Abstract
Objective
This study aims to investigate sex, age, and cause-specific contributions to changes and trend disparities in life expectancy (LE) and health-adjusted life expectancy (HALE) attributed to disability and mortality from 1990 to 2019 in China, which provides insight into policy-making, health systems planning, and resource allocation.
Methods
Contributions of disability and mortality to changes and trend disparities in LE and HALE were estimated with standard abridged life table, Sullivan's method, and decomposition method, using retrospective demographic analysis based on mortality and years lived with disability (YLD) rates extracted from Global Burden of Disease Study 2019 (GBD 2019).
Results
From 1990 to 2019, LE and HALE increased by 10.49 and 8.71 years for both sexes, mainly due to noncommunicable diseases (NCDs) (5.83 years, 55.58% for LE and 6.28 years, 72.10% for HALE). However, HIV/AIDS and sexually transmitted infections had negative effects on changes in LE (−0.03 years, −0.29%) and HALE (−0.05 years, −0.57%). Lung cancer and ischemic heart disease caused the biggest reduction in LE (−0.14 years, −1.33%) and HALE (−0.42 years, −4.82%). Also, cardiovascular diseases (−0.08 years, −0.92%), neurological disorders (−0.08 years, −0.92%), diabetes and kidney diseases (−0.06 years, −0.69%), and transport injuries (−0.06 years, −0.69%) had main negative disability effects in HALE. Moreover, life expectancy lived with disability (LED) increased by 1.78 years, mainly attributed to respiratory infections and tuberculosis (1.04 years, 58.43%) and maternal and neonatal disorders (0.78 years, 43.82%).
Conclusion
The LE and HALE in China have grown rapidly over the past few decades, mainly attributed to NCDs. It is necessary to further reduce the negative mortality effect of HIV/AIDS, lung cancer, colon and rectum cancer, pancreatic cancer, and ischemic heart disease and the negative disability effect of stroke, diabetes mellitus, and road injuries. In addition, the signs of disparities in mortality and disability of different sexes and ages call for targeted and precise interventions for key groups such as males and the elderly. According to the decomposition results, we may better determine the key objects of health policies that take into account substantial cause-specific variations to facilitate the realization of “healthy China 2030” plan.
Keywords: life expectancy, health-adjusted life expectancy, disability effect, mortality effect, decomposition
Introduction
Life expectancy (LE) is one of the most commonly used population health summary indicators, which is based on a set of observed age-specific mortalities (1). Unlike LE, health-adjusted life expectancy (HALE) is more comprehensive and captures both the length and the quality of life (2, 3). LE and HALE are important indicators of socioeconomic and medical development, which had increased steadily in the past several years in China due to improvements in living conditions, education, and healthcare practices (4, 5). However, HALE has grown at a slower rate than LE, resulting in longer LE for patients with disabilities (LED) (6, 7).
Due to population aging and urbanization, the leading causes of death in China have undergone an epidemiological transition from communicable, maternal, neonatal, and nutritional diseases (CMNNs) to noncommunicable diseases (NCDs) (8, 9). China is rapidly catching up with this epidemic, like most developed countries (10). Despite China's progress in improving health, NCDs were still responsible for 1.65 million (88%) of China's total deaths in 2019, including leading contributors to mortality and disability such as cardiovascular diseases (0.88 million, 46%) and cancer (0.45 million, 24%) (11). In addition, far less is known about cause-specific trends in mortality and disability, and detailed information on sex, age, and cause-specific LE obtained in LE and HALE is not yet well characterized. The question of whether some population groups or causes remain disadvantaged and left behind as LE and HALE grow should be focused on.
While cause-eliminated life tables are often used to evaluate the impact of different causes on LE and HALE (12, 13), this approach only focuses on the cross-sectional study and is unable to access the impact on changes. Thus, we used a decomposition method, which was more comparative and allowed assigned contributions of mortality and disability variation to specific age groups or causes of death (14). Additionally, the advantages of using data from the Global Burden of Disease (GBD) study, which involved comprehensive data sources and methods, were obvious.
The Chinese government has attached great importance to population health. The Healthy China 2030 plan was implemented as a national health policy in 2016 (15). Two of the goals are to improve LE and HALE. At present, a comprehensive and comparable assessment of cause-specific effects on LE and HALE and how they change over time is not available. Understanding changes and trend disparities in LE and HALE at the national level is crucial to tracking progress toward the goals and promoting population wellbeing. Thus, this study aimed to investigate sex, age, and cause-specific contributions to changes and trend disparities in LE and HALE attributed to disability and mortality in China from 1990 to 2019, thereby providing insights into policy-making, health systems planning, and resource allocation.
Materials and Methods
Data Sources
All the data for the period 1990–2019 in China, as tabulated in different causes, sexes, and age groups (<1 year, 1–4 years, 5–9 years, ..., 95+ years), were retrieved from the Global Burden of Disease Study 2019 (GBD 2019) (10), including mortality and years lived with disability (YLD) rates. The main data sources are the China Disease Surveillance Points (DSP) system, Maternal and Child Surveillance System, Cause of Death Reporting System of Chinese Center for Disease Control and Prevention (CDC), and Cancer Registry data. The methods for data collecting, processing, and analyzing are briefly described below, and the details can be found in the GBD 2019 (16, 17). A crucial step in data processing is correcting for known bias by redistributing deaths from unspecified codes to more specific disease categories, and by adjusting data with alternative case definitions or measurement methods to the reference method. Another important aspect is that cause-specific estimates are modeled using standardized tools such as the Cause of Death Ensemble model (CODEm), spatiotemporal Gaussian process regression (ST-GPR), and DisMod-MR to generate estimates of each quantity of interest by age, sex, location, and year.
Causes of death are organized in a hierarchical list containing 3 levels. At the highest level (Level 1), all causes are divided into three mutually exclusive and collectively exhaustive categories, namely, CMNNs, NCDs, and injuries. Level 2 contains 22 cause groups, such as cardiovascular diseases, neoplasms, and transport injuries. Level 3 disaggregates these causes further, including 168 more specific causes. The corresponding International Classification of Diseases (ICD9 and ICD10) codes are detailed in Supplementary Table S1.
Statistical Analysis
The LE at birth was computed with a standard abridged life table (18), using mortality in the infant age group (<1 year) and 19 non-infant age groups starting with age 1–4 years, then proceeding in 5-year age groups (5–9 years, 10–14 years, …) until the terminal age group of 95+ years. Next, the probability of dying, the number of individuals alive, and the number of person-years lived in each age group were computed. HALE refers to the number of years that a person can expect to live in good health, taking into account both mortality and disability, which were computed with Sullivan's method based on the standard abridged life table (19). YLD rates were used to represent the disability prevalence.
where n is the last age group in the life table; lx is the number of individuals alive at age x; Lx is the number of person-years lived in age group; YLDx is all-cause disability prevalence in age group.
Contributions to the changes in LE were estimated with Arriaga's decomposition method (20, 21), while contributions to the changes in HALE were estimated with an extended method based on Arriaga (22). LE and HALE changes in the period of 1990–2019 and 10-year intervals (1990–1999, 2000–2009, and 2010–2019) were both decomposed. All the analyses were carried out with R version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria). Detailed procedures and formulas are described below.
Step 1: To decompose LE by age group. The total contribution of an age group to the LE gap (in years) is the sum of two mathematical terms. The first term represents the direct effect of age group, which consists of the years an age group contributes to LE changes. The second term represents indirect and interaction effect. For example, higher mortality in the 30–34 years age group may leave fewer survivors at the age of 35 years.
Step 2: To decompose HALE by age group. The total contribution of an age group to the HALE gap (in years) is also the sum of two mathematical terms. The first term represents the mortality effect of age group (ME), which is the changes in HALE caused by the changes in person-years lived in age group. The second term represents the disability effect (DE), which is the changes in HALE caused by the changes in YLD rates in age group.
Step 3: To decompose LE by cause-specific death within an age group. The total contribution of a given age group to the LE gap (in years) is further partitioned into the years contributed by each cause. The total contribution of each cause to the LE gap is obtained by summing cause-specific contributions across all age groups.
Step 4: To decompose HALE by cause-specific death within an age group. The mortality and disability effect of a given age group to the HALE gap (in years) is further partitioned into the years contributed by each cause based on the specific percentage of gap of mortality or YLD rates in the total change. The total contribution of each cause to the HALE gap is also obtained by summing cause-specific mortality and disability effect across all age groups.
where TEx is the total contribution between ages x and x+n, lx is the number of individuals alive at age x, l0is the cohort size at the start, Lx is the number of person-years lived between ages x and x+n, and Tx+n is the total number of person-years lived above age x+n. lx+n is the number of individuals alive at age x+n. is the disability prevalence at age x. is the total contribution between ages x and x+n due to cause i, is the specific mortality rate between ages x and x+n due to cause i. is the all-cause mortality rate between ages x and x+n. is the specific disability prevalence between ages x and x+n due to cause i. is the all-cause YLD rate between ages x and x+n. “A” and “B” represent different years.
Results
Changes in LE and HALE
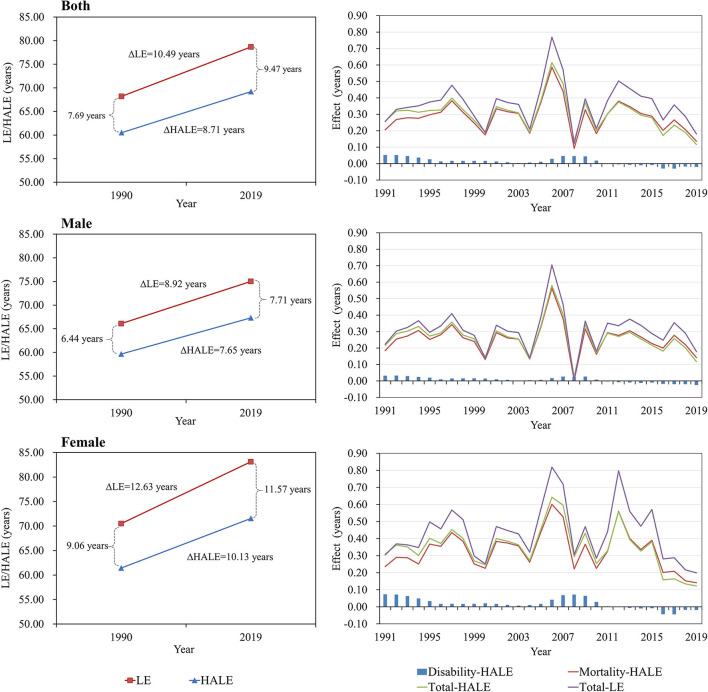
From 1990 to 2019, LE increased by 10.49 years for both sexes, while HALE increased by 8.71 years as a result of reduced mortality (8.30 years, 95.29%) and disability (0.41 years, 4.71%). LED was the difference between LE and HALE, with an average increase of 1.78 years for both sexes (Table 1). The total effect on the change in LE and HALE was greater for females than for males with higher LEDs. LE and HALE showed an increasing trend every year, varying significantly from year to year, with the overall effect being positive (Figure 1). For changes in HALE, the disability effects of all causes were at a low level, with both males and females showing a negative effect after 2011. In addition, from 1990 to 1999, LE and HALE increased by 3.20 and 2.85 years for males and females. Starting in 2000, LE and HALE further increased by 3.65 and 3.16 years for both sexes. However, the growth rate has decreased since 2010, resulting in 3.24 and 2.30 years for both sexes, respectively, until 2019, especially in terms of the total effect of HALE changes. From 2010 to 2019, a negative effect of disability was observed. Thus, LED increased from 0.35 to 0.94 years for both sexes in the past three decades, and females also had a higher total effect of changes in LE and HALE than males with a higher LED in each decade (Table 2).
Table 1.
Effects of mortality and disability on changes in life expectancy (LE) and health-adjusted life expectancy (HALE) (years) from 1990 to 2019.
| Population | ΔLE | ΔHALE | ΔLED | ||
|---|---|---|---|---|---|
| TE | ME | DE | TE | ||
| Both sexes | 10.49 | 8.30 | 0.41 | 8.71 | 1.78 |
| Males | 8.92 | 7.42 | 0.23 | 7.65 | 1.27 |
| Females | 12.63 | 9.53 | 0.60 | 10.13 | 2.51 |
TE, total effect; ME, mortality effect; DE, disability effect.
Figure 1.
Trends and effects of mortality and disability on changes in life expectancy (LE) and health-adjusted life expectancy (HALE) across year to year.
Table 2.
Effects of mortality and disability on changes in life expectancy (LE) and health-adjusted life expectancy (HALE) (years) for 10-year interval.
| Intervals | Population | ΔLE | ΔHALE | ΔLED | ||
|---|---|---|---|---|---|---|
| TE | ME | DE | TE | |||
| 1990–1999 | Both sexes | 3.20 | 2.57 | 0.28 | 2.85 | 0.35 |
| Males | 2.84 | 2.39 | 0.20 | 2.59 | 0.25 | |
| Females | 3.72 | 2.85 | 0.37 | 3.22 | 0.50 | |
| 2000–2009 | Both sexes | 3.65 | 2.96 | 0.20 | 3.16 | 0.49 |
| Males | 3.00 | 2.53 | 0.12 | 2.65 | 0.35 | |
| Females | 4.56 | 3.54 | 0.30 | 3.84 | 0.72 | |
| 2010–2019 | Both sexes | 3.24 | 2.43 | −0.13 | 2.30 | 0.94 |
| Males | 2.76 | 2.21 | −0.12 | 2.09 | 0.67 | |
| Females | 3.83 | 2.71 | −0.14 | 2.57 | 1.26 | |
TE, total effect; ME, mortality effect; DE, disability effect.
Mortality and Disability Effect on Changes in LE and HALE
From 1990 to 2019, better control of NCDs contributed most to changes in LE (5.83 years, 55.58%) and HALE (6.28 years, 72.10%) for both sexes, followed by control of CMNNs (3.46 years, 32.98% for LE and 1.32 years, 15.15% for HALE) and injuries (1.20 years, 11.44% for LE and 1.11 years, 12.74% for HALE) (Table 3). For level 2 causes of CMNNs, respiratory infections and tuberculosis contributed most to the changes in LE (1.86 years, 17.73%) and HALE (0.82 years, 9.41%). Only HIV/AIDS and sexually transmitted infections had negative total effects both on changes in LE (−0.03 years, −0.29%) and HALE (−0.05 years, −0.57%) because of the negative effect of mortality. HALE also decreased by 0.09 years (1.03%) owing to a reduction in the disability of maternal and neonatal disorders. For level 2 causes of NCDs, chronic respiratory diseases contributed most to the changes in LE (2.02 years, 19.26%) and HALE (2.83 years, 32.49%), followed by cardiovascular diseases (1.77 years, 16.87% for LE and 1.82 years, 20.90% for HALE). Moreover, 5 causes had negative disability effects on changes in HALE such as cardiovascular diseases (−0.08 years, −0.92%), neurological disorders (−0.08 years, −0.92%), and diabetes and kidney diseases (−0.06 years, −0.69%). For level 2 causes of injuries, unintentional injuries contributed the most to changes in LE (0.57 years, 5.43%), and self-harm injuries and interpersonal violence contributed most to the changes in HALE (0.59 years, 6.77%). Among them, transport injuries (−0.06 years, −0.69%) and unintentional injuries (−0.01 years, −0.11%) had negative disability effects on changes in HALE.
Table 3.
Cause-specific effects on changes in life expectancy (LE) and health-adjusted life expectancy (HALE) from 1990 to 2019 (years, levels 1–2).
| Causes | Level | ΔHALE | ΔLE | ΔLED | ||
|---|---|---|---|---|---|---|
| ME | TE | TE | TE | |||
| Communicable, maternal, neonatal, and nutritional diseases | A | 1.09 | 0.23 | 1.32 | 3.46 | 2.14 |
| HIV/AIDS and sexually transmitted infections | A.1 | −0.05 | <0.01 | −0.05 | −0.03 | 0.02 |
| Respiratory infections and tuberculosis | A.2 | 0.78 | 0.04 | 0.82 | 1.86 | 1.04 |
| Enteric infections | A.3 | 0.07 | <0.01 | 0.07 | 0.29 | 0.21 |
| Neglected tropical diseases and malaria | A.4 | 0.01 | 0.10 | 0.11 | 0.01 | −0.10 |
| Other infectious diseases | A.5 | 0.17 | 0.02 | 0.19 | 0.45 | 0.26 |
| Maternal and neonatal disorders | A.6 | 0.07 | −0.09 | −0.02 | 0.76 | 0.78 |
| Nutritional deficiencies | A.7 | 0.03 | 0.16 | 0.20 | 0.11 | −0.08 |
| Non-communicable diseases | B | 6.05 | 0.23 | 6.28 | 5.83 | −0.45 |
| Neoplasms | B.1 | 0.71 | −0.04 | 0.66 | 0.83 | 0.17 |
| Cardiovascular diseases | B.2 | 1.84 | −0.08 | 1.77 | 1.82 | 0.06 |
| Chronic respiratory diseases | B.3 | 2.72 | 0.11 | 2.83 | 2.02 | −0.81 |
| Digestive diseases | B.4 | 0.50 | 0.05 | 0.54 | 0.49 | −0.06 |
| Neurological disorders | B.5 | 0.05 | −0.08 | −0.03 | 0.05 | 0.08 |
| Mental disorders | B.6 | <0.01 | 0.04 | 0.04 | <0.01 | −0.04 |
| Substance use disorders | B.7 | 0.06 | 0.01 | 0.07 | 0.04 | −0.02 |
| Diabetes and kidney diseases | B.8 | 0.08 | −0.06 | 0.02 | 0.09 | 0.07 |
| Skin and subcutaneous diseases | B.9 | 0.01 | −0.01 | <0.01 | 0.01 | 0.01 |
| Sense organ diseases | B.10 | <0.01 | 0.05 | 0.05 | <0.01 | −0.05 |
| Musculoskeletal disorders | B.11 | <0.01 | 0.11 | 0.10 | <0.01 | −0.11 |
| Other non-communicable diseases | B.12 | 0.08 | 0.14 | 0.22 | 0.48 | 0.26 |
| Injuries | C | 1.16 | −0.05 | 1.11 | 1.20 | 0.09 |
| Transport injuries | C.1 | 0.21 | −0.06 | 0.15 | 0.21 | 0.05 |
| Unintentional injuries | C.2 | 0.37 | −0.01 | 0.36 | 0.57 | 0.21 |
| Self-harm and interpersonal violence | C.3 | 0.58 | 0.01 | 0.59 | 0.42 | −0.17 |
TE, total effect; ME, mortality effect; DE, disability effect.
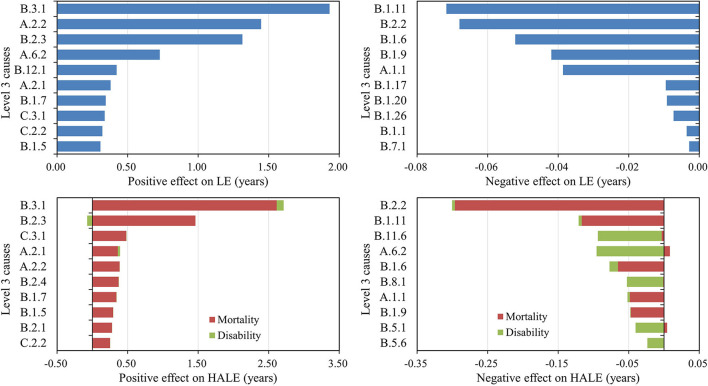
Figure 2 shows the top 10 level 3 causes that positively/negatively influenced the changes in LE and HALE. Chronic obstructive pulmonary disease contributed the most to changes in LE (1.93 years, 18.40%) and HALE (2.71 years, 31.11%). More than 70% of improvement in both LE and HALE was attributed to better control of these top 10 level 3 causes, and 7 of them were shown simultaneously in both lists, including chronic obstructive pulmonary disease, stroke, lower respiratory infections, tuberculosis, stomach cancer, liver cancer, and drowning. But it is worth noting that stroke (−0.07 years, −0.80%) had a negative disability effect on changes in HALE. Lung cancer and ischemic heart disease caused the biggest reduction in LE (−0.14 years, −1.33%) and HALE (−0.42 years, −4.82%). More than 10% of the decline in HALE was attributed to poorer control of these top 10 level 3 causes with a negative effect. More details are summarized in Supplementary Table S2.
Figure 2.
Leading causes with positive/negative effects on changes in life expectancy (LE) and health-adjusted life expectancy (HALE) from 1990 to 2019 (level 3).
In the past three decades, the most prominent causes of the increases in LE between 1990 and 1999 were NCDs (1.59 years, 49.66%) and CMNNs (1.29 years, 40.32%), including cardiovascular diseases (0.63 years, 19.86%), chronic respiratory diseases (0.55 years, 17.27%), and respiratory infections and tuberculosis (0.76 years, 23.92%). The most prominent cause of the increases in HALE was also NCDs (1.58 years, 55.35%), followed by CMNNs (0.89 years, 31.24%). Subsequently, the positive total effects of NCDs on changes in LE increased, reaching 2.25 years between 2010 and 2019, mainly attributed to a reduction in mortality of neoplasms (0.37 years, 11.47%) and cardiovascular diseases (0.95 years, 29.27%). However, the positive total effects of NCDs on changes in HALE decreased since 2010 to 1.93 years, mainly attributed to an increase in disability rate of neoplasms (0.26 years, 11.20%), chronic respiratory diseases (0.63 years, 27.48%), and digestive diseases (0.10 years, 4.51%). For CMNNs, the positive total effects both on changes in LE and HALE decreased to a low level (0.49 years, 15.02%) from 2010 to 2019, which was mainly due to HIV/AIDS and sexually transmitted infections (−0.02 years, −0.62%) and maternal and neonatal disorders (−0.03 years, −0.93%) with negative effects. For injuries (0.50 years, 15.50%), which mainly attributed to transport injuries (−0.04 years, −1.24%) and unintentional injuries (−0.11 years, −3.40%) with negative disability effects. More details are summarized in Supplementary Tables S3–S5.
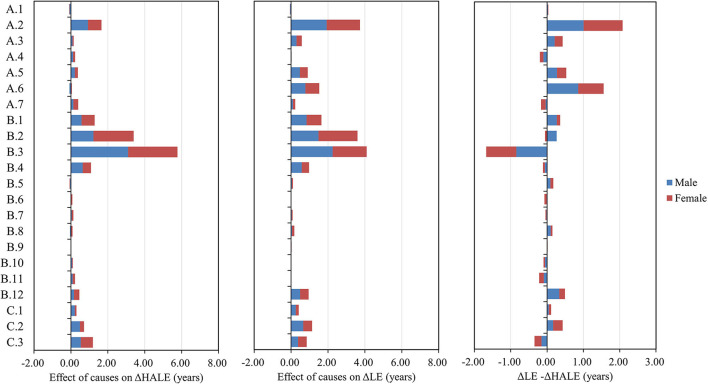
Sex and Age-Specific Effect on Changes in LE and HALE
From 1990 to 2019, better control of NCDs contributed most to the changes in LE (4.50 years, 50.45% for males; 7.68 years, 60.81% for females) and HALE (5.24 years, 68.50% for males; 7.65 years, 75.52% for females). Figure 3 shows level 2 causes with total effect on changes in LE and HALE. For males, more than 60% (5.89 years) of improvement in LE was attributed to better control of the following 5 diseases: respiratory infections and tuberculosis (1.71 years), chronic respiratory diseases (1.49 years), cardiovascular diseases (1.19 years), neoplasms (0.76 years), and maternal and neonatal disorders (0.74 years). More than 70% (5.79 years) of improvement in HALE was attributed to better control of the following 5 diseases: chronic respiratory diseases (2.53 years), cardiovascular diseases (1.21 years), respiratory infections and tuberculosis (0.83 years), neoplasms (0.62 years), and digestive diseases (0.60 years). Similarly, for females, more than 70% (9.24 years) was due to cardiovascular diseases (2.77 years), chronic respiratory diseases (2.68 years), respiratory infections and tuberculosis (2.04 years), neoplasms (0.96 years), and maternal and neonatal disorders (0.79 years). More than 75% (7.97 years) of improvement in HALE was attributed to better control of the following 5 diseases: chronic respiratory diseases (3.31 years), cardiovascular diseases (2.41 years), respiratory infections and tuberculosis (0.85 years), neoplasms (0.74 years), and self-harm and interpersonal violence (0.66 years). More details are summarized in Supplementary Table S6.
Figure 3.
Cause-specific effects on changes in life expectancy (LE) and health-adjusted life expectancy (HALE) (levels 1–2) for males and females from 1990 to 2019.
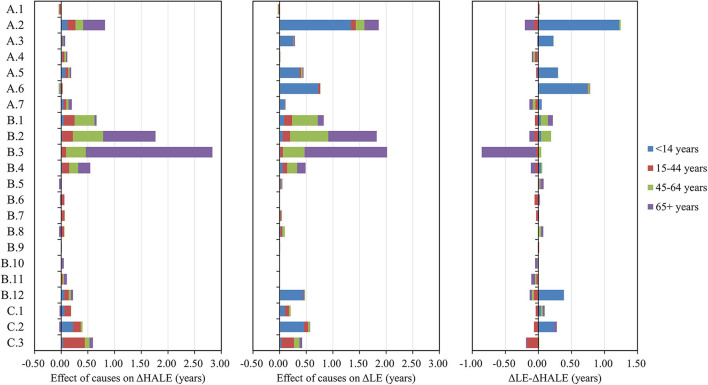
From 1990 to 2019, better control of NCDs in elderly aged more than 65 years old contributed most to the changes in HALE (3.68 years, 42.25%) (Figure 4). Better control of CMNNs in children aged under 14 years old had the greatest impact on LE (2.80 years, 26.69%). For injuries, more attention should be paid to older adults over 65 years of age, which had a smaller effect on changes in LE and a negative effect on changes in HALE. For children under 14 years old, LE improvements of more than 20% (2.53 years) were attributed to better control of the following 3 diseases: respiratory infections and tuberculosis (1.34 years), maternal and neonatal disorders (0.73 years), and unintentional injuries (0.46 years). But the total effect on improvement in HALE was very small (0.74 years, 8.50%). For youth aged 15–44 years, 10.10% (1.06 years) of improvement in LE and 21.47% (1.87 years) of improvement in HALE were attributed to all causes. For adults aged 45–64 years, the top level 2 cause with a positive effect on changes in LE and HALE was cardiovascular diseases (0.72 years, 6.86% and 0.57 years, 6.54%). Among older adults aged 65 years or older, the top 3 level 2 causes with a positive effect on changes in LE and HALE were chronic respiratory diseases (1.55 years, 14.78% and 2.37 years, 27.21%), cardiovascular diseases (0.91 years, 8.67% and 0.98 years, 11.25%), and respiratory infections and tuberculosis (0.27 years, 2.57% and 0.41 years, 4.71%). More details are summarized in Supplementary Table S7.
Figure 4.
Cause-specific effects on changes in life expectancy (LE) and health-adjusted life expectancy (HALE) (levels 1–2) for different age groups from 1990 to 2019.
Changes in LED
The LED, which refers to the difference between LE and HALE, increased by 1.78 years, mainly attributed to respiratory infections and tuberculosis (1.04 years, 58.43%) and maternal and neonatal disorders (0.78 years, 43.82%). The slow reduction in disability resulted in a longer LED. Additionally, LED increased by 1.27 years for males, through respiratory infections and tuberculosis (0.88 years, 69.29%) and maternal and neonatal disorders (0.82 years, 64.57%). LED increased by 2.51 years for females due to respiratory infections and tuberculosis (1.19 years, 47.41%) and maternal and neonatal disorders (0.76 years, 30.28%). Compared with the other level 2 causes and age groups, respiratory infections and tuberculosis (1.23 years, 69.10%) and maternal and neonatal disorders (0.74 years, 41.57%) in children aged <14 years contributed the most to increased LED, while chronic respiratory diseases in elderly aged more than 65 years old showed a negative effect (−0.82 years, −46.07%) on LED. For level 3 causes and both sexes, lower respiratory infections (1.06 years, 59.55%) and neonatal disorders (0.82 years, 46.07%,) contributed the most to increased LED. More details are summarized in Supplementary Tables S2, S6, S7.
Discussion
This study was based on the largest epidemiological dataset to date in the 30-year history of GBD 2019 and continued to provide representative, comprehensive, and updated national estimates of the burden of diseases and injuries by integrating all available data. LE is a population health indicator of overall population health, and HALE is a more comprehensive indicator that incorporates mortality and disability into a single statistic (23). Arriaga's decomposition method was used to investigate sex-, age-, and cause-specific contributions in changes in LE and HALE across time in China, which is ideal for determining whether seemingly positive disparities are associated with large differences in cause-specific mortality or disability.
With improvement in the national economy and healthcare system, LE and HALE in China increased by 10.49 years and 8.71 years from 1990 to 2019, largely due to better control of NCDs (5.83 years, 55.58% for LE and 6.28 years, 72.10% for HALE) and, to a lesser extent, CMNNs (3.46 years, 32.98% for LE and 1.32 years, 15.15% for HALE) and injuries (1.20 years, 11.44% for LE and 1.11 years, 12.74% for HALE). According to the global research (24), NCDs were the main positive factor for HALE changes in high-income countries, while low-income countries experienced the most improvement from CMNNs. The results in China were more similar to those for high-income countries. Moreover, for level 3 causes, the top 10 positive factors leading to changes in LE were chronic obstructive pulmonary disease, lower respiratory infections, stroke, neonatal disorders, congenital birth defects, tuberculosis, liver cancer, self-harm, drowning, and stomach cancer; the top 10 positive factors leading to changes in HALE were chronic obstructive pulmonary disease, stroke, self-harm, tuberculosis, lower respiratory infections, hypertensive heart disease, liver cancer, stomach cancer, rheumatic heart disease, and drowning. According to previous studies (25–28), mortality from the above causes has decreased globally in the last decades, as it has in China, although they may have different effects on LE and HALE.
However, negative mortality and disability effects persist, especially in the period of 2010 to 2019. Both HIV/AIDS and sexually transmitted infections had negative mortality effects on changes in LE and HALE. According to GBD 2019, HIV/AIDS has become the leading cause of death in infectious diseases in China since 2009, with increasing mortality (29), as in other western countries (17). Theoretically, with the advent of antiretroviral treatment, the mortality rate would decrease significantly. However, those patients who did not meet the treatment criteria or had poor compliance may have higher mortality rates (30). For NCDs, level 3 causes of lung cancer, colon and rectum cancer, pancreatic cancer, and ischemic heart disease caused the main reduction in LE and HALE due to increased mortality, as has been proved in previous studies (31–35). For lung cancer, more emphasis should be placed on early screening, and tobacco control, and improving air pollution by reducing industrial energy consumption and dust (36, 37). For colon and rectum cancer, screening also has been shown to reduce their incidence and mortality, and in the longer term, primary prevention should be promoted (38). For pancreatic cancer, a timely and accurate diagnosis can improve the current poor prognosis of this disease (39). Improved dietary quality is associated with a reduced risk of pancreatic cancer (40). For ischemic heart disease, interventions should be expanded to control risk factors such as hypertension, hyperlipidemia, diabetes, and smoking, and eating more fresh fruit helps reduce the incidence of ischemic heart disease (41, 42). In addition, cardiovascular diseases (stroke), neonatal and neurological disorders, diabetes mellitus, and transport injuries (road injuries) had negative disability effects on changes in HALE as a result of increased disability rates. Consistent with previous studies (43–46), main causes such as stroke, diabetes mellitus, and road injuries are associated with an increased risk of disability. How well these diseases are rehabilitated is very important and more effective measures should be developed to decline the mortality of specific diseases, along with disability rates.
In addition, LEDs have increased in both sexes over the past three decades, which was mainly attributed to CMNNs, including lower respiratory infections and neonatal disorders. This is because the rate of mortality reduction has been much faster than the rate of disability reduction. The slow reduction in disability resulted in a longer LED. For most diseases and injuries, the mortality effect was dominant in influencing changes in HALE. It is noteworthy that the decline in mortality contributes more than 95% to the change of HALE in China, while disability reduction contributed <5%. HALE could not catch up with the growth rate of LE, which increased the additional personal, family, and social costs of medical services and long-term care for the elderly.
For different populations, more than 38% of improvement in LE was attributable to children under 14 years due to decreased mortality (47, 48). As the population ages, those over 65 years of age are coming to dominate the changes in LE and HALE. China is encountering formidable healthcare challenges brought about by the problem of aging (49, 50). Major diseases that need more attention in the elderly include cancer, cardiovascular diseases, diabetes, and injuries such as falls (13, 51). The increases in LE and HALE for females were higher than for males. More than 50% of improvement in LE and HALE for males and females was attributed to better control of the following 4 diseases: cardiovascular diseases, chronic respiratory diseases, respiratory infections and tuberculosis, and neoplasms. Similar to other studies worldwide (24), Chinese women had higher LED than men, along with higher incremental LED.
The rapid rise in NCDs driven by urbanization, income growth, and aging, as well as the transition to chronic disability, has brought major challenges to China's health system. Changes in cause-specific mortality and disability will require an integrated government response to improve primary healthcare and take necessary action to address key risks, especially for those diseases that are increasing with negative effects such as lung cancer, colon and rectum cancer, pancreatic cancer, stroke, ischemic heart disease, diabetes mellitus, and road injury. Analyses of changes and trend disparities in LE and HALE attributed to disability and mortality provide a useful framework to guide evidence-based policy responses to the changing disease spectrum in China, including timely adjustments to health programs and interventions. In the future, more studies should be implemented to investigate the drivers of heterogeneity observed in the changes and trend disparities in China, which may help guide more cost-effective and precise policies in China and other developing countries.
Nevertheless, there are several limitations in this study. First, the quality of mortality and disability data varied across years, which may affect the accuracy of the estimated changes in LE and HALE. We may overlook the cause-specific contributions between smaller time intervals. In the future, cause-specific contributions between each year will be explored. Second, data comparability over time should be considered. Different surveillance scope and completeness, diagnostic technology, and healthcare accessibility of diseases may affect the data quality. Third, this study shared the same limitations as the GBD 2019 study in the process of collecting and analyzing data on mortality and disability in China. Finally, this study only included levels 1–3 causes. Different diseases may have an opposite effect even in the same cause. More comprehensive studies will be required.
Conclusion
The LE and HALE in China have grown rapidly over the past few decades, mainly attributed to NCDs. It is necessary to further reduce the negative mortality effect of HIV/AIDS, lung cancer, colon and rectum cancer, pancreatic cancer, and ischemic heart disease and the negative disability effect of stroke, diabetes mellitus, and road injuries. In addition, the signs of disparities in mortality and disability of different sexes and ages call for targeted and precise interventions for key groups such as males and the elderly. According to the decomposition results, we may better determine the key objects of health policies that take into account substantial cause-specific variations to facilitate the realization of “healthy China 2030” plan.
As a next step, to further improve LE and HALE, the construction of national demonstration areas for comprehensive prevention and control of NCDs should be expanded, including the national healthy lifestyle action and the project for early diagnosis and treatment of cancer. At the same time, we should not neglect to strengthen the prevention and control of HIV/AIDS and anti-virus treatment, as well as the rehabilitation after various diseases and injuries.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: http://ghdx.healthdata.org/gbd-results-tool.
Author Contributions
HC: conceptualization, visualization, and writing review and editing. LC: literature research, statistical analysis, and writing original draft preparation. YQ: methodology, data interpretation, and curation. LW: supervision and validation. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Medical Key Discipline Program of Wuxi Health Commission (ZDXK010), Wuxi Tai Lake Talent Program, High-end Talent, Wuxi Eminent Medical Talents (ZDRC004), Wuxi Youth Medical Talents (QNRC050), Jiangsu Province Six-one Project for High-level Health Talents Research Fund (LGY2018014), Wuxi Precision Medicine Project (J202006), Top Talent Support Program for young and middle-aged people of Wuxi Health Committee (BJ2020096), and Youth Foundation of Wuxi Health Commission (Q202164).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.925114/full#supplementary-material
References
- 1.Luy M, Di Giulio P, Di Lego V, Lazarevič P, Sauerberg M. Life expectancy: frequently used, but hardly understood. Gerontology. (2020) 66:95–104. 10.1159/000500955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sullivan DF. A single index of mortality and morbidity. HSMHA Health Rep. (1971) 86:347–54. 10.2307/4594169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robine JM, Ritchie K. Healthy life expectancy: evaluation of global indicator of change in population health. BMJ. (1991) 302:457–60. 10.1136/bmj.302.6774.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen H, Hao L, Yang C, Yan B, Sun Q, Sun L, et al. Understanding the rapid increase in life expectancy in shanghai, China: a population-based retrospective analysis. BMC Public Health. (2018) 18:256. 10.1186/s12889-018-5112-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luo W, Xie Y. Economic growth, income inequality and life expectancy in China. Soc Sci Med. (2020) 256:113046. 10.1016/j.socscimed.2020.113046 [DOI] [PubMed] [Google Scholar]
- 6.Meyer AC, Drefahl S, Ahlbom A, Lambe M, Modig K. Trends in life expectancy: did the gap between the healthy and the ill widen or close? BMC Med. (2020) 18:41. 10.1186/s12916-020-01514-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cao X, Hou Y, Zhang X, Xu C, Jia P, Sun X, et al. A comparative, correlate analysis and projection of global and regional life expectancy, healthy life expectancy, and their GAP: 1995-2025. J Glob Health. (2020) 10:020407. 10.7189/jogh.10.020407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. (2013) 381:1987–2015. 10.1016/S0140-6736(13)61097-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li X, Song J, Lin T, Dixon J, Zhang G, Ye H. Urbanization and health in China, thinking at the national, local and individual levels. Environ Health. (2016) 15 (Suppl 1):32. 10.1186/s12940-016-0104-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME) (2020). Available online at: http://ghdx.healthdata.org/gbd-results-tool (accessed June, 2021).
- 11.National Center for Chronic and Non-communicable Disease Control and Prevention Chinese Center for Disease Control and Prevention Statistical Statistical Information Center of the National Health Commission . China death surveillance data set 2019. Beijing: China Science and Technology Press. (2020). [Google Scholar]
- 12.Aburto JM, Wensink M, van Raalte A, Lindahl-Jacobsen R. Potential gains in life expectancy by reducing inequality of lifespans in Denmark: an international comparison and cause-of-death analysis. BMC Public Health. (2018) 18:831. 10.1186/s12889-018-5730-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu X, Sun X, Li Y, Gu Y, Huang M, Wei J, et al. Potential gains in health-adjusted life expectancy from reducing four main non-communicable diseases among Chinese elderly. BMC Geriatr. (2019) 19:16. 10.1186/s12877-019-1032-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beltran-Sanchez H, Preston S H, Canudas-Romo V. An integrated approach to cause-of-death analysis: Cause-deleted life tables and decompositions of life expectancy. Demogr Res. (2008) 19:1323–50. 10.4054/DemRes.2008.19.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan X, Zhang Y, Shao H. Healthy China 2030, a breakthrough for improving health. Glob Health Promot. (2019) 26:96–9. 10.1177/1757975917743533 [DOI] [PubMed] [Google Scholar]
- 16.GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1160–203. 10.1016/S0140-6736(20)30977-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiang CL. A stochastic study of the life table and its applications. II Sample variance of the observed expectation of life and other biometric functions. Hum Biol. (1960) 32:221–38. [PubMed] [Google Scholar]
- 19.Imai K, Soneji S. On the Estimation of Disability-Free Life Expectancy: Sullivan' Method and Its Extension. J Am Stat Assoc. (2007) 102:1199–211. 10.1198/016214507000000040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arriaga EE. Measuring and explaining the change in life expectancies. Demography. (1984) 21:83–96. 10.2307/2061029 [DOI] [PubMed] [Google Scholar]
- 21.Auger N, Feuillet P, Martel S, Lo E, Barry AD, Harper S. Mortality inequality in populations with equal life expectancy: Arriaga's decomposition method in SAS, Stata, and Excel. Ann Epidemiol. (2014) 24:575–80. e1. 10.1016/j.annepidem.2014.05.006 [DOI] [PubMed] [Google Scholar]
- 22.Nusselder WJ, Looman CWN. Decomposition of differences in health expectancy by cause. Demography. (2004) 41:315–34. 10.1353/dem.2004.0017 [DOI] [PubMed] [Google Scholar]
- 23.Ruan X, Li Y, Jin X, Deng P, Xu J, Li N, et al. Health-adjusted life expectancy (HALE) in Chongqing, China, 2017: an artificial intelligence and big data method estimating the burden of disease at city level. Lancet Reg Health West Pac. (2021) 9:100110. 10.1016/j.lanwpc.2021.100110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen H, Chen G, Zheng X, Guo Y. Contribution of specific diseases and injuries to changes in health adjusted life expectancy in 187 countries from 1990 to 2013: retrospective observational study. BMJ. (2019) 364:1969. 10.1136/bmj.l969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.GBD Chronic Respiratory Disease Collaborators . Prevalence and attributable health burden of chronic respiratory diseases, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med. (2020) 8:585–96. 10.1016/S2213-2600(20)30105-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. (2021) 20:795–820. 10.1016/S1474-4422(21)00252-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Disease Cancer Collaboration G . Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. (2019) 5:1749–68. 10.1001/jamaoncol.2019.2996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.James SL, Castle CD, Dingels ZV, Fox JT, Hamilton EB, Liu Z, et al. Global injury morbidity and mortality from 1990 to 2017: results from the Global Burden of Disease Study 2017. Inj Prev. (2020) 26(Supp 1):i96–i114. 10.1136/injuryprev-2019-043494corr1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao D, Zou Z, Dong B, Zhang W, Chen T, Cui W, et al. Secular trends in HIV/AIDS mortality in China from 1990 to 2016: Gender disparities. PLoS ONE. (2019) 14:e0219689. 10.1371/journal.pone.0219689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang F, Dou Z, Ma Y, Zhang Y, Zhao Y, Zhao D, et al. Effect of earlier initiation of antiretroviral treatment and increased treatment coverage on HIV-related mortality in China: a national observational cohort study. Lancet Infect Dis. (2011) 11:516–24. 10.1016/S1473-3099(11)70097-4 [DOI] [PubMed] [Google Scholar]
- 31.Cao M, Chen W. Epidemiology of lung cancer in China. Thorac Cancer. (2019) 10:3–7. 10.1111/1759-7714.12916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Araghi M, Soerjomataram I, Jenkins M, Brierley J, Morris E, Bray F, et al. Global trends in colorectal cancer mortality: projections to the year 2035. Int J Cancer. (2019) 144:2992–3000. 10.1002/ijc.32055 [DOI] [PubMed] [Google Scholar]
- 33.Zhao C, Gao F, Li Q, Liu Q, Lin X. The distributional characteristic and growing trend of pancreatic cancer in China. Pancreas. (2019) 48:309–14. 10.1097/MPA.0000000000001222 [DOI] [PubMed] [Google Scholar]
- 34.Wang C, Wang C, Liu M, Chen Z, Liu S. Temporal and spatial trends of ischemic heart disease burden in Chinese and subgroup populations from 1990 to 2016: socio-economical data from the 2016 global burden of disease study. BMC Cardiovasc Disord. (2020) 20:243. 10.1186/s12872-020-01530-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Downing NS, Li J. Ischaemic heart disease in China: the time to address rising mortality rates. Eur Heart J Qual Care Clin Outcomes. (2017) 3:4–5. 10.1093/ehjqcco/qcw049 [DOI] [PubMed] [Google Scholar]
- 36.Gao S, Li N, Wang S, Zhang F, Wei W, Li N, et al. Lung Cancer in People's Republic of China. J Thorac Oncol. (2020) 15:1567–76. 10.1016/j.jtho.2020.04.028 [DOI] [PubMed] [Google Scholar]
- 37.Hong QY, Wu GM, Qian GS, Hu CP, Zhou JY, Chen LA, et al. Prevention and management of lung cancer in China. Cancer. (2015) 121 Suppl 17:3080–8. 10.1002/cncr.29584 [DOI] [PubMed] [Google Scholar]
- 38.Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet. (2014) 383:1490–502. 10.1016/S0140-6736(13)61649-9 [DOI] [PubMed] [Google Scholar]
- 39.Zhang L, Sanagapalli S, Stoita A. Challenges in diagnosis of pancreatic cancer. World J Gastroenterol. (2018) 24:2047–60. 10.3748/wjg.v24.i19.2047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zheng J, Guinter MA, Merchant AT, Wirth MD, Zhang J, Stolzenberg-Solomon RZ, et al. Dietary patterns and risk of pancreatic cancer: a systematic review. Nutr Rev. (2017) 75:883–908. 10.1093/nutrit/nux038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang ZQ, Zhang L, Zheng H, Guo WB, Gao Y, Zhao YF, et al. Burden and trend of ischemic heart disease and colorectal cancer attributable to a diet low in fiber in China, 1990-2017: findings from the Global Burden of Disease Study 2017. Eur J Nutr. (2021) 60:3819–27. 10.1007/s00394-021-02556-6 [DOI] [PubMed] [Google Scholar]
- 42.Du H, Li L, Bennett D, Guo Y, Key TJ, Bian Z, et al. Fresh fruit consumption and major cardiovascular disease in China. N Engl J Med. (2016) 374:1332–43. 10.1056/NEJMoa1501451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Han Y, Hu K, Wu Y, Fang Y. Future life expectancy with disability among elderly Chinese individuals: a forecast based on trends in stroke and dementia. Public Health. (2021) 198:62–8. 10.1016/j.puhe.2021.06.013 [DOI] [PubMed] [Google Scholar]
- 44.Tabesh M, Shaw JE, Zimmet PZ, Söderberg S, Koye DN, Kowlessur S, et al. Association between type 2 diabetes mellitus and disability: what is the contribution of diabetes risk factors and diabetes complications? J Diabetes. (2018) 10:744–52. 10.1111/1753-0407.12659 [DOI] [PubMed] [Google Scholar]
- 45.Weijermars W, Bos N, Filtness A, Brown L, Bauer R, Dupont E, et al. Burden of injury of serious road injuries in six EU countries. Accid Anal Prev. (2018) 111:184–92. 10.1016/j.aap.2017.11.040 [DOI] [PubMed] [Google Scholar]
- 46.Jiang B, Liang S, Peng ZR, Cong H, Levy M, Cheng Q, et al. Transport and public health in China: the road to a healthy future. Lancet. (2017) 390:1781–91. 10.1016/S0140-6736(17)31958-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu XH, Dong H, Li L, Liu WH, Lin GZ, Ou CQ. Trends and seasonality in cause-specific mortality among children under 15 years in Guangzhou, China, 2008-2018. BMC Public Health. (2020) 20:1117. 10.1186/s12889-020-09189-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McAllister DA, Liu L, Shi T, Chu Y, Reed C, Burrows J, et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Health. (2019) 7:e47–57. 10.1016/S2214-109X(18)30408-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang W, Wu B, Tan SY, Li B, Lou VWQ, Chen ZA, et al. Understanding health and social challenges for aging and long-term care in China. Res Aging. (2021) 43:127–35. 10.1177/0164027520938764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. (2015) 24(Pt B):197–205. 10.1016/j.arr.2015.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen H, Wang H, Crimmins EM, Chen G, Huang C, Zheng X. The contributions of diseases to disability burden among the elderly population in China. J Aging Health. (2014) 26:261–82. 10.1177/0898264313514442 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: http://ghdx.healthdata.org/gbd-results-tool.