Take-home points
• The odds ratio (OR) shows the association between test results and the presence or absence of a disease in diagnostic research studies and can be obtained from both case-control and diagnostic cohort designs.
• The OR approximates the relative risk (RR), which cannot be obtained from the case-control design, when the disease prevalence in the population of interest is very low.
• The hazard ratio (HR) shows the association between test results and the events occurring over time and contextualizes the RR of the events in a time-to-event analysis.
• Reporting OR and HR should include a clear definition of events, a specification of the reference category for categorical variables, and a description of the one-unit amount for continuous variables.
The odds ratio (OR) is a statistic commonly used to show the strength of association between test results (such as imaging findings) and the presence or absence of a disease in diagnostic research studies. Similarly, the hazard ratio (HR) is frequently used in diagnostic research studies to show the association between test results and events occurring over time [1]. Although these statistics are widely used in radiology research, it is not rare to see them described or interpreted unclearly or imprecisely in diagnostic research manuscripts, particularly at the peer review stage before publication. Therefore, this article aims to promote a clearer and more accurate reporting of OR and HR in diagnostic research studies.
How to Calculate and Report OR
OR is the ratio between the odds values. Odds are defined as the probability that the event will occur divided by the probability that the event will not occur as follows:
Therefore, odds and probability are different ways of expressing the same concept—how likely it is that an event will occur?
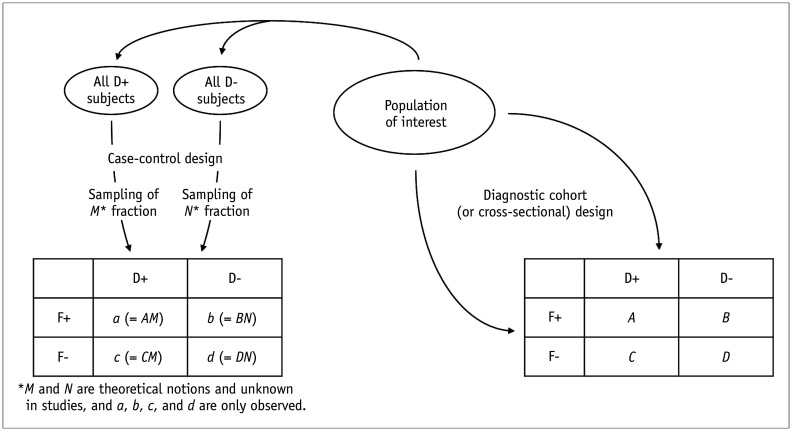
The OR can be obtained from both case-control and diagnostic cohort (or more generally referred to as cross-sectional) designs (Fig. 1). The diagnostic cohort design selects all participants together from the population of interest, whereas the case-control design selects participants based on the column variable (i.e., D+ vs. D-) in the diagnostic cross-table, as shown in Figure 1 [2,3]. Taking the diagnosis of lung cancer (D+ vs. D-) according to the findings on chest computed tomography (CT) (F+ vs. F-) as an example, the diagnostic cohort design defines the population of interest by establishing certain eligibility criteria (for example, adults aged 55 years and older with X pack-year smoking history) and recruits all patients who meet the criteria. Some of the recruited patients may have lung cancer according to the natural prevalence, and patients will have F+ and F- on chest CT according to the natural distribution of the CT findings. Therefore, all numbers (A, B, C, and D) in the diagnostic cross-table shown in Figure 1 are naturally determined. In contrast, the case-control design separately collects a certain number of participants with (case) and without (control) lung cancer, and the case-to-control ratio is arbitrarily chosen by the researchers (determined by M and N in Fig. 1). In retrospective diagnostic research studies using convenience sampling, even though the study samples are not precisely collected in a case-control manner, they may be similar to case-control samples because of the various participant selection steps involved [4].
Fig. 1. Diagnostic cross-tables showing the case-control and diagnostic cohort designs.
D+ = patients with the disease, D- = patients without the disease, F+ = patients with a finding in the test, F- = patients without a finding in the test
In the cross-tables shown in Figure 1, the investigators want to know whether and to what degree the disease is more common in patients with F+ (i.e., whether F+ would indicate a diagnosis of the disease), for which the tabulated data need to be analyzed in the horizontal direction. Odds and OR can be calculated from the diagnostic cohort design as follows:
However, in the case-control design, the corresponding odds values are not meaningful because it selects participants based on the column variable (D+ vs. D-), and the odds values depend partly on the arbitrary ratio of D+ and D- participants investigators chose to include in the study. Nevertheless, the OR is still valid in a case-control design, even though the individual odds values are not valid, as demonstrated by the calculations below.
As M and N are dropped out of the calculations, the OR calculated using the case-control design is the same as that obtained using the diagnostic cohort design. Furthermore, the OR can be calculated even if we do not know M and N.
Some items should be described transparently when reporting the OR in a research manuscript. First, a clear mention of how the odds value was defined (i.e., the odds of what) is needed to calculate the OR. In the above example, the odds of D+ was used. Second, the reference category for OR calculation must be specified for categorical variables. In the example above, the reference category is F-. If these designations are switched, that is, by using either the odds of D- instead of D+ or setting the reference category as F+ instead of F-, the OR will have a reciprocal value. Therefore, describing these items clearly will prevent confusion. Additionally, as the OR can also be calculated for a continuous variable, the one-unit amount for OR should be specified if the OR is reported for a continuous variable. For example, Yang et al. [5] reported an OR value of 2.04 for patient age in predicting malignancy in patients with hemophagocytic lymphohistiocytosis. Their results specifically mention that the OR was for every increase of 10 years. Without this explanation, readers might mistake it as an OR of 2.04 for every 1-year increase, which would erroneously make the OR for a 10-year increase 1248.25 (2.0410). Also, caution is required, when imaging or laboratory measurements have extensive or small ranges of values. For such cases, the one-unit amount for calculating OR may have been redefined for practical estimation of OR; for example, the OR per 1 × 102 or 1 × 10-2 increase in value instead of one original unit value.
When 34 original research studies reporting OR published in the Korean Journal of Radiology in 2020–2021 [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38] were evaluated against a rigorous standard (i.e., complete transparency in reporting), 91.2% (31/34) clearly mentioned how they defined the odds, 62.1% (18/29) unmistakably described the reference category for OR calculation for categorical variables, and 42.9% (9/21) specified the one-unit amount for OR for continuous variables. Therefore, there is room for improvement in reporting.
How to Interpret OR
An OR value greater than 1 in the example above indicates that the disease is more likely when the test result is F+ than F-. The greater the OR value, the more likely the patient with F+ has the disease. In this case, how can the exact OR value, for instance, an OR of 5, be interpreted? One should avoid being tempted to think that F+ patients are five times more likely to have the disease than F- patients, as such an interpretation may be incorrect. This interpretation is valid for a relative risk (RR) of 5. The RR is the ratio of probability values and can be obtained from the diagnostic cohort design as follows:
| Probability of D+ in F+ (from the diagnostic cohort design) = A/(A + B) |
| Probability of D+ in F- (from the diagnostic cohort design) = C/(C + D) |
The RR cannot be directly calculated with data from a case-control study because, unlike the OR calculation, M and N do not drop out of the RR calculation, as shown in the following equation:
When the disease prevalence is very low in the population of interest in the study, the OR, which can also be calculated from a case-control design, approximates the true RR. If the disease prevalence is very low, A must be much smaller than B, and C must be much smaller than D. In this case, the RR equation can be simplified by ignoring A and C in the respective denominators as shown below as an approximation.
It is appropriate to interpret the OR obtained from a case-control study as an approximation of RR in a setting like this. However, the assumption of very low prevalence often does not hold in diagnostic research studies.
How to Report HR
The hazard is the slope of a survival curve, which is the rate of developing events in a time period [1]. The HR is the ratio of hazards of two survival curves and essentially describes the RR of the events occurring in a survival analysis (more generally referred to as time-to-event analysis) over time [1]. Similar to the reporting of OR, a few items should be explicitly described when reporting HR in research studies. First, a clear definition of events for survival analysis should be provided. Second, the reference category for HR calculation must be clarified for categorical variables. Finally, if HR is reported for a continuous variable, the one-unit amount for HR should be specified.
When 28 original research studies reporting HR published in the Korean Journal of Radiology in 2020–2021 [11,15,32,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63] were evaluated against a rigorous standard, 96.4% (27/28) explicitly defined the events for HR, 48.1% (13/27) unmistakably described the reference category for HR calculation for categorical variables, and only 50% (10/20) clearly described the one-unit amount for HR for continuous variables. Therefore, further improvements are required.
Examples of Clear, Accurate Reporting of OR and HR
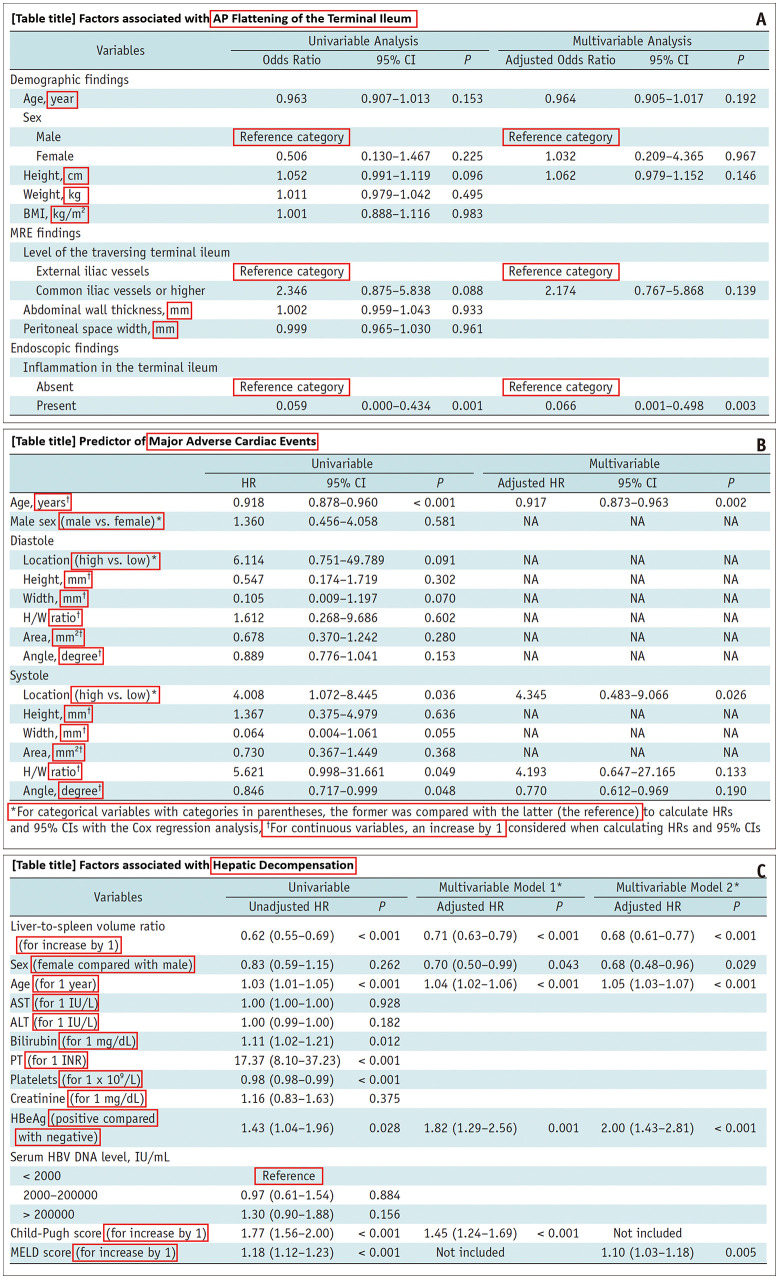
Figure 2 shows slightly different styles to clearly and accurately report OR or HR [19,41,45]. Examples can be found in other published articles [15,28,33,37,38,52,59,62].
Fig. 2. Examples of transparent, accurate reporting of odds ratio and hazard ratio.
A-C. Red rectangles indicate areas of note. (A) Modified from Kim et al. Korean J Radiol 2021;22:1640-1649, with permission of the Korean Society of Radiology [19]. (B) Modified from Kim et al. Korean J Radiol 2022;23:172-179, with permission of the Korean Society of Radiology [41]. (C) Modified from Kwon et al. Korean J Radiol 2021;22:1985-1995, with permission of the Korean Society of Radiology [45].
Conclusion
Further efforts to report OR and HR more clearly and accurately in research manuscripts, as explained in this article, would facilitate a more effective delivery of scientific information.
Footnotes
Conflicts of Interest: Seong Ho Park and Kyunghwa Han who are on the editorial board of the Korean Journal of Radiology were not involved in the editorial evaluation or decision to publish this article.
Funding Statement: None
Availability of Data and Material
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
References
- 1.Park SH, Han K, Park SY. Mistakes to avoid for accurate and transparent reporting of survival analysis in imaging research. Korean J Radiol. 2021;22:1587–1593. doi: 10.3348/kjr.2021.0579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park SH. Diagnostic case-control versus diagnostic cohort studies for clinical validation of artificial intelligence algorithm performance. Radiology. 2019;290:272–273. doi: 10.1148/radiol.2018182294. [DOI] [PubMed] [Google Scholar]
- 3.Park SH, Choi J, Byeon JS. Key principles of clinical validation, device approval, and insurance coverage decisions of artificial intelligence. Korean J Radiol. 2021;22:442–453. doi: 10.3348/kjr.2021.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park SH, Han K. Methodologic guide for evaluating clinical performance and effect of artificial intelligence technology for medical diagnosis and prediction. Radiology. 2018;286:800–809. doi: 10.1148/radiol.2017171920. [DOI] [PubMed] [Google Scholar]
- 5.Yang X, Lu X, Liu J, Kan Y, Wang W, Zhang S, et al. Development and validation of 18F-FDG PET/CT-based multivariable clinical prediction models for the identification of malignancy-associated hemophagocytic lymphohistiocytosis. Korean J Radiol. 2022;23:466–478. doi: 10.3348/kjr.2021.0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi BH, Ko SM, Shin JK, Chee HK, Kim JS. The association between morphological and functional characteristics of the bicuspid aortic valve and bicuspid aortopathy. Korean J Radiol. 2021;22:890–900. doi: 10.3348/kjr.2020.0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tang G, An X, Xiang H, Liu L, Li A, Lin X. Automated breast ultrasound: interobserver agreement, diagnostic value, and associated clinical factors of coronal-plane image features. Korean J Radiol. 2020;21:550–560. doi: 10.3348/kjr.2019.0525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim MY, Park EA, Lee W, Lee SP. Cardiac magnetic resonance feature tracking in aortic stenosis: exploration of strain parameters and prognostic value in asymptomatic patients with preserved ejection fraction. Korean J Radiol. 2020;21:268–279. doi: 10.3348/kjr.2019.0441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung HK, Kim JY, Lee MS, Lee JY, Park JS, Hyun M, et al. Characteristics of COVID-19 patients who progress to pneumonia on follow-up chest radiograph: 236 patients from a single isolated cohort in Daegu, South Korea. Korean J Radiol. 2020;21:1265–1272. doi: 10.3348/kjr.2020.0564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang HS, Park JJ. Circularity index on contrast-enhanced computed tomography helps distinguish fat-poor angiomyolipoma from renal cell carcinoma: retrospective analyses of histologically proven 257 small renal tumors less than 4 cm. Korean J Radiol. 2021;22:735–741. doi: 10.3348/kjr.2020.0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hong EK, Choi SH, Shin DJ, Jo SW, Yoo RE, Kang KM, et al. Comparison of genetic profiles and prognosis of high-grade gliomas using quantitative and qualitative MRI features: a focus on G3 gliomas. Korean J Radiol. 2021;22:233–242. doi: 10.3348/kjr.2020.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong W, Kim MJ, Lee SM, Ha HI, Park HC, Yeo SG. Computed tomography findings associated with treatment failure after antibiotic therapy for acute appendicitis. Korean J Radiol. 2021;22:63–71. doi: 10.3348/kjr.2019.0823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hong W, Yoon SH, Goo JM, Park CM. Cone-beam CT-guided percutaneous transthoracic needle lung biopsy of juxtaphrenic lesions: diagnostic accuracy and complications. Korean J Radiol. 2021;22:1203–1212. doi: 10.3348/kjr.2020.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahn Y, Yun SC, Lee SS, Son JH, Jo S, Byun J, et al. Development and validation of a simple index based on non-enhanced CT and clinical factors for prediction of non-alcoholic fatty liver disease. Korean J Radiol. 2020;21:413–421. doi: 10.3348/kjr.2019.0703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim NH, Lee SR, Kim YH, Kim HJ. Diagnostic performance and prognostic relevance of FDG positron emission tomography/computed tomography for patients with extrahepatic cholangiocarcinoma. Korean J Radiol. 2020;21:1355–1366. doi: 10.3348/kjr.2019.0891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kang C, Shin HJ, Yoon H, Han JW, Lyu CJ, Lee MJ. Differentiation between clear cell sarcoma of the kidney and Wilms’ tumor with CT. Korean J Radiol. 2021;22:1185–1193. doi: 10.3348/kjr.2020.0882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jeong DY, Kang TW, Min JH, Song KD, Lee MW, Rhim H, et al. Effect of perfluorobutane microbubbles on radiofrequency ablation for hepatocellular carcinoma: suppression of steam popping and its clinical implication. Korean J Radiol. 2020;21:1077–1086. doi: 10.3348/kjr.2019.0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dong YJ, Liu ZH, Zhou JQ, Zhan WW. Efficacy of lauromacrogol injection for ablation of benign predominantly cystic thyroid nodules and related factors: a prospective study. Korean J Radiol. 2022;23:479–487. doi: 10.3348/kjr.2020.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim DW, Park SH, Lee JS, Kim HJ, Kim AY, Ye BD, et al. Flattening in the anteroposterior direction of the terminal ileum or sigmoid colon lying across the psoas muscle on magnetic resonance enterography in patients with Crohn’s disease. Korean J Radiol. 2021;22:1640–1649. doi: 10.3348/kjr.2020.1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu CC, Cheung YC, Ueng SH, Chen SC. Impact of non-calcified specimen pathology on the underestimation of malignancy for the incomplete retrieval of suspicious calcifications diagnosed as flat epithelial atypia or atypical ductal hyperplasia by stereotactic vacuum-assisted breast biopsy. Korean J Radiol. 2020;21:1220–1229. doi: 10.3348/kjr.2019.0786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ha JY, Choi YH, Cho YJ, Lee S, Lee SB, Choi G, et al. Incidence and risk factors of nausea and vomiting after exposure to low-osmolality iodinated contrast media in children: a focus on preparative fasting. Korean J Radiol. 2020;21:1178–1186. doi: 10.3348/kjr.2019.0835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ha J, Park SH, Son JH, Kang JH, Ye BD, Park SH, et al. Is the mixed use of magnetic resonance enterography and computed tomography enterography adequate for routine periodic follow-up of bowel inflammation in patients with Crohn’s disease? Korean J Radiol. 2022;23:30–41. doi: 10.3348/kjr.2021.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim SJ, Koo HJ, Cho MS, Nam GB, Kang JW, Yang DH. Late gadolinium enhancement of left ventricular papillary muscles in patients with mitral regurgitation. Korean J Radiol. 2021;22:1609–1618. doi: 10.3348/kjr.2020.1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang YW, Kang HM, Lee EJ. Long-term follow-up ultrasonographic findings of intrathyroidal thymus in children. Korean J Radiol. 2020;21:1248–1255. doi: 10.3348/kjr.2019.0973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shin HS, Na DG, Paik W, Yoon SJ, Gwon HY, Noh BJ, et al. Malignancy risk stratification of thyroid nodules with macrocalcification and rim calcification based on ultrasound patterns. Korean J Radiol. 2021;22:663–671. doi: 10.3348/kjr.2020.0381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park H, Kim BM, Baek JH, Kim JH, Heo JH, Kim DJ, et al. Predictors of good outcomes in patients with failed endovascular thrombectomy. Korean J Radiol. 2020;21:582–587. doi: 10.3348/kjr.2019.0578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim JH, Park KJ, Kim MH, Kim JK. Preoperative assessment of renal sinus invasion by renal cell carcinoma according to tumor complexity and imaging features in patients undergoing radical nephrectomy. Korean J Radiol. 2021;22:1323–1331. doi: 10.3348/kjr.2020.0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoon J, Kim EK, Kim MJ, Moon HJ, Yoon JH, Park VY. Preoperative magnetic resonance imaging features associated with positive resection margins in patients with invasive lobular carcinoma. Korean J Radiol. 2020;21:946–954. doi: 10.3348/kjr.2019.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cha DI, Jang KM, Kim SH, Kim YK, Kim H, Ahn SH. Preoperative prediction for early recurrence can be as accurate as postoperative assessment in single hepatocellular carcinoma patients. Korean J Radiol. 2020;21:402–412. doi: 10.3348/kjr.2019.0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim J, Albakheet SS, Han K, Yoon H, Lee MJ, Koh H, et al. Quantitative MRI assessment of pancreatic steatosis using proton density fat fraction in pediatric obesity. Korean J Radiol. 2021;22:1886–1893. doi: 10.3348/kjr.2020.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kwon C, Kang KM, Choi YH, Yoo RE, Sohn CH, Han SS, et al. Renal safety of repeated intravascular administrations of iodinated or gadolinium-based contrast media within a short interval. Korean J Radiol. 2021;22:1547–1554. doi: 10.3348/kjr.2020.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salguero J, Gómez-Gómez E, Valero-Rosa J, Carrasco-Valiente J, Mesa J, Martin C, et al. Role of multiparametric prostate magnetic resonance imaging before confirmatory biopsy in assessing the risk of prostate cancer progression during active surveillance. Korean J Radiol. 2021;22:559–567. doi: 10.3348/kjr.2020.0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hwang JA, Min JH, Kim SH, Choi SY, Lee JE, Moon JY. Total bilirubin level as a predictor of suboptimal image quality of the hepatobiliary phase of gadoxetic acid-enhanced MRI in patients with extrahepatic bile duct cancer. Korean J Radiol. 2022;23:389–401. doi: 10.3348/kjr.2021.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park C, Lee IS, Nam KH, Song YS, Lee TH, Han IH, et al. Transiting nerve rootlet abnormalities on MRI after lumbar laminectomy: associations with persistent postoperative pain. Korean J Radiol. 2021;22:225–232. doi: 10.3348/kjr.2020.0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Negro R, Greco G, Deandrea M, Rucco M, Trimboli P. Twelve-month volume reduction ratio predicts regrowth and time to regrowth in thyroid nodules submitted to laser ablation: a 5-year follow-up retrospective study. Korean J Radiol. 2020;21:764–772. doi: 10.3348/kjr.2019.0798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen H, Zhou L, Liao B, Cao Q, Jiang H, Zhou W, et al. Two-dimensional shear wave elastography predicts liver fibrosis in jaundiced infants with suspected biliary atresia: a prospective study. Korean J Radiol. 2021;22:959–969. doi: 10.3348/kjr.2020.0885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim SY, Cho N, Choi Y, Shin SU, Kim ES, Lee SH, et al. Ultrafast dynamic contrast-enhanced breast MRI: lesion conspicuity and size assessment according to background parenchymal enhancement. Korean J Radiol. 2020;21:561–571. doi: 10.3348/kjr.2019.0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim J, Lee KH, Cho JY, Kim J, Shin YJ, Lee KW. Usefulness of CT-guided percutaneous transthoracic needle lung biopsies in patients with suspected pulmonary infection. Korean J Radiol. 2020;21:526–536. doi: 10.3348/kjr.2019.0492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Z, Jin C, Wu CC, Liang T, Zhao H, Wang Y, et al. Association between initial chest CT or clinical features and clinical course in patients with coronavirus disease 2019 pneumonia. Korean J Radiol. 2020;21:736–745. doi: 10.3348/kjr.2020.0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zheng Y, Xiao A, Yu X, Zhao Y, Lu Y, Li X, et al. Development and validation of a prognostic nomogram based on clinical and CT features for adverse outcome prediction in patients with COVID-19. Korean J Radiol. 2020;21:1007–1017. doi: 10.3348/kjr.2020.0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim JY, Hong YJ, Han K, Lee S, Kim YJ, Choi BW, et al. Evaluation of the ostium in anomalous origin of the right coronary artery with an interarterial course using dynamic cardiac CT and implications of ostial findings. Korean J Radiol. 2022;23:172–179. doi: 10.3348/kjr.2021.0270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim EK, Lee GY, Jang SY, Chang SA, Kim SM, Park SJ, et al. The extent of late gadolinium enhancement can predict adverse cardiac outcomes in patients with non-ischemic cardiomyopathy with reduced left ventricular ejection fraction: a prospective observational study. Korean J Radiol. 2021;22:324–333. doi: 10.3348/kjr.2020.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Park C, Kim JH, Kim PH, Kim SY, Gwon DI, Chu HH, et al. Imaging predictors of survival in patients with single small hepatocellular carcinoma treated with transarterial chemoembolization. Korean J Radiol. 2021;22:213–224. doi: 10.3348/kjr.2020.0325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kwon MR, Ko ES, Park MS, Jeong WK, Hwang NY, Kim JH, et al. Impact of skeletal muscle loss and visceral obesity measured using serial CT on the prognosis of operable breast cancers in Asian patients. Korean J Radiol. 2022;23:159–171. doi: 10.3348/kjr.2020.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwon JH, Lee SS, Yoon JS, Suk HI, Sung YS, Kim HS, et al. Liver-to-spleen volume ratio automatically measured on CT predicts decompensation in patients with B viral compensated cirrhosis. Korean J Radiol. 2021;22:1985–1995. doi: 10.3348/kjr.2021.0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chung H, Kim BY, Kim HS, Kim HO, Lee JM, Woo JS, et al. Long-term clinical effects of carotid intraplaque neovascularization in patients with coronary artery disease. Korean J Radiol. 2020;21:900–907. doi: 10.3348/kjr.2019.0550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Suh YS, Choi JW, Yoon JH, Lee DH, Kim YJ, Lee JH, et al. Radiofrequency ablation using internally cooled wet electrodes in bipolar mode for the treatment of recurrent hepatocellular carcinoma after locoregional treatment: a randomized prospective comparative study. Korean J Radiol. 2021;22:1974–1984. doi: 10.3348/kjr.2021.0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kwon JH, Gwon DI, Kim JW, Chu HH, Kim JH, Ko GY, et al. Percutaneous biliary metallic stent insertion in patients with malignant duodenobiliary obstruction: outcomes and factors influencing biliary stent patency. Korean J Radiol. 2020;21:695–706. doi: 10.3348/kjr.2019.0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee SJ, Kim JH, Kim SY, Won HJ, Shin YM, Kim PN. Percutaneous radiofrequency ablation for metachronous hepatic metastases after curative resection of pancreatic adenocarcinoma. Korean J Radiol. 2020;21:316–324. doi: 10.3348/kjr.2019.0647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pak E, Choi KS, Choi SH, Park CK, Kim TM, Park SH, et al. Prediction of prognosis in glioblastoma using radiomics features of dynamic contrast-enhanced MRI. Korean J Radiol. 2021;22:1514–1524. doi: 10.3348/kjr.2020.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moon JY, Min JH, Kim YK, Cha D, Hwang JA, Ko SE, et al. Prognosis after curative resection of single hepatocellular carcinoma with a focus on LI-RADS targetoid appearance on preoperative gadoxetic acid-enhanced. Korean J Radiol. 2021;22:1786–1796. doi: 10.3348/kjr.2020.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim W, Lee SM, Lee JB, Seo JB, Kim HK, Kim J, et al. Prognosis for pneumonic-type invasive mucinous adenocarcinoma in a single lobe on CT: is it reasonable to designate it as clinical T3? Korean J Radiol. 2022;23:370–380. doi: 10.3348/kjr.2021.0465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ahn Y, Koo HJ, Kang JW, Choi WJ, Kim DH, Song JM, et al. Prognostic implication of right ventricle parameters measured on preoperative cardiac MRI in patients with functional tricuspid regurgitation. Korean J Radiol. 2021;22:1253–1265. doi: 10.3348/kjr.2020.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Park B, Park J, Lim JK, Shin KM, Lee J, Seo H, et al. Prognostic implication of volumetric quantitative ct analysis in patients with COVID-19: a multicenter study in Daegu, Korea. Korean J Radiol. 2020;21:1256–1264. doi: 10.3348/kjr.2020.0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jo SW, Choi SH, Lee EJ, Yoo RE, Kang KM, Yun TJ, et al. Prognostic prediction based on dynamic contrast-enhanced MRI and dynamic susceptibility contrast-enhanced MRI parameters from non-enhancing, T2-high-signal-intensity lesions in patients with glioblastoma. Korean J Radiol. 2021;22:1369–1378. doi: 10.3348/kjr.2020.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yoon SH, Kim E, Jeon Y, Yi SY, Bae HJ, Jang IK, et al. Prognostic value of coronary CT angiography for predicting poor cardiac outcome in stroke patients without known cardiac disease or chest pain: the assessment of coronary artery disease in stroke patients study. Korean J Radiol. 2020;21:1055–1064. doi: 10.3348/kjr.2020.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Im DJ, Hur J, Han K, Suh YJ, Hong YJ, Lee HJ, et al. Prognostic value of dual-energy CT-based iodine quantification versus conventional CT in acute pulmonary embolism: a propensity-match analysis. Korean J Radiol. 2020;21:1095–1103. doi: 10.3348/kjr.2019.0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kang Y, Hong EK, Rhim JH, Yoo RE, Kang KM, Yun TJ, et al. Prognostic value of dynamic contrast-enhanced MRI-derived pharmacokinetic variables in glioblastoma patients: analysis of contrast-enhancing lesions and non-enhancing T2 high-signal intensity lesions. Korean J Radiol. 2020;21:707–716. doi: 10.3348/kjr.2019.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim SH, Song BI, Kim HW, Won KS, Son YG, Ryu SW. Prognostic value of restaging F-18 fluorodeoxyglucose positron emission tomography/computed tomography to predict 3-year post-recurrence survival in patients with recurrent gastric cancer after curative resection. Korean J Radiol. 2020;21:829–837. doi: 10.3348/kjr.2019.0672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yoen H, Park HE, Kim SH, Yoon JH, Hur BY, Bae JS, et al. Prognostic value of tumor regression grade on MR in rectal cancer: a large-scale, single-center experience. Korean J Radiol. 2020;21:1065–1076. doi: 10.3348/kjr.2019.0797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hwang HJ, Lee SM, Seo JB, Kim JE, Choi HY, Kim N, et al. Quantitative vertebral bone density seen on chest CT in chronic obstructive pulmonary disease patients: association with mortality in the Korean obstructive lung disease cohort. Korean J Radiol. 2020;21:880–890. doi: 10.3348/kjr.2019.0551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Won SY, Park HS, Kim EK, Kim SI, Moon HJ, Yoon JH, et al. Survival rates of breast cancer patients aged 40 to 49 years according to detection modality in Korea: screening ultrasound versus mammography. Korean J Radiol. 2021;22:159–167. doi: 10.3348/kjr.2019.0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Park S, Lee JM, Park J, Lee J, Bae JS, Kim JH, et al. Volumetric CT texture analysis of intrahepatic mass-forming cholangiocarcinoma for the prediction of postoperative outcomes: fully automatic tumor segmentation versus semi-automatic segmentation. Korean J Radiol. 2021;22:1797–1808. doi: 10.3348/kjr.2021.0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.