Lifestyle behaviors are an important contributor to both physical and mental health (Murray et al., 2013; Sarris et al., 2014; Walsh, 2011). Systematic, meta-analytic, and narrative reviews demonstrate that there are consistent associations between mental health and behaviors such as exercise, diet, social interaction, time spent in nature, relaxation or meditation and substance use (Ashdown-Franks et al., 2020; Hoang et al., 2019; Lassale et al., 2019). Further, trials involving lifestyle interventions indicate that lifestyle change can improve mental health (Firth et al., 2019; Schuch et al., 2016), suggesting directional or causal relations. However, the direction of the relationships between these major lifestyle behaviors and mental health conditions are complex because theory and empirical work indicate that mental health conditions, particularly depressive disorders, have an apparently reciprocal effect on many lifestyle behaviors (e.g. exercise predicts reduced depressive symptoms, while depressive symptoms predict reduced exercise; Bao et al., 2017; Pereira et al., 2014). Further complicating the interpretation of previous findings, theory has argued that lifestyle behaviors influence each other and there is evidence that lifestyle behaviors cluster together (e.g. physical activity promotes healthy diet; Authors, 2020; Egger et al., 2019; Meader et al., 2016). Social determinants of health such as income and racial discrimination also impact health behaviors and outcomes as well (Braveman and Gottlieb, 2014). Regression models, with their inherent directional emphasis may fail to account for the complexity of these associations and may not be able to identify the most influential variables in the model. As such, the objective of this study is to build on previous research by looking at simultaneous associations among multiple lifestyle behaviors, social determinants of health, and depression using network models and longitudinal data.
Bidirectional Relationships Between Depression and Lifestyle Behaviors
Theoretical and empirical research demonstrate bidirectional relationships between depression and four lifestyle behaviors relevant to this study: physical activity, sleep, social interaction, and smoking.
Depression and Physical Activity
Depression has been theorized to lead to reduced physical activity via the anhedonia, slowed cognition, and low energy that characterize depression (Jerstad et al., 2010; Roshanaei-Moghaddam et al., 2009). Alternatively, exercise has been theorized to have positive impacts on mental health through a variety of biological (e.g. neurogeneration, inflammation, oxidative stress, endocrine functioning) and psychological mechanisms (e.g. self-esteem, social support, self-efficacy; Kandola et al., 2019). In general, longitudinal studies found bidirectional relationships between physical activity and depression (e.g. Azevedo Da Silva et al., 2012; Pereira et al., 2014), although the evidence is mixed (e.g. Choi et al., 2019).
Depression and Sleep
Depression and sleep impairment are both characterized by impaired Hypothalamic-pituitary-adrenal (HPA) axis and neurotransmitter functioning (Bao et al., 2017; Wulff et al., 2010). In fact, sleep impairment is one of the symptoms of major depressive and other mood disorders (American Psychiatric Association, 2013). The comorbidity of depression and insomnia may have common underlying factors such as increased arousal, which is implicated in both conditions (Staner, 2010). Sleep deprivation and depression are also both associated with similar daily patterns of cortisol levels (Adam et al., 2017). Low levels of serotonin, as well as a shared genetic basis related to the 5' regulatory region of the serotonin transporter gene, further supports the associations between depression and sleep disturbance (Cowen and Browning, 2015; Deuschle et al., 2010). Another conceptual model linking depression and insomnia frames dopamine dysregulation as a central factor such that depression may lead to dopamine dysregulation which impacts arousal and sleep (Finan and Smith, 2013). There is no consensus on the mechanisms or directions by which incident depression or insomnia might lead to the other disorder, although there is longitudinal evidence from meta-analyses showing bidirectional associations between depression and sleep in older adults (Bao et al., 2017) and college students (Dinis and Bragança, 2018).
Depression and Social Interaction
Various mechanisms may link depression with social interaction. In their review, Cruwys et al. (2014) argued that “depression is a fundamentally social disorder, with reduced social connectedness implicated as a cause, symptom, and target for treatment of depression” (p. 215). Depressed individuals have an underlying dysfunction in avoidance and approach activity patterns and as a result fail to engage positive activities such as social interaction (Trew, 2011). Behavioral activation, an efficacious treatment for depression, focuses on increasing approach behaviors and reducing avoidance goals in an effort to help the person have positive experiences which will lead to increased approach motivations (Jacobson et al., 2001). While perceived social integration (i.e. social support, a sense of belonging) seems to be more closely tied to depression than objective social interactions (i.e. social contacts, social network size), both are associated with depression (Wade and Kendler, 2000). Notably, social interactions have been associated with later social support, which in turn was associated with depressive symptoms (Peirce et al., 2000). Bidirectional, longitudinal associations between social disconnectedness and depression/anxiety (mediated by perceived isolation) were found in a sample of adults (age 57-85; Santini et al., 2020), underscoring the need to consider bidirectional interactions
Depression and Smoking
Some research has shown that depression and smoking also have strong positive associations across a range of research designs (e.g. Chaiton et al., 2009; Weinberger et al., 2017). It has been argued that depression, which often involves negative mood, might lead to smoking as a form of self-medication given that smokers often report mood enhancing effects while smoking (Munafò and Araya, 2010). At the same time, smoking may affect neurotransmitter functioning and involve mood-related withdrawal symptoms, which can contribute to depressive symptoms (Picciotto and Mineur, 2014). Some longitudinal research supports the argument that smoking leads to later depression (Boden et al., 2010), but findings from a systematic review indicate that the current understanding of direction of causation is not clear (Fluharty et al., 2017).
Lifestyle Behavior Clustering
Both theory and previous research posit that lifestyle behaviors influence each other and there is evidence that lifestyle behaviors cluster together, meaning that individuals who engage in a particular lifestyle behavior tend to engage in other behaviors. For example, exercise and smoking can predict sleep quality (positively for exercise and negatively for smoking; Brook et al., 2015; Kishida & Elavsky, 2016) while insomnia can in turn negatively affect social interaction (Hom et al., 2017), and chronic loneliness can positively predict smoking (Kobayashi and Steptoe, 2018). A systematic review demonstrated further associations of relationships among lifestyle behaviors, with alcohol and tobacco co-occurring with the greatest frequency (Meader et al., 2016).
Looking beyond paired associations, past research indicates that multiple lifestyle behaviors cluster together, meaning that they tend to co-occur with each other and are thus not independent. One theoretical model argues that “anthropogens”–man-made environments and lifestyle behaviors that can affect health and well-being–are also expected to impact engagement in other behaviors (Egger et al., 2019). Studies have shown that behaviors do cluster together, with some behaviors, including sleep, being more central within the network of behaviors (Nudelman et al., 2019). A systematic review also found evidence of clustering among four common lifestyle behaviors (smoking, nutrition, alcohol, and physical activity; Noble et al., 2015). Almost universally, research on lifestyle clustering occurs at the between-person level (variations/associations across individuals), without regard to the within-person level (variations/associations within individuals over time). One notable exception is Chevance et al., (2020) who explored within-person associations in some health behaviors following a weight management intervention. This study found that when people consumed less sugar than their average, they also consumed less fat than their average. Another exception was Authors (2020) who identified lifestyle clustering at the daily level across 14 days, where higher-than-average time spent in nature was associated with higher-than-average social interaction and exercise. In sum, the theoretical and empirical research indicate that lifestyle behaviors are associated with each other, and that multiple behaviors often cluster together, but there is less support at the within-person level.
Social Determinants of Health
Social and economic factors also play a role in lifestyle behaviors, with socioeconomic status being negatively associated with positive health behaviors. In Nudelman et al.’s (2019) study on behavior clustering, there were some differences in the most central behaviors between males and females and between low SES and high SES individuals. At the environmental level, there is a linear relationship between socioeconomic depravation and the geographic clustering of businesses or outlets that support unhealthy behavior such as establishments providing fast food, tobacco, gambling and alcohol (Macdonald et al., 2018). Systematic reviews have also found consistent associations between risk behaviors and both occupational status (Meader et al., 2016) and SES (Noble et al., 2015). Further, in one large longitudinal study, risk factors for all-cause mortality were disproportionately harmful to individuals who were of lower SES (Foster et al., 2018). Thus, the economic factors that might underly any behavior clustering must be accounted for. In light of the complexity of these relations, observational research seeking to explore how lifestyle and mental health are associated should account for the impact of social determinants of health.
The Present Study
While there is significant evidence for bidirectional associations between lifestyle behaviors and depression, as well as clustering among the lifestyle behaviors, research which accounts for all of these relationships simultaneously is needed. Following the approach of Chevance et al., (2020) who investigated changes in behavior over a one-year period as part of a weight-loss intervention, this study sought to build off of previous research by utilizing network models (Epskamp and Fried, 2018) to explore simultaneous associations between the behaviors and depression at the within- and between-person levels using three waves of surveys across two decades in a large sample of adults in the U.S. As such, this study builds on previous research by looking at the clustering of all of these factors in a national longitudinal dataset.
Methods
Data
Participants for this study were drawn from the Midlife Development in the United States (MIDUS) longitudinal panel study. This was a high-quality probability sample of adults in the contiguous United States, aged 25 to 74 years old (M = 47) at the first of three waves of data collection. The first wave of data collection occurred between 1995 and 1996, with a second wave occurring between 2004 and 2006 and a third wave between 2012 and 2014. Random digit dialing was used to recruit a representative sample, which was also accompanied by a selection of siblings, oversamples of five urban cities, and a national sample of twins (total N = 7,108). Seventy five percent (n = 4,963) of the Wave 1 sample completed the Wave 2 phone survey, adjusted for mortality (Radler and Ryff, 2010). And 78% of Wave 2 completers also participated in Wave 3 (n = 3924) and of those, 2,425 completed the self-administered questionnaire, which included many of the relevant variables for this study. A screening of the smoking variables showed discrepancies in 210 participants responses, wherein they reported a history of smoking at one wave and no history of smoking at a later wave. As such, these participants were excluded from the analysis, resulting in a sample of 6,898 participants.
Measures
Trained interviewers, who received 20 hours of general and study-specific training, administered the depression measure and smoker status item by phone, while the other items being collected by self-administered questionnaires. For the variables that were measured at each time point, the person mean centered values were included in the within-person analyses while the person means were included in the between-person analyses. Descriptive statistics are listed in Table 1.
Table 1.
Participant Characteristics
| Available data | Imputed
data (n = 7,108 per imputation) |
Completers’ data (n = 2,005) |
||
|---|---|---|---|---|
| % | n = | % | % | |
| Female | 51.49 % | 6896 | 51.50% | 53.17% |
| Minority status | 9.50% | 6062 | 9.82% | 4.67% |
| Depression W1 | 13.25% | 6898 | 13.25% | 11.99% |
| Depression W2 | 10.58% | 4753 | 10.69% | 10.33% |
| Depression W3 | 9.90% | 3132 | 9.44% | 8.41% |
| Smoker status W1 | 23.24% | 6898 | 23.24% | 16.11% |
| Smoker status W2 | 16.05% | 4753 | 15.52% | 13.19% |
| Smoker status W3 | 9.74% | 3132 | 9.91% | 9.09% |
| M (SD) | M (SD) | M (SD) | ||
| Age | 46.38 (12.98) | 6895 | 46.35 (13.00) | 44.52 (10.60) |
| Income W1 | $73,303 ($64,868) | 5921 | $73,248 ($64,821) | $84,944 ($66,697) |
| Income W2 | $71,494 ($60,434) | 3690 | $73,451 ($63,200) | $81,052 ($61,323) |
| Income W3 | $87,843 ($73,508) | 2591 | $83,496 ($69,607) | $93,148 ($73,142) |
| Exercise W1 | 43.03 (15.56) | 6073 | 43.66 (17.70) | 45.42 (13.85) |
| Exercise W2 | 74.03 (47.01) | 3501 | 69.06 (44.08) | 77.36 (44.22) |
| Exercise W3 | 77.37 (48.06) | 2561 | 81.34 (46.59) | 78.51 (47.57) |
| Social W1 | 3.05 (1.26) | 6035 | 3.04 (1.26) | 2.95 (1.21) |
| Social W2 | 3.02 (1.28) | 3817 | 3.02 (1.27) | 2.91 (1.23) |
| Social W3 | 2.98 (1.27) | 2742 | 3.01 (1.27) | 2.93 (1.25) |
| Sleep problems W1 | 1.38 (1.66) | 6059 | 1.39 (1.66) | 1.31 (1.58) |
| Sleep problems W2 | 2.10 (1.77) | 4006 | 1.99 (1.77) | 2.01 (1.73) |
| Sleep problems W3 | 2.25 (1.77) | 2759 | 2.32 (1.79) | 2.19 (1.74) |
n = number of participants who responded to the item.
Depression
As part of the telephone interview, the participants completed a version of the World Health Organization’s Composite International Diagnostic Interview Short Form (Kessler et al., 1998), which was based on the third edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 1987). Participants were asked if, over the past 12 months, they had a period of two weeks where they felt sad or blue for all or most of the day for all or most days. If they screened positive, they then reported on anhedonia and depressed affect during those two weeks. If they reported feeling either of those symptoms at least most of the day on almost every day or more, they were then screened for other symptoms such as feeling down, changes in appetite, or low energy. If the participant reported anhedonia or depressed affect and four other symptoms, they were coded as having had a depressive episode. The short-form version was shown to have high sensitivity and specificity relative to the full Composite International Diagnostic Interview (Kessler et al., 1998), which itself has demonstrated high inter-rater reliability, but has received some criticism for potentially resulting in false positives (Kurdyak and Gnam, 2005).
Physical Activity
As part of the self-administered questionnaire, participants reported on how often they engaged in moderate or vigorous physical activity. In Wave 1, this included a total of four items, asking about each intensity of physical activity in summer and winter. In Waves 2 and 3, physical activity was measured with twelve items: moderate or vigorous activity related to work, leisure, or chores, in both summer and winter. These twelve items were reduced to four items by summing the three domains of physical activity (work, leisure, or chores) for both vigorous and moderate exercise. Then for all waves, the summer and winter vigorous activity variables were averaged and then multiplied by a metabolic value (7), while the summer and winter moderate activity variables were averaged and then multiplied by a different value (5) to represent metabolic units (Buchner, 2010). Finally, these weighted values were summed to represent average physical activity. The values were standardized within each wave for the network models to aid in cross-wave comparisons.
Smoking
Participants were asked if they currently smoke cigarettes. Cigarette smoker status was listed as either 1 (current smoker) or 0 (current non-smoker) for each wave. These values were person-mean-centered for within-person analyses and the person means were included for between-person analyses.
Sleep Complaints
Participants reported on how often they had trouble getting to sleep or staying asleep during the past 30 days. The response options included “Almost every day,” “Several times a week,” “Once a week,” “Several times a month,” “Once a month,” and “Not at all.” Responses were coded such that values ranged from 0 (“Not at all”) to 5 (“Almost every day”).
Social Interaction
Two items were used to measure social interaction behaviors. The two items are “How often do you have any contact, even something as simple as saying ‘hello’, with any of your neighbors?” and “How often do you have a real conversation or get together socially with any of your neighbors?”. Responses were on a 6-point continuum (1 = almost every day; 6 = never or hardly ever). Previous research used this composite variable to demonstrate longitudinal associations between social interaction and eudaimonic well-being (Greenfield and Reyes, 2015).
Income
Participants reported their total household income at each wave.
Racial/Ethnic Minority Status
All participants reported on their racial and ethnic status. White, non-Hispanic participants were the reference group (coded as 0) and participants who were racial or ethnic minorities were coded as 1.
Time
The wave number was also included in the analyses (scaled to 0, .5, and 1) to assess the influence of the passage of time on the other variables in the within-person network models. For example, a negative within-person association between physical activity and time would indicate that as people age, they exercise less.
Analyses
This dataset included a mixture of variable types, with some dichotomous (smoking, depression) some continuous (income) and some ordinal (sleep problems). The variables were person centered for the within-person model and the person-means were calculated in the between-person model. Because most network model software is focused on one type of data (all dichotomous/binary or all continuous normal) we utilized the BGGM package (Williams and Mulder, 2020) in R (R Core Team, 2020) and RStudio (R Studio Team, 2020), which can analyze mixed data types. Similar to other software, the network models produced by BGGM are correlations controlling for the other variables in the model (partial correlations). The Bayesian approach of BGGM results in estimated posterior means, standard deviations, and credible lower and upper bounds.
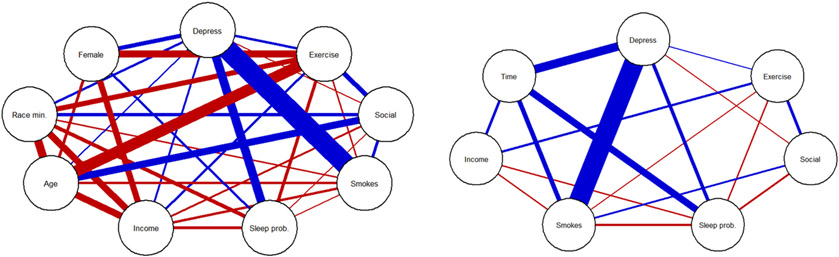
To visualize the network models, partial correlation matrices obtained from BGGM were graphed with the package qgraph (Epskamp et al., 2012). When the percentile-based 95% credible interval of the edge estimates failed to include 0, they were represented as a line in the network model. Solid edges represent a positive association between pairs of variables while dashed edges represent negative associations. The thickness of the lines represent the size of the association, with thicker lines representing larger partial correlations.
Two different models were run: a between-person network model and a within-person network model. The between-person network model represents the partial correlations between the averages of the lifestyle behaviors, depression, and other variables. To carry out this model, participant means of each variable were obtained by averaging the variables across the three waves of data. This model explored how average levels of variables, across a 20-year span, are associated with each other. For example, do people who have a history of smoking across those 20 years also tend to have a history of depression? The second model, the within-person network model, represents the associations between the study variables at each wave, after subtracting out the person-means from the three waves of data (see Costantini et al., 2019). This process results in three waves of person-centered variables for each participant. The within-person network model can, for example, can be used to examine whether fluctuations around each participant's mean of exercise in a given wave are associated with fluctuations in the participant’s sleep – or in other words, if someone is exercising more than their average at a certain wave, do they also have better quality of sleep than their average?
Along with the direction and size of associations, it was also of interest to assess the centrality of the variables in the network. Strength centrality indices were calculated to observe which variables are most central within the networks, meaning that they have many connections to the other variables. Although there are many forms of centrality, strength has assumptions that fit psychological/behavioral network models better than other indices (Bringmann et al., 2019). Strength centrality is a calculation of the absolute edge weights for each node, such that the value is a composite of all associations (positive or negative) a node has with other nodes.
To handle missing data, multilevel multiple imputation was conducted with the mice package (van Buuren and Groothuis-Oudshoorn, 2011) using the available data. Sensitivity analyses were also completed using participants who provided complete data on all three waves of data. The network models described in the manuscript are based on fifteen imputed datasets, while the networks using the data from only participants who provided data at all three waves are provided in the supplementary materials. All analyses were conducted with the R statistical software and the statistical code can be obtained at https://osf.io/fhuqz/.
Data Sharing Statement
Are de-identified individual participant data available (including data dictionaries)? Yes, from the Inter-university Consortium for Political and Social Research (https://www.icpsr.umich.edu/web/ICPSR/series/203). What data in particular are shared? All of the individual participant data collected during the study were made available, after de-identification. What other documents are available? The author’s script for running the data cleaning and analysis in R, analyses output, and an overview of the supporting documentation.
Results
Demographic variables can be seen in Table 1, with summary statistics given for all available data, for the imputed data, and for completers only. Based off the imputed data participants were on average 46 years old (SD = 12.98), slightly more likely to be female (51.59%), mostly White (91.18%), and had an average salary at Wave 1 of $73,394 (SD = $65,023). At Wave 1, 13.25% of individuals reported being depressed and by Wave 3 that value was 9.67%. Twenty three percent of participants smoked at Wave 1, while 15.52% smoked at Wave 2 and 10.12% smoked at Wave 3. In an investigation of the missing data, minority individuals, lower income individuals, and participants who smoked at Wave 1 were less likely to complete all three waves of data collection. This differential attrition supports the use of the multiple imputation technique.
Between-Person Network
The between-person network model–based on the partial correlation matrices for person means of the relevant variables–is depicted in Figure 1. The larger effects involving the depression and the lifestyle behavior variables are discussed here, while the complete partial correlation estimates can be seen in the supplementary materials. Based on the weight of the edges, the models revealed that the association between smoking and depression was one of the stronger relationships (rp = .63, 95% CI [.61, .64])–the proportion of waves of being a smoker was associated with proportion of waves being depressed, controlling for other associations. Depression was also positively associated with sleep problems (rp = .26, 95% CI [.24, .27]), being female (rp = .13, 95% CI [.09, .24]) and surprisingly, exercise (rp = .06, 95% CI [.04, .09]). Exercise was negatively associated with baseline age (rp = −.35, 95% CI [−.36, −.33]), being female (rp = −.21, 95% CI [−.23, −.19]), and being a minority (rp = −.16, 95% CI [−.18, −.12]), while it was positively associated with social interaction (rp = .14, 95% CI [.13, .16]). Social interaction was positively associated with baseline age (rp = .22, 95% CI [.21, .24]) and racial minority participants tended to have fewer sleep problems (rp = −.12, 95% CI [−.15, −.10]).
Figure 1. Between-person and within-person network model.
Nodes (circles) on the left represent the between-person variables (averaged across all waves for variables measured more than once). Nodes on the right represent the within-person variables (person-centered). Edges (lines) represent partial correlations among the variables. The type of the lines indicate the direction of association: blue = positive; red = negative. The width of the lines represent the size of the associations: thicker = larger; thinner = smaller.
The strength centrality indices suggested that the most central nodes were depression (1.25), age (1.18), exercise (1.09), and smoker status (0.93). The other nodes, in descending order of centrality, were race (0.90), income (0.87), sleep (0.67), female gender (0.66), and social interaction (0.63).
Within-Person Network
As with the between-person network, depression and smoking were strongly positively related at the within-person level (rp = .54, 95% CI [.53, .55]). This indicates that fluctuations in depression, around one’s average chance of being depressed, was positively associated with fluctuations in smoking status. Time had some of the stronger relationships as well including positive associations with depression (rp = .23, 95% CI [.22, .25]), sleep problems (rp = .19, 95% CI [.16, .20]), and smoker status (rp = .14, 95% CI [.12, .15]), indicating that as time progressed, participants were more likely to report depression, sleep problems, and transition to smoker status. Exercise surprisingly had a small positive association with depression (rp = .02, 95% CI [.001, .04]), while it was also positively associated with social interaction (rp = .08, 95% CI [.05, .09]), and income (rp = .05, 95% CI [.03, .07]), and negatively associated with sleep problems (rp = −.03, 95% CI [−.04, −.01]). Besides these associations, there were other small associations which can be seen in the figure and supplementary materials.
The strength centrality indices were highest for depression (0.91) and lowest for social interaction (0.17). Falling between these values were smoker status (0.83), time (0.63), sleep problems (0.45), income (0.20), and exercise (0.19).
Discussion
Consistent with the extensive prior research on lifestyle behaviors and depression that uses bivariate analyses, the current study’s the network models revealed a number of associations between the network nodes. These findings represent an important initial step in exploring the complex ways in which behaviors may influence each other and mental health. Further, we found that certain variables–in particular, smoking–are related to other variables to a higher degree, while some variables–notably social interaction with neighbors–have weaker associations to other components in the network.
In both the between and within-person models, depression and smoking were some of the most central components in the network. Across the within- and between-person models, the centrality indices for the common variables were generally similar with depression and smoker status being high, while social interaction was the lowest. However, exercise was a more central variable in the between-person network model than in the within-person model.
The clustering of lifestyle behaviors in this and previous studies (e.g., Authors, 2020; Nudelman et al., 2019) has potentially useful clinical implications. For instance, if certain behaviors are strongly associated, controlling for all other associations, attempting to intervene on one may potentially bring about changes in the others. As such, this model indicates that smoker status may be the variable that is most highly linked to depression and may be the best target of lifestyle change if depression is the outcome of interest. Viewed from an alternative angle, some behaviors may be resistant to change unless the other highly related variables are also targeted, meaning that if smoker status is the target of change, seeking to directly intervene on smoking might be more effective if depressive symptoms are also treated (Brown et al., 2001). Thus, future research could test whether highly associated nodes can support change in untargeted variables (e.g., smoking cessation treatment leads to reduced depression) or create resistances to change in targeted variables (e.g., smoking cessation will not be successful unless depression is also targeted).
A parallel argument can be made for the centrality indices. If a behavior or condition is highly central, as depression and smoking were, then that behavior or condition may have a disproportionate effect on the rest of the network. As such, future research questions center on whether targeting change in that central behavior or condition may have especially beneficial impact on overall lifestyle profile. Alternatively, it may be better to work on peripheral nodes, which may be more amenable to change because they are less tied to other change-resistant behaviors or disorders. In moving forward to test these hypotheses, the literature on multiple behavior change indicates that focusing on a moderate number of behaviors (e.g. 2-3), rather than too few (1) or too many (≥ 4) tends to have the greatest outcomes (Wilson et al., 2015). The findings from network studies, especially for individualized networks, might guide practitioners in focusing on those two or three behaviors that are core to the network of health.
Income, as one indicator of socioeconomic status, had a positive association with depression at the between person level, but fluctuations in income at the within-person level was not associated with depression. At the within-person level, income was also less central in the network, potentially indicating that change in income, by itself, may not have large effects on this network of behaviors and conditions, but it is important to recognize that even small effects are important in behavior change and health (Paulus and Thompson, 2019). At the between-person level, females were more likely to be depressed, less likely to exercise, more likely to have sleep problems, and tended to have lower incomes. When making sense of the disparities in depression diagnoses across gender (Van de Velde et al., 2010), these models indicate that some of these gender-associated lifestyle behaviors and determinants of health need to be accounted for.
This large-interval longitudinal study shows some of the between-person associations with lifestyle behaviors as well as within-person fluctuations across 8 or 9 years at a time. The within-person data analysis perspective is essential for understanding changes over time, which is missed in analyses focused on between-person associations (Hamaker, 2012). Future research could focus on how to individualize behavior change targets by conducting intensive experience sampling studies to measure lifestyle behaviors and conditions of interest, such as depression, anxiety, and pain. An adequate (> 40-50, depending on model complexity; Epskamp et al., 2018) number of measurements allows for the creation of personalized network models, showing unique edge weights and node centrality for each person. Using this information, providers could be informed as to what behaviors are most influential within the person’s life or potentially, which are more amenable to change. Integrating this form of measurement into personalized lifestyle interventions would be especially enlightening to show changes in the individualized networks over time.
There were some limitations to this study. First, in terms of measurement, many epidemiological studies such as the MIDUS study assess numerous constructs and as such, the measurement of specific constructs may be limited. This was especially the case for sleep problems, which was measured with a single item. Second, the MIDUS surveys involved a significant amount of attrition. The imputation appears to have been generally effective, but there may be some sources of bias in the findings due to loss of participants over the two decades. Self-reported physical activity was measured somewhat differently in Waves 2 and 3 relative to Wave 1, which raises some concerns. However, longitudinal measurement invariance analyses (available at https://osf.io/fhuqz/) provide evidence that the items performed similarly across waves. Despite efforts to specifically recruit minority participants, the sample was mostly white, with higher household income than the average family. As such, the findings may not be fully generalizable to the U.S. population. Lastly, there were a number of important lifestyle factors that were not assessed in this study (e.g. dietary patterns, sedentary time, and alcohol consumption). If future studies include those variables, we may see changes to the observed network structure, including novel associations and modifications of the associations demonstrated in this study.
Overall, this study elucidates the complex networks of lifestyle behaviors, social determinants of health, and depression. Studies often consider unidirectional relationships between these variables, but a thorough review of the literature commonly reveals bidirectional associations. The use of network models in this study allowed for an examination of how all of these factors are related at the between-person and within-person levels over about two decades, in a large sample of U.S. adults. With certain behaviors having strong bivariate partial correlations and high centrality in the networks (e.g. depression and smoking), future research should examine how lifestyle interventions can be personalized to account for these variables’ place within networks of lifestyle and health.
Supplementary Material
Acknowlegments:
Writing of this manuscript was supported by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment - Department of Veterans Affairs, the VISN 17 Center of Excellence for Research on Returning War Veterans, and the Central Texas Veterans Health Care System. Adam P. Mcguire is partially supported by a Small Projects in Rehabilitation Research Award I21-RX003035, Sheila B. Frankfurt is supported by Career Development Award IK2 RX003495, and Yvette Z. Szabo is supported by Career Development Award IK1-RX003122 from the United States Department of Veterans Affairs, Rehabilitation Research and Development Service. The views expressed herein are those of the authors and do not necessarily reflect the official policy or position of the Department of Veterans Affairs or the United States Government.
References
- Adam EK, Quinn ME, Tavernier R, et al. (2017) Diurnal cortisol slopes and mental and physical health outcomes: A systematic review and meta-analysis. Psychoneuroendocrinology 83: 25–41. DOI: 10.1016/j.psyneuen.2017.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (1987) Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R). Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. American Psychiatric Association. DOI: 10.1176/appi.books.9780890425596. [DOI] [Google Scholar]
- Ashdown-Franks G, Firth J, Carney R, et al. (2020) Exercise as medicine for mental and substance use disorders: A meta-review of the benefits for neuropsychiatric and cognitive outcomes. Sports Medicine 50(1): 151–170. DOI: 10.1007/s40279-019-01187-6. [DOI] [PubMed] [Google Scholar]
- Azevedo Da Silva M, Singh-Manoux A, Brunner EJ, et al. (2012) Bidirectional association between physical activity and symptoms of anxiety and depression: the Whitehall II study. European Journal of Epidemiology 27(7): 537–546. DOI: 10.1007/s10654-012-9692-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y-P, Han Y, Ma J, et al. (2017) Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: Meta-analysis and systematic review. Neuroscience & Biobehavioral Reviews 75: 257–273. DOI: 10.1016/j.neubiorev.2017.01.032. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM and Horwood LJ (2010) Cigarette smoking and depression: tests of causal linkages using a longitudinal birth cohort. The British Journal of Psychiatry 196(6). Cambridge University Press: 440–446. DOI: 10.1192/bjp.bp.109.065912. [DOI] [PubMed] [Google Scholar]
- Braveman P and Gottlieb L (2014) The social determinants of health: It’s time to consider the causes of the causes. Public Health Reports 129(1_suppl2). SAGE Publications Inc: 19–31. DOI: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann LF, Elmer T, Epskamp S, et al. (2019) What do centrality measures measure in psychological networks? Journal of Abnormal Psychology 128(8). US: American Psychological Association: 892–903. DOI: 10.1037/abn0000446. [DOI] [PubMed] [Google Scholar]
- Brook JS, Zhang C, Seltzer N, et al. (2015) Insomnia in adults: The impact of earlier cigarette smoking from adolescence to adulthood. Journal of Addiction Medicine 9(1): 40–45. DOI: 10.1097/ADM.0000000000000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Niaura R, et al. (2001) Cognitive–behavioral treatment for depression in smoking cessation. Journal of Consulting and Clinical Psychology 69(3). US: American Psychological Association: 471–480. DOI: 10.1037/0022-006X.69.3.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchner DM (2010) Health benefits of physical activity. In: Brown D, Heath G, and Martin S (eds) Promoting Physical Activity: A Guide for Community Action. 2nd ed. Champaign, IL: Human Kinetics, pp. 1–20. [Google Scholar]
- Chaiton MO, Cohen JE, O’Loughlin J, et al. (2009) A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC public health 9: 356. DOI: 10.1186/1471-2458-9-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevance G, Golaszewski NM, Baretta D, et al. (2020) Modelling multiple health behavior change with network analyses: results from a one-year study conducted among overweight and obese adults. Journal of Behavioral Medicine 43(2): 254–261. DOI: 10.1007/s10865-020-00137-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KW, Chen C-Y, Stein MB, et al. (2019) Assessment of bidirectional relationships between physical activity and depression among adults: A 2-sample mendelian randomization study. JAMA Psychiatry 76(4): 399–408. DOI: 10.1001/jamapsychiatry.2018.4175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowen PJ and Browning M (2015) What has serotonin to do with depression? World Psychiatry 14(2): 158–160. DOI: 10.1002/wps.20229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantini G, Richetin J, Preti E, Casini E, Epskamp S, & Perugini M (2019). Stability and variability of personality networks: A tutorial on recent developments in network psychometrics. Personality and Individual Differences, 136, 68–78. 10.1016/j.paid.2017.06.011 [DOI] [Google Scholar]
- Cruwys T, Haslam SA, Dingle GA, et al. (2014) Depression and social identity: An integrative review. Personality and Social Psychology Review 18(3): 215–238. DOI: 10.1177/1088868314523839. [DOI] [PubMed] [Google Scholar]
- Deuschle M, Schredl M, Schilling C, et al. (2010) Association between a serotonin transporter length polymorphism and primary insomnia. Sleep 33(3): 343–347. DOI: 10.1093/sleep/33.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinis J and Bragança M (2018) Quality of sleep and depression in college students: a systematic review. Sleep Science 11(4). Brazilian Association of Sleep and Latin American Federation of Sleep: 290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger G, Stevens J, Binns A, et al. (2019) Psychosocial determinants of chronic disease: implications for lifestyle medicine. American Journal of Lifestyle Medicine 13(6): 526–532. DOI: 10.1177/1559827619845335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S and Fried EI (2018) A tutorial on regularized partial correlation networks. Psychological Methods 23(4): 617–634. DOI: 10.1037/met0000167. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, et al. (2012) Qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software 48(4). University of California at Los Angeles: 1–18. [Google Scholar]
- Epskamp S, van Borkulo CD, van der Veen DC, et al. (2018) Personalized network modeling in psychopathology: the importance of contemporaneous and temporal connections. Clinical Psychological Science 6(3): 416–427. DOI: 10.1177/2167702617744325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finan PH and Smith MT (2013) The comorbidity of insomnia, chronic pain, and depression: Dopamine as a putative mechanism. Sleep Medicine Reviews 17(3): 173–183. DOI: 10.1016/j.smrv.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J, Teasdale SB, Allott K, et al. (2019) The efficacy and safety of nutrient supplements in the treatment of mental disorders: a meta-review of meta-analyses of randomized controlled trials. World psychiatry: official journal of the World Psychiatric Association (WPA) 18(3): 308–324. DOI: 10.1002/wps.20672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fluharty M, Taylor AE, Grabski M, et al. (2017) The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine & Tobacco Research 19(1). Oxford Academic: 3–13. DOI: 10.1093/ntr/ntw140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster HME, Celis-Morales CA, Nicholl BI, et al. (2018) The effect of socioeconomic deprivation on the association between an extended measurement of unhealthy lifestyle factors and health outcomes: a prospective analysis of the UK Biobank cohort. The Lancet Public Health 3(12): e576–e585. DOI: 10.1016/S2468-2667(18)30200-7. [DOI] [PubMed] [Google Scholar]
- Greenfield EA and Reyes L (2015) Continuity and change in relationships with neighbors: implications for psychological well-being in middle and later life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 70(4): 607–618. DOI: 10.1093/geronb/gbu084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamaker E (2012) Why researchers should think ‘within-person’: A paradigmatic rationale. In: Mehl MR and Conner TS (eds) Handbook of Research Methods for Studying Daily Life, pp. 43–61. [Google Scholar]
- Hoang D, Kristoffersen I and Li IW (2019) All in the mind? Estimating the effect of mental health on health behaviours. Social Science & Medicine 225: 69–84. DOI: 10.1016/j.socscimed.2019.02.017. [DOI] [PubMed] [Google Scholar]
- Hom MA, Hames JL, Bodell LP, et al. (2017) Investigating insomnia as a cross-sectional and longitudinal predictor of loneliness: Findings from six samples. Psychiatry Research 253: 116–128. DOI: 10.1016/j.psychres.2017.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Martell CR and Dimidjian S (2001) Behavioral activation treatment for depression: returning to contextual roots. Clinical Psychology: Science and Practice 8(3): 255–270. DOI: 10.1093/clipsy.8.3.255. [DOI] [Google Scholar]
- Jerstad SJ, Boutelle KN, Ness KK, et al. (2010) Prospective reciprocal relations between physical activity and depression in female adolescents. Journal of Consulting and Clinical Psychology 78(2). US: American Psychological Association: 268–272. DOI: 10.1037/a0018793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandola A, Ashdown-Franks G, Hendrikse J, et al. (2019) Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neuroscience and Biobehavioral Reviews 107: 525–539. DOI: 10.1016/j.neubiorev.2019.09.040. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, et al. (1998) The World Health Organization composite international diagnostic interview short-form (CIDI-SF). International journal of methods in psychiatric research 7(4). Wiley Online Library: 171–185. [Google Scholar]
- Kishida M and Elavsky S (2016) An intensive longitudinal examination of daily physical activity and sleep in midlife women. Sleep Health 2(1). Sleep Health in Early Care and Education: 42–48. DOI: 10.1016/j.sleh.2015.12.001. [DOI] [PubMed] [Google Scholar]
- Kobayashi LC and Steptoe A (2018) Social isolation, loneliness, and health behaviors at older ages: longitudinal cohort study. Annals of Behavioral Medicine 52(7): 582–593. DOI: 10.1093/abm/kax033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurdyak PA and Gnam WH (2005) Small signal, big noise: Performance of the cidi depression module. The Canadian Journal of Psychiatry 50(13). SAGE Publications Inc: 851–856. DOI: 10.1177/070674370505001308. [DOI] [PubMed] [Google Scholar]
- Lassale C, Batty GD, Baghdadli A, et al. (2019) Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Molecular Psychiatry 24(7): 965–986. DOI: 10.1038/s41380-018-0237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macdonald L, Olsen JR, Shortt NK, et al. (2018) Do ‘environmental bads’ such as alcohol, fast food, tobacco, and gambling outlets cluster and co-locate in more deprived areas in Glasgow City, Scotland? Health & Place 51: 224–231. DOI: 10.1016/j.healthplace.2018.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meader N, King K, Moe-Byrne T, et al. (2016) A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health 16. DOI: 10.1186/s12889-016-3373-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munafò MR and Araya R (2010) Cigarette smoking and depression: a question of causation. The British Journal of Psychiatry 196(6). Cambridge University Press: 425–426. DOI: 10.1192/bjp.bp.109.074880. [DOI] [PubMed] [Google Scholar]
- Murray CJL, Abraham J, Ali MK, et al. (2013) The state of US health, 1990-2010: Burden of diseases, injuries, and risk factors. JAMA 310(6). American Medical Association: 591–606. DOI: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble N, Paul C, Turon H, et al. (2015) Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Preventive Medicine 81: 16–41. DOI: 10.1016/j.ypmed.2015.07.003. [DOI] [PubMed] [Google Scholar]
- Nudelman G, Kalish Y and Shiloh S (2019) The centrality of health behaviours: A network analytic approach. British Journal of Health Psychology 24(1): 215–236. DOI: 10.1111/bjhp.12350. [DOI] [PubMed] [Google Scholar]
- Paulus MP and Thompson WK (2019) The Challenges and opportunities of small effects: The new normal in academic psychiatry. JAMA Psychiatry 76(4): 353. DOI: 10.1001/jamapsychiatry.2018.4540. [DOI] [PubMed] [Google Scholar]
- Peirce RS, Frone MR, Russell M, et al. (2000) A longitudinal model of social contact, social support, depression, and alcohol use. Health Psychology 19(1). US: American Psychological Association: 28–38. DOI: 10.1037/0278-6133.19.1.28. [DOI] [PubMed] [Google Scholar]
- Pereira SMP, Geoffroy M-C and Power C (2014) Depressive symptoms and physical activity during 3 decades in adult life: Bidirectional associations in a prospective cohort study. JAMA Psychiatry 71(12): 1373–1380. DOI: 10.1001/jamapsychiatry.2014.1240. [DOI] [PubMed] [Google Scholar]
- Picciotto MR and Mineur YS (2014) Molecules and circuits involved in nicotine addiction: The many faces of smoking. Neuropharmacology 76. NIDA 40th Anniversary Issue: 545–553. DOI: 10.1016/j.neuropharm.2013.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2020) R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. Available at: https://www.R-project.org/. [Google Scholar]
- R Studio Team (2020) RStudio: Integrated Development for R. Boston, MA: RStudio, PBC. Available at: https://www.rstudio.com/. [Google Scholar]
- Radler BT and Ryff CD (2010) Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well-being. Journal of Aging and Health 22(3): 307–331. DOI: 10.1177/0898264309358617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roshanaei-Moghaddam B, Katon WJ and Russo J (2009) The longitudinal effects of depression on physical activity. General Hospital Psychiatry 31(4): 306–315. DOI: 10.1016/j.genhosppsych.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Santini ZI, Jose PE, Koyanagi A, et al. (2020) Formal social participation protects physical health through enhanced mental health: A longitudinal mediation analysis using three consecutive waves of the Survey of Health, Ageing and Retirement in Europe (SHARE). Social Science & Medicine (1982) 251: 112906. DOI: 10.1016/j.socscimed.2020.112906. [DOI] [PubMed] [Google Scholar]
- Sarris J, O’Neil A, Coulson CE, et al. (2014) Lifestyle medicine for depression. BMC Psychiatry 14: 107. DOI: 10.1186/1471-244X-14-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch FB, Vancampfort D, Richards J, et al. (2016) Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. Journal of Psychiatric Research 77: 42–51. DOI: 10.1016/j.jpsychires.2016.02.023. [DOI] [PubMed] [Google Scholar]
- Staner L (2010) Comorbidity of insomnia and depression. Sleep Medicine Reviews 14(1): 35–46. DOI: 10.1016/j.smrv.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Trew JL (2011) Exploring the roles of approach and avoidance in depression: An integrative model. Clinical Psychology Review 31(7): 1156–1168. DOI: 10.1016/j.cpr.2011.07.007. [DOI] [PubMed] [Google Scholar]
- van Buuren S and Groothuis-Oudshoorn K (2011) mice: Multivariate imputation by chained equations in R. Journal of Statistical Software 045(103). Foundation for Open Access Statistics. Available at: https://ideas.repec.org/a/jss/jstsof/v045i03.html (accessed 4 March 2021). [Google Scholar]
- Van de Velde S, Bracke P and Levecque K (2010) Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Social Science & Medicine 71(2): 305–313. DOI: 10.1016/j.socscimed.2010.03.035. [DOI] [PubMed] [Google Scholar]
- Wade TD and Kendler KS (2000) The relationship between social support and major depression: Cross-sectional, longitudinal, and genetic perspectives. The Journal of Nervous and Mental Disease 188(5). United States: Lippincott Williams & Wilkins, Inc: 251–258. DOI: 10.1097/00005053-200005000-00001. [DOI] [PubMed] [Google Scholar]
- Walsh R (2011) Lifestyle and mental health. American Psychologist 66(7): 579–592. DOI: 10.1037/a0021769. [DOI] [PubMed] [Google Scholar]
- Weinberger AH, Kashan RS, Shpigel DM, et al. (2017) Depression and cigarette smoking behavior: A critical review of population-based studies. The American Journal of Drug and Alcohol Abuse 43(4). Taylor & Francis: 416–431. DOI: 10.3109/00952990.2016.1171327. [DOI] [PubMed] [Google Scholar]
- Williams D and Mulder J (2020) BGGM: Bayesian gaussian graphical models in R. Journal of Open Source Software 5(51): 2111. DOI: 10.21105/joss.02111. [DOI] [Google Scholar]
- Wilson K, Senay I, Durantini M, et al. (2015) When it comes to lifestyle recommendations, more is sometimes less: A meta-analysis of theoretical assumptions underlying the effectiveness of interventions promoting multiple behavior domain change. Psychological Bulletin 141(2). American Psychological Association: 474–509. DOI: 10.1037/a0038295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wulff K, Gatti S, Wettstein JG, et al. (2010) Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nature Reviews Neuroscience 11(8). 8. Nature Publishing Group: 589–599. DOI: 10.1038/nrn2868. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.