Abstract
Purpose:
GEN-1 (phIL-12-005/PPC), an IL12 plasmid formulated with polyethyleneglycol-polyethyleneimine cholesterol lipopolymer, has preclinical activity when combined with platinum-taxane intravenous chemotherapy and administered intraperitoneally in epithelial ovarian cancer (EOC) models. OVATION I was a multicenter, nonrandomized, open-label phase IB trial to evaluate the safety, preliminary antitumor activity, and immunologic response to GEN-1 in combination with neoadjuvant chemotherapy (NACT) carboplatin-paclitaxel in patients with advanced EOC.
Patients and Methods:
A total of 18 patients with newly diagnosed stage IIIC and IV EOC were enrolled. A standard 3+3 dose-escalation design tested four GEN-1 doses (36, 47, 61, 79 mg/m2) to determine the maximum tolerated dose and dose-limiting toxicities (DLTs). GEN-1 was administered in eight weekly intraperitoneal infusions starting at cycle 1 week 2 in combination with three 21-day cycles of NACT carboplatin AUC 6 and weekly paclitaxel 80 mg/m2.
Results:
The most common treatment-emergent adverse events at least possibly related were nausea, fatigue, abdominal pain/cramping, anorexia, diarrhea, and vomiting. Eight patients experience grade 4 neutropenia attributed to NACT. No DLTs occurred. A total of 14 patients were evaluable for response and 12 (85.7%) had radiological response (two complete response and 10 partial response) prior to debulking; nine were R0 at debulking and one patient had complete pathologic response. IL12 and its downstream cytokine, IFNγ, increased in peritoneal washings but not as much in blood. Increased levels of myeloid dendritic cells and T-effector memory cells in peritoneal fluid, plus elevated CD8+ T cells and reduced immunosuppression within the tumor microenvironment were found. A median time to treatment failure of 18.4 months (95% confidence interval, 9.2–24.5) was observed in the intention-to-treat population.
Conclusions:
Adding GEN-1 to standard NACT is safe, appears active, and has an impact on the tumor microenvironment.
Translational Relevance.
GEN-1 administration in patients with recurrent epithelial ovarian cancer has consistently demonstrated evidence of immunologic changes including rise in IL12, IFNγ, and TNFα levels supporting an immunostimulatory role for this gene-based IL12 therapy. These studies were limited to ascites and blood for cytokine measurement. The OVATION I study applied GEN-1 in patients undergoing neoadjuvant chemotherapy which allows for access to treatment-naïve primary tumor and posttreatment tissue to study immunologic changes in the tumor microenvironment as well as in blood and ascites. The results constitute the first systematic evaluation of cellular and cytokine changes in ascites/peritoneal washes, blood, and tumor tissue following GEN-1 treatment and provide insights into the translational mechanisms underlying GEN-1′s activity. A better understanding of the GEN-1 mechanisms of action at molecular and cellular level may help optimize GEN-1 dosing, improve treatment follow-up, and most of all, identify rational combination therapies based on novel mechanisms of action.
Introduction
Epithelial ovarian cancer (EOC) is the fifth deadliest malignancy among women in the United States (1). There are approximately 22,000 new cases of ovarian cancer every year and the majority, approximately 70% of cases, are diagnosed in advanced stages III and IV. EOC is characterized by dissemination of tumor in the peritoneal cavity with a high risk of recurrence (75%, stage III and IV) after seemingly successful surgery and chemotherapy (2). Maintenance therapy after a complete or partial remission for patients with a germline or somatic breast cancer gene (BRCA) 1/2 mutation using poly adenosine diphosphate-ribose polymerase inhibitors, olaparib or niraparib prolongs time to recurrence. These maintenance therapies have not yet demonstrated improved overall survival (3, 4). Similarly, the angiogenesis inhibitor bevacizumab improves progression-free survival (PFS) as a primary treatment in EOC without improving overall survival (5). Because the 5-year survival rates of patients with stages III and IV disease at diagnosis are poor, at 41% and 20%, respectively, there remains a need for a therapy that not only reduces the recurrence rate but also meaningfully improves overall survival (1, 6).
Immunotherapy interventions are considered promising candidates for the treatment of ovarian cancer considering the immunogenic nature of the malignancy (7). The evidence of immune activation in ovarian cancer has been demonstrated in the production of antibodies or antitumor T-cell lymphocytes in primary tumor, ascites, and blood (8–10). Presence of tumor-infiltrating cytotoxic T-cell lymphocytes has been linked to better prognosis while presence of immunosuppressive regulatory T cells (Tregs) has been associated with poor prognosis in ovarian cancer (11–13). The peritoneal cavity of patients with advanced ovarian cancer contains the primary tumor environment and is an attractive target for a regional approach to immune modulation.
Interleukin 12 (IL12) is a pluripotent cytokine associated with stimulation of innate and adaptive immune response against cancer. Clinical responses to recombinant IL12 have been observed in multiple cancers (14–16). For optimal effect, cytokines must be present over an extended period of time, which is not achievable with recombinant IL12 due to its short half-life when a single dose is administered in humans (16, 17). Toxicity is a serious dose-limiting concern with systemic exposure, leading researchers to explore alternative means of IL12 delivery (18).
GEN-1 is a gene therapy that produces safe and durable local levels of IL12 to stimulate innate and adaptive components of the immune system. The GEN-1 nanoparticle comprises a DNA plasmid encoding IL12 gene and a synthetic polymer facilitating plasmid delivery (19). Intraperitoneal (i.p.) administration of GEN-1 in patients with recurrent ovarian cancer and in preclinical models of the disease has been shown to elevate IL12 and its downstream cytokines interferon gamma (IFNγ) and tumor necrosis factor alpha (TNF-α) levels locally at tumor site for several days after a single injection and have resulted in encouraging efficacy results (20–23). In these studies, GEN-1 was well tolerated, and unlike previous studies of IL12 no dose-limiting toxicities (DLTs) were identified up to the highest evaluated dose of 36 mg/m2.
Recent preclinical and clinical studies evaluating the timing of immunotherapy suggest that the greatest opportunity for effectiveness is in the neoadjuvant setting (24). In mouse models, neoadjuvant immunotherapy generated persistent levels of tumor-specific CD8 T cells in the blood even after the mice were tumor free and throughout life (25). Furthermore, clinically, NACT has been shown to be associated with increased concentrations of CD3 and CD8 T cells, CD8 TIA-1 T cells, and CD20 B cells. Meanwhile, the immunosuppressive cells forkhead box p3 (Foxp3), indoleamine 2,3-dioxygenase-1 (IDO1), programmed cell death protein-1 (PD-1), and CD68 programmed death-ligand1 (PD-L1) macrophages remain unchanged (26).
The OVATION I study evaluated escalating doses of GEN-1 (36, 47, 61, and 79 mg/m2) in combination with a standard carboplatin/paclitaxel neoadjuvant regimen. This setting ensured the patient's immune system had not been weakened by prior therapies and maximized the potential for complementary or synergistic effects of the immune stimulator and chemotherapy. Moreover, the neoadjuvant setting allowed for collection of treatment-naïve and posttreatment primary tumor tissue at interval debulking for translational studies that was not possible in previous GEN-1 studies conducted in recurrent disease.
Patients and Methods
Study design and patient eligibility
The OVATION I study was a multi-center open-label phase IB trial that enrolled newly diagnosed patients with advanced EOC who were candidates for NACT. The study used a standard 3+3 dose-escalation design to determine the safety, biological activity, and preliminary activity of GEN-1 in combination with a standard neoadjuvant dose dense paclitaxel with triweekly carboplatin regimen. A recommended phase II dose would be based on a maximum tolerated dose (MTD) or a maximum biological activity dose.
A histologic diagnosis of epithelial ovarian, fallopian tube, or primary peritoneal carcinoma with an epithelial cell type of either: high-grade serous adenocarcinoma, endometrioid adenocarcinoma, undifferentiated carcinoma, clear cell adenocarcinoma, mixed epithelial carcinoma, or adenocarcinoma not otherwise specified (see Table 1) was required prior to enrollment. Patients were at least 18 years old, with adequate bone marrow, renal, hepatic, and neurologic functions and had to be free of active infection requiring parenteral antibiotics or a serious uncontrolled medical illness/disorder within 4 weeks of study entry. Patients were also required to have an ECOG performance score of 0, 1, or 2 and had to be free of any condition/anomaly that would interfere with the appropriate placement of the i.p. catheter for GEN-1 administration.
Table 1.
Patient characteristics (N = 18).
| Characteristics | |
|---|---|
| Age median (range) | 63.3 (48–79) |
| Race/ethnicity | |
| White, non-Hispanic | 15 (83%) |
| Black | 3 (17%) |
| FIGO | |
| IIIC | 12 (67%) |
| IV | 6 (33%) |
| Staging laparoscopy findings | |
| Omental disease | 14 (78%) |
| Carcinomatosis | 14 (78%) |
| Diaphragmatic carcinomatosis | 10 (56%) |
| Mesenteric retraction | 8 (44%) |
| Bowel infiltration | 7 (39%) |
| Stomach infiltration | 1 (6%) |
| Liver infiltration | 4 (22%) |
| Histology | |
| High-grade, serous adenocarcinoma | 17 (95%) |
| Adenocarcinoma NOS | 1 (6%) |
| Homologous recombination deficiency (HRD) | 5 (28%) |
| BRCA 1 | 1 (6%) |
| BRCA 2 | 1 (6%) |
| HRD unknown | 1 (6%) |
Patients who were treated previously with GEN-1 or with chemotherapy or radiotherapy for any tumor of the abdominal cavity or pelvis were excluded, as were patients who had received oral or parenteral corticosteroids within 2 weeks of study entry or required ongoing systemic immunosuppressive therapy. Additional exclusion criteria included active autoimmune disease requiring treatment, active hepatitis, other invasive malignancies (other than non-melanoma skin cancer), a history or evidence of central nervous system disease, and a concurrent severe medical problem unrelated to the malignancy that would expose the patient to extreme risk or decreased life expectancy.
Four centers in the United States participated in OVATION I. This study was sponsored by Celsion Corporation and registered with ClinicalTrials.gov (NCT02480374). The protocol was approved by the Institutional Review Board (IRB) or central IRB and biological safety committees of each institution, and all patients provided written informed consent before enrollment and performance of any study-related procedures. The study was conducted in compliance with the protocol, International Conference on Harmonization Good Clinical Practice Guidelines E6 (ICH-GCP), NIH Guidelines for Research Involving Recombinant DNA Molecules (April 2002) and with the Declaration of Helsinki and its amendments. The study was monitored for safety and dose escalation decisions by an independent Data Safety Monitoring Board (DSMB).
Treatment
This study evaluated four dose levels of GEN-1 (36, 47, 61, and 79 mg/m2 every week i.p. for up to 8 weeks) in combination with a standard NACT regimen, carboplatin (AUC of 6 mg/mL/min intravenously (i.v.) every 3 weeks for three cycles) and paclitaxel (80 mg/m2 every week i.v. for 9 weeks). The starting dose of 36 mg/m2 was chosen because it was the highest dose examined in a previous study combining GEN-1 with pegylated liposomal doxorubicin without evidence of DLT in patients with platinum-resistant ovarian cancer (22). Eighteen patients were enrolled, and an i.p. catheter with subcutaneous reservoir was implanted. GEN-1 dosing commenced on cycle 1 day 8 to skip administration during dexamethasone pretreatment given on cycle 1 day 1. Steroids may blunt the effects of immunotherapies such as GEN-1; therefore, concurrent administration was not permitted (27). The DSMB met to review safety data for subjects in each cohort before the next highest dosage strength was assessed. Patients had to have at least four doses of GEN-1 to be evaluated for safety at each dose level. Treated patients were planned to undergo interval debulking surgery after three cycles of NACT with weekly GEN-1 followed by three additional cycles of adjuvant chemotherapy. The dose escalation was stopped at 79 mg/m2 due to limitations in the manufacturing of additional doses. These limitations were overcome for a subsequent trial of GEN-1 currently ongoing where the starting dose has been determined to be 100 mg/m2 (28).
Assessments
Toxicities were graded according to the NCI Common Terminology Criteria for Adverse Events version 4.0 and DLTs were defined in the DSMB charter (29). Clinical endpoints included objective response rate (RECIST version 1.1), R0 resection rate, pathologic response, chemotherapy response score (CRS), and PFS per physician assessment (30–32). All enrolled patients were assessed for toxicity however patients had to complete four administrations of GEN-1 to be considered evaluable for a dose level.
Tumor, ascites, and blood samples were collected at the time of initial staging and at interval debulking surgery. Venous blood and peritoneal fluid samples (via i.p. port) were taken prior to and 24 hours after each of the first four GEN-1 treatments. Cytokine enzyme-linked immunosorbent asssays (ELISAs), flow cytometry, and IHC analyses were conducted at Roswell Park Cancer Institute (Buffalo, NY).
IHC
IHC assays and automated digital pathology analysis were performed on formalin-fixed paraffin-embedded tissue blocks. Tissue sections (4–5 μm) were prepared on slides loaded on a DAKO autostainer (Dako) and after serum-free protein block the respective primary antibodies for CD3, CD4, CD8, Foxp3, IDO1, PD-1, and PD-L1 were applied separately. The EnVision+ horseradish peroxidase system (Dako) and DAB (3,3-diaminobenzidine) chromogen were used for visualization. Slides were digitally scanned using Aperio Scanscope (Aperio Technologies, Inc.) with 20 × bright-field microscopy. These images were then accessible using Spectrum (Aperio Technologies, Inc.), a web-based digital pathology information management system. Slide images are automatically associated to a digital slide created in the Digital Slide table in Aperio eSlide Manager. Once slides are scanned, Aperio ImageScope version 11.2.0.780 (Aperio Technologies, Inc.) was used to view images for image analysis. An outline of the tumor and the size of the analysis area were defined, and the lymphocytes were counted using an optimized algorithm for each stain and results were normalized to number of lymphocytes per square millimeter.
ELISA
Cytokine levels in plasma and peritoneal fluid were measured using ELISA kits according to the manufacturer's protocol. The IL12 ELISA kit was purchased from R&D Systems and the IFNγ ELISA kit was purchased from Thermo Fisher Scientific. For peritoneal fluid or wash samples, the cytokine data were normalized with total protein concentration which was quantified with a Pierce BCA protein assay kit from Thermo Fisher Scientific. Optical Density of triplicate wells was read by BioTek Synergy HT microplate reader and concentration was determined from standard curve. The cytokine values generated from each treatment were used to generate the overall mean for each cohort.
Flow cytometry
Peripheral blood mononuclear cells and cells from peritoneal fluid were isolated by density gradient centrifugation and cryopreserved in liquid nitrogen freezer until analysis. The cells were stained with fixable viability stain 700 (BD Horizon) and incubated with FcR block (Miltenyi Biotec) followed by staining with various antibodies for T-cell phenotype (APC/H7-CD45, PerCP/Cy5.5-CD3, BUV395-CD4, BV650-CD45RA, and BV421-CCR7) and myeloid dendritic cells (mDCs; APC/H7-CD45, PE-CD11c, and BV650-CD123). The stained cells were acquired by BD Fortessa flow cytometer and analyzed using FlowJo software.
Statistical design
This study utilized a standard 3 + 3 design to identify the MTD of GEN-1 with NACT in patients with newly diagnosed EOC. Dose escalation would be considered by the DSMB after a cohort of at least three patients who received at least four doses of GEN-1 were evaluated. If no patients of three in a specific dose level demonstrated a DLT, then the study can proceed to the next higher dose level. If one of three patients demonstrated a DLT, an additional three patients were to be enrolled at that dose level. If two or more patients experience a DLT then the GEN-1 dose must be dropped to the previous level. Less than two patients of six can experience a DLT before declaring an MTD. PFS is defined as the duration of time from start of treatment (cycle 1 day 1) to time of progression or death, whichever occurs first. The data were expressed as the median value for the intention-to-treat (ITT) or per-protocol population. Resection scores were expressed as a percentage of total patients for a defined group. Translational data were tabulated as mean ± SD except for instances where average values were plotted for trend analysis and where comparisons are expressed as a percentage of baseline. Data were analyzed using Student t test. For comparison of pretreatment and posttreatment paired samples, Wilcoxon matched pairs signed-rank test was used, after checking that for most differences in cell density, the normality assumption was violated.
Results
Four centers enrolled 18 patients between September 2015 and May 2017 (ITT). Six patients did not receive the full regimen of GEN-1 treatments due to port-related infection (0 GEN-1 doses), bowel perforation (one dose of GEN-1), bowel obstruction (one dose of GEN-1), dosing delays of >21 days due to myelotoxicity (six doses of GEN-1), sepsis, and congestive heart failure (five doses of GEN-1), and altered taste (five doses of GEN-1). One patient voluntarily withdrew from GEN-1 treatment due to altered taste attributed to GEN-1. In addition, one patient died within 40 days of her first dose of chemotherapy due to complications of the ovarian cancer. As a result, 15 patients were evaluable for safety of dose (received four administrations of GEN-1). Fourteen patients underwent interval debulking and thus were evaluable for RECIST, for resection status, and pathologic response (per-protocol population). Biological samples (i.e., blood, ascites/peritoneal washes, and tumor tissue) were collected from 12 patients who received the full complement of eight doses of GEN-1 for translational data.
Safety
The DSMB reviewed the safety data at the completion of every dosing cohort which would comprise at least three patients who completed at least four doses of GEN-1. Table 2 summarizes the adverse events (AE) that were at least possibly related to GEN-1 by frequency and severity for those 15 patients treated with at least four doses of GEN-1. In general, all dose levels were well tolerated. Most AEs were grade 1 or 2 in nature. The most commonly reported AEs at least possibly attributed to GEN-1 in descending order include nausea (67%), fatigue (53%), abdominal pain/cramping (40%), anorexia (40%), diarrhea (40%), and vomiting (40%). Of the grade 3 and 4 reported AEs, the following were at least possibly attributed to GEN-1: nausea (n = 2), fatigue (n = 2), abdominal pain/cramping (n = 1), anorexia (n = 1), diarrhea (n = 2), dehydration (n = 2), vomiting (n = 1), hypokalemia (n = 1), sepsis (n = 1), and vasovagal reaction (n = 1). Hematologic toxicities were also reported as possibly being attributed to GEN-1 which were also associated with chemotherapy. There were no DLTs detected and an MTD was not reached at the doses evaluated in this study. Limiting dexamethasone premedication to cycle 1 day 1 did not result in any clinically significant hypersensitivity reactions at subsequent cycles of chemotherapy administration. A supplementary table is provided which presents all AEs for all patients (N = 18) regardless of attribution.
Table 2.
Frequency and severitya of AEs at least possibly related to GEN-1 (N = 15).
| Term | Frequency | Percentage | Grade 1–2 | Grade 3 | Grade 4 | Grade 5 |
|---|---|---|---|---|---|---|
| Nausea | 10 | 67% | 8 | 2 | 0 | 0 |
| Fatigue | 8 | 53% | 6 | 2 | 0 | 0 |
| Neutropeniab | 8 | 53% | 2 | 1 | 5 | 0 |
| Abdominal pain/cramping | 6 | 40% | 5 | 1 | 0 | 0 |
| Leukopeniab | 6 | 40% | 3 | 2 | 1 | 0 |
| Anorexia | 6 | 40% | 5 | 1 | 0 | 0 |
| Diarrhea | 6 | 40% | 4 | 2 | 0 | 0 |
| Vomiting | 6 | 40% | 5 | 1 | 0 | 0 |
| Anemiab | 6 | 40% | 2 | 4 | 0 | 0 |
| Thrombocytopeniab | 5 | 33% | 2 | 1 | 2 | 0 |
| Weakness | 5 | 33% | 5 | 0 | 0 | 0 |
| Chills | 4 | 27% | 4 | 0 | 0 | 0 |
| Fever | 4 | 27% | 4 | 0 | 0 | 0 |
| Dehydration | 3 | 20% | 1 | 2 | 0 | 0 |
| Hypomagnesemia | 3 | 20% | 3 | 0 | 0 | 0 |
| Constipation | 2 | 13% | 2 | 0 | 0 | 0 |
| Dysguesia | 2 | 13% | 2 | 0 | 0 | 0 |
| Hypokalemia | 2 | 13% | 1 | 1 | 0 | 0 |
| Alopecia | 1 | 7% | 1 | 0 | 0 | 0 |
| Creatinine increased | 1 | 7% | 1 | 0 | 0 | 0 |
| Cytokine release syndrome | 1 | 7% | 1 | 0 | 0 | 0 |
| Dizziness | 1 | 7% | 1 | 0 | 0 | 0 |
| Dyspnea | 1 | 7% | 1 | 0 | 0 | 0 |
| Elevated alkaline phosphatase | 1 | 7% | 1 | 0 | 0 | 0 |
| Elevated ALT | 1 | 7% | 1 | 0 | 0 | 0 |
| Elevated AST | 1 | 7% | 1 | 0 | 0 | 0 |
| Erythema (port site) | 1 | 7% | 1 | 0 | 0 | 0 |
| Hot flash | 1 | 7% | 1 | 0 | 0 | 0 |
| Hyperglycemia | 1 | 7% | 1 | 0 | 0 | 0 |
| Hypocalcemia | 1 | 7% | 1 | 0 | 0 | 0 |
| Nasal congestion | 1 | 7% | 1 | 0 | 0 | 0 |
| Neuropathy | 1 | 7% | 1 | 0 | 0 | 0 |
| Pain | 1 | 7% | 1 | 0 | 0 | 0 |
| Port infection | 1 | 7% | 1 | 0 | 0 | 0 |
| Sepsis | 1 | 7% | 0 | 0 | 1 | 0 |
| Sinus disorder | 1 | 7% | 1 | 0 | 0 | 0 |
| Tremor | 1 | 7% | 1 | 0 | 0 | 0 |
| Vasovagal reaction | 1 | 7% | 0 | 1 | 0 | 0 |
aCommon Terminology Criteria for Adverse Events (CTCAE) version 4.0.
bHematologic toxicities were also reported as possibly being attributed to GEN-1 which were also associated with chemotherapy.
Clinical response
All patients were evaluated for efficacy (ITT) and a per-protocol assessment was conducted for patients who underwent interval debulking. Time to treatment failure (TTF) of 18.4 months with 95% confidence interval (CI, 9.2–24.5; range, 0.1–48.4 months) was observed in the ITT population (N = 18) while a TTF of 21 months with 95% CI (11.5–33.8; range, 9.3–48.4 months) in the per-protocol population (n = 14).
Table 3 presents radiographic tumor response, surgical outcome, pathologic response, and chemotherapy response score by dose. Objective response rates to NACT/GEN-1 appeared to favor higher doses of GEN-1 between the two high- and two low-dose cohorts as calculated for RECIST-evaluable patients, with 100% of the high-dose cohorts having a complete or partial response (one CR and seven PRs) and 67% of the low-dose patients (one CR and three PRs). Patients in the high-dose cohort achieved 88% R0 resection, versus 33% in the low-dose cohorts. There was a single case of a complete pathologic response at 36 mg/m2. Similarly, pathologic response favored the higher dose cohort with 50% of subjects achieving the optimal CRS of 3 while only 17% of patients did so at the lower doses. In addition, one patient remains progression free at 4 years of follow-up.
Table 3.
Tumor response, surgical outcome, pathologic response, and chemotherapy response score with NACT/GEN-1 escalating doses.
| Cohort 1 | Cohort 2 | Cohort 3 | Cohort 4 | |||
|---|---|---|---|---|---|---|
| Radiographic response | Total (n) | 36 mg/m2 | 47 mg/m2 | 61 mg/m2 | 79 mg/m2 | |
| Tumor response | CR | 2 | 1 | 0 | 0 | 1 |
| PR | 10 | 0 | 3 | 3 | 4 | |
| SD | 2 | 2 | 0 | 0 | 0 | |
| Objective response rate | 67% | 100% | ||||
| Surgical outcome | R0 | 9 | 2 | 0 | 2 | 5 |
| R1 | 3 | 1 | 2 | 0 | 0 | |
| R2 | 2 | 0 | 1 | 1 | 0 | |
| R0 resection rate | 33% | 88% | ||||
| Pathologic response | cPR | 1 | 1 | 0 | 0 | 0 |
| Micro | 8 | 1 | 2 | 1 | 4 | |
| Macro | 5 | 1 | 1 | 2 | 1 | |
| cPR/micro rate | 60% | 63% | ||||
| Chemotherapy | CRS 3 | 5 | 1 | 0 | 2 | 2 |
| Response | CRS 2 | 5 | 2 | 1 | 0 | 2 |
| Score | CRS 1 | 4 | 0 | 2 | 1 | 1 |
| CRS 3 rate | 17% | 50% | ||||
Translational responses
GEN-1 i.p. treatment increased IL12 and IFNγ levels in ascites in a dose-response manner, as shown in Fig. 1. IL12 levels in ascites increased 3.2- and 23-fold at the lowest and highest GEN-1 doses (36 and 79 mg/m2), respectively, while IFNγ levels rose 3.1- and 67-fold. The differences in IFNγ increase between the various dose levels were statistically significant. The increase in IL12 levels followed a similar dose pattern, but the differences between various dose levels were statistically not as significant as seen with IFNγ. As expected, GEN-1 had a much smaller effect on IL12 and IFNγ expression in the blood, where both cytokines' levels increased between 1.2- and 3.1-fold (Supplementary Fig. S1). (The graphs present data from patients in RECIST-evaluable cohorts of Table 2 with one exception—a subject in the 79 mg/m2 cohort could not be assayed.)
Figure 1.
Changes in IL12 and IFNγ levels in ascites/peritoneal wash before and 24 hours after i.p. administration of GEN-1 and expressed relative to total protein in the sample (pg/mg protein). Fold changes over pretreatment values for individual samples are represented by circles and the mean for each group is represented by the solid lines. The differences between the dose groups were determined by the Student t test.
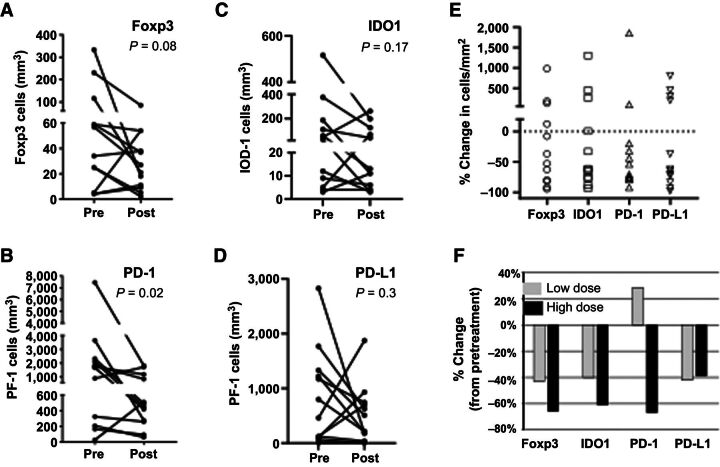
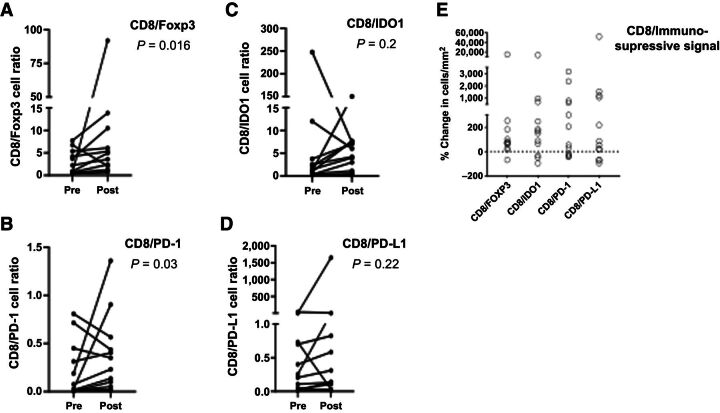
The effects of GEN-1/NACT included reductions in four immunosuppressive markers in the tumor microenvironment: Foxp3, IDO1, PD-1, and PD-L1. The pre- and posttreatment density of cells with immunosuppressive markers on an individual patient basis are shown in Fig. 2A–D, and percent changes from pretreatment values for each patient are provided in Fig. 2E. The combination regimen reduced the cell density of all four indicators of immunosuppression between the initial biopsy sample and tumor resection in the majority of patients. Reduction in Foxp3, IDO1, PD-1, and PD-L1 was observed in 67%, 67%, 83%, and 67% of patients, respectively. The range of inhibition in these patients varied from 8% to 95% (Foxp3), 33% to 94% (IDO1), 20% to 92% (PD-1), and 37% to 98% (PD-L1). Although from a small sample size, these trends are instructive since the Foxp3, IDO1, and PD-1 changes occurred generally in a GEN-1 dose-dependent manner (Fig. 2F) and are consistent with the changes in IL12 and IFNγ levels in ascites. The ratio of CD8 cells to each of the four immunosuppressive markers also increased in the majority of patients (Fig. 3A–D). The increase in CD8/Foxp3, CD8/IDO1, CD8/PD-1, and CD8/PD-L1 ratio was observed in 91%, 75%, 67%, and 75% of patients, respectively. The increase in CD8/Foxp3 and CD8/PD-1 ratio was statistically significant with P values of 0.016 and 0.03, respectively. The percent change in the ratio of CD8 cells to immunosuppressive markers is plotted in Fig 3E and demonstrating a positive shift in CD8 ratios in the majority of patients.
Figure 2.
Changes in immunosuppressive markers in the tumor microenvironment following GEN-1 and NACT treatment. Changes in Foxp3 (A), PD-1 (B), IDO1 (C), and PD-L1 (D) immune cell markers before treatment (pre) and after treatment and at debulking surgery (post) for individual patients. E, Percent changes in each of the cell types. F, Percent changes between the low-dose group (36, 47 mg/m2; n = 4) and the high-dose group (61, 79 mg/m2; n = 8). The paired comparison of pre- and posttreatment values was done by using Wilcoxon matched pairs signed-rank test.
Figure 3.
Changes in the ratio of CD8 cells to immunosuppressive markers following GEN-1 and chemotherapy treatment. A–D, Changes in the ratio of CD8 T cells to Foxp3, PD-1, IDO1, and PD-L1 markers in tumors of individual patients before treatment (pre) and after treatment and at debulking surgery (post). E, Percent change in CD8/Foxp3, CD8/PD-1, CD8/IDO1, CD8/PD-L1 ratio before (pre) and after treatment (post) for individual patients. The paired comparison of pre- and posttreatment values was done by using Wilcoxon matched pairs signed-rank test.
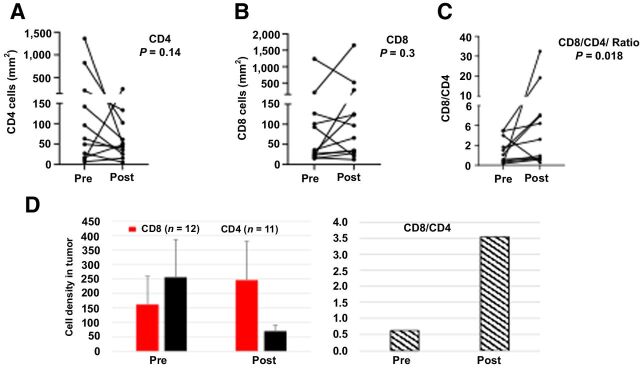
GEN-1/NACT therapy also altered the densities of CD4 and CD8 T cells in tumor specimens collected at enrollment and during debulking surgery. The pre- and posttreatment density of CD4 and CD8 cells and the CD8/CD4 cell ratio on an individual patient basis and the mean values (n = 11 for CD4 and n = 12 for CD8) are shown in Fig. 4. The CD8 cell density increased in 67% of patients, CD4 cell density decreased in 72% of patients, and the CD8/CD4 ratio increased in 82% of patients (Fig. 4A–C). These changes noted on an individual patient basis are consistent with the mean values where the CD8 T-cell density increased 53% between pre- and posttreatment versus a decline of 73% in CD4 T cells (Fig. 4D). Thus, the ratio of CD8/CD4 T cells increased 483% from 0.63 prior to GEN-1/NACT to 3.54 after. Again, these changes, although from a small sample size, are consistent with reports of an increased CD8 T-cell density after NACT (26).
Figure 4.
Changes in CD4 and CD8 cell density following GEN-1 and chemotherapy treatment. A and B, Changes in CD4 and CD8 cell density in individual patients before treatment (pre) and after treatment and at debulking surgery (post). C, CD8/CD4 cell ratio at pre- and post-treatment. D, Mean values. The paired comparison of pre- and posttreatment values was done by using Wilcoxon matched pairs signed-rank test.
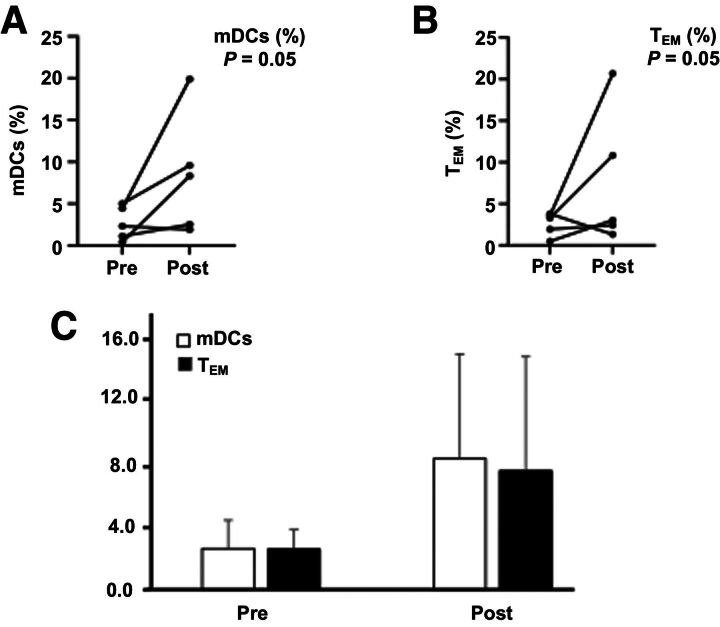
An assessment of the effects of GEN-1/NACT on immune cells in ascites found favorable trends in mDCs and effector memory T-cell (TEM) populations. The pre- and posttreatment density of mDCs and TEM cells (mDCs: CD45dump (CD3/CD56/CD19/CD14) −CD123− CD11c and TEM: CD45 CD3 CD4 CD8 CD45RA− CCR7−) on an individual patient basis are shown in Fig. 5A and B. For both mDCs and TEM, the cell density increased in four of five patients, and the percentage of total cells (mean ± SE, n = 5) increased approximately threefold in response to therapy (Fig. 5C).
Figure 5.
The effect of GEN-1 on mDCs and CD8 TEM cells in peritoneal fluid. A and B, Changes in mDCs and CD8 TEM cell density in individual patients (n = 5) before treatment (pre) and after treatment at debulking surgery (post). C, The average pre- and posttreatment data. The paired comparison of pre- and posttreatment values was done by using Wilcoxon matched pairs signed rank test.
Discussion
Escalating GEN-1 to doses up to 79 mg/m2 i.p. administered weekly for up to eight dosages was safe and reasonably tolerated when administered in combination with NACT in patients with newly diagnosed epithelial ovarian cancer. There were no dose-limiting toxicities detected and an MTD was not reached. The majority of AEs attributed to GEN-1 were low grade, and manageable. These safety findings are consistent with previous studies of GEN-1 in patients with ovarian cancer (20–22). Moreover, the OVATION I study data support that GEN-1 may be safely administered with standard NACT.
The safety profile of GEN-1 is consistent with its local administration and appears to have a distinct advantage over recombinant IL12 therapy which is associated with systemic DLT. The activity of i.p. administered GEN-1 appears to be localized to the peritoneal cavity and draining lymph nodes and potentially in the resident B cells, macrophages, and DCs (33). The increases detected in IL12 and IFNγ levels were primarily peritoneal with relatively little increases in systemic circulation resulting in this favorable safety profile.
There appears to be a suggestion of clinical activity with the addition of GEN-1 to NACT with the apparent high degree of R0 resection rates and the median times of PFS seen in the study subjects. Our population included five subjects that tested homologous-recombination deficient (Table 1) with three receiving niraparib during maintenance and a fourth was randomized to either niraparib or placebo in a subsequent clinical study. Historically, large, randomized studies of patients with EOC treated similarly with NACT have reported an R0 rate of about 50% and a median time to progression of 12 months (34, 35).
The results from our translational studies show activation of a multitude of immune responses following GEN-1 + NACT treatment. First, there was a dose-dependent increase in powerful immunostimulatory cytokines IL12 and its downstream cytokine IFNγ in ascitic fluid. The anti-cancer effects of these cytokines have been widely recognized in human malignancies (36). The dose dependence of the cytokine response to GEN-1 at a fixed NACT dose suggests that it is GEN-1 related. In addition, given the accumulation of the IL12 plasmid in mesenteric lymph nodes in an animal model, it is likely that GEN-1 had a similar effect on the stimulatory cytokines in those key secondary lymphoid organs where ovarian metastases commonly occur. Second, the proportion of myeloid DCs in the peritoneal fluid trended higher, by 3.1-fold, accompanied by a similar 3.0-fold rise in CD8 TEM cells. Such concomitant changes in these cell types is noteworthy, given the important role of antigen-presenting cells in stimulating a cytotoxic T-cell response and fostering immunological memory. Third, GEN-1 appeared to reduce four immunosuppressive signals (Foxp3, IDO1, PD-1, and PD-L1) within the tumor microenvironment, a trend not seen with NACT therapy (9–13).
Finally, the GEN-1 gene therapy was associated with an apparent increase in the cytotoxic state of T cells within the tumor microenvironment as indicated by the increases in the ratios of CD8/CD4 and CD8/Tregs. Indeed, higher CD8/CD4 T cell and CD8/Treg ratios have been considered prognostic for prolonged survival (12, 13, 37). The OVATION I study results are consistent with the known activities of IL12 and its related downstream cytokines IFNγ including a reduction in the production of IL2 which is required for proliferation of immunosuppressive Tregs. As such, these cytokines render ovarian cancer cells more sensitive to platinum chemotherapy by inhibiting cancer-associated fibroblasts' production of glutathione and cysteine, and conversion of tumor-associated macrophages from the immunosuppressive M2 to the antitumor M1 phenotype (38–40).
The immune changes resulting from GEN-1 + NACT treatment are distinct from those reported with NACT therapy in epithelial ovarian cancer. First, the intraepithelial CD4 and CD8 T-cell densities following NACT increased or remained unchanged, and the CD8/CD4 ratio remain unchanged (13, 26, 41, 42). In comparison, our study shows an increase in CD8 cell density, decrease in CD4 cell density, and increase in CD8/CD4 ratio in the majority of patients, although the magnitude of the increase highly varied from patient to patient. These data suggest that the addition of GEN-1 to NACT produces a different pattern of immune response that is not typically associated with the NACT alone. Second, the NACT increased or produced no change in immunosuppressive markers (13, 26, 41, 42). In one of the studies, NACT produced a doubling of CD8 cell density but failed to relieve the immunosuppression markers including Foxp3, IDO1, PD-1, PD-L1 in tumor tissue (26). In another study, NACT-treated tumors had higher PD-L1 expression on tumor-infiltrating immune cells and persistent high levels of PD-1–expressing and CTLA-4–expressing cells (41). In a separate study, NACT therapy increased tumor infiltrating lymphocytes but did not affect Foxp3 cells (13). In another study, NACT increased PD-L1–positive cells from 30% to 53% (42). These studies consistently demonstrate an increase or no change in the immunosuppressive signals following NACT in advanced epithelial ovarian cancer. In comparison, the current study demonstrates a reduction in Foxp3, IDO1, PD-1, and PD-L1 signals and an increase in the ratio of CD8 cells to Foxp3, IDO1, PD-1, and PD-L1 cells in the majority of patients suggesting GEN-1 may have a role in the observed immune changes in NACT combination setting. A decrease in immunosuppressive markers in this study is consistent with the inhibitory action of IL12 on PD-1 expression in malignant melanoma and peripheral lymphocytes and on Foxp3 and other Tregs in lymphocyte cultures (43–45).
A parallel increase in IFNγ and decrease in PD-1/PD-L1 after GEN-1/NACT therapy is interesting because an increase in IFNγ has been associated with upregulation of PD-1/PD-L1 expression in the action of some immunotherapy agents (46). The mechanism of a parallel increase in IFNγ and inhibition of immunosuppressive markers following GEN-1 treatment in the current study warrants further investigation. However, there is some evidence in the literature to suggest that these parallel effects could be explained by dual action of IL12 on immune cells. IL12 increases IL2 receptor expression on CD4 and CD8 cells to produce IFNγ but diminishes its expression on immunosuppressive T cells resulting in the starvation of immunosuppressive T cells thereby favoring the outgrowth of non-Tregs (45). In another study, IL12-stimulated IFNγ production from CD8 cells and countered IFNγ-mediated PD-L1 expression by downregulating IFNγ receptors (47). The stimulation of IFNγ and inhibition of immunosuppressive markers in our study may be explained by dual actions of IL12 involving IFNγ-independent mechanisms (48).
The multifactorial nature of GEN-1 immune response built on a durable local production of IL12 may be activating the innate and adaptive immune system creating a unique tumor microenvironment potentially favorable to antitumor responses and also conducive to other therapeutic drugs that may be suboptimal as single agents due to highly immunosuppressive tumor microenvironment in ovarian cancer. For example, checkpoint inhibitors despite having demonstrated activity in some cancer types are only of limited to modestly active in ovarian cancer (49, 50). Combination with GEN-1 could potentiate CD8 T-cell infiltration and reduce immunosuppressive tumor microenvironment to improve the efficacy of checkpoint inhibitors and produce an overall better quality of clinical response against cancer. Similarly, the efficacy of adaptive T-cell therapies may also be improved by remodeling the peritoneal cavity with GEN-1 pre-treatment reducing the tumor immunosuppressive environment and improving the T-cell survival and clinical efficacy. Similarly, other novel combinations with GEN-1 may also be investigated to improve clinical outcome in ovarian cancer.
This study was limited by its small sample size and termination of dose escalation at 79 mg/m2 even though an MTD was not achieved. A maximum biological dose was not established as well. Another limitation is that a control arm was not employed to evaluate the full impact of GEN-1 on the immune response as well as therapeutic response when GEN-1 is combined with chemotherapy. Future studies will evaluate GEN-1 at higher doses in this patient population with a control group to address these limitations.
In conclusion, weekly i.p. GEN-1 treatment in conjunction with standard NACT in advanced epithelial ovarian cancer patients is safe, well tolerated, and appears to be active. Repeated durable increases in lL12 and IFNγ levels at tumor site for an 8-week treatment period provides for an unprecedented pharmacology remodeling of the tumor microenvironment as evidenced by reduction in immunosuppressive signals Foxp3, IDO1, PD-1, and PD-L1 and potentiation of immunostimulatory signals including the increases in the ratios of CD8/CD4 and CD8/Tregs and increases in mDCs and CD8 TEM cells. These immunomodulatory effects of GEN-1 may result in an increased sensitivity of tumor microenvironment to other anti-cancer agents including cytotoxic drugs and immunotherapies such as checkpoint inhibitors and adaptive T-cell therapies. OVATION II (NCT03393884) is a phase I/II study of concurrent GEN-1 at a dose of 100 mg/m2 weekly for up to 17 doses administered during chemotherapy and is currently actively accruing.
Authors' Disclosures
P.H. Thaker reports personal fees and other support from Celsion during the conduct of the study; personal fees from Aravive, Novocure, Iovance, AstraZeneca, and Mana Therapeutics; grants and personal fees from Merck, Tesaro/GlaxoSmithKline outside the submitted work. C.A. Leath reports personal fees from Celsion during the conduct of the study; grants from NIH; personal fees from Clovis Oncology, AbbVie, GlaxoSmithKline; and other support from AbbVie outside the submitted work. C. Gunderson Jackson reports personal fees from GlaxoSmithKline; grants from Clovis, Genentech, and Eli Lilly outside the submitted work. N. Borys reports other support from Celsion Corporation during the conduct of the study. K. Anwer reports other support from Celsion Corporation during the conduct of the study. L. Musso reports other support from Celsion Corporation during the conduct of the study. J. Matsuzaki reports other support from Celsion during the conduct of the study. W. Bshara reports other support from Celsion during the conduct of the study. K. Odunsi is co-founder of Tactiva Therapeutics and received research funding from AstraZeneca and Tessaro. No disclosures were reported by the other authors.
Supplementary Material
Adverse Events by Body System and Grade
Changes in IL-12 and IFN-γ levels in blood samples
Acknowledgments
This work was partially conducted at Roswell Park's Pathology Network and Immune Analysis Shared Resources, P30CA016056. This study was funded by Celsion Corporation, Lawrenceville, NJ.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
Footnotes
Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/).
Authors' Contributions
P.H. Thaker: Conceptualization, data curation, supervision, investigation, visualization, methodology, writing–original draft, writing–review and editing. W.H. Bradley: Conceptualization, investigation, methodology, writing–review and editing. C.A. Leath III: Conceptualization, formal analysis, investigation, methodology, writing–original draft, writing–review and editing. C. Gunderson Jackson: Investigation, writing–review and editing. N. Borys: Conceptualization, resources, data curation, formal analysis, supervision, funding acquisition, validation, methodology, writing–original draft, project administration, writing–review and editing. K. Anwer: Conceptualization, resources, data curation, formal analysis, supervision, funding acquisition, validation, visualization, methodology, writing–original draft, project administration, writing–review and editing. L. Musso: Data curation, software, formal analysis, validation, investigation, visualization, methodology, writing–original draft, project administration, writing–review and editing. J. Matsuzaki: Data curation, software, formal analysis, validation, investigation, visualization, methodology. W. Bshara: Resources, data curation, formal analysis, validation, investigation, visualization, writing–review and editing. K. Odunsi: Conceptualization, data curation, formal analysis, supervision, validation, investigation, visualization, methodology, writing–review and editing. R.D. Alvarez: Conceptualization, writing–original draft, writing–review and editing.
References
- 1. Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. . SEER Cancer Statistics Review, 1975–2017, Bethesda, MD: NCI. Available from: https://seer.cancer.gov/csr/1975_2017. [Google Scholar]
- 2. du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials. Cancer 2009;115:1234–44. [DOI] [PubMed] [Google Scholar]
- 3. Moore KN, Colombo N, Scambia G, Kim B-G, Oaknin A, Friedlander M, et al. Maintenance olaparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med 2018;379:2495–505. [DOI] [PubMed] [Google Scholar]
- 4. Gonzalez-Martin A, Pothuri B, Vergote I, Christensen RD, Greybill W, Mirza MR, et al. Niraparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med 2019;381:2391–402. [DOI] [PubMed] [Google Scholar]
- 5. Tewari KS, Burger RA, Enserro D, Norquist BM, Swisher EM, Brady MF, et al. Final overall survival of a randomized trial of bevacizumab for primary treatment of ovarian cancer. J Clin Oncol 2019;37:2317–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Siegel RL, DeSantis C, Virgo KS, Stein K, Mariotto AB, Smith T, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin 2012;62:220–41. [DOI] [PubMed] [Google Scholar]
- 7. Ghisoni E, Imbimbo M, Zimmermann S, Valabrega G. Ovarian cancer immunotherapy: turning up the heat. Int J Mol Sci 2019;20:2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fortner RT, Damms-Machado A, Kaaks R. Systematic review: tumor-associated antigen autoantibodies and ovarian cancer early detection. Gynecol Oncol 2017;147:465–80. [DOI] [PubMed] [Google Scholar]
- 9. Singh M, Loftus T, Webb E, Benencia F. Minireview: regulatory T cells and ovarian cancer. Immunol Invest 2016;45:712–20. [DOI] [PubMed] [Google Scholar]
- 10. Odunsi K. Immunotherapy in ovarian cancer. Ann Oncol 2017;28:viii1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Toker A, Nguyen LT, Stone SC, Yang SYC, Katz SR, Shaw P, et al. Regulatory T cells in ovarian cancer are characterized by a highly activated phenotype distinct from that in melanoma. Clin Cancer Res 2018;24:5685–96. [DOI] [PubMed] [Google Scholar]
- 12. Curiel TJ, Coukos G, Zhou L. Specific recruitment of regulatory T-cells in ovarian carcinoma foster immune privilege and predicts reduced survival. Nat Med 2004;10:942–7. [DOI] [PubMed] [Google Scholar]
- 13. Polcher M, Braun M, Friedrichs N. Foxp3(+) cell infiltration and granzyme B(+)/Foxp3(+) cell ratio are associated with outcome in neoadjuvant chemotherapy-treated ovarian carcinoma. Cancer Immunol Immunother 2010;59:909–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lu X. Impact of IL-12 in cancer. Curr Cancer Drug Targets 2017;17:682–97. [DOI] [PubMed] [Google Scholar]
- 15. Tugues S, Burkhard SH, Ohs I. New insights into IL-12 mediated tumor suppression. Cell Death Differ 2015;22:237–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lenzi R, Rosenblum MG, Verschraegen CF, Kudelka AP, Kavanagh JJ, Hicks ME, et al. Phase I study of intraperitoneal recombinant human interleukin 12 in patients with müllerian carcinoma, gastrointestinal primary malignancies, and mesothelioma. Clin Cancer Res 2002;8:3686–95. [PubMed] [Google Scholar]
- 17. Bajetta E, Del Vecchio M, Mortarini R, Nadeau R, Rakhit A, Rimassa L, Fowst C, et al. Pilot study of subcutaneous recombinant human interleukin 12 in metastatic melanoma. Clin Cancer Res 1998;4:75–85. [PubMed] [Google Scholar]
- 18. Marshall E. Cancer trial of interleukin-12 halted. Science 1995;2681555. [Google Scholar]
- 19. Fewell JG, Matar M, Slobodkin G, Han S-o, Rice J, Hovanes B, et al. Synthesis and application of a non-viral gene delivery system for immunogene therapy of cancer. J Control Release 2005;109:288–98. [DOI] [PubMed] [Google Scholar]
- 20. Anwer K, Barnes MN, Fewell JG, Lewis DH, Alvarez RD. Phase-I clinical trial of IL-12 plasmid/lipopolymer complexes for the treatment of recurrent ovarian cancer. Gene Ther 2010;17:360–9. [DOI] [PubMed] [Google Scholar]
- 21. Anwer K, Kelly FJ, Chu CS, Fewell JG, Lewis DH, Alvarez RD. Phase I trial of a formulated IL-12 plasmid in combination with carboplatin and docetaxel chemotherapy in the treatment of platinum-sensitive recurrent ovarian cancer. Gynecol Oncol 2013;131:169–73. [DOI] [PubMed] [Google Scholar]
- 22. Thaker PH, Brady WE, Lankes HA, Odunsi K, Bradley WH, Moore KN, et al. A phase I trial of intraperitoneal GEN-1, an IL-12 plasmid formulated with PEG-PEI-cholesterol lipopolymer, administered with pegylated liposomal doxorubicin in patients with recurrent or persistent epithelial ovarian, fallopian tube or primary peritoneal cancers: an NRG Oncology/Gynecologic Oncology Group study. Gynecol Oncol 2017;147:283–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thaker PH, Borys N, Fewell JG, Anwer K. GEN-1 immunotherapy for the treatment of ovarian cancer. Future Oncol 2019;15:421–38. [DOI] [PubMed] [Google Scholar]
- 24. O'Donnell JS, Hoefsmit EP, Smyth MJ, Blank CU, Teng MWL. The promise of neoadjuvant immunotherapy and surgery for cancer treatment. Clin Cancer Res 2019;25:5743–51. [DOI] [PubMed] [Google Scholar]
- 25. Liu J, Blake SJ, Yong MC, Harjunpaa H, Ngiow SF, Takeda K. Improved efficacy of neoadjuvant compared to adjuvant immunotherapy to eradicate metastatic disease. Cancer Discov 2016;6:1382–99. [DOI] [PubMed] [Google Scholar]
- 26. Lo CS, Sanii S, Kroeger DR, Milne K, Talhouk A, Chiu DS, et al. Neoadjuvant chemotherapy of ovarian cancer results in three patterns of tumor-infiltrating lymphocyte response with distinct implications for immunotherapy. Clin Cancer Res 2017;23:925–34. [DOI] [PubMed] [Google Scholar]
- 27. Meriggi F, Zaniboni A. Antibiotics and steroids, the double enemies of anticancer immunotherapy: a review of the literature. Cancer Immunol Immunother 2021;70:1511–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thaker PH, Holloway RW, Kuroki L, DePasquale SE, Bradley W, ElNagger A, et al. A phase I/II study evaluating intraperitoneal GEN-1 in combination with neoadjuvant chemotherapy in patients with newly diagnosed advanced epithelial ovarian cancer (EOC) [abstract]. In: Proceedings of the SGO 2021 Virtual Annual Meeting on Women's Cancer, Virtual; 2021. [Google Scholar]
- 29. Common Terminology Criteria for Adverse Events (CTCAE): Version 4.0. Available from: http://www.acrin.org/Portals/0/Administration/Regulatory/CTCAE_4.02_2009–09–15_QuickReference_5x7.pdf.
- 30. Rustin GJS, Vergote I, Eisenhauer EA, Pujade-Lauraine E, Quinn M, Thigpen T, et al. Definitions for response and progression in ovarian cancer clinical trials incorporating RECIST 1.1 and CA 125 agreed by the Gynecological Cancer Intergroup (GCIG). Int J Gynecol Cancer 2011;21:419–23. [DOI] [PubMed] [Google Scholar]
- 31. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. [DOI] [PubMed] [Google Scholar]
- 32. Cohen PA, Cohen PA, Powell A, Böhm S, Gilks CB, Stewart CJ, et al. Pathological chemotherapy response score is prognostic in tubo-ovarian high-grade serous carcinoma: a systematic review and meta-analysis of individual patient data. Gynecol Oncol 2019;154:441–8. [DOI] [PubMed] [Google Scholar]
- 33. Brunhoeber E, Matar M, Anwer K, Fewell JG. Biodistribution and cearance following intraperitoneal injection of murine interleukin-12 plasmid formulated with a novel polymeric delivery system. Mol Ther 2006;13:S109. [Google Scholar]
- 34. Kehoe S, Hook J, Nankivell M, Jayson GC, Kitchener HC, Lopes T, et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomised, controlled, non-inferiority trial. Lancet 2015;386:249–57. [DOI] [PubMed] [Google Scholar]
- 35. Vergote I, Tropé CG, Amant F, Ehlen T, Reed N, Casado A. Neoadjuvant chemotherapy is the better treatment option in some patients with stage IIIc to IV ovarian cancer. J Clin Oncol 2011;29:4076–8. [DOI] [PubMed] [Google Scholar]
- 36. Conlon KC, Miljkovic MD, Waldmann TA. Cytokines in the treatment of cancer. J Interferon Cytokine Res 2019;39:6–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sato E, Olson SH, Ahn J, Bundy BN, Nishikawa H, Qian F, et al. Intraepithelial CD8+ tumor-infiltrating lymphocytes and a high CD8+/regulatory T cell ratio are associated with favorable prognosis in ovarian cancer. Proc Natl Acad Sci U S A 2005;102:18538–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cao X, Leonard K, Collins LI, Cai SF, Mayer JC, Payton JE, et al. Interleukin 12 stimulates IFN-γ–mediated inhibition of tumor-induced regulatory T-cell proliferation and enhances tumor clearance. Cancer Res 2009;69:8700–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wang W, Kryczek I, Dostal L, Lin H, Tan L, Zhao L, et al. Effector T cells abrogate stroma-mediated chemoresistance in ovarian cancer. Cell 2016;165:1092–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Watkins SK, Egilmez NK, Suttles J, Stout RD. IL-12 rapidly alters the functional profile of tumor-associated and tumor-infiltrating macrophages in vitro and in vivo. J Immunol 2007;178:1357–62. [DOI] [PubMed] [Google Scholar]
- 41. Bohm S, Montfort A, Pearce OM, Topping J, Chakravarty P, Everitt GL, et al. Neoadjuvant chemotherapy modulates the immune microenvironment in metastases of tubo-ovarian high-grade serous carcinoma. Clin Cancer Res 2016;22:3025–36. [DOI] [PubMed] [Google Scholar]
- 42. Mesnage SJ, Auguste A, Genestie C, Dunant A, Pain E, Drusch F, et al. Neoadjuvant chemotherapy (NACT) increases immune infiltration and programmed death-ligand 1 (PD-L1) expression in epithelial ovarian cancer (EOC). Ann Oncol 2016;28:651–7. [DOI] [PubMed] [Google Scholar]
- 43. Liu Y, Xy H, Lai N, Yang Z, Kang S. Interleukin-12 over-espressionin malignant melanoma B16 cells reduces programmed death-1 expression on T cells in mice with immune reconstitution. Nan Fang Yi Ke Da Xue Xue Bao 2020;40:856–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Costa SF, Gomes VO, dos Santos Maciel MO, Melo LM, Venturin GL, Bragato JP. Combined in vitro IL-12 and IL-15 stimulation promotes cellular immune resonse in dogs with visceral leishmaniasis. PLoS Negl Trop Dis 2020;14:e0008021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhao J, Zhao J, Perlman S. Differential effects of IL-12 on Tregs and non-Treg cells: roles of IFN-g, IL-2 and IL-2R. PLoS One 2012;7:e46241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lai Q, Wang H, Li A, Xu Y, Tang L, Chen Q, et al. Decitibine improve the efficiency of anti-PD-1 therapy via activating the response to IFN/PD-L1 signal of lung cancer cells. Oncogene 2018;37:2302–12. [DOI] [PubMed] [Google Scholar]
- 47. Lin L, Rayman P, Pavicic PG, Tannenbaum C, Hamilton T, Montero A. Ex vivo conditioning with IL-12 protects tumor infiltrating CD8+T cells from negative regulation by local IFN-γ. Cancer Immunol Immunother 2019;68:395–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Eisenring M, vom Berg J, Kristiansen G, Saller E, Becher B. IL-12 initiates tumor rejection via lymphoid tissue-inducer cells bearing the natural cytotoxicity receptor NKp46. Nat Immunol 2010;11:1030–8. [DOI] [PubMed] [Google Scholar]
- 49. Moore KN, Bookman M, Sehouli J, Miller A, Anderson C, Scambia G, et al. Atezolizumab, bevacizumab, and chemotherapy for newly diagnosed stage III or IV ovarian cancer: placebo-controlled randomized phase III trial (IMagyn050/GOG 3015/ENGOT-OV39). J Clin Oncol 2021;39:1842–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. González-Martín A, Sánchez-Lorenzo L. Immunotherapy with checkpoint inhibitors in patients with ovarian cancer: still promising? Cancer 2019;125:4616–22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Adverse Events by Body System and Grade
Changes in IL-12 and IFN-γ levels in blood samples