Abstract
Background:
End-stage ankle osteoarthritis often requires one of 2 major surgical procedures: total ankle arthroplasty or ankle arthrodesis. Although the gold standard has been arthrodesis, patients with diabetes represent a unique cohort that requires additional considerations because of their decreased mobility and risk factors for cardiovascular complications. The purpose of this study is to review odds of major and minor adverse events for patients with diabetes and patients without diabetes in both total ankle arthroplasty and ankle arthrodesis.
Methods:
A total of 14 articles published between 2010 and 2020 were included in this review. Databases included PubMed, Scopus, MEDLINE/Embase, and Cochrane Library. Key words included ankle arthroplasty, total ankle arthroplasty, ankle arthrodesis, and diabetes.
Results:
The total number of procedures was 26 287, comprising 13 830 arthroplasty and 12 457 arthrodesis procedures. There was a significant association between patients with diabetes treated with arthrodesis and major adverse events (odds ratio [OR] 1.880, 95% CI 1.279, 2.762), whereas no significant association was observed between patients with diabetes treated with arthroplasty and major adverse events (OR 1.106, 95% CI 0.871, 1.404).
Conclusion:
This meta-analysis suggests patients with diabetes to be at significantly higher risk for major and minor adverse events after undergoing ankle arthrodesis. However, it suggests no significant differences in major adverse events between patients with diabetes and patients without diabetes having undergone total ankle arthroplasty.
Level of Evidence:
Level III, systematic review and meta-analysis.
Keywords: arthrodesis, arthroplasty, diabetes, ankle replacement, total ankle arthroplasty, ankle arthrodesis
Introduction
Osteoarthritis (OA) is a debilitating disease of the joints that affects approximately 31 million or 13.8% of the adult population in the United States. 6 OA has severe humanistic, clinical, and economic burdens at both the individual and population levels. In 2019, it was estimated that the adjusted incremental annual total health care costs among adults with OA were $1778 per person and $45 billion at the national level. 36 Adults with OA have significantly poorer health-related quality of life (HRQOL) compared with their healthy counterparts because disease progression directly impacts their ability to ambulate and maintain overall independence.27,36 The ability to ambulate has been strongly linked to overall health and mortality.13,20 These affected individuals are more likely to report pain interference with activities and functional limitations related to activities of daily living. 21 Patients with diabetes have approximately twice the likelihood to develop OA compared to patients without diabetes and deemed as more complex because of the pathophysiology of the disease and presence of other comorbidities.14,19,28 Maintaining mobility and independence is of heightened importance in patients with diabetes as diabetes is already associated with fewer steps per day, an increased risk for experiencing cardiovascular morbidity, and overall mortality.2,4,12
Total ankle arthroplasty (TAA) and ankle arthrodesis (AA) are the 2 primary surgical options for patients who suffer from chronic osteoarthritis of the ankle that have failed conservative treatment. AA has been the gold standard in treatment of end-stage OA of the ankle. 15 However, to maintain ankle motion, improve gait, and preserve adjacent joints, TAA was developed as an alternative technique. 15 Diabetes has historically been a relative contraindication for TAA because of increased comorbidity and poor surgical outcomes compared with nondiabetics. 10 However, patients with diabetes may stand to gain the most from a TAA due to TAA’s inherit ability to maintain joint motion and in turn promote more steps per day, continued mobility, and encourage functional independence.30,32 The investigators sought to investigate the odds of major and minor adverse events for patients with diabetes and patients without diabetes in both TAA and AA.
Materials and Methods
A systematic review was conducted across 4 databases between November 15, 2021, and December 15, 2021. Two researchers independently searched the following 4 databases: PubMed, MEDLINE/Embase, Cochrane, and Web of Science. The search algorithm incorporated the keywords ankle arthroplasty, total ankle arthroplasty, ankle arthrodesis, and diabetes.
The following inclusion and exclusion criteria were used for the article selection. All citations must have been written in English, be full-length, and have a comparative study design. Data must have also met the inclusion criteria of containing extractable, 2 × 2 information. Major adverse events (MAEs) were defined by complications post TAA or AA that involved the patient returning to the operating room, having a major amputation (below-the-knee amputation), mortality, or myocardial infarction. Minor adverse events (AEs) were defined as all complications exclusive of MAEs as well as any other complications including infections. True positive data indicated subjects were diabetic and had a positive outcome of MAE or AE. False positive were nondiabetics with an outcome of MAE or AE. True negative were nondiabetics that did not have an outcome of revision or MAE or AE. False negatives were diabetics who did not have an outcome of MAE or AE. All study cohorts must consist of adults (>18 years) and have been treated with either total ankle arthroplasty or ankle arthrodesis. Historical systematic reviews, study proposals, meta-analyses, and case studies were excluded. This systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Once each database was screened, Mendeley (Elsevier) was used to check and delete duplicate citations. Two reviewers then independently examined and screened titles and abstracts using inclusion and exclusion criteria. Any disagreements were resolved by consensus discussion with a third reviewer.
One author completed holistic data extraction for article publication date, author, study design, patient demographics, gender, ethnicity, mean age, diabetes status, and ankle surgery. The complete search strategy is detailed in Supplemental Figure S1. The primary outcome examined in this review is diabetics who underwent TAA or AA and their clinical driven outcomes of MAE or AE in comparison to nondiabetics that also underwent TAA or AA. Diabetes status was extracted from demographics provided in each citation.
All data were compiled using Microsoft Office Excel software and flow chart diagrams were generated using Microsoft Office PowerPoint. Comprehensive Meta-Analysis Software (Biostat, Englewood, NJ, 2006) was implemented to calculate odds ratios (ORs) and effect sizes for outcomes. Statistical heterogeneity was evaluated using the Cochrane Q test and I 2 statistic ranging from 0% to 100%. CIs of 95% were calculated and can be visualized on forest plots generated by the Comprehensive Meta-Analysis Software. For analyzing publication bias, funnel plots and Eggers test were used (Supplemental Figure S2). Remaining statistical assessments were performed in SAS statistical software, version 9.3 (SAS, Cary, NC).
Results
Initial literature searches yielded 597 total abstracts, of which 449 citations were full articles that underwent further review. Title screening and duplicate removal generated 41 articles that were reviewed in their entirety. Fourteen citations met the inclusion criteria and were included in this study. Of these articles, 8 presented results exclusively on TAA whereas 5 presented results exclusively on arthrodesis. One article contained results for both surgeries. Basic study characteristics are presented in Table 1.
Table 1.
Study Characteristics.
| General Characteristics | Year | Technique Examined | Age, y | Follow-up |
|---|---|---|---|---|
| Schipper et al29 | 2015 | TAR and arthrodesis | 59 (diabetes) 55 (no diabetes) |
NA |
| Patton et al22 | 2015 | TAR | 54 | 55 mo |
| Best et al3 | 2020 | TAR | 64 | NA |
| Raikin et al25 | 2010 | TAR | NA | NA |
| Pitts et al24 | 2020 | Arthrodesis | 54 | 13 mo |
| Wukich et al 35 | 2011 | Arthrodesis | 61 (diabetes) 54 (no diabetes) |
33 mo |
| Myers et al18 | 2012 | Arthrodesis | 57 | ≥6 mo |
| Wukich et al 34 | 2015 | Arthrodesis | 59 (diabetes) 57 (no diabetes) |
12 mo |
| Lee et al17 | 2021 | Arthrodesis | 61 | 28 mo |
| Gross et al 11 | 2015 | TAR | 62 | 1 y |
| Woo Lee et al17 | 2021 | TAR | 69 | 5 y |
| Cunningham et al 7 | 2018 | TAR | 63 | 3 mo |
| Choi et al5 | 2014 | TAR | 66 | 2 y |
| Althoff et al1 | 2018 | TAR | NA | 3 and 6 mo |
Abbreviations: NA, not available; TAR, total ankle replacement.
Among the TAA citations, a total of 13 830 TAA procedures were conducted. Of these, 3261 procedures were conducted in patients with diabetes whereas 10 569 procedures were conducted in patients without diabetes. Among the arthrodesis citations, a total of 12 457 arthrodesis procedures were performed. In addition, 2595 procedures were conducted in patients with diabetes, whereas 9862 procedures were conducted in patients without diabetes. The number of subjects by study with and without diabetes treated with either TAA or AA is displayed in Table 2. The average age of subjects ranged from 54 to 69 years and follow-up information ranged between 3 months and 5 years.
Table 2.
Number of Diabetics and Nondiabetics by Treatment.
| Study | Year | TAR, Diabetics | TAR, No Diabetes | Arthrodesis, Diabetes | Arthrodesis, No Diabetes |
|---|---|---|---|---|---|
| Schipper et al29 | 2015 | 302 | 2607 | 2400 | 9631 |
| Patton et al22 | 2015 | 6 | 81 | – | – |
| Best et al3 | 2020 | 30 | 264 | – | – |
| Raikin et al25 | 2010 | 11 | 93 | – | – |
| Pitts et al24 | 2020 | – | – | 36 | 65 |
| Wukich et al 35 | 2011 | – | – | 17 | 23 |
| Myers et al18 | 2012 | – | – | 74 | 74 |
| Wukich et al 34 | 2015 | – | – | 61 | 56 |
| Lee et al17 | 2021 | – | – | 7 | 13 |
| Gross et al 11 | 2015 | 50 | 55 | – | – |
| Woo Lee et al17 | 2021 | 676 | 1481 | – | – |
| Cunningham et al 7 | 2018 | 130 | 894 | – | – |
| Choi et al5 | 2014 | 43 | 130 | – | – |
| Althoff et al1 | 2018 | 2013 | 4964 |
Abbreviation: TAR, total ankle replacement.
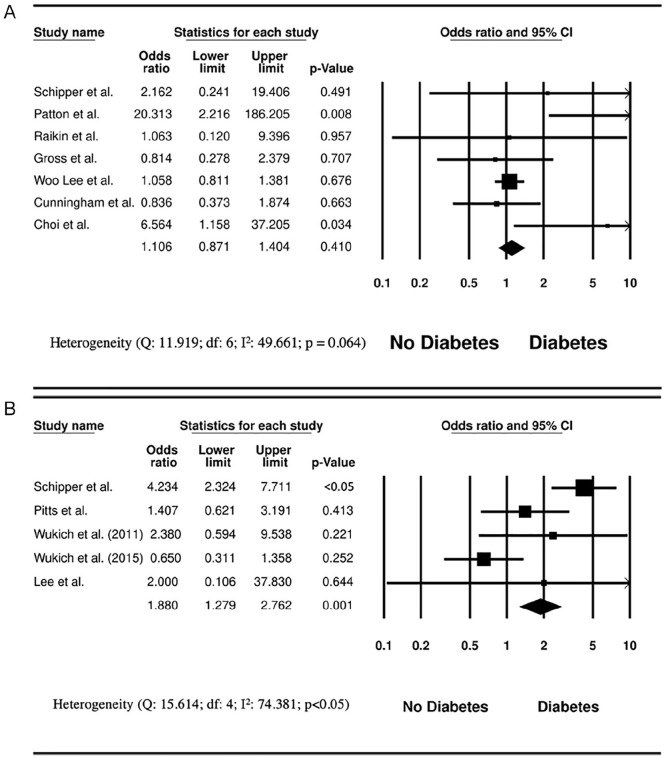
MAEs were consolidated within 7 TAA articles. The overall association between patients with diabetes treated with TAA and occurrence of an MAE was as follows: OR 1.106, 95% CI 0.871, 1.404 (Figure 1A). In comparison, the association between patients with diabetes treated with arthrodesis and MAE was as follows: OR 1.880, 95% CI 1.279, 2.762 (Figure 1B). Larger population studies (n > 1000) also tended to show no significant associations compared with smaller population trials.
Figure 1.
(A) Total ankle arthroplasty and major adverse events. (B) Arthrodesis and major adverse events.
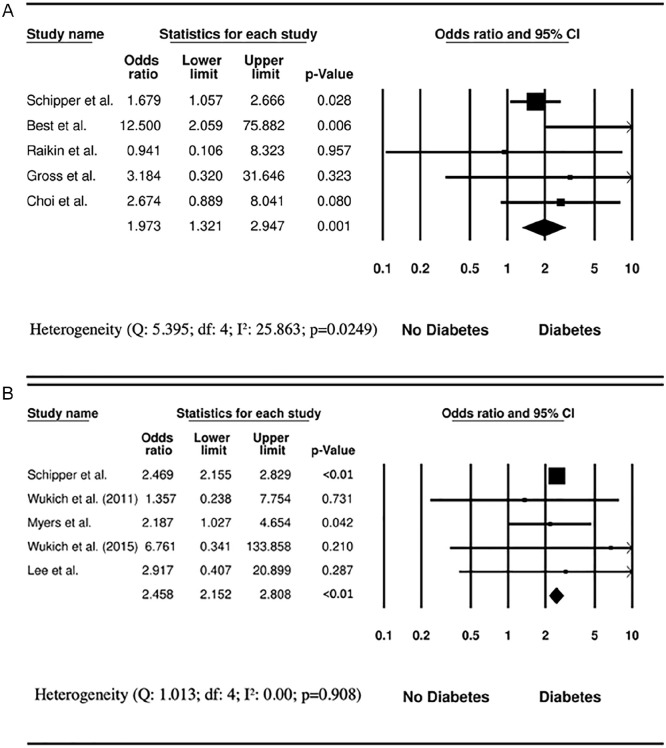
The overall association between patients with diabetes with TAA and minor complications was as follows: OR 1.973, 95% CI 1.321, 2.947 (Figure 2A). The association between patients with diabetes with arthrodesis and minor complications was as follows: OR 2.458, 95% CI 2.152, 2.808 (Figure 2B).
Figure 2.
(A) Total ankle arthroplasty and minor adverse events. (B) Arthrodesis and minor adverse events.
Supplemental Figure S2 presents the Eggers funnel plot of tests related to TAA or AA in patients with diabetes with the outcome as MAE. Interpretation of this plot revealed no signs of publication bias (P > .05), suggesting both negative and positive results have been observed in prior literature.
Discussion
In the present study, the authors investigated the differences in MAE and AE between patients with diabetes and patients without diabetes in both TAA and AA for the treatment of chronic OA. The results of this meta-analysis suggest patients with diabetes undergoing AA have significantly more MAE and AE than nondiabetic patients. For patients undergoing TAA, there was significantly more AE in the patients with diabetes cohort; however, no difference in MAE was observed between patients with diabetes and patients without diabetes.
End-stage OA continues to be a major complication requiring surgical management in the aging population. Patients with diabetes are at an increased risk for developing OA and have diminished mobility and quality of life compared to patients without diabetes. Joint replacement surgery has been shown to provide major benefits to quality of life in patients by reducing pain, improving depressive symptoms, and conserving mobility and functionality.26,31 The current surgical management of end-stage OA of the tibial talar (TT) joint includes AA and TAA. TAA has been shown to improve quality of life, ankle mobility, and pain reduction all while maintaining motion at the TT joint.9,30 Preservation of the TT joint in diabetics may be of increased importance as decreased mobility has been associated with multiple cardiovascular and cerebrovascular complications. 33 As TAA does preserve anatomical movement compared to arthrodesis, these functional improvements are key considerations to reducing the morbidity and mortality associated with diabetes and may be important for the operator to consider when discussing surgical options. 8
TAA and AA have generally shown similar clinical outcomes including nonsignificant differences in complication rates, revision rates, and amputation rates.9,16 Our findings suggest that patients with diabetes undergoing TAA have the same odds of MAE as patients without diabetes. This finding may be important to clinical practice as preserving motion at the TT joint may have cardiovascular benefits that are critical to the patients with diabetes. What’s more, functional outcomes of TAA, including visual analog scale (VAS), quality of life assessments, and Foot Ankle Ability Score (FAAS) for sports and daily living activities, were significantly higher in patients treated with TAA compared to AA.9,23,26,31 In addition, with the diminished mobility and quality of life diabetes brings, retaining functionality of the joint becomes an important consideration when electing the therapy to use. Although this study observed a reduced complication rate for patients treated with TAA compared to AA, further research, especially RCTs, are necessary to understand how TAA and arthrodesis can be applicable to the diabetic population.
Caution should be taken in their interpretation as several limitations were noted during the present authors’ review—one of which was the lack of randomization across each study included in this analysis. All studies were retrospective in their design, and only 1 article comparatively examined a cohort of patients with diabetes that received TAA with a cohort of patients with diabetes that received AA. Additionally, the severity of diabetes was not well defined. Of the 14 citations, only 2 discussed HbA1c levels whereas another classified diabetes as controlled or uncontrolled. This review does not have the ability to determine if patients with diabetes are in excellent control with no comorbidities vs other levels of disease manifestations. The lack of randomization and inability to discern levels of glycemic control across cohorts may lead to a selection bias that has not been controlled for. Quality of life questionnaires data were limited across both TAA and AA studies as well. Of the narrowed literature specific for patients with diabetes cohorts, only 2 citations for TAA and 2 citations for AA highlighted patient AOFAS scores. For TAA, average scores ranged from 81 to 84 points, whereas for arthrodesis, average scores ranged from 55 to 59 points.7,11,34,35 Although these data are scarce, improved scores were observed for the TAA-treated cohort. However, extrapolating a conclusion for this topic necessitates further studies involving different quality of life and pain questionnaires.
Appendix
Supplemental Figure S1.
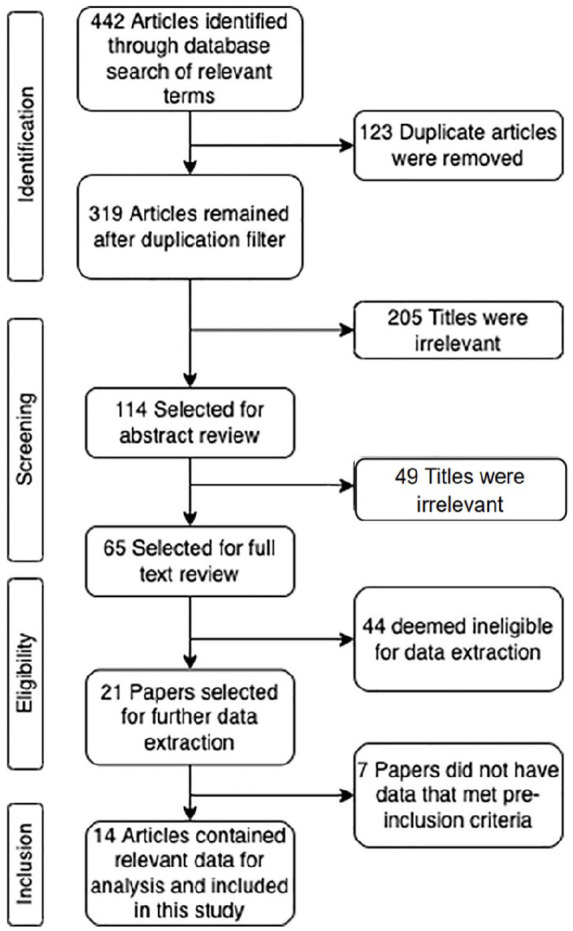
Flow Chart of Literature Search and Screening Results in Accordance with PRISMA Guidelines.
S2: Search Strategy
PubMed:
Search Terms: (((ankle arthroplasty) OR (total ankle arthroplasty)) OR (Ankle Arthrodesis)) AND (Diabetes)
(((“ankle”[MeSH Terms] OR “ankle”[All Fields] OR “ankle joint”[MeSH Terms] OR (“ankle”[All Fields] AND “joint”[All Fields]) OR “ankle joint”[All Fields] OR “ankles”[All Fields] OR “ankle s”[All Fields]) AND (“arthroplasty”[MeSH Terms] OR “arthroplasty”[All Fields] OR “arthroplasties”[All Fields])) OR (“arthroplasty, replacement, ankle”[MeSH Terms] OR (“arthroplasty”[All Fields] AND “replacement”[All Fields] AND “ankle”[All Fields]) OR “ankle replacement arthroplasty”[All Fields] OR (“total”[All Fields] AND “ankle”[All Fields] AND “arthroplasty”[All Fields]) OR “total ankle arthroplasty”[All Fields]) OR ((“ankle”[MeSH Terms] OR “ankle”[All Fields] OR “ankle joint”[MeSH Terms] OR (“ankle”[All Fields] AND “joint”[All Fields]) OR “ankle joint”[All Fields] OR “ankles”[All Fields] OR “ankle s”[All Fields]) AND (“arthrodesed”[All Fields] OR “arthrodesing”[All Fields] OR “arthrodesis”[MeSH Terms] OR “arthrodesis”[All Fields] OR “arthrodese”[All Fields] OR “arthrodeses”[All Fields]))) AND (“diabete”[All Fields] OR “diabetes mellitus”[MeSH Terms] OR (“diabetes”[All Fields] AND “mellitus”[All Fields]) OR “diabetes mellitus”[All Fields] OR “diabetes”[All Fields] OR “diabetes insipidus”[MeSH Terms] OR (“diabetes”[All Fields] AND “insipidus”[All Fields]) OR “diabetes insipidus”[All Fields] OR “diabetic”[All Fields] OR “diabetics”[All Fields] OR “diabets”[All Fields])
354 Results
| Embase/ MEDLINE | Web of Science | Cochrane |
|---|---|---|
| 1. Ankle Arthroplasty | 1. Ankle Arthroplasty | 1. Ankle Arthroplasty |
| 2. Total Ankle Arthroplasty | 2. Total Ankle Arthroplasty | 2. Total Ankle Arthroplasty |
| 3. Ankle Arthrodesis | 3. Ankle Arthrodesis | 3. Ankle Arthrodesis |
| 4. Diabetes | 4. Diabetes | 4. Diabetes |
| 5. 1 and 4 or 2 and 4 or 3 and 4 | 5. 1 and 4 or 2 and 4 or 3 and 4 | 5. 1 and 4 or 2 and 4 or 3 and 4 |
| 6. Full text | 6. Full text | 6. 2010-2022 |
| 7. English Only | 7. English Only | |
| 8. 2010-2022 | 8. 2010-2022 |
Supplemental Figure S2.
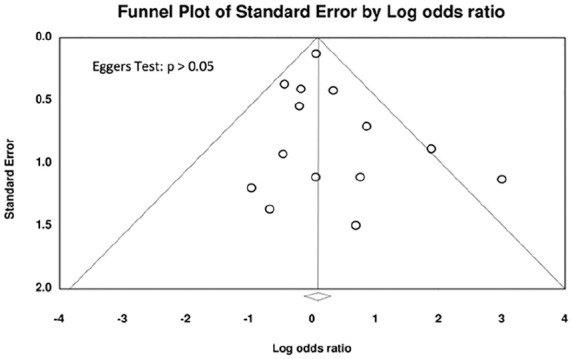
Eggers test and funnel plot for publication bias.
Footnotes
Ethical Approval: Ethical approval was not sought for the present study. This manuscript is a systematic review and study level meta-analysis; as such no human or animal subjects were included. All studies included were approved by their respective ethics committees or institutional review boards.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Arthur Tarricone, DPM, MPH,  https://orcid.org/0000-0001-5311-6283
https://orcid.org/0000-0001-5311-6283
References
- 1. Althoff A, Cancienne JM, Cooper MT, Werner BC. Patient-related risk factors for periprosthetic ankle joint infection: an analysis of 6977 total ankle arthroplasties. J Foot Ankle Surg. 2018;57(2):269-272. doi:10.1053/j.jfas.2017.09.006 [DOI] [PubMed] [Google Scholar]
- 2. Ballin M, Nordström P, Niklasson J, et al. Daily step count and incident diabetes in community-dwelling 70-year-olds: a prospective cohort study. BMC Public Health. 2020;20(1):1-10. doi: 10.1186/S12889-020-09929-2/FIGURES/2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Best MJ, Nguyen S, Shafiq B, Ficke JR. Risk factors for complications, longer hospital stay, and readmission after total ankle arthroplasty. Foot Ankle Spec. 2022;15(2):142-149. doi:10.1177/1938640020950147 [DOI] [PubMed] [Google Scholar]
- 4. Bianchi L, Volpato S. Muscle dysfunction in type 2 diabetes: a major threat to patient’s mobility and independence. Acta Diabetol. 2016;53(6):879-889. doi: 10.1007/S00592-016-0880-Y [DOI] [PubMed] [Google Scholar]
- 5. Choi WJ, Lee JS, Lee M, Park JH, Lee JW. The impact of diabetes on the short- to mid-term outcome of total ankle replacement. Bone Joint J. 2014;96-B(12):1674-1680. doi:10.1302/0301-620X.96B12.34364 [DOI] [PubMed] [Google Scholar]
- 6. Cisternas MG, Murphy L, Sacks JJ, Solomon DH, Pasta DJ, Helmick CG. Alternative methods for defining osteoarthritis and the impact on estimating prevalence in a US population-based survey. Arthritis Care Res. 2016;68(5):574-580. doi: 10.1002/acr.22721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cunningham D, Karas V, DeOrio J, Nunley J, Easley M, Adams S. Patient risk factors do not impact 90-day readmission and emergency department visitation after total ankle arthroplasty: implications for the comprehensive care for joint replacement (CJR) bundled payment plan. J Bone Joint Surg Am. 2018;100(15):1289-1297. doi: 10.2106/JBJS.17.01149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dalat F, Trouillet F, Fessy MH, Bourdin M, Besse JL. Comparison of quality of life following total ankle arthroplasty and ankle arthrodesis: retrospective study of 54 cases. Orthop Traumatol Surg Res. 2014;100(7):761-766. doi: 10.1016/J.OTSR.2014.07.018 [DOI] [PubMed] [Google Scholar]
- 9. Fanelli D, Mercurio M, Castioni D, Sanzo V, Gasparini G, Galasso O. End-stage ankle osteoarthritis: arthroplasty offers better quality of life than arthrodesis with similar complication and re-operation rates-an updated meta-analysis of comparative studies. Int Orthop. 2021;45(9):2177-2191. doi: 10.1007/S00264-021-05053-X [DOI] [PubMed] [Google Scholar]
- 10. Gougoulias NE, Khanna A, Maffulli N. History and evolution in total ankle arthroplasty. Br Med Bull. 2009;89(1):111-151. doi: 10.1093/BMB/LDN039 [DOI] [PubMed] [Google Scholar]
- 11. Gross CE, Green CL, DeOrio JK, Easley M, Adams S, Nunley JA. Impact of diabetes on outcome of total ankle replacement. Foot Ankle Int. 2015;36(10):1144-1149. doi: 10.1177/1071100715585575 [DOI] [PubMed] [Google Scholar]
- 12. Halter JB, Musi N, Horne FMF, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578. doi: 10.2337/DB14-0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hirvensalo M, Rantanen T, Heikkinen E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J Am Geriatr Soc. 2000;48(5):493-498. [DOI] [PubMed] [Google Scholar]
- 14. Iglay K, Hannachi H, Howie PJ, et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32(7):1243-1252. [DOI] [PubMed] [Google Scholar]
- 15. Lawton CD, Butler BA, Dekker RG, Prescott A, Kadakia AR. Total ankle arthroplasty versus ankle arthrodesis—a comparison of outcomes over the last decade. J Orthop Surg Res. 2017;12(1):1-11. doi: 10.1186/s13018-017-0576-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lawton CD, Prescott A, Butler BA, et al. Modern total ankle arthroplasty versus ankle arthrodesis: a systematic review and meta-analysis. Orthop Rev (Pavia). 2020;12(3):8279. doi: 10.4081/OR.2020.8279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lee JW, Im WY, Song SY, Choi JY, Kim SJ. Analysis of early failure rate and its risk factor with 2157 total ankle replacements. Sci Rep. 2021;11(1):1901. doi:10.1038/s41598-021-81576-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Myers TG, Lowery NJ, Frykberg RG, Wukich DK. Ankle and hindfoot fusions: comparison of outcomes in patients with and without diabetes. Foot Ankle Int. 2012;33(1):20-28. doi:10.3113/FAI.2012.0020 [DOI] [PubMed] [Google Scholar]
- 19. Nieves-Plaza M, Castro-Santana LE, Font YM, Mayor AM, Vilá LM. Association of hand or knee osteoarthritis with diabetes mellitus in a population of Hispanics from Puerto Rico. J Clin Rheumatol. 2013;19(1):1-6. doi: 10.1097/RHU.0B013E31827CD578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Olaya B, Moneta MV, Doménech-Abella J, et al. Mobility difficulties, physical activity, and all-cause mortality risk in a nationally representative sample of older adults. J Gerontol A Biol Sci Med Sci. 2018;73(9):1272-1279. doi: 10.1093/GERONA/GLX121 [DOI] [PubMed] [Google Scholar]
- 21. Palazzo C, Nguyen C, Lefevre-Colau MM, Rannou F, Poiraudeau S. Risk factors and burden of osteoarthritis. Ann Phys Rehabil Med. 2016;59(3):134-138. doi: 10.1016/J.REHAB.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 22. Patton D, Kiewiet N, Brage M. Infected total ankle arthroplasty: risk factors and treatment options. Foot Ankle Int. 2015;36(6):626-634. doi:10.1177/1071100714568869 [DOI] [PubMed] [Google Scholar]
- 23. Pedowitz DI, Kane JM, Smith GM, Saffel HL, Comer C, Raikin SM. Total ankle arthroplasty versus ankle arthrodesis: a comparative analysis of arc of movement and functional outcomes. Bone Joint J. 2016;98-B(5):634-640. doi: 10.1302/0301-620X.98B5.36887 [DOI] [PubMed] [Google Scholar]
- 24. Pitts C, Alexander B, Washington J, et al. Factors affecting the outcomes of tibiotalocalcaneal fusion. Bone Joint J. 2020;102-B(3):345-351. doi:10.1302/0301-620X.102B3.BJJ-2019-1325.R1 [DOI] [PubMed] [Google Scholar]
- 25. Raikin SM, Kane J, Ciminiello ME. Risk factors for incision-healing complications following total ankle arthroplasty. J Bone Joint Surg Am. 2010;92(12):2150-2155. doi:10.2106/JBJS.I.00870 [DOI] [PubMed] [Google Scholar]
- 26. Rajapakshe S, Sutherland JM, Wing K, et al. Health and quality of life outcomes among patients undergoing surgery for end-stage ankle arthritis. Foot Ankle Int. 2019;40(10):1129-1139. doi: 10.1177/1071100719856888 [DOI] [PubMed] [Google Scholar]
- 27. Saltzman CL, Zimmerman MB, O’Rourke M, Brown TD, Buckwalter JA, Johnston R. Impact of comorbidities on the measurement of health in patients with ankle osteoarthritis. J Bone Joint Surg Am. 2006;88(11):2366-2372. [DOI] [PubMed] [Google Scholar]
- 28. Schett G, Kleyer A, Perricone C, et al. Diabetes is an independent predictor for severe osteoarthritis: results from a longitudinal cohort study. Diabetes Care. 2013;36(2):403-409. doi: 10.2337/dc12-0924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Schipper ON, Jiang JJ, Chen L, Koh J, Toolan BC. Effect of diabetes mellitus on perioperative complications and hospital outcomes after ankle arthrodesis and total ankle arthroplasty. Foot Ankle Int. 2015;36(3):258-267. doi:10.1177/1071100714555569 [DOI] [PubMed] [Google Scholar]
- 30. Shofer JB, Ledoux WR, Orendurff MS, et al. Step activity after surgical treatment of ankle arthritis. J Bone Joint Surg Am. 2019;101(13):1177-1184. doi: 10.2106/JBJS.18.00511 [DOI] [PubMed] [Google Scholar]
- 31. Sproule JA, Chin T, Amin A, et al. Clinical and radiographic outcomes of the mobility total ankle arthroplasty system: early results from a prospective multicenter study. Foot Ankle Int. 2013;34(4):491-497. doi: 10.1177/1071100713477610 [DOI] [PubMed] [Google Scholar]
- 32. Syed F, Ugwuoke A. Ankle arthroplasty: a review and summary of results from joint registries and recent studies. EFORT Open Rev. 2018;3(6):391. doi: 10.1302/2058-5241.3.170029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Welmer AK, Angleman S, Rydwik E, Fratiglioni L, Qiu C. Association of cardiovascular burden with mobility limitation among elderly people: a population-based study. PLoS One. 2013;8(5):e65815. doi: 10.1371/JOURNAL.PONE.0065815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wukich DK, Mallory BR, Suder NC, Rosario BL. Tibiotalocalcaneal arthrodesis using retrograde intramedullary nail fixation: comparison of patients with and without diabetes mellitus. J Foot Ankle Surg. 2015;54(5):876-882. doi: 10.1053/J.JFAS.2015.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wukich DK, Shen JYC, Ramirez CP, Irrgang JJ. Retrograde ankle arthrodesis using an intramedullary nail: a comparison of patients with and without diabetes mellitus. J Foot Ankle Surg. 2011;50(3):299-306. doi: 10.1053/J.JFAS.2010.12.028 [DOI] [PubMed] [Google Scholar]
- 36. Zhao X, Shah D, Gandhi K, et al. Clinical, humanistic, and economic burden of osteoarthritis among noninstitutionalized adults in the United States. Osteoarthritis Cartilage. 2019;27(11):1618-1626. doi: 10.1016/j.joca.2019.07.002 [DOI] [PubMed] [Google Scholar]