Introduction
Uterine atony is a serious condition that can occur any time after childbirth and can lead to disastrous results if not addressed and treated at the right time. According to WHO maternal mortality is unacceptably high, most of the deaths (94%), occurring in low-resource countries and deaths that can be easily prevented [1].
With respect to sustainable development goals (SDG) and maternal mortality, all countries have committed to pursuing and achieving a new goal of maternal mortality reduction by 2030. SDG3 includes the target of “reducing global maternal mortality rate to 70 per 100,000 births, with no country having a maternal mortality rate of more than 2 times the global average.”
According to the WHO, the majority of women die during or as a result of pregnancy and childbirth. Some complications may exist before pregnancy, but are worsened by pregnancy and childbirth and lack of proper care. Major complications that account for nearly 75% of MMR are [2]
Bleeding after childbirth—especially Postpartum Hemorrhage (PPH)
Infection after childbirth.
Pre-eclampsia, eclampsia and essential hypertension during pregnancy
Complications from delivery
Unsafe abortions.
Uterine atony is the commonest cause of PPH. According to population-based studies conducted in developed countries, the prevalence of PPH following vaginal birth ranges between 0.8 and 7.9 percent [3–6].
Uterine balloon tamponade is a non-surgical method of treating refractory atonic PPH.
The principles of physics behind the balloon tamponade are the same. But the once-considered second-line treatment by the RCOG and ACOG in management in obstetrics is now making and newer and effective comeback in equally treating uterine bleeding disorders in modern operative gynecology.
This article reviews the several benefits of this simple, cost-effective and yet therapeutic uses of the balloon tamponade in obstetrics as well as gynecology.
Principle of Treatment
Intrauterine balloon intervention is based on the principle that the device exerts an inward to outward pressure that is greater than the systemic arterial pressure of the patient in order to maintain a “hemostatic effect” and prevent continuous hemorrhaging
The “tamponade test” brilliantly elicits the timing of intervention, both medical or surgical in management of obstetric hemorrhage [7].
There are case reports that prove that through ultrasonic intervention, through a transabdominal ultrasound in patients undergoing treatment with balloon tamponade, there might be an alternative mechanism of action. In a first case report documentation of this hypothesis—while the sonographic position is incorrect for conventional uterine balloon catheter use, it suggests an alternate mechanism of action for the balloon: not tamponade of the uterine cavity, but hydrostatic pressure directly around the uterine arteries, a mechanism like mechanical uterine artery embolization or ligation. This concept not only explains how a balloon catheter works, but also challenges conventional wisdom regarding the management of intrauterine bleeding in both obstetrics and gynecology [8].
This principle is now widely used in conditions in modern obstetrics and gynecology, where uterine bleeding is a common complication, e.g., first and second trimester termination of pregnancy [9, 10], cervical pregnancy [11–15], knife cone biopsy [16], laser ablation of the endometrium, dysfunctional uterine bleeding [17], multiple vaginal lacerations [18] and bleeding from cervical stump following postcesarean section sub-hysterectomy [19].
Uses of Uterine Balloon Tamponade in Obstetrics
The concept of developing and using condom as a balloon tamponade was simultaneously invented and evaluated as a life-saving technique in low-resource countries like India and Bangladesh, where procuring standard balloon tamponade methods were not affordable given the increased patient load and lesser financial access to standard techniques. This in turn proved to be the basis of several tamponade techniques that have now become the standard norm of practice in controlling uterine bleeding in OBGYN practice.
Prof Sayeba Akhter [20] and Prof Shivkar [21] worked simultaneously, unaware of each others work at around the same time, in order to create a successful tamponade for atonic PPH.
The failure of initial management in controlling atonic PPH prompts the use of balloon tamponade and “Shivkar’s pack”[21].
Using aseptic precautions, a standard condom is rolled over Foley's catheter #20 and is tied and secured at two places at least 1 centimeter apart. A transvaginal insertion of this Foley's catheter is done using the following techniques.
Condom along with the catheter is inserted into the uterine cavity, and the bulb of the Foley’s catheter is inflated to ensure it is placed safely in the uterine cavity. The distal end of the Foley’s is then strapped to either of the thighs to secure its position. The vagina is loosely packed with the roller gauze. And pad dressings are placed outside the vagina. An indwelling bladder catheter is kept in place till the tamponade is secured. The fundal height of the uterus is marked on the abdomen.
The distal end of Foley's catheter is connected to a fluid source, preferably a liter of ringer lactate solution.
The fluid source is placed at a distance of at least 60 centimeters above the uterus with the patient in horizontal position. The patient is not placed in lithotomy position from here on, i.e., after the successful insertion of the “Shivkar’s pack.”
The condom balloon is now inflated. And an airway needle is placed on the bag containing the fluid source to expose the system to external environmental pressure.
The equilibrium between this hydrostatic pressure and uterine tone is the basis for "Shivkar's pack."
Fluid is rushed through the tubing after the flow controller is released, inflating and pressurizing the uterovaginal canal. As pressure builds up inside the condom balloon, the fluid flow gradually decreases and eventually stops if there is sufficient uterovaginal tone. If the flow continues indefinitely or eventually increases, we have reached the point of uterovaginal overstretching. This condition will likely result in additional hemorrhage. The fluid source is gradually reduced until the fluid flow is completely stopped or, more preferably, reversal of the fluid flow is observed. This will guard against a uterovaginal condition that is overstretched. After inflating to 300–400 ml of warm saline with a 20-ml syringe, the fluid source is lowered to 25 cm below the abdomen to observe the flow reversal. If no reversal of flow occurs, further lowering by 5 cm every 5 minutes is recommended to observe the reversal of flow. Following observation of the flow reversal, the height of the fluid source is increased if necessary and possible without causing additional appreciable distension (not greater than 50 ml). All uterine tone-increasing measures, such as uterotonics, blood transfusion, oxygen, must be maintained. After packing, blood loss is determined by maintaining a kidney tray at the perineum. When blood loss is less than 25 milliliters per hour, it should be ignored. If it was less than 50 ml, the availability of blood for transfusion is determined. If it exceeds 50 ml, an alternative treatment was sought. However, it is not always necessary [22].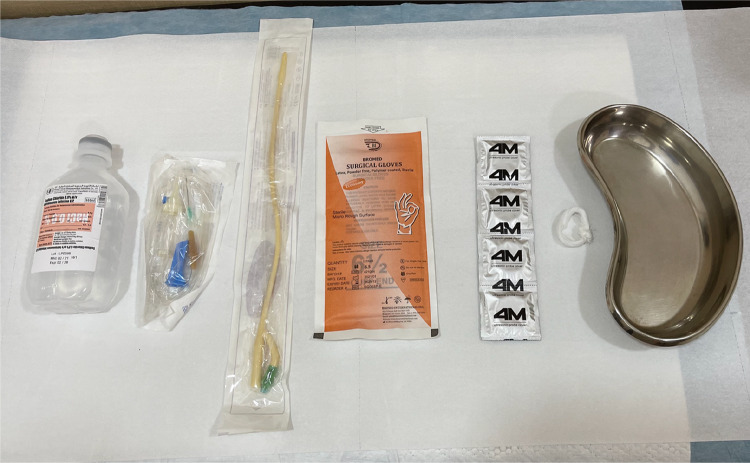
Equipment used in shivkar’s pack—provides and excellent alternative for low- to medium-resource countries
Role of Uterine Balloon Tamponade in Gynecological Procedures
One of the earliest use of Foley’s balloon tamponade was made by Goldrath et al. [23] expanding the horizon for use of compression balloon tamponade to reduce intrauterine bleeding after hysteroscopic resection of submucous myomas. Since then it has been used with success in several hysteroscopic myoma resections as a means of reducing hemorrhage after gynecological hysteroscopic surgeries.
A prospective randomized controlled trial was conducted to determine the efficacy of routine Foley’s catheter tamponade in reducing blood loss following hysteroscopic myoma resection. Dan U et al [24] were clearly able to demonstrate the effectiveness of simple Foley’s balloon tamponade in managing immediate postoperative bleeding following hysteroscopic resection of myomas.
The volume of distention of the Foley's was determined in this randomized study based on the preoperative myoma size. For drainage, 5–7ml of saline was injected into the balloon; for tamponade, 10–40ml of normal saline was injected, and the volume determined by the submucous myoma measured on ultrasound prior to the procedure. Surgery was done in the early proliferative phase of the menstrual cycle. Immediately after the surgery Foley’s catheter no 20 was introduced into the uterine cavity and patients were divided into 2 groups—Group A—where Foley’s was introduced for drainage of uterine collection—and Group B—where Foley’s was introduced for tamponade.
This randomized control trial was successful in demonstrating that the use of balloon tamponade was successful in reducing postoperative blood loss after resection of large submucous myomas as compared to the control group. It was however recommended by the study that in order to avoid pressure necrosis of the resected bed, it was wise to sustain the tamponade pressure for maximum upto 6 hours following which the intrauterine Foley’s was deflated to 5–7ml for drainage purpose only.
Modifications of the Intrauterine Balloon Tamponade to Prevent Uterine Hemorrhage
Several modifications of the balloon tamponade are in use today to control intrauterine hemorrhage. It is to be noted that Rusch balloon and condom catheter used in Shivkar’s pack, and both do not have extra channel to monitor the uterine drainage and subsequent blood loss. Blood loss in these latter two balloon tamponades is monitored by vaginal packs and pads that are soaked, and hence do not provide the exact estimate of total blood loss, while the former three modifications of the balloon tamponade provide and extra channel where the approximate blood loss could be monitored and further actions could be initiated.
Indications, Contraindiactions and Timing of Use of Balloon Tamponade in Obstetrics and Gynecology
The Sheffield guidelines suggest the use of Rusch’s balloon as a prophylactic measure in women who are at a high risk of postpartum hemorrhage and/or when impending postpartum hemorrhage could jeopardize the pre-existing co-morbidities in a pregnant woman [25].
However, in low- to medium-income countries, the simple condom catheter (Shivkar’s pack) could be equally effective in controlling severe atonic PPH along with other supportive modalities like
uterotonic medications like oxytocin, carbetocin, prostaglandins.
Surgical modalities like—B-Lynch brace sutures, internal artery ligation
Appropriate antibiotic coverage to prevent sepsis
Pain relief medications—NSAIDs
The Tamponade Test
The “tamponade test” is considered positive if control of intrauterine bleeding is achieved after the intrauterine balloon is inflated [7]. This test was originally referenced with the use of Sengstaken-Blakemore tube, but can be used with any intrauterine balloon preparation.
This test is a helpful first-step guide to initiate hemostasis after uncontrolled uterine bleeding is established.
In the event that the intrauterine balloon was unable to control the uterine hemorrhage, i.e., negative tamponade test, then further management such as exploratory laparotomy with SOS hysterectomy might become necessary [7].
The rate of deflation of the balloon differs depending on various operators. At the current moment, there is not a standard rate of deflation of the intrauterine balloon advocated by any guidelines and warrants randomized control study to indicate the timing and rate of deflating the balloon should the intrauterine bleeding be arrested. Most articles have advocated that the balloon is deflated within 48 hours after inflation to reduce the incidence of a vascular necrosis of the healthy endometrial tissue. The rates of deflation carry from 20ml/hour to half the volume in the balloon gradually over 12 hours [7, 26].
Contraindications
The most common contraindications for insertion of balloon tamponade are infection and sepsis. It is postulated that prolonged second stage and prolonged labor increase the risk of endometritis and are a contraindication to insert the tamponade [25]. However, this can be controlled by the use of intrapartum antibiotic prophylaxis even in a low-resource setting.
Another obvious contraindication for tamponade use is Latex and rubber allergies.
Timing of Placement of the Balloon Catheter
In a review article published in 2007, it was clearly concluded that timing of placement of the intrauterine balloon prior to decision making for laparotomy significantly reduced the need for laparotomy with success rates of 90% and balloon tamponade was effective in reducing atonic PPH in almost 100 percent of cases under this study [27]. Hence the early use if balloon tamponade insertion, the moment atonic PPH is recognized will also help buy time to prepare for exploratory laparotomy and arrangement of packed cells and blood products by keeping the patient hemodynamically stable. The “tamponade test” plays a major role in this decision making, thereby resulting in decreased blood loss and decrease in maternal morbidity and mortality [28].
Complications
Fewer studies have demonstrated the failure of balloon tamponade in controlling uterine bleeding due to PPH or hysteroscopic surgeries. These failures could be due to the following reasons
Obstruction of the uterine cavity by a large myoma in a case of atonic PPH.
Damage to the intrauterine balloon
Difficulties in placement of the intrauterine balloon after a B-Lynch suture [27].
Insufficient insufflation of the balloon causing more than one balloons to be placed to control the bleeding [29].
Uterine rupture from uterine over distention [30].
Uterine perforation during uterine insertion of the balloon [30].
Other complications, such as air embolization, are used as a distention media.
Future Prognosis
Very limited literature exists regarding long-term follow-up and subsequent future pregnancies in patients who were subjected to use of balloon tamponade to control uterine bleeding. However, there is a documentation of single successful pregnancy after the previous pregnancy PPH complications controlled by balloon tamponade alone [31] and a record of 2 pregnancies after previous delivery complications were managed by combination of B-Lynch brace sutures and balloon tamponade [32], warranting a need for future prospective randomized trials researching the effect of balloon tamponade on future fertility of the patient.
Newer Modifications
Vacuum-Induced Uterine Tamponade
In a preliminary study done on patient’s where primary line of management of patient is suffering from PPH, a novel technique of vacuum-induced uterine tamponade was used by creating a device introduced into the uterine cavity and negative suction pressure used to create a state of hemostasis and reduction of blood flow from the uterine cavity [33]. The suction created an immediate seal at the cervical os, causing the uterus to immediately collapse and restore hemostasis, while other vaginal and perineal lacerations were immediately repaired.
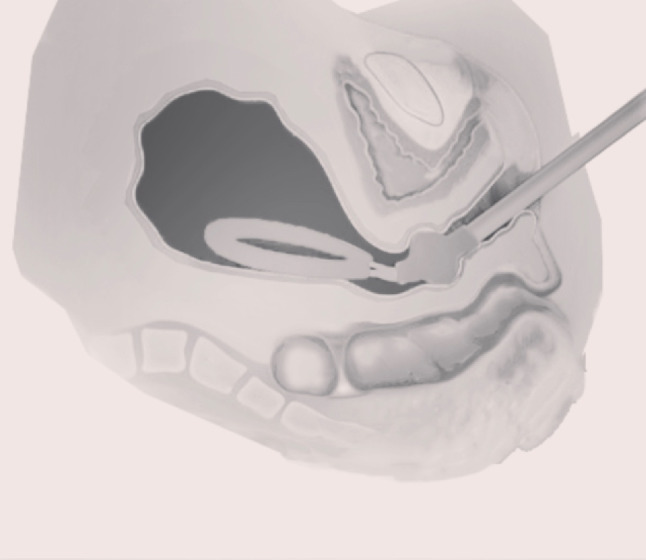
Image courtesy—Lattitude Media LLC
This novel method though preliminary needs further evaluation and further modifications to suit the needs of low- to medium-resource countries where the incidences of atonic PPH are relatively high.
Bakri 1 Modification System

Image courtesy—Lattitude Media LLC
This novel Bakri 1 modification system uses 2 levels of inflation of balloons one—intrauterine to create a tamponade and second—at the level of the internal os creating a tight seal, instead of vaginal packs to estimate the amount of blood loss. Inflation of the vaginal balloon at the level of the internal os fixes the uterine balloon and prevents slipping out of the uterine balloon. An internal suction system estimates the blood loss and appropriate measures can be undertaken. This device is marketed as Ebb (complete tamponade system) [34]
However, as promising and pragmatic this approach is, it still is a challenge when it comes to employing this method in low- to medium-resource countries.
Conclusion
Postpartum hemorrhage, although potentially life threatening, can most of the times be easily avoided by simple techniques like the uterine balloon tamponade. The correct application of the intrauterine balloon, be it the S-B tube or a simple Foley’s condom catheter tamponade (Shivkar’s pack) can be a simple yet highly effective modality in avoiding maternal morbidity and mortality. Furthermore, this technique has proven to be a successful alternative to a radical surgery as well as the first line of management while awaiting blood and its products to save a patients life. We hope that this simple yet effective means of therapy become a part of a guideline in managing intrauterine bleeding in both obstetric and gynecology settings, rather than an independent mode of treatment. Hopefully, this article will raise the awareness among practicing obstetricians and gynecologists to incorporate balloon tamponade in the form of evidence-based therapy in reducing intrauterine bleeding in both obstetric and gynecological cases.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Trends in maternal mortality: 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization; 2019
- 2.Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels JD, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health. 2014;2(6):e323–3. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 3.Kramer MS, Berg C, Abenhaim H, Dahhou M, Rouleau J, Mehrabadi A, et al. Incidence, risk factors, and temporal trends in severe postpartum hemorrhage. Am J Obstet Gynecol. 2013;209(5):449. doi: 10.1016/j.ajog.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Al-Zirqi I, Vangen S, Forsen L, Stray-Pedersen B. Prevalence and risk factors of severe obstetric haemorrhage. BJOG. 2008;115(10):1265–72. doi: 10.1111/j.1471-0528.2008.01859.x. [DOI] [PubMed] [Google Scholar]
- 5.Lutomski JE, Byrne BM, Devane D, Greene RA. Increasing trends in atonic postpartum haemorrhage in Ireland: an 11-year population-based cohort study. BJOG. 2012;119(3):306–14. doi: 10.1111/j.1471-0528.2011.03198.x. [DOI] [PubMed] [Google Scholar]
- 6.Mehrabadi A, Hutcheon JA, Lee L, Kramer MS, Liston RM, Joseph KS. Epidemiological investigation of a temporal increase in atonic postpartum haemorrhage: a population-based retrospective cohort study. BJOG. 2013;120(7):853–62. doi: 10.1111/1471-0528.12149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Condous GS, Arulkumarah S, Symonds I, Chapman R, Sinha A, Razvi K. The, “tamponade test” in the management of massive postpartum hemorrhage. Obstet Gynecol. 2003;101:767–72. doi: 10.1016/s0029-7844(03)00046-2. [DOI] [PubMed] [Google Scholar]
- 8.Cho Y, Rizvi C, Uppal T, Condous G. Ultrasonographic visualization of balloon placement for uterine tamponade in massive primary postpartum hemorrhage. Ultrasound Obstet Gynecol. 2008;32(5):711–713. doi: 10.1002/uog.5408. [DOI] [PubMed] [Google Scholar]
- 9.Bakri YN, Amri A, Jabbar FA. Tamponade-balloon for obstetrical bleeding. Int J Gynaecol Obstet. 2001;74:139–42. doi: 10.1016/S0020-7292(01)00395-2. [DOI] [PubMed] [Google Scholar]
- 10.Olamijulo JA, Doufekas K. Intrauterine balloon tamponade for uncontrollable bleeding during first trimester surgical termination of pregnancy. J Obstet Gynaecol. 2007;27:441–2. doi: 10.1080/01443610701359696. [DOI] [PubMed] [Google Scholar]
- 11.Thomas RL, Gingold BR, Gallagher M. Cervical pregnancy. J Reprod Med. 1991;36:459–62. [PubMed] [Google Scholar]
- 12.Okeahialam MG, Tuffnell DJ, O’Donovan PO, Sapherson DA. Cervical pregnancy managed by suction evacuation and balloon tamponade. Eur J Obstet Gynecol Reprod Biol. 1998;79:89–90. doi: 10.1016/S0301-2115(98)00014-1. [DOI] [PubMed] [Google Scholar]
- 13.Fylstra DL, Coffey MD. Treatment of cervical pregnancy with cerclage, curettage and balloon tamponade: a report of three cases. J Reprod Med. 2001;46:71–4. [PubMed] [Google Scholar]
- 14.Bakour SH, Thompson PK, Khan KS. Successful conservative management of cervical ectopic pregnancy with combination of methotrexate, mifepristone, surgical evacuation and tamponade using a double balloon three-way catheter. J Obstet Gynaecol. 2005;25:616–18. doi: 10.1080/01443610500243620. [DOI] [PubMed] [Google Scholar]
- 15.De La Vega GA, Avery C, Nemiroff R, Marchiano D. Treatment of early cervical Pregnancy with cerclage, carboprost, curettage and balloon tamponade. Obstet Gynecol. 2007;109:505–7. doi: 10.1097/01.AOG.0000220599.74326.94. [DOI] [PubMed] [Google Scholar]
- 16.De Loor JA, van Dam PA. Foley catheters for uncontrollable obstetric or gynecologic hemorrhage. Obstet Gynecol. 1996;88:737–8. doi: 10.1016/0029-7844(96)00158-5. [DOI] [PubMed] [Google Scholar]
- 17.Goldrath MH. Uterine tamponade for the control of acute uterine bleeding. Am J Obstet Gynecol. 1983;147:869–72. doi: 10.1016/0002-9378(83)90237-5. [DOI] [PubMed] [Google Scholar]
- 18.Condi RG, Buxton EJ, Payne ES. Successful use of the Sengstaken-Blakemore tube to control massive postpartum haemorrhage. Br J Obstet Gynaecol. 1994;101:1023–4. doi: 10.1111/j.1471-0528.1994.tb13058.x. [DOI] [PubMed] [Google Scholar]
- 19.Fahy U, Sved A, Burke G. Successful balloon tamponade of post caesarean hysterectomy pelvic bleeding: a case report. Acta Obstet Gynecol Scand. 2003;82:97–8. doi: 10.1034/j.1600-0412.2003.820119.x. [DOI] [PubMed] [Google Scholar]
- 20.Akhter S, Begum MR, Kabir Z, Rashid M, Laila TR, Zabeen F. Use of a condom to control massive postpartum hemorrhage. MedGenMed. 2003;5(3):38. [PubMed] [Google Scholar]
- 21.Shivkar KS, Khadilkar S, Gandhewar M. Pressure balloon therapy in uncontrolled obstetric hemorrhage. J Obstet Gynecol Ind. 2003;53(4):338–41. doi: 10.1007/s13224-015-0790-x. [DOI] [Google Scholar]
- 22.Hasabe R, Gupta K, Rathode P. Use of condom tamponade to manage massive obstetric hemorrhage at a tertiary center in Rajasthan. J Obstet Gynaecol India. 2016;66(Suppl 1):88–93. doi: 10.1007/s13224-015-0790-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldrath MH, Fuller TA, Segal S. Laser photovaporization of endometrium for the treatment of menorrhagia. Am J Obstet Gynecol. 1981;104:14. doi: 10.1016/0002-9378(81)90251-9. [DOI] [PubMed] [Google Scholar]
- 24.Yu D, Li TC, Xia E, et al. A prospective randomized controlled trial on the effectiveness of routine Foley balloon tamponade on the reduction of bleeding after hysteroscopic resection of myoma. Gynecol Surg. 2006;3:93. doi: 10.1007/s10397-006-0188-y. [DOI] [Google Scholar]
- 25.Keriakos R, Mukhopadhyay A. The use of the Rusch balloon for management of severe postpartum haemorrhage. J Obstet Gynaecol. 2006;26:335–8. doi: 10.1080/01443610600595077. [DOI] [PubMed] [Google Scholar]
- 26.Katesmark M, Brown R, Raju KS. Successful use of a Sengstaken-Blakemore tube to control massive postpartum haemorrhage. Br J Obstet Gynaecol. 1994;101:259–60. doi: 10.1111/j.1471-0528.1994.tb13124.x. [DOI] [PubMed] [Google Scholar]
- 27.Dabelea V, Schultze PM, McDuffie RS., Jr Intrauterine balloon tamponade in the management of postpartum hemorrhage. Am J Perinatol. 2007;24(6):359–64. doi: 10.1055/s-2007-984402. [DOI] [PubMed] [Google Scholar]
- 28.Knight M. Peripartum hysterectomy in the UK: management and outcomes of the associated haemorrhage. BJOG. 2007;114:1380–7. doi: 10.1111/j.1471-0528.2007.01507.x. [DOI] [PubMed] [Google Scholar]
- 29.Seror J, Allouche C, Elhaik S. Use of Sengstaken-Blakemore tube in massive postpartum hemorrhage: a series of 17 cases. Acta Obstet Gynecol Scand. 2005;84:660–4. doi: 10.1111/j.0001-6349.2005.00713.x. [DOI] [PubMed] [Google Scholar]
- 30.Francis PN, Perkin KW, Pain MCF. Rupture of the oesophagus following use of the Sengstaken-Blakemore tube. Med J Aust. 1963;1:582–4. doi: 10.5694/j.1326-5377.1963.tb23312.x. [DOI] [PubMed] [Google Scholar]
- 31.Johanson R, Kumar M, Obhrai M, Young P. Management of massive postpartum haemorrhage: use of a hydrostatic balloon catheter to avoid laparotomy. BJOG. 2001;108:420–2. doi: 10.1111/j.1471-0528.2001.00102.x. [DOI] [PubMed] [Google Scholar]
- 32.Nelson WL, O’Brien JM. The uterine sandwich for persistent uterine atony: combining the B‐Lynch compression suture and an intrauterine Bakri balloon. Am J Obstet Gynecol 2007;e9–10. [DOI] [PubMed]
- 33.Purwosunu Y, Sarkoen W, Arulkumaran S, Segnitz J. Control of postpartum hemorrhage using vacuum-induced uterine tamponade. Obstet Gynecol. 2016;128(1):33–6. doi: 10.1097/AOG.0000000000001473. [DOI] [PubMed] [Google Scholar]
- 34.Mcquivey Ross, Block Jon, Massaro Robert. ebb® Complete tamponade system: effective hemostasis for postpartum hemorrhage. Med Dev : Evi Res. 2018;11:57–63. doi: 10.2147/MDER. [DOI] [PMC free article] [PubMed] [Google Scholar]


