Abstract
The knee is a complex structure composed of bone, cartilage, menisci, ligaments and muscles, which all work synergistically to optimize congruence, stability, and function. Osteotomies are procedures addressing an abnormal joint alignment, shifting the mechanical load from a diseased joint compartment to a healthier one. Preoperative planning is an important art of identifying the source of abnormal load distribution to the joint, enabling the surgeon to simulate a deformity correction ahead of the surgical procedure.
Osteotomies Around the Knee: A Life-Changing Procedure
John Rhea Barton performed the first documented osteotomy around the knee in 1835.1 The patient was a physician who had a significant knee flexion contracture. The procedure was performed without anesthesia and lasted no more than five minutes. A bone wedge was removed from the anterior aspect of the distal femur, preserving the integrity of the posterior cortex. In the postoperative time, the knee was gradually straightened with serial cast changes. The surgical outcomes were so promising that the patient was able to work and ride horses again, reporting later that the procedure gave him a new life.
A Surgical Treatment for Knee Osteoarthritis
The use of osteotomies to manage degenerative disorders of the knee began in the 1950s. The concept was to correct an existing metaphyseal deformity around the knee by breaking the proximal tibia and reorienting the load pattern to the joint2 (Figure 1).
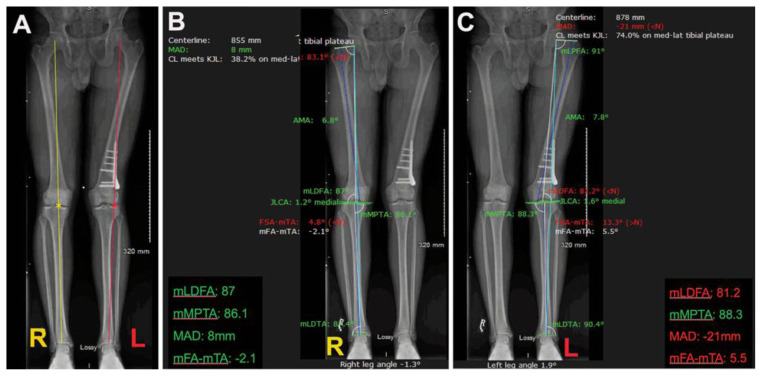
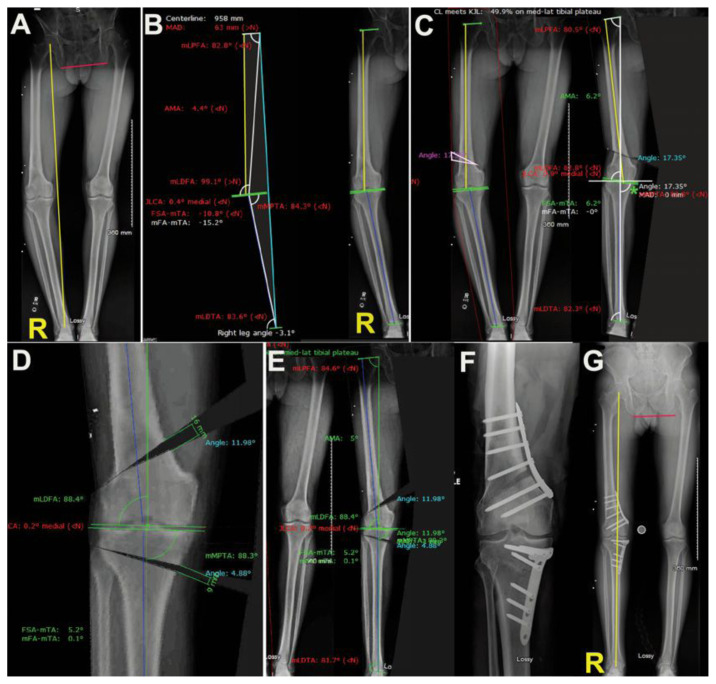
Figure 1.
Assessment and interpretation of extremity alignment studies in a 21-year-old male. A: Extremity alignment revealing a right lower extremity (R) neutral mechanical axis. Observe that the yellow line (Mikulicz line) connecting the center of the hip and the center of the ankle, bisects the knee at its center (yellow asterisk). The left lower extremity (L) has a shift of the mechanical axis to the lateral compartment of the joint. Observe that the Mikulicz line (red) is bisecting the joint (asterisk) on the lateral compartment, which determines a valgus alignment of this lower extremity. B: A software is utilized to determine the joint orientation angles on each one of the lower extremities. Observe that all joint orientation angles around the right knee are marked in green, indicating that they are within normal values. In the left lower extremity, there is a valgus mechanical femoral tibial angle of 5.5 degrees. In this case the deformity is generated at the level of distal femur, as the mechanical lateral distal femur is 81.2 degrees (normal range 85 to 90 degrees). Preoperative planning using digital software provides precise quantification and location of the deformity in the lower extremity.
The tibial osteotomies for the treatment of unicompartmental knee arthritis were popularized by Jackson (infra-tuberosity osteotomy), and Coventry (supra-tuberosity osteotomy).3,4 The only implants available to fix osteotomies around the knee were staples, and therefore casting in the postoperative time was a common practice in the postoperative period of these procedures.5 The lack of surgical standardization, fixation techniques, and postoperative protocols resulted in multiple failures. Infection, malunion, nonunion, knee stiffness, obliquity of the joint line, patella Baja, and a series of other potential complications generated a perception that osteotomies around the knee should be avoided, and knee arthroplasty should be the alternative of choice for the management of symptomatic arthritic knees.6–8 It was clear that a total knee arthroplasty would be a better choice especially for the elderly population.9 The question remained open while dealing with young and active adults, as in this group of patients the outcomes of joint arthroplasty were still mixed.10 In the last two decades, recent publications revealed favorable outcomes associated with osteotomies around the knee for the management of individuals with unstable and/or arthritic joints.11–13 The improvement of image study modalities, the development of new technologies for preoperative and intra-operative guidance, and a new generation of implants have contributed for reproducible and remarkable outcomes.14–16
Understanding the Deformity and its Clinical Implications
Osteotomies around the knee are controlled fractures aiming to improve the performance of the joint. Osteotomies aim to address any sort of deformity or malalignment of the knee. The deformity may take place in the coronal plane (varus/ valgus), sagittal plane (procurvatum/recurvatum), and/or axial plane (torsion). The deformity may be extra-articular (metaphysis/diaphysis) and/or intra-articular (epiphysis). The precise identification of the deformity site(s) is critical for a precise execution of an osteotomy around the knee.17 The most typical deformities associated with arthritic knees are described in the coronal plane. Varus knees (bowed legs) are characterized by the pathological shift of the mechanical axis to the medial compartment of the joint. The opposite occurs with valgus knees (crooked legs), which tend to wear out initially on the lateral compartment. Valgus knees are also associated with patellofemoral malalignment and/or instability.18 In the sagittal plane, the measurement of the tibial slope is of importance, especially in cases where recurrent anteroposterior instability is present. An increased tibial slope is associated with anterior translation of the tibia, which poses significant tension to the anterior cruciate ligament.19 In the other way around, a decreased tibial slope may be detrimental to the posterior cruciate ligament function.20 In the axial plane, torsional deformities determine patellofemoral instability and pain.21 The three-dimensional analysis of the knee allows for a better understanding of clinical findings and optimal decision making.
Interpreting Image Studies
An extremity alignment study (EAS) is a gold standard radiograph obtained to assess the alignment of the knee in the coronal plane.22 This image study includes a single radiograph that captures the alignment of the hip, the knee, and the ankle. The line that connects the center of the hip to the center of the ankle corresponds to the mechanical axis of the lower limb. If the alignment of the knee is neutral, this line will seat slightly medial to the medial tibial spine, close to the center of the knee. Deviations of the mechanical axis from the center of the knee to either one of the compartments of the joint determines excessive load to that compartment and, therefore, increases the likelihood of degenerative changes in that site.23
A tangent line to the femoral condyles, and a tangent line to the tibial plateau should intersect the mechanical axis to determine joint alignment angles. Three angles are of critical importance. The mechanical proximal tibial angle (MPTA) which is determined by a tangent to the tibial plateau and the mechanical axis on the medial side of the joint. The MPTA normally ranges from 85 to 90 degrees, and its standard value is 87 degrees.17,22 On the lateral aspect of the knee, the angle determined by the tangent to the femoral condyles and the mechanical axis is named mechanical lateral distal femoral angle (mLDFA). The mLDFA normally ranges from 85 to 90 degrees and its standard value is 88 degrees.17,22 Another important angle is determined by the tangent lines to the femoral condyles and to the tibial plateau. These two lines should be parallel or slightly convergent medially. These two lines determine the Joint Line Convergence Angle (JLCA) which varies from 0 to 2 degrees.17,22 The angle determined between the mechanical axis of the femur and the mechanical axis of the tibia is named mechanical tibiofemoral angle, which normal value varies from 0 to 2 degrees (Figure 1).
Joint orientation angles are of critical importance while determining the biomechanics of the knee and how the joint is routinely loaded. Knee deformities in the coronal plane will generate bowed or crooked legs. The bowed legs are present when the knee has a varus alignment, while the crooked legs are associated with a valgus alignment of the joint. Joint orientation angles will guide the surgeon to determine if the deformity is originated at the level of the femoral metaphysis, tibial metaphysis, joint surface, or a combination of these sites.
Deformities in the axial plane will generate abnormal torsion to bone segments. They may be constitutional or inherited post-trauma. They have significant impact to the mechanics of the patellofemoral joint.
Varus Knees
A varus deformity implies in the shift of the mechanical load to the medial compartment of the knee. As a result, degenerative changes may take place in this compartment, which may cause pain and mechanical symptoms.24 Traditionally, the deformity was meant to be originated in the upper metaphysis of the tibia and, therefore, osteotomies to correct varus knees were traditionally performed on the upper portion of the tibia. However, the systematic measurement of the joint orientation angles revealed that in some cases the deformity is not located in the proximal tibia but in the distal femur or at the level of the joint line (Figure 2).
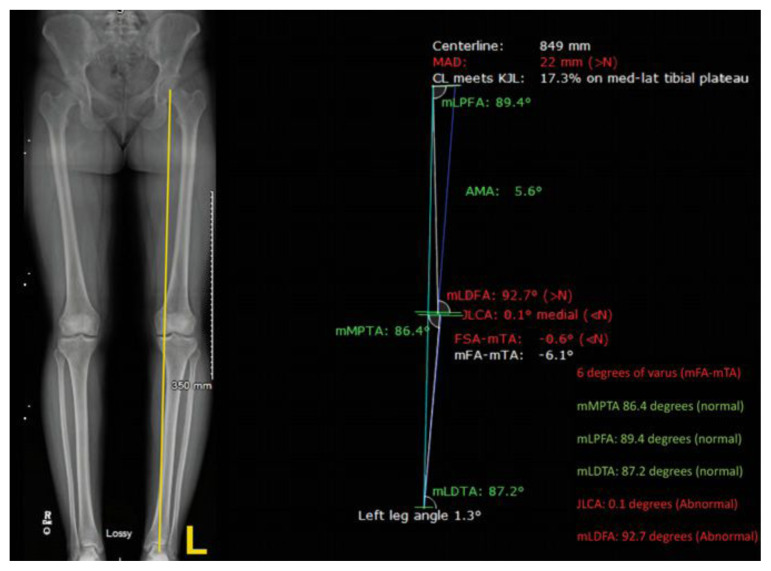
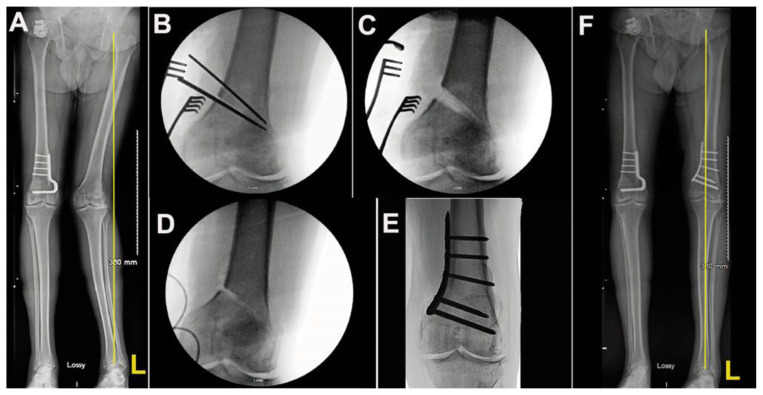
Figure 2.
The importance of preoperative planning. This is an alignment study of a 25-year-old male with complaints of medial knee pain. His extremity alignment study shows varus alignment, with displacement of the mechanical axis to the medial compartment of the left knee. He was told that he would benefit of a knee arthroscopy for the management of a medial meniscal tear. The patient was also told that a possible high tibial osteotomy to correct the varus deformity would be necessary. We were asked to evaluate the patient and we confirmed that his mechanical proximal tibial angle was withing normal values (86.4 degrees), but the varus was originated on the distal femur (abnormal mLDFA superior to 90 degrees). In this case, preoperative planning was able to identify that the correct site for the osteotomy in this case would be the distal femur and not the proximal tibia.
Osteotomies should be considered as a joint preservation option in the management of symptomatic varus knees. The main goal of this procedure is to shift the mechanical load from the diseased medial compartment to a healthier lateral compartment of the joint. Medial open wedge high tibia osteotomies became the most popular method of correcting varus knees25 (Figure 3). Sometimes, however, the deformity is not located on the tibia, but on the femur, which prompts the correction to take place at the level of the distal femur (Figure 4).
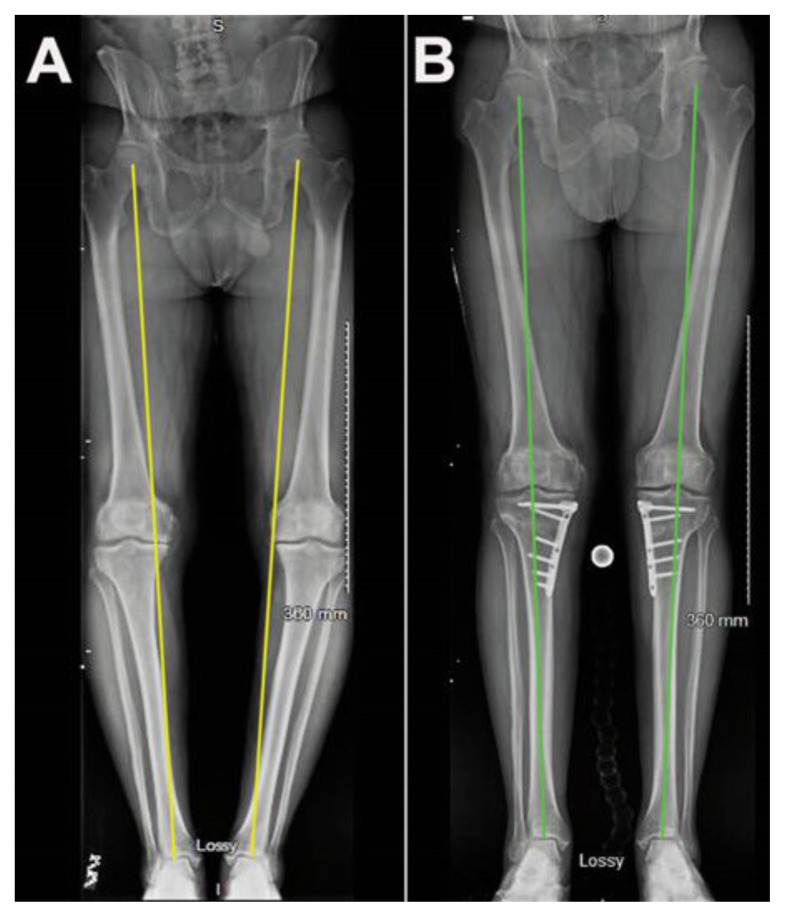
Figure 3.
Medial open wedge valgus producing high tibial osteotomy. A: Extremity alignment study of a 47-year-old male with bilateral knee pain and varus deformity. He was told that the best option for his knee would be bilateral total knee replacement when he would get older. He is currently not able to stand on his feet to perform the activities of his daily living. B: Patient underwent a staged treatment for his lower extremities. Initially he was submitted to a left high tibial osteotomy. After complete recovery of this surgical procedure, he received a right high tibia osteotomy. Patient was able to resume his professional activities with minimal discomfort in his lower limbs, improved gait pattern, and improved alignment of the lower limbs.
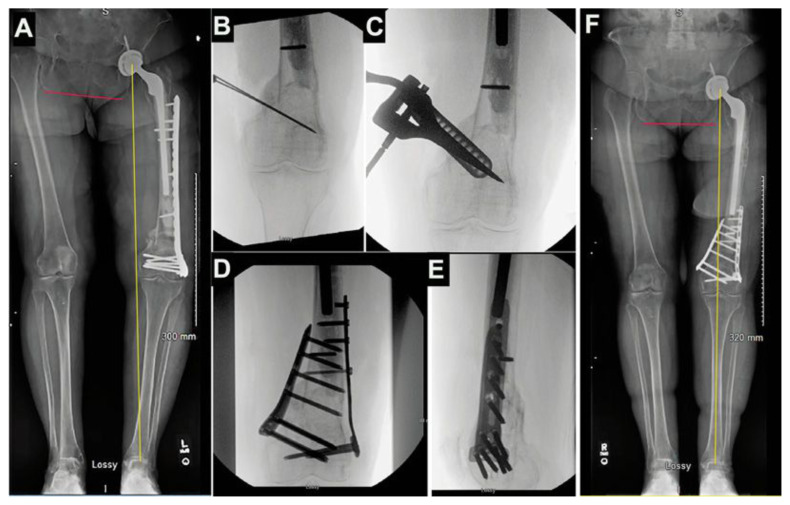
Figure 4.
Status after failed left distal femur periprosthetic fracture. A: Extremity alignment study of a 62-year-old female patient 5 months after an open reduction and internal fixation of the left distal femur. Patient has varus alignment (yellow line) and shortening of the left lower limb. The leg length discrepancy may be noted by the obliquity of the pelvis (red line). The list of problems includes significant pain, disability to bear weight, osteoporosis, previous infected left total hip replacement on chronic antibiotic suppression, short distal femur segment, left knee arthritis. B: Intraoperative image illustrating the direction of an medial distal femur open wedge valgus producing osteotomy. C: A special tool is used to open a wedge of 18mm on the medial aspect of the distal femur; D: Final intraoperative aspect of the osteotomy on the anteroposterior and E: lateral projections of the knee; F: Final extremity alignment study revealing neutral alignment of the lower limb and neutral pelvis obliquity. The leg length discrepancy was improved significantly as well as patient’s stability and ability to perform her activities of daily living.
Meticulous preoperative planning helps to determine how to improve the alignment of the lower limb, as well as the distribution of loads in the joint, without generating a secondary deformity at the level of the knee. If the osteotomy is not correctly indicated or is placed at a site that does not correspond to the center of the deformity. In a few cases, we have noticed that the deformity was not located just in one of the long bones, but in both. In these cases, a double level osteotomy, which implies in performing two simultaneous osteotomies, one at the level of the femur and one at the level of the tibia should be carried out26 (Figure 5).
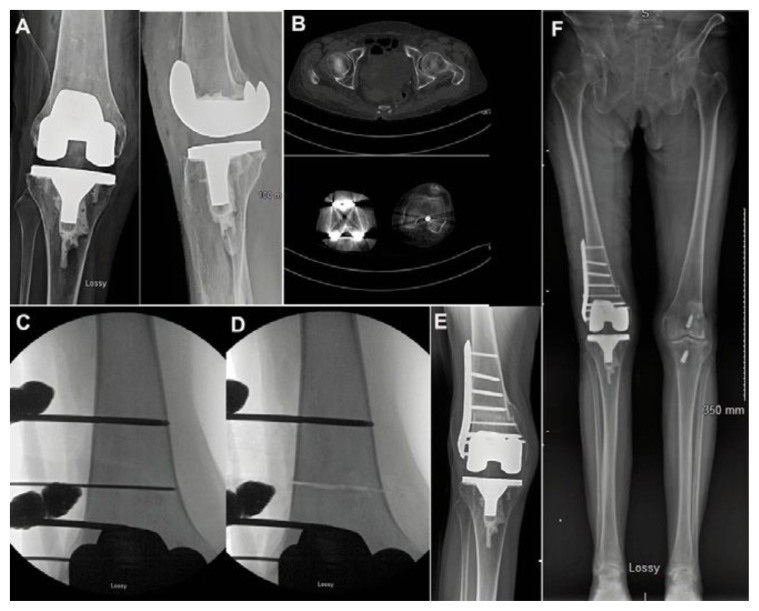
Figure 5.
Illustrative case of a double level osteotomy to correct a varus alignment. A: Extremity alignment study revealing significant varus alignment in a 49-year-old male, with history of significant knee pain. Patient received an indication for a right total knee replacement and came to our office for a second opinion. Past medical history significant for a right distal femur fracture when he was 15 years of age. B: Digital preoperative planning revealing a varus deformity of 15.2 degrees and abnormal MPTA, mLDFA, and JLCA; C: A simulation to correct the varus deformity with an osteotomy performed at the level of his previous fracture resulted in correction of the mechanical axis to the expense of obliquity of the joint line (green asterisk). This indicated that the correction could not be performed just at that level; D: Considering that the patient had significant shortening of the lower limb we proposed a double level osteotomy, opening a medial wedge on the distal femur and on the proximal tibia. We were able to propose a correction superior to 2cm in length discrepancy bringing the MPTA and mLDFA to a normal range. E: Simulation of the alignment study revealing neutral mechanical axis and normal joint orientation angles; F: Postoperative radiograph on the anteroposterior projection. Bone graft was used to fill the open wedge gaps; G: Final extremity alignment study revealing neutral mechanical axis (yellow line) and normalization of the pelvic obliquity (red line). This patient has four years of follow up and has not complained of any knee pain since his lower extremity alignment has been corrected.
Valgus Knees
The lateral compartment of the knee is the one exposed to extra loading in cases of a valgus deformity. The patellofemoral joint is also exposed to mechanical forces which pull out the patella towards the lateral aspect of the femoral trochlea. Correction of a valgus deformity offloads the lateral compartment of the knee and improves the patellofemoral tracking. The most typical site for deformity correction is the distal aspect of the femur27 (Figure 6). Occasionally, the osteotomy should be performed at the level of the tibia or at a double level, femur, and tibia, as it has been demonstrated in the examples of varus knees.
Figure 6.
Illustrative case of a valgus deformity correction. A: Extremity alignment study of a 46-year-old male who complains of left knee pain and instability. He has past medical history significant for a right distal femur osteotomy to correct a similar deformity. B: Intraoperative image illustrating the resection of a medial distal femur cortical. The wedge has a base measuring 16 mm. C: Fluoroscopy pictures revealing the wedge resection, prior to correction of the deformity; D: The osteotomy gap is gently closed. Observe that the opposite hinge is intact and no translation between the distal and proximal fragments take place; E: Final radiograph depicting a good coaptation of the osteotomy. F: Final extremity alignment study revealing neutral alignment of the lower limb. This procedure was performed four years ago, and the patient has not complained of knee pain since.
Torsional Deformities
Deformities in the axial plane are not very intuitive as they are not easily caught by radiographs. The clinical exam with a detailed analysis of the gait, rotations of the hip, and thigh-foot angle are an essential part of the assessment of these patients. The computed tomography is the image modality that determined with precision the alignment of the limb in the axial plane. Torsional corrections are obtained when the osteotomy is performed perpendicular to the axis of the long bone allowing for detorsion of the segment28 (Figure 7).
Figure 7.
Illustrative case of torsional deformity. A: Radiographs of a 63-year-old female who underwent a right total knee replacement elsewhere. She had previous valgus alignment and a history of patellectomy many years ago. After her knee replacement she developed significant instability of her extensor mechanism, with recurrent dislocations. She received the indication to revise her total knee replacement. B: In our clinic a computed tomography was performed, and we noticed that she had 24 degrees of internal torsion of the distal femur. She was two months out of her total knee replacement. Instead of revising the components of the knee replacement we proposed an osteotomy to correct the torsional deformity. C: Intraoperative pictures illustrating the orientation of the osteotomy, perpendicular to the axis of the femur; D: The osteotomy has been completed. The femur does not displace because it has been provisionally fixed with an external fixator. E. Final radiograph one year after surgery with complete healing of the osteotomy. Patient has no more symptoms of extensor mechanism dislocation; F: Final alignment study depicting that the osteotomy did not introduce deformity in the coronal plane.
Conclusion
The alignment of the knee has direct implications on its mechanical performance. Knee pain could be the expression of degenerative changes caused by mechanical overloading of one of the compartments of the joint. Extremity alignment studies are of critical importance to understand how the loads are distributed on the knee. The mechanical axis of the lower limb should connect the center of the hip, the center of the knee, and the center of the ankle. A deviation of the mechanical axis in the coronal plane is present in cases of varus deformities or valgus deformities. Correction of deformities around the knee promotes a better distribution of the load among the different compartments of the joint, restoring the knee mechanical homeostasis. Deformity correction is a precise art. It requires meticulous preoperative planning based on the identification of the site(s) of deformity. The site of deformity is indicated by abnormal joint orientation angles. The location of the abnormal angle should correspond to the site of the osteotomy aiming to restore the mechanical axis. The goal of deformity correction is not only to shift the mechanical load to a healthier compartment of the joint, but to perform it without causing an obliquity of the joint line, or significant leg length discrepancy. Preoperative planning allows for a three-dimensional understanding of the deformity and its correction in one or more spatial planes. Restoring knee alignment and stability may preserve the joint for many years until a joint replacement may be at consideration. This is especially important in young and active individuals, where the survivorship of a joint replacement is not expected to be greater than the patient’s life expectancy.
Footnotes
Mauricio Kfuri, MD, PhD, (above), is the James P. Stannard and Carolyn A. Stannard Distinguished Professor in Orthopaedic Surgery; and Brett D. Crist, MD, and James P. Stannard, MD, are all in the Department of Orthopaedic Surgery, University of Missouri - Columbia School of Medicine, Columbia, Missouri.
Disclosure
MK: AOTrauma board or committee member.
BDC: KCI: paid consultant; Orthopaedic Implant Company and RomTech: stock/stock options; Springer: publishing royalties, financial, or material support; AO Trauma North America: board or committee member; Globus Medical: IP royalties; International Geriatric Fracture Society: board or committee member; Journal of Hip Preservation: editorial or governing board; Journal of Orthopaedic Trauma: editorial or governing board; Orthopaedic Trauma Association: board or committee member; Osteocentric: unpaid consultant; SLACK Incorporated: editorial or governing board; Synthes: paid consultant; research support.
JPS: DePuy, Orthopedica Designs North America, and Smith and Nephew: paid consultant; National Institutes of Health: research grant; American Orthopaedic Association: board or committee member; AO Foundation: board or committee member; AO North America: board or committee member; Journal of Knee Surgery: editorial or governing board; Mid-America Orthopaedic Association: board or committee member; Thieme: publishing royalties, financial, or material support; and U.S. Department of Defense: research support.
References
- 1. Smith JO, Wilson AJ, Thomas NP. Osteotomy around the knee: evolution, principles and results. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2013;21(1):3–22. doi: 10.1007/s00167-012-2206-0. [DOI] [PubMed] [Google Scholar]
- 2. Brittain HA. Treatment of genu valgum; the discarded iron. Br Med J. 1948;2(4572):385–387. doi: 10.1136/bmj.2.4572.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43-B:746–751. doi: 10.1302/0301-620X.43B4.746. [DOI] [PubMed] [Google Scholar]
- 4. Coventry MB. OSTEOTOMY OF THE UPPER PORTION OF THE TIBIA FOR DEGENERATIVE ARTHRITIS OF THE KNEE A PRELIMINARY REPORT. J Bone Joint Surg Am. 1965;47:984–990. [PubMed] [Google Scholar]
- 5. Surin V, Markhede G, Sundholm K. Factors influencing results of high tibial osteotomy in gonarthrosis. Acta Orthop Scand. 1975;46(6):996–1007. doi: 10.3109/17453677508989289. [DOI] [PubMed] [Google Scholar]
- 6. Bauer GC, Insall J, Koshino T. Tibial osteotomy in gonarthrosis (osteo-arthritis of the knee) J Bone Joint Surg Am. 1969;51(8):1545–1563. [PubMed] [Google Scholar]
- 7. Benjamin A. Double osteotomy for the painful knee in rheumatoid arthritis and osteoarthritis. J Bone Joint Surg Br. 1969;51(4):694–699. [PubMed] [Google Scholar]
- 8. Seal PV, Chan RN. Tibial osteotomy for osteoarthrosis of the knee. Acta Orthop Scand. 1975;46(1):141–151. doi: 10.3109/17453677508989202. [DOI] [PubMed] [Google Scholar]
- 9. Ranawat CS. History of total knee replacement. J South Orthop Assoc. 2002;11(4):218–226. [PubMed] [Google Scholar]
- 10. Charette RS, Sloan M, DeAngelis RD, Lee GC. Higher Rate of Early Revision Following Primary Total Knee Arthroplasty in Patients Under Age 55: A Cautionary Tale. J Arthroplasty. 2019;34(12):2918–2924. doi: 10.1016/j.arth.2019.06.060. [DOI] [PubMed] [Google Scholar]
- 11. Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br. 2008;90(12):1548–1557. doi: 10.1302/0301-620X.90B12.21198. [DOI] [PubMed] [Google Scholar]
- 12. Hofmann S, Lobenhoffer P, Staubli A, Van Heerwaarden R. [Osteotomies of the knee joint in patients with monocompartmental arthritis]. Orthopade. 2009;38(8):755–769. doi: 10.1007/s00132-009-1458-y. quiz 770. [DOI] [PubMed] [Google Scholar]
- 13. Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2013;21(1):170–180. doi: 10.1007/s00167-012-2087-2. [DOI] [PubMed] [Google Scholar]
- 14. Staubli AE, De Simoni C, Babst R, Lobenhoffer P. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia--early results in 92 cases. Injury. 2003;34(Suppl 2):B55–62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 15. Staubli AE, Jacob HAC. Evolution of open-wedge high-tibial osteotomy: experience with a special angular stable device for internal fixation without interposition material. Int Orthop. 2010;34(2):167–172. doi: 10.1007/s00264-009-0902-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yan J, Musahl V, Kay J, Khan M, Simunovic N, Ayeni OR. Outcome reporting following navigated high tibial osteotomy of the knee: a systematic review. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2016;24(11):3529–3555. doi: 10.1007/s00167-016-4327-3. [DOI] [PubMed] [Google Scholar]
- 17.Paley D. Principles of Deformity Correction. Springer; 2002. [Google Scholar]
- 18. Tan SHS, Hui SJ, Doshi C, Wong KL, Lim AKS, Hui JH. The Outcomes of Distal Femoral Varus Osteotomy in Patellofemoral Instability: A Systematic Review and Meta-Analysis. J Knee Surg. 2020;33(5):504–512. doi: 10.1055/s-0039-1681043. [DOI] [PubMed] [Google Scholar]
- 19. Lin LJ, Akpinar B, Meislin RJ. Tibial Slope and Anterior Cruciate Ligament Reconstruction Outcomes. JBJS Rev. 2020;8(4):e0184. doi: 10.2106/JBJS.RVW.19.00184. [DOI] [PubMed] [Google Scholar]
- 20. Bernhardson AS, DePhillipo NN, Daney BT, Kennedy MI, Aman ZS, LaPrade RF. Posterior Tibial Slope and Risk of Posterior Cruciate Ligament Injury. Am J Sports Med. 2019;47(2):312–317. doi: 10.1177/0363546518819176. [DOI] [PubMed] [Google Scholar]
- 21. Imhoff FB, Cotic M, Dyrna FGE, et al. Dynamic Q-angle is increased in patients with chronic patellofemoral instability and correlates positively with femoral torsion. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2021;29(4):1224–1231. doi: 10.1007/s00167-020-06163-6. [DOI] [PubMed] [Google Scholar]
- 22. Schröter S, Elson DW, Ateschrang A, et al. Lower Limb Deformity Analysis and the Planning of an Osteotomy. J Knee Surg. 2017;30(5):393–408. doi: 10.1055/s-0037-1603503. [DOI] [PubMed] [Google Scholar]
- 23. Pape D, Hoffmann A, Seil R. [Imaging and preoperative planning for osteotomies around the knee]. Oper Orthopadie Traumatol. 2017;29(4):280–293. doi: 10.1007/s00064-017-0496-6. [DOI] [PubMed] [Google Scholar]
- 24. Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum. 2009;61(4):459–467. doi: 10.1002/art.24336. [DOI] [PubMed] [Google Scholar]
- 25. Webb M, Dewan V, Elson D. Functional results following high tibial osteotomy: a review of the literature. Eur J Orthop Surg Traumatol Orthop Traumatol. 2018;28(4):555–563. doi: 10.1007/s00590-017-2112-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nakayama H, Iseki T, Kanto R, et al. Physiologic knee joint alignment and orientation can be restored by the minimally invasive double level osteotomy for osteoarthritic knees with severe varus deformity. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2020;28(3):742–750. doi: 10.1007/s00167-018-5103-3. [DOI] [PubMed] [Google Scholar]
- 27. van Heerwaarden R, Brinkman JM, Pronk Y. Correction of Femoral Valgus Deformity. J Knee Surg. 2017;30(8):746–755. doi: 10.1055/s-0037-1602138. [DOI] [PubMed] [Google Scholar]
- 28. Schröter S, Nakayama H, Ihle C, et al. Torsional Osteotomy. J Knee Surg. 2020;33(5):486–495. doi: 10.1055/s-0039-1678677. [DOI] [PubMed] [Google Scholar]