Abstract
Background
Impaired cough results in airway secretion retention, atelectasis and pneumonia in individuals with Duchenne muscular dystrophy (DMD). Lung volume recruitment (LVR) stacks breaths to inflate the lungs to greater volumes than spontaneous effort. LVR is recommended in DMD clinical care guidelines but is not well studied. We aimed to determine whether twice-daily LVR, compared with standard of care alone, attenuates the decline in FVC at 2 years in boys with DMD.
Methods
In this multicentre, assessor-blinded, randomised controlled trial, boys with DMD, aged 6–16 years with FVC >30% predicted, were randomised to receive conventional treatment or conventional treatment plus manual LVR twice daily for 2 years. The primary outcome was FVC % predicted at 2 years, adjusted for baseline FVC % predicted, age and ambulatory status. Secondary outcomes included change in chest wall distensibility (maximal insufflation capacity minus FVC) and peak cough flow.
Results
Sixty-six boys (36 in LVR group, 30 in control) were evaluated (median age (IQR): 11.5 years (9.5–13.5), median baseline FVC (IQR): 85% predicted (73–96)). Adjusted mean difference in FVC between groups at 2 years was 1.9% predicted (95% CI −6.9% to 10.7%; p=0.68) in the direction of treatment benefit. We found no differences in secondary outcomes.
Conclusion
There was no difference in decline in FVC % predicted with use of twice-daily LVR for boys with DMD and relatively normal lung function. The burden associated with routine LVR may outweigh the benefit. Benefits of LVR to maintain lung health in boys with worse baseline lung function still need to be clarified.
Trial registration number
Keywords: child, Duchenne muscular dystrophy, lung volume recruitment, randomized controlled trial, respiratory therapy
Key messages.
What is the key question?
Does twice-daily lung volume recruitment (LVR) reduce decline in FVC in boys with Duchenne muscular dystrophy?
What is the bottom line?
The burden associated with routine LVR may outweigh the benefit in boys with relatively normal lung function.
Why read on?
This multicentre randomised controlled trial is the first to evaluate the effects of routine lung volume recruitment on decline in FVC % predicted, peak cough flow and chest wall distensibility (maximum insufflation capacity minus FVC) over a 2-year period in boys with Duchenne muscular dystrophy, with relatively normal baseline lung function.
Introduction
Duchenne muscular dystrophy (DMD) is a progressive neuromuscular disease that presents in childhood.1 Respiratory complications are the primary cause of morbidity and mortality and consist of nocturnal hypoventilation, chest wall restriction with loss of lung function and impaired cough resulting in retention of airway secretions, atelectasis and pneumonia.2 Respiratory management of DMD aims to maintain lung function, support respiration with non-invasive ventilation and clear the airways of secretions.3–6
Lung volume recruitment (LVR) is an ‘assisted inflation’ technique accomplished by stacking breaths to inflate the lungs to a volume greater than that achieved with spontaneous effort.7–9 Breath stacking aims to expand the lungs, reduce atelectasis, improve ventilation-perfusion matching, increase elastic recoil of the chest wall and increase expiratory airflow and airway wall shear forces to remove secretions. Regular inflation above spontaneous inspiratory capacity is hypothesised to maintain ‘range of movement’ or flexibility of the chest wall and lungs, preventing stiffening and contractures of costovertebral and costochondral joints.10 11 Retrospective studies in individuals with neuromuscular disease indicate LVR slows the decline in FVC,12 13 maintains maximum insufflation capacity (MIC)—a measure of chest wall distensibility—11 14–16 and maintains or increases peak cough flow (PCF).11 17 Only one prospective randomised controlled trial of long-term LVR has been published in a cohort of people with amyotrophic lateral sclerosis, a more rapidly progressive adult-onset condition.18 No trials of long-term LVR as the sole intervention exist in children with neuromuscular disease.
Despite this lack of robust evidence, several care guidelines recommend the use of LVR and similar airway clearance techniques for individuals with neuromuscular weakness.3–6 19 Although LVR is advocated for airway clearance, there is clinical equipoise regarding the benefit of regular routine LVR use. We therefore undertook a randomised controlled trial in boys with DMD to assess whether LVR, compared with standard of care alone, attenuates decline in FVC % predicted at 2 years (primary outcome), as well as the effect of LVR on PCF and chest wall distensibility (difference between MIC and vital capacity (VC)). We hypothesised that routine long-term use of LVR twice daily would attenuate FVC decline, maintain chest wall distensibility and compliance (MIC−VC difference) and increase PCF (assisted by LVR), compared with usual care in boys with DMD.
Methods
Trial design and setting
A prospective, multicentre, single blind, randomised controlled trial of boys with DMD was conducted (Clinicaltrials.gov)).
Participants
Children were identified through neuromuscular clinics. Eligibility criteria included: 6–16 years old, DMD confirmed by genetic testing or muscle biopsy, baseline FVC >30% predicted, caregiver willing to provide LVR therapy and fluent in English or French. As there is clinical equipoise on ideal timing for initiation of regular LVR, we also included boys with normal lung function (ie, FVC ≥80% predicted) to evaluate the effect of LVR across a spectrum of disease severity.
Reasons for ineligibility included enrolment in other intervention trials, patient-reported regular (daily) LVR or mechanical in-exsufflation therapy use (outside of a respiratory infection), inability to perform pulmonary function tests, endotracheal or tracheostomy tube, increased susceptibility to pneumothorax (including uncontrolled asthma or obstructive lung disease) or symptomatic cardiomyopathy. A research assistant obtained informed written consent/assent for all participants and caregivers prior to conducting study procedures.
Randomisation
Following baseline assessment, participants were randomised to conventional treatment or conventional treatment plus LVR, for a 2-year period. Concealed randomisation was conducted using an online website housed at the coordinating study site, using a minimisation allocation strategy developed using Taves’ method.20 The allocation strategy included study site, use of systemic glucocorticoids,21 baseline FVC (% predicted),22 degree of scoliosis,2 age and ambulatory status. Each treatment arm had a 50% chance of allocation when the minimisation scores were balanced, otherwise individuals were assigned according to the minimisation algorithm with an 80:20 allocation probability. Sites were not aware of allocation balance across study centres. The research assistant entered the participant’s information at the time of randomisation, and a treatment arm was allocated immediately. The research assistant informed families of their treatment arm and instructed them not to share this information with the blinded assessor in order to maintain blinding. Blinding was further maintained by not recording treatment allocation in the participant’s medical chart.
Study arms
Participants in the control arm received standard of care for DMD, which included physiotherapy, nutritional support, oral or intravenous antibiotics for respiratory infections, non-invasive ventilation for sleep-disordered breathing and/or use of systemic glucocorticoids.23
Participants and caregivers in the intervention arm were taught manual LVR therapy by a respiratory therapist or physiotherapist during an in-person clinic visit of approximately 30 min duration. During the training session, the parent and child were given a demonstration and then tried it independently, until the clinician felt confident in the family’s ability to properly administer LVR.
The provided LVR kit for home use comprised a self-inflating resuscitation bag, one-way valve, mouthpiece and written instructions (LVR kit item number 1034502; Mercury Medical, Florida, USA). Therapy consisted of 3–5 sequential bag compressions with a breath-hold between each, delivered by a caregiver in coordination with the child’s own inspiration to achieve one maximal inflation to MIC, followed by a cough. Insufflation volume was individually titrated and determined by clinical evaluation. This consisted of visual inspection of chest wall excursion24 and patient comfort, to a maximum of 40 cmH2O due to a pressure-release valve.15 24 Three to five maximal inflation repetitions were performed in each session.
Participants were advised to conduct LVR twice daily, prior to meals or at least 2 hours after. In line with clinical practice, LVR technique was re-evaluated at follow-up visits, with additional training provided as necessary.
All participants were permitted to use manual and mechanically assisted cough techniques during acute respiratory exacerbations, if advised by their physician. Brief use of LVR or mechanical in-exsufflator was considered unlikely to affect the primary outcome.
Outcome measures
The primary outcome was FVC %-predicted at 2 years. Secondary outcome measures included change in MIC−VC (L), PCF (L/min), total lung capacity (TLC) (L), maximal inspiratory pressure (MIP) (cm H2O) and maximal expiratory pressure (MEP) (cm H2O).
Pulmonary function tests were performed every 6 months by blinded respiratory therapists or pulmonary function technologists as part of standard clinical care, according to American Thoracic Society recommendations.25 Review of the MIC technique was conducted at all sites during site onboarding. If fatigue prevented repeated manoeuvres, a single trial was included if the flow-volume loop met acceptability criteria.25–27 The Stanojevic normative equations were used to calculate % predicted values for FVC and FEV1.28 Measurements of MIC, MIP, MEP and PCF were performed according to established protocols.17 29–32 TLC was measured with plethysmography.
At this visit, the research assistant obtained LVR adherence data from children in the intervention arm. Adherence data were downloaded from a battery-powered data logger fitted to the LVR kit (Omega OM-CP-State101A data logger, OMEGA Engineering, Inc; Stamford, Connecticut, USA). The data logger was wired to two pressure switches connected in series (Model 7411–711, PSF102 Series pressure switch, TLCtDesignFlex Switches, A World Magnetics Company; Traverse City, Michigan, USA). The data logger measured date-stamped and time-stamped time-at-pressure, enabling calculation of the number of sessions per day. Logger data was supplemented by self-report adherence diaries, collected by the research assistant every 3 months by telephone or in-person. Intervention adherence, defined through investigator consensus, was considered as at least one LVR session per day on at least 50% of days.
Sample size
The sample size was informed by a survey of Canadian Paediatric Respirologists and Neuromuscular Specialists,33 which suggested that a 30% relative reduction in decline in FVC % predicted was the minimal clinically important difference. Assuming a decline in FVC of 12% predicted over 2 years,34 35 a minimal difference of 3.6% predicted, a SD of 5.5%35 and a two-sided test, 76 participants would yield 80% power and type I error of 5%. We targeted a sample size of 110 to account for non-compliance, crossovers and loss to follow-up.
Statistical methods
Analyses were conducted in R V.4.0.2.36 The primary analysis was an analysis of covariance (ANCOVA) multivariable model that analysed FVC % predicted at 2 years, adjusted for baseline FVC % predicted as a means of assessing change over time. Age and ambulatory status were also included in the model as they were part of the minimisation strategy. Missing data in an intention-to-treat population was addressed with longitudinal (time-raster) multiple imputation methods using chained equations to account for irregularly timed or missing FVC measurements (mice package V.3.11).37 The linear mixed model included time as a fixed effect and participant as a random effect (lme4 package V.1.1.23). A preplanned sensitivity analysis to account for treatment adherence used a complier average causal effect estimation method that applied a propensity score based on overall LVR adherence over the 2-year period (inverse probability weighting applied to control participants).38 Preplanned analyses were also repeated by subgroups, defined as baseline MIC−VC difference less than or greater than 10% of the FVC to explore whether baseline chest distensibility and recruitment volume was associated with a long-term effect. Time to an absolute decrease of 10% in FVC % predicted between control and intervention groups was compared using a Cox proportional hazards model, adjusting for age and ambulatory status.
Linear mixed models were used for analysis of secondary outcomes. The proportion of missing data for TLC, MIC−VC and assisted-unassisted PCF did not support imputation and descriptive analyses were performed.
Results
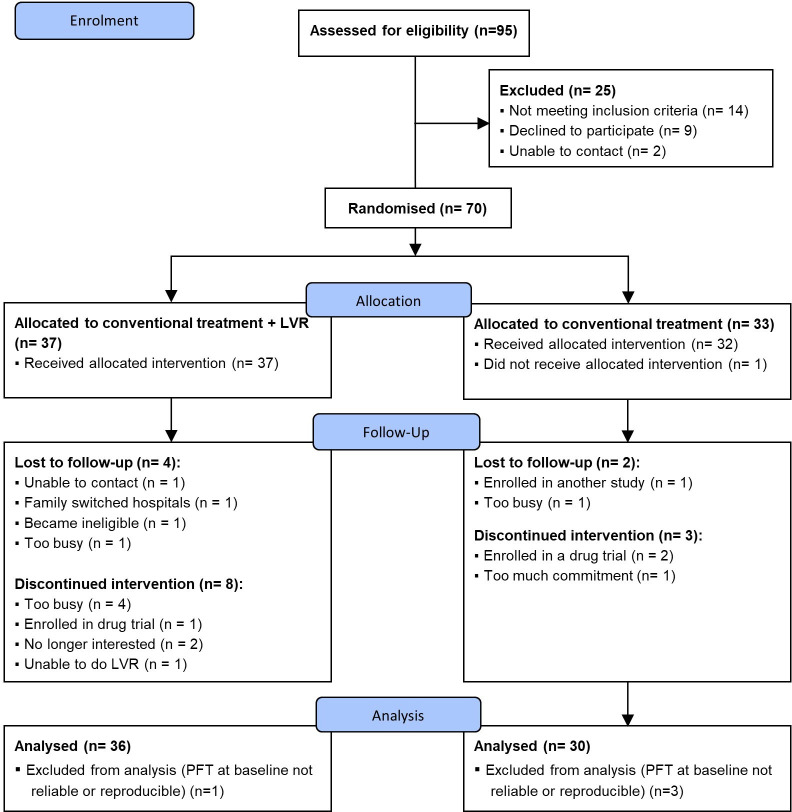
Ninety-five boys with DMD were assessed for eligibility; 25 were excluded (figure 1). We enrolled the remaining 70 boys. However, four did not have reliable or reproducible FVC measurements at baseline and were subsequently excluded. This left 66 participants, of which 36 were randomised to the intervention and 30 to control. Fifty-three participants (76%) completed the 2-year study. Recruitment occurred between December 2013 and September 2016 (predetermined end date); the final study visit was in November 2018. Baseline characteristics were similar between groups (table 1). Median age was 11.5 years (IQR: 9.5–13.5). At baseline, median FVC was 84.8% predicted (IQR: 73.3–95.5); 52 participants had MIC−VC greater than 10% of FVC. Most participants (59/66, 89%) were receiving systemic steroids; the corticosteroid regime was daily deflazacort in the majority of cases. Almost one-third (32%) were wheelchair assisted; 6% used non-invasive ventilation for nocturnal hypoventilation; and no participants used an in-exsufflator. No participants reported new initiation of non-invasive ventilation during the follow-up period. One participant in the non-LVR arm started using an in-exsufflator for respiratory exacerbations during follow-up. Three participants had chest infections requiring antibiotics (two in the LVR arm, one in the conventional treatment group).
Figure 1.
CONSORT flow diagram. CONSORT, Consolidated Standards of Reporting Trials; LVR, lung volume recruitment; PFT, pulmonary function test.
Table 1.
Baseline characteristics
| Variable | Overall | Conventional treatment* | Conventional treatment +LVR* |
| n=66 | n=30 | n=36 | |
| Age (years), median (IQR) | 11.5 (9.5–13.5) | 11.5 (9.2–13.0) | 11.5 (9.5–13.9) |
| FVC (%-predicted), median (IQR) | 84.8 (73.3–95.5) | 85.6 (73.8–98.8) | 84.0 (73.9–92.4) |
| Wheelchair assisted, n (%) | 21 (32) | 10 (33) | 11 (31) |
| Scoliosis, n (%) | 9 (14) | 3 (10) | 6 (17) |
| Non-invasive ventilation, n (%) | 4 (6) | 2 (7) | 2 (6) |
| Steroid use, n (%) | 59 (89) | 27 (90) | 32 (89) |
*There were no differences in baseline characteristics between the intervention and control groups (p>0.05).
LVR, lung volume recruitment.
Of 330 planned pulmonary function tests, 47 (14%) were not done. Of 283 pulmonary function tests, 217 (77%) were both reliable and reproducible. In 50 instances (18%), a single reliable measurement was obtained. An additional 16 pulmonary function tests (6%) were neither reliable nor reproducible and were treated as missing.
Twenty (59%) participants were adherent to LVR in year 1, 21 (62%) in year 2 and 14 (41%) were LVR-adherent in both years. There was no crossover between study groups. At each study time point, between one and four participants in the control arm reported rescue LVR treatment, with a range of 1–11 LVR sessions performed per individual.
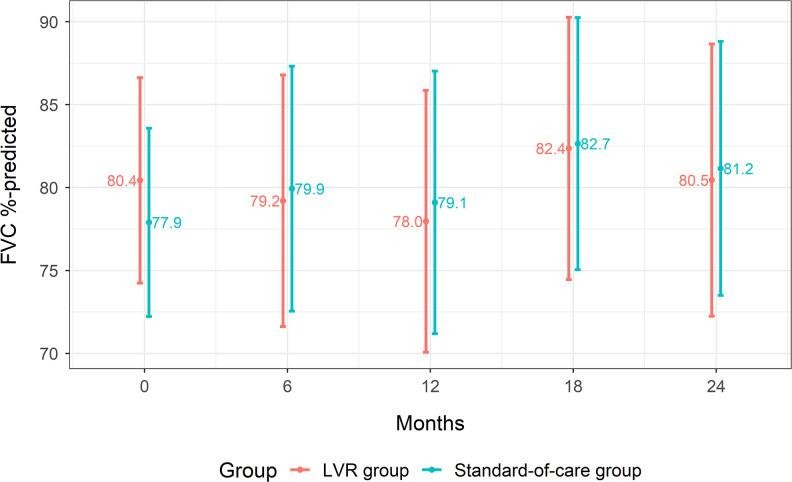
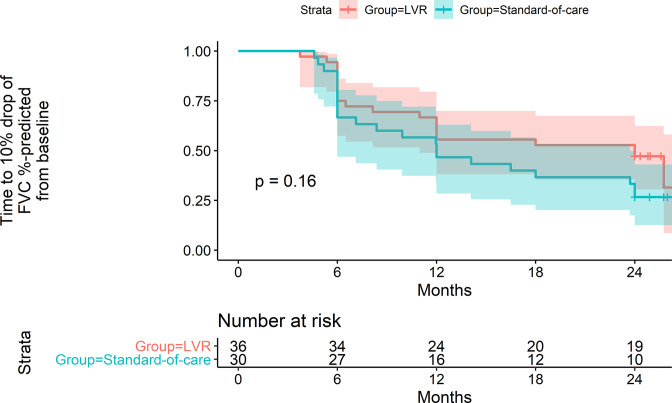
All 66 children were included in the primary analyses. For the primary analysis, the ANCOVA-estimated adjusted mean difference in FVC between study groups at 2 years was 1.9% predicted (95% CI −6.9 to 10.7; p=0.68; R2=0.66; n=66), with the point estimate in the direction of treatment benefit. Secondary analyses of FVC % predicted at each time point showed no evidence of a time-by-intervention group interaction (p=0.94; R2=0.41; n=66; figure 2). In the per-protocol analysis adjusted for adherence, the ANCOVA-estimated adjusted mean difference between LVR and standard-of-care groups at 2 years was 2.7% predicted FVC (95% CI −8.3 to 13.6; p=0.64; R2=0.68; n=66). Cox regression of time to absolute 10% decrease in FVC % predicted did not identify a difference between groups (HR 0.7, 95% CI 0.3 to 1.4; p=0.30; n=66; figure 3).
Figure 2.
Secondary analysis of FVC % predicted over time. Marginal means by group with 95% CI from mixed effect model of FVC % predicted, adjusted for age and ambulatory status, at 6-month intervals. LVR, lung volume recruitment.
Figure 3.
Kaplan-Meier curve for a single missing data imputation. LVR, lung volume recruitment.
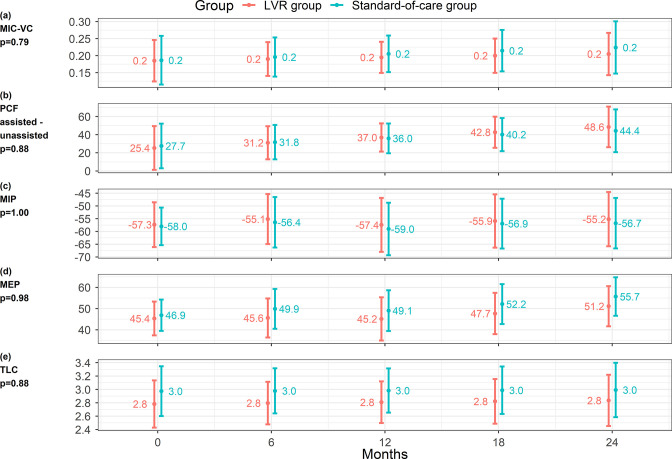
For MIC−VC, PCF assisted − PCF unassisted and TLC, imputation of missing data was not feasible, and observed data were used. Change over time in trajectory of MIC−VC and PCF assisted unassisted were not different between study groups (p=0.79; R2=0.29; n=42 and p=0.88; R2=0.26; n=45, respectively; figure 4a, b). No statistical differences were detected between study groups over time in MIP (p=1.00; R2=0.07; n=66), MEP (p=0.98; R2=0.05; n=66), nor TLC (p=0.88; R2=0.69; n=35; figure 4c–e). A secondary analysis considering change in FVC % predicted over time among subgroups with baseline MIC−VC less than or greater than 10% of the FVC did not detect a difference in the slope of FVC % predicted over time (p=0.19; R2=0.67; n=14, and p=0.13; R2=0.92; n=12, respectively, online supplemental figure S1a, b).
Figure 4.
Change in secondary outcomes (MIC−VC (L), PCF-assisted – PCF-unassisted (L/min), MIP (cm H2O), MEP (cm H2O) and TLC (L) over time. Marginal means by group with 95% CI from mixed effect model of secondary outcomes, adjusted for age and ambulatory status, at 6-month intervals. MEP, maximal expiratory pressure; MIC, maximum insufflation capacity; MIP, maximal inspiratory pressure; PCF, peak cough flow; TLC, total lung capacity.
thoraxjnl-2021-218196supp001.pdf (74.3KB, pdf)
No serious adverse events were reported. One individual in the intervention arm experienced a syncopal episode probably related to LVR and subsequently withdrew from the study. Two individuals had mild chest discomfort resulting in brief interruptions of LVR treatment; one had cough during LVR, which did not result in change in LVR use.
Discussion
In this, to our knowledge, first-ever randomised controlled trial of LVR in children with neuromuscular disease, we found no difference in FVC % predicted at 2 years of follow-up among boys with DMD and relatively normal baseline pulmonary function using twice-daily LVR in addition to usual care compared with usual care alone. As many study participants had normal lung function at baseline, it is not surprising that a large improvement in the downward trajectory of FVC % predicted was not observed with twice-daily LVR. This may be because the expected loss of FVC % predicted over a 2-year period is small in those with relatively normal lung function at baseline.22 26 34 The use of systemic glucocorticoids in the majority of our study population may have further helped to preserve lung function.21
Our study suggests there may be less benefit of LVR therapy in less advanced disease. Current clinical care guidelines for individuals with DMD recommend implementation of regular LVR treatment when there is evidence of weak cough (ie, PCF below 270 L/min and/or FVC <60% predicted).4 6 23 As an impact on the decline in FVC was not demonstrated in our cohort of boys with relatively normal lung function, our results suggest that twice-daily LVR may not be necessary when lung function is normal, providing novel, high-quality evidence to support current clinical care guidelines. This is an important finding as LVR represents an additional treatment burden for children and families. This is reflected in our study adherence data, where only 41% of participants were adherent to LVR across both study years. While low, this adherence rate is similar to that reported in children prescribed non-invasive ventilation.39 It will be necessary to further explore the reasons behind the low LVR adherence rates, as LVR likely still has an important role in assisting airway clearance during pulmonary exacerbations in this population, when pulmonary function may be expected to be reduced, as well as for preservation of chest wall compliance.
Furthermore, although differences in FVC % predicted were not detected in our study, LVR may be beneficial for maintenance of other important aspects of lung function in those with relatively normal lung health. We speculate that long-term regular LVR therapy initiated prior to onset of lung function abnormalities may help to preserve distensibility of the chest wall, akin to prevention of other joint contractures with the use of range-of-motion exercises, by preventing stiffening and fixed restriction of the chest wall which maintains the ability to expand the chest and lungs.40 Sustained improvements in respiratory system compliance may delay the onset of respiratory failure, the need for ventilatory support and/or allow adequate non-invasive ventilation at lower airway pressures. Improved airway clearance of secretions may also prevent atelectasis and pneumonia. Such potential benefits of LVR in those with relatively normal lung function will require further exploration. There is thus a paradox where clinical benefit of regular LVR likely exists even among those with normal lung function, although our study was unable to demonstrate it. Future studies may compare measures of chest wall compliance or respiratory symptoms over time when routine LVR is initiated at different thresholds of lung function or age. This may be best accomplished through examination of registry data, as lack of clinical equipoise may preclude inclusion of individuals with more advanced neuromuscular disease in randomised trials. Understanding of the role of LVR to maintain all aspects of lung and chest wall health will be especially critical as new therapies for DMD appear on the horizon that may ultimately change the trajectory of the natural history of disease.
Due to our recruitment of participants with essentially normal lung function, despite inclusion criteria of FVC >30% predicted, important knowledge gaps remain in those with more advanced disease. These include the optimal timing for LVR introduction, frequency of use and efficacy in maintaining or improving lung function.9 LVR may be more beneficial in boys with lower baseline lung function and more advanced disease. This was observed in our previous retrospective cohort of individuals with more advanced disease, although differences in MIC−VC over time were not seen between treatment groups in the current study.11
This study has several strengths. We used a rigorous multicentre randomised design that incorporated a minimisation strategy to ensure well-balanced study groups at baseline. Adherence to LVR therapy was objectively recorded with an in-line data logger. Longitudinal follow-up over a 2-year period was achieved.
Our study also has limitations. Although we recruited a nationally representative sample of boys with DMD, due to recruitment challenges (several pharmaceutical trials competed for recruitment of the same population), the study sample was smaller than planned, meaning our study is likely underpowered. Furthermore, low adherence may have limited our ability to detect between-group differences. Despite eligibility criteria that aimed to recruit individuals with a broad range of baseline lung function, most participants had relatively normal lung function. This may have been due to existing regular use of LVR or other airway clearance therapy in those with lower baseline lung function, rendering them ineligible for study participation. While there were no routinely applied criteria for initiation of regular LVR therapy at the time of the study start, guidelines published later in the study period may have influenced clinicians’ LVR prescription practices,41 thereby decreasing our eligible pool of participants. Finally, although our study had a long intervention period—that is, 2 years, which is a strength—some data were missing. This was mitigated, where possible, by imputation of missing values. These limitations highlight the challenges of conducting large-scale studies in children with neuromuscular disease.
Conclusion
In this randomised controlled trial of 66 boys with DMD and relatively normal lung function, we found no difference in rate of decline in FVC % predicted over 2 years when twice-daily LVR was used. This novel, high-quality evidence supports clinical guidelines that recommend LVR initiation only once lung function is below a certain threshold. Therefore, in boys with DMD and normal lung function, the treatment burden of twice-daily routine LVR may outweigh the therapeutic benefit. However, the benefits of LVR as prophylactic regular therapy for boys with DMD with lower lung function still needs further research.
thoraxjnl-2021-218196supp002.pdf (938.3KB, pdf)
Acknowledgments
The study team wishes to thank the children, families, research coordinators and sites who participated in the trial.
Footnotes
Twitter: @lbfwolfe
Presented at: 1. Katz SL, Momoli M, Barrowman N, Bijelic V, Mah JK, McMillan H, Campbell C, Blinder H, McKim D, for the STEADFAST Study Group. Stacking Exercises Attenuate the Decline in Forced Vital Capacity and Sick Time (STEADFAST). CHEST 2019. New Orleans, Louisiana, USA. October 21, 2019 (publication citation: Katz SL, Momoli M, Barrowman N, Bijelic V, Mah JK, McMillan H, Campbell C, Blinder H, McKim D, for the STEADFAST Study Group. Stacking Exercises Attenuate the Decline in Forced Vital Capacity and Sick Time (STEADFAST). CHEST. 2019; 156(4): A245-6). 2. Katz SL, Blinder H, Bijelic V, Barrowman N, Hoey L, Momoli F, Campbell, C, MacLusky, IB, Mah, JK, McMillan, H, McKim D, on behalf of the STEADFAST Study Group. Adherence to Lung Volume Recruitment in Youth with Duchenne Muscular Dystrophy. 15th International Conference on Home Mechanical Ventilation (JIVD). Lyon, France. March 15, 2018 (no publication citation).
Contributors: SLK conceptualised and designed this study, oversaw the acquisition, analysis and interpretation of study data across all sites and wrote the first draft of this manuscript. SLK serves as the guarantor of this work. CC, JKM, LCM, TTDN, MT, DFW and DZ oversaw acquisition and interpretation of study data at their respective sites. SDA, NB, FM and HJM substantially contributed to the design of this study and oversaw the analysis and interpretation of the data. VB conducted the analysis and interpretation of the study data. SDA, DJB, DM, HJM, LR, NS and LW and substantially contributed to the interpretation of the data. HB substantially contributed to the acquisition of the study data. All authors critically revised the manuscript for important intellectual content, gave final approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: This study was generously funded by Jesse’s Journey.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Children’s Hospital of Eastern Ontario Research Ethics Board (REB), Ottawa, Canada #12/26E; Conjoint Health REB, Calgary, Canada #24998; University of British Columbia / Children’s and Women’s Health Centre of British Columbia REB, Vancouver, Canada # H13-03192; Holland Bloorview REB, Toronto, Canada #13-458; Hamilton Integrated REB, Hamilton, Canada #14-167; McGill University Health Centre Pediatric REB, Montreal, Canada #13-423-PED; CHU Sainte-Justine Comité d’éthique de la recherche, Montreal, Canada #E4747; University of Western Ontario Health Sciences REB, London, Canada #104817; and University of Alberta Health REB, Edmonton, Canada #Pro00044241. Participants gave informed consent to participate in the study before taking part.
References
- 1. Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol 2018;17:251–67. 10.1016/S1474-4422(18)30024-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Panitch HB. The pathophysiology of respiratory impairment in pediatric neuromuscular diseases. Pediatrics 2009;123 Suppl 4:S215–8. 10.1542/peds.2008-2952C [DOI] [PubMed] [Google Scholar]
- 3. Hull J. British thoracic Society guideline for respiratory management of children with neuromuscular weakness: commentary. Thorax 2012;67:654–5. 10.1136/thoraxjnl-2012-202043 [DOI] [PubMed] [Google Scholar]
- 4. Amin R, MacLusky I, Zielinski D, et al. Pediatric home mechanical ventilation: a Canadian thoracic Society clinical practice guideline executive summary. Can J Respir Crit Care Sleep Med 2017;1:7–36. 10.1080/24745332.2017.1300463 [DOI] [Google Scholar]
- 5. Bushby K, Finkel R, Birnkrant DJ. Diagnosis and management of Duchenne muscular dystrophy, part 2: implementation of multidisciplinary care.[Erratum appears in Lancet Neurol. 2010 Mar;9(3):237]. Lancet Neurol 2010;9:177–89. [DOI] [PubMed] [Google Scholar]
- 6. McKim DA, Road J, Avendano M, et al. Home mechanical ventilation: a Canadian thoracic Society clinical practice guideline. Can Respir J 2011;18:197–215. 10.1155/2011/139769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lynne Katz S, On behalf of the CTS Pediatric Home Ventilation Guidelines Panel . Section 5: airway clearance. Can J Respir Crit Care Sleep Med 2018;2:32–40. 10.1080/24745332.2018.1494979 [DOI] [Google Scholar]
- 8. Chatwin M, Toussaint M, Gonçalves MR, et al. Airway clearance techniques in neuromuscular disorders: a state of the art review. Respir Med 2018;136:98–110. 10.1016/j.rmed.2018.01.012 [DOI] [PubMed] [Google Scholar]
- 9. Sheers N, Howard ME, Berlowitz DJ. Respiratory adjuncts to NIV in neuromuscular disease. Respirology 2019;24:512–20. 10.1111/resp.13431 [DOI] [PubMed] [Google Scholar]
- 10. Bach JR, Mahajan K, Lipa B, et al. Lung insufflation capacity in neuromuscular disease. Am J Phys Med Rehabil 2008;87:720–5. 10.1097/PHM.0b013e31817fb26f [DOI] [PubMed] [Google Scholar]
- 11. Katz SL, Barrowman N, Monsour A, et al. Long-term effects of lung volume recruitment on maximal inspiratory capacity and vital capacity in Duchenne muscular dystrophy. Ann Am Thorac Soc 2016;13:217–22. 10.1513/AnnalsATS.201507-475BC [DOI] [PubMed] [Google Scholar]
- 12. McKim DA, Katz SL, Barrowman N, et al. Lung volume recruitment slows pulmonary function decline in Duchenne muscular dystrophy. Arch Phys Med Rehabil 2012;93:1117–22. 10.1016/j.apmr.2012.02.024 [DOI] [PubMed] [Google Scholar]
- 13. Chiou M, Bach JR, Jethani L, et al. Active lung volume recruitment to preserve vital capacity in Duchenne muscular dystrophy. J Rehabil Med 2017;49:49–53. 10.2340/16501977-2144 [DOI] [PubMed] [Google Scholar]
- 14. Kang SW, Bach JR. Maximum insufflation capacity. Chest 2000;118:61–5. 10.1378/chest.118.1.61 [DOI] [PubMed] [Google Scholar]
- 15. Fauroux B, Guillemot N, Aubertin G, et al. Physiologic benefits of mechanical insufflation-exsufflation in children with neuromuscular diseases. Chest 2008;133:161–8. 10.1378/chest.07-1615 [DOI] [PubMed] [Google Scholar]
- 16. Molgat-Seon Y, Hannan LM, Dominelli PB, et al. Lung volume recruitment acutely increases respiratory system compliance in individuals with severe respiratory muscle weakness. ERJ Open Res 2017;3. 10.1183/23120541.00135-2016. [Epub ahead of print: 14 03 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kang SW, Bach JR. Maximum insufflation capacity: vital capacity and cough flows in neuromuscular disease. Am J Phys Med Rehabil 2000;79:222–7. 10.1097/00002060-200005000-00002 [DOI] [PubMed] [Google Scholar]
- 18. Rafiq MK, Bradburn M, Proctor AR, et al. A preliminary randomized trial of the mechanical insufflator-exsufflator versus breath-stacking technique in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 2015;16:448–55. 10.3109/21678421.2015.1051992 [DOI] [PubMed] [Google Scholar]
- 19. Birnkrant DJ, Bushby KMD, Amin RS, et al. The respiratory management of patients with Duchenne muscular dystrophy: a DMD care considerations Working group specialty article. Pediatr Pulmonol 2010;45:739–48. 10.1002/ppul.21254 [DOI] [PubMed] [Google Scholar]
- 20. Taves DR. Minimization: a new method of assigning patients to treatment and control groups. Clin Pharmacol Ther 1974;15:443–53. 10.1002/cpt1974155443 [DOI] [PubMed] [Google Scholar]
- 21. Biggar WD, Harris VA, Eliasoph L, et al. Long-Term benefits of deflazacort treatment for boys with Duchenne muscular dystrophy in their second decade. Neuromuscul Disord 2006;16:249–55. 10.1016/j.nmd.2006.01.010 [DOI] [PubMed] [Google Scholar]
- 22. Rideau Y, Jankowski LW, Grellet J. Respiratory function in the muscular dystrophies. Muscle Nerve 1981;4:155–64. 10.1002/mus.880040213 [DOI] [PubMed] [Google Scholar]
- 23. Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol 2018;17:347–61. 10.1016/S1474-4422(18)30025-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Boitano LJ. Equipment options for cough augmentation, ventilation, and noninvasive interfaces in neuromuscular respiratory management. Pediatrics 2009;123 Suppl 4:S226–30. 10.1542/peds.2008-2952F [DOI] [PubMed] [Google Scholar]
- 25. American Thoracic S . Standardization of spirometry, 1994 update. AJRCCM 1994;1995:1107–36. [DOI] [PubMed] [Google Scholar]
- 26. Mayer OH, Finkel RS, Rummey C, et al. Characterization of pulmonary function in Duchenne muscular dystrophy. Pediatr Pulmonol 2015;50:487–94. 10.1002/ppul.23172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J 2005;26:511–22. 10.1183/09031936.05.00035005 [DOI] [PubMed] [Google Scholar]
- 28. Stanojevic S, Wade A, Stocks J, et al. Reference ranges for spirometry across all ages: a new approach. Am J Respir Crit Care Med 2008;177:253–60. 10.1164/rccm.200708-1248OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kang S-W, Kang Y-S, Sohn H-S, et al. Respiratory muscle strength and cough capacity in patients with Duchenne muscular dystrophy. Yonsei Med J 2006;47:184–90. 10.3349/ymj.2006.47.2.184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kang SW, Shin JC, Park CI, et al. Relationship between inspiratory muscle strength and cough capacity in cervical spinal cord injured patients. Spinal Cord 2006;44:242–8. 10.1038/sj.sc.3101835 [DOI] [PubMed] [Google Scholar]
- 31. Sancho J, Servera E, Díaz J, et al. Predictors of ineffective cough during a chest infection in patients with stable amyotrophic lateral sclerosis. Am J Respir Crit Care Med 2007;175:1266–71. 10.1164/rccm.200612-1841OC [DOI] [PubMed] [Google Scholar]
- 32. Suárez AA, Pessolano FA, Monteiro SG, et al. Peak flow and peak cough flow in the evaluation of expiratory muscle weakness and bulbar impairment in patients with neuromuscular disease. Am J Phys Med Rehabil 2002;81:506–11. 10.1097/00002060-200207000-00007 [DOI] [PubMed] [Google Scholar]
- 33. Katz SL, McKim D, Hoey L, et al. Respiratory management strategies for Duchenne muscular dystrophy: practice variation amongst Canadian sub-specialists. Pediatr Pulmonol 2013;48:59–66. 10.1002/ppul.22548 [DOI] [PubMed] [Google Scholar]
- 34. Phillips MF, Quinlivan RC, Edwards RH, et al. Changes in spirometry over time as a prognostic marker in patients with Duchenne muscular dystrophy. Am J Respir Crit Care Med 2001;164:2191–4. 10.1164/ajrccm.164.12.2103052 [DOI] [PubMed] [Google Scholar]
- 35. Velasco MV, Colin AA, Zurakowski D, et al. Posterior spinal fusion for scoliosis in Duchenne muscular dystrophy diminishes the rate of respiratory decline. Spine 2007;32:459–65. 10.1097/01.brs.0000255062.94744.52 [DOI] [PubMed] [Google Scholar]
- 36. R Core Team . R: a language and environment for statistical computing. Vienna, Austria: R foundation for statistical computing, 2020. Available: https://www.R-project.org/
- 37. van Buuren S, Groothius-Oudshoorn K. Multivariate imputation by chained equations in R. J Stat Softw 2011;45:1–67. [Google Scholar]
- 38. Herbert RD, Kasza J, Bo K. Analysis of randomised trials with long-term follow-up. BMC Med Res Methodol 2018;18:48. 10.1186/s12874-018-0499-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Blinder H, Momoli F, Bokhaut J, et al. Predictors of adherence to positive airway pressure therapy in children: a systematic review and meta-analysis. Sleep Med 2020;69:19–33. 10.1016/j.sleep.2019.12.015 [DOI] [PubMed] [Google Scholar]
- 40. Kravitz RM. Airway clearance in Duchenne muscular dystrophy. Pediatrics 2009;123 Suppl 4:Suppl-5–235. 10.1542/peds.2008-2952G [DOI] [PubMed] [Google Scholar]
- 41. Proulx F, Blinder H, Barrowman N, et al. Current practice and evolution of pediatric respiratory management of Duchenne muscular dystrophy in Canada. Can J Respir Crit Care Sleep Med 2021;13:1–15. 10.1080/24745332.2020.1867486 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
thoraxjnl-2021-218196supp001.pdf (74.3KB, pdf)
thoraxjnl-2021-218196supp002.pdf (938.3KB, pdf)
Data Availability Statement
No data are available.