Abstract
The aim of this observation was to report a rare case of symptomatic and non-functional cystic parathyroid adenoma in a 52-year-old female, diagnosed with imaging and treated by surgical resection of the gland.
Keywords: Dysphagia, Neck mass, Parathyroid cyst
Introduction
Cystic parathyroid adenoma is a rare clinical and histological entity. It represents 1% to 3.3% of parathyroid pathology [1]. It occurs mainly in women between 40 and 50 years old. It can be non-secreting or secreting and therefore responsible for hyperparathyroidism in 10% to 15% of cases [2].
Symptoms may be variable, with local or hormonal repercussions of the adenoma. While fewer than 300 cases are currently described in the literature, we report an additional rare case of non-functioning cystic parathyroid adenoma.
Observation
A 52-year-old female with a history of treated breast neoplasia and history of right temporal ischemic cerebrovascular accident was admitted to the hospital for swelling in the right lateral neck with dysphagia with dysphagia which evolved over 8 months. Clinical examination revealed a renitent and painless mass on the left side of the lower anterior part of the neck, with no inflammatory signs.
The biological assessment showed euthyroidism with TSH level at 2 mIU/L, T4 at 90 nmol and a normal parathyroid assessment: PTH at 35 pg/mlmL, calcemia at 93 mg/l. For initial evaluation, neck ultrasound revealed a large, roughly rounded, multiloculated, and anechoic mass with few thin septa.
Neck CT scan confirms the cystic nature of the mass, plunging into the level of anterosuperior of mediastinum. This non-enhancing mass compressed the trachea and oesophagus, and measured 68 × 45 × 37 mm (Fig. 1).
Fig. 1. (.
A-C) Post-contrast neck CT scan with axial (A, B) and sagittal (C) sections showing a hypodense laterocervical mass at the level of the left parathyroid compartment compressing and displacing the trachea, thyroid gland (orange arrow in Fig. 1A), and esophagus (yellow arrow in Fig. 1B).
The patient underwent surgical excision of the mass, with a simple postoperative course (Fig. 2). The anatomopathological study is in favor of a cystic parathyroid adenoma (Figs. 3 and 4). The patient recovered well after 10 months of follow-up.
Fig. 2.

Surgical specimen after total removal of the mass.
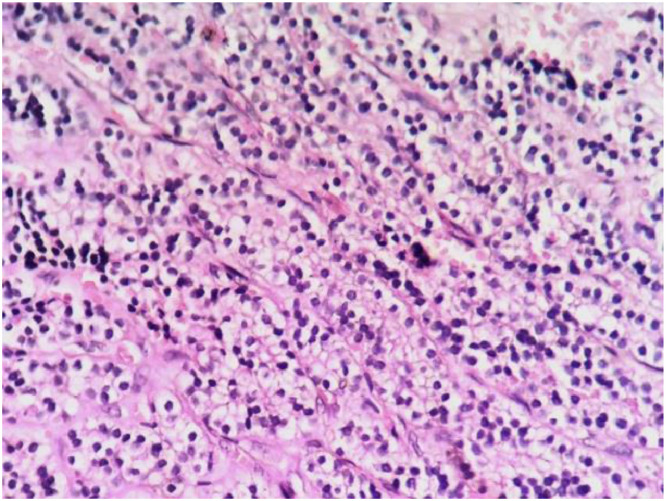
Fig. 3.
Microphotograph showing a cystic structure covered by benign tumor growth which is made of main parathyroid cells.
Fig. 4.
The tumor proliferation is made of main cells that are arranged in trabeculae and cords. Their nucleus is rounded and their cytoplasm is clear.
Discussion
Cystic parathyroid adenoma is a rare clinical and histological entity. It represents 1% to 3.3% of parathyroid pathology [1]. Sandstrom described the first parathyroid cyst in 1880 [3], and Goris reported the first successful resection of a parathyroid cyst in 1905 [4]. Parathyroid cysts are seen at any age but are most often discovered in the fourth to sixth decades of life [5]. They are asymptomatic and mostly discovered incidentally [2]. Nevertheless, cases of dysphagia, recurrent paralysis, and thrombosis of innominate veins are described in the literature, related to compression of adjacent structures by giant cysts [6].
The majority of cysts are non-secreting. Secreting parathyoid cysts were reported in the literature in 10% to 15% of cases, in which patients presented with signs of primary hyperparathyroidism with high blood levels of PTH [7]. Nonfunctional cysts are 2.5 times more common in women than in men, whereas functional cysts are 1.6 times more common in men than in women [8].
Various causes have been suspected to explain the development of parathyroid cysts: degeneration or hemorrhage of a parathyroid gland or adenoma leading to active cysts [9]; abnormal development of embryological residues [10]; retention of secretion in colloid vesicles or enlargement of microcysts by retention leading to inactive cysts with clear fluid [11].
Ultrasound is the first-line imaging investigation for the exploration of neck masses, and it confirms the cystic nature of the mass. Fine needle ultrasound-guided puncture allows the determination of PTH in the fluid and therefore confirms its parathyroid origins [12]. The high level of PTH in the fluid does not mean that the cyst is active [13]. Only a blood test can distinguish between an active and an inactive cyst.
CT and MRI should be performed in cases of solitary neck cystic where ultrasound and ultrasound-guided puncture cannot provide a precise diagnosis. Differential diagnoses include thyroglossal duct cyst, brachial cleft cyst, and parathyroid carcinoma [14].
Dual-phase 99m Tc sestamibi parathyroid scintigraphy may be positive in some patients [15] but may be negative even in functional parathyroid glands with high intra-cystic PTH levels, depending on the amount of covered parathyroid tissue.
The histopathologic features of the parathyroid cyst are usually a thin layer of cuboidal or columnar epithelium that stains positively with glycogen, which forms the cystic mucosa. The presence of parathyroid tissue in the cyst wall confirms the diagnosis [14].
Besides its diagnostic role, ultrasound can be used to perform ultrasound-guided puncture in the treatment of inactive cysts, but recurrence is often possible. In this case, intra-cystic injection of a sclerosing agent is a treatment option [7]. Functional parathyroid cysts are treated with surgical resection. The procedure consists of resection of the cyst and part of the adjacent parathyroid [16].
Conclusion
The diagnosis of cystic adenoma of the parathyroid gland is rarely made and must be based primarily on ultrasound features and on parathormone levels in the fluid.
Patient consent statement
The patient agreed with a written informed consent to anonymously publish medical information.
Footnotes
Competing Interests: There is no conflict of interest to declare.
References
- 1.Delaunay T, Peillon C, Manouvrier JL, Deotto JF, Doucet J, Nicaise JM, et al. Parathyroid cysts. A report of six cases. Ann Chir. 1990;44:231–235. [PubMed] [Google Scholar]
- 2.Chaffanjon1 P.C.J, Cardin N, et al. Parathyroid cysts. Ann Chir. 2001;126:456–458. doi: 10.1016/s0003-3944(01)00530-2. [DOI] [PubMed] [Google Scholar]
- 3.Sandstrom I. Om en ny körtel hos människan och åtskilliga däggdjur. Uppsala Lakarforenings Forhandlingar. 1880;15:441–471. [Google Scholar]
- 4.Goris D. Removal of three cystic parathyroid lobules. Ann Soc Belge Chir. 1905;5:394–400. [Google Scholar]
- 5.Safran D. Functioning parathyroid cyst. South Med J. 1998;91:978–980. doi: 10.1097/00007611-199810000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Ramos-Gabatin A, Young RL, Schenk D. Parathyroid cyst: medical diagnosis and therapy. South Med J. 1982;75:1138–1140. [PubMed] [Google Scholar]
- 7.Akel M, Salti I, Azar ST. Successful treatment of parathyroid cyst using ethanol sclerotherapy. Am J Med Sci. 1999;317:50–52. doi: 10.1097/00000441-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Gurbuz AT, Peetz ME. Giant mediastinal parathyroid cyst: an unusual cause of hypercalcemic crisis—case report and review of the literature. Surgery. 1996;120:795–800. doi: 10.1016/s0039-6060(96)80086-9. [DOI] [PubMed] [Google Scholar]
- 9.Garin E, Le Gall F, Sevestre H, Le Clech G. Latent forms of parathyroid cysts. Report of two cases. Ann Pathol. 1994;14:415–418. [PubMed] [Google Scholar]
- 10.Spitz AF. Management of a functioning mediastinal parathyroid cyst. J Clin Endocrinol Metab. 1995;80:2866–2868. doi: 10.1210/jcem.80.10.7559866. [DOI] [PubMed] [Google Scholar]
- 11.Calandra DB, Shah KH, Prinz RA, Sullivan H, Hofmann C, Oslapas R. Parathyroid cysts: a report of eleven cases including two associated with hyperparathyroid crisis. Surgery. 1983;94:887–892. [PubMed] [Google Scholar]
- 12.Nozeran S, Duquenne M, Guyetant S, Rodien P, Rohmer V, Ronceray J. Diagnosis of parathyoid cyst: value of parathormon level in puncture fluid. Presse Med. 2000;13:939–941. [PubMed] [Google Scholar]
- 13.DeRaimo AJ, Kane RA, Katz JF, Rolla AP. Parathyroid cyst: diagnosis by sonography and needle aspiration. AJR. 1984:1421227–1421228. doi: 10.2214/ajr.142.6.1227. [DOI] [PubMed] [Google Scholar]
- 14.Fortson JK, Patel VG, Henderson VJ. Parathyroid cysts: a case report and review of the literature. Laryngoscope. 2001;111:1726–1728. doi: 10.1097/00005537-200110000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Wani S, Hao Z. Atypical cystic adenoma of the parathyroid gland: case report and review of the literature. Endocr Pract. 2005;11(6):389–393. doi: 10.4158/EP.11.6.389. [DOI] [PubMed] [Google Scholar]
- 16.Sanchez A, Carretto H. Treatment of a nonfunctioning parathyroid cyst with tetracycline injection. Head Neck. 1993;15:263–265. doi: 10.1002/hed.2880150317. [DOI] [PubMed] [Google Scholar]