Abstract
Hepatocellular carcinoma (HCC) is the fifth most common malignant cancer and the third most frequent cause of tumour-related mortality worldwide. Currently, several surgical and medical therapeutic strategies are available for HCCs; however, the interaction between neoplastic cells and non-neoplastic stromal cells within the tumour microenvironment (TME) results in strong therapeutic resistance of HCCs to conventional treatment. Therefore, the development of novel treatments is urgently needed to improve the survival of patients with HCC. The first step in developing efficient chemotherapeutic drugs is the establishment of an appropriate system for studying complex tumour culture and microenvironment interactions. Three-dimensional (3D) culture model might be a crucial bridge between in vivo and in vitro due to its ability to mimic the naturally complicated in vivo TME compared to conventional two-dimensional (2D) cultures. In this review, we shed light on various established 3D culture models of HCC and their role in the investigation of tumour-TME interactions and HCC-related therapeutic resistance.
Graphical Abstract
Keywords: HCC, 3D cell culture, TME, Drug resistance, 2D cell culture, Chemotherapeutic drugs
Introduction
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death worldwide [1–3] and commonly has a poor prognosis. In particular, patients with HCC usually develop severe chronic hepatic damage, including inflammatory, fibrotic, and cirrhotic lesions. Thus, these patients frequently show poor systemic chemotherapeutic tolerance [4]. Currently, efficient strategies for treating HCCs are still lacking due to the continuous growth of tumour cells and the genetic complexity involving molecular factors that affect interactions between tumour cells and their surrounding tumour microenvironment (TME) [5–7].
Investigating the complex features of neoplastic cells and the tumour-TME interaction has proven to be a consistent challenge. Therefore, the production of optimal in vivo and in vitro systems involved in the complex neoplastic and non-neoplastic cell interactions requires more effort [8]. Most of the available data regarding in vitro systems are derived from two-dimensional (2D) culture systems, which are simple, inexpensive, cell-based models. However, these methods cannot replicate the specific architecture and biochemical signalling of cells in vivo. Hence, switching from a 2D system to a three-dimensional (3D) system is necessary to better understand HCC tumour biology [9, 10] Developing appropriate 3D models that better mimic the specificity of the TME has received great scientific interest, and there were more than 1000 publications on this topic in 2016 alone [8]. The current review provides an overview of the different 3D culture models of HCC and their role in investigating tumour-TME interactions as well as HCC-related therapeutic resistance. Topics covered in this review include the therapeutic resistance of HCC to conventional treatment, TME factors affecting HCC progression, differences between 2 and 3D culture models, and the development of novel models of HCC 3D culture spheroids. Our aim is to provide a comprehensive review to expand the knowledge in the field of HCC treatment strategies.
HCC and resistance to conventional therapeutics
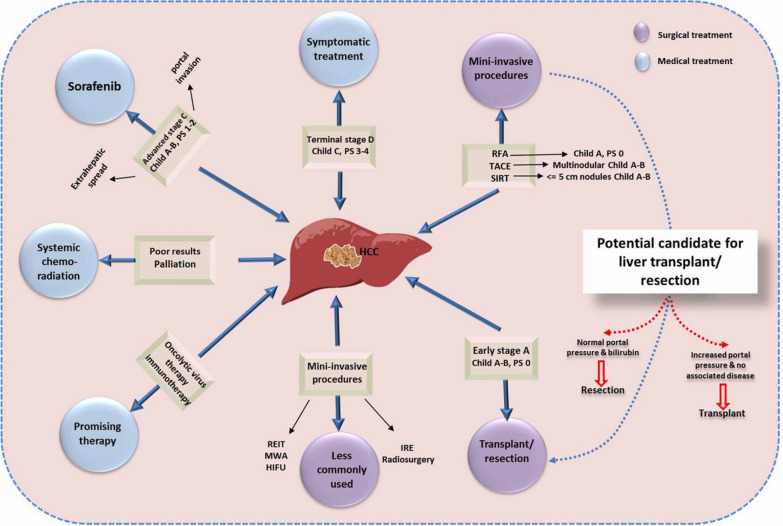
HCC is well established as the most common form of primary liver malignancy, the fifth most common type of overall malignant cancerglobally [11–13]. Currently, several modalities, including liver transplantation, surgical intervention, radiology, systemic chemotherapy, and trans-arterial chemoembolization, are available for the treatment of patients with late-stage HCC [14]. However, the cure rate of patients with HCC is very low [15–17], and the recurrence rate of HCC after surgical resection is usually high due to tumour metastasis and a reduced efficacy of conventional chemotherapy [13, 18, 19] The low survival rateof patients with late stage HCC could be due tp the lack of highly reliable biomarkers to identify the early stage cancer, besides the presence of primary underlying liver dysfunction, which limits the efficacy of available radio and chemotherapy like sorafenib [20, 21]. Sorafenib, the multi-kinase inhibitor that is the only Food and Drug Administration (FDA)-approved molecular targeted drug for advanced-stage HCC [22, 23], provides about three months survival on average [24]. Additionally, HCC is known for its poor response and increased intrinsic resistance for both local regional and systemic cytotoxic chemotherapy [22]. Several factors could control the tumor resistance including abnormal TME, activation of epithelial-mesenchymal transition (EMT), heterogeneity of HCC, and induction of various signalling pathways [25]. Among them, TME is the most widely investigated factor due to its role in tumor progression and chemotherapeutic resistance [26, 27]. Therefore, evaluation of the potential anticancer efficacy of novel drugs commonly targets the TME as a marker for therapeutic competence against HCC [28, 29]. The role of tumour staging according to the Child–Pugh classification in guiding treatment decisions is summarized in Fig. 1.
Fig. 1.
The role of tumour staging in guiding the treatment decisions according to the Child–Pugh classification
TME factors affect HCC progression and therapeutic resistance
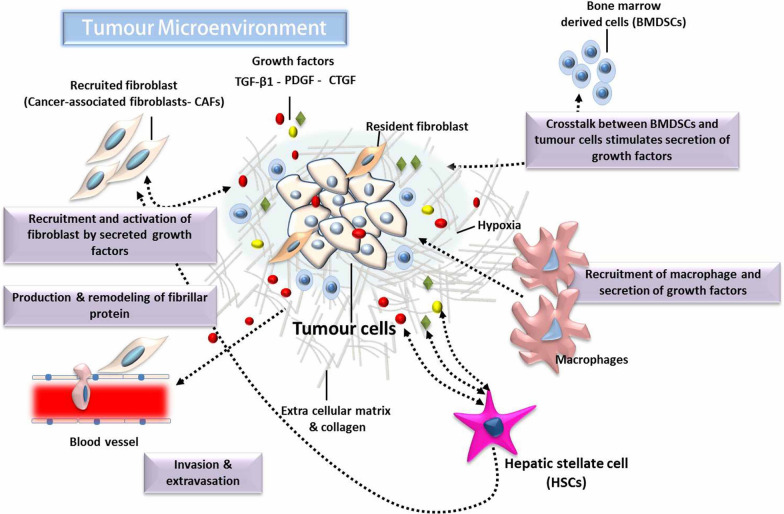
The TME comprises various non-neoplastic cells that contribute to multiple aspects of disease progression, including growth, metastasis, migration, and the development of chemotherapeutic resistance [8]. As represented in Fig. 2, the major components of the HCC microenvironment are malignant tumour cells and various non-cancerous stromal cells. Cancer-associated fibroblasts (CAFs) and hepatic stellate cells (HSCs) are the main cells within the HCC stroma, in addition to endothelial, immune, and inflammatory cells [30]. All these cell types play specific roles in promoting tumour structure and function [31].
Fig. 2.
The cellular components comprise the HCC microenvironment. TGF-β1 Transforming growth factor beta, PDGF Platelet-derived growth factor, CTGF Connective tissue growth factor
CAFs could be produced from several cell types, including resident and bone marrow-derived fibroblasts, and they play a pivotal role in the promotion of HCC growth and metastasis via the production of various growth factors and cytokines [32]. However, the major production site of activated CAFs is HSCs [33, 34]. HSCs could flood the TME with increased amounts of different types of growth factors, such as connective tissue growth factor (CTGF), transforming growth factor β1 (TGF-β1), and platelet-derived growth factor (PDGF). These factors are able to activate HCC cells and HSCs through both paracrine and autocrine pathways [35, 36]. Bidirectional activation of the TME consequently resulted in enhanced extracellular matrix (ECM) synthesis, tumour proliferation and invasion, as well as increased therapeutic resistance [37, 38].
It is now strongly suggested that the continuous changes in the histopathologic sequences of different tumours might result from the interaction between cancer cells and the surrounding non-neoplastic cells during tumorigenesis, which indicates the importance of investigating the TME [39]. Therefore, targeting HCC-HSCs and the HCC-CAF interaction became crucial in the investigation of supressing HCC growth [36, 40]. To better understand such interactions, the use of appropriate models for tumour cells and microenvironment culture is essential. Hence, the development of gradational 3D cancer models, which may largely mimic the interaction between TME and cancer cells, is crucial to investigate the mechanisms of tumour progression and promising novel chemotherapeutic drugs.
The superiority of 3d cell culture over traditional 2D cell culture
The pathogenesis and potential therapeutic agents for HCC have been extensively studied in various animal models. However, the presence of several factors limited the efficacy of those models, including increased cost, long implementation, and difficulty in obtaining human fibroblasts [41]. In addition, certain experimental conditions may result in the development of many questions about the animals’ pain and discomfort. As such, the immune systems of animal models may be compromised during the experiment with subsequent alterations of tumour cell-TME interaction (unlike in humans), which limits the clinical application of novel investigations [42]. Obtaining a convenient link between clinical trials and experimental animal models is an everyday challenge [43].
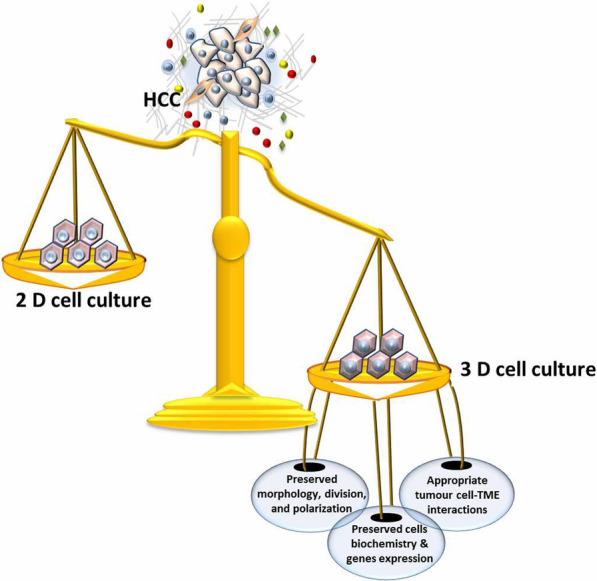
2D cell cultures are a well-known, attractive laboratory method used for simple assays that probe cell physiology and behaviour. In 2D cultures, the cell culture monolayer grows on polystyrene or glass materials in a simple environment that does not realistically recapitulate in vivo tissue physiology. Therefore, the resultant cells usually have modifications in their architecture, polarity, biochemical signalling, and, importantly, cell–cell interactions [9]. Additionally, in 2D tumour cell cultures, several major features of cancer cells, including heterogeneity as well as morphological and genetic profiles, are mostly lost [8]. Hence, switching from a 2D system to a 3D system may provide a better simulation of the complex biology of malignant tumours for study. An ideal 3D culture would overcome 2D culture limitations and allow direct drug applications in human models by conserving the original cell morphology, polarity, heterogeneity, and genetic profile of both neoplastic and non-neoplastic stromal cells [8, 44]. Although there are great advantages of 3D culture versus 2D culture, the simplicity and low cost of 2D systems, as well as the lack of a universal model for a 3D system, has limited the use of 3D cultures. Currently, several 3D culture models have been developed for liver, pancreatic, and breast cancer to clarify the role of the tumour-TME interaction in drug resistance [45–48]. Interestingly, 3D tumour homo-spheroids were observed to exhibit increased resistance to tested chemotherapy compared to the responses in 2D cancer models [49–51]. The advantages and disadvantages of 3D and 2D cell culture systems are summarized in Table 1.
Table 1.
Advantages and disadvantages of three dimensional (3D) and two dimensional (2D) cell culture systems
| Items | 2D cell culture | 3D cell culture | Refs. | |
|---|---|---|---|---|
| Disadvantages | Time required for culture formation | Minutes to a few hours | A few hours to a few days | [52] |
| Quality of culture |
Simple long-term culture Easy to interpret results High performance and reproducibility |
More difficult to culture Difficult to interpret results Poor performance and reproducibility | [53] | |
| Cost of culture maintenance |
Less time consuming Inexpensive Commercially available media and assay materials |
More time consuming More expensive Fewer commercially available assay materials |
[44, 45] | |
| Advantages | In vivo imitation | Cannot mimic the natural tumour mass structure | Can mimic in vivo tissue structures | [55] |
| Cell interactions |
No cell–cell or cell- extracellular microenvironment interactions No “niches” or in vivo-like microenvironment |
Appropriate cell–cell and cell-extracellular microenvironment interactions Microenvironment “niches” are present |
[56–58] | |
| CellCharacteristics |
Altered morphology from physiological tissue Altered cell division activity Lack of diverse phenotypes and polarization |
Preserved morphology Preserved cell division activity Presence of diverse phenotypes and polarization |
[59, 60] | |
| Access to essential compounds | Limited access to nutrients, oxygen, metabolites, and signalling molecules | Variable access to nutrients, oxygen, metabolites, and signalling molecules | [61, 62] | |
| Molecular mechanisms |
Alterations in cellular biochemistry Alterations in gene expression, mRNA splicing, and topology |
Preserved cellular biochemistry Preserved gene expression, mRNA splicing, and topology |
[63, 64] | |
| Angiogenesis | Only observational | Could be functional | [65] | |
| Mathematical model | Possible | Better geometry and structure–function links | [65] | |
Biomaterial-based 3D liver models
The construction of three-dimensional (3D) tissue models in vitro is critical for drug discovery research and development. The use of biomaterials to improve the design of cell function and activity is critical in this regard. Despite the fact that the 2D and 3D systems were utilized for different purposes, the 3D culture is preferable in terms of drug development because it closely resembles the in vivo cancer environment. The active use of biomaterials is another way for improving cell functioning [66].
Cell culture is frequently carried out on a dish or plate made primarily of polystyrene. Because the artificial environment differs significantly from the in vivo body environment of cancer cells, evaluating therapeutic impact or cytotoxicity is technologically constrained. Biomaterials containing extracellular matrix (ECM) components have been shown to improve cell activity and function. Cells will be able to improve their proliferation, differentiation, and biological capabilities as a result of their interaction with biomaterials, resulting in the realisation of cancer cell–environment interaction. Several studies have been published on 3D cancer models integrated with biomaterials to reproduce the cancer environment and illnesses in vitro [67–70].
Natural biomaterials are sourced from animals or plants, while synthetic biomaterials are created artificially. Polysaccharide (amylose, cellulose, alginate, chitosan, or hyaluronic acid), peptide (collagen or gelatin), nucleic acid, or polyhydroxyalkanoates are all examples of natural biomaterials. Most natural biomaterials can be destroyed enzymatically since the degradative enzyme and metabolic system already exist in the body [71]. Natural biomaterials are frequently employed to construct the 3D culture system of cancer cells because the components that make up the cancer environment, such as the ECM, contribute to cancer diseases. Although natural biomaterials are highly biocompatible, they do have some immunogenicity and homogeneity limits. Synthetic biomaterials are employed to avoid the problems. The majority of synthetic biomaterials are destroyed nonenzymatically through simple hydrolysis. Synthetic biomaterials have several advantages, such as the ability to control characteristics, high rigidity, and property clarity [66].
Several 3D cancer cell culture systems including biomaterials are presented. In the 3D culturing system of cancer cells, two types of biomaterials have been used so far. One is a cancer cell culturing system using biomaterials in a spherical shape. Cancer cells spontaneously form a cell aggregate with a tissue-like 3D structure when incubated with microspheric hydrogels of biomaterial, which simulates the cancer environment [72]. The difficulty of separating cells from cell-hydrogel complexes is one of the system's drawbacks, and as a result, the results are sometimes inconsistent. The other is a cancer cell culture method using non-spherical biomaterials such as sponge forms or nonwoven textiles. Cells effectively multiply and move on the scaffold in this system; this form is appropriate for immunohistochemistry [66].
Basement membrane extract (BME/Matrigel) is a well-defined soluble basement membrane extract that derived from an epithelial tumor [73]. It has a composition similar to real basement membrane and forms a hydrogel at 24–37 °C [74]. It's utilized in vitro as a 3D cell culture substrate, in suspension for spheroid culture, and for a variety of tests, including angiogenesis, invasion, and dormancy. However in vivo, BME/Matrigel is used for angiogenesis experiments and to promote the take and growth of xenograft and patient-derived biopsy samples [75]. According to several studies, the rigidity of the BME/Matrigel and its components are both responsible for its activity with so many distinct cell types. BME/Matrigel is widely used in assays and models to help the better understanding of tumor biology and develop treatment methods [73].
Individual tumor types can be better modeled with BME/Matrigel. For example, new stiffer and acidic matrices including extra ECM proteins are holding promise for more physiologically relevant models because they better simulate tumor settings. Coculture in vitro and in vivo has advanced the establishment of a physiological tumor microenvironment significantly [73, 76]. Many malignancies are fibrotic, and the use of fibroblasts has helped us better understand how these cells interact with tumors [77]. Cancer stem cells have emerged as a key 'actor' in the tumor field, with BME/Matrigel-based assays assisting in defining their identity, biology, and involvement in malignancy. When BME/Matrigel was first characterized in 1986 as a "basement membrane complex with biological activity," it seemed to play a key function in cell differentiation [73]. Multiple uses in cancer biology, such as 3D culture, invasion assays, endothelial tube tests, dormancy assays, multicellular tumor spheroids, xenografts, and patient-derived xenografts, were not anticipated [78].
In terms of tumor metastasis, coculture of tumor cells with endothelial cells has revealed some unexpected interactions for some tumor types with vasculature [79]. The use of a BME/Matrigel based assay to better understand the genes and processes of this type of metastatic spread along the outside of vasculature and nerves will begin to address the selection of therapeutic methods.
Development of novel 3D models for HCC
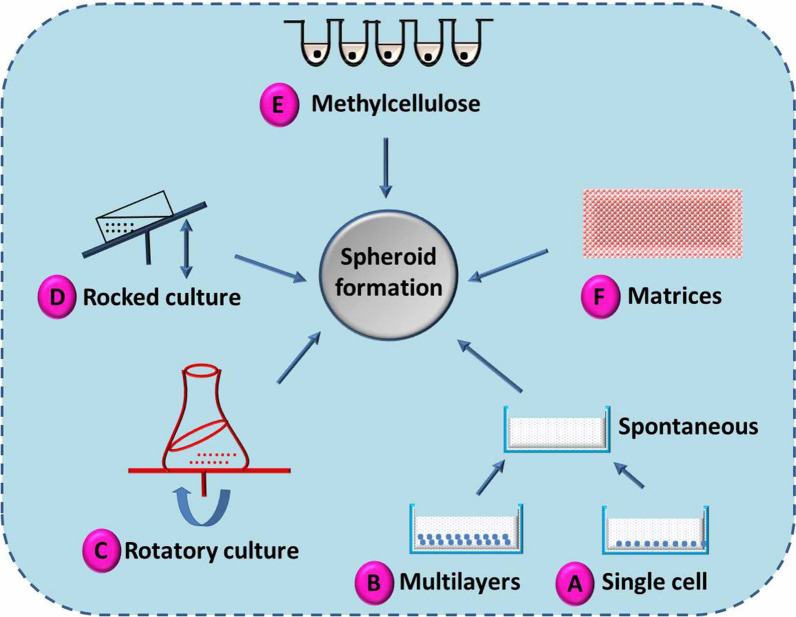
The aggregation of cells into a spheroid structure provides the advantage of minimizing the exposed cell surface area [64, 80], with marked mimicking of natural cell organogenesis and morphogenesis [81]. Hence, the development of 3D spheroid cultures may be vital to investigate in vivo systems more efficiently, including cell morphology and the surrounding environment, which are reflected in the biological behaviour and gene expression of the cells. Several approaches are well established for the generation of 3D spheroid structures (Fig. 3).
Fig. 3.
Various approaches for the development of 3D spheroid systems
Recently, a variety of 3D models have been developed to better understand the molecular and cellular interactions between various cell types with regard to HCC progression [82, 83]. In 2011, Tang and colleagues [84] established a novel 3D model for metastatic HCC by culturing MHCC97H cells on molecular scaffolds. Chemical, morphological, and pathological characterizations of the model showed several attributes that mirrored in vivo HCC, such as the morphological and ultrastructural features of neoplastic cells, gene expression patterns, apoptotic signals, glucose metabolism, and protein production. Additionally, xenografts of such 3D HCC spheroids in nude mice livers led to carcinogenesis and distant metastatic effects.
Another model of 3D multicellular hetero-spheroids was established by Yip and Cho [51] in a collagen hydrogel culture system to investigate the effect of TME, multicellularity, and the ECM barrier on the potential resistance of the tested anticancer drug. The uniform hetero-spheroid was formed with the hanging drop method and via co-culture of stromal fibroblasts with liver carcinoma followed by encapsulation in collagen gel to form a 3D spheroid. The results revealed that the chemotherapeutic resistance of the 3D hetero-spheroid model was higher than that of the homo-spheroid cultures and the 2D monolayer culture. In another study, Liu et al., [85] explored the relationship between HCC therapeutic resistance and 3D matrix stiffness using a model of alginate gel (ALG) beads with controlled matrix rigidity. They concluded that HCC cells in the ALG model with 105 kPa stiffness showed the highest therapeutic resistance against cisplatin, 5-FU, and paclitaxel. The authors suggested the role of endoplasmic reticulum stress-related genes in HCC drug resistance due to their upregulation in the 3D model compared to the 2D model.
In 2015, Terashima and colleagues [86] studied the expression of the drug-metabolizing enzymes CYP1A1 and CYP1A2 and their encoding genes in a 3D spheroid model of HCC cells (JHH1, Huh7, and HepG2). Results confirmed the increased expression of CYP1A1 and CYP1A2 in 3D spheroids compared to 2D cultured cells. As such, the authors concluded that the pregnane X receptor (PXR) increased CYP1A2 expression in JHH1, HepG2, and Huh7 spheroids. This study demonstrated the variation in gene expression between 3D spheroids and 2D cultured cells and between two different culture conditions.
Liu et al. [85] investigated the safety of in vitro co-culturing of umbilical cord mesenchymal stem cells (UCMSC), a common vehicle for anticancer drug delivery, on the growth and characteristics of cancer stem cells (CSCs) and on metastasis and therapeutic resistance of 3D-cultured HCC cells. The authors concluded that the metastatic ability of 3D HCC spheroids was greatly enhanced compared to the other cultures; this increase was confirmed to be due to upregulation of migration abilities, the expression of matrix metalloproteinases (MMPs), and EMT-related genes. However, the therapeutic resistance and cell growth of HCC cells were not affected. Moreover, the addition of the TGF-β receptor inhibitor SB431542 into 3D HCC cultures resulted in the reversion of EMT and downregulation of MMP-2 and migration ability.
Takai et al. [87] studied the biological features and signalling pathways of tumour cells in a 3D organoid-like spheroid model for HCC. They demonstrated that 3D spheroid cells could mimic the in vivo features of glandular epithelium and hepatic stem cells. Moreover, the authors showed the role of Wnt/β-catenin signalling activation in EpCAM + HCC spheroid formation and reported the chemotherapeutic resistance of EpCAM + HCC spheroids and their sensitivity to TGF-β-induced EMT.
Interestingly, Jung and colleagues [48] established a spheroid-forming unit to produce economic, large, and homogenous spheroids of liver neoplastic cells using Huh7 HCC cells. In these spheroids, proliferation and apoptotic signalling were present at the surface and centre of the spheroids, respectively, due to activation of ERK signal and hypoxia-induced factor-1 alpha (HIF-1α). Co-culturing of Huh7 HCC spheroids with 2% human umbilical vein endothelial cells (HUVECs) led to the expression of HCC-related genes, with a subsequent reduction in necrosis at the spheroid core and enhanced tumorigenic characteristics. Moreover, these 3D Huh7 cell spheroids showed increased therapeutic resistance against high concentrations of the chemotherapeutic drugs doxorubicin and sorafenib.
Recently, Sun et al. [88] developed novel 3D spheroid cell cultures by culturing HCCLM3 cells in 1% de-cellularized liver matrix-alginate (DLM–ALG) hybrid gel beads. They demonstrated that the DLM–ALG beads enhanced the activities of matrix MMPs, including MMP-2 and MMP-9, in HCCLM3 cells; a direct relationship was detected between MMP activities in HCCLM3 cells and the concentration of DLM powder used.
Another 3D HCC system was developed by Le et al. [89]; this model consisted of HCC cells, stromal cells in the form of fibroblasts, and nanofibrous membranes to imitate the complex TME. This model was fabricated by three methods of culturing: (1) a mono model in which tumour cells grow directly on the nanofibrous membrane, (2) a layer model in which fibroblasts grow on the nanofibrous membrane, and (3) a mixed model in which both tumour cells and fibroblasts develop on the nanofibrous membrane. Results showed that both the mono and layer models exhibited similar tissue features, while the mixed model resulted in phenotypic alterations of the neoplastic cells. In addition, the authors concluded that the mixed models enhanced the neoplastic cells’ resistance to chemotherapeutic drugs as well as the expression of vimentin and fibronectin.
Another 3D mixed-cell spheroid model using Huh-7 HCC cells and LX-2 stellate cells was recently developed by Khawar et al. [14] to mimic the natural in vivo TME and tumour-CAF interactions. The 3D system was cultured as mono-spheroids by culturing tumour cells alone or as mixed-cell spheroids in ultra-low attachment plates. ed Results showed enhanced type I collagen production and expression of pro‐fibrotic factors, including TGF-β1 and CTGF, compared to their levels in mono-spheroids. In addition, the expression of vimentin and E-cadherin was changed in the mixed-cell spheroids; these proteins promote the EMT phenotype. Drug sensitivity was enhanced in mixed-cell spheroids, and an anti-proliferative effect was shown only after combined treatment with sorafenib and oxaliplatin in a dose-dependent manner. Co-treatment with TGF-β inhibitors enhanced the therapeutic activity of sorafenib in the mixed-cell spheroids, suggesting the role of TGF-β in drug resistance.
Ma et al. [90] recently cultured HCC cell lines and fresh primary tumour cells in serum-free and ultra-low attachment conditions to enable the forming of HCC spheres and discovered that all cell lines and primary tumour cells shaped spheres. HCC spheres were capable of self-renewal, replication, and drug tolerance, as well as containing various subpopulations of CSCs. In immunocompromised animals, 500 sphere-forming Huh7 cells or 200 primary tumour cells could produce tumours. The shape of spheres was associated with tumour scale, numerous tumours, satellite lesions, and advanced stage. They came to the conclusion that there-forming culture would effectively enrich subpopulations with stem-cell properties, which are retained by activating the PPAR-SCD1 axis.
Xie et al. [91] developed a novel modelling method utilising three-dimensional (3D) bioprinting technology and constructed hepatorganoids with HepaRG cells, which maintain liver function and extend the survival of mice with liver failure after abdominal transplantation in an updated review. Following surgery, they collected HCC specimens from six people. Following that, patient-derived three-dimensional bio-printed HCC (3DP-HCC) models were successfully developed and grew well in long-term culture. These models maintained the characteristics of parental HCCs, such as stable biomarker expression, stable genetic mutations, and expression profiles. 3DP-HCC models are capable of showing drug screening outcomes both intuitively and quantitatively. They conclude that 3DP-HCC models are faithful in vitro models that can forecast patient-specific drugs for customised care and are accurate in long-term culture.
Overall, these results confirmed that different models of HCC 3D cell spheroids efficiently represent the physiological in vivo structure and function of HCC and the TME. Thus, these 3D models could be useful in advancing the study of tumour-stroma interactions as well as the molecular mechanisms underlying the therapeutic resistance of HCC.
Conclusion
The development of an optimal experimental model is necessary to maximize the usefulness of preclinical investigations and to pave the way for creating and testing more novel, potential therapeutic drugs. Accordingly, obtaining in vitro models with high similarity to the natural in vivo conditions of HCC is key in future cancer studies. The use of 3D spheroid culture of HCC cells is promising for clarifying tumour-TME interactions and the mechanistic details of chemotherapeutic resistance, as well as for subsequently detecting more safe and effective anti-neoplastic drugs.
Acknowledgements
Not applicable.
Author contributions
AFK designed and drafted this article. SAM contributed to visualization. LA, MMA revised the manuscript. All authors participated in the review, editing, and revision of the manuscript. All authors read and approved the final manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Asmaa F. Khafaga, Email: asmaa.khafaga@alexu.edu.eg
Mohamed M. Abdel-Daim, Email: abdeldaim.m@vet.suez.edu.eg
References
- 1.El-Serag HB. Hepatocellular carcinoma: recent trends in the United States. Gastroenterology. 2004;127(5):27–34. doi: 10.1053/j.gastro.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J cancer. 2015;136(5):359–386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 3.De Toni EN, Schlesinger-Raab A, Fuchs M, Schepp W, Ehmer U, Geisler F, Ricke J, Paprottka P, Friess H, Werner J, Gerbes AL. Age independent survival benefit for patients with hepatocellular carcinoma (HCC) without metastases at diagnosis: a population-based study. Gut. 2020;69(1):168–176. doi: 10.1136/gutjnl-2018-318193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song Y, Kim JS, Kim SH, Park YK, Yu E, Kim KH, Seo HR. Patient-derived multicellular tumor spheroids towards optimized treatment for patients with hepatocellular carcinoma. J Exp Clin Cancer Res. 2018;37(1):1–13. doi: 10.1186/s13046-018-0752-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pietras K, Östman A. Hallmarks of cancer: interactions with the tumor stroma. Exp cell res. 2010;316(8):1324–1331. doi: 10.1016/j.yexcr.2010.02.045. [DOI] [PubMed] [Google Scholar]
- 6.McMillin DW, Negri JM, Mitsiades CS. The role of tumour–stromal interactions in modifying drug response: challenges and opportunities. Nat Rev Drug Discovery. 2013;12(3):217–228. doi: 10.1038/nrd3870. [DOI] [PubMed] [Google Scholar]
- 7.Zanconato F, Cordenonsi M, Piccolo S. YAP and TAZ: a signalling hub of the tumour microenvironment. Nat Rev Cancer. 2019;19(8):454–464. doi: 10.1038/s41568-019-0168-y. [DOI] [PubMed] [Google Scholar]
- 8.Hoarau-Véchot J, Rafii A, Touboul C, Pasquier J. Halfway between 2D and animal models: are 3D cultures the ideal tool to study cancer-microenvironment interactions? Int J molec sci. 2018;19(1):181. doi: 10.3390/ijms19010181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamada KM, Cukierman E. Modeling tissue morphogenesis and cancer in 3D. Cell. 2007;130(4):601–610. doi: 10.1016/j.cell.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Saglam-Metiner P, Sultan G, Cigir BA. Bioengineering-inspired three-dimensional culture systems: organoids to create tumor microenvironment. Gene. 2019;686:203–212. doi: 10.1016/j.gene.2018.11.058. [DOI] [PubMed] [Google Scholar]
- 11.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 12.Sia D, Villanueva A, Friedman SL, Llovet JM. Liver cancer cell of origin, molecular class, and effects on patient prognosis. Gastroenterology. 2017;152(4):745–761. doi: 10.1053/j.gastro.2016.11.048. [DOI] [PubMed] [Google Scholar]
- 13.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61(4):212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 14.Khawar IA, Park JK, Jung ES, Lee MA, Chang S, Kuh HJ. Three dimensional mixed-cell spheroids mimic stroma-mediated chemoresistance and invasive migration in hepatocellular carcinoma. Neoplasia. 2018;20(8):800–812. doi: 10.1016/j.neo.2018.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bruix J, Colombo M. Hepatocellular carcinoma: current state of the art in diagnosis and treatment. Best Pract Res Clin Gastroenterol. 2014;28(5):751. doi: 10.1016/j.bpg.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Marchetti A, Bisceglia F, Cozzolino AM, Tripodi M. New tools for molecular therapy of hepatocellular carcinoma. Diseases. 2015;3(4):325–340. doi: 10.3390/diseases3040325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sia D, Llovet JM. Translating'–omics' results into precision medicine for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2017;14(10):571–572. doi: 10.1038/nrgastro.2017.103. [DOI] [PubMed] [Google Scholar]
- 18.Llovet JM. Burroughs A, and Bruix. J Hepatocellular carcinoma Lancet. 2003;362:1907–1917. doi: 10.1016/S0140-6736(03)14964-1. [DOI] [PubMed] [Google Scholar]
- 19.Bupathi M, Kaseb A, Meric-Bernstam F, Naing A. Hepatocellular carcinoma: where there is unmet need. Mol Oncol. 2015;9(8):1501–1509. doi: 10.1016/j.molonc.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown KS. Chemotherapy and other systemic therapies for hepatocellular carcinoma and liver metastases. In: Seminars in interventional radiology, Vol. 23, No. 1. Thieme Medical Publishers; 2006, 99. 10.1055/s-2006-939845 [DOI] [PMC free article] [PubMed]
- 21.Waly RS, Yangde Z, YuXiang C. Hepatocellular carcinoma: focus on different aspects of management. Int Scholar Res Notices. 2012 doi: 10.5402/2012/421673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deng GL, Zeng S, Shen H. Chemotherapy and target therapy for hepatocellular carcinoma: New advances and challenges. World J Hepatol. 2015;7(5):787. doi: 10.4254/wjh.v7.i5.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Couri T, Anjana P. Goals and targets for personalized therapy for HCC. Hep Intl. 2019;13(2):125–137. doi: 10.1007/s12072-018-9919-1. [DOI] [PubMed] [Google Scholar]
- 24.Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, De Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 25.Nishida N, Kitano M, Sakurai T, Kudo M. Molecular mechanism and prediction of sorafenib chemoresistance in human hepatocellular carcinoma. Dig Dis. 2015;33(6):771–779. doi: 10.1159/000439102. [DOI] [PubMed] [Google Scholar]
- 26.Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21(3):309–322. doi: 10.1016/j.ccr.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 27.Khawar IA, Kim JH, Kuh HJ. Improving drug delivery to solid tumors: priming the tumor microenvironment. J Control Release. 2015;201:78–89. doi: 10.1016/j.jconrel.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 28.Hernandez-Gea V, Toffanin S, Friedman SL, Llovet JM. Role of the microenvironment in the pathogenesis and treatment of hepatocellular carcinoma. Gastroenterology. 2013;144(3):512–527. doi: 10.1053/j.gastro.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen F, Zhong Z, Tan HY, Wang N, Feng Y. The Significance of circulating tumor cells in patients with hepatocellular carcinoma: real-time monitoring and moving targets for cancer therapy. Cancers. 2020;12(7):1734. doi: 10.3390/cancers12071734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leonardi GC, Candido S, Cervello M, Nicolosi D, Raiti F, Travali S, Spandidos DA, Libra M. The tumor microenvironment in hepatocellular carcinoma. Int J Oncol. 2012;40(6):1733–1747. doi: 10.3892/ijo.2012.1408. [DOI] [PubMed] [Google Scholar]
- 31.Tlsty TD, Coussens LM. Tumor stroma and regulation of cancer development. Annu Rev Pathol Mech Dis. 2006;1:119–150. doi: 10.1146/annurev.pathol.1.110304.100224. [DOI] [PubMed] [Google Scholar]
- 32.Friedl P, Alexander S. Cancer invasion and the microenvironment: plasticity and reciprocity. Cell. 2011;147(5):992–1009. doi: 10.1016/j.cell.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 33.Kubo N, Araki K, Kuwano H, Shirabe K. Cancer-associated fibroblasts in hepatocellular carcinoma. World J Gastroenterol. 2016;22(30):6841. doi: 10.3748/wjg.v22.i30.6841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Affo S, Yu LX, Schwabe RF. The role of cancer-associated fibroblasts and fibrosis in liver cancer. Annu Rev Pathol. 2017;12:153–186. doi: 10.1146/annurev-pathol-052016-100322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carloni V, Luong TV, Rombouts K. Hepatic stellate cells and extracellular matrix in hepatocellular carcinoma: more complicated than ever. Liver Int. 2014;34(6):834–843. doi: 10.1111/liv.12465. [DOI] [PubMed] [Google Scholar]
- 36.Coulouarn C, Clément B. Stellate cells and the development of liver cancer: therapeutic potential of targeting the stroma. J Hepatol. 2014;60(6):1306–1309. doi: 10.1016/j.jhep.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 37.Yang MC, Wang CJ, Liao PC, Yen CJ, Shan YS. Hepatic stellate cells secretes type I collagen to trigger epithelial mesenchymal transition of hepatoma cells. Am J Cancer Res. 2014;4(6):751. [PMC free article] [PubMed] [Google Scholar]
- 38.Kobayashi H, Enomoto A, Woods SL, Burt AD, Takahashi M, Worthley DL. Cancer-associated fibroblasts in gastrointestinal cancer. Nat Rev Gastroenterol Hepatol. 2019;16(5):282–295. doi: 10.1038/s41575-019-0115-0. [DOI] [PubMed] [Google Scholar]
- 39.Tarin D. Clinical and biological implications of the tumor microenvironment. Cancer microenvironment. 2012;5(2):95–112. doi: 10.1007/s12307-012-0099-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mazzocca A, Fransvea E, Dituri F, Lupo L, Antonaci S, Giannelli G. Down-regulation of connective tissue growth factor by inhibition of transforming growth factor β blocks the tumor–stroma cross-talk and tumor progression in hepatocellular carcinoma. Hepatology. 2010;51(2):523–534. doi: 10.1002/hep.23285. [DOI] [PubMed] [Google Scholar]
- 41.He L, Tian DA, Li PY, He XX. Mouse models of liver cancer: Progress and recommendations. Oncotarget. 2015;6(27):23306. doi: 10.18632/oncotarget.4202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cekanova M, Rathore K. Animal models and therapeutic molecular targets of cancer: utility and limitations. Drug Des Dev Ther. 1911;2014:8. doi: 10.2147/DDDT.S49584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Voskoglou-Nomikos T, Pater JL, Seymour L. Clinical predictive value of the in vitro cell line, human xenograft, and mouse allograft preclinical cancer models. Clin Cancer Res. 2003;9(11):4227–4239. [PubMed] [Google Scholar]
- 44.Weiswald LB, Bellet D, Dangles-Marie V. Spherical cancer models in tumor biology. Neoplasia. 2015;17(1):1–15. doi: 10.1016/j.neo.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Majety M, Pradel LP, Gies M, Ries CH. Fibroblasts influence survival and therapeutic response in a 3D co-culture model. PLoS ONE. 2015;10(6):e0127948. doi: 10.1371/journal.pone.0127948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Song Y, Kim SH, Kim KM, Choi EK, Kim J, Seo HR. Activated hepatic stellate cells play pivotal roles in hepatocellular carcinoma cell chemoresistance and migration in multicellular tumor spheroids. Sci Rep. 2016;6(1):1–14. doi: 10.1038/s41598-016-0001-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ware MJ, Keshishian V, Law JJ, Ho JC, Favela CA, Rees P, Mith B, Mohammad S, Hwang RF, Rajapakshe K, Coarfa C, Curley SA. Generation of an in vitro 3D PDAC stroma rich spheroid model. Biomaterials. 2016;108:129–142. doi: 10.1016/j.biomaterials.2016.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jung HR, Kang HM, Ryu JW, Kim DS, Noh KH, Kim ES, Lee HJ, Chung KS, Cho HS, Kim NS, Im DS. Cell spheroids with enhanced aggressiveness to mimic human liver cancer in vitro and in vivo. Sci Rep. 2017;7(1):1–14. doi: 10.1038/s41598-016-0028-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang TM, Barbone D, Fennell DA, Broaddus VC. Bcl-2 family proteins contribute to apoptotic resistance in lung cancer multicellular spheroids. Am J Respir Cell Mol Biol. 2009;41(1):14–23. doi: 10.1165/rcmb.2008-0320OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hirschhaeuser F, Menne H, Dittfeld C, West J, Mueller-Klieser W, Kunz-Schughart LA. Multicellular tumor spheroids: an underestimated tool is catching up again. J Biotechnol. 2010;148(1):3–15. doi: 10.1016/j.jbiotec.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 51.Yip D, Cho CH. A multicellular 3D heterospheroid model of liver tumor and stromal cells in collagen gel for anti-cancer drug testing. Biochem Biophys Res Commun. 2013;433(3):327–332. doi: 10.1016/j.bbrc.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 52.Baker BM, Chen CS. Deconstructing the third dimension–how 3D culture microenvironments alter cellular cues. J Cell Sci. 2012;125(13):3015–3024. doi: 10.1242/jcs.079509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hickman JA, Graeser R, de Hoogt R, Vidic S, Brito C, Gutekunst M, van der Kuip H. Three-dimensional models of cancer for pharmacology and cancer cell biology: capturing tumor complexity in vitro/ex vivo. Biotechnol J. 2014;9(9):1115–1128. doi: 10.1002/biot.201300492. [DOI] [PubMed] [Google Scholar]
- 54.Krishnamurthy S, Nör JE. Orosphere assay: a method for propagation of head and neck cancer stem cells. Head Neck. 2013;35(7):1015–1021. doi: 10.1002/hed.23076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Griffith LG, Swartz MA. Capturing complex 3D tissue physiology in vitro. Nat Rev Mol Cell Biol. 2006;7(3):211–224. doi: 10.1038/nrm1858. [DOI] [PubMed] [Google Scholar]
- 56.Cawkill D, Eaglestone SS. Evolution of cell-based reagent provision. Drug Discovery Today. 2007;12(19–20):820–825. doi: 10.1016/j.drudis.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 57.Lee J, Cuddihy MJ, Kotov NA. Three-dimensional cell culture matrices: state of the art. Tissue Eng Part B Rev. 2008;14(1):61–86. doi: 10.1089/teb.2007.0150. [DOI] [PubMed] [Google Scholar]
- 58.Gilbert PM, Havenstrite KL, Magnusson KE, Sacco A, Leonardi NA, Kraft P, Nguyen NK, Thrun S, Lutolf MP, Blau HM. Substrate elasticity regulates skeletal muscle stem cell self-renewal in culture. Science. 2010;329(5995):1078–1081. doi: 10.1126/science.1191035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mseka T, Bamburg JR, Cramer LP. ADF/cofilin family proteins control formation of oriented actin-filament bundles in the cell body to trigger fibroblast polarization. J Cell Sci. 2007;120(24):4332–4344. doi: 10.1242/jcs.017640. [DOI] [PubMed] [Google Scholar]
- 60.Kilian KA, Bugarija B, Lahn BT, Mrksich M. Geometric cues for directing the differentiation of mesenchymal stem cells. Proc Natl Acad Sci. 2010;107(11):4872–4877. doi: 10.1073/pnas.0903269107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Frieboes HB, Zheng X, Sun CH, Tromberg B, Gatenby R, Cristini V. An integrated computational/experimental model of tumor invasion. Can Res. 2006;66(3):1597–1604. doi: 10.1158/0008-5472.CAN-05-3166. [DOI] [PubMed] [Google Scholar]
- 62.Breslin S, O’Driscoll L. Three-dimensional cell culture: the missing link in drug discovery. Drug Discovery Today. 2013;18(5–6):240–249. doi: 10.1016/j.drudis.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 63.Birgersdotter A, Sandberg R, Ernberg I. Gene expression perturbation in vitro—a growing case for three-dimensional (3D) culture systems. Semin Cancer Biol. 2005 doi: 10.1016/j.semcancer.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 64.Ghosh S, Spagnoli GC, Martin I, Ploegert S, Demougin P, Heberer M, Reschner A. Three-dimensional culture of melanoma cells profoundly affects gene expression profile: a high density oligonucleotide array study. J Cell Physiol. 2005;204(2):522–531. doi: 10.1002/jcp.20320. [DOI] [PubMed] [Google Scholar]
- 65.Hoarau-Véchot J, Rafii A, Touboul C, Pasquier J. Halfway between 2D and animal models: are 3D cultures the ideal tool to study cancer-microenvironment interactions? Int J Mol Sci. 2018;19(1):181. doi: 10.3390/ijms19010181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nii T, Makino K, Tabata Y. Three-dimensional culture system of cancer cells combined with biomaterials for drug screening. Cancers. 2020;12(10):2754. doi: 10.3390/cancers12102754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fridman IB, Kostas J, Gregus M, Ray S, Sullivan MR, Ivanov AR, Cohen S, Konry T. High-throughput microfluidic 3D biomimetic model enabling quantitative description of the human breast tumor microenvironment. Acta Biomater. 2021;132:473–488. doi: 10.1016/j.actbio.2021.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Turtoi M, Anghelache M, Bucatariu SM, Deleanu M, Voicu G, Safciuc F, Manduteanu I, Fundueanu G, Simionescu M, Calin M. A novel platform for drug testing: Biomimetic three-dimensional hyaluronic acid-based scaffold seeded with human hepatocarcinoma cells. Int J Biol Macromol 2021;185:604-619. [DOI] [PubMed]
- 69.Nii T, Toshie K, Kimiko M, Yasuhiko T. A co-culture system of three-dimensional tumor-associated macrophages and three-dimensional cancer-associated fibroblasts combined with biomolecule release for cancer cell migration. Tissue Eng Part A. 2020;26(23–24):1272–1282. doi: 10.1089/ten.tea.2020.0095. [DOI] [PubMed] [Google Scholar]
- 70.Le MCN, Xu K, Wang Z, Beverung S, Steward RL, Florczyk SJ. Evaluation of the effect of 3D porous Chitosan-alginate scaffold stiffness on breast cancer proliferation and migration. J Biomed Mater Res, Part A. 2021;109(10):1990–2000. doi: 10.1002/jbm.a.37191. [DOI] [PubMed] [Google Scholar]
- 71.Bassas-Galia M, Follonier S, Pusnik M, Zinn M. Natural polymers: A source of inspiration. In: Bioresorbable polymers for biomedical applications. Woodhead Publishing. 2017, pp. 31–64. 10.1016/B978-0-08-100262-9.00002-1
- 72.Park Y, Huh KM, Kang SW. Applications of biomaterials in 3D cell culture and contributions of 3D cell culture to drug development and basic biomedical research. Int J Mol Sci. 2021;22(5):2491. doi: 10.3390/ijms22052491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Benton G, Arnaoutova I, George J, Kleinman HK, Koblinski J. Matrigel: from discovery and ECM mimicry to assays and models for cancer research. Adv Drug Deliv Rev. 2014;15(79):3–18. doi: 10.1016/j.addr.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 74.Xue H, Hu L, Xiong Y, Zhu X, Wei C, Cao F, Zhou W, Sun Y, Endo Y, Liu M, Liu Y. Quaternized chitosan-Matrigel-polyacrylamide hydrogels as wound dressing for wound repair and regeneration. Carbohyd Polym. 2019;15(226):115302. doi: 10.1016/j.carbpol.2019.115302. [DOI] [PubMed] [Google Scholar]
- 75.Liu X, Fang J, Huang S, Wu X, Xie X, Wang J, Liu F, Zhang M, Peng Z, Hu N. Tumor-on-a-chip: From bioinspired design to biomedical application. Microsyst Nanoeng. 2021;7(1):1–23. doi: 10.1038/s41378-020-00227-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cox MC, Reese LM, Bickford LR, Verbridge SS. Toward the broad adoption of 3D tumor models in the cancer drug pipeline. ACS Biomater Sci Eng. 2015;1(10):877–894. doi: 10.1021/acsbiomaterials.5b00172. [DOI] [PubMed] [Google Scholar]
- 77.Sahai E, Astsaturov I, Cukierman E, DeNardo DG, Egeblad M, Evans RM, Fearon D, Greten FR, Hingorani SR, Hunter T, Hynes RO. A framework for advancing our understanding of cancer-associated fibroblasts. Nat Rev Cancer. 2020;20(3):174–186. doi: 10.1038/s41568-019-0238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Radhakrishnan J, Varadaraj S, Dash SK, Sharma A, Verma RS. Organotypic cancer tissue models for drug screening: 3D constructs, bioprinting and microfluidic chips. Drug Discov Today. 2020;25(5):879–890. doi: 10.1016/j.drudis.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 79.Buess M, Rajski M, Vogel-Durrer BM, Herrmann R, Rochlitz C. Tumor-Endothelial interaction links the CD44+/CD24-phenotype with poor prognosis in early-stage breast cancer. Neoplasia. 2009;11(10):987–1002. doi: 10.1593/neo.09670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yeo M, Chae S, Kim G. An in vitro model using spheroids-laden nanofibrous structures for attaining high degree of myoblast alignment and differentiation. Theranostics. 2021;11(7):3331. doi: 10.7150/thno.53928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Duguay D, Foty RA, Steinberg MS. Cadherin-mediated cell adhesion and tissue segregation: qualitative and quantitative determinants. Dev Biol. 2003;253(2):309–323. doi: 10.1016/S0012-1606(02)00016-7. [DOI] [PubMed] [Google Scholar]
- 82.Van Zijl F, Mikulits W. Hepatospheres: Three dimensional cell cultures resemble physiological conditions of the liver. World J Hepatol. 2010;2(1):1. doi: 10.4254/wjh.v2.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kim E, Lisby A, Ma C, Lo N, Ehmer U, Hayer KE, Furth EE, Viatour P. Promotion of growth factor signaling as a critical function of β-catenin during HCC progression. Nat Commun. 2019;10(1):1–17. doi: 10.1038/s41467-018-07882-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tang J, Cui J, Chen R, Guo K, Kang X, Li Y, Gao D, Sun L, Xu C, Chen J, Tang Z. A three-dimensional cell biology model of human hepatocellular carcinoma in vitro. Tumor Biol. 2011;32(3):469–479. doi: 10.1007/s13277-010-0140-7. [DOI] [PubMed] [Google Scholar]
- 85.Liu C, Liu Y, Xie HG, Zhao S, Xu XX, Fan LX, Guo X, Lu T, Sun GW, Ma XJ. Role of three-dimensional matrix stiffness in regulating the chemoresistance of hepatocellular carcinoma cells. Biotechnol Appl Biochem. 2015;62(4):556–562. doi: 10.1002/bab.1302. [DOI] [PubMed] [Google Scholar]
- 86.Terashima J, Goto S, Hattori H, Hoshi S, Ushirokawa M, Kudo K, Habano W, Ozawa S. CYP1A1 and CYP1A2 expression levels are differentially regulated in three-dimensional spheroids of liver cancer cells compared to two-dimensional monolayer cultures. Drug Metab Pharmacokinet. 2015;30(6):434–440. doi: 10.1016/j.dmpk.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 87.Takai A, Fako V, Dang H, Forgues M, Yu Z, Budhu A, Wang XW. Three-dimensional organotypic culture models of human hepatocellular carcinoma. Sci Rep. 2016;6(1):1–11. doi: 10.1038/srep21174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sun D, Liu Y, Wang H, Deng F, Zhang Y, Zhao S, Ma X, Wu H, Sun G. Novel decellularized liver matrix-alginate hybrid gel beads for the 3D culture of hepatocellular carcinoma cells. Int J Biol Macromol. 2018;109:1154–1163. doi: 10.1016/j.ijbiomac.2017.11.103. [DOI] [PubMed] [Google Scholar]
- 89.Le BD, Kang D, Yun S, Jeong YH, Kwak JY, Yoon S, Jin S. Three-dimensional hepatocellular carcinoma/fibroblast model on a nanofibrous membrane mimics tumor cell phenotypic changes and anticancer drug resistance. Nanomaterials. 2018;8(2):64. doi: 10.3390/nano8020064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ma XL, Sun YF, Wang BL, Shen MN, Zhou Y, Chen JW, Hu B, Gong ZJ, Zhang X, Cao Y, Pan BS. Sphere-forming culture enriches liver cancer stem cells and reveals Stearoyl-CoA desaturase 1 as a potential therapeutic target. BMC Cancer. 2019;19(1):1–12. doi: 10.1186/s12885-018-5219-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Xie F, Sun L, Pang Y, Xu G, Jin B, Xu H, Lu X, Xu Y, Du S, Wang Y, Feng S. Three-dimensional bio-printing of primary human hepatocellular carcinoma for personalized medicine. Biomaterials. 2021;265:120416. doi: 10.1016/j.biomaterials.2020.120416. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.