m/s, European Working Group on Sarcopenia in Older People (EWGSOP2) is a better predictor for mortality risk in older adults.
Low gait speed (LGS) ≤0.8 m/s is a better mortality risk predictor only when low muscle strength (LMS) is defined using low cut-off.
Introduction
Two operational definitions for sarcopenia were proposed by the European Working Group on Sarcopenia in Older People (EWGSOP): 2010 (EWGSOP1) [1] and 2019 (EWGSOP2) [2]. The EWGSOP1 proposed the diagnosis of sarcopenia in the presence of low muscle mass (LMM) and low muscle function determined by the reduction in muscle strength or physical performance. Severe sarcopenia was defined when the three components were present [1]. The EWGSOP2 proposed the diagnosis of sarcopenia by the combination of low muscle strength (LMS) and LMM. Physical performance, which was previously a central component of the definition, categorised the severity of the condition in the new definition. However, the two guidelines have little diagnostic agreement, generating discrepancies in the prevalence of sarcopenia, which ranges from 11 to 27.7% when the EWGSOP1 is applied and 4.6 to 13.6% when the EWGSOP2 is applied [3–7].
Recent studies comparing these definitions have found an association with a greater risk of mortality when sarcopenia is defined by the EWGSOP1 but not when defined by the EWGSOP2 [4, 8–10]. One explanation for this disagreement may be the inclusion of gait speed (GS) in the assessment, which was previously part of the diagnosis of sarcopenia and not only an indicator of its severity. Another explanation for this divergence may reside in the use of lower cut-off points for LMS, which is a primary parameter in the EWGSOP2. This argument is supported by the use of different cut-off for handgrip strength (HGS) reported in the literature for different outcomes [11–14].
Lauretani et al. [12] demonstrated that a HGS <30 kg for men and < 20 kg for women was associated with mobility limitation. However, the authors did not report sensitivity, specificity or other components of accuracy analysis. Alley et al. [14] found that HGS <26 kg for men (23.4% sensitivity and 96.6% specificity) and < 16 kg for women (30.6% sensitivity and 87.5% specificity) were the best indicators of weakness associated with mobility limitation. More recently, Delinocente et al. [13] found that a HGS <32 kg for men (49.1% sensitivity, 79.8% specificity and area under the curve of 0.82) and < 21 kg for women (58.6% sensitivity, 72.9% specificity and area under the curve of 0.83) were the best cut-off for identifying mobility limitation. Furthermore, the EWGSOP2 recommends HGS <27 kg for men and < 16 kg for women for LMS; these cut-off were obtained based on population distribution rather than diagnostic accuracy analysis [2], and were tested by Costanzo et al. to identify a 3-year follow-up mortality risk with 48% of sensitivity and 84% of specificity [15].
However, the accuracy of HGS and GS to define mortality risk in a sarcopenia context using a long follow-up period has not been tested. Furthermore, no study has compared the two definitions testing different cut-off for LMS or analysed the importance of LGS to the diagnosis of sarcopenia and its association with mortality. Therefore, the aims of the present study were (i) To analyse the accuracy of HGS and GS to identify mortality risk; (ii) To compare the association between mortality and sarcopenia defined by the EWGSOP1 and EWGSOP2 using the cut-off found in the present study and those recommended in the literature (<32, <30, <27 and < 26 kg for men; <21, <20 and < 16 kg for women) and (iii) To verify whether slowness is better than these two definitions to identify the risk of death in older adults.
Methods
Study population
Data were extracted from the English Longitudinal Study of Ageing (ELSA), which is a panel study started in 2002 with a representative sample of community-dwelling English men and women aged 50 years or older [16]. Details on the ELSA methods can be found in a previous publication [17].
We used the second wave of the ELSA study (2004) as the baseline, which is when anthropometric measures and physical performance were investigated for the first time, involving 6,182 participants aged 60 years or older.
Muscle strength assessment
HGS was measured using a dynamometer. HGS was analysed as a continuous variable in the accuracy analysis. In the mortality analyses, LMS was considered when HGS was <32, <30, <27 and < 26 kg for men and < 21, <20 and < 16 kg for women [1, 2, 11–14]. Detailed information can be found in the Supplemental Material (Section Muscle strength assessment).
Appendicular skeletal muscle mass assessment
Appendicular skeletal muscle mass (ASMM) was determined using the Lee equation [18, 19]. In a study investigating the association between multimorbidity at baseline and the onset of sarcopenia over 12 years of follow-up in a large representative sample of the English older adult population, Veronese et al. also used this equation to estimate ASMM [20]. LMM was considered when the ASMMI was <9.24 kg/m2 for men and < 6.52 kg/m2 for women [21, 22]. Detailed information can be found in the Supplemental Material (Section Appendicular skeletal muscle mass assessment).
Physical performance
GS was used for the assessment of physical performance [23, 24]. GS was analysed as a continuous variable in the accuracy analysis. In the mortality analyses, GS ≤0.8 m/s was considered to have LGS [1, 2]. Detailed information can be found in the Supplemental Material (Section Physical performance).
All measures used for the definition and diagnosis of sarcopenia were taken at baseline.
Definition and diagnosis of sarcopenia
The criteria proposed by the EWGSOP1 [1] and EWGSOP2 [2] were used for the definition of sarcopenia. Detailed information can be found in the Supplemental Material (Section Definition and diagnosis of sarcopenia).
Covariates
The covariates included in the present analysis constitute a broad spectrum of factors associated with mortality [8, 10, 25] as sex, age, total household wealth, marital status, level of education [26, 27], smoking status, alcohol intake, physical activity level [26, 28, 29], self-report of systemic arterial hypertension, diabetes, cancer, lung disease, heart disease, stroke, falls, depressive symptoms [30], memory status [31], number of medications and abdominal obesity [32, 33]. Detailed information can be found in the Supplemental Material (Section Covariates).
Mortality
Mortality data were obtained from the Office for National Statistics of England.
Statistical analysis
We imputed missing data due to item non-response using multiple imputation by chained equations, which included all variables (including the survival outcome) in the prediction model to generate 20 imputed datasets (each had a final n = 6,182) [34]. Owing to the greater precision offered, we present the analyses from the imputed datasets in this paper. We have also used longitudinal weights in all models.
Sensitivity, specificity, log-likelihood positive (LR+), negative (LR−), area under the receiver operating characteristic curves and Youden Index values were calculated to determine the accuracy of HGS and GS in identifying mortality [35, 36].
The sample characteristics at baseline were expressed as mean, standard deviation and proportion. We examined all deaths occurred in the 14-year follow-up period. The follow-up time was defined by the date of the last visit/interview and the date of death. The time for those who deceased was calculated by the difference between the date of death (day/month/year) and date of the oldest interview. The time for those who lived through the end of the follow-up period was calculated by the difference between the last data recorded (visit/interview) and the data from the baseline interview.
Survival curves were analysed using the Kaplan–Meier method to explore the association between the different definitions of sarcopenia and mortality. Differences between curves were evaluated using the log-rank test.
Based on proportional risk models, Cox regression analysis was applied to explore the association between sarcopenia and mortality. For such, unadjusted and adjusted hazard ratios (HRs) and respective 95% confidence intervals (CIs) were estimated. The adjusted models were controlled for all sociodemographic, behavioural, clinical and anthropometric variables.
The definitions of sarcopenia according to the EWGSOP1 and EWGSOP2 were constructed with different cut-off points for HGS. The diagnosis proposed by the EWGSOP1 was used for Constructs 1–4, as follows: Construct 1: LMS <26/16 kg; Construct 2: LMS <27/16 kg; Construct 3: LMS <30/20 kg; Construct 4: LMS <32/21 kg. The diagnosis proposed by the EWGSOP2 was used for Constructs 6–9, as follows: Construct 6: LMS <26/16 kg; Construct 7: LMS <27/16 kg; Construct 8: LMS <30/20 kg; Construct 9: LMS <32/21 kg.
LMM, LMS and LGS as isolated conditions were also analysed to identify which had a stronger association with an increased risk of mortality.
All models were compared using the concordance index or C-index. A C-index of 0.5 indicates a poor performing model, whereas a value of 1 indicates a model with perfect prediction [37, 38].
The Stata 16.1® statistical package was used for all analyses, with a P-value <0.05 considered indicative of statistical significance.
Results
Among the 6,182 participants of the study (Figure 1), 2,669 died in the 14-year follow-up period. The sociodemographic, behavioural, clinical and anthropometric characteristics and components of sarcopenia of the participants at baseline are displayed in Table 1.
Figure 1.
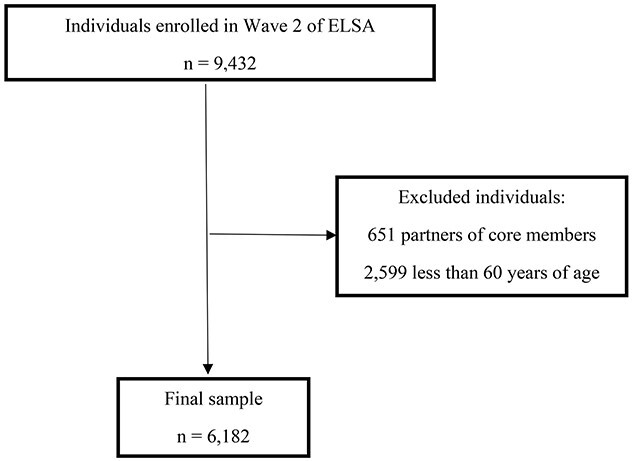
Flowchart of participant selection process.
Table 1.
Baseline characteristics of 6,182 older adults participating in ELSA study (2004)
| Variables | ELSA n = 6,182 |
|---|---|
| Sociodemographic characteristics | |
| Age, years | 71.4 ± 7.9 |
| Age groups, (%) | |
| 60–69 | 46.5 |
| 70–79 | 35.4 |
| ≥ 80 | 18.1 |
| Sex (female), (%) | 55.5 |
| Marital status (with conjugal life), (%) | 63.1 |
| Total household wealth, (%) | |
| 1st quintile (highest quintile) | 20.0 |
| 2nd quintile | 19.6 |
| 3rd quintile | 19.9 |
| 4th quintile | 20.0 |
| 5th quintile (lowest quintile) | 19.5 |
| Not reported, (%) | 1.0 |
| Educational level, (%) | |
| > 13 years | 20.6 |
| 12–13 years | 19.3 |
| 0–11 years | 60.1 |
| Behavioural characteristics | |
| Smoking status, (%) | |
| Never smoked | 36.0 |
| Former smoker | 51.2 |
| Current smoker | 12.8 |
| Alcohol intake, (%) | |
| Non-drinker or rare drinker | 19.5 |
| Frequent drinker | 37.1 |
| Daily drinker | 28.5 |
| Did not answer | 14.9 |
| Sedentary lifestyle, (%) | 42.3 |
| Clinical characteristics | |
| Arterial hypertension (yes), (%) | 48.7 |
| Diabetes (yes), (%) | 10.2 |
| Cancer (yes), (%) | 9.2 |
| Lung disease (yes), (%) | 18.8 |
| Heart disease (yes), (%) | 26.9 |
| Stroke (yes), (%) | 6.9 |
| Falls (yes), (%) | 32.9 |
| Depressive symptoms (yes), (%) | 15.5 |
| Memory Score, points | 9.1 ± 3.7 |
| Medications, number | 0.5 ± 0.7 |
| Waist circumference, (%) | |
| Non-abdominal obesity | 47.6 |
| Abdominal obesity | 52.4 |
| Waist circumference, cm | |
| Men | 101.7 ± 12.1 |
| Women | 91.0 ± 13.5 |
| Components of sarcopenia | |
| Grip strength, kg | |
| Men | 36.9 ± 10.4 |
| Women | 21.9 ± 7.1 |
| LMS (< 26 kg ♂; < 16 kg ♀), (%) | 15.2 |
| LMS (< 27 kg ♂; < 16 kg ♀), (%) | 16.3 |
| LMS (< 30 kg ♂; < 20 kg ♀), (%) | 28.4 |
| LMS (< 32 kg ♂; < 21 kg ♀), (%) | 36.2 |
| LMS (< 36 kg ♂; < 23 kg ♀), (%) | 49.6 |
| Appendicular skeletal muscle mass index, kg/m2 | |
| Men | 10.1 ± 1.2 |
| Women | 7.6 ± 1.5 |
| LMM, (%) | 19.9 |
| GS, m/s | |
| Men | 0.91 ± 0.3 |
| Women | 0.84 ± 0.3 |
| Low gait speed (≤ 0.8 m/s), (%) | 40.9 |
Data expressed as proportion, mean and standard deviation.
The sample was composed predominantly of women (55.5%) as well as individuals with a conjugal life (63.1%) and low schooling (0–11 years) (60.1%). Regarding behavioural characteristics, most were former-smokers (51.2%) with an active lifestyle (57.7%) and 37.1% reported frequent alcohol intake. Among the chronic diseases investigated, systemic arterial hypertension was the most prevalent (48.7%), followed by heart disease (26.9%). The majority had abdominal obesity (52.4%) (Table 1).
LMS defined as HGS <36 kg for men (sensitivity = 58.59%, specificity = 72.96%, LR+ = 2.17, LR− = 0.57, AUC = 0.66 and Youden = 0.32) and < 23 kg for women (sensitivity = 68.90%, specificity = 59.03%, LR+ = 1.68, LR− = 0.53, AUC = 0.64 and Youden = 0.28) was more accurate in identifying mortality (Table 2). LGS defined as GS ≤0.8 m/s (sensitivity = 53.72%, specificity = 74.02%, LR+ = 2.07, LR− = 0.62, AUC = 0.64 and Youden = 0.28) was more accurate in identifying mortality, confirming what is recommended by the consensus (Table 3). Based on these cut-off points, Construct 5 (EWGSOP1 with LMS <36/23 kg) and Construct 10 (EWGSOP2 com LMS <36/23 kg) were created.
Table 2.
Diagnostic properties of HGS cut-off to identify mortality (ELSA study)
| Cut-off (kg) | Sensitivity | Specificity | Correct Classification | LR+ | LR− | AUC | Youden |
|---|---|---|---|---|---|---|---|
| Men | |||||||
| <24 | 11.17 | 95.96 | 58.74 | 2.76 | 0.93 | 0.54 | 0.07 |
| <25 | 13.28 | 95.05 | 59.16 | 2.68 | 0.91 | 0.54 | 0.08 |
| <26 | 15.49 | 94.31 | 59.71 | 2.72 | 0.90 | 0.55 | 0.10 |
| <27 | 18.55 | 92.91 | 60.27 | 2.62 | 0.88 | 0.56 | 0.11 |
| <28 | 20.86 | 92.17 | 60.87 | 2.66 | 0.86 | 0.56 | 0.13 |
| <29 | 24.45 | 90.85 | 61.70 | 2.67 | 0.83 | 0.58 | 0.15 |
| <30 | 26.98 | 89.53 | 62.07 | 2.58 | 0.82 | 0.58 | 0.17 |
| <31 | 34.25 | 87.14 | 63.92 | 2.66 | 0.75 | 0.61 | 0.21 |
| <32 | 38.78 | 84.91 | 64.66 | 2.57 | 0.72 | 0.62 | 0.24 |
| <33 | 43.73 | 82.36 | 65.40 | 2.48 | 0.68 | 0.63 | 0.26 |
| <34 | 47.63 | 79.72 | 65.63 | 2.35 | 0.66 | 0.64 | 0.27 |
| <35 | 52.37 | 77.08 | 66.23 | 2.28 | 0.62 | 0.65 | 0.29 |
| <36 | 58.59 | 72.96 | 66.65 | 2.17 | 0.57 | 0.66 | 0.32 |
| <37 | 62.38 | 67.68 | 65.36 | 1.93 | 0.56 | 0.65 | 0.30 |
| <38 | 67.02 | 63.64 | 65.12 | 1.84 | 0.52 | 0.65 | 0.31 |
| <39 | 70.71 | 59.52 | 64.43 | 1.75 | 0.49 | 0.65 | 0.30 |
| Women | |||||||
| <11 | 5.62 | 97.02 | 64.92 | 1.88 | 0.97 | 0.51 | 0.03 |
| <12 | 7.56 | 96.20 | 65.07 | 1.99 | 0.96 | 0.52 | 0.04 |
| <13 | 10.80 | 95.32 | 65.64 | 2.31 | 0.94 | 0.53 | 0.06 |
| <14 | 13.50 | 94.27 | 65.91 | 2.36 | 0.92 | 0.54 | 0.08 |
| <15 | 17.49 | 92.93 | 66.44 | 2.47 | 0.89 | 0.55 | 0.10 |
| <16 | 23.65 | 90.77 | 67.20 | 2.56 | 0.84 | 0.57 | 0.14 |
| <17 | 28.73 | 87.55 | 66.89 | 2.31 | 0.81 | 0.58 | 0.16 |
| <18 | 34.67 | 84.98 | 67.31 | 2.31 | 0.77 | 0.60 | 0.20 |
| <19 | 42.76 | 81.30 | 67.77 | 2.29 | 0.70 | 0.62 | 0.24 |
| <20 | 47.08 | 78.14 | 67.24 | 2.15 | 0.68 | 0.63 | 0.25 |
| <21 | 55.94 | 70.95 | 65.68 | 1.93 | 0.62 | 0.63 | 0.27 |
| <22 | 61.45 | 65.05 | 63.78 | 1.76 | 0.59 | 0.63 | 0.27 |
| <23 | 68.90 | 59.03 | 62.50 | 1.68 | 0.53 | 0.64 | 0.28 |
| <24 | 73.97 | 53.24 | 60.52 | 1.58 | 0.49 | 0.64 | 0.27 |
| <25 | 79.27 | 46.52 | 58.02 | 1.48 | 0.45 | 0.63 | 0.26 |
| <26 | 85.53 | 38.81 | 55.21 | 1.40 | 0.37 | 0.62 | 0.24 |
| <27 | 88.77 | 31.74 | 51.76 | 1.30 | 0.35 | 0.60 | 0.21 |
| <28 | 91.14 | 26.07 | 48.92 | 1.23 | 0.34 | 0.59 | 0.17 |
| <29 | 93.20 | 20.86 | 46.26 | 1.18 | 0.33 | 0.57 | 0.14 |
| <30 | 84.82 | 16.13 | 43.76 | 1.13 | 0.32 | 0.55 | 0.01 |
LR+: positive Log-likelihood; LR−: negative Log-likelihood; AUC: area under curve
Table 3.
Diagnostic properties of GS cut-off to identify mortality (ELSA study)
| Cut-off (m/s) | Sensitivity | Specificity | Correct Classification | LR+ | LR− | AUC | Youden |
|---|---|---|---|---|---|---|---|
| ≤0.3 | 3.80 | 99.38 | 62.09 | 6.16 | 0.97 | 0.52 | 0.03 |
| ≤0.4 | 8.51 | 98.39 | 63.32 | 5.29 | 0.93 | 0.53 | 0.07 |
| ≤0.5 | 16.32 | 96.34 | 65.11 | 4.45 | 0.87 | 0.56 | 0.13 |
| ≤0.6 | 27.18 | 91.82 | 66.60 | 3.32 | 0.79 | 0.59 | 0.19 |
| ≤0.7 | 40.29 | 84.77 | 67.41 | 2.64 | 0.70 | 0.62 | 0.25 |
| ≤0.8 | 53.72 | 74.02 | 66.10 | 2.07 | 0.62 | 0.64 | 0.28 |
| ≤0.9 | 68.43 | 59.74 | 63.13 | 1.70 | 0.53 | 0.64 | 0.28 |
| ≤1.0 | 80.10 | 44.03 | 58.10 | 1.43 | 0.45 | 0.62 | 0.24 |
| ≤1.1 | 88.76 | 30.64 | 53.32 | 1.28 | 0.37 | 0.60 | 0.19 |
| ≤1.2 | 93.69 | 18.76 | 48.00 | 1.15 | 0.34 | 0.56 | 0.12 |
| ≤1.3 | 96.74 | 10.75 | 44.30 | 1.08 | 0.30 | 0.54 | 0.07 |
| ≤1.4 | 98.13 | 6.03 | 41.96 | 1.04 | 0.31 | 0.52 | 0.04 |
| ≤1.5 | 98.88 | 3.25 | 40.56 | 1.02 | 0.34 | 0.51 | 0.02 |
| ≤1.6 | 99.41 | 1.88 | 39.94 | 1.01 | 0.31 | 0.51 | 0.01 |
lr+: positive log-likelihood; lr−: negative log-likelihood; auc: area under curve
Regarding the components of sarcopenia, 49.6%, 36.2%, 28.4%, 16.3% and 15.2% had LMS using the cut-off of <36, <32, <30, <27 and < 26 kg for men and < 23, <21, <20 and < 16 kg for women, respectively. LMM was found in 19.9% and LGS was found in 40.9% of the individuals (Table 1).
Higher prevalence values for sarcopenia were found when the LMS cut-off were < 36/23 kg for both EWGSOP1 and EWGSOP2. However, EWGSOP2 was better in identifying sarcopenia with 33.9% probable sarcopenia, 6.2% sarcopenia and 8.6% severe sarcopenia (Table 4).
Table 4.
Prevalence and cox proportional hazard for different constructs of sarcopenia to predict mortality in 14-year follow-up among 6,182 older adults from ELSA study
| Prevalence (%) (95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Construct 1 | Construct 2 | Construct 3 | Construct 4 | Construct 5 | Construct 6 | Construct 7 | Construct 8 | Construct 9 | Construct 10 | |
| No sarcopenia | 78.8 (77.5–79.9) | 78.8 (77.5–79.9) | 78.8 (77.5–79.9) | 78.8 (77.5–79.9) | 78.8 (77.5–79.9) | 86.3 (85.3–87.3) | 85.2 (84.3–86.2) | 73.0 (71.7–74.2) | 65.0 (63.7–66.3) | 51.3 (49.8–52.7) |
| Pre-sarcopenia1 | 9.9 (9.0–10.7) | 9.8 (8.9–10.6) | 8.4 (7.6–9.2) | 7.2 (6.4–8.0) | 5.1 (4.5–5.8) | 9.0 (8.1–9.9) | 9.6 (8.7–10.4) | 18.2 (17.1–19.3) | 23.6 (22.3–24.9) | 33.9 (32.6–35.2) |
| Sarcopenia2 | 7.6 (6.8–8.4) | 7.4 (6.6–8.2) | 6.7 (6.0–7.6) | 6.8 (6.1–7.7) | 7.7 (6.9–8.5) | 1.2 (0.9–1.6) | 1.4 (1.1–1.7) | 2.8 (2.3–3.3) | 4.2 (3.6–4.7) | 6.2 (5.5–6.9) |
| Severe Sarcopenia | 3.7 (3.2–4.2) | 4.0 (3.5–4.5) | 6.1 (5.4–6.7) | 7.2 (6.5–7.9) | 8.4 (7.7–9.2) | 3.5 (2.9–4.0) | 3.8 (3.2–4.4) | 6.0 (5.2–6.7) | 7.2 (6.5–8.0) | 8.6 (7.8–9.3) |
| Adjusted Model HR (95% CI) | ||||||||||
| Construct 1 | Construct 2 | Construct 3 | Construct 4 | Construct 5 | Construct 6 | Construct 7 | Construct 8 | Construct 9 | Construct 10 | |
| No sarcopenia | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Pre-sarcopenia1 | 1.11 (0.94–1.32) | 1.10 (0.93–1.31) | 1.11 (0.91–1.34) | 1.07 (0.86–1.33) | 0.95 (0.71–1.28) | 1.06 (0.90–1.24) | 1.03 (0.90–1.18) | 1.08 (0.95–1.23) | 1.12 (1.00–1.26) | 1.30 (1.16–1.46) |
| Sarcopenia2 | 1.37 (1.17–1.61) | 1.38 (1.17–1.63) | 1.32 (1.12–1.56) | 1.26 (1.06–1.49) | 1.23 (1.05–1.45) | 1.02 (0.73–1.42) | 1.06 (0.77–1.45) | 1.08 (0.86–1.36) | 1.21 (0.99–1.48) | 1.48 (1.24–1.78) |
| Severe Sarcopenia | 1.36 (1.11–1.67) | 1.36 (1.12–1.65) | 1.37 (1.16–1.61) | 1.43 (1.22–1.68) | 1.48 (1.27–1.73) | 1.21 (0.97–1.50) | 1.19 (0.95–1.50) | 1.29 (1.08–1.53) | 1.44 (1.21–1.71) | 1.78 (1.49–2.12) |
| C-index | 0.7779 | 0.7780 | 0.7777 | 0.7781 | 0.7785 | 0.7765 | 0.7765 | 0.7771 | 0.7779 | 0.7794 |
HR: hazard ratio; CI: confidence interval. Models adjusted for sex, age, total household wealth, marital status, smoking status, alcohol intake, physical activity level, systemic arterial hypertension, diabetes, cancer, lung disease, heart disease, stroke, falls in the previous year, depressive symptoms, memory performance, number of medications and waist circumference; 1 probable sarcopenia in EWGSOP2; 2 or confirmed sarcopenia in EWGSOP2
EWGSOP1:
Construct 1—LMS <26/16 kg; Construct 2—LMS <27/16 kg; Construct 3—LMS <30/20 kg; Construct 4—LMS <32/21 kg; Construct 5—LMS <36/23 kg
EWGSOP2:
Construct 6—LMS <26/16 kg; Construct 7—LMS <27/16 kg; Construct 8—LMS <30/20 kg; Construct 9—LMS <32/21 kg; Construct 10—LMS <36/23 kg
Associations between sarcopenia status and mortality using the EWGSOP1 and EWGSOP2 definitions are presented in Table 4 and Supplemental Table 1. EWGSOP2 using the cut-off of <36/23 kg to define LMS was the best mortality risk predictor in older adults in 14-year follow-up period. In the completely adjusted models, individuals with probable sarcopenia showed 30% higher mortality risk than non-sarcopenic. This was the only significant cut-off value for probable sarcopenia. The mortality risk increased to 48% for those with sarcopenia and 78% for those with severe sarcopenia (Table 4).
Table 5 shows the analysis of the sarcopenia components separately. A LGS ≤ 0.8 m/s was a better mortality risk predictor only when LMS was defined using low cut-off values. When the cut-off <36/23 kg were used, the mortality risk for those individuals with LMS was 35% (95%CI 1.22–1.49) higher than those with HGS ≥36/23 kg and 36% (95%CI 1.23–1.50) higher for those with LGS than those with GS >0.8 m/s i.e. the mortality risks were practically the same.
Table 5.
Cox proportional hazard of sarcopenia components predicting mortality in 14-year follow-up among 6,182 older adults from ELSA study
| Unadjusted model HR (95% CI) | Adjusted model HR (95% CI) | |
|---|---|---|
| References: Normal muscle strength/normal muscle mass/normal GS | 1.00 | 1.00 |
| Model 1 | ||
| LMS (< 26/16 kg) | 1.62 (1.47–1.80) | 1.10 (0.99–1.24) |
| LMM (< 6.52 kg/m2; < 9.24 kg/m2) | 2.01 (1.83–2.21) | 1.24 (1.09–1.42) |
| Low gait speed (≤ 0.8 m/s) | 2.54 (2.33–2.76) | 1.39 (1.26–1.54) |
| C-index | 0.6606 | 0.7789 |
| Model 2 | ||
| LMS (< 27/16 kg) | 1.63 (1.47–1.80) | 1.08 (0.97–1.21) |
| LMM (< 6.52 kg/m2; < 9.24 kg/m2) | 2.00 (1.82–2.19) | 1.24 (1.09–1.42) |
| Low gait speed (≤ 0.8 m/s) | 2.53 (2.32–2.75) | 1.39 (1.26–1.54) |
| C-index | 0.6618 | 0.7789 |
| Model 3 | ||
| LMS (< 30/20 kg) | 1.70 (1.55–1.86) | 1.14 (1.03–1.26) |
| LMM (< 6.52 kg/m2; < 9.24 kg/m2) | 1.94 (1.76–2.13) | 1.23 (1.08–1.40) |
| Low gait speed (≤ 0.8 m/s) | 2.41 (2.21–2.62) | 1.38 (1.25–1.52) |
| C-index | 0.6679 | 0.7790 |
| Model 4 | ||
| LMS (< 32/21 kg) | 1.81 (1.66–1.98) | 1.16 (1.04–1.28) |
| LMM (< 6.52 kg/m2; < 9.24 kg/m2) | 1.90 (1.73–2.09) | 1.23 (1.08–1.41) |
| Low gait speed (≤ 0.8 m/s) | 2.35 (2.16–2.56) | 1.38 (1.25–1.52) |
| C-index | 0.6724 | 0.7791 |
| Model 5 | ||
| LMS (< 36/23 kg) | 2.09 (1.91–2.29) | 1.35 (1.22–1.49) |
| LMM (< 6.52 kg/m2; < 9.24 kg/m2) | 1.86 (1.69–2.04) | 1.23 (1.08–1.39) |
| Low gait speed (≤ 0.8 m/s) | 2.32 (2.14–2.52) | 1.36 (1.23–1.50) |
| C-index | 0.6829 | 0.7800 |
HR: hazard ratio; CI: confidence interval. Models adjusted for sex, age, total household wealth, marital status, smoking status, alcohol intake, physical activity level, systemic arterial hypertension, diabetes, cancer, lung disease, heart disease, stroke, falls in the previous year, depressive symptoms, memory performance, number of medications and waist circumference.
Model 1: HGS <26/16 kg.
Model 2: HGS <27/16 kg.
Model 3: HGS <30/20 kg.
Model 4: HGS <32/21 kg.
Model 5: HGS <36/23 kg.
Discussion
We found that LMS <36 kg for men and < 23 kg for women and LGS ≤0.8 m/s were more accurate in identifying mortality. EWGSOP2 using these cut-off was more accurate in identifying mortality risk than EWGSOP1. In addition, LGS ≤0.8 m/s was a better predictor of mortality risk only when lower LMS cut-off were used.
Petermann-Rocha et al. [8], Locquet et al. [4, 39], Sobestiansky et al. [9], Costanzo et al. [15], Phu et al. [7], Reiss et al. [3], and Yang et al. [5], cross-sectionally and longitudinally, and a recent systematic review by Fernandes et al. [40] found that the prevalence of sarcopenia by EWGSOP2 was considerably lower than EWGSOP1. In all the studies aforementioned, EWGSOP2 was used with lower LMS cut-off and, as a result, a lower prevalence of sarcopenia was reported. Our findings corroborate previous findings in relation to the use of low HGS cut-off to define LMS. However, the prevalence of sarcopenia is higher and more similar between EWGSOP1 and EWGSOP2 when both define LMS as HGS <36/23 kg.
With regards to the association between sarcopenia, defined by EWGSOP2, and higher mortality risk, previous studies showed conflicting results which could be attributed to how probable sarcopenia, sarcopenia and severe sarcopenia were analysed, length of follow-up, age and type of participants. For example, Petermann-Rocha et al. [8], analysing 469,858 UK Biobank community-dwelling participants aged between 40 and 69 and followed-up for 2 years, found that sarcopenia [(LMS <27 kg for men and < 16 kg for women) + (LMM <7.0 kg/m2 for men and < 5.5 kg/m2 for women)] was not associated with mortality risk (HR = 1.25 CI 95% 0.99–1.58). Sobestiansky et al. [9], analysing data from 287 community-dwelling men aged between 85 and 89 of the Uppsala Longitudinal Study of Adult Men (ULSAM) during a 3-year follow-up, also did not find an association between sarcopenia defined as LMS <27 kg + LMM <7.0 kg/m2 or as LMS <26 Kg + LMM <7.0 kg/m2 and mortality (HR = 1.70 95%CI 0.94–3.05 and HR = 1.65 95%CI 0.94–3.05), respectively. Costanzo et al. [15], analysing 535 participants of the InCHIANTI study aged 65 or older followed-up for 3 years, did not find an association between sarcopenia [(LMS <27 kg for men and < 16 kg for women) + (LMM <7.0 kg/m2 for men and < 6.0 kg/m2 for women)] and mortality (HR = 1.96 95%CI 0.63–6.15). Finally, Bachettini et al. [10], analysing 1,291 community-dwelling individuals aged 60 or older and followed-up for 2.6 years, also did not find an association between sarcopenia [(LMS <29.7 kg for men and < 16.2 kg for women) + (LMM ≤34 cm of calf circumference for men and ≤ 33 cm for women)] and mortality (HR = 1.36 95%CI 0.52–3.57).
On the other hand, Malafarina et al. [41], analysing 187 individuals with an average age of 85 years undergoing post-surgical hip fracture rehabilitation during a 7 follow-up period, found an association between sarcopenia [(LMS <27 kg for men and < 16 kg for women) + (LMM <7.0 kg/m2 for men and < 6.0 kg/m2 for woman)] and mortality (HR = 1.67 95%CI 1.11–2.51). Bianchi et al. [42], analysing 527 hospitalised individuals with an average age of 80 years after a 3-year follow-up, also found an association between sarcopenia [(LMS <27 kg for men and < 16 kg for women) + (LMM <7.0 kg/m2 for men and < 5.5 kg/m2 for women)] and mortality (HR = 1.84 95%CI 1.33–2.57).
However, despite the conclusions from a recent meta-analysis involving 42,108 individuals aged 49 and older showing that sarcopenia is associated to a higher mortality risk, independent of the type of population investigated, sarcopenia definition, length of follow-up and risk of bias, only five studies using the EWGSOP2 definition were included with very conflicting results [25]. Therefore, when our findings are compared with the ones from previous studies, the use of higher LMS cut-off in the EWGSOP2 definition to identify community-dwelling older adults with sarcopenia is a better approach not only in terms of estimating prevalence but also to identify mortality risk. Such approach could be very useful to promote preventive strategies and treatment. It is likely that the identification of the best cut-off value in our study was because ELSA has a long follow-up period. Lower cut-off in combination with short follow-up periods showed in the literature are more useful in hospital settings.
Our key findings also highlighted that slowness, separately, was the best mortality risk predictor only when lower LMS cut-off were used (<32, 30, 27 and 26 kg for men and < 21, 20 and 16 kg for women). When the cut-off <36/23 kg were tested, the mortality risk for those who had LMS and LGS compared with those with normal HGS and GS was practically the same. However, despite these two components having very similar mortality risks, their order of entry in the flowchart of the two consensuses on sarcopenia modified the results of the association between sarcopenia status and mortality. It is better when the initial identification process is done with muscle strength before GS, which confirms the advantage of using the algorithm proposed by EWGSOP2.
This study has limitations and strengths that should be acknowledged. Our findings should be considered in the context of community-dwelling individuals aged 60 years or older. Caution should be exercised regarding the interpretation of the results in the clinical/hospital setting and in nursing homes. Another important limitation regards the determination of ASMM using an equation. However, this does not invalidate our findings, as the equation has been validated using gold-standard methods, such as magnetic resonance and dual-energy X-ray absorptiometry. This study also has strong points, such as the inclusion of a large representative sample of community-dwelling older English adults, a 14-year follow-up period and the fact that it is the first study to compare the association of sarcopenia defined by the EWGSOP1 and EWGSOP2 using different cut-off for HGS recommended in the literature and proposed by the present study. Moreover, our survival analysis was adjusted for a wide range of covariates associated with mortality.
Conclusion
LMS <36 kg for men and < 23 kg for women and LGS ≤0.8 m/s demonstrated best accuracy for mortality. LMS <36/23 kg and LGS ≤0.8 m/s, EWGSOP2 predicts better mortality risk in older adults. LGS is a better mortality risk predictor only when LMS is defined using lower cut-off.
Supplementary Material
Acknowledgements
The authors are grateful to all collaborators and participants of the English Longitudinal Study of Ageing. The English Longitudinal Study of Ageing received approval from the National Research Ethics Service [London Multicentre Research Ethics Committee (MREC/01/2/91)]. All participants signed a statement of informed consent.
Contributor Information
Maria Claudia Bernardes Spexoto, Food, Nutrition and Health Postgraduate Program, Federal University of Grande Dourados, Dourados, Brazil; Gerontology Postgraduate Program, Federal University of Sao Carlos, Sao Carlos, Brazil.
Paula Camila Ramírez, Escuela de Fisioterapia, Universidad Industrial de Santander, Bucaramanga, Colombia; Physical Therapy Postgraduate Program, Federal University of Sao Carlos, Sao Carlos, Brazil.
Roberta de Oliveira Máximo, Physical Therapy Postgraduate Program, Federal University of Sao Carlos, Sao Carlos, Brazil.
Andrew Steptoe, Department of Epidemiology and Public Health, University College London, London, UK.
Cesar de Oliveira, Department of Epidemiology and Public Health, University College London, London, UK.
Tiago da Silva Alexandre, Gerontology Postgraduate Program, Federal University of Sao Carlos, Sao Carlos, Brazil; Physical Therapy Postgraduate Program, Federal University of Sao Carlos, Sao Carlos, Brazil; Department of Epidemiology and Public Health, University College London, London, UK; Department of Gerontology, Federal University of Sao Carlos, Sao Carlos, Brazil.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
ELSA is supported by the National Institute on Aging USA (grant number R01AG017644) and a consortium of UK government coordinated by the Economic and Social Research Council (ESRC). TSA was supported by the National Council of Scientific and Technological Development (CNPq) (grant numbers 303981/2017–2 and 303577/2020–7), the Sao Paulo Research Foundation (FAPESP) (grant number 18/13917–3) and Coordination for the Improvement of Higher Education Personnel (CAPES) Institution Internalisation Program (CAPESPrInt grant number 88887.570076/2020–00). This work was supported by the Economic and Social Research Council [grant number ES/T008822/1].
References
- 1. Cruz-Jentoft AJ, Baeyens JP, Bauer JMet al. . Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing 2010; 39: 412–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cruz-Jentoft AJ, Bahat G, Bauer Jet al. . Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019; 48: 601. 10.1093/ageing/afz046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Reiss J, Iglseder B, Alzner Ret al. . Consequences of applying the new EWGSOP2 guideline instead of the former EWGSOP guideline for sarcopenia case finding in older patients. Age Ageing 2019; 48: 719–24. [DOI] [PubMed] [Google Scholar]
- 4. Locquet M, Beaudart C, Petermans J, Reginster J-Y, Bruyère O. EWGSOP2 versus EWGSOP1: impact on the prevalence of sarcopenia and its major health consequences. J Am Med Dir Assoc 2019; 20: 384–5. [DOI] [PubMed] [Google Scholar]
- 5. Yang L, Yao X, Shen Jet al. . Comparison of revised EWGSOP criteria and four other diagnostic criteria of sarcopenia in Chinese community-dwelling elderly residents. Exp Gerontol 2020; 130: 110798. 10.1016/j.exger.2019.110798. [DOI] [PubMed] [Google Scholar]
- 6. Shafiee G, Keshtkar A, Soltani A, Ahadi Z, Larijani B, Heshmat R. Prevalence of sarcopenia in the world: a systematic review and meta-analysis of general population studies. J Diabetes Metab Disord 2017; 16: 1–10. 10.1186/s40200-017-0302-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Phu S, Vogrin S, Zanker J, Bani Hassan E, Al Saedi A, Duque G. Agreement between initial and revised European working group on sarcopenia in older people definitions. J Am Med Dir Assoc 2019; 20: 382–383.e1. [DOI] [PubMed] [Google Scholar]
- 8. Petermann-Rocha F, Chen M, Gray SR, Ho FK, Pell JP, Celis-Morales C. New versus old guidelines for sarcopenia classification: what is the impact on prevalence and health outcomes? Age Ageing 2020; 49: 300–4. [DOI] [PubMed] [Google Scholar]
- 9. Sobestiansky S, Michaelsson K, Cederholm T. Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85-89 year old community-dwelling men: a report from the ULSAM study. BMC Geriatr 2019; 19: 318. 10.1186/s12877-019-1338-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bachettini NP, Bielemann RM, Barbosa-Silva TG, Menezes AMB, Tomasi E, Gonzalez MC. Sarcopenia as a mortality predictor in community-dwelling older adults: a comparison of the diagnostic criteria of the European working group on sarcopenia in older people. Eur J Clin Nutr 2020; 74: 573–80. [DOI] [PubMed] [Google Scholar]
- 11. Dodds RM, Syddall HE, Cooper Ret al. . Grip strength across the life course: normative data from twelve British studies. PLoS One 2014; 9: e113637. 10.1371/journal.pone.0113637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lauretani F, Russo CR, Bandinelli Set al. . Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol (1985) 2003; 95: 1851–60. [DOI] [PubMed] [Google Scholar]
- 13. Delinocente MLB, Carvalho DHT, Oliveira Máximo Ret al. . Accuracy of different handgrip values to identify mobility limitation in older adults. Arch Gerontol Geriatr 2021; 94: 104347. 10.1016/j.archger.2021.104347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alley DE, Shardell MD, Peters KWet al. . Grip strength cutpoints for the identification of clinically relevant weakness. J Gerontol A Biol Sci Med Sci 2014; 69: 559–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Costanzo L, De Vincentis A, Di Iorio Aet al. . Impact of low muscle mass and low muscle strength according to EWGSOP2 and EWGSOP1 in community- dwelling older people. J Gerontol A Biol Sci Med Sci 2020; 75: 1324–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mindell J, Biddulph JP, Hirani Vet al. . Cohort profile: the health survey for England. Int J Epidemiol 2012; 41: 1585–93.. [DOI] [PubMed] [Google Scholar]
- 17. Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: the English longitudinal study of ageing. Int J Epidemiol 2013; 42: 1640–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lee RC, Wang Z, Heo M, Ross R, Janssen I, Heymsfield SB. Total-body skeletal muscle mass: development and cross-validation of anthropometric prediction models. Am J Clin Nutr 2000; 72: 796–803. [DOI] [PubMed] [Google Scholar]
- 19. Al-Gindan YY, Hankey C, Govan L, Gallagher D, Heymsfield SB, Lean MEJ. Derivation and validation of simple equations to predict total muscle mass from simple anthropometric and demographic data. Am J Clin Nutr 2014; 100: 1041–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Veronese N, Smith L, Cereda Eet al. . Multimorbidity increases the risk for sarcopenia onset: longitudinal analyses from the English longitudinal study of ageing. Exp Gerontol 2021; 156: 111624. 10.1016/j.exger.2021.111624. [DOI] [PubMed] [Google Scholar]
- 21. Delmonico MJ, Harris TB, Lee JSet al. . Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc 2007; 55: 769–74. [DOI] [PubMed] [Google Scholar]
- 22. Coin A, Sarti S, Ruggiero Eet al. . Prevalence of sarcopenia based on different diagnostic criteria using DEXA and appendicular skeletal muscle mass reference values in an Italian population aged 20 to 80. J Am Med Dir Assoc 2013; 14: 507–12. [DOI] [PubMed] [Google Scholar]
- 23. Guralnik JM, Simonsick EM, Ferrucci Let al. . A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994; 49: M85–94. [DOI] [PubMed] [Google Scholar]
- 24. Guralnik JM, Ferrucci L, Pieper CFet al. . Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 2000; 55: M221–31. [DOI] [PubMed] [Google Scholar]
- 25. Xu J, Wan CS, Ktoris K, Reijnierse EM, Maier AB. Sarcopenia is associated with mortality in adults: a systematic review and meta-analysis. Gerontology 2022; 68: 361–76. [DOI] [PubMed] [Google Scholar]
- 26. Silva Alexandre T, Scholes S, Ferreira Santos JL, Oliveira Duarte YA, Oliveira C. The combination of dynapenia and abdominal obesity as a risk factor for worse trajectories of IADL disability among older adults. Clinical nutrition (Edinburgh, Scotland) 2018; 37: 2045–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Banks J, Kumari M, Smith JP, Zaninotto P. What explains the American disadvantage in health compared with the English? The case of diabetes. J Epidemiol Community Health 2012; 66: 259–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Silva Alexandre T, Scholes S, Santos JLF, Oliveira C. Dynapenic abdominal obesity as a risk factor for worse trajectories of ADL disability among older adults: the ELSA cohort study. J Gerontol A Biol Sci Med Sci 2019; 74: 1112–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rivilis I, Hay J, Cairney J, Klentrou P, Liu JFB, Faught BE. Physical activity and fitness in children with developmental coordination disorder: a systematic review. Res Dev Disabil 2011; 32: 894–910. [DOI] [PubMed] [Google Scholar]
- 30. Radloff LS. The CES-D scale. Appl Psychol Measur 1977; 1: 385–401. [Google Scholar]
- 31. Steel N, Huppert FA, McWilliams B. Physical and cognitive function. In: Marmot M, Banks J, Blundell R, Lessof C, Nazroo J, editors. Health, Wealth and Lifestyles of the Older Population in England: The 2002 English Longitudinal Study of Ageing. London: Institute for Fiscal Studies; 2003; 249–300.
- 32. Banks J, Breeze E, Lessof C, Nazroo J. Retirement, health and relationships of the older population in England: the 2004 English Longitudinal Study of Ageing. London: Institute for Fiscal Studies, 2006. [Google Scholar]
- 33. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults – the evidence report. National Institutes of Health. Obes Res 1998; 6: 51S–209. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2003/. [PubMed] [Google Scholar]
- 34. Zaninotto P, Wardle J, Steptoe A. Sustained enjoyment of life and mortality at older ages: analysis of the English longitudinal study of ageing. BMJ (Clinical research ed) 2016; 355: i6267. 10.1136/bmj.i6267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. McGee S. Evidence-based physical diagnosis e-book. 4th edition. Philadelphia: Elsevier Health Sciences, 2016. [Google Scholar]
- 36. Youden WJ. Index for rating diagnostic tests. Cancer 1950; 3: 32–5. [DOI] [PubMed] [Google Scholar]
- 37. Harrell FEJ, Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA 1982; 247: 2543–6. [PubMed] [Google Scholar]
- 38. Harrell FEJ, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 1996; 15: 361–87. [DOI] [PubMed] [Google Scholar]
- 39. Locquet M, Beaudart C, Hajaoui M, Petermans J, Reginster J-Y, Bruyère O. Three-year adverse health consequences of sarcopenia in community-dwelling older adults according to 5 diagnosis definitions. J Am Med Dir Assoc 2019; 20: 43–46.e2. [DOI] [PubMed] [Google Scholar]
- 40. Fernandes LV, Paiva AEG, Silva ACBet al. . Prevalence of sarcopenia according to EWGSOP1 and EWGSOP2 in older adults and their associations with unfavorable health outcomes: a systematic review. Aging Clin Exp Res 2022; 34: 505–14. [DOI] [PubMed] [Google Scholar]
- 41. Malafarina V, Malafarina C, Biain Ugarte A, Martinez JA, Abete Goñi I, Zulet MA. Factors associated with sarcopenia and 7-year mortality in very old patients with hip fracture admitted to rehabilitation units: a pragmatic study. Nutrients 2019; 11: 2243. 10.3390/nu11092243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bianchi L, Maietti E, Abete Pet al. . Comparing EWGSOP2 and FNIH sarcopenia definitions: agreement and 3-year survival prognostic value in older hospitalized adults: the GLISTEN study. J Gerontol A Biol Sci Med Sci 2020; 75: 1331–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


