Abstract
Introduction
How care‐related time and emotional health over the day differ for those assisting older adults with and without dementia is unclear.
Methods
Using 2134 time diaries from the National Study of Caregiving, we compared emotional health and care time for caregivers of older adults with and without dementia.
Results
Caregivers to older adults with dementia experienced worse (higher scores) on a composite measure of negative emotional health (4.2 vs 3.3; P < .05) and provided more physical/medical care (33.7 vs 16.2 minutes; P < .05) and less transportation assistance (12.6 vs 24.8 minutes; P < .05) than other caregivers. In models, providing physical/medical care was associated with worse emotional health (β = 0.15; P < .01) and socializing with the care recipient was associated with worse emotional health when the recipient had dementia (β = 0.28; P < .01).
Discussion
Findings highlight the opportunity for targeted interventions to address the emotional consequences of different types of care time in the context of dementia.
Keywords: care activities, dementia, emotional health, family caregiving, time use, well‐being
1. INTRODUCTION
Impending increases in the number of older adults who will be living with dementia 1 , 2 have raised concerns about the demands that will be placed on family and unpaid caregivers who provide the bulk of assistance to older adults with and without dementia. 3 , 4 Family caregiving most commonly takes the form of help with household activities (making meals or shopping) as well as help with physical care (eg, help bathing, dressing, or walking) or medical activities (eg, managing medications, overseeing medical care). In addition, social aspects of care and transportation are increasingly recognized as important care tasks. 4
The distinctive implications for well‐being of caring for someone living with dementia have been well documented. 5 , 6 , 7 Much of this research focuses on appraisals of personal and role‐related strains that may be a consequence of providing substantial amounts of care to older adults with dementia. 8 , 9 , 10 Emotional differences by types of tasks have been described previously. 11 , 12 For example, family caregivers who assist with more household, personal care, and health care–related tasks are more likely than others to report emotional difficulty with care. 12 Whether caregivers to older adults with dementia spend more time in emotionally challenging activities than other caregivers‐or whether particular activities are more likely to elicit negative emotion in the context of dementia‐remains unclear.
A growing number of studies have used time diaries to examine the activities and emotional responses (hereafter, “emotional health”) of caregivers as they are experienced, typically on the prior day. An advantage of analyzing a day in the life of caregivers is the ability to characterize their highly individualized rhythm of assistance and recollection of mood as experienced over the day. 13 For example, using the American Time Use Study (ATUS), He et al. found relative to non‐caregivers, worse emotional health among caregivers to older adults. 14 Other studies have documented differences in caregivers’ daily emotional health and stressors by care‐recipient characteristics and engagement level. 15 , 16 , 17 , 18 Yet, emotional health has not been compared systematically for caregivers who are assisting older adults with dementia and those assisting for other reasons. Moreover, investigations into the emotional implications of different types of care time, and how they may differ when the care recipient is living with dementia, are lacking. A better understanding of differences in care time may help identify ways to help family caregivers navigate care while preserving emotional health.
This study examines the relationship between amount of time spent providing care and four negative emotions—frustration, worry, sadness, and stress—experienced on the prior day among caregivers to older adults with and without dementia. We investigate three questions:
How does the emotional health of caregivers differ for these groups?
How does care time differ?
Does the association between care time and emotional health differ?
Based on prior evidence, we expect that caregivers to older adults with dementia will have worse emotional health and will spend more time than other caregivers on care tasks that are more emotionally challenging. We further expect that care time activities will be associated with worse emotional health for caregivers to older adults with dementia.
2. DATA AND METHODS
2.1. Data
This observational study draws upon time diary data from the National Study of Caregiving (NSOC) linked to comprehensive information from older adults participating in the National Health and Aging Trends Study (NHATS). We used data from the linked 2017 NSOC and NHATS. NHATS is an ongoing panel study of Medicare beneficiaries ages 65 and older. Annual NHATS interviews assess participants’ physical and cognitive functioning along with assistance in daily activities. 19 In 2017, family and unpaid caregivers of NHATS participants were contacted and invited to complete a 30‐minute survey by telephone. Trained interviewers asked questions about care‐related topics including activities for which help was provided, effects of providing assistance, and demographic information. The vast majority of NSOC interviews were completed within 4 weeks of the NHATS interview. NHATS had an initial response rate of 71% and consistently had response rates in the 85% to 95% range at follow‐up rounds; the 2017 NSOC response rate was ≈ 60%.
HIGHLIGHTS
Caregivers to older adults with dementia experience worse emotional health than other caregivers.
Caregivers provide more physical and medical care to recipients with dementia.
Time spent on physical and medical care is associated with worse emotional health.
Social time is associated with worse emotional health in the context of dementia.
RESEARCH IN CONTEXT
Systematic Review: The authors identified articles on caregiving to older adults with dementia, emotional health, and time use using PubMed. Review articles are cited documenting worse well‐being for caregivers assisting those with dementia and time diary studies are cited comparing emotional health of caregivers with other adults and differences among caregivers.
Interpretation: Findings regarding worse emotional health on the prior day for caregivers assisting those with dementia are consistent with peer‐reviewed publications finding worse well‐being for this group. We also newly document two reasons for worse emotional health: compared to other caregivers, those assisting recipients with dementia provide more physical and medical assistance, which is more emotionally challenging than other activities, and socializing with the care recipient is emotionally challenging when the recipient has dementia.
Future Directions: We call for targeted training efforts to address the emotional consequences associated with different types of care time in the context of dementia.
Following the NSOC interview, a time diary interview was completed by telephone with 82% of eligible respondents (N = 2136). The NSOC time diary interview asked about all activities occurring on the previous day. Descriptions of main activities and up to five secondary activities (defined as activities carried out at the same time as the main activity but not the primary focus of the respondent) were recorded in open‐text fields. For each main activity, respondents were asked follow‐up questions about how long the activity took, where they were, with whom they were doing the activity, who else was there, and for household and care activities for whom the activity was carried out. After the interview, trained coders assigned each activity to a detailed set of three‐digit categories that captured all possible activities in the day, including care activities. 20 After removing two diaries that were missing detailed well‐being responses, the final analytic sample consisted of 2134 NSOC respondents with completed diary interviews.
The Johns Hopkins Bloomberg School of Public Health Institutional Review Board approved this study.
2.2. Measures
2.2.1. Caregiver emotional health
The NSOC time diaries measured experienced well‐being over the day. 13 For three randomly selected activities (the first selected from 8 am to 12 pm; the second from 12 pm to 4 pm, and the third from 4 pm to 8 pm), respondents were asked to report how intensely they felt four negative emotions—frustration, worry, sadness, and stress—using a scale from 0 (not at all) to 6 (very strong). A fifth negative construct (tired) did not differ by whether the care recipient had dementia and was not as strongly related to the other items so was omitted. This approach, referred to originally as the Day Reconstruction Method, 21 has been incorporated into several national surveys and validated for psychometric properties, including the identification of a strong negative emotional domain. 22 We averaged each of the emotions over the three activities to form average frustration, worry, sadness and stress, and also summed these averages to form a composite of negative emotional health. In our sample, the scale ranged from 0 to 24 and Cronbach's alpha = 0.89.
2.2.2. Dementia
Using responses to the 2017 NHATS, we classified each care recipient as having probable dementia (N = 701) or not (N = 1433). Individuals were classified as having probable dementia if they met the following criteria: (1) the participant or a proxy respondent reported that a doctor had ever told the sample person that he/she had dementia or Alzheimer's disease; (2) a proxy gave responses to the Eight‐item Interview to Differentiate Aging and Dementia (AD8) screener that met the likely dementia threshold (a score of 2 or higher 23 , 24 ); or (3) an individual scored at or below 1.5 SDs from the mean in at least two cognitive domains based on test items that evaluate the sample person's memory, orientation, and executive function. The NHATS probable dementia classification was validated against a consensus panel's research diagnosis of dementia for a sample of 121 participants in the Health and Retirement Study's Aging, Demographics and Memory Study (ADAMS), which based its determination on a 3‐ to 4‐hour structured in‐home clinical assessment and medical records. 25 Relative to ADAMS, the NHATS classification had 66% sensitivity and 87% specificity. 26
2.2.3. Care activities
Based on NSOC's three‐digit activity coding scheme, we classified main activities reported in the diary into one of four types of care activities (or not a care activity): (1) household activities (eg, meal preparation, laundry, indoor/outdoor cleaning, home repairs, shopping) done with or for the care recipient; (2) physical or medical care provided to the care recipient (eg, help with dressing, bathing, feeding, grooming, or mobility, looking after, providing, or obtaining medical care); (3) socializing or visiting with the care recipient; or (4) transporting or waiting for the care recipient. We then summed time spent in each of the four types of care activities. Follow‐up details necessary to classify secondary activities (eg, who the activity was done with or for) were not collected; however, secondary activities were rare—only about 5% of main activities had a secondary activity—so this omission is unlikely to bias findings appreciably.
Other control variables included descriptors of the caregiver, care recipient, and care arrangement that may be potential confounders in the relationship between being a caregiver to an older adult with dementia and emotional health. (1) Caregiver characteristics included age (measured continuously), gender (male vs female), education (bachelor's degree or higher vs less than a bachelor's degree), and race (white, non‐Hispanic vs other). We also examined two measures of competing time demands: whether the caregiver has living children and whether the caregiver reported working for pay in the last week. (2) Care recipient characteristics included dementia (previously described), age (measured continuously), and level of need (assistance with self‐care or mobility activities or with only household activities). (3) Care arrangement characteristics. We combined information on caregiver relationship and co‐residence, which were highly correlated, to form four categories: spouse or partner, co‐resident parent, non‐resident parent, and all other relationships. We also included the number of years the caregiver had been providing care and whether the caregiver was the only person providing care. To measure relationship quality with the care recipient, we summed four items from the main NSOC interview, each reported on a scale from 1 (a lot) to 4 (not at all), so that a higher value meant a higher‐quality relationship (range 4 to 16; Cronbach's alpha = 0.67): how much the caregiver enjoyed being with the care recipient, how much the recipient argued with them (reversed), how much they felt appreciated by the recipient, and how often the recipient got on their nerves (reversed). Finally, we controlled for whether the diary day was a weekend or a weekday and whether the diary day was reported to be typical.
2.3. Statistical approach
We first examined differences in emotional health outcomes and in other caregiver, recipient, and care arrangement characteristics by whether the care recipient had dementia. We tested for differences using t‐tests for differences in means and χ2 for differences in proportions.
To assess whether care time on the prior day differed, we graphed for each group the percentage of caregivers participating in care at each 15‐minute time interval overall and by type of activity. If more than one type of care activity fell in a given interval, we assigned the interval to the type of activity with the most minutes in the given interval. We tested for differences by whether the recipient had dementia using the non‐parametric two‐sample Kolmogorov‐Smirnov test for equality. 27 To summarize differences, we calculated for each group the mean care minutes overall and by activity among those assisting on the prior day.
Next we estimated ordinary least‐square regression models predicting the composite of negative emotional health as well as each component (frustration, worry, sadness, and stress). To facilitate interpretation, we rescaled care time so each unit equaled 15 minutes. For each outcome, we estimated an unadjusted model with only dementia and care time activities and an adjusted model also controlling for caregiver, recipient, and care situation characteristics. In the final models, we also included an interaction between the indicator of whether the care recipient had dementia and care time activities to test whether care time had a more negative effect on emotional health for caregivers assisting recipients with dementia. Tables present coefficients, standard errors, and statistical tests for dementia, care time and interactions between the two (see Appendix for full models).
All analyses were weighted using diary‐level weights, and standard errors were adjusted to account for NSOC's complex sample design. When weighted, the sample represents the average daily experience of family caregivers who assisted an older adult with limitations in the prior month.
3. RESULTS
As shown in Table 1, frustration, worry, sadness, and stress were all higher for caregivers who assisted older adults with dementia relative to other caregivers on the prior day. The composite of negative emotional health was also significantly higher (worse) when the recipient had dementia (4.2 vs 3.3; P < .05).
TABLE 1.
Weighted percent distribution and means (SDs) of family caregiver's emotional health on the prior day and caregiver, care recipient, and caregiving situation characteristics
| All caregivers | Recipient without dementia | Recipient with dementia | |
|---|---|---|---|
| Caregiver emotional health | |||
| Frustrated (0‐6) | 1.06 (1.28) | 1.00 (1.21) | 1.25 (1.47) * |
| Worried (0‐6) | 0.83 (1.28) | 0.77 (1.22) | 1.01 (1.44) ** |
| Sad (0‐6) | 0.50 (1.01) | 0.47 (0.98) | 0.61 (1.10) * |
| Stressed (0‐6) | 1.11 (1.39) | 1.04 (1.33) | 1.32 (1.54) ** |
| Composite: Negative emotional health (0‐24) | 3.50 (4.22) | 3.27 (3.80) | 4.20 (5.44) ** |
| Caregiver characteristics | |||
| Gender | |||
| Male | 36.8 | 38.0 | 33.0 |
| Female | 63.3 | 62.0 | 67.0 |
| Age | 60.4 (14.9) | 60.4 (14.5) | 60.9 (15.5) |
| Education | |||
| Less than bachelor's degree | 67.8 | 67.5 | 68.6 |
| Bachelor's degree or higher | 32.3 | 32.5 | 31.4 |
| Race | |||
| White, non‐Hispanic | 74.1 | 75.8 | 68.9 |
| Other | 25.9 | 24.2 | 31.1 |
| Any living children | |||
| No | 21.7 | 21.2 | 23.4 |
| Yes | 78.3 | 78.8 | 76.6 |
| Worked for pay last week | |||
| Yes | 39.8 | 38.5 | 43.7 |
| No/Retired | 60.2 | 61.5 | 56.3 |
| Care recipient characteristics | |||
| Age | 80.6 (8.2) | 79.3 (7.5) | 84.5 (8.8) *** |
| Level of need | |||
| Self‐care/mobility activity limitations | 62.5 | 56.4 | 81.5 ˆˆˆ |
| Only household activity limitations | 37.5 | 43.6 | 18.5 |
| Caregiving situation characteristics | |||
| Number years provided care | 6.5 (8.0) | 6.5 (7.6) | 6.6 (9.3) |
| More than one caregiver | |||
| Yes | 76.6 | 74.1 | 84.5 ˆˆˆ |
| No | 23.4 | 25.9 | 15.5 |
| Relationship quality | 13.8 (2.1) | 13.9 (1.9) | 13.5 (2.6) ** |
| Relationship type | |||
| Spouse | 23.2 | 26.1 | 14.4 ˆˆˆ |
| Co‐resident parent | 14.1 | 13.4 | 16.2 |
| Non‐resident parent | 34.1 | 31.4 | 42.6 |
| Other relationship | 28.6 | 29.1 | 26.8 |
| Diary day of week | |||
| Week day | 70.5 | 70.3 | 71.2 |
| Weekend | 29.5 | 29.7 | 28.8 |
| Diary typical day | |||
| No | 32.5 | 32.7 | 31.9 |
| Yes | 67.5 | 67.3 | 68.1 |
| N | 2134 | 1433 | 701 |
* P < .10; ** P < .05; *** P < .01 for t‐tests for differences between caregivers to recipients with and without dementia.
ˆ P < .10; ˆˆ P < .05; ˆˆˆ P < .01 for chi‐square test for differences between caregivers to recipients with and without dementia.
The two groups of caregivers were similar with respect to mean age and distributions of gender, education, race/ethnicity, and whether they had living children and worked for pay. However, caregivers assisting recipients with dementia cared for older recipients on average (mean age 85 vs 79) and were more likely to care for an older adult with self‐care or mobility limitations. They also were less likely to be the only caregiver, less likely to be caring for a spouse, and more likely to be caring for a non‐resident parent.
For caregivers assisting older adults with dementia, time spent providing care yesterday followed a roller‐coaster pattern over the day (black line, bottom panel, Figure 1), with the highest percentages of caring (about 30%) coinciding roughly with mealtimes (12 to 1 pm and 5 to 6 pm). For caregivers assisting other older adults, participation in any care activity increased steadily from 4 am to 10 am when it reached 20% to 25% and declined steadily after 6 pm (black line, top panel; P‐value for difference in black lines across figures P < .05). Two additional distinctions between groups stood out: caregivers caring for older adults with dementia were more likely to provide physical and medical care (P < .01 for difference in red lines) and less likely to provide transportation throughout the day (P < .05 for difference in maize lines).
FIGURE 1.
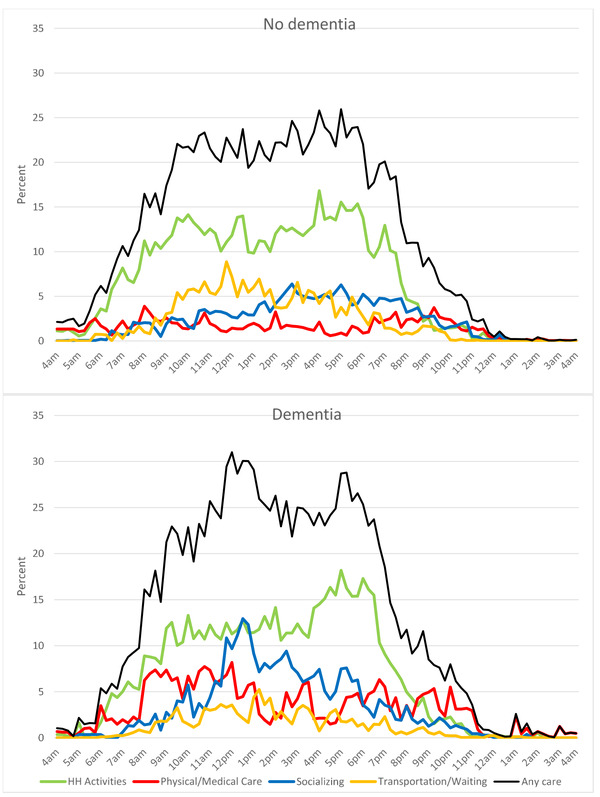
Percentage of family caregivers providing care on the prior day, by time of day, type of activity and whether recipient has dementia. Note: Kolmogorov‐Smirnov tests for differences in percentage providing care over the day between caregivers to recipients with and without dementia are significant for Any Care P < .01, Physical Care P < .01, and Transportation P < .05
Overall, caregivers to older adults with dementia spent on average 163 minutes (2.8 hours) on care days compared to 153 minutes (2.6 hours) for caregivers assisting other older adults (see “Any care” in Table 2). Despite similarities in the overall mean care time, caregivers to older adults with dementia spent twice as much time as other caregivers on physical and medical care (34 vs 16 minutes; P < .01) and half as much time on transportation (13 vs 25 minutes; P < .01).
TABLE 2.
Mean minutes of care over the prior day provided by family caregivers by type of care and whether recipient has dementia
| Total | Recipient without dementia | Recipient with dementia | |
|---|---|---|---|
| Any care | 156.1 | 153 | 167 |
| Household care | 83.3 | 83.9 | 81.0 |
| Physical and medical care | 20.3 | 16.2 | 33.7 ** |
| Socializing with care recipient | 30.5 | 28.0 | 39.1 |
| Transportation | 22.0 | 24.8 | 12.6 ** |
Note: Restricted to caregivers who provided assistance yesterday; N = 1314.
* P < .10, ** P < .05, *** P < .01 for Kolmogorov‐Smirnov test for difference between caregivers to recipients with and without dementia in percentage providing care over the day.
In regression models, both the recipient having dementia and time spent on care activities were related to the caregiver's negative emotional health (Table 3). Focusing on the composite measure, worse negative emotional health persisted for those caring for older adults with dementia after accounting for care time (β = 0.85; P < .05; unadjusted) and when other confounders were also adjusted (β = 0.70; P < .05; adjusted). In addition, time spent on physical and medical care was associated with the composite measure both before (β = 0.16; P < .01) and after (β = 0.14; P < .05) adjusting for potential confounders. Focusing on specific emotions showed that physical and medical care time was associated with greater stress among caregivers to older adults with and without dementia in both unadjusted (β = 0.08; P < .01) and adjusted (β = 0.07; P < .01) models.
TABLE 3.
Regression coefficients (standard errors) predicting family caregivers’ emotional health on the prior day
| Negative emotional health | Frustrated | Worried | Sad | Stressed | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted a | Unadjusted | Adjusted a | Unadjusted | Adjusted a | Unadjusted | Adjusted a | Unadjusted | Adjusted a | |
| Care recipient has dementia | 0.85 ** | 0.70 ** | 0.25 * | 0.20 * | 0.22 * | 0.19 * | 0.13 * | 0.11 | 0.25 * | 0.19 |
| (0.39) | (0.33) | (0.13) | (0.12) | (0.12) | (0.11) | (0.07) | (0.07) | (0.14) | (0.12) | |
| Minutes providing household care b | −0.02 | −0.02 | −0.01 | −0.01 | −0.01 | −0.01 | 0.00 | −0.00 | −0.00 | −0.01 |
| (0.02) | (0.02) | (0.01) | (0.01) | (0.01) | (0.01) | (0.00) | (0.00) | (0.01) | (0.01) | |
| Minutes providing physical and medical care b | 0.16 *** | 0.14 ** | 0.01 | 0.01 | 0.05 ** | 0.04 * | 0.03 * | 0.02 | 0.08 *** | 0.07 *** |
| (0.06) | (0.05) | (0.02) | (0.02) | (0.02) | (0.02) | (0.01) | (0.02) | (0.03) | (0.02) | |
| Minutes socializing with care recipient b | 0.03 | 0.01 | 0.00 | 0.00 | 0.03 | 0.02 | 0.01 | 0.00 | −0.01 | −0.02 |
| (0.05) | (0.04) | (0.02) | (0.01) | (0.02) | (0.02) | (0.01) | (0.01) | (0.02) | (0.01) | |
| Minutes providing transportation b | 0.06 | 0.06 | 0.01 | 0.01 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 |
| (0.07) | (0.07) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | |
| Constant | 3.14 *** | 8.66 *** | 1.01 *** | 2.40 *** | 0.71 *** | 2.43 *** | 0.42 *** | 1.04 *** | 1.00 *** | 2.78 *** |
| (0.19) | (1.22) | (0.06) | (0.40) | (0.06) | (0.40) | (0.05) | (0.30) | (0.06) | (0.44) | |
| R‐squared | 0.01 | 0.12 | 0.01 | 0.10 | 0.02 | 0.09 | 0.01 | 0.06 | 0.03 | 0.14 |
*** P < .01, ** P < .05, * P < .10.
aAdjusted models control for characteristics of caregiver (female, continuous age, college educated, non‐Hispanic white, have living child, worked last week), the care recipient (age, whether receives assistance with self‐care or mobility activities), and the care situation (number of years cared for recipient, whether only caregiver, relationship quality, relationship to care recipient, whether a weekend day, whether a typical day).
bExpressed in 15‐minute units.
N = 2134.
Interactions in Table 4 suggest two notable differences between the groups in the association between care time and negative emotional health. First, for caregivers to older adults without dementia, there was no association between household care and negative emotional health (β = ‐0.00; P > .10), but the coefficient on the interaction term was negative (β = ‐0.09; P < .01), implying a negative effect when the recipient had dementia. Second, for caregivers to older adults without dementia, socializing was associated with less stress (β = ‐0.05; P < 0.01), whereas for caregivers to older adults with dementia socializing was associated with worse negative emotion for the composite outcome (β = 0.28; P < .01) as well as frustration (β = 0.08; P < .05), worry (β = 0.08; P < .05), and stress (β = 0.08; P < .05). Tests of whether socializing effects for caregivers assisting recipients with dementia (sum of main socializing effect and interaction term) differed from zero (not shown) indicated significant associations with composite negative emotional health and worry (β = 0.195 and β = 0.07, respectively, P < .05).
TABLE 4.
Regression coefficients (standard errors) predicting family caregivers’ emotional health on the prior day: adjusted models with interaction between whether recipient has dementia and care activities a
| Negative emotional health | Frustrated | Worried | Sad | Stressed | |
|---|---|---|---|---|---|
| Care recipient has dementia | 0.62 * | 0.19 | 0.14 | 0.07 | 0.21 * |
| (0.35) | (0.13) | (0.11) | (0.08) | (0.12) | |
| Minutes providing household care b | −0.00 | −0.00 | 0.00 | −0.00 | 0.00 |
| (0.02) | (0.01) | (0.01) | (0.00) | (0.01) | |
| Minutes providing physical and medical care b | 0.15 *** | 0.02 | 0.03 | 0.01 | 0.09 ** |
| (0.06) | (0.03) | (0.03) | (0.02) | (0.04) | |
| Minutes socializing with care recipient b | −0.09 * | −0.03 * | −0.01 | −0.01 | −0.05 *** |
| (0.05) | (0.01) | (0.02) | (0.01) | (0.01) | |
| Minutes providing transportation b | 0.05 | −0.00 | 0.02 | 0.02 | 0.01 |
| (0.08) | (0.02) | (0.02) | (0.02) | (0.02) | |
| Minutes providing household care b × care recipient has dementia | −0.09 *** | −0.03 *** | −0.02 ** | −0.01 | −0.03 ** |
| (0.03) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Minutes providing physical and medical care b × care recipient has dementia | 0.01 | −0.00 | 0.02 | 0.03 | −0.04 |
| (0.11) | (0.04) | (0.04) | (0.03) | (0.05) | |
| Minutes socializing with care recipient b × care recipient has dementia | 0.28 *** | 0.08 ** | 0.08 ** | 0.04 * | 0.08 ** |
| (0.11) | (0.04) | (0.04) | (0.02) | (0.03) | |
| Minutes providing transportation b × care recipient has dementia | −0.11 | −0.00 | −0.03 | −0.04 | −0.03 |
| (0.16) | (0.04) | (0.05) | (0.04) | (0.06) | |
| Constant | 8.80 *** | 2.44 *** | 2.48 *** | 1.07 *** | 2.81 *** |
| (1.21) | (0.39) | (0.40) | (0.30) | (0.44) | |
| R‐squared | 0.13 | 0.11 | 0.10 | 0.07 | 0.15 |
*** P < .01, ** P < .05, * P < .10.
aAll models control for characteristics of caregiver (female, continuous age, college educated, non‐Hispanic white, have living child, worked last week,), the care recipient (age, whether receives assistance with self‐care or mobility activities), and the care situation (number of years cared for recipient, whether only caregiver, relationship quality, relationship to care recipient, whether a weekend day, whether a typical day).
bExpressed in 15‐minute units.
N = 2134.
4. DISCUSSION
4.1. Findings and interpretation
We used time diary data from a national sample of family caregivers to examine a day in the life of caregivers assisting older adults with and without dementia and to contrast their care time and emotional health. We found that both groups of caregivers provided similar amounts of care on the prior day. Our estimates of total time, 2.8 versus 2.6 hours for recipients with and without dementia, align well with estimates from ATUS (ie, 2.8 hours). 28 Accumulating these small daily differences over time and in some cases across multiple caregivers, also yields more substantial differences, which is consistent with estimates more commonly reported from the older adults’ perspective. 1 , 29
Consistent with the voluminous literature on caregiver well‐being, we found that emotional health experienced on the prior day was worse for those caring for older adults with dementia. We also uncovered two care‐related reasons for these gaps. First, caregivers assisting those with dementia provided more physical and medical care than other caregivers, and provision of physical and medical care was associated with negative emotional health—especially reports of stress—for both groups. This finding is in line with studies of longer timeframes, which have found that caregivers assisting those with dementia were more likely than caregivers assisting other older adults to participate in physical and medical care activities in the last month. 11 It also echoes recent literature, which highlights greater emotional, physical, and financial difficulty reported by caregivers providing substantial assistance with health care relative to other caregivers. 30 Second, although time spent socializing with the care recipient was similar for both groups of caregivers, this activity was associated with worse emotional health, overall, and with greater worry in particular, among caregivers assisting older adults with dementia. The challenges of interacting socially with a family member or friend living with dementia have received less attention in the caregiving literature and in discussions of caregiver training. How to better equip caregivers to emotionally manage social aspects of care may be a fruitful area for future research.
4.2. Limitations
This study has several limitations. First, although time diaries provide highly granular measures of care, in this study we were limited to one diary per caregiver administered for a random day of the week. Furthermore, about one‐third of caregivers completed the time diary on an atypical day. Thus even though this national sample of caregiver time diaries represents the average experiences of caregivers to older adults with and without dementia on a random day, our ability to speculate about routine patterns is limited. Second, we focused on caregiving to older adults living with probable dementia and thus cannot draw conclusions about the substantial number of care partners that assist and provide support to older adults living with mild cognitive impairment. Third, this analysis treated non‐care as a monolithic set of activities. Incorporating additional information about non‐care activities, including leisure and work, is an important next step. Fourth, although the emotions we included provide important insights into the emotional health of caregivers, they do not supplant clinically relevant measures of psychological well‐being (anxiety, depressive symptoms), which were beyond the scope of this analysis. Finally, our findings did not take into account potential differences in the physical abilities of caregivers; how caregivers’ own health and functioning affects care time and emotional well‐being may be a fruitful area for future research.
4.3. Implications for research and practice
This study has implications for future research aimed at strengthening the evidence base for improving the emotional health of caregivers who are assisting those living with dementia. 31 Researchers previously have pointed to the negative consequences of inadequate training for family caregivers called upon to provide physical and medical care. 32 Our analysis raises the question as to whether training efforts could be better targeted at inhibiting the negative emotional consequences associated with providing physical and medical assistance and, uniquely in the context of dementia, with social interaction with the care recipient. Promising research has documented associations between caregivers’ use of adult day services for recipients with dementia and the stability of their negative emotions, 33 but additional time diary studies are needed to investigate the responsiveness of emotional health to training and other intervention efforts.
Our findings also have implications for efforts to systematically assess caregiver needs with standardized assessment tools administered in health care settings. Caregiver assessments are designed to identify the challenges and strengths of family caregivers to maintain the caregiver's ability to provide care and produce better care recipient outcomes. 34 To date, caregiver assessment tools have emphasized appraised burden, which identifies caregivers who are most at risk for adverse outcomes. Because time diaries can be used to characterize the highly individualized daily rhythms of caregiving, both in terms of care time and emotions, they may be a useful supplemental tool for pinpointing care activities that diminish the emotional health of those caring for older adults with dementia.
5. CONCLUSION
Using national time diary data, we identified two reasons that caregivers to older adults with dementia experience worse emotional health than other caregivers: they provide more physical and medical assistance, which is more emotionally challenging than other activities, and stronger negative emotions appear to be associated during social time in the context of dementia. Given that care‐time measures appear useful for identifying care activities that diminish emotional health, we suggest that diary‐based measures may be a useful supplement to caregiver assessments and call for additional diary‐based research on the responsiveness of caregiver's emotional health to training and other intervention efforts. If successful, such efforts might benefit not only family caregivers but also the individuals with dementia whom they assist.
CONFLICTS OF INTEREST
The National institute on Aging provided funding for this work through grants to the University of Michigan. Vicki Freedman and Sarah Patterson received funding from other grants from the National Institute on Aging made to the University of Michigan. Vicki Freedman received consulting fees from the American Enterprise Institute/Brookings and support for attending meetings and/or travel from American Enterprise Institute/Brookings and the National Academies of Science, Medicine and Engineering. Vicki Freedman also has served on advisory boards for research centers at Johns Hopkins University and the University of Michigan. Sarah Patterson received support for attending meetings and/or travel from the University of Michigan and served as an editorial board member for the Journals of Gerontology: Series B, Social Sciences. Jennifer Cornman had contracts with the University of Michigan and Georgetown University and provided consulting services to the University of Michigan. Jennifer Wolf received funding from grants from the National Institute on Aging, the Commonwealth Fund, and the John A. Hartford Foundation made to Johns Hopkins University, consulting fees from Yale University and the Mayo Clinic, and served on advisory boards for National Academy for State Health Policy (NASHP) and Rush.
ACKNOWLEDGEMENTS
The views expressed are those of the authors alone and do not represent those of their employers or the funding agency. This work was supported by the National Institute on Aging of the National Institutes of Health (R01AG054004; T32AG000221). The sponsors had no role in the design of this analysis or interpretation of the data, writing of the report, or decision to submit the report for publication.
1.
Freedman VA, Patterson SA, Cornman JC, Wolff JL. A day in the life of caregivers to older adults with and without dementia: Comparisons of care time and emotional health. Alzheimer's Dement. 2022;18:1650‐1661. https://doi.org/10.1002/alz.12550
TABLE A1 Regression coefficients (standard errors) predicting family caregivers’ emotional health on the prior day
| Negative emotional health | Frustrated | Worried | Sad | Stressed | |
|---|---|---|---|---|---|
| Recipient has dementia | 0.70** | 0.20* | 0.19* | 0.11 | 0.19 |
| (0.33) | (0.12) | (0.11) | (0.07) | (0.12) | |
| Minutes providing household carea | −0.02 | −0.01 | −0.01 | −0.00 | −0.01 |
| (0.02) | (0.01) | (0.01) | (0.00) | (0.01) | |
| Minutes providing physical and medical carea | 0.14** | 0.01 | 0.04* | 0.02 | 0.07*** |
| (0.05) | (0.02) | (0.02) | (0.02) | (0.02) | |
| Minutes socializing with care recipienta | 0.01 | 0.00 | 0.02 | 0.00 | −0.02 |
| (0.04) | (0.01) | (0.02) | (0.01) | (0.01) | |
| Minutes providing transportationa | 0.06 | 0.01 | 0.02 | 0.02 | 0.02 |
| (0.07) | (0.02) | (0.02) | (0.02) | (0.02) | |
| Caregiver characteristics | |||||
| Female | −0.10 | −0.09 | −0.08 | 0.04 | 0.03 |
| (0.27) | (0.09) | (0.10) | (0.06) | (0.09) | |
| Age | 0.02 | 0.01 | 0.00 | 0.01** | 0.00 |
| (0.01) | (0.00) | (0.00) | (0.00) | (0.00) | |
| Bachelor's degree or higher | 0.56* | 0.09 | 0.14 | 0.07 | 0.26** |
| (0.30) | (0.10) | (0.10) | (0.07) | (0.11) | |
| White, non‐Hispanic (vs Other) | 0.75*** | 0.29*** | 0.12 | 0.09 | 0.25*** |
| (0.26) | (0.08) | (0.09) | (0.06) | (0.09) | |
| Any living children | −0.29 | −0.22 | −0.09 | 0.07 | −0.06 |
| (0.44) | (0.16) | (0.15) | (0.08) | (0.16) | |
| Worked last week | −0.11 | 0.17* | −0.18* | −0.09 | 0.00 |
| (0.30) | (0.10) | (0.10) | (0.07) | (0.11) | |
| Care recipient characteristics | |||||
| Age | −0.01 | −0.00 | −0.01 | 0.00 | −0.00 |
| (0.02) | (0.01) | (0.01) | (0.00) | (0.01) | |
| Needs help with self‐care/mobility | 0.03 | −0.03 | 0.01 | 0.02 | 0.02 |
| (0.29) | (0.10) | (0.10) | (0.07) | (0.10) | |
| Caregiving situation characteristics | |||||
| Number years caring | −0.02 | −0.01* | −0.00 | 0.00 | −0.01 |
| (0.01) | (0.00) | (0.00) | (0.00) | (0.01) | |
| One caregiver | 0.22 | −0.04 | −0.05 | 0.15 | 0.15 |
| (0.44) | (0.15) | (0.15) | (0.10) | (0.16) | |
| Relationship quality | −0.44*** | −0.11*** | −0.11*** | −0.07*** | −0.15*** |
| (0.07) | (0.02) | (0.02) | (0.02) | (0.02) | |
| Relationship to care recipient (vs Spouse) | |||||
| Co‐resident parent | 1.09* | 0.10 | 0.25 | 0.29** | 0.45** |
| (0.56) | (0.16) | (0.18) | (0.13) | (0.20) | |
| Non‐resident parent | 0.86 | 0.16 | 0.25 | 0.11 | 0.34* |
| (0.53) | (0.17) | (0.18) | (0.12) | (0.19) | |
| Other | 0.06 | −0.07 | −0.03 | 0.12 | 0.04 |
| (0.48) | (0.15) | (0.14) | (0.13) | (0.16) | |
| Weekend day (vs weekday) | −1.05*** | −0.32*** | −0.30*** | −0.10* | −0.33*** |
| (0.27) | (0.09) | (0.09) | (0.06) | (0.09) | |
| Yesterday was typical day | −0.56* | −0.19** | −0.15 | −0.09 | −0.13 |
| (0.29) | (0.10) | (0.10) | (0.07) | (0.10) | |
| Constant | 8.66*** | 2.40*** | 2.43*** | 1.04*** | 2.78*** |
| (1.22) | (0.40) | (0.40) | (0.30) | (0.44) | |
| R‐squared | 0.12 | 0.10 | 0.09 | 0.06 | 0.14 |
Expressed in 15‐minute units *** P < .01, ** P < .05, * P < .10.
Freedman VA, Patterson SE, Cornman JC, Wolff JL. A day in the life of caregivers to older adults with and without dementia: Comparisons of care time and emotional health. Alzheimer's Dement. 2022;18:1650–1661. 10.1002/alz.12550
REFERENCES
- 1. Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010‐2050) estimated using the 2010 census. Neurology. 2013:80:1778‐1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rocca WA, Petersen RC, Knopman DS, et al. Trends in the incidence and prevalence of Alzheimer's disease, dementia, and cognitive impairment in the United States. Alzheimers Dement. 2011:7:80‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kasper JD, Freedman VA, Spillman BC, Wolff JL. The disproportionate impact of dementia on family and unpaid caregiving to older adults. Health Aff (Millwood). 2015:34:1642‐1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schulz R, Eden J (Eds). Families Caring for an Aging America. Washington DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 5. Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta‐analysis. Psychol Aging. 2003:18:250‐267. [DOI] [PubMed] [Google Scholar]
- 6. Pinquart M, Sörensen S. Associations of caregiver stressors and uplifts with subjective well‐being and depressive mood: a meta‐analytic comparison. Aging Ment Health. 2004:8:438‐449. [DOI] [PubMed] [Google Scholar]
- 7. Sallim AB, Sayampanathan AA, Cuttilan A, Chun‐Man HR. Prevalence of mental health disorders among caregivers of patients with Alzheimer disease. J Am Med Dir Assoc. 2015:16:1034‐1041. [DOI] [PubMed] [Google Scholar]
- 8. Zarit SH, Orr NK, Zarit JM. The Hidden Victims of Alzheimer's Disease: Families Under Stress . New York: New York University Press; 1985. [Google Scholar]
- 9. Zarit SH, Reever KE, Bach‐Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980:20:649‐655. [DOI] [PubMed] [Google Scholar]
- 10. Bédard M, Pedlar D, Martin NJ, Malott O, Stones MJ. Burden in caregivers of cognitively impaired older adults living in the community: methodological issues and determinants. Int Psychogeriatr. 2000:12:307‐332. [DOI] [PubMed] [Google Scholar]
- 11. Riffin C, Van Ness PH, Wolff JL, Fried T. Family and other unpaid caregivers and older adults with and without dementia and disability. J Am Geriatr Soc. 2017:65:1821‐1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Riffin C, Van Ness PH, Wolff JL, Fried T. Multifactorial examination of caregiver burden in a national sample of family and unpaid caregivers. J Am Geriatr Soc. 2019:67:277‐283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. National Research Council , Subjective Well‐Being: Measuring Happiness, Suffering, and Other Dimensions of Experience. Washington DC: National Academies of Sciences Press; 2013. [PubMed] [Google Scholar]
- 14. He W, Weingartner RM, Sayer LC. Subjective well‐being of eldercare providers 2012‐2013. Current Population Reports P23‐215. Washington, DC: US Census Bureau; 2018. [Google Scholar]
- 15. Hammersmith AM, Lin IF. Evaluative and experienced well‐being of caregivers of parents and caregivers of children. J Gerontol B Psychol Sci Soc Sci. 2019:74:339‐352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wong JD, Shobo Y. Types of family caregiving and daily experiences in midlife and late adulthood: the moderating influences of marital status and age. Res Aging. 2017:39:719‐740. [DOI] [PubMed] [Google Scholar]
- 17. Bangerter LRY, Liu KK, Zarit SH, Birditt KS, Fingerman KL. Everyday support to aging parents: links to middle‐aged children's diurnal cortisol and daily mood. Gerontologist. 2018:58:654‐662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Freedman VA, Cornman JC, Carr D, Lucas RE. Time use and experienced wellbeing of older caregivers: a sequence analysis. Gerontologist. 2019:59:441‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Freedman VA, Kasper JD. Cohort profile: the National Health and Aging Trends Study. Int J Epidemiol. 2019:48:1044‐1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Freedman VA, Cornman JC. National Study of Caregiving III Time Diary User Guide. Baltimore: Johns Hopkins Bloomberg School of Public Health; 2019. [Google Scholar]
- 21. Lucas R, Freedman VA, Carr C. Measuring experiential well‐being among older adults. J Posit Psychol. 2019:14:538‐547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kahneman D, Krueger AB, Schkade D, Schwarz N, Stone AA. A survey method for characterizing daily life experience: The Day Reconstruction Method (DRM). Science. 2004:306:1776‐1780. [DOI] [PubMed] [Google Scholar]
- 23. Galvin JE, Roe CM, Powlishta KK, et al. The AD8: a brief informant interview to detect dementia. Neurology. 2005:65:559‐564. [DOI] [PubMed] [Google Scholar]
- 24. Galvin JE, Roe CM, Xiong C, Morris JC. Validity and reliability of the AD8 informant interview in dementia. Neurology. 2006:67:1942‐1948. [DOI] [PubMed] [Google Scholar]
- 25. Langa KM, Plassman BL, Wallace RB, et al. The aging, demographics, and memory study: study design and methods. Neuroepidemiology. 2005:25:181‐91. [DOI] [PubMed] [Google Scholar]
- 26. Kasper JD, Freedman VA, Spillman B. Classification of Persons by Dementia Status in the National Health and Aging Trends Study. Baltimore: Johns Hopkins University School of Public Health; 2013. Technical Paper #5. [Google Scholar]
- 27. Conover WJ. Practical Nonparametric Statistics, 3rd ed. New York: Wiley; 1999. [Google Scholar]
- 28. US Bureau of Labor Statistics . Time Spent Providing Eldercare and Percent of Eldercare Providers Engaging in Caregiving, by Sex and Caregiving Activity, Averages for the Combined Years 2015‐16 (Table 5). Bureau of Labor Statistics; 2017. [Google Scholar]
- 29. Reckrey JM, Bollens‐Lund E, Husain M, Ornstein KA, Kelley AS. Family caregiving for those with and without dementia in the last 10 years of life. JAMA Intern Med. 2021:181:278‐279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wolff JL, Spillman BC, Freedman VA, Kasper JD. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med. 2016:176:372‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Larson E, Stroud C. Meeting the Challenge of Caring for Persons Living with Dementia and Their Care Partners and Caregivers: A Way Forward, Eds. Washington, DC: The National Academies Press; 2021. [PubMed] [Google Scholar]
- 32. Burgdorf JG, Arbaje AI, Stuart EA, Wolff JL. Unmet family caregiver training needs associated with acute care utilization during home health care. J Am Geriatr Soc. 2021;69(7):1887‐1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Liu Y, Kim K, Almeida DM, Zarit SH. Daily fluctuation in negative affect for family caregivers of individuals with dementia. Health Psychol. 2014:34:729‐740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Feinberg L, Houser A. Assessing Family Caregiver Needs: Policy and Practice Considerations AARP Public Policy Institute Fact Sheet 258. AARP; 2012. [Google Scholar]


