Abstract
Background/aims
To assess the accuracy of real-time telemedicine to diagnose and manage paediatric eye conditions.
Methods
Design: Prospective, non-inferiority study analysing agreement in diagnoses and management plans between telemedicine and in-person examinations. Setting: Paediatric ophthalmology clinic. Population: Children 0–17 years, English-speaking or Spanish-speaking, able to participate in age-appropriate manner, either previously seen by the optometrist and required ophthalmology referral or newly referred from outside source. Procedures: Paediatric optometrist conducted examinations using digital equipment and streamed live to a paediatric ophthalmologist who recorded diagnoses and management plans, then re-examined patients in-person. Subjects were masked to the fact they would see the ophthalmologist in-person, same-day. Main outcome measures: Discrepancy in management plan or diagnosis between telemedicine and in-person examinations. Non-inferiority threshold was <1.5% for management plan or <15% for diagnosis discrepancies.
Results
210 patients participated in 348 examinations. 131 (62.4%) had strabismus as primary diagnosis. In these patients, excellent and almost perfect agreement was observed for angle measurements (intraclass correlation coefficients=0.98–1.00) and disease categorisation (kappa=0.94–1.00) (p<0.0001 in all cases). No primary diagnoses changed, and no management plans changed following in-person examination. 54/55 patients who consented for surgery at the initial visit did so while masked to receiving an in-person examination. Families felt comfortable with the quality of the telemedicine examination (98.5%) and would participate in another in the future (97.1%).
Conclusion
Paediatric ophthalmic conditions can be reliably diagnosed and managed via telemedicine. Access for underserved populations may be improved by collaboration between ophthalmologists and optometrists using this technology.
Keywords: child health (paediatrics), telemedicine, angle
Introduction
Worldwide, an estimated 19 million children aged 0–14 years are blind or visually impaired from mostly treatable or preventable conditions.1 2 Global prevalence of strabismus and amblyopia in children under 20 is 1.78% and 1.63%, respectively.3 4 The demand for paediatric eye care is immense, and even the wealthiest countries see geographic and socioeconomic disparities in access to care affecting timely diagnosis.5 6 This may result in lifetime visual impairment with economic costs to both the individual and society.
Telemedicine may expand access to specialists, especially for underserved populations, and reduce the burden of disease. In ophthalmology, asynchronous telemedicine, in which images are sent to a remote specialist for interpretation, predominates. In paediatric populations, the use of asynchronous telemedicine for retinopathy of prematurity has been well validated.7–12 Until recently, real-time telemedicine had been less explored in ophthalmology, especially for a strictly paediatric population.13–16
At The Vision Center at Children’s Hospital Los Angeles (CHLA), 70%–80% of our patient population is underserved. We sought to leverage telemedicine in partnership with paediatric optometrists within our practice to provide timely ophthalmic consultations in community-based settings. Previously, we conducted prospective validation studies for each device used in our telemedicine examinations.17–19 In this investigation, we study agreement between telemedicine and in-person examinations for diagnosing and managing paediatric eye conditions.
Materials and methods
Between February 2016 and April 2018, we conducted a prospective, non-inferiority study assessing agreement in diagnosis and management plan between telemedicine and in-person examinations in The Vision Center. A paediatric optometrist within our practice (JC-S) on the patient’s side conducted the telemedicine examination, while a paediatric ophthalmologist (SN) watched in real time and counselled the family on her findings and plan. To determine the accuracy of the telemedicine examination, she subsequently re-examined the patient in-person later the same day. Informed consent was obtained from a parent/legal guardian of all patient subjects. Assent was obtained from children aged ≥7 years, if cognitively able.
Eligibility/study population
Typically one (sometimes two) patient subject(s) and one parent/guardian were enrolled per family. Patient subjects were recruited from one of two sources: either they were newly referred to The Vision Center from an outside source (eg, paediatrician, other specialist or outside optometrist) (‘comprehensive examinations’) or they had been seen by our paediatric optometrist and required referral to a paediatric ophthalmologist for surgical consultation or diagnostic and management questions (‘consultation examinations’). Eligible patients included children <18 years who were able to participate in an age-appropriate manner.
Platform
The telemedicine system consisted of a Polycom RealPresence Group 500 video conferencing system (Polycom, San Jose, California, USA), Pivothead glasses (Pivothead, Denver, Colorado, USA), a Topcon SLD4 digital slit lamp with DC4 camera attachment (Topcon, Tokyo, Japan) and a Keeler Vantage Plus LED Digital Wireless Indirect Ophthalmoscope (Keeler, Windsor, UK). The Pivothead is a wireless, wearable device with a built-in high-definition camera at the nasal bridge and touch controls on the frame, allowing first person point-of-view video capture. Each device connects to a local computer to live-stream videos. To transmit videos to a remote examiner, the desktop was shared through an encrypted Polycom-to-Polycom video call over the hospital’s internal network at 4–6 Mbps. Videos were formatted most often at 720p (range 480–1080) and 29 frames/second for the Pivothead, 964p (range 900–964) and 20 frames/second (range 17–30) for the slit lamp, and always 576p and 25 frames/second for the indirect ophthalmoscope. Videos of the telemedicine system in use are provided in online supplemental material (https://drive.google.com/file/d/1QBCs8i2HH9prxOGXHNGgNWJszGQmJxTZ/view?usp=sharing).
bjophthalmol-2020-318385supp001.pdf (22.8KB, pdf)
Design
During recruitment, subjects were given the choice between a telemedicine (research) or in-person (standard) examination, on the premise that there was a shorter wait for research appointments by an order of months. Subjects were masked to the fact that if they opted for telemedicine, they would also see the ophthalmologist in-person. This was done to gauge willingness to participate in telemedicine examinations as well as trust in management plans (including surgical recommendations) attained via telemedicine.
At the visit, the optometrist obtained history, performed preliminary testing (vision, stereoacuity, intraocular pressure) and conducted the telemedicine examination. At the outset of the call, the optometrist presented the patient, stating her specific question or the reason for referral from the outside provider. The optometrist directed the ophthalmologist to areas of interest, while the latter viewed and guided the examination, from a remote but nearby location, and recorded diagnoses with ICD-10 codes and management plans for each diagnosis. Non-medical diagnoses such as refractive errors were not included. There was opportunity for dialogue between the optometrist and ophthalmologist, but interpretation of the examination findings was left up to the ophthalmologist. Patient counselling and consenting for surgery were conducted via telemedicine. Afterward, the ophthalmologist performed an in-person examination and again recorded diagnoses and management plans.
Examinations were modified depending on whether the patient required a dilated fundus examination. Patients referred by the optometrist for a specific question (consultation examinations) were not dilated unless clinically indicated. In these cases, strabismus measurements were verified in-person immediately following the telemedicine call. New referrals from an outside source underwent a comprehensive examination including sensorimotor, slit lamp if age appropriate and dilated indirect ophthalmoscopy (comprehensive examinations), all via telemedicine. Comprehensive examinations were conducted in two parts: at the completion of the undilated examination, the optometrist ended the call, dilated the patient and performed cycloplegic refraction. When finished, she called the ophthalmologist back for the dilated examination. Strabismus measurements, which cannot be accurately performed post-dilation, were not re-checked in-person following comprehensive telemedicine examinations. All strabismus measurements during consultation and follow-up telemedicine visits, including pre- and post-op examinations, were verified in-person.
The ophthalmologist, optometrist and parent/guardian completed surveys at different time points capturing demographics, patient and provider satisfaction, optometrist’s knowledge gain, technical challenges, duration of examination, whether or not the patient consented to surgery via telemedicine, and duration of patient’s commute and time missed from school and work. Patient satisfaction was captured before subjects were unmasked to seeing the ophthalmologist in-person. This paper primarily focuses on clinical outcomes, while experience and access data will be reported separately.
Outcome measures and data analysis
The primary outcome measure was agreement in diagnoses and management plans between the telemedicine and in-person evaluations. Patients were classified as having no change, change in management plan or change in diagnosis.
The threshold of non-inferiority was set at <1.5% for management plan or <15% for diagnosis discrepancies. In establishing these limits, an acceptable level of imprecision was balanced with the practicality of running this study in a realistic timeframe and with minimal disruption in a clinic already experiencing long waits for care. Although it would be ideal to establish conclusively that telemedicine was equal to in-person examinations, the number of cases required to compute a confidence interval (CI) around an outcome of zero management plan discrepancies grows exponentially as the upper bound approaches zero. For example, the upper limit of the CI would be <1% if 300 cases were evaluated and <0.5% for 600 cases. Given the practical challenges of evaluating 100–300 extra cases, an upper limit of 1.5% was chosen, which exceeds the upper limit of the CI (1.42%) if no discrepancies were found in 210 cases. This result would suggest that no more than 3 individuals out of 210 might result in a management plan discrepancy in 95% of study replications. If the current study identified a single case of management plan discrepancy, it would conclude that telemedicine is inferior, as the CI around the estimate of 1 case ranges from 0.01% to 2.62%. Diagnosis discrepancies were considered less important to the overall course of patient care, so a higher threshold of 15% was chosen, corresponding to 21 observed changes (CI=6.3%–14.9%).
Secondary outcome measures were obtained from clinical evaluations and participant surveys, which encompassed the aforementioned metrics. For patients with strabismus, angle measurements and disease category were compared between telemedicine and in-person evaluations.
For strabismus disease category, agreement was determined by weighted kappa (κ), where adjacent categorisations (eg, exotropia vs intermittent exotropia) were considered near matches, while distant categories were considered fair (eg, exotropia vs exophoria) or poor matches (eg, exotropia vs esotropia; see online supplemental table 1). Interpretation of κ is based on the following scale: 0.0–0.20, no agreement; 0.21–0.39, minimal agreement; 0.40–0.59, weak; 0.60–0.79, moderate; 0.80–0.90, strong; >0.90, almost perfect.20
To quantify agreement of angle measurements, intraclass correlation coefficients (ICCs) were calculated. Because angle measurements were obtained from the same rater under two study conditions (in-person vs telemedicine), two-way mixed models evaluating absolute agreement of single scores were used (ICC(A,1) based on the McGraw and Wong (1996) nomenclature).21 Interpretation of ICC is as follows: <0.50, poor agreement; 0.50–0.75, moderate; 0.75–0.90, good;>0.90, excellent.22
All analyses were conducted using Stata/SE V.14.2 (StataCorp, College Station, Texas, USA). All p values <0.05 were considered statistically significant.
Results
Clinical outcomes
Two hundred ten patients (ages 0–17 years, median age=6 years, 3 sets of 2 siblings) and one parent/guardian per family participated. Table 1 presents patient demographics. Of 210 initial encounters, 94 were comprehensive and 116 were consultation examinations. In total, 348 examinations were conducted. Sixty-six patients had at least one follow-up examination (median=2). Results are reported for initial visit only unless stated otherwise.
Table 1.
Patient demographics
| N (%) | |
| Boys | 93 (44) |
| Girls | 117 (56) |
| Race | |
| American Indian or Alaska Native | 4 (2) |
| Asian | 13 (6) |
| Black or African American | 20 (10) |
| Native Hawaiian or Other Pacific Islander | 0 (0) |
| White | 166 (79) |
| Mixed or other | 7 (3) |
| Ethnicity | |
| Hispanic or Latino | 163 (78) |
| Not Hispanic or Latino | 47 (22) |
| Primary language | |
| English | 94 (45) |
| Spanish | 106 (50) |
| English and Spanish equally | 3 (1) |
| Other | 7 (3) |
| Insurance type | |
| Public (Medicaid) | 201 (96) |
| Private | 9 (4) |
The mean number of diagnoses per patient was 1.75 (range, 0–5). Sixty-two per cent of patients were primarily diagnosed with strabismus (n=131); other common primary diagnoses included eyelid abnormalities (n=12), glaucoma suspect (n=10) and conjunctival disorders (n=9) (table 2). Among primary diagnoses, we saw 135 (64.3%) motility findings, 22 (10.5%) oculoplastic, 21 (10.0%) posterior segment, 17 (8.1%) anterior segment and 15 (7.1%) ‘other’ or systemic disease.
Table 2.
Diagnoses
| Condition name | ICD-10 codes | Primary diagnosis | Non-primary diagnosis | ||
| N | % | N | % | ||
| Strabismus | H50, H49.1, H51.1, H51.8 | 131 | 62.4 | 39 | 18.6 |
| Esotropias | H50.01–H50.08, H50.31–H50.32, H50.4 | 40 | 19.0 | 4 | 1.9 |
| Constant | 37 | 17.6 | 3 | 1.4 | |
| With A or V pattern* | 6 | 2.9 | 0 | ||
| Congenital* | 4 | 1.9 | 0 | ||
| Accommodative and partially accommodative* |
17 | 8.1 | 1 | 0.5 | |
| Intermittent | 2 | 1.0 | 1 | 0.5 | |
| Accommodative | 2 | 1.0 | 0 | ||
| Exotropias | H50.11–H50.18, H50.33–H50.34 | 70 | 33.3 | 10 | 4.8 |
| Constant | 13 | 6.2 | 2 | 1.0 | |
| With A or V pattern | 8 | 3.8 | 0 | ||
| Intermittent | 57 | 27.1 | 8 | 3.8 | |
| With A or V pattern | 11 | 5.2 | 0 | ||
| Vertical strabismus | H50.2 | 3 | 1.4 | 0 | |
| Intermittent heterotropia | H50.30 | 0 | 1 | 0.5 | |
| Heterophoria | H50.5 | 9 | 4.3 | 10 | 4.8 |
| Brown syndrome | H50.6 | 1 | 0.5 | 1 | 0.5 |
| Duane’s syndrome | H50.8 | 2 | 1.0 | 1 | 0.5 |
| Superior oblique palsy | H49.1 | 5 | 2.4 | 0 | |
| Convergence insufficiency | H51.11 | 1 | 0.5 | 8 | 3.8 |
| Dissociated vertical deviation | H51.8 | 0 | 10 | 4.8 | |
| Functional vision loss | F45.8 | 1 | 0.5 | 0 | |
| Eyelid abnormalities and lesions | D22.10, H00.1, H01.0, H02.4, H05.221, Q10.0, Q82.5 | 12 | 5.7 | 18 | 8.6 |
| Conjunctivitis and conjunctival disorders | D31.0, H10, H11 | 9 | 4.3 | 7 | 3.3 |
| Keratitis and corneal abnormalities | D31.1, H16, H17 | 5 | 2.4 | 2 | 1.0 |
| Infantile and juvenile cataract | H26.0 | 1 | 0.5 | 1 | 0.5 |
| CHRPE and other specified retinal disorders | D31.31, H31.002, H35, Q14.1 | 3 | 1.4 | 6 | 2.9 |
| Glaucoma suspect | H40.0, Q14.2, Q15.0 | 10 | 4.8 | 1 | 0.5 |
| Vitreous floaters | H43.391 | 1 | 0.5 | 2 | 1.0 |
| Optic nerve disorders | H47, Q14.2 | 8 | 3.8 | 0 | |
| Optic nerve hypoplasia | H47.03 | 1 | 0.5 | 0 | |
| Optic disc anomaly | H47.09, H47.39 | 3 | 1.4 | 0 | |
| Optic disc cupping | H47.39, Q14.2 | 4 | 1.9 | 0 | |
| Amblyopia | H53.0 | 3 | 1.4 | 20 | 9.5 |
| Nystagmus | H55.0 | 2 | 1.0 | 2 | 1.0 |
| Anisocoria | H57.02 | 0 | 2 | 1.0 | |
| Ocular pain | H57.10 | 0 | 1 | 0.5 | |
| Pseudostrabismus | Q10.3 | 2 | 1.0 | 6 | 2.9 |
| Congenital nasolacrimal duct obstruction | Q10.5 | 8 | 3.8 | 0 | |
| Anterior segment abnormalities/malformations | D31.4, H21.273, Q13 | 2 | 1.0 | 3 | 1.4 |
| Non-ocular conditions† | |||||
| Type 1 diabetes | E10.9 | 3 | 1.4 | 0 | |
| Type 2 diabetes | E11.9 | 1 | 0.5 | 0 | |
| Facial nerve palsy | G51.0 | 2 | 1.0 | 0 | |
| Juvenile idiopathic arthritis | L40.54 | 1 | 0.5 | 0 | |
| Torticollis | M43.6, R29.3 | 2 | 1.0 | 0 | |
| Unspecified cleft palate with unilateral cleft lip | Q37.9 | 1 | 0.5 | 0 | |
| Neurofibromatosis, type 1 | Q85.01 | 1 | 0.5 | 0 | |
| No medical diagnosis | 1 | 0.5 | 0 | ||
*Strabismus conditions are not mutually exclusive.
†These were patients undergoing screening examinations who had no ocular clinical examination findings.
CHRPE, congenital hypertrophy of the retinal pigment epithelium.
No primary diagnoses were changed between the telemedicine and in-person examinations, although two non-primary diagnoses were: a tiny non-visually significant lens opacity and a small intermittent vertical deviation. Both were noted in-person but not seen via telemedicine; neither affected management. No management plans, including surgical plans, were changed following in-person examination.
Of 348 visits, we completed 310 Pivothead, 128 digital slit-lamp and 102 digital indirect ophthalmoscope examinations. The Pivothead was by far the most useful to the ophthalmologist in attaining diagnosis for sensorimotor findings and also nystagmus, nasolacrimal duct obstruction (NLDO) and eyelid findings.
We performed slit-lamp biomicroscopy on 79 patients (59 dilated, 20 undilated; median age=9 years, age range=2–17 years) and gonioscopy once on an 8-year-old. All were successfully evaluated by the ophthalmologist via telemedicine.
Comprehensive examinations versus consultation examinations
The percentage of patients requiring surgery was slightly higher in the consultation compared with the comprehensive group (table 3). In the ophthalmologist’s estimation, more children in the consultation group had conditions warranting being seen by a paediatric ophthalmologist (78.4% vs 55.3% in the comprehensive group). The remaining patients either did not need to be seen at all or could have been seen by a qualified paediatric optometrist. Similarly, more children in the consultation group required follow-up care with ophthalmology (30.2% consultation vs 24.5% comprehensive) as opposed to follow-up exclusively with the optometrist or co-managed through telemedicine, although this difference may not be clinically significant.
Table 3.
Comprehensive examinations vs consultation examinations
| Comprehensive examinations | Consultation examinations | Total | |
| Subjects | 94 | 116 | 210 |
| Median age (years) | 6 | 7 | 6 |
| Surgeries | |||
| Subjects for whom surgery was indicated (including at initial and follow-up visits) | 31 (33.0%) | 40 (34.5%) | 71 (33.8%) |
| Subjects who had surgery | 27 (28.7%) | 35 (30.2%) | 62 (29.5%) |
| According to the ophthalmologist, this patient needed to be seen by an ophthalmologist | 52 (55.3%) | 91 (78.4%) | 143 (68.1%) |
| According to the ophthalmologist, follow-up care after initial visit: | |||
| Can be managed exclusively by paediatric optometrist | 53 (56.4%) | 69 (59.5%) | 122 (58.1%) |
| Can be co-managed by optometrist and ophthalmologist via telemedicine | 18 (19.1%) | 12 (10.3%) | 30 (14.3%) |
| Requires paediatric ophthalmology | 23 (24.5%) | 35 (30.2%) | 58 (27.6%) |
| According to the optometrist, she would have referred this patient to ophthalmology | 54 (57.4%) | NA | NA |
NA, not available.
Patients with strabismus
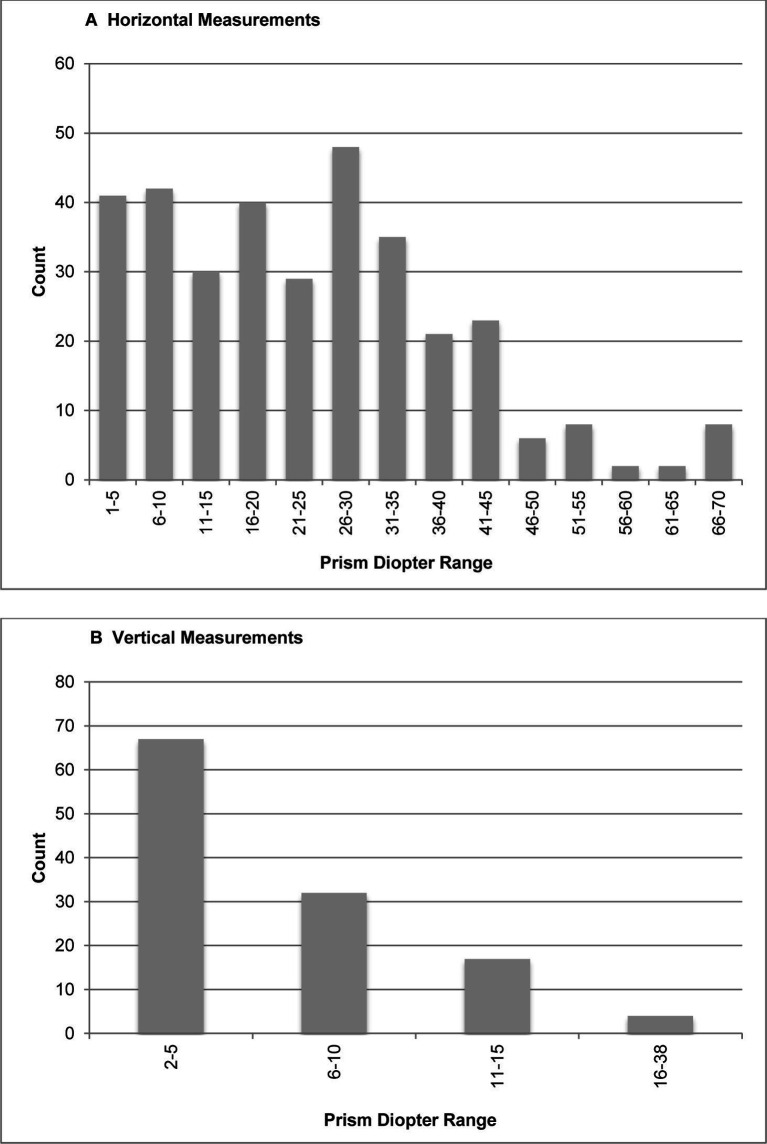
In pre-op and post-op patients with strabismus, excellent or almost perfect agreement between telemedicine and in-person examinations was observed for angle measurements (ICC=0.98–1.00) and disease categorisation (κ=0.94–1.00) (table 4). All agreement statistics were highly significant (p<0.0001). Measurement variations were minimal. Prism dioptres ranged from 1 to 70 in horizontal and 2–38 in vertical measurements (figure 1).
Table 4.
Agreement between telemedicine and in-person examinations for patients with strabismus
| Distance without correction | Near without correction | Distance with correction | Near with correction | ||
| Primary gaze angle measurements (ICC) |
Horizontal | 1.00 (n=47) |
1.00 (n=61) |
1.00 (n=26) |
1.00 (n=34) |
| Vertical | 0.98 (n=19) |
1.00 (n=15) |
0.98 (n=13) |
0.98 (n=12) |
|
| Motility disease categorisation (kappa) |
Horizontal | 0.98 (n=54) |
1.00 (n=69) |
0.96 (n=31) |
0.97 (n=36) |
| Vertical | 1.00 (n=54) |
0.94 (n=69) |
1.00 (n=31) |
1.00 (n=36) |
Angle measurement agreement is expressed as an intraclass correlation coefficient (ICC), and disease categorisation agreement is expressed as a kappa coefficient. N refers to the number of pairs evaluated.
Figure 1.
Range of prism dioptres in strabismus examinations for horizontal (A) and vertical (B) measurements.
Surgical patients
Sixty-two subjects (ages 0.5–17 years, median=6 years) had surgery, and three had more than one within 1 year of initial examination. Three surgeries were for NLDO; all others were for strabismus. Surgical measurements were obtained by Krimsky or Hirschberg in four patients, all others by alternate prism cover test.
Almost all patients who consented for surgery at the initial visit (54/55) did so during the telemedicine examination, while masked to receiving an in-person examination. One subject who declined surgery during the telemedicine encounter changed his mind after seeing the surgeon in-person. Four patients declined entirely. Twenty patients consented for surgery at follow-ups; however, these subjects had already been unmasked to the study design.
After the initial visit, 122 (58.1%) patients without active disease were deemed by the ophthalmologist to be appropriate to be seen in follow-up exclusively by the optometrist. Thirty (14.3%) with active disease requiring close follow-up could be co-managed through telemedicine. The remaining 58 (27.6%) required follow-up care with the ophthalmologist either for surgery (with pre-op and post-op visits via telemedicine, n=55) or for referral to another specialist (glaucoma or retina, n=3).
Process and experience outcomes
Forty of 348 (11.5%) examinations had some delay due to equipment challenges. Most delays lasted 5–10 min and involved the Pivothead or Polycom. Averaged across all encounters, this is approximately 1 min extra per encounter. In all 348 examinations, the ophthalmologist was able to hear and see the patient and visualise areas of interest.
Nearly all parents felt comfortable with the quality of the telemedicine examination (98.5%) and reported they would participate in another one in the future (97.1%).
Discussion
At The Vision Center, our motivation to study telemedicine was driven by an access problem, with the demand for paediatric ophthalmology care outstripping supply, and waits for a new appointment running over 5 months. Telemedicine offers considerable opportunity to address workforce shortages, links specialists with primary providers in the management of complex patients and speed access to care. Confidence with telemedicine among eye care providers is increasing, but at least one-third continue to feel “not at all confident” in remote screening for eye care.23 This underscores a need for research in clinical validation and also into participant experience.
Our study demonstrates the non-inferiority of real-time telemedicine relative to in-person examinations for diagnosing and managing paediatric ophthalmic conditions. In contrast to earlier studies with older technology,24 25 the ophthalmologist was able to make accurate diagnoses, plans and measurements in virtually every telemedicine encounter. This held true even with video resolution as low as 480p with the Pivothead.
It should be noted that we did not examine any children with anterior uveitis and cannot comment on the ability to detect anterior chamber inflammation by digital slit lamp. Also, only children who were able to participate in an age-appropriate manner were eligible to enrol, excluding many with developmental delays.
As for technical difficulties, indirect ophthalmoscopy took longer via telemedicine, in part because the working distance must be adjusted due to a discrepancy between what is seen and what is streamed. The digital indirect also uses a brighter LED light, making it difficult for young children. Furthermore, equipment delays added slightly more time to telemedicine exams.
The number of patients consenting for surgery during the telemedicine encounter indicates trust in the platform. Only five patients (8.1%) declined surgery at the initial telemedicine visit. For three of those, surgery was reconstructive and not for visual function (one changed his mind following the in-person examination). In another case, the patient already had surgery and the parent wanted to try a different treatment approach first. In the fifth case, the parents declined surgery recommended to improve binocularity, even after seeing the ophthalmologist in-person.
Unexpectedly, the ophthalmologist’s surgical volume increased 25% from the same period the year prior, despite closing regular, much higher (average 4×) volume clinics to conduct the study. We suspect the increase was due in part to the study presenting the optometrist with a faster route to get surgical patients seen. Whatever the cause, this suggests possible improved access for surgical patients, although this should be evaluated in future studies.
Real-time telemedicine is optimal for consultation examinations addressing a specific concern of the referring provider, rather than comprehensive examinations. While the ophthalmologist felt almost a third (31.9%) of patients overall did not need to be seen by an ophthalmologist, the difference between comprehensive (44.7%) and consultation (21.6%) subjects is striking. This—in combination with the fact that surgical volumes were similar between the comprehensive (28.7%) and consultation (30.2%) examinations—suggests the consultation group may have had a higher number of medical diagnoses requiring advanced care. This difference in complexity might also explain the higher rate of consultation examination patients who required follow-up care with an ophthalmologist after the initial visit (30.2% consultation vs 24.5% comprehensive).
The fact that close to half (44.7%) of comprehensive examinations did not require ophthalmology may support a care model in which paediatric optometrists see a majority of new patients first, with telemedicine offering targeted ophthalmology consultations as needed, although further study testing this hypothesis is required, particularly in diverse practice settings. Such a model could enable high-volume clinics to shift stable, low-acuity and/or postoperative patients out to be managed by paediatric optometrists from the same practice—ideally in a setting closer to the patient’s home—thereby freeing ophthalmologists to focus on acute or surgical patients. At CHLA, our optometrists travel to remote locations where they can manage our more stable patients, while our ophthalmologists block time for telemedicine consults, which are usually surgical cases pre-screened by the optometrist.
This telemedicine model is advantageous when patients live far from the surgical practice or when wait times are excessively long. The model holds less value in settings where patients face fewer barriers to care. The cost of equipment could present a challenge to scaling; however, the most useful piece of equipment in this study—the Pivothead—is relatively inexpensive (<US$1000). We also foresee that software video-conferencing capabilities will improve sufficiently to replace the need for the more expensive hard-wired conferencing system in the near future.
The principal limitation of this study was that examinations were performed by one ophthalmologist and one optometrist who became adept at working together, operating the equipment and troubleshooting glitches. There is a learning curve, and less experienced providers may take time to become proficient, possibly impacting adoption. The optometrist must be trained in paediatric optometry and highly competent with cycloplegic retinoscopy, as this component is not repeated by the ophthalmologist and can greatly impact managment. Future research should examine the feasibility of someone other than a paediatric optometrist on the patient’s end, such as an orthoptist, technician or paediatrician, as availability of pediatrics-trained optometrists could be a limiting factor.
Another limitation is confirmation bias, as the same ophthalmologist performed the telemedicine examination and the in-person examination. While the ophthalmologist was invested in study outcomes, this was outweighed by her interest in safe and correct patient care.
Finally, this study was conducted entirely on our internal network. It would not be unreasonable to expect connectivity challenges at external sites with less robust broadband connection.
This study demonstrates paediatric ophthalmic conditions can be reliably managed through real-time telemedicine. This model answers the specialist shortage, allows physicians to focus on surgical and medically complex patients, and helps ease access to care for underserved children.
Footnotes
Presented at: American Association of Pediatric Ophthalmology and Strabismus Annual Meeting 2019
Contributors: CS participated in study planning, conduct, data collection and analysis, interpretation of results, and writing and editing the manuscript. JC-S participated in study design, planning, conduct, and data collection and analysis, and provided critical revisions to the manuscript. MWR contributed to experimental design, performed data analysis, and provided figures/tables and critical revisions to the manuscript. TCH contributed to study design and interpretation of results, and provided critical revisions to the manuscript. TCL contributed to study conception and design, and provided intellectual contributions to the manuscript. SN led and directly participated in all facets of study conception and design, planning, conduct, data collection and analysis, interpretation of results, and writing and editing the manuscript.
Funding: We gratefully acknowledge the Margie & Robert E. Petersen Foundation for funding this research (no award number).
Disclaimer: The sponsor had no role in the design or conduct of this research.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. De-identified participant data may be available on reasonable request. Please contact the Principal Investigator, Dr. Sudha Nallasamy (sudha.nallasamy@gmail.com).
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the CHLA Institutional Review Board and conducted in accordance with the Helsinki Declaration.
References
- 1. Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol 2012;96:614–8. 10.1136/bjophthalmol-2011-300539 [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization . World report on vision. Geneva: World Health Organization, 2019. [Google Scholar]
- 3. Hashemi H, Pakzad R, Heydarian S, et al. Global and regional prevalence of strabismus: a comprehensive systematic review and meta-analysis. Strabismus 2019;27:54–65. 10.1080/09273972.2019.1604773 [DOI] [PubMed] [Google Scholar]
- 4. Hashemi H, Pakzad R, Yekta A, et al. Global and regional estimates of prevalence of amblyopia: a systematic review and meta-analysis. Strabismus 2018;26:168–83. 10.1080/09273972.2018.1500618 [DOI] [PubMed] [Google Scholar]
- 5. Hamm LM, Black J, Burn H, et al. Interventions to promote access to eye care for non-Indigenous, non-dominant ethnic groups in high-income countries: a scoping review protocol. BMJ Open 2020;10:e033775. 10.1136/bmjopen-2019-033775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ehrlich JR, Anthopolos R, Tootoo J, et al. Assessing geographic variation in strabismus diagnosis among children enrolled in Medicaid. Ophthalmology 2016;123:2013–22. 10.1016/j.ophtha.2016.05.023 [DOI] [PubMed] [Google Scholar]
- 7. Quinn GE, Ying G-shuang, Daniel E, et al. Validity of a telemedicine system for the evaluation of acute-phase retinopathy of prematurity. JAMA Ophthalmol 2014;132:1178–84. 10.1001/jamaophthalmol.2014.1604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang SK, Callaway NF, Wallenstein MB, et al. SUNDROP: six years of screening for retinopathy of prematurity with telemedicine. Can J Ophthalmol 2015;50:101–6. 10.1016/j.jcjo.2014.11.005 [DOI] [PubMed] [Google Scholar]
- 9. Weaver DT, Murdock TJ. Telemedicine detection of type 1 ROP in a distant neonatal intensive care unit. J AAPOS 2012;16:229–33. 10.1016/j.jaapos.2012.01.007 [DOI] [PubMed] [Google Scholar]
- 10. Murakami Y, Jain A, Silva RA, et al. Stanford University Network for Diagnosis of Retinopathy of Prematurity (SUNDROP): 12-month experience with telemedicine screening. Br J Ophthalmol 2008;92:1456–60. 10.1136/bjo.2008.138867 [DOI] [PubMed] [Google Scholar]
- 11. Silva RA, Murakami Y, Jain A, et al. Stanford University Network for Diagnosis of Retinopathy of Prematurity (SUNDROP): 18-month experience with telemedicine screening. Graefes Arch Clin Exp Ophthalmol 2009;247:129–36. 10.1007/s00417-008-0943-z [DOI] [PubMed] [Google Scholar]
- 12. Morrison D, Bothun ED, Ying G-S, et al. Impact of number and quality of retinal images in a telemedicine screening program for ROP: results from the e-ROP study. J AAPOS 2016;20:481–5. 10.1016/j.jaapos.2016.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Areaux RG, de Alba Campomanes AG, Indaram M, et al. Your eye doctor will virtually see you now: synchronous patient-to-provider virtual visits in pediatric tele-ophthalmology. J AAPOS 2020;24:197–203. 10.1016/j.jaapos.2020.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rathi S, Tsui E, Mehta N, et al. The current state of teleophthalmology in the United States. Ophthalmology 2017;124:1729–34. 10.1016/j.ophtha.2017.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sreelatha OK, Ramesh SV. Teleophthalmology: improving patient outcomes? Clin Ophthalmol 2016;10:285–95. 10.2147/OPTH.S80487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Caffery LJ, Taylor M, Gole G, et al. Models of care in tele-ophthalmology: a scoping review. J Telemed Telecare 2019;25:106–22. 10.1177/1357633X17742182 [DOI] [PubMed] [Google Scholar]
- 17. Ho T, Lee TC, Choe J-Y, et al . Evaluation of real-time video from the digital indirect ophthalmoscope for telemedicine consultations in retinopathy of prematurity. J Telemed Telecare 2020;Published Online First:10.1177/1357633X2095824. 10.1177/1357633X20958240 [DOI] [PubMed] [Google Scholar]
- 18. Ho T, Kolin T, Stewart C, et al . Evaluation of high-definition video-smart glasses for real-time telemedicine strabismus consultations. J AAPOS in press. [DOI] [PubMed] [Google Scholar]
- 1919. Mulchandani D, Reiser BJ, Ho TC, et al. Evaluation of digital slit-lamp videos for paediatric anterior segment telemedicine consultations. J Telemed Telecare 2021:1357633X21990991. 10.1177/1357633X21990991 [DOI] [PubMed] [Google Scholar]
- 20. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med 2012;22:276–82. 10.11613/BM.2012.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McGraw KO, Wong SP. Forming inferences about some intraclass correlation coefficients. Psychol Methods 1996;1:30–46. 10.1037/1082-989X.1.1.30 [DOI] [Google Scholar]
- 22. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15:155–63. 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. De Lott LB, Newman-Casey PA, Lee PP, et al. Change in ophthalmic clinicians' attitudes toward telemedicine during the coronavirus 2019 pandemic. Telemed J E Health 2021;27:231–5. 10.1089/tmj.2020.0222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cheung JC, Dick PT, Kraft SP, et al. Strabismus examination by telemedicine. Ophthalmology 2000;107:1999–2005. 10.1016/s0161-6420(00)00377-8 [DOI] [PubMed] [Google Scholar]
- 25. Dawson E, Kennedy C, Bentley C, et al. The role of telemedicine in the assessment of strabismus. J Telemed Telecare 2002;8:52–5. 10.1258/1357633021937361 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjophthalmol-2020-318385supp001.pdf (22.8KB, pdf)
Data Availability Statement
Data are available on reasonable request. De-identified participant data may be available on reasonable request. Please contact the Principal Investigator, Dr. Sudha Nallasamy (sudha.nallasamy@gmail.com).