Abstract
While the negative effects of Coronavirus Disease-2019 (COVID-19) on general mental health are well-established, less is known about the impact on those with severe mental illness. Thus, this study examined symptom severity among psychiatric inpatients admitted prior to versus during the COVID pandemic. Self-reported anxiety (GAD-7), depression (PHQ-9), emotional dysregulation (DERS-SF), sleep quality (PSQI), nightmares (DDNSI), and suicidal ideation (SBQ-R) were examined in 470 adults (n = 235 admitted pre-pandemic) and 142 children and adolescents (n = 65 admitted pre-pandemic) at admission. Adults also completed measures of disability (WHODAS) and substance use (WHOASSIST). Adults admitted during the COVID pandemic reported significantly higher levels of anxiety [p < .001, partial η2=0.18], depression [p < .001, partial η2=0.06], emotion dysregulation [p < .001, partial η2=0.05], nightmares [p = .013, partial η2=0.01], and disability [p < .001, partial η2=0.04] compared to adults admitted pre-COVID. Levels of anxiety [p = .005, partial η2=0.05], depression [p = .005, partial η2=0.06], and sleep quality [p = .011, partial η2=0.05] were significantly higher among adolescents admitted during COVID compared to pre-COVID. The findings help identify areas of prioritization for future mental health prevention/intervention efforts for future disease outbreaks.
Keywords: COVID-19, Inpatient, Psychiatry, Adolescent, Adult, Mental health
1. Introduction
“The frequency of mental disturbances accompanying the acute illness in the epidemic has been the subject of frequent comment, and the wave of psychiatric material that followed in its wake was unexpectedly large and correspondingly interesting.”
-Dr. KarlMenninger, 1919(Menninger, 1919)
In 1919, Dr. Karl Menninger was the first to examine the mental health impact of a pandemic: one hundred cases of ‘mental illness’ that he hypothesized were related to individuals contracting the influenza virus (Menninger, 1919). Dr. Menninger's groundbreaking research quantitively described the relationship between the influenza H1N1 virus and psychosis, as well as examined the differences between groups with and without preexisting psychiatric illness (e.g., alcohol use, paranoia). Since Dr. Menninger's seminal research, numerous studies have investigated the mental health effects of numerous outbreaks.
Most studies of psychiatric illness during a pandemic look beyond the mental health symptoms related to direct viral infections and examine the mental health toll of pandemic-related stress events among those who are not infected. Results have indicated that these disease outbreaks are associated with broad deterioration of mental health (Ko et al., 2006; Lau et al., 2005; Reardon, 2015), psychological distress (Cenat et al., 2020; Douglas et al., 2009; Lau et al., 2005), a higher prevalence of sleep problems (Cenat et al., 2020; Lau et al., 2005) and substance use (Cenat et al., 2020; Lau et al., 2005), an increase in suicide rates (Cenat et al., 2020; Cheung et al., 2008), an increase in anxiety (Cenat et al., 2020; Jalloh et al., 2018; Jeong et al., 2016; Lau et al., 2005) and depressive symptoms (Cenat et al., 2020; Jalloh et al., 2018; Ko et al., 2006; Lau et al., 2005), and an overall need for psychiatric services due to a surge of psychiatric illness (Cenat et al., 2020; Douglas et al., 2009; Jalloh et al., 2018; Lau et al., 2005; Mak et al., 2009).
The World Health Organization (WHO) declared COVID-19 a pandemic in March of 2020 after the rapid outbreak of this novel virus (WHO, 2020). The novelty and severity of COVID-19 led to rapid global shutdowns and restrictions including city-wide lockdowns, social distancing, and business closures to prevent the spread of the virus. These events significantly altered each person's personal freedom and autonomy, financial security, social stability, and individual lifestyle (Ammar et al., 2020). Taken individually, each of these changes and stressors can have a negative impact on general mental health. Studies have shown an overall increase in prevalence of current mental health disorders in the context of COVID-19 (Czeisler et al., 2020; Winkler et al., 2020).
Those with preexisting mental health conditions may be particularly vulnerable to these effects because they are more susceptible to experiencing high levels of stress during a crisis (Jankowski and Hamblen, 2019) and are more likely to experience isolation/despair during confinement compared to the general population (Muruganandam et al., 2020). There is substantial heterogeneity in the literature regarding the effect of the COVID-19 pandemic on people with pre-existing psychiatric disorders with some studies reporting no evidence of worsening of symptoms (Chakraborty et al., 2020; Robinson et al., 2022). However, most research reports that since the beginning of COVID-19, adults with preexisting psychiatric illness also have presented with higher rates of sleep problems (Franchini et al., 2020; Hao et al., 2020; Muruganandam et al., 2020; Van Rheenen et al., 2020), stress and anxiety (Blithikioti et al., 2021; Carmassi et al., 2020; Rogers et al., 2021), depression (Blithikioti et al., 2021; Ma et al., 2020), substance misuse (Chappuy et al., 2021; Columb et al., 2020; Bar-Or et al., 2021; Muruganandam et al., 2020; Van Rheenen et al., 2020), behavioral addiction (e.g., gambling) (Chappuy et al., 2021; Columb et al., 2020; Bar-Or et al., 2021), anger and impulsivity (Hao et al., 2020; Muruganandam et al., 2020), suicidal ideation (Hao et al., 2020; Muruganandam et al., 2020; Van Rheenen et al., 2020), and physical problems (Franchini et al., 2020; Hao et al., 2020). In addition, the pandemic has decreased access to mental health care and presented additional barriers to complying with treatment, further heightening the risk of exacerbation of preexisting symptoms and/or relapse (Muruganandam et al., 2020).
Children and adolescents are similarly vulnerable to the disruptions of the COVID-19 pandemic, which have included changes in their routine, closing of schools, virtual learning, media exposure, social isolation, and intrafamilial conflicts – all of which have had demonstrable consequences to youth mental health (Singh et al., 2020). Youth are also at a particularly heightened risk for the psychological effects of COVID-19 due to their developmental stage (Lamblin et al., 2017). The pandemic has been associated with increased youth depression and anxiety symptoms (Duan et al., 2020; Ma et al., 2021; Magson et al., 2020; Racine et al., 2021; Xie et al., 2020; Zhou et al., 2020), increased rates of suicide ideation and attempts (Hill et al., 2021), increased sleep problems (Ma et al., 2021), increased presentation of posttraumatic stress symptoms (Ma et al., 2021)), significant sleep problems (Ravens-Sieberer et al., 2021), an increase in emotion regulation problems (Amoros-Reche et al., 2022; Ravens-Sieberer et al., 2021) and a significant decrease in life satisfaction (Magson et al., 2020). Parents also report their children are experiencing significantly increased irritability, worry, sleep disorders, fatigue, and agitation coinciding with COVID-19 (Jiao et al., 2020). As with adults, children and adolescents with preexisting mental health problems are at particularly high risk (Fegert et al., 2020); however, studies examining the effect of COVID-19 on this subgroup are limited. For youth with preexisting psychiatric illness, the COVID-19 pandemic confers numerous additional challenges, including lack of continued access to mental health services and the potential for added stress to further exacerbate symptoms (Fegert et al., 2020; Guessoum et al., 2020; Lee, 2020). A survey of UK adolescents with existing mental health difficulties found that 83% of respondents agreed the COVID-19 pandemic had worsened their mental health. In fact, 26% reported they were no longer even able to access mental health support (YoungMiNDS, 2020).
To better understand how COVID-19 has impacted those at high risk for the exacerbation of mental health symptoms – those with preexisting psychiatric illness – we examined the differences in symptom severity across youth and adults when admitted to an inpatient psychiatric hospital in the United States prior to the COVID-19 pandemic (both admission and discharge prior to December 31st, 2019) and during the COVID-19 pandemic (admission after March 11, 2020). In line with prior research, we hypothesized that adolescents between the ages of 12 to 17 and adults admitted during the COVID-19 pandemic would demonstrate significantly higher symptom severity than patients admitting prior to the COVID-19 pandemic. Specifically, we predicted that both adult and adolescent patients being admitted during COVID-19 would report significantly worse anxiety, depression, problems with emotional regulation, nightmares, nighttime sleep quality, suicide risk, and disability at admission relative to patients admitted prior to the COVID-19 pandemic.
2. Method
Admission after March 11th, 2020, was used for membership in the during pandemic group, as this was the date that COVID-19 was declared a global pandemic by the World Health Organization. Admission and discharge before December 31st, 2019, were used as the pre-pandemic control, as this was the date a cluster of pneumonia cases was first reported to the World Health Organization in China.
2.1. Participants
Adults. The present study included 470 adults admitted to an inpatient psychiatric hospital in Houston, Texas who were between 18 and 79 years of age (M = 34.86, SD = 15.30), half who were admitted pre-pandemic (n = 235) and half who were admitted during the COVID-19 pandemic (n = 235). The majority of participants (56.0%, n = 263) were male, and a large majority (85.7%) were Caucasian. The greatest number of participants reported completing some college (38.5%), followed by a Bachelor's degree (29.2%), and a graduate degree (20.7%). The average length of stay for the adult pre-pandemic (M = 37.74, SD = 16.21) and during-pandemic (M = 35.79, SD = 17.13) sample was 36.14 days and there was not a significant difference between groups (p = .205). In the present sample, 321 patients (69.9%) reported no previous suicide attempts while 138 (30.1%) reported at least one prior attempt. For those patients reporting a previous attempt, the number of lifetime suicide attempts ranged from one to 24 (M = 3.19, SD = 4.08). Participants in the sample also indicated preexisting mental health history, including an extensive treatment history, reporting several previous therapists (M = 4.17, SD = 12.10) and psychiatrists (M = 3.40, SD = 3.66). Similarly, just over half indicated a previous acute hospital admission (n = 240, 51.0%), and just less than half reported an extended admission (n = 216, 46.6%). Diagnostic information from the SCID was available for 392 adults (83.4%). Of those participants, 156 adults met the criteria for MDD, 74 met the criteria for GAD, 27 met the criteria for Bipolar, and 60 met the criteria for PTSD.
Youth. The present study included 142 adolescents admitting to an inpatient psychiatric hospital in Houston, Texas who were between 12 and 17 years of age (M = 15.10, SD = 1.49), about half of who were admitted pre-pandemic (n = 65) and half of who were admitted during the COVID-19 pandemic (n = 77). Most participants (77.5%, n = 110) were female, and a large majority (86.7%) were Caucasian. The average length of stay for the adolescent pre-pandemic (M = 22.95, SD = 9.41) and during-pandemic (M = 22.83, SD = 7.37) sample was 22.89 days and there was not a significant difference between groups (p = .934). In the present sample, 62 patients (44.9%) reported no previous suicide attempts while 76 (55.1%) reported at least one prior attempt. For those patients reporting a previous attempt, the number of lifetime suicide attempts ranged from one to 13 (M = 2.59, SD = 2.19). Adolescents in the sample also indicated preexisting mental health history, reporting previous therapists (M = 2.76, SD = 1.57) and psychiatrists (M = 1.88, SD = 1.50). Diagnostic information from the KSADS was available for 115 adolescents (81.0%). Of those participants, 19 adolescents met the criteria for MDD, 48 met the criteria for GAD, 34 met the criteria for ADHD, and 27 met the criteria for PTSD.
2.2. Procedures
As part of clinical standard of care, adults and adolescents admitted to the inpatient psychiatric programs completed a clinical outcomes battery as part of their admission. These outcome measures were administered through computer-based HIPAA-compliant survey software and an iPad. The admission clinical outcomes battery assesses anxiety, depression, emotion regulation problems, disability, substance use, sleep, and suicide ideation, among other constructs. Adolescent patients did not complete the substance use and disability questionnaires. Those measures are not included in the current adolescent outcomes battery as the substance use assessment has only been validated with adults (Gryczynski et al., 2015) and the disability assessment is not recommended for use in subjects below the age of 18 years (Ustun et al., 2010). Approximately 5% of the patients admitted to the inpatient psychiatric programs were unable to complete these outcome measures at admission due to various reasons (e.g., psychosis, refusal, etc.). Clinical outcomes data were retrospectively extracted and de-identified to examine symptom differences. This study was approved by the Institutional Review Board at Baylor College of Medicine.
2.3. Measures
2.3.1. Clinical outcomes
The Generalized Anxiety Disorder Scale (GAD-7) is a 7-item self-report measure evaluating symptoms and severity of anxiety (Spitzer et al., 2006). Items in the GAD-7 include “not being able to stop or control worrying”, “trouble relaxing,” and “feeling afraid as if something awful might happen.” Participants rated these items on a scale of 0 to 3, with 0 equaling “not at all” and 3 being “nearly every day.” There is a strong association between increasing GAD-7 scores and worsening functional impairment. Research has shown that the GAD-7 is both valid and reliable as a screening method and in assessing anxiety severity in clinical practice and research (Lowe et al., 2008). Adult and adolescent patients complete this assessment at admission.
The Patient Health Questionnaire (PHQ-9) (Spitzer et al., 1999) is a self-report 9 item scale that assesses depression severity of adults. The PHQ-9 also includes items that assess sleep, anhedonia, and appetite, and it is considered a reliable and valid measure of depressive symptoms. Participants rated these items on a 4-point scale (0= not at all, 1= several days, 2= more than half the days, 3= nearly every day) (Lowe et al., 2004). A final question asks respondents how difficult daily functioning is as a result of these depressive symptoms; the response options range from “not difficult at all” to “extreme difficulty.”
The Patient Health Questionnaire for Adolescents (PHQ-A) (Johnson et al., 2002) is a 9 item self-report severity measure for depression adapted for adolescents aged 11 through 17 years old. Participants rated these items on a 4-point scale (0= not at all, 1= several days, 2= more than half the days, 3=nearly every day). A final question asks respondents how difficult daily functioning is as a result of these depressive symptoms; the response options range from “not difficult at all” to “extreme difficulty.”
The Difficulties in Emotion Regulation Scale- Short Form (DERS-SF) (Weiss et al., 2015) is an 18 item self-report measure that rates patient's emotional regulation in six domains: strategies, non-acceptance, impulse, goals, awareness, and clarity. Individual items are rated on a 5-point scale reflecting the proportion of time that emotion regulation is problematic; almost never, 0–10%; sometimes, 11–35%; about half the time, 36–65%; most of the time, 66–90%; almost always, 91–100%. All 6 subscales are graphed on a 15-point scale, with a rating of 15 indicating the most and 3 the least difficulty in emotional regulation. This measure is completed by adults and adolescents at admission.
The World Health Organization Disability Assessment Scale (WHODAS) (Axelsson et al., 2017) is a 12-item scale that pertains to difficulties associated with physical and mental health problems. These focus on difficulties in daily living, physical activities, and social relationships. Participants rated these items on a 5-point scale (1 = none, 2 = mild 2, 3 = moderate, 4 = severe, 5 = extreme or cannot do), with the total score being the sum of these items. The score ranges from 12 to 60, with higher scores indicating greater disability or loss of function. This assessment is completed by adults at admission.
The World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (WHOASSIST) (WHO, 2010) is a comprehensive assessment which includes lifetime non-medical use of various substances as well as past-three-month frequency of use, urges to use, impairment related to use, others’ expression of concern related to use, and efforts to control their use. Patients are first asked if they have used any substance for non-medical purposes; if they respond positively, they are asked six additional questions to determine level of use. Scores are summed, and the cutoffs are different for alcohol than for those for other substances. The alcohol-risk cutoffs are as follows; low, 0–10; moderate, 11–26; high, 27+. The other substance risk cutoffs are as follows; low, 0–3; moderate, 4–26; high, 27+. The WHO-ASSIST has shown strong validity and the ability to screen adequately for substances of low-to-high risk (Humeniuk et al., 2008). This questionnaire is completed by adults at admission.
The Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989) is a 10-item self-report measure pertaining to sleep quality, patterns, and difficulty sleeping. The tenth item on the survey asks about a bed partner or roommates and is excluded from this survey. It is scored from 0 to 21; a score greater than 5 indicates poor sleep quality. This assessment is completed by adults and adolescents at admission.
The Disturbing Dream and Nightmare Severity Index (DDNSI) (Krakow et al., 2002) is a 5-item self-report questionnaire pertaining to nightmare frequency and disturbance. It is scored from 0 to 37, based on the scores of 5 components. A score greater than 10 indicates a nightmare disorder. This scale is completed by adults and adolescents at admission.
The Suicide Behaviors Questionnaire-Revised (SBQ-R) (Osman et al., 2001) is a 4-item self-report measure intended to assess suicide risk. The questionnaire asks about suicidal thoughts/attempts, telling somebody about plans to commit suicide, and the likelihood of attempting suicide someday. The total score ranges from 3 to 18, with clinical data suggesting a score greater than or equal to 8 for psychiatric inpatients is considered significantly elevated. This assessment is completed by adults and adolescents at admission.
2.4. Data analysis
The current study utilized Propensity Score Matching (PSM), to match groups based on a propensity score, or balancing score, so the distribution of baseline covariates was similar among both groups (Austin, 2011; Rubin, 1983). Once the groups were matched based on the propensity score, this ensured results were more related to the COVID-19 pandemic and not to baseline demographic confounds (Austin, 2011). The use of Propensity Score Matching (PSM) (Austin, 2011) has expanded substantially in recent years. While PSM was originally more popular in a medical model or medical research (Stürmer et al., 2006), it has recently seen greater utility in psychiatric (Hansen et al., 2012; Marangell et al., 2008) and psychotherapy research (Bartak et al., 2010; Ye and Kaskutas, 2009). Once groups were matched, analyses of variance (ANOVAs) were conducted to determine if there were significant differences in the severity of admission scores pre- and during the pandemic on key mental health variables. Comparisons of means are presented, with standard Cohen's d effect sizes utilized (small = 0.20, medium = 0.50, large = 0.80) (Cohen, 1988).
3. Results
PSM was used to match patients who were admitted to the hospital before and during COVID-19 on relevant variables to create comparable groups from before and during the COVID-19 pandemic. Accordingly, pre-pandemic and during-pandemic groups were matched for age and gender. PSM was conducted separately for adult and adolescent patients.
3.1. Comparison of adults pre- and during the COVID pandemic
The mean age of the pre-pandemic group was 34.83 (SD = 15.23) and the mean age of the during-pandemic group was 34.88 (SD = 15.41). The pre-pandemic group had 99 females and 136 males, while the during-pandemic group was 108 females and 127 males. Further breakdown of descriptive statistics for adult inpatients is shown in Table 3.
Table 3.
Distribution of demographic variables.
| Adults Pre-Pandemic(n = 235) N (% of total) | Adults During-Pandemic (n = 235) N (% of total) | Adolescents Pre-Pandemic(n = 65) N (% of total) | Adolescents During-Pandemic(n = 77) N (% of total) | |
|---|---|---|---|---|
| Gender | ||||
| Male | 136 (57.9) | 127 (54.0) | 16 (24.6) | 16 (20.8) |
| Female |
99 (42.1) | 108 (46.0) | 49 (75.4) |
61 (79.2) |
| Race | ||||
| Caucasian | 209 (88.9) | 194 (82.5) | 56 (86.5) |
67 (86.8) |
| Other | 26 (11.1) | 41 (17.5) | 9 (13.5) | 10 (13.2) |
|
Education |
||||
| College education | 117 (50.0) | 116 (49.8) | – | – |
| No college education | 117 (50.0) | 117 (50.2) | – | – |
| MDD | 77 (38.5) | 86 (44.8) | 13 (23.2) | 6 (10.2) |
| GAD | 19 (9.5) | 55 (28.6) | 15 (17.9) | 35 (59.3) |
| Bipolar | 16 (8.0) | 11 (5.7) | 0 (0.0) | 0 (0.0) |
| ADHD | – | – | 20 (35.7) | 14 (23.7) |
| PTSD | 25 (12.5) | 35 (18.2) | 10 (17.9) | 17 (28.8) |
| Mean (SD) | Mean (SD) | Mean (SD) |
Mean (SD) | |
| Age | 34.83 (15.23) | 34.88 (15.41) | 15.03 (1.48) |
15.16 (1.51) |
| Length of Stay (LOS) | 37.74 (16.21) | 35.79 (17.13) | 22.95 (9.41) |
22.83 (7.37) |
| Lifetime Suicide Attempts | 3.00 (1.15) | 3.38 (4.86) | 2.16 (1.71) |
2.95 (2.49) |
| Previous therapists | 5.50 (20.36) | 3.21 (4.05) | 3.40 (1.69) |
2.22 (1.25) |
| Previous Psychiatrists | 3.23 (2.97) | 3.21 (4.05) | 2.10 (1.68) |
1.69 (1.33) |
| Previous acute admissions | 1.50 (4.69) | 1.47 (3.08) | - |
– |
| Previous extended admissions | 0.95 (1.56) | 1.65 (8.37) | - |
– |
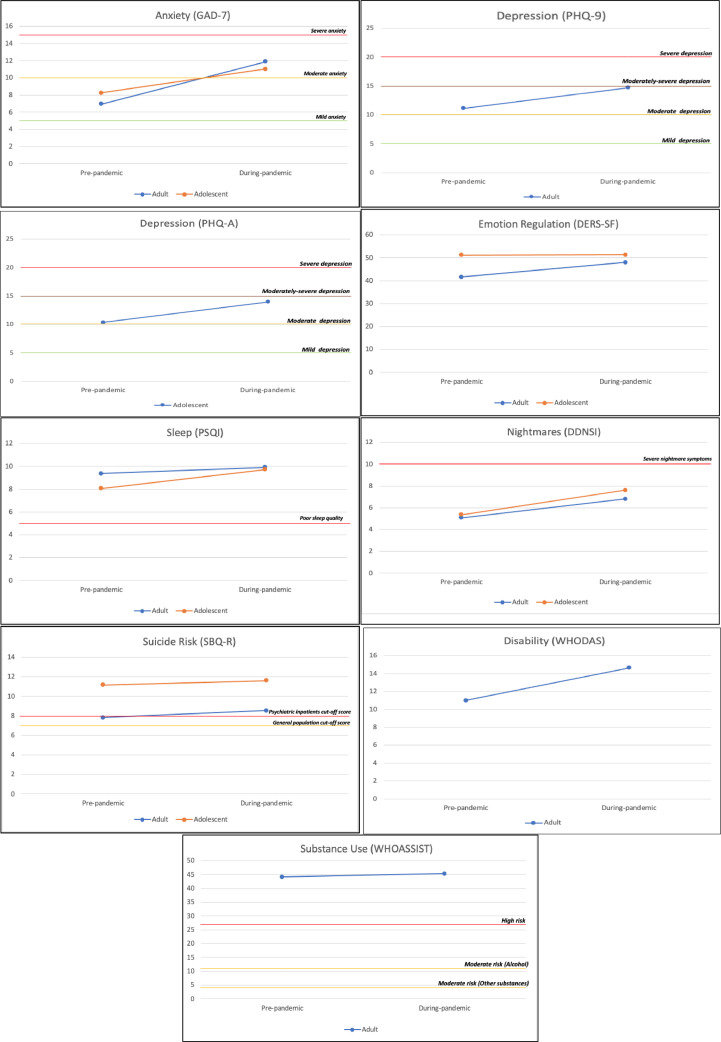
Next, analyses of variance (ANOVAs) were conducted to determine if there were significant differences in the severity of admission scores pre- and during the pandemic on key mental health variables. Results revealed significant differences in anxiety [F(1468) = 104.88, p < .001, partial η2=0.18], depression [F(1466) = 29.44, p < .001, partial η2=0.06], emotion regulation [F(1461) = 26.10, p < .001, partial η2=0.05], nightmares [F(1462) = 6.17, p = .013, partial η2=0.01] and disability [F(1456) = 18.62, p < .001, partial η2=0.04]. As hypothesized, scores were higher for all measures during the COVID pandemic (see Table 1 for means, standard deviations, and Cohen's d) and effect sizes demonstrate small (nightmares), medium (depression, emotion regulation, disability), and large effects (anxiety). However, there were no significant differences on measures of substance use [F(1416) = 0.002, p = .965, partial η2=0.00], sleep [F(1462) = 2.32, p = .128, partial η2=0.01], and suicide risk [F(1458) = 3.09, p = .080, partial η2=0.01] (see Table 1 for means, standard deviations, and Cohen's d). See Fig. 1 for differences in outcomes pre-pandemic vs. during-pandemic.
Table 1.
Means, standard deviations, and effect sizes for adult sample.
| Pre-Pandemic | During-Pandemic | d | |
|---|---|---|---|
| Anxiety (GAD-7) | 6.97 (4.14) | 11.88 (6.07) | .95⁎⁎⁎ |
| Depression (PHQ-9) | 11.15 (6.73) | 14.71 (7.41) | .50⁎⁎⁎ |
| Emotion Regulation (DERS-SF) | 41.66 (12.14) | 47.96 (14.27) | .48⁎⁎⁎ |
| Sleep (PSQI) | 9.37 (3.80) | 9.92 (3.93) | .14 |
| Nightmares (DDNSI) | 5.08 (6.95) | 6.81 (8.03) | .23* |
| Suicide Risk (SBQ-R) | 7.83 (4.38) | 8.56 (4.89) | .16 |
| Disability (WHODAS) | 11.00 (8.79) | 14.65 (9.31) | .40⁎⁎⁎ |
| Substance Use (WHOASSIST) | 44.15 (40.54) | 45.32 (39.26) | .00 |
Note.
= p <0.05;
⁎⁎ = p <0.01;.
= p < .001.
Fig. 1.
Differences in outcomes at admission pre-pandemic vs. during-pandemic for adolescent and adult samples. The substance use and disability assessment are only completed by the adult sample. Clinical cut-off scores are included.
3.2. Comparison of adolescents Pre- and during the COVID pandemic
Using the same PSM process as with the adults, comparisons revealed no significant differences between the pre- and during pandemic groups for either of the control variables for the adolescents [age: t(140) = 0.497, p = .620; gender: χ2(1) = 0.297, p = .586]. The mean age of the pre-pandemic group was 15.03 (SD = 1.48) and the mean age of the during-pandemic group was 15.16 (SD = 1.51). The pre-pandemic group had 49 females and 61 males, while the during-pandemic group was 61 females and 16 males. Further breakdown of descriptive statistics for the adolescent inpatients is show in Table 3.
We then proceeded with ANOVAs to determine if there were significant differences in the severity of admission scores between pre- and during pandemic groups. Results revealed there were significant differences in anxiety [F(1140) = 8.03, p = .005, partial η2=0.05], depression [F(1140) = 8.18, p = .005, partial η2=0.06], and sleep [F(1140) = 6.61, p = .011, partial η2=0.05] for adolescents, all in the hypothesized direction with scores significantly increased during the COVID pandemic (see Table 2 for means, standard deviations, and Cohen's d). Effect sizes indicate medium effects for all significant findings. There were no significant differences for emotion regulation [F(1140) = 0.001, p = .973, partial η2=0.00], nightmares [F(1139) = 2.54, p = .113, partial η2=0.02], or suicide risk [F(1139) = 0.404, p = .526, partial η2=0.00] (see Table 2 for means, standard deviations, and Cohen's d). Despite the lack of statistically significant differences in nightmares, effect sizes indicate a non-negligible effect (0.27) for adolescents. See Fig. 1 for differences in outcomes pre-pandemic vs. during-pandemic.
Table 2.
Means, standard deviations, and effect sizes for adolescent sample.
| Pre-Pandemic | During-Pandemic | d | |
|---|---|---|---|
| Anxiety (GAD-7) | 8.26 (5.81) | 11.04 (5.83) | .48⁎⁎ |
| Depression (PHQ-A) | 10.34 (7.81) | 13.94 (7.16) | .48⁎⁎ |
| Emotion Regulation (DERS-SF) | 51.28 (16.03) | 51.36 (14.14) | .01 |
| Sleep (PSQI) | 8.06 (3.80) | 9.71 (3.82) | .43* |
| Nightmares (DDNSI) | 5.37 (7.08) | 7.61 (9.22) | .27 |
| Suicide Risk (SBQ-R) | 11.17 (4.27) | 11.63 (4.33) | .11 |
Note.
= p <0.05;.
= p <0.01;
⁎⁎⁎ = p < .001.
4. Discussion
This study found significantly increased mental health symptom severity at admission to an inpatient psychiatric hospital during the COVID-19 pandemic compared to patients admitted before the COVID-19 pandemic. Specifically, adults demonstrated significantly greater anxiety, depression, emotion regulation problems, nightmares, and disability at admission relative to adults who were admitted before the pandemic. Adolescents who were admitted during the pandemic demonstrated significantly greater anxiety, depression, and sleep problems when compared to adolescents who were admitted pre-pandemic. These findings of increased symptom severity during an infectious disease pandemic are consistent with previous research (Blithikioti et al., 2021; Carmassi et al., 2020; Cenat et al., 2020; Chappuy et al., 2021; Franchini et al., 2020; Fegert et al., 2020; Guessoum et al., 2020; Hao et al., 2020; Jalloh et al., 2018; Jeong et al., 2016; Ko et al., 2006; Lau et al., 2005; Lee, 2020; Bar-Or et al., 2021; Ma et al., 2020; Neelam et al., 2021; Rogers et al., 2021; Van Rheenen et al., 2020) that focused on the psychiatric effects of disease outbreaks, including COVID-19. Importantly, our findings extend the understanding of the effects of a pandemic on the youth and adults who have significant preexisting mental health symptoms and utilize mental health's highest level of care intensity.
In the current study, for the adults admitted inpatient, no significant differences were found pre-pandemic vs. during the pandemic in measures of sleep quality, suicide risk, or substance use. Other studies have shown increased sleep problems during COVID, but results are inconsistent; patients’ reports vary from worsened insomnia symptoms (Sun et al., 2021) and increased sleep disruptions (Muruganandam et al., 2020) to sleeping more (Van Rheenen et al., 2020). This inconsistency in the literature may be attributed to the measure of sleep used in each study which would assess different aspects of sleep problems. In this study, the sleep assessment used is the PSQI which includes many components of sleep in its total score and may have lacked the specificity needed to find a significant difference in sleep health in our adult population. Other studies have also observed higher levels of suicidal ideation; 14.4% of patients with severe mental illness reported suicidal ideation during COVID-19; 5.3% of those patients reported an increase in suicidal ideation compared to before the pandemic (Muruganandam et al., 2020), and psychiatric patients were more likely to report worries about suicidal ideation than healthy controls (Hao et al., 2020). Additionally, most of the literature on addiction psychiatry has shown elevated levels of substance use during the COVID-19 pandemic compared to 2019 (Czeisler et al., 2020) and an increased need for addiction counseling services (Columb et al., 2020). The inpatient psychiatric facility to which our adult sample were admitted to treats individuals both with and without substance use disorders, which may explain the inconsistency between the literature and our findings. Finally, because this study is conducted in an inpatient psychiatric setting, patients present with significantly elevated sleep problems, suicide risk, and substance use problems at admission leading to a “ceiling effect” (Ho and Yu., 2015). This may explain the lack of a significant difference for those psychiatric symptoms between pre-pandemic and during-pandemic.
In adolescents, no significant differences were found in emotion regulation, nightmares, or suicide risk pre-pandemic vs. during the pandemic. Although studies have shown emotional deterioration (Ravens-Sieberer et al., 2021) and an increase in emotion regulation problems (Amoros-Reche et al., 2022) among children and adolescents during the pandemic (Ravens-Sieberer et al., 2021), our findings do not show a significant increase. This adolescent sample admitted to the inpatient psychiatric program with significantly high emotional problems score pre-pandemic leading to a ceiling effect. This may explain the lack of a significant difference in emotion regulation scores during the pandemic. The lack of statistical significance for nightmares may be due to the small sample size. Most research focusing on the effects of the COVID-19 pandemic on children and adolescent mental health has had little to no emphasis on these specific psychiatric symptoms among youth with preexisting mental health conditions.
Findings in the current study have several limitations. First, the racial homogeneity of our sample limits the generalizability of the results. The race/ethnicity of the participants is predominantly Caucasian (85.7% of our adult population and 86.7% of our adolescent population). Future studies should replicate these results with a more diverse sample. Second, although typically an objective measure of executive functioning (the NIH Toolbox) (Gershon et al., 2013) is conducted at admission, social distancing restrictions and safety precautions prevented its administration during COVID. Therefore, all of the studied measures rely on patient self-report which makes the data subject to bias (Bhandari and Wagner, 2006). However, since these measures are administered as part of the usual standard care and are used clinically, patients may be motivated to answer honestly and provide valid responses. Although all patients provided documentation of a negative COVID test at admission, this study does not differentiate among individuals who may have had a COVID-19 infection prior to hospitalization. Examining whether or not patients had COVID-19 prior to hospitalization, may help clarify whether the increased psychiatric symptom severity is attributable to the stressors of the pandemic and/or is a biological sequelae such as alterations in neurotransmitter levels leading to symptoms caused by the virus itself (Boldrini et al., 2021). Lastly, due to the significant developmental differences (e.g., adolescent sample begins at age 12 vs. our adults) and the differences in treatment, future directions include to examine the between group differences due to COVID while controlling for these variables.
Although it is unclear what factors are directly responsible for the increase in psychiatric symptom severity for those admitting during the COVID-19 pandemic, there are possibilities and factors that can be explored. One possible reason is that those with preexisting mental illness simply became even more ill during the pandemic. Another possibility or factor could be that patients delayed longer prior to admitting during the pandemic (perhaps due to fear of going into a hospital with other people in proximity), resulting in higher symptom severity at admission. Although the primary reason is unknown, our hospital responded to this increase in mental health issues across our admission criteria by maintaining and/or increasing staffing and opening access to our inpatient services (e.g., through scholarships for services, revision of admission criteria), Examining the impact of these institutional changes are outside the scope of the current article; however, these among other factors could be explored further by future studies.
Ultimately, this study contributes to a growing body of literature highlighting youth and adults with preexisting mental illness as groups particularly vulnerable to the stressors of COVID-19, and further elucidates which components of mental health are affected and to what degree. Despite the many competing demands for scarce resources during a global health crisis, these results emphasize that, mental health needs must not be overlooked, particularly for those with preexisting psychiatric conditions. Findings further demonstrate the need for continuity in and expansion of access to mental health care for all.
CRediT authorship contribution statement
Danna Ramirez: Conceptualization, Writing – review & editing. Katrina A. Rufino: Conceptualization, Formal analysis, Writing – review & editing. Megan E. Rech: Writing – review & editing. Edward Poa: Writing – review & editing. Michelle A. Patriquin: Conceptualization, Writing – review & editing.
Declaration of Competing Interest
No authors have conflicts of interest to declare.
Acknowledgments
Role of Funding source
This research was supported by The Menninger Clinic and The Menninger Clinic Foundation. None of these funding sources had a role in the study design, collection, analysis, or interpretation of the data, writing the article, or in the decision to submit the article for publication.
Acknowledgment
We would like to acknowledge the significant efforts of the research team at The Menninger Clinic for their important contributions to research and data collection.
References
- Ammar A., Mueller P., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Bouaziz B., Brach M., Schmicker M., Bentlage E., How D., Ahmed M., Aloui A., Hammouda O., Paineiras-Domingos L.L., Braakman-Jansen A., Wrede C., Bastoni S., Pernambuco C., .…, Consortium E.-C. Psychological consequences of COVID-19 home confinement: the ECLB-COVID19 multicenter study. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0240204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amorós-Reche V., Belzunegui-Pastor A., Hurtado G., Espada J.P. Emotional problems in Spanish children and adolescents during the COVID-19 pandemic: a systematic review. Clín. Salud. 2022;33(1):19–28. doi: 10.5093/clysa2022a2. [DOI] [Google Scholar]
- Austin P.C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Mult. Behav. Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelsson E., Lindsäter E., Ljótsson B., Andersson E., Hedman-Lagerlöf E. The 12-item self-report World Health Organization disability assessment schedule (WHODAS) 2.0 administered via the internet to individuals with anxiety and stress disorders: a psychometric investigation based on data from two clinical trials. JMIR Ment. Health. 2017;4(4):e58. doi: 10.2196/mental.7497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartak A., Spreeuwenberg M.D., Andrea H., Holleman L., Rijnierse P., Rossum B.V., Hamers E.F., Meerman A.M., Aerts J., Busschbach J.J., Verheul R., Stijnen T., Emmelkamp P.M. Effectiveness of different modalities of psychotherapeutic treatment for patients with cluster C personality disorders: results of a large prospective multicentre study. Psychother. Psychosom. 2010;79(1):20–30. doi: 10.1159/000254902. [DOI] [PubMed] [Google Scholar]
- Bhandari A., Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med. Care Res. Rev. 2006;63(2):217–235. doi: 10.1177/1077558705285298. [DOI] [PubMed] [Google Scholar]
- Blithikioti, Nuño L., Paniello B., Gual A., Miquel L. Impact of COVID-19 lockdown on individuals under treatment for substance use disorders: risk factors for adverse mental health outcomes. J. Psychiatr. Res. 2021;139:47–53. doi: 10.1016/j.jpsychires.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boldrini M., Canoll P.D., Klein R.S. How COVID-19 Affects the Brain. JAMA Psychiatry. 2021 doi: 10.1001/jamapsychiatry.2021.0500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse D.J., Reynolds C.F., 3rd, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Carmassi, Bertelloni C.A., Dell’Oste V., Barberi F.M., Maglio A., Buccianelli B., Cordone A., Dell’Osso L. Tele-psychiatry assessment of post-traumatic stress symptoms in 100 patients with bipolar disorder during the COVID-19 pandemic social-distancing measures in Italy. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.580736. 580736–580736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cenat J.M., Felix N., Blais-Rochette C., Rousseau C., Bukaka J., Derivois D., Noorishad P.G., Birangui J.P. Prevalence of mental health problems in populations affected by the Ebola virus disease: a systematic review and meta-analysis. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113033. [DOI] [PubMed] [Google Scholar]
- Chakraborty, Karmakar S. Impact of COVID-19 on obsessive compulsive disorder (OCD) Iran. J. Psychiatry. 2020;15(3):256–259. doi: 10.18502/ijps.v15i3.3820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chappuy, Peyrat M., Lejeune O., Duvernay N., David B., Joubert P., Lack P. Drug consumption during prolonged lockdown due to COVID-19 as observed in French addiction center. Therapie. 2021;76(4):379–382. doi: 10.1016/j.therap.2021.01.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung Y.T., Chau P.H., Yip P.S. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2008;23(12):1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- Cohen J. 2nd edition. Lawrence Erlbaum Associates; New Jersey: 1988. Statistical Power Analysis For the Behavioral Sciences. [Google Scholar]
- Columb D., Hussain R., O'Gara C. Addiction psychiatry and COVID-19: impact on patients and service provision. Ir J Psychol Med. 2020;37(3):164–168. doi: 10.1017/ipm.2020.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic - United States, June 24-30, 2020. Centers for Disease Control and Prevention (CDC) 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas P.K., Douglas D.B., Harrigan D.C., Douglas K.M. Preparing for pandemic influenza and its aftermath: mental health issues considered. Int. J. Emerg. Ment. Health. 2009;11(3):137–144. https://www.ncbi.nlm.nih.gov/pubmed/20437844 [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry Mental Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franchini, Ragone N., Seghi F., Barbini B., Colombo C. Mental health services for mood disorder outpatients in Milan during COVID-19 outbreak: the experience of the health care providers at San Raffaele hospital. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113317. 113317–113317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon R.C., Wagster M.V., Hendrie H.C., Fox N.A., Cook K.F., Nowinski C.J. NIH toolbox for assessment of neurological and behavioral function. Neurology. 2013;80(11 Suppl 3):S2–S6. doi: 10.1212/WNL.0b013e3182872e5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gryczynski J., Kelly S.M., Mitchell S.G., Kirk A., O'Grady K.E., Schwartz R.P. Validation and performance of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) among adolescent primary care patients. Addiction. 2015;110(2):240–247. doi: 10.1111/add.12767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen R.A., Dusetzina S.B., Ellis A.R., Stürmer T., Farley J.F., Gaynes B.N. Risk of adverse events in treatment-resistant depression: propensity-score-matched comparison of antidepressant augment and switch strategies. Gen. Hosp. Psychiatry. 2012;34(2):192–200. doi: 10.1016/j.genhosppsych.2011.10.001. [DOI] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill R.M., Rufino K., Kurian S., Saxena J., Saxena K., Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021;147(3) doi: 10.1542/peds.2020-029280. [DOI] [PubMed] [Google Scholar]
- Ho, Yu C.C. Descriptive statistics for modern test score distributions: skewness, kurtosis, discreteness, and ceiling effects. Educ. Psychol. Meas. 2015;75(3):365–388. doi: 10.1177/0013164414548576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humeniuk R., Ali R., Babor T.F., Farrell M., Formigoni M.L., Jittiwutikarn J., de Lacerda R.B., Ling W., Marsden J., Monteiro M., Nhiwatiwa S., Pal H., Poznyak V., Simon S. Validation of the alcohol, smoking and substance involvement screening test (ASSIST) Addiction. 2008;103(6):1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Jalloh M.F., Li W., Bunnell R.E., Ethier K.A., O’Leary A., Hageman K.M., Sengeh P., Jalloh M.B., Morgan O., Hersey S., Marston B.J., Dafae F., Redd J.T. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob. Health. 2018;3(2) doi: 10.1136/bmjgh-2017-000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankowski K., Hamblen J. U.S. Department of Veterans Affairs; 2019. The Effects of Disaster on People with Severe Mental Illness.https://www.ptsd.va.gov/professional/treat/specific/disaster_mental_illness.asp [Google Scholar]
- Jeong H., Yim H.W., Song Y.J., Ki M., Min J.A., Cho J., Chae J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020;221:264–266. doi: 10.1016/j.jpeds.2020.03.013. e261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J.G., Harris E.S., Spitzer R.L., Williams J.B. The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J. Adolesc. Health. 2002;30(3):196–204. doi: 10.1016/s1054-139x(01)00333-0. [DOI] [PubMed] [Google Scholar]
- Ko C.H., Yen C.F., Yen J.Y., Yang M.J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin. Neurosci. 2006;60(4):397–403. doi: 10.1111/j.1440-1819.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- Krakow B.J., Melendrez D.C., Johnston L.G., Clark J.O., Santana E.M., Warner T.D., Hollifield M.A., Schrader R., Sisley B.N., Lee S.A. Sleep Dynamic Therapy for Cerro Grande Fire evacuees with posttraumatic stress symptoms: a preliminary report. J. Clin. Psychiatry. 2002;63(8):673–684. doi: 10.4088/jcp.v63n0804. [DOI] [PubMed] [Google Scholar]
- Lamblin M., Murawski C., Whittle S., Fornito A. Social connectedness, mental health and the adolescent brain. Neurosci. Biobehav. Rev. 2017;80:57–68. doi: 10.1016/j.neubiorev.2017.05.010. [DOI] [PubMed] [Google Scholar]
- Lau J.T., Yang X., Pang E., Tsui H.Y., Wong E., Wing Y.K. SARS-related perceptions in Hong Kong. Emerging Infect. Dis. 2005;11(3):417–424. doi: 10.3201/eid1103.040675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health. 2020;4(6):421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar-Or Lev, Shalit N., Shpitzer R., Kor A., Lev-Ran S. Self-reported changes in use of addictive substances and behaviors among patients treated in an addiction treatment clinic during the COVID-19 quarantine. Isr. Med. Assoc. J. 2021;23(1):11. [PubMed] [Google Scholar]
- Lowe B., Decker O., Muller S., Brahler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Lowe B., Grafe K., Zipfel S., Witte S., Loerch B., Herzog W. Diagnosing ICD-10 depressive episodes: superior criterion validity of the Patient Health Questionnaire. Psychother. Psychosom. 2004;73(6):386–390. doi: 10.1159/000080393. [DOI] [PubMed] [Google Scholar]
- Ma, Hua T., Zeng K., Zhong B., Wang G., Liu X. Influence of social isolation caused by coronavirus disease 2019 (COVID-19) on the psychological characteristics of hospitalized schizophrenia patients: a case-control study. Transl Psychiatry. 2020;10(1) doi: 10.1038/s41398-020-01098-5. 411–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, Mazidi M., Li K., Li Y., Chen S., Kirwan R., Zhou H., Yan N., Rahman A., Wang W., Wang Y. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;293:78–89. doi: 10.1016/j.jad.2021.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson N.R., Freeman J.Y.A., Rapee R.M., Richardson C.E., Oar E.L., Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc. 2020 doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I.W., Chu C.M., Pan P.C., Yiu M.G., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31(4):318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marangell L.B., Dennehy E.B., Wisniewski S.R., Bauer M.S., Miyahara S., Allen M.H., Martinez M., Al Jurdi R.K., Thase M.E. Case-control analyses of the impact of pharmacotherapy on prospectively observed suicide attempts and completed suicides in bipolar disorder: findings from STEP-BD. J. Clin. Psychiatry. 2008;69(6):916–922. doi: 10.4088/jcp.v69n0605. [DOI] [PubMed] [Google Scholar]
- Menninger K.A. Psychoses associated with influenza: i. General data: statistical analysis. J. Am. Med. Assoc. 1919;72(4):235–241. doi: 10.1001/jama.1919.02610040001001. [DOI] [Google Scholar]
- Muruganandam P., Neelamegam S., Menon V., Alexander J., Chaturvedi S.K. COVID-19 and severe mental illness: impact on patients and its relation with their awareness about COVID-19. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neelam K., Duddu V., Anyim N., Neelam J., Lewis S. Pandemics and pre-existing mental illness: a systematic review and meta-analysis. Brain Behav. Immun. Health. 2021;10 doi: 10.1016/j.bbih.2020.100177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A., Bagge C.L., Gutierrez P.M., Konick L.C., Kopper B.A., Barrios F.X. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Psychol. Assess. Resour. 2001;8(4):443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Racine, McArthur B.A., Cooke J.E., Eirich R., Zhu J., Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. Arch. Pediatr. Adolesc. Med. 2021;175(11):1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravens-Sieberer, Kaman A., Erhart M., Otto C., Devine J., Löffler C., Hurrelmann K., Bullinger M., Barkmann C., Siegel N.A., Simon A.M., Wieler L.H., Schlack R., Hölling H. Quality of life and mental health in children and adolescents during the first year of the COVID-19 pandemic: results of a two-wave nationwide population-based study. Eur. Child Adolesc. Psychiatry. 2021 doi: 10.1007/s00787-021-01889-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon S. Ebola's mental-health wounds linger in Africa. Nature. 2015;519(7541):13–14. doi: 10.1038/519013a. [DOI] [PubMed] [Google Scholar]
- Robinson, Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers Bogiaizian D., Salazar P.L., Solari A., Garey L., Fogle B.M., Schmidt N.B., Zvolensky M.J. COVID-19 and anxiety sensitivity across two studies in Argentina: associations with COVID-19 worry, symptom severity, anxiety, and functional impairment. Cognit. Ther. Res. 2021;45(4):697–707. doi: 10.1007/s10608-020-10194-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum P.R., Rubin D.B. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. doi: 10.1093/biomet/70.1.41. [DOI] [Google Scholar]
- Singh S., Roy D., Sinha K., Parveen S., Sharma G., Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stürmer T., Joshi M., Glynn R.J., Avorn J., Rothman K.J., Schneeweiss S. A review of the application of propensity score methods yielded increasing use, advantages in specific settings, but not substantially different estimates compared with conventional multivariable methods. J. Clin. Epidemiol. 2006;59(5):437–447. doi: 10.1016/j.jclinepi.2005.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Q., Qin Q., Basta M., Chen B., Li Y. Psychological reactions and insomnia in adults with mental health disorders during the COVID-19 outbreak. BMC Psychiatry. 2021;21(1):19. doi: 10.1186/s12888-020-03036-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ustun, Tevfik Bedirhan, Kostanjesek, N, Chatterji, S, Rehm, J, World Health Organization., 2010. Measuring health and disability : manual for WHO disability assessment schedule (WHODAS 2.0). World Health Organization. 10665/43974.
- Van Rheenen T.E., Meyer D., Neill E., Phillipou A., Tan E.J., Toh W.L., Rossell S.L. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: initial results from the COLLATE project. J. Affect. Disord. 2020;275:69–77. doi: 10.1016/j.jad.2020.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss N.H., Gratz K.L., Lavender J.M. Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: the DERS-positive. Behav. Modif. 2015;39(3):431–453. doi: 10.1177/0145445514566504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler P., Formanek T., Mlada K., Kagstrom A., Mohrova Z., Mohr P., Csemy L. Increase in prevalence of current mental disorders in the context of COVID-19: analysis of repeated nationwide cross-sectional surveys. Epidemiol. Psychiatry Sci. 2020;29:e173. doi: 10.1017/S2045796020000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2010). WHO-ASSIST The alcohol, smoking and substance involvement screening test (ASSIST): manual for use in primary care.http://whqlibdoc.who.int/publications/2010/9789241599382_eng.pdf.
- World Health Organization (WHO). (2020, April 27). Archived: WHO Timeline- COVID-19. https://www.who.int/news/item/27-04-2020-who-timeline-covid-19.
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;174(9):898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Y., Kaskutas L.A. Using propensity scores to adjust for selection bias when assessing the effectiveness of Alcoholics Anonymous in observational studies. Drug Alcohol. Depend. 2009;104(1–2):56–64. doi: 10.1016/j.drugalcdep.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- YoungMiNDS. (2020). Coronavirus: impact on young people with mental health needs. https://youngminds.org.uk/media/3708/coronavirus-report_march2020.pdf.
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Liu M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]