Abstract
Introduction:
Pregnant Black women are at disproportionate risk for adverse birth outcomes, in part associated with higher prevalence of stress. Stress increases risk of depression, a known risk factor for preterm birth. In addition, multiple dimensions of stress, including perceived stress and stressful life events, are associated with adverse birth outcomes, independent of their association with prenatal depression. We use an intersectional and contextualized measure of gendered racial stress to assess whether gendered racial stress constitutes an additional dimension to prenatal depression, independent of stressful life events and perceived stress.
Methods:
In this cross-sectional study of 428 Black women, we assessed gendered racial stress (using the 39-item Jackson Hogue Phillips Reduced Common Contextualized Stress Measure), perceived stress (using the Perceived Stress Scale), and stressful life events (using a Stressful Life Event Index) as psychosocial predictors of depressive symptoms (measured by the Edinburgh Depression Scale). We used bivariate analyses and multivariable regression to assess the association between the measures of stress and prenatal depression.
Results:
Results revealed significant bivariate associations between participant scores on the full Jackson Hogue Phillips Reduced Common Contextualized Stress Measure and its 5 subscales, and the Edinburgh Depression Scale. In multivariable models that included participant Perceived Stress Scale and/or Stressful Life Event Index scores, the Jackson Hogue Phillips Reduced Common Contextualized Stress Measure contributed uniquely and significantly to Edinburgh Depression Scale score, with the burden subscale being the strongest contributor among all variables. No sociodemographic characteristics were found to be significant in multivariable models.
Conclusion:
For Black women in early pregnancy, gendered racial stress is a distinct dimension of stress associated with increased depressive symptoms. Intersectional stress measures may best uncover nuances within Black women’s complex social environment.
Keywords: depression, gendered racism, pregnancy, racial disparities, stress
Introduction
Prenatal depression, potentially associated with stress both preceding and during pregnancy, is common and poses significant health risks to pregnant women and their children.1–3 Mothers with elevated depressive symptoms during pregnancy are more likely to give birth preterm or to low birthweight infants, and to report higher psychosocial stress.3–5 In the United States, Black women are over 50% more likely to give birth preterm than White women (14.13% vs 9.09%), and more than twice as likely to deliver a low birthweight infant (14.07% vs 6.91%). 6 In addition, Black pregnant women report greater psychosocial stress than their White counterparts, in part due to social factors including racism and discrimination.7–10 Prenatal psychosocial stress, which occurs when a pregnant woman feels unable to cope with her demands, can be embodied physiologically and expressed behaviorally. 11 Among the complex mechanisms purported to underlie birth outcomes, stress-induced immune dysregulation is one pathway that has received considerable attention. 12 Research also indicates that chronic racial stress may prematurely weather Black women’s stress response, leading to increased allostatic load.13,14 Prenatal psychosocial stress, which is commonly measured with self-reported measures of stressful life events and/or perceived stress,15,16 is associated with poor birth outcomes.17–19 Specifically, adverse earlier life experiences (as measured by stressful life events inventories) and appraisal of experiences as stressful (as measured by perceived stress scales) may independently increase risk for depression,19,20 and adverse birth outcomes.19,21,22 Considerable evidence further suggests that depression-causing stress may contribute to Black-White racial disparities in adverse birth outcomes,23–28 though some mixed results suggest the link is unclear. 29 Given the potential impact of prenatal depression on Black maternal and infant health, it is critically important to identity the unique dimensions of stress that may cause depression among Black women.
The most widely used stressful life event and perceived stress instruments may not adequately assess chronic stress associated with racial discrimination, 30 and thus may not capture that integral part of American Black women’s historical and contemporary social context. 31 Researchers have found that racism is a stressor for pregnant Black women,10,32,33 and that racial stress is linked with depression and adverse birth outcomes.34–37 Moreover, for Black women, additional exposure to stress over the lifecourse may not only be due to race, but both race and gender.38–40 This type of stress—contextualized in Black women’s intersecting social identities—is known as gendered racial stress, and is brought on by gendered racism, a hybrid form of oppression.38,41,42 Gendered racial theory states that, by virtue of being both Black and women, Black women uniquely experience psychosocial stressors that go beyond reports of perceived instances of racism, 43 and which may operate independently of other known sources of stress. 8 Some studies of Black individuals have demonstrated that gender moderates the link between particular types of racism and mental health, such that women who report interpersonal racism experience worse mental health outcomes than men. 44 Compared to Black men, Black women may also experience racism via a wider range of potential sources, inclusive of microaggressions, personal slights, and invalidations. 45 Thus, gender is a salient factor in determining the impact of race-related stress on mental health. 46 Research also supports that Black women appraise experiences of gendered racism as stressful due to the simultaneous experience of racism and sexism, and not just due to one or the other. 40 Furthermore, experiences with gendered racism related to Black women’s sexuality and their gendered role as mothers are associated with greater pregnancy-specific stress. 47 Thus, it is necessary to understand the contribution of gendered racial stress to Black women’s total burden of stress.
Studies of contextualized gendered racial stress to date offer support for positive associations with psychosocial stress,39,40,43,48–54 and adverse birth outcomes among Black women.25,47 While some earlier research on gendered racism adapted unidimensional measures of sexism, 40 scholars of intersectionality theory call for the use of multidimensional measures that explore experiences of racism and sexism together, without disentangling them.39,55–62 Although empirical research on gendered racism is becoming more prevalent, only a few intersectional instruments for gendered racism exist to our knowledge, including (1) the Gendered Racial Microaggressions Scale, 48 and (2) the Jackson Hogue Phillips (JHP) Contextualized Stress Measure©. 63 Given that the JHP© was developed using a grounded theory approach in collaboration with nearly 500 metropolitan Black women, and was later validated for use in pregnancy (Cronbach’s alpha = .89), 43 that instrument was selected for use in the present Atlanta-based study. We examined the association of gendered racial stress with depression, and pose the following questions:
Among a sample of urban, socioeconomically diverse pregnant Black women, is there a significant association of gendered racial stress with depressive symptoms?
Does gendered racial stress constitute an additional dimension to stress-associated depressive symptoms beyond stressful life events and perceived stress?
Methods
Study population
This cross-sectional study uses first trimester prenatal data from the first consecutively enrolled participants in the prospective Biobehavioral Determinants of the Microbiome and Preterm Birth in Black Women study (n = 485), which aims to provide a biopsychosocial understanding of within-race risk for adverse birth outcomes among a socioeconomically diverse sample of Black women. 64 At enrollment, participants were receiving prenatal care at either Grady Memorial Hospital or Emory University Hospital Midtown—two Atlanta-area facilities (public and private, respectively) that see approximately 10% of Georgia’s singleton live births to Black women. Eligible women were between 18 and 40 years of age, identified as African-American (i.e., US-born and of African-American or Black race), were carrying a singleton pregnancy between 8 and 14 weeks’ gestation, and had no reported chronic medical conditions or conditions requiring long-term prescription management. During the baseline study visit, sociodemographic, psychosocial, and other health information was collected via self-report. This study was reviewed for ethical and safety considerations by the Internal Review Boards (IRB00068441) of both Emory University and Grady Memorial Hospital and was approved by both Boards. All participants provided written informed consent, and received financial compensation for their participation. Fifty-seven women were excluded from these analyses due to missing data on gendered racial stress and/or depression, leaving an analytic sample of 428. Sample size was based on the available data from the Biobehavioral Determinants of the Microbiome and Preterm Birth in Black Women study, for which a power analysis has been published previously. 64
Measures
Depression
The Edinburgh Depression Scale (EDS) is a 10-item self-report questionnaire ascertaining symptoms of depression in the last 7 days. 65 While originally developed for use in the postnatal period, the scale has been used and validated in studies of pregnant women and shows high sensitivity and specificity for the detection of prenatal major depressive disorder.66–68 The EDS maintains high internal consistency reliability in studies of Black pregnant populations.69,70 We summed items, coded 0 to 3, where higher scores indicate greater depressive symptomology. In our sample, scores range from 0 to 25. Using generally recommended thresholds, an EDS score ⩾ 10 indicates the presence of depressive symptomology, and a score ⩾ 13 may further indicate clinical depression.65,71,72 While some reports indicate that an EDS score of ⩾ 15 should be used antenatally, 73 studies of the EDS in urban and low-income pregnant women, and studies of prenatal depression screening across trimesters, suggest that lower cutoff scores may most effectively identify women in early pregnancy in need of diagnosis and treatment.69,74,75 Thus, we present an array of EDS score categories in our descriptions of participant characteristics, and use EDS score as a continuous variable in linear regression analyses. 76 In this sample, Cronbach’s alpha for the EDS was .85.
Gendered racial stress
To operationalize gendered racial stress, we use continuous scores from the 39-item JHP©, which we call the JHP-Reduced Common (JHP-RC©; see Supplemental Table 1). This reduced scale includes items from the original 68-item JHP63,77 that were found to be most commonly experienced by Black women who worked at one of two public hospitals and were enrolled in a federally funded worksite fitness study. 78 The JHP-RC© assesses specific exposure to chronic racial and gendered stress among Black women, and consists of four subscales measuring stressors (burden, personal history, racism, and work) and one measuring stress mediators (coping), with 5-level Likert-type scoring from greatest agreement to greatest disagreement. The burden subscale includes 10 items that measure gendered role strain, and distress due to inadequate resources to meet demands. It includes 3 of the 4 items from the original JHP Scale referred to as “stress states.”63,77 The personal history subscale includes 5 items that assess experiences with emotional, physical, and substance abuse by a family member or partner. The 5 racism items capture racial stereotypes, White privilege, and the perceived impact of racism on children’s lives. The 5-item work subscale assesses racism and sexism in the workplace. The 14 coping items measure coping resources (including support from and belonging to one’s community) and capacity for coping based on race and gender. To calculate total and subscale JHP-RC© scores, we coded items 1–5 and reverse coded items, as necessary, so higher values for each item indicated greater gendered racial stress. In our sample, total JHP-RC© score ranges from 47 to 159. Ranges for the subscales are: burden = 10–50, coping = 16–66, personal history = 3–25, racism = 4–25, and work = 2–25. Confirmatory factor analysis (CFA) was conducted on the JPH-RC©. The hypothesized factor structure was found to be an adequate fit to our data (root mean square error of approximation = 0.042, comparative fit index = 0.93, and Tucker–Lewis index = 0.91). Cronbach’s alpha coefficient for the full JHP-RC© was .86 in the present study. The subscales had the following alpha coefficients: burden = .84, coping = .82, personal history = .87, racism = .75, and work = .82. These values indicate acceptable to high internal reliability consistency.
Covariates
We considered sociodemographic and psychosocial health covariates. Along with gendered racial stress, the psychosocial factors are independent variables, considered covariables for the purpose of determining the independent association of gendered racism to psychosocial risks. Psychosocial health factors include:
Perceived stress: Cohen’s 14-item Perceived Stress Scale (PSS) assesses “the degree to which individuals appraise situations in their lives as stressful” over the last month. 79 We summed items, coded 0 to 4, where higher values indicate greater perceived stress. In our sample, scores ranged from 0 to 45. The PSS is among the most widely used instruments of perceived stress, and demonstrates acceptable internal consistency in this sample (Cronbach’s alpha = .72).
Stressful life events: A 13-item Stressful Life Events Inventory (SLEI) assessed whether particular life events (e.g. death of a loved one, loss of home, loss of employment) had occurred over the life course. 80 We scored stressful life events dichotomously as either present (1) or absent (0), and computed an index by summing the total number of events present (range: 0–12, in our sample). Cronbach’s alpha in this sample was .74.
Sociodemographic factors include:
Age (years).
Education: participants reported whether they had completed less than high school, high school, some college, or college graduate or more (coded 0, 1, 2, or 3, respectively). For adjusted regression analyses, we used dummy coding, with “less than high school” as the referent group.
Insurance status: participants reported whether they were privately or publicly insured (i.e., receiving Medicaid). We coded these responses as either 0 (public insurance) or 1 (private insurance).
Relationship status: participants reported whether or not they were married or cohabiting. We coded these responses as either 0 (not married or cohabiting) or 1 (married or cohabiting).
Statistical analyses
We performed preliminary testing to check for the conditions required for our statistical analyses (e.g., normally distributed dependent variable and absence of multicollinearity); results indicated that analytic assumptions were met. Using univariate analyses, we tabulated descriptive statistics for all variables of interest among the analytic dataset and, separately, among participants excluded from our analyses due to missing data. We conducted a sensitivity analysis to determine whether there were any statistically significant differences in variables of interest between included and excluded participants. For the included sample, we assessed bivariate relationships between JHP-RC© scores, EDS scores, and all covariates, using Pearson correlation coefficients, t-tests, or analyses of variance (ANOVAs). We used simple linear regression to assess the association between scores on each psychosocial measure of stress (PSS, SLEI, and JHP-RC©) and depressive symptoms. We then used stepwise regression to estimate any additional variance in depressive symptoms explained by the inclusion of additional psychosocial data (particularly, JHP-RC© data) and covariates. We included all covariates significantly associated with JHP-RC© score or EDS score on the bivariate level. Finally, in order to identify a parsimonious model that explained the most variance in depression, we performed stepwise backward elimination, in which a model including all psychosocial and sociodemographic data was reduced to include only those variables with a statistically significant contribution to the model. These regression analyses were repeated separately for each of the five JHP-RC© subscales (burden, coping, personal history, racism, and work). In addition to parameter estimates, we report standardized estimates, which remove the units of measurement, given that our dependent and independent psychosocial variables are scored on different scales. We considered p ⩽ 0.05 statistically significant on two-tailed tests. CFA was conducted using Stata SE 17.0, and we used SAS 9.4 for all other analyses.
Results
Descriptive and bivariate analyses
We present characteristics of our analytic sample of 428 Black women in early pregnancy (8–14 weeks’ gestation) in Table 1. Mean (SD) age was 25 (4.8) years. Across education categories, the highest proportion of participants (38.6%) completed high school only. Nearly 80% were insured through Medicaid during pregnancy, and nearly 50% were married or cohabiting. In all, 53.7% had previously given birth. Mean JHP-RC© score was 95.6 (20.5). Mean EDS score was 7.2 (5.5), with about 31% of participants scoring 10 or higher. Mean PSS and SLEI scores were 23.6 (7.5) and 4.0 (2.7), respectively. Relationship status was the only characteristic for which there was a significant difference between the 428 included and 57 excluded participants (Chi-square = 7.4, p < .01; Supplemental Table 2). Among participants excluded from analysis due to missing data, 68.4% were married or cohabiting.
Table 1.
Characteristics of Atlanta-area Black women in the study sample (N = 428).
| Mean (SD) | n (%) | |
|---|---|---|
| Sociodemographic factors | ||
| Age | 25.0 (4.8) | |
| Education | ||
| Less than high school | 71 (16.6) | |
| High school | 165 (38.6) | |
| Some college | 120 (28.0) | |
| College graduate or more | 72 (16.8) | |
| Insurance status | ||
| Public (Medicaid) | 342 (79.9) | |
| Private | 86 (20.1) | |
| Parity | 0.9 (1.0) | |
| 0 | 198 (46.3) | |
| ⩾1 | 230 (53.7) | |
| Relationship status | ||
| Married or cohabiting | 211 (49.3) | |
| Not married or cohabiting | 217 (50.7) | |
| Psychosocial factors | ||
| JHP-RC©a | 95.6 (20.5) | |
| Burden | 28.3 (8.4) | |
| Coping | 33.0 (8.9) | |
| Personal History | 10.5 (5.4) | |
| Racism | 13.3 (4.5) | |
| Work | 10.5 (4.1) | |
| EDS a | 7.2 (5.5) | |
| 0–9 | 295 (68.9) | |
| 10–12 | 53 (12.4) | |
| 13–14 | 29 (6.8) | |
| ⩾15 | 51 (11.9) | |
| PSSa, b | 23.6 (7.5) | |
| SLEIa, b | 4.0 (2.7) | |
JHP-RC©: 39-item Jackson Hogue Phillips Reduced Common Contextualized Stress Measure; EDS: 10-item Edinburgh Depression Scale; PSS: 14-item Perceived Stress Scale; SLEI: 13-item Stressful Life Events Index.
Variable (n, % missing): PSS (13, 3.0%), SLEI (6, 1.4%). There were no missing data for variables without this superscript.
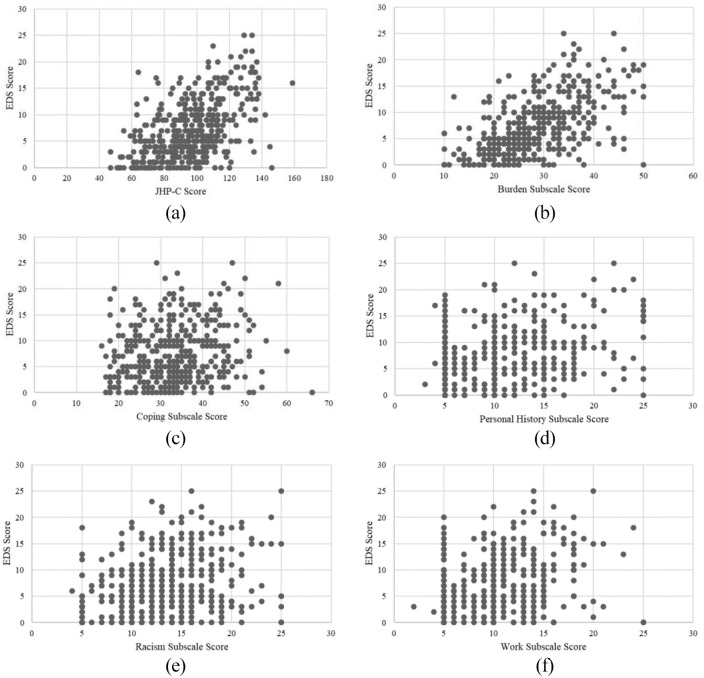
Scatterplots in Figure 1 illustrate the relationships between the EDS, the JHP-RC©, and its subscales. The full JHP-RC© and EDS were moderately correlated (r = .53, p < .0001). EDS score was significantly correlated with each of the JHP-RC© subscales; Pearson correlation coefficients (r) ranged from .21 (coping) to .58 (burden). In Table 2, we compare mean JHP-RC© scores (full and subscale) across EDS score categories. Given no statistically significant differences in mean JHP-RC© or any of its subscales between the 13–14 and ⩾ 15 EDS score categories (Supplemental Table 3), we present mean JHP-RC scores across 3 EDS score categories: 0–9, 10–12, and ⩾13. In general, full and subscale JHP-RC© scores increased as EDS score increased. F-tests for overall differences in JHP-RC© score across EDS categories were each statistically significant (p-values < .0001; data not shown). For the JHP-RC© and all subscales, mean scores in the highest EDS score category (⩾13) were statistically significantly higher than mean scores in the lowest EDS score category (0–9). For the full JHP-RC©, and its burden and personal history subscales, mean scores across the 3 EDS score categories were all statistically significantly different from each other. The differences in mean gendered racial stress between the highest and lowest EDS score category were as follows: JHP-RC©= 24.4; burden = 10.4, coping = 4.1, personal history = 4.3, racism =2.7, and work = 2.8.
Figure 1.
Correlations of the Edinburgh Depression Scale (EDS) with the full Jackson Hogue Phillips Reduced Common Contextualized Stress Measure (JHP-RC) and JHP-RC subscales. EDS Scores are along the horizontal axis, and gendered racial stress scores are along the vertical axis. The correlation of the full JHP-RC is shown in panel A. Panels B-F show correlations with the five JHP-RC subscales: burden, coping, personal history, racism, and work. (a) JHP-RC©: r = .53, p < .0001. (b) Burden: r = .58, p < .0001. (c) Coping: r = .21, p < .0001. (d) Personal history: r = .34, p < .0001. (e) Racism: r = .24, p < .0001. (f) Work: r = .29, p < .0001.
Table 2.
Mean full and subscale-specific Jackson Hogue Phillips Reduced Common Contextualized Stress Measure (JHP-RC©) scores across Edinburgh Depression Scale (EDS) score categories (3 levels).
| Mean (standard deviation) |
||||||
|---|---|---|---|---|---|---|
| JHP-RC© | Burden | Coping | Personal history | Racism | Work | |
| EDS score category | ||||||
| 0–9 | 89.7 b c (18.4) | 25.8
b
c
(7.4) |
32.0
c
(8.9) |
9.5
b
c
(4.9) |
12.7
c
(4.6) |
9.7
b
c
(3.8) |
| 10–12 | 100.3 a c (17.0) | 30.7
a
c
(6.3) |
33.3 (7.7) |
11.4
a
c
(5.0) |
13.5
c
(3.7) |
11.4
a
(3.9) |
| ⩾13 | 114.1
a
b
(18.2) |
36.2
a
b
(7.9) |
36.1
a
(9.1) |
13.8
a
b
(6.2) |
15.4
a
b
(4.1) |
12.5
a
(4.5) |
Significantly different (p ⩽ .05) from the mean JHP-RC© score (full or domain-specific) in the 0-9 EDS score category.
Significantly different (p ⩽ .05) from the mean JHP-RC© score (full or domain-specific) in the 10-12 EDS score category.
Significantly different (p ⩽ .05) from the mean JHP-RC© score (full or domain-specific) in the ⩾ 13 EDS score category.
In Table 3, we show Pearson’s correlation coefficients between the JHP-RC© and its subscales, the PSS, and SLEI. The JHP-RC© and all subscales were positively and significantly (p < .05) correlated with the PSS. The full scale showed the strongest correlation with the PSS (r = .50), with burden being the most strongly correlated of the subscales (r = .47). The burden subscale measures gendered role strain, and distress due to inadequate resources to meet demands (e.g. “I am taking care of everyone else, but no one is taking care of me”). The full JHP-RC© and all subscales were positively correlated with the SLEI; however, neither the coping nor work subscales were significantly correlated with the SLEI. Of the statistically significant relationships with the SLEI, the personal history subscale showed the strongest correlation (r = .40). The PSS and SLEI were moderately correlated (r = .23, p < .0001).
Table 3.
Pearson’s correlation coefficients for the Jackson Hogue Phillips Reduced Common Contextualized Stress Measure (JHP-RC©) and its subscales with the Perceived Stress Scale (PSS) and Stressful Life Events Index (SLEI).
| PSS | SLEI | |
|---|---|---|
| Total JHP-RC© | 0.50 <.0001 n = 415 |
0.33 <.0001 n = 422 |
| Burden | 0.47 <.0001 n = 415 |
0.34 <.0001 n = 422 |
| Coping | 0.31 <.0001 n = 415 |
0.07 n.s. n = 422 |
| Personal history | 0.30 <.0001 n = 415 |
0.40 <.0001 n = 422 |
| Racism | 0.16 <.001 n = 415 |
0.15 <.01 n = 422 |
| Work | 0.29 <.0001 n = 415 |
0.07 n.s. n = 422 |
| PSS | 1.00 n = 415 |
0.23 <.0001 n = 410 |
n.s. connotes not statistically significant at p ⩽ .05.
Regression analyses
In simple linear regression (Table 4), JHP-RC© score explained 27% of the variance in EDS; perceived stress explained 45% of the variation in EDS score. Because none of the sociodemographic covariates contributed significantly to any of the models to which they were added, our final model included only JHP-RC score, SLEI score, and PSS Score. The final model explained 52% of the variance in EDS score. As shown by the standardized estimates, for every 1-standard deviation increase in JHP-RC© score, EDS score increases by .22 standard deviations, with all other variables held constant. This increase is higher than the contribution of a 1-standard deviation increase in SLEI score (standardized b = .17), but lower than the contribution of a 1-standard deviation increase in PSS score (standardized b = .52).
Table 4.
Regression analysis models for depressive symptoms (measured by the Edinburgh Depression Scale) and the full Jackson Hogue Phillips Reduced Common Contextualized Stress Measure (JHP-RC©).
| Model parameter(s) | R2 | Standardized estimate | Parameter estimate (standard error) |
Parameter estimate 95% CI | p-value | |
|---|---|---|---|---|---|---|
| JHP-RC© only model | JHP-RC©a | 0.27 | 0.53 | 0.14 (0.01) | 0.12, 0.16 | <.0001 |
| PSS only model | PSS a | 0.45 | 0.67 | 0.49 (0.03) | 0.44, 0.54 | <.0001 |
| SLEI only model | SLEI a | 0.13 | 0.36 | 0.74 (0.09) | 0.55, 0.93 | <.0001 |
| SLEI & PSS model | SLEI | 0.49 | 0.22 | 0.45 (0.07) | 0.30, 0.59 | <.0001 |
| PSS | 0.62 | 0.45 (0.03) | 0.40, 0.51 | <.0001 | ||
| Stepping JHP-RC© into SLEI model | JHP-RC© | 0.32 | 0.46 | 0.12 (0.01) | 0.10, 0.15 | <.0001 |
| SLEI | 0.21 | 0.43 (0.09) | 0.26, 0.60 | <.0001 | ||
| Stepping JHP-RC© into PSS model | JHP-RC© | 0.50 | 0.27 | 0.07 (0.01) | 0.05, 0.09 | <.0001 |
| PSS | 0.54 | 0.39 (0.03) | 0.34, 0.45 | <.0001 | ||
| Stepping JHP-RC© into SLEI + PSS model | JHP-RC© | 0.53 | 0.22 | 0.06 (0.01) | 0.03, 0.08 | <.0001 |
| SLEI | 0.17 | 0.35 (0.07) | 0.21, 0.50 | <.0001 | ||
| PSS | 0.52 | 0.38 (0.03) | 0.32, 0.44 | <.0001 | ||
| Stepping covariates into SLEI + JHP-RC© model | JHP-RC© | 0.34 | 0.47 | 0.13 (0.01) | 0.10, 0.15 | <.0001 |
| SLEI | 0.22 | 0.46 (0.09) | 0.28, 0.64 | <.0001 | ||
| Age | –0.11 | −0.12 (0.06) | −0.23, –0.02 | 0.02 | ||
| Education
b
(Level 2 vs. Level 1) |
0.01 | 0.13 (0.66) | −1.2, 1.4 | n.s. | ||
| Education
b
(Level 3 vs. Level 1) |
0.06 | 0.73 (0.71) | −0.66, 2.12 | n.s. | ||
| Education
b
(Level 4 vs. Level 1) |
–0.06 | −0.91 (0.87) | −2.61, 0.80 | n.s. | ||
| Parity | –0.003 | −0.04 (0.47) | −0.97, 0.89 | n.s. | ||
| Stepping covariates into PSS + JHP-RC© model | JHP-RC© | 0.50 | 0.26 | 0.07 (0.01) | 0.05, 0.09 | <.0001 |
| PSS | 0.54 | 0.39 (0.03) | 0.33, 0.46 | <.0001 | ||
| Age | –0.02 | −0.02 (0.05) | −0.12, 0.07 | n.s. | ||
| Education
b
(Level 2 vs. Level 1) |
–0.01 | −0.11 (0.57) | −1.23, 1.00 | n.s. | ||
| Education
b
(Level 3 vs. Level 1) |
0.06 | 0.83 (0.61) | −0.37, 2.03 | n.s. | ||
| Education
b
(Level 4 vs. Level 1) |
0.01 | 0.28 (0.75) | −1.19, 1.76 | n.s. | ||
| Parity | 0.05 | 0.44 (0.41) | −0.37, 1.25 | n.s. | ||
| Stepping covariates into SLEI + PSS + JHP-RC© model | JHP-RC© | 0.53 | 0.21 | 0.06 (0.01) | 0.04, 0.08 | <.0001 |
| SLEI | 0.18 | 0.36 (0.08) | 0.19, 0.50 | <.0001 | ||
| PSS | 0.52 | 0.38 (0.03) | 0.31, 0.43 | <.0001 | ||
| Age | –0.04 | −0.05 (0.04) | −0.11, 0.07 | n.s. | ||
| Education
b
(Level 2 vs. Level 1) |
0.01 | 0.13 (0.57) | −1.08, 1.16 | n.s. | ||
| Education
b
(Level 3 vs. Level 1) |
0.05 | 0.66 (0.61) | −0.66, 1.81 | n.s. | ||
| Education
b
(Level 4 vs. Level 1) |
0.01 | 0.19 (0.75) | −1.58, 1.65 | n.s. | ||
| Parity | 0.06 | 0.66 (0.41) | −0.15, 1.47 | n.s. | ||
| Backward regression | JHP-RC© | 0.53 | 0.22 | 0.06 (0.01) | 0.04, 0.08 | <.0001 |
| SLEI | 0.17 | 0.35 (0.07) | 0.21, 0.50 | <.0001 | ||
| PSS | 0.52 | 0.38 (0.03) | 0.33, 0.44 | <.0001 |
JHP-RC©: 39-item Jackson Hogue Phillips Reduced Common Contextualized Stress Measure; PSS: 14-item Perceived Stress Scale; SLEI: 13-item Stressful Life Events Index.
Levels of education: 1 = less than high school, 2 = high school, 3 = some college, 4 = college graduate or more.
n.s. connotes not statistically significant at p ⩽ .05.
Table 5 shows regression analyses for each JHP-RC© subscale. In simple linear regression, each subscale explained between 4% (coping) and 34% (burden) of the variance in EDS score. For each subscale, multivariable modeling with backward selection identified stressful life events and perceived stress, but no sociodemographic covariates, as significant covariates in the relationship between JHP-RC© and EDS score. Coping was the only subscale that was not retained in backward selection model. When the burden subscale was added to a model that included SLEI and PSS scores (R2 = .49, p < .0001; Table 4), R2 increased from .49 to .56 (p < .0001). In separate models, coping, personal history, racism, and work increased the explanation of variance in depressive symptoms by 0 to 1 percentage points (as compared to the model that only included stressful life events and perceived stress).
Table 5.
Unadjusted and adjusted backward regression models for depressive symptoms (measured by the Edinburgh Depression Scale) and Jackson Hogue Phillips Reduced Common Contextualized Stress Measure (JHP-RC©) subscales.
| JHP-RC© subscale | Model parameter(s) | R2 | Standardized estimate | Parameter estimate (standard error) | Parameter estimate 95% CI |
p-value |
|---|---|---|---|---|---|---|
| Burden | Burden only | .34 | 0.58 | 0.38 (0.03) | 0.33, 0.43 | <.0001 |
| Adjusted model: | .56 | |||||
| Burden | 0.30 | 0.20 (0.03) | 0.15, 0.25 | <.0001 | ||
| SLEI a | 0.14 | 0.30 (0.07) | 0.15, 0.44 | <.0001 | ||
| PSS a | 0.49 | 0.36 (0.03) | 0.31, 0.42 | <.0001 | ||
| Coping | Coping only | .04 | 0.21 | 0.13 (0.02) | 0.07, 0.18 | <.0001 |
| Adjusted model: | .49 | |||||
| Coping b | 0.007 | 0.004 (0.02) | –0.04, 0.04 | n.s. | ||
| SLEI | 0.22 | 0.45 (0.07) | 0.30, 0.60 | <.0001 | ||
| PSS | 0.62 | 0.45 (0.03) | 0.40, 0.51 | <.0001 | ||
| Personal history | Personal history only | .12 | 0.34 | 0.34 (0.05) | 0.25, 0.43 | <.0001 |
| Adjusted model: | .50 | |||||
| Personal history | 0.10 | 0.10 (0.04) | 0.02, 0.18 | .01 | ||
| SLEI | 0.18 | 0.38 (0.08) | 0.22, 0.53 | <.0001 | ||
| PSS | 0.60 | 0.44 (0.03) | 0.39, 0.49 | <.0001 | ||
| Racism | Racism only | .05 | 0.24 | 0.29 (0.06) | 0.17, 0.40 | <.0001 |
| Adjusted model: | .50 | |||||
| Racism | 0.10 | 0.12 (0.04) | 0.04, 0.21 | .004 | ||
| SLEI | 0.21 | 0.42 (0.07) | 0.28, 0.57 | <.0001 | ||
| PSS | 0.61 | 0.45 (0.03) | 0.39, 0.50 | <.0001 | ||
| Work | Work only | .08 | 0.29 | 0.38 (0.06) | 0.26, 0.50 | <.0001 |
| Adjusted model: | .50 | |||||
| Work | 0.10 | 0.13 (0.05) | 0.04, 0.23 | .005 | ||
| SLEI | 0.22 | 0.45 (0.07) | 0.30, 0.59 | <.0001 | ||
| PSS | 0.59 | 0.43 (0.03) | 0.38, 0.49 | <.0001 |
JHP-RC©: 39-item Jackson Hogue Phillips Reduced Common Contextualized Stress Measure; PSS: 14-item Perceived Stress Scale; SLEI: 13-item Stressful Life Events Index.
Though not significant, the coping subscale was forced into this model to yield estimates, given it is a parameter of interest.
n.s. connotes not statistically significant at p ⩽ .05.
Discussion
While a few studies have tested the association of the JHP© with depression and/or perceived stress, to our knowledge ours is the first to: (1) use the 39-item version of the JHP© (i.e. the JHP-RC©), which may offer moderate time-saving benefits over longer versions of the scale as well as insight into intersectional stresses common to most Black women; (2) examine these associations in a socioeconomically diverse sample of pregnant Black women, as compared to studies of non-pregnant, 63 highly educated pregnant,43,54 or predominately low-income pregnant Black women; 52 (3) examine whether the JHP-RC© added significantly to the variance in depressive symptoms beyond both perceived stress and stressful life events, as compared to beyond perceived stress alone; 43 and (4) report on these associations across the instrument’s subscales. Our results coincide with findings that contextualized gendered racial stress is prevalent among pregnant Black women.43,54 Furthermore, we found that higher gendered racial stress was not only associated with increased depressive symptoms but was also a distinct dimension of psychosocial stress contributing to depressive symptoms among Black women in early pregnancy.
Gendered racial stress and depression
Concurrent with previous research on depression and the JHP©, 43 this study adds to a growing consensus that gendered racism can deleteriously affect Black women’s psychosocial health.40,47,52,63. Beyond extant studies, we postulated that differences in correlations with depression across the JHP-RC© subscales may shed light on nuanced pathways between pregnant Black women’s stress and health during a particularly vulnerable time in their life course. We found that burden may be among the most salient depression-causing components of commonly experienced gendered racial stress for pregnant Black women (r = .58, p < .0001). For example, pregnant women may have greater family burdens than women who are not mothers or women whose childrearing days have passed. 81
The importance of burden may extend beyond pregnancy, as well. In addition to assessing perceived lack of material and personal resources, the burden subscale captures the “imposed and embraced nurturing and caretaker roles associated with gender identity.” 63 As such, items associated with burden may approach measurement of some components of the Superwoman Schema (SWS), which describes Black women’s sociocontextually derived obligations to (1) exhibit strength, (2) suppress emotions, (3) resist vulnerability, (4) succeed independently and against any odds, and (5) prioritize care for others over self-care. 82 Specifically, burden subscale items like “I am taking care of everyone else but no one is taking care of me” may reflect Black women’s obligation to nurture others at their own expense (i.e. (e) above), which was found to be most strongly correlated with depression. 83 Recent empirical studies highlight pertinent findings, namely: (1) a significant association between internalization of the SWS and psychological distress, 84 including depression, anxiety, and loneliness,85,86 and (2) the stress burden of Black women’s obligation to help others may worsen the negative physiological effect that experiencing racial discrimination has on their allostatic load. 87 Still, further study is needed to directly quantify the associations of SWS with intersectional gendered racial stress measures, including the JHP©, with the SWS. 83
Dimensions of psychological stress
Prior research supports that measures of perceived stress and stressful life events assess largely independent dimensions of stress. 16 The PSS was designed to measure how “unpredictable, uncontrollable, and overloading” respondents find their lives. 79 Stressful life events are discrete events that can disrupt normal psychosocial functioning. 88 The correlation between the PSS and SLEI in our study (r = .23, p < .001) matched that found by Kingston et al., 16 implying that each instrument assesses distinct stress dimensions in racially heterogeneous pregnant populations.
We found the JHP-RC© to be more strongly correlated with perceived stress than stressful life events (r = .50 vs .32, p < .0001), which could be explained by the chronicity, recency, and type of stress each measure captures. For example, some life events we measured (like, “I was homeless”) may be considered acute or chronic stressors, depending on how frequently they happened or how intensive the experience was. 88 However, stress measures that are not contextualized in Black women’s lived experience may be limited in their ability to assess the unique chronic and acute stress exposure associated with gendered racism. 63
Our findings suggest that intersectional measures of gendered racial stress, like the JHP-RC©, may capture a component of pregnant Black women’s stress milieu that is distinct from both perceived stress and stressful events. Research has shown that lack of control over one’s life circumstances, in addition to stressor severity, can exacerbate the negative effects of stress on health. 88 Exposure to gendered racism creates an environment in which Black women feel they must be persistently vigilant in anticipation of racist events against themselves and their children. 63 Race-related vigilance is associated with feelings of helplessness in Black populations.89,90 For pregnant Black women, helplessness associated with gendered racial stress may increase susceptibility to depression.91–95
Improved prediction of depression using multiple stress measures
Over 31% of women were experiencing depressive symptoms (EDS scores ⩾ 10), supporting suggestions from other studies of gendered racial stress in Black women 52 that depression may be more prevalent in this group than among the general US female population (21.8%). 96 To identify underlying and potentially treatable causes of depression among pregnant Black women, our study supports measuring gendered racial stress to provide context when used in conjunction with generalized stress appraisal and general lifecourse stressors. Notably, of the JHP-RC© subscales, burden was most strongly correlated with perceived stress, and personal history was most strongly correlated with stressful life events. In recent work on the Superwoman Schema, Black women’s obligation to suppress emotions was most strongly associated with perceived stress (r = .40, p < .05), further implying that Black women’s gendered racial stress burden may be linked to cognitive and emotional stress appraisal, and to internalization of the superwoman identity. 83 The personal history subscale captures discrete stressors associated with a history of physical and mental abuse and neglect, 63 which were also captured in our stressful life events checklist.
When measures of perceived stress, stressful life events, and gendered racism were assessed in the same study, we found that the magnitude of the relationship between measures of prenatal psychosocial stress and depressive symptoms varied based on the stress measure. These findings suggest that, when considered collectively, each aspect of stress may uniquely contribute to depression. In our study, the contribution of gendered racial stress to depressive symptoms was generally greater than that of stressful life events, but smaller than that of perceived stress. The only other report of the JHP© measure’s relative contribution to variance in prenatal depression in the context of other stress measures found that when added to a model containing the PSS and covariates, the 68-item JHP© increased the explanation of variance in Black women’s EDS scores from roughly 42% to 46%. 43 In our study, the 39-item JHP-RC© improved the explanation of variance in EDS scores over perceived stress alone, from 45% to 50%. Furthermore, when added to a model including both perceived stress and stressful life events, gendered racial stress contributes similarly, adding 3 percentage points to the total explanation of variance in EDS scores. Previously, researchers found that gendered racism (operationalized specifically as racialized sexual harassment) was not independently associated with depressive symptoms among non-pregnant, mostly low-income Black women, but that a model containing gendered racism, racist events, sexual objectification, and coping via internalization explained 42% of the variance in depression. 50
Of note, the JHP-RC© burden subscale contributed most to predicting depressive symptoms in multivariable regression, perhaps for aforementioned reasons. Our backwards selection models dropped all sociodemographic covariates (i.e. age, education, and parity), indicating that those variables did not contribute significantly to predicting depressive symptoms over and above the combination of perceived stress, stressful life events, and gendered racial stress. Given the limited number of covariates we considered, additional investigation is needed to clarify which variables pose the greatest threat to pregnant Black women’s psychosocial health, and to identify whether sociodemographic factors like education alter one’s experience of embodiment of gendered racial stress.
Future research
Arguments that Black women’s depression may not be accurately detected by conventional tools (particularly, those originally developed in non-Black populations, like the EDS) may warrant use of a lower EDS cut-off score.43,69,73 While not the focus of these analyses, future work may further investigate the sociodemographic factors associated with gendered racial stress and depression. There is evidence that poor social support from intimate partner relationships 97 and lower socioeconomic position 98 are linked to stress and poor outcomes in pregnancy. These factors may influence the role of gendered racism on maternal and infant outcomes. 54
Limitations
In this cross-sectional analysis, we examined the relative contribution of gendered racial stress to comorbid depression in early pregnancy but could not test an hypothesis that gendered racial stress predated depressive symptoms. Furthermore, our reliance on self-report of gendered racial stress, stressful life events, perceived stress, and depression introduces the possibility of recall and social desirability bias. This issue is inherent in efforts to understand Black women’s lived experiences centered on Black women’s own accounts. Psychometrically sound self-report measures may thus be viewed as helpful tools rather than drawbacks in analyzing constructs related to intersectionality. Last, previous research indicates that Black women appraise their obligation to protect children in their community from racism as stressful. 42 Our 39-item version of the JHP© excludes four items in the original JHP© pertaining to Black women’s own children. 42 Because 46% of our sample of pregnant women were nulliparous, these questions could not be considered to be “common” intersectional stresses. The JHP-RC© contains one of two original items regarding discriminatory practices that may affect one’s own children as well as infants once born (i.e. “The African American youth in my community are more likely than other youth to have a negative experience with law enforcement”). Jackson, et al. (2017) found this item to be significantly associated with prenatal depressive symptoms among all women in their study, as well as higher associations among pregnant women with a preschool-aged male child in the household. Additional analyses stratified by parity may point to components of gendered racial stress that are most troubling for Black mothers.
Conclusion
This study adds to a growing literature on the impact of psychosocial stress on depression among pregnant Black women. Our findings not only highlight that gendered racial stress may have important and distinct associations but also demonstrate the advantages of using intentionally intersectional stress measures to uncover nuances within Black women’s complex social environment. Disproportionate rates of adverse birth outcomes and their stress-related correlates among Black women are troubling and untenable, particularly given far-reaching physiological and psychosocial consequences for women and children. Furthermore, though most Black women may experience gendered racism, homogeneity among its causes and consequences is unlikely even within-race. While we did not investigate birth outcomes here, future work can expand upon our findings to: (1) investigate the distinct contribution of gendered racial stress to preterm birth, for instance, and (2) explore factors that may offer protection for pregnant Black against the detrimental effects of stress on health. Concerted investigation of Black women’s unique psychosocial experiences holds promise to highlight and mitigate etiological sources of the Black-White disparity in reproductive health.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455057221104657 for The unique contribution of gendered racial stress to depressive symptoms among pregnant Black women by Lasha S Clarke, Halley EM Riley, Elizabeth J Corwin, Anne L Dunlop and Carol J Rowland Hogue in Women’s Health
Acknowledgments
The authors express gratitude to the women who generously agreed to participate in this research, to the research coordinators who interface with the participating women to carefully collect research data, and to the clinical providers, nursing and laboratory staff at the prenatal care clinics of Grady Memorial Hospital and Emory University Hospital Midtown without whose cooperation this research would not be possible.
Footnotes
ORCID iD: Lasha S Clarke  https://orcid.org/0000-0003-4043-9870
https://orcid.org/0000-0003-4043-9870
Supplemental material: Supplemental material for this article is available online.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval and consent to participate: This study was reviewed for ethical and safety considerations by the Internal Review Boards (IRB00068441) of both Emory University and Grady Memorial Hospital and was approved by both Boards. All participants provided written informed consent, and received financial compensation for their participation.
Consent for publication: Not applicable.
Author contribution(s): Lasha S Clarke: Conceptualization; Formal analysis; Methodology; Writing—original draft; Writing—review & editing.
Halley EM Riley: Conceptualization; Formal analysis; Writing—review & editing.
Elizabeth J Corwin: Conceptualization; Funding acquisition; Investigation; Writing—review & editing.
Anne L Dunlop: Conceptualization; Funding acquisition; Writing—review & editing.
Carol J Rowland Hogue: Conceptualization; Supervision; Writing—review & editing.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a grant from the National Institutes of Health, National Institute of Nursing Research (R01NR014800; PIs: Elizabeth Corwin, Anne Dunlop) and National Institute of Environmental Health Sciences (R24ES029490; PIs: Anne Dunlop, Dean Jones). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Availability of data and materials: Supporting information is available as supplementary material, and further supporting data may be available from the authors on request.
Guarantor: C.J.R.H. is the guarantor of this article.
References
- 1. Hogue CJ, Bremner JD. Stress model for research into preterm delivery among black women. Am J Obstet Gynecol 2005; 192(Suppl. 5): S47–S55. [DOI] [PubMed] [Google Scholar]
- 2. Davalos DB, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch Women Ment Health 2012; 15(1): 1–14. [DOI] [PubMed] [Google Scholar]
- 3. Schetter CD, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatr 2012; 25(2): 141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatr 2010; 67(10): 1012–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alder J, Fink N, Bitzer J, et al. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fet Neonat Med 2007; 20(3): 189–209. [DOI] [PubMed] [Google Scholar]
- 6. Martin JA, Hamilton BE, Osterman MJK, et al. Births: final data for 2018. Natl Vital Stat Rep 2019; 68(13): 1–47. [PubMed] [Google Scholar]
- 7. Ncube CN, Enquobahrie DA, Gavin AR. Racial differences in the association between maternal antenatal depression and preterm birth risk: a prospective cohort study. J Women Health 2017; 26(12): 1312–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rosenthal L, Lobel M. Explaining racial disparities in adverse birth outcomes: unique sources of stress for Black American women. Soc Sci Med 2011; 72(6): 977–983. [DOI] [PubMed] [Google Scholar]
- 9. Wallace M, Harville E, Theall K, et al. Preconception biomarkers of allostatic load and racial disparities in adverse birth outcomes: the Bogalusa Heart Study. Paediatr Perinat Epidemiol 2013; 27(6): 587–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dominguez TP, Dunkel Schetter C, Glynn LM, et al. Racial differences in birth outcomes: the role of general, pregnancy, and racism stress. Health Psychol 2008; 27(2): 194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Woods SM, Melville JL, Guo Y, et al. Psychosocial stress during pregnancy. Am J Obstet Gynecol 2010; 202(1): 61.e1–61.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Christian LM. Stress and immune function during pregnancy: an emerging focus in mind-body medicine. Curr Dir Psychol Sci 2015; 24(1): 3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Geronimus AT, Hicken MT, Keene DR, et al. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. Am J Public Health 2006; 96(5): 826–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci 1999; 896: 30–47. [DOI] [PubMed] [Google Scholar]
- 15. Matthey S, Phillips J, White T, et al. Routine psychosocial assessment of women in the antenatal period: frequency of risk factors and implications for clinical services. Arch Women Ment Health 2004; 7(4): 223–229. [DOI] [PubMed] [Google Scholar]
- 16. Kingston D, Heaman M, Fell D, et al. Factors associated with perceived stress and stressful life events in pregnant women: findings from the Canadian Maternity Experiences Survey. Matern Child Health J 2012; 16(1): 158–168. [DOI] [PubMed] [Google Scholar]
- 17. Pagel MD, Smilkstein G, Regen H, et al. Psychosocial influences on new born outcomes: a controlled prospective study. Soc Sci Med 1990; 30(5): 597–604. [DOI] [PubMed] [Google Scholar]
- 18. Dominguez TP, Schetter CD, Mancuso R, et al. Stress in African American pregnancies: testing the roles of various stress concepts in prediction of birth outcomes. Ann Behav Med 2005; 29(1): 12–21. [DOI] [PubMed] [Google Scholar]
- 19. Staneva A, Bogossian F, Pritchard M, et al. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: a systematic review. Women Birth 2015; 28(3): 179–193. [DOI] [PubMed] [Google Scholar]
- 20. Kessler RC. The effects of stressful life events on depression. Ann Rev Psychol 1997; 48: 191–214. [DOI] [PubMed] [Google Scholar]
- 21. Witt WP, Cheng ER, Wisk LE, et al. Maternal stressful life events prior to conception and the impact on infant birth weight in the United States. Am J Public Health 2014; 104(Suppl. 1): S81–S89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Witt WP, Cheng ER, Wisk LE, et al. Preterm birth in the United States: the impact of stressful life events prior to conception and maternal age. Am J Public Health 2014; 104(Suppl. 1): S73–S80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Christian LM, Glaser R, Porter K, et al. Stress-induced inflammatory responses in women: effects of race and pregnancy. Psychosom Med 2013; 75(7): 658–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Frazier T, Hogue CJR, Bonney EA, et al. Weathering the storm; a review of pre-pregnancy stress and risk of spontaneous abortion. Psychoneuroendocrinology 2018; 92: 142–154. [DOI] [PubMed] [Google Scholar]
- 25. Giscombé CL, Lobel M. Explaining disproportionately high rates of adverse birth outcomes among African Americans: the impact of stress, racism, and related factors in pregnancy. Psychol Bull 2005; 131(5): 662–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kramer MR, Hogue CJ, Dunlop AL, et al. Preconceptional stress and racial disparities in preterm birth: an overview. Acta Obstet Gynecol Scand 2011; 90(12): 1307–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kramer MR, Hogue CR. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiol Rev 2009; 31: 84–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rich-Edwards JW, Grizzard TA. Psychosocial stress and neuroendocrine mechanisms in preterm delivery. Am J Obstet Gynecol 2005; 192(Suppl. 5): S30–S35. [DOI] [PubMed] [Google Scholar]
- 29. Lu MC, Chen B. Racial and ethnic disparities in preterm birth: the role of stressful life events. Am J Obstet Gynecol 2004; 191(3): 691–699. [DOI] [PubMed] [Google Scholar]
- 30. Masho SW, Price SK, Kinser PA. Racial disparities in the association between stress and preterm birth. J Health Dispar Res Pract 2014; 8(4): 6. [Google Scholar]
- 31. Prather C, Fuller TR, Jeffries WL, et al. Racism, African American women, and their sexual and reproductive health: a review of historical and contemporary evidence and implications for health equity. Health Equity 2018; 2(1): 249–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Clark R, Anderson NB, Clark VR, et al. Racism as a stressor for African Americans. A biopsychosocial model. Am Psychol 1999; 54(10): 805–816. [DOI] [PubMed] [Google Scholar]
- 33. Stancil TR, Hertz-Picciotto I, Schramm M, et al. Stress and pregnancy among African-American women. Paediatr Perinat Epidemiol 2000; 14(2): 127–135. [DOI] [PubMed] [Google Scholar]
- 34. Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Ann Rev Clin Psychol 2015; 11: 407–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Ann Rev Psychol 2007; 58: 201–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med 2009; 32(1): 20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Murrell NL. Stress, self-esteem, and racism: relationships with low birth weight and preterm delivery in African American women. J Natl Black Nurse Assoc 1996; 8(1): 45–53. [PubMed] [Google Scholar]
- 38. Essed P. Understanding everyday racism: an interdisciplinary theory, vol. 2. Thousand Oaks, CA: SAGE, 1991. [Google Scholar]
- 39. Lewis JA, Williams MG, Peppers EJ, et al. Applying intersectionality to explore the relations between gendered racism and health among Black women. J Couns Psychol 2017; 64(5): 475–486. [DOI] [PubMed] [Google Scholar]
- 40. Thomas AJ, Witherspoon KM, Speight SL. Gendered racism, psychological distress, and coping styles of African American women. Cult Diver Ethn Minor Psychol 2008; 14(4): 307–314. [DOI] [PubMed] [Google Scholar]
- 41. Lewis TT, Van Dyke ME. Discrimination and the health of African Americans: the potential importance of intersectionalities. Curr Direct Psychol Sci 2018; 27(3): 176–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Jackson FM, Phillips MT, Hogue CJ, et al. Examining the burdens of gendered racism: implications for pregnancy outcomes among college-educated African American women. Matern Child Health J 2001; 5(2): 95–107. [DOI] [PubMed] [Google Scholar]
- 43. Jackson FM, Rowley DL, Curry Owens T. Contextualized stress, global stress, and depression in well-educated, pregnant, African-American women. Women Health Issues 2012; 22(3): e329–e336. [DOI] [PubMed] [Google Scholar]
- 44. Greer TM, Laseter A, Asiamah D. Gender as a moderator of the relation between race-related stress and mental health symptoms for African Americans. Psychol Women Quart 2009; 33(3): 295–307. [Google Scholar]
- 45. Devillard S, Hunt V, Yee L. Still looking for room at the top: ten years of research on women in the workplace. McKins Quart 2018; 2: 106–115. [Google Scholar]
- 46. Brownlow BN, Sosoo EE, Long RN, et al. Sex differences in the impact of racial discrimination on mental health among Black Americans. Curr Psychiatr Rep 2019; 21(11): 1–14. [DOI] [PubMed] [Google Scholar]
- 47. Rosenthal L, Lobel M. Gendered racism and the sexual and reproductive health of Black and Latina women. Ethn Health 2020; 25(3): 367–392. [DOI] [PubMed] [Google Scholar]
- 48. Lewis JA, Neville HA. Construction and initial validation of the gendered racial microaggressions scale for Black women. J Couns Psychol 2015; 62(2): 289–302. [DOI] [PubMed] [Google Scholar]
- 49. Szymanski DM, Lewis JA. Gendered racism, coping, identity centrality, and African American college women’s psychological distress. Psychol Women Quart 2016; 40(2): 229–243. [Google Scholar]
- 50. Carr ER, Szymanski DM, Taha F, et al. Understanding the link between multiple oppressions and depression among African American women: the role of internalization. Psychol Women Quart 2014; 38(2): 233–245. [Google Scholar]
- 51. Mehra R, Boyd LM, Magriples U, et al. Black pregnant women “get the most judgment”: a qualitative study of the experiences of Black women at the intersection of race, gender, and pregnancy. Women Health Issues 2020; 30(6): 484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Jackson FM, James SA, Owens TC. Anticipated negative police-youth encounters and depressive symptoms among pregnant African American women: a brief report. J Urban Health 2017; 94(2): 259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Perry BL, Pullen EL, Oser CB. Too much of a good thing? Psychosocial resources, gendered racism, and suicidal ideation among low socioeconomic status African American women. Soc Psychol Quart 2012; 75(4): 334–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Curry Owens T, Jackson FM. Examining life-course socioeconomic position, contextualized stress, and depression among well-educated African-American pregnant women. Women Health Issues 2015; 25(4): 382–389. [DOI] [PubMed] [Google Scholar]
- 55. Bowleg L. When Black+ lesbian+ woman≠ Black lesbian woman: the methodological challenges of qualitative and quantitative intersectionality research. Sex Roles 2008; 59(5–6): 312–325. [Google Scholar]
- 56. Cho S, Crenshaw KW, McCall L. Toward a field of intersectionality studies: theory, applications, and praxis. Sign J Women Cult Soc 2013; 38(4): 785–810. [Google Scholar]
- 57. Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med 2014; 110: 10–17. [DOI] [PubMed] [Google Scholar]
- 58. Bowleg L, Bauer G. Invited reflection: quantifying intersectionality. Psychol Women Quart 2016; 40(3): 337–341. [Google Scholar]
- 59. Moradi B, Subich LM. A concomitant examination of the relations of perceived racist and sexist events to psychological distress for African American women. Counsel Psychol 2003; 31(4): 451–469. [Google Scholar]
- 60. Cole ER. Intersectionality and research in psychology. Am Psychol 2009; 64(3): 170–180. [DOI] [PubMed] [Google Scholar]
- 61. Thomas AJ, Hacker JD, Hoxha D. Gendered racial identity of Black young women. Sex Roles 2011; 64(7–8): 530–542. [Google Scholar]
- 62. Nuru-Jeter A, Dominguez TP, Hammond WP, et al. “It’s the skin you’re in”: African-American women talk about their experiences of racism. An exploratory study to develop measures of racism for birth outcome studies. Matern Child Health J 2009; 13(1): 29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Jackson FM, Hogue CJ, Phillips MT. The development of a race and gender-specific stress measure for African-American women: Jackson, Hogue, Phillips contextualized stress measure. Ethn Dis 2005; 15(4): 594–600. [PubMed] [Google Scholar]
- 64. Corwin EJ, Hogue CJ, Pearce B, et al. Protocol for the Emory University African American vaginal, oral, and gut microbiome in pregnancy cohort study. BMC Pregnancy Childbirth 2017; 17(1): 161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatr 1987; 150: 782–786. [DOI] [PubMed] [Google Scholar]
- 66. Kozinszky Z, Dudas RB. Validation studies of the Edinburgh postnatal depression scale for the antenatal period. J Affect Disord 2015; 176: 95–105. [DOI] [PubMed] [Google Scholar]
- 67. Grobman WA, Parker C, Wadhwa PD, et al. Racial/ethnic disparities in measures of self-reported psychosocial states and traits during pregnancy. Am J Perinatol 2016; 33(14): 1426–1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Bergink V, Kooistra L, Lambregtse-van den Berg MP, et al. Validation of the Edinburgh depression scale during pregnancy. J Psychosom Res 2011; 70(4): 385–389. [DOI] [PubMed] [Google Scholar]
- 69. Tandon SD, Cluxton-Keller F, Leis J, et al. A comparison of three screening tools to identify perinatal depression among low-income African American women. J Affect Disord 2012; 136(1): 155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Yonkers KA, Ramin SM, Rush AJ, et al. Onset and persistence of postpartum depression in an inner-city maternal health clinic system. Am J Psychiatr 2001; 158(11): 1856–1863. [DOI] [PubMed] [Google Scholar]
- 71. Kendler KS, Karkowski LM, Prescott CA. Stressful life events and major depression: risk period, long-term contextual threat, and diagnostic specificity. J Nerv Ment Dis 1998; 186(11): 661–669. [DOI] [PubMed] [Google Scholar]
- 72. Kessler RC. Epidemiology of women and depression. J Affect Disord 2003; 74(1): 5–13. [DOI] [PubMed] [Google Scholar]
- 73. Matthey S, Henshaw C, Elliott S, et al. Variability in use of cut-off scores and formats on the Edinburgh postnatal depression scale: implications for clinical and research practice. Arch Women Ment Health 2006; 9(6): 309–315. [DOI] [PubMed] [Google Scholar]
- 74. Chaudron LH, Szilagyi PG, Tang W, et al. Accuracy of depression screening tools for identifying postpartum depression among urban mothers. Pediatrics 2010; 125(3): e609–e617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Bunevicius A, Kusminskas L, Pop VJ, et al. Screening for antenatal depression with the Edinburgh depression scale. J Psychosom Obstet Gynecol 2009; 30(4): 238–243. [DOI] [PubMed] [Google Scholar]
- 76. English S, Steele A, Williams A, et al. Modelling of psychosocial and lifestyle predictors of peripartum depressive symptoms associated with distinct risk trajectories: a prospective cohort study. Sci Rep 2018; 8(1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Jackson FM, Hogue CJR, Phillips MT. Jackson, Hogue, Phillips contextualized stress measure, 2014 (clinical form). Technical Manual, 2014. Unpublished. [Google Scholar]
- 78. Freeman A. A validity assessment of the contextualized Jackson, Hogue, Phillips measure: a gender-and race-specific stress measure used in a worksite fitness study for African American women, in Department of Behavioral Sciences & Health Education. Electronic Theses and Dissertations Repository, Rollins School of Public Health, Emory University, 2009. [Google Scholar]
- 79. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983; 24: 385–396. [PubMed] [Google Scholar]
- 80. Hogue CJ, Parker CB, Willinger M, et al. A population-based case-control study of stillbirth: the relationship of significant life events to the racial disparity for African Americans. Am J Epidemiol 2013; 177(8): 755–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Umberson D, Pudrovska T, Reczek C. Parenthood, childlessness, and well-being: a life course perspective. J Marr Fam 2010; 72(3): 612–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Woods-Giscombé CL. Superwoman schema: African American women’s views on stress, strength, and health. Qualitat Health Res 2010; 20(5): 668–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Woods-Giscombe CL, Allen AM, Black AR, et al. The Giscombe Superwoman Schema Questionnaire: psychometric properties and associations with mental health and health behaviors in African American women. Issue Ment Health Nurs 2019; 40(8): 672–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Watson-Singleton NN. Strong Black woman schema and psychological distress: the mediating role of perceived emotional support. J Black Psychol 2017; 43(8): 778–788. [Google Scholar]
- 85. Liao KYH, Wei M, Yin M. The misunderstood schema of the strong Black woman: exploring its mental health consequences and coping responses among African American women. Psychol Women Quart 2020; 44(1): 84–104. [Google Scholar]
- 86. Watson NN, Hunter CD. Anxiety and depression among African American women: the costs of strength and negative attitudes toward psychological help-seeking. Cult Diver Ethn Minor Psychol 2015; 21(4): 604–612. [DOI] [PubMed] [Google Scholar]
- 87. Allen AM, Wang Y, Chae DH, et al. Racial discrimination, the superwoman schema, and allostatic load: exploring an integrative stress-coping model among African American women. Ann N Y Acad Sci 2019; 1457(1): 104–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Crosswell AD, Lockwood KG. Best practices for stress measurement: how to measure psychological stress in health research. Health Psychol Open 2020; 7(2): 0933072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Davis GY, Stevenson HC. Racial socialization experiences and symptoms of depression among Black youth. J Child Fam Stud 2006; 15(3): 293–307. [Google Scholar]
- 90. Powell LR, Jesdale WM, Lemon SC. On edge: the impact of race-related vigilance on obesity status in African-Americans. Obes Sci Pract 2016; 2(2): 136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Abramson LY, Seligman ME, Teasdale JD. Learned helplessness in humans: critique and reformulation. J Abnorm Psychol 1978; 87(1): 49–74. [PubMed] [Google Scholar]
- 92. Abramson LY, Garber J, Seligman ME. Learned helplessness in humans: an attributional analysis. Hum Helpless Theor Appl 1980; 3: 34. [Google Scholar]
- 93. Fernando S. Racism as a cause of depression. Int J Soc Psychiatr 1984; 30(1–2): 41–49. [DOI] [PubMed] [Google Scholar]
- 94. Broman CL, Mavaddat R, Hsu SY. The experience and consequences of perceived racial discrimination: a study of African Americans. J Black Psychol 2000; 26(2): 165–180. [Google Scholar]
- 95. Ursin H, Eriksen HR. The cognitive activation theory of stress. Psychoneuroendocrinology 2004; 29(5): 567–592. [DOI] [PubMed] [Google Scholar]
- 96. Villarroel MA, Terlizzi EP. Symptoms of depression among adults: United States, 2019. NCHS Data Brief 2020; 379: 1–8. [PubMed] [Google Scholar]
- 97. Orr ST. Social support and pregnancy outcome: a review of the literature. Clin Obstet Gynecol 2004; 47(4): 842–855. [DOI] [PubMed] [Google Scholar]
- 98. Kramer MS, Séguin L, Lydon J, et al. Socio-economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr Perinat Epidemiol 2000; 14(3): 194–210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455057221104657 for The unique contribution of gendered racial stress to depressive symptoms among pregnant Black women by Lasha S Clarke, Halley EM Riley, Elizabeth J Corwin, Anne L Dunlop and Carol J Rowland Hogue in Women’s Health