Highlights
-
•
Rotaviruses are the most common cause of acute gastroenteritis among children.
-
•
In Haiti, the most frequent genotype in the pre-vaccine period was G12P[8].
-
•
Equine-like G3P[8] strains dominated most years following vaccine introduction.
Keywords: Rotavirus genotypes, RT-PCR, Pre- and post-vaccination, Haiti
Abstract
Background
Haiti introduced a monovalent human group A rotavirus (RVA) vaccine (Rotarix) into its routine infant immunization program in April 2014. The goal of the surveillance program was to characterize RVA strains circulating in Haiti before and after RVA vaccine introduction.
Methods
Stool samples were collected from children <5 years old presenting with acute gastroenteritis at 16 hospitals in Haiti. RVA antigen enzyme immunoassay (EIA) testing was performed, and G and P genotypes were determined for positive specimens. In this study, genotype data for samples collected from May 2012 through April 2014 (the pre-vaccine introduction era) and May 2014 through July 2019 (post-vaccine introduction era) were analyzed.
Results
A total of 809 specimens were tested by the Centers for Disease Control and Prevention. During the pre-vaccine introduction era (May 2012 through April 2014), G12P[8] was the predominant genotype, detected in 88–94% of specimens. There was a high prevalence of the equine-like G3P[8] genotype among Haitian children with RVA after vaccine introduction.
Conclusions
The predominance of equine-like G3P[8] in three of five RVA seasons post-vaccine introduction suggests possible vaccine-specific selection pressure in Haiti. These temporal variations in RVA genotype predominance will require continued monitoring in Haiti as the vaccination program continues.
1. Introduction
Group A rotaviruses (RVA) are a major cause of diarrhea and death among children under five globally (Aliabadi et al., 2019). In 2016, there were an estimated 128 500 deaths by RVA worldwide, of which most occurred in developing countries (Troeger et al., 2018). In addition, nearly 40% of hospitalizations for severe diarrhea are due to RVA (MMWR, n.d.).
RVA belong to the Reoviridae family. They possess a triple-layered icosahedral capsid enclosing a genome of 11 segments of double-stranded RNA encoding six structural and five or six non-structural proteins (Esona and Gautam, 2015; Estes and Greenberg, 2013). The outer capsid proteins VP7 and VP4 define the G and P genotypes, respectively (Crawford et al., 2017). Currently, RVA are classified into 36 G and 51 P genotypes (Rotavirus Classification Working Group (RCWG), https://rega.kuleuven.be/cev/viralmetagenomics/virus-classification), and although a large number of G/P genotype combinations have been reported, the RVA genotypes G1P[8], G2P[4], G3P[8], G4P[8], G9P[8], and G12P[8] together are responsible for an estimated 90–95% of all RVA infections worldwide (Bányai et al., 2012; Esona and Gautam, 2015).
Monovalent Rotarix (GlaxoSmithKline, Rixensart, Belgium) and RotaTeq (Merck & Co., West Point, PA, USA) RVA vaccines have been approved and licensed in many countries. More recently, two additional vaccines, Rotavac (Bharat Biotech, Hyderabad, India) and Rotasil (Serum Institute of India, Pune, India) have been prequalified by the World Health Organization (WHO) for global use (Kirkwood and Steele, 2018). The introduction of RVA vaccines has been accompanied globally by a 59% reduction in hospitalization and emergency room visits for confirmed RVA cases and a 36% reduction in mortality due to gastroenteritis in children under 5 years of age (Burnett et al., 2020).
In Haiti, data from the 2010–2012 RVA seasons showed that acute diarrhea accounted for 26% of hospitalizations in children under 5 years and 13% of hospital deaths (Vinekar et al., 2015). Prior to vaccine introduction, G1P[8] was the predominant genotype circulating in Haiti, followed by G9P[8] (Esona et al., 2015). In April 2014, the Ministry of Health introduced the monovalent vaccine, Rotarix, which is an attenuated human G1P[8] RVA strain (Esona et al., 2015; Ward et al., 2008). Unusual RVA strains, such as the equine-like G3P[8], have been reported from the neighboring Dominican Republic, and these strains have been found to undergo genetic reassortment with locally circulating RVA strains of other genotypes (Katz et al., 2019). Studies have shown that RVA genotypes may change following the introduction of vaccines (Matthijnssens et al., 2009). It is known that as RVA are segmented viruses, they frequently undergo genetic changes through reassortment, but so far there is uncertainty about the link between genotype changes and vaccination, since RVA, by their nature as RNA viruses, have high mutagenic potential. (Desselberger, 2014). The consequences of these mutations on vaccine effectiveness are not yet established (Cates et al., 2021a). The objective of this study was to assess the impact of RVA vaccine introduction on the genotype distribution in Haiti, perform additional characterization of RVA strains detected, and look for vaccine strains in surveillance samples.
2. Materials and methods
2.1. Study design, specimen handling and transport
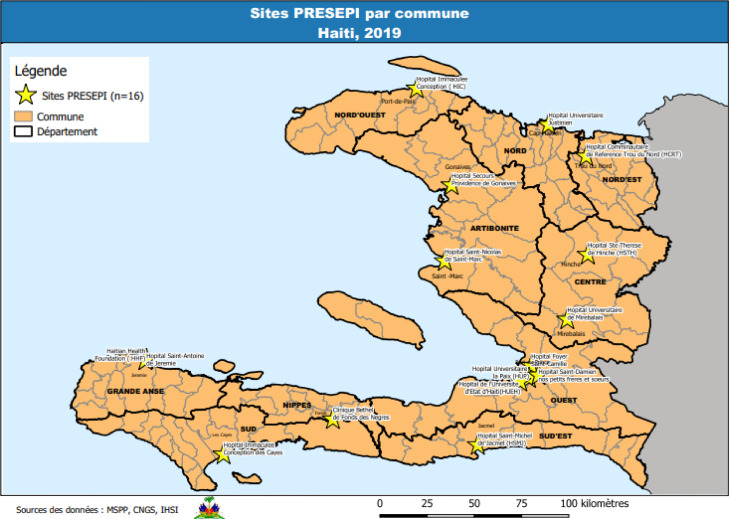
The enhanced laboratory-based surveillance system – PRESEpi – has been described previously (Lucien et al., 2015; Juin et al., 2017). In brief, it is an ongoing active surveillance system in which children <5 years old with acute gastroenteritis (AGE) are recruited from sentinel hospitals in Haiti. PRESEpi started with four hospitals, but had increased to 17 hospitals by the end of the study period in 2019 (Figure 1). This analysis includes data collected from May 2012 through April 2014 (pre-vaccination period, Table 1) and May 2014 through July 2019 (post-vaccination period, Table 2).
Figure 1.
Distribution of sites involved in the surveillance project in Haiti in 2019.
Table 1.
Distribution of specimens collected by site during the pre-vaccination period (May 2012 to April 2014).
| Site name | Frequency | Percentage |
| Hôpital Foyer Saint Camille (HFSC) | 601 | 37.45 |
| Hôpital de la Paix in Port-au-Prince (HUP) | 376 | 23.43 |
| Hôpital Saint Michel in Jacmel (SMJ) | 210 | 13.08 |
| Hôpital Saint Nicolas in St Marc (HSN) | 418 | 26.04 |
| Total | 1605 | 100 |
Table 2.
Distribution of specimens collected by site during the post-vaccination period (May 2014 to July 2019).
| Site name | Frequency | Percentage |
| Centre a Lit de Béthel (CAL) | 30 | 0.54 |
| Centre Médico-Social de Ouanaminthe (CMSO) | 5 | 0.09 |
| Hôpital Communautaire de Référence Trou du Nord | 3 | 0.05 |
| Hôpital Foyer Saint Camille | 895 | 16.07 |
| Haitian Health Foundation in Jeremie (HHF) | 7 | 0.13 |
| Hôpital Universitaire de la Paix in Port-au-Prince (HUP) | 745 | 13.38 |
| Hôpital de l'Université d'Etat d'Haiti | 445 | 7.99 |
| Hôpital Immaculée Conception de Port de Paix (HICP) | 36 | 0.65 |
| Hôpital Immaculée Conception des Cayes (HICC) | 55 | 0.99 |
| Hôpital la Providence des Gonaives (HPG) | 109 | 1.96 |
| Hôpital Saint Antoine de Jeremie (HSA) | 46 | 0.83 |
| Hôpital Saint Damien (HSD) | 1508 | 27.08 |
| Hôpital Saint Michel de Jacmel (SMJ) | 589 | 10.58 |
| Hôpital Saint Nicolas de St Marc (HSN) | 896 | 16.09 |
| Hôpital Sainte Thérèse de Hinche | 19 | 0.34 |
| Hôpital Universitaire de Mirebalais (HUM) | 57 | 1.02 |
| Hôpital Universitaire Justinien (HUJ) | 123 | 2.21 |
| Total | 5568 | 100.00 |
After obtaining informed consent from the parent(s) or adult guardian, a single diarrheal stool sample was collected from each enrolled child. The specimens were stored at the sites at 4°C until they were transported on ice packs to the National Public Health laboratory in Port-au-Prince, Haiti. All diarrheal stool specimens were screened for RVA antigen using the Rotaclone enzyme immunoassay (EIA) kit (Premier Rotaclone; Meridian Diagnostics, Cincinnati, OH, USA), according to the manufacturer's instructions. This testing was done at the National Laboratory of Public Health in Haiti. RVA-positive stool specimens were shipped on dry ice to the US Centers for Disease Control and Prevention (CDC), Atlanta, GA, USA for genotyping and sequencing analysis.
2.2. Stool processing and nucleic acid extraction
A 10% stool suspension was prepared for each sample using phosphate-buffered saline, and RNA was extracted from the suspension using the MagNA Pure Compact RNA extraction kit on the MagNA Pure Compact instrument (Roche Applied Science, Indianapolis, IN, USA) following the manufacturer's instructions. Prior to each of the above extraction procedures, 2 µl of 109 U/µl of MS2 bacteriophage RNA (ZeptoMetrix, Buffalo, NY, USA) were spiked into a 98 µl volume of 10% stool suspension to serve as an internal process control.
2.3. Real-time reverse transcription PCR detection of wild-type RVA (NSP3), equine-like G3 (VP7), and RVA vaccine strains (RV5 and RV1)
Viral RNA extract from each sample was tested by NSP3 (Mijatovic-Rustempasic et al., 2013) and VP7 equine-like G3 (Katz et al., 2021) quantitative reverse transcription PCR (qRT-PCR) assays. RV5 and RV1 qRT-PCR assays (Gautam et al., 2016) were used to screen for RVA vaccine strains.
2.4. VP7 and VP4 genotyping and sequencing
Genotyping was performed using reverse transcription PCR (RT-PCR) to determine the G and P genotypes. VP7 and VP4 genotyping RT-PCR was performed using a conventional multiplexed one-step amplification process with slight modifications (Esona et al., 2015). In brief, the genotype G2 (G2-R4), G4 (G4-R2), and G9 (G9-R2) specific primers were replaced with updated versions: G2-R1 (TAT GTA GTC CAT YGT ATT AGT), G4-R1 (GAG CAT TCG MTA ATA MTG ATA ATA C), and G9-R3 (CAG AGT ATY YTT CCA TTC HGT ATC TCC) (Esona et al., 2021). The VP7 and VP4 conventional multiplexed one-step RT-PCR genotyping product was electrophoresis on 3% agarose gel containing GelRed (Biotium, Heyward, CA, USA) for 2–3 h at 100 V, and the products were detected under UV transillumination or were analyzed on the LabChip GX instrument (Caliper Life Sciences, Hopkinton, MA, USA) using the HT DNA 5K reagent kit (Dual Protocol DNA Analysis and Quantitation) with the HT Extended Range LabChip (Caliper Life Sciences), as described previously (Esona et al., 2015).
For VP7 and VP4 genotype confirmation, nucleotide sequencing of all samples that were assigned a G and P genotype was performed using previously published consensus primer pair 9Con1-L/VP7R or VP7Rdeg for VP7 (Esona et al., 2009; Das et al., 1994; Hull et al., 2011) and con3/con2 for VP4 (Gentsch et al., 1992). Analysis of RT-PCR reactions by gel electrophoresis, amplicon purification, and DNA sequencing was conducted as described previously (Hull et al., 2011; Esona et al., 2009). Forward and reverse sequences were assembled using Sequencer software version 4.8 (Gene Codes Corporation, Inc., Ann Arbor, MI, USA). The consensus sequences obtained were compared with existing RVA sequences in the GenBank database using the BLASTN program at the National Center for Biotechnology Information website (available at: http://www.ncbi.nlm.gov/BLAST/).
3. Results
A total of 1605 stool specimens were collected during the pre-vaccination period (Table 1), while 5568 stool specimens were collected during the post-vaccination period (Table 2). Of the 7173 stool specimens collected, 6257 (87.2%) were screened for RVA antigen, of which 980 (15.7%) tested positive for RVA antigen. Of these 980 RVA antigen-positive specimens, 809 (82.6%) were shipped and tested at CDC; 171 specimens had insufficient volume and were not shipped.
3.1. qRT-PCR and RT-PCR data
All 809 RVA antigen-positive samples tested at the CDC contained amplifiable RVA RNA by NSP3 qRT-PCR, and the VP7 equine-like G3 qRT-PCR assay was able to detect equine-like G3 in 387 (48%) samples that were confirmed by Sanger sequencing. Thus, VP7 (G) and VP4 (P) genotypes were assigned to all 809 RVA-positive samples. Equine-like G3P[8] represented the predominant genotype (48%) circulating in Haiti during the study period, followed by G12P[8] (21%), G1P[8] (13.4%), G3P[6] (8.2%), and G12P[6] (4.3%). Other uncommon genotypes such as G4P[6], G3P[8] (non-equine-like G3P[8]), G9P[8], G2P[4], and mixed (G9G4P[8], G3G12P[6]P[8], G3G2P[8]/P[4]) were found circulating at low levels (≤1%). Twenty-two samples (3%) could not be assigned both G and P type (non-typeable samples) (Table 3, Figure 2). The genotype distribution differed according to the vaccination period.
Table 3.
Overall distribution of rotavirus G and P types detected in Haitian children between 2012 and 2019. RVA seasons 2012–2013 and 2013–2014 are the pre-vaccination periods; seasons 2014–2015 through 2018–2019 are the post-vaccination periods.
| 2012-2013 | 2013-2014 | 2014-2015 | 2015-2016 | 2016-2017 | 2017-2018 | 2018-2019 | Totals | |
|---|---|---|---|---|---|---|---|---|
| G3P[8]* | 0 | 0 | 0 | 227 | 9 | 82 | 69 | 387 (48%) |
| G12P[8] | 53 | 82 | 30 | 4 | 1 | 0 | 0 | 170 (21%) |
| G1P[8] | 2 | 1 | 6 | 2 | 68 | 25 | 4 | 108 (13.4%) |
| G3P[6] | 0 | 3 | 58 | 4 | 1 | 0 | 0 | 66 (8.2%) |
| G12P[6] | 2 | 0 | 2 | 0 | 0 | 0 | 31 | 35 (4.3%) |
| G4P[6] | 0 | 0 | 2 | 0 | 0 | 3 | 3 | 8 (1%) |
| G3P[8] | 1 | 1 | 3 | 1 | 0 | 0 | 0 | 6 (<1%) |
| G9P[8] | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 2 (<1%) |
| G2P[4] | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 (<1%) |
| GNTP[NT] | 0 | 0 | 0 | 1 | 0 | 9 | 12 | 22 (3%) |
| Mixed | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 4 (<1%) |
| Total | 60 (7%) | 87 (10.8%) | 102 (12.6%) | 240 (29.7%) | 79 (9.8%) | 121 (15%) | 120 (15%) | 809 (100%) |
Equine-like G3 strains.
Figure 2.
Genotype prevalence by season. Mixed genotypes included G3G2P[4]/[8], G12G3P[6]/[8], G4G9P[8], and G12P[6]/[8]. The pre- and post-vaccination periods are indicated above the chart.
3.2. Genotype distribution during the pre-vaccination period (May 2012 to April 2014)
From May 2012 to April 2014, 147 specimens were genotyped and confirmed by Sanger sequencing. The most frequent G genotypes were as follows (in order of frequency): G12 (n = 135, 91.8%) specimens, G1 (n = 4, 2.0%), and non-equine-like G3 (n = 5, 3.5%). The most common P genotypes were P[8] (n = 140, 95.2%) and P[6] (n = 5, 3.4%). The predominant G and P combination was G12P[8] (n = 135, 91.4%), followed by G1P[8] (n = 3, 2.0%) and G3P[6] (n = 3, 2.0%); G12P[6] and non-equine-like G3P[8] had two specimens each (1.4%). In the two pre-vaccine years analyzed, there was an overwhelming predominance of the same genotype, G12P[8], at 88.3% in 2012–2013 and 94.3% in 2013–2014 (Table 3, Figure 2).
3.3. Genotype distribution during the post-vaccination period (May 2014 to July 2019)
From May 2014 to July 2019, 662 RVA-positive specimens were genotyped and confirmed by Sanger sequencing. The most frequent G genotypes were as follows: G3 (n = 454, 68.6%), G1 (n = 105, 15.9%), and G12 (n = 68, 10.3%). The most prevalent P genotypes were P[8] (n = 531, 80.2%) and P[6] (n = 104, 15.7%). The most frequent G and P combinations were equine-like G3P[8] (n = 387, 58.5%), G1P[8] (n = 105, 15.9%), and G12P[8] (n = 35, 5.3%). During the 2014–2015 vaccination period there was a predominance of G3P[6] (n = 58, 56.9%) and a decline in G12P[8] (n = 30, 29.4%) by comparison with the pre-vaccine period. The equine-like G3P[8] genotype dramatically emerged in 2015–2016 (n = 227, 94.6%) and dominated in both the 2017–2018 (n = 82, 67.8%) and 2018–2019 (n = 69, 57.5%) seasons. Genotype G1P[8] dominated in 2016–2017 (n = 68, 86.1%) and equine-like G3P[8] receded to 11.4% (n = 9) (Table 3, Figure 2). Vaccine strains were not detected in any specimens.
4. Discussion
This study is novel in providing a detailed report of RVA genotype data from Haiti. In this study, it was found that the most frequent genotype in the pre-vaccine introduction period was G12P[8] and that equine-like G3P[8] strains dominated in most of the years following vaccine introduction.
The G12 genotype remained the predominant genotype for the 2 years (2012–2014) of the pre-vaccination period at a percentage of more than 90%, and after that it dropped drastically. In some countries, the emergence of G12 followed the introduction of RVA vaccine, whereas in other countries, G12 pre-existed the introduction of RVA vaccine (Lartey et al., 2018; Steele et al., 2012). Regarding the European countries, the predominant genotype in England during the pre-vaccine period (2006–2013) was G1P[8] at 55%, and after the introduction of Rotarix, the predominant genotype was G2P[4] at 26% (Hungerford et al., 2019). In Brazil, a study conducted during the post-vaccine period shown that G3P[8] was the most prevalent genotype during the 2-year period 2018–2019, and sequencing some of the strains proved that they were equine-like G3P[8] genotype (Gutierrez et al., 2020). In the United States, there was a predominance of G1P[8] from 1996 to 2005 before the vaccine introduction, but after introduction of Rotarix and RotaTeq vaccines, G1P[8] was replaced first by G3P[8] and then by G12P[8] (Esona et al., 2021). In Australia, during the pre-vaccine period (1995–2006), the predominant genotype was G1P[8], but after vaccine introduction there was a replacement of the genotype with G12P[8] in locations using RotaTeq, and equine-like G3P[8] and G2P[4] in those using Rotarix (Roczo-Farkas et al., n.d.). G12 is a genotype that was discovered in 1987 in the Philippines in children (Taniguchi et al., 1990), subsequently spreading across Asia and the world (Rahman et al., 2007). Rotarix demonstrated efficacy against G12 (51.5%) in a study conducted in South Africa and Malawi (Steele et al., 2012); in the USA, Rotarix vaccine effectiveness against G12P[8] was 82% (Payne et al., 2015).
During the post-vaccination period in the present study, there was a shift to equine-like G3P[8] predominance, with the dramatic appearance of equine-like G3P[8] in 2015–2016 accompanied by a surge in RVA activity in Haiti. Equine-like strains have been identified in many other countries (Tacharoenmuang et al., 2020; Perkins et al., 2017; Utsumi et al., 2018; Kikuchi et al., 2018). Nevertheless, the importance of equine-like G3 strains seems to vary both between countries and inside the same country. Between periods: in Australia, for example, it represented 37% of positive fecal samples in 2013 and 14.4% in 2014 (Cowley et al., 2016). In other countries, like the Dominican Republic, the introduction of monovalent rotavirus vaccine was followed by the emergence and predominance of equine-like strains (Katz et al., 2019). It was observed that in areas where monovalent rotavirus vaccine was used, there was a predominance of equine-like G3P[8] and G2P[4], whereas in locations where RotaTeq vaccine was used, there was a predominance of G12P[8]. Hence this suggests that the type of vaccine used can have a different impact on strain circulation (Roczo-Farkas et al., n.d.). The impact of vaccination on these equine-like strains needs to be monitored and studied (Cates et al., 2021b). The change in genotype predominance between the pre- and post-vaccination period could potentially be related to vaccine introduction. In Haiti, the vaccine effectiveness estimate for Rotarix against this genotype was 64% and was comparable to the vaccine effectiveness against other genotypes in the country (Burnett et al., 2021).
The P[8] genotype was the most frequent both in the pre-vaccination and post-vaccination periods. This ties in with its determining role in the etiology of numerous RVA infections in several countries (Aydin and Aktaş, 2017). It is also interesting to note that G1P[8] did not constitute a major genotype in the present study and dominated only in 2016–2017. Historically, G1P[8] has been the most frequent genotype worldwide before vaccine introduction (Ward et al., 2008) and its prevalence typically decreases after the introduction of vaccines (Kirkwood et al., 2011). In Haiti, the predominance of G1P[8] for a single season, 2016–2017, during the post-vaccination period does not follow this trend, and its short-term predominance during this period is difficult to explain, especially after the emergence of the equine-like G3P[8] genotype in the preceding season.
In this study, the P[6] genotype was detected in 13.5% of the 809 RVA-positive specimens. Except in Africa, where it has a higher prevalence, the P[6] genotype is generally absent in others areas of the world (Todd et al., 2010). One explanation for this observation is that Lewis-negative susceptibility is more common in that population and is associated with RVA P[6] susceptibility (Sharma et al., 2020). In Haiti, most of the population traces its origins to Africa, and perhaps this helps explain the high P[6] prevalence in the present study. It was also noted that the overall P[6] genotype prevalence during the pre-vaccination period was 2%, while during the post-vaccination period it was 15%, potentially indicating that vaccine selection pressure played a role in this increase in P[6] genotype detection.
The fluctuation in RVA genotypes is a known phenomenon and is observed sometimes in countries before and after vaccine introduction. However, to date, there is no clear relationship between vaccine introduction and genotype fluctuation, because this type of fluctuation has been observed during the pre-vaccine periods (Buesa and Martínez-Costa, 2014).
Despite the excellent data obtained in this study, limitations are as follows: (1) more sites participated and more patients were enrolled during the post-vaccine period compared to the pre-vaccine period, which may have affected the interpretation of the genotype distribution; (2) no transition window was observed between the pre-vaccine and post-vaccine periods. This transition period must also be correlated with the vaccination coverage, which can have an impact on the circulation of rotavirus strains.
In conclusion, this study highlights that there was genotype fluctuation between the pre-vaccine period (May 2012 to April 2014) and the post-vaccine period (May 2014 to July 2019) in Haiti. A high prevalence of the equine-like G3P[8] genotype was observed among Haitian children with RVA after vaccine introduction. Further, the study revealed that the strains that are circulating in Haiti are generally reported as vaccine-sensitive. Therefore, it is important to continue to conduct epidemiological surveillance to help identify new genotypes that could emerge and continue to monitor genetic diversity.
Acknowledgments
Acknowledgements
We thank the staff of the Viral Gastroenteritis Branch at the Centers for Disease Control and Prevention, as well as those in Laboratoire National de Santé Publique, Haiti, Pan American Health Organization (PAHO), and CDC Country Office, Haiti who participated in this study. We also, thank all of the children and their parents who participated in this study.
Declarations
Funding source
This research was supported by the Pan American Health Organization (PAHO/WHO) and the US Centers for Disease Control and Prevention (https://www.cdc.gov/) for the technical expertise, and the Haiti Ministry of Public Health and Population.
Ethics statement
Verbal consent was obtained from the parents or guardians of minors. The verbal consent procedures and the other activities described in this evaluation were approved as part of a non-research surveillance activity by both the CDC Institutional Review Board and the Haiti National Bioethics Committee.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Disclaimer:
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Names of specific vendors, manufacturers, or products are included for public health and informational purposes; inclusion does not imply endorsement of the vendors, manufacturers, or products by the Centers for Disease Control and Prevention or the US Department of Health and Human Services.
References
- Aliabadi Negar, Antoni Sébastien, Mwenda Jason M., Weldegebriel Goitom, Biey Joseph N.M., Cheikh Dah, Fahmy Kamal, et al. “Global Impact of Rotavirus Vaccine Introduction on Rotavirus Hospitalisations among Children under 5 Years of Age, 2008–16: Findings from the Global Rotavirus Surveillance Network”. The Lancet Global Health. 2019;7(7):e893–e903. doi: 10.1016/S2214-109X(19)30207-4/ATTACHMENT/33BE31E6-AD23-44E6-8965-175ADB0BC4E6/MMC1.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aydin Hakan, Aktaş Osman. “Rotavirus Genotypes in Children with Gastroenteritis in Erzurum: First Detection of G12P[6]and G12P[8]Genotypes in Turkey”. Przeglad Gastroenterologiczny. 2017;12(2):122–127. doi: 10.5114/pg.2016.59423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bányai Krisztián, László Brigitta, Duque Jazmin, Duncan Steele A., Anthony S. Nelson E., Gentsch Jon R., Parashar Umesh D. “Systematic Review of Regional and Temporal Trends in Global Rotavirus Strain Diversity in the Pre Rotavirus Vaccine Era: Insights for Understanding the Impact of Rotavirus Vaccination Programs”. Vaccine. 2012;30(SUPPL. 1) doi: 10.1016/j.vaccine.2011.09.111. [DOI] [PubMed] [Google Scholar]
- Buesa Javier, Martínez-Costa Cecilia. “Rotavirus Infections, Vaccines and Virus Variability”. Enfermedades Infecciosas y Microbiología Clínica. 2014;32(5):277–279. doi: 10.1016/J.EIMC.2014.03.001. [DOI] [PubMed] [Google Scholar]
- Burnett Eleanor, Juin Stanley, Esona Mathew D., Desormeaux Anne Marie, Aliabadi Negar, Pierre Manise, Andre-Alboth Jocelyn, et al. “Effectiveness of Monovalent Rotavirus Vaccine against Hospitalizations Due to All Rotavirus and Equine-like G3P[8]Genotypes in Haiti 2014-2019”. Vaccine. 2021;39(32):4458–4462. doi: 10.1016/J.VACCINE.2021.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett Eleanor, Parashar Umesh D., Tate Jacqueline E. “Global Impact of Rotavirus Vaccination on Diarrhea Hospitalizations and Deaths Among Children <5 Years Old: 2006–2019”. The Journal of Infectious Diseases. 2020;222(10):1731–1739. doi: 10.1093/INFDIS/JIAA081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cates Jordan E., Amin Avnika B., Tate Jacqueline E., Lopman Ben, Parashar Umesh. “Do Rotavirus Strains Affect Vaccine Effectiveness? A Systematic Review and Meta-Analysis”. The Pediatric Infectious Disease Journal. 2021;40(12):1135–1143. doi: 10.1097/INF.0000000000003286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cates Jordan E., Amin Avnika B., Tate Jacqueline E., Lopman Ben, Parashar Umesh. “Do Rotavirus Strains Affect Vaccine Effectiveness? A Systematic Review and Meta-Analysis”. Pediatric Infectious Disease Journal. 2021;40(12):1135–1143. doi: 10.1097/INF.0000000000003286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowley Daniel, Donato Celeste M., Roczo-Farkas Susie, Kirkwood Carl D. “Emergence of a Novel Equine-like G3P[8]Intergenogroup Reassortant Rotavirus Strain Associated with Gastroenteritis in Australian Children”. Journal of General Virology. 2016;97(2):403–410. doi: 10.1099/JGV.0.000352/CITE/REFWORKS. [DOI] [PubMed] [Google Scholar]
- Crawford Sue E., Ramani Sasirekha, Tate Jacqueline E., Parashar Umesh D., Svensson Lennart, Hagbom Marie, Franco Manuel A., et al. “Rotavirus Infection”. Nature Reviews Disease Primers. 2017;3(November):17083. doi: 10.1038/nrdp.2017.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das B.K., Gentsch J.R., Cicirello H.G., Woods P.A., Gupta A., Ramachandran M., Kumar R., Bhan M.K., Glass R.I. “Characterization of Rotavirus Strains from Newborns in New Delhi, India”. Journal of Clinical Microbiology. 1994 doi: 10.1128/jcm.32.7.1820-1822.1994. American Society for Microbiology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desselberger Ulrich. Virus Research. Elsevier; 2014. “Rotaviruses”. [DOI] [PubMed] [Google Scholar]
- Esona M.D., Geyer A., Page N., Trabelsi A., Fodha I., Aminu M., Agbaya V.A., et al. “Genomic Characterization of Human Rotavirus G8 Strains from the African Rotavirus Network: Relationship to Animal Rotaviruses”. Journal of Medical Virology. 2009;81(5):937–951. doi: 10.1002/jmv.21468. [DOI] [PubMed] [Google Scholar]
- Esona M.D., Buteau J., Lucien M.A.B., Joseph G.A., Leshem E., Boncy J., Katz M.A., Bowen M.D., Balajee S.A. “Rotavirus Group A Genotypes Detected through Diarrheal Disease Surveillance in Haiti, 2012”. American Journal of Tropical Medicine and Hygiene. 2015;93(1) doi: 10.4269/ajtmh.14-0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esona Mathew D., Gautam Rashi. Clinics in Laboratory Medicine. W.B. Saunders; 2015. “Rotavirus”. [DOI] [PubMed] [Google Scholar]
- Esona Mathew D., Gautam Rashi, Tam Ka Ian, Williams Alice, Mijatovic-Rustempasic Slavica, Bowen Michael D. “Multiplexed One-Step RT-PCR VP7 and VP4 Genotyping Assays for Rotaviruses Using Updated Primers”. Journal of Virological Methods. 2015;223(October):96–104. doi: 10.1016/j.jviromet.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esona Mathew D., Leanne Ward M., Wikswo Mary E., Rustempasic Slavica M., Gautam Rashi, Perkins Charity, Selvarangan Rangaraj, et al. “Rotavirus Genotype Trends and Gastrointestinal Pathogen Detection in the United States, 2014–2016: Results From the New Vaccine Surveillance Network”. The Journal of Infectious Diseases. 2021;224(9):1539–1549. doi: 10.1093/INFDIS/JIAB177. [DOI] [PubMed] [Google Scholar]
- Esona Mathew D, Leanne Ward M., Wikswo Mary E., Rustempasic Slavica M., Gautam Rashi, Perkins Charity, Selvarangan Rangaraj, et al. “Rotavirus Genotype Trends and Gastrointestinal Pathogen Detection in the United States, 2014–2016: Results From the New Vaccine Surveillance Network”. The Journal of Infectious Diseases. 2021;XX(April):1–11. doi: 10.1093/INFDIS/JIAB177. [DOI] [PubMed] [Google Scholar]
- Estes, MK, and HB Greenberg. 2013. Rotaviruses. Edited by DM Knipe, PM Howley, JI Cohen, DE Griffin, RA Lamb, MA Martin, VR Racaniello, and B Roizman. 6th ed. Wolters Kluwer/Lippincott, Williams and Wilkins.
- Gautam Rashi, Mijatovic-Rustempasic Slavica, Esona Mathew D., Tam Ka Ian, Quaye Osbourne, Bowen Michael D. “One-Step Multiplex Real-Time RT-PCR Assay for Detecting and Genotyping Wild-Type Group A Rotavirus Strains and Vaccine Strains (Rotarix® and RotaTeq®) in Stool Samples”. PeerJ. 2016;4(1) doi: 10.7717/PEERJ.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentsch J.R., Glass R.I., Woods P., Gouvea V., Gorziglia M., Flores J., Das B.K., Bhan M.K. “Identification of Group A Rotavirus Gene 4 Types by Polymerase Chain Reaction”. Journal of Clinical Microbiology. 1992;30(6):1365–1373. doi: 10.1128/jcm.30.6.1365-1373.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez Meylin Bautista, Fialho Alexandre Madi, Maranhão Adriana Gonçalves, Malta Fábio Correia, Andrade Juliana da Silva Ribeiro de, Assis Rosane Maria Santos de, Mouta Sérgio da Silva E, Miagostovich Marize Pereira, Leite José Paulo Gagliardi, Fumian Tulio Machado. “Rotavirus A in Brazil: Molecular Epidemiology and Surveillance during 2018-2019”. Pathogens (Basel, Switzerland) 2020;9(7):1–15. doi: 10.3390/pathogens9070515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull Jennifer J., Teel Elizabeth N., Kerin Tara K., Freeman Molly M., Esona Mathew D., Gentsch Jon R., Cortese Margaret M., Parashar Umesh D., Glass Roger I., Bowen Michael D. “United States Rotavirus Strain Surveillance from 2005 to 2008: Genotype Prevalence before and after Vaccine Introduction”. Pediatric Infectious Disease Journal. 2011;30(SUPPL. 1) doi: 10.1097/INF.0b013e3181fefd78. [DOI] [PubMed] [Google Scholar]
- Hungerford Daniel, Allen David J., Nawaz Sameena, Collins Sarah, Ladhani Shamez, Vivancos Roberto, Iturriza-Gómara Miren. “Impact of Rotavirus Vaccination on Rotavirus Genotype Distribution and Diversity in England, September 2006 to August 2016”. Eurosurveillance. 2019;24(6) doi: 10.2807/1560-7917.ES.2019.24.6.1700774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juin Stanley, Schaad Nicolas, Lafontant Donald, Joseph Gerard A., Barzilay Ezra, Boncy Jacques, Barrais Robert, et al. “Strengthening National Disease Surveillance and Response-Haiti, 2010-2015”. The American Journal of Tropical Medicine and Hygiene. 2017;97(4_Suppl):12–20. doi: 10.4269/AJTMH.16-0948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz Eric M., Esona Mathew D., Betrapally Naga S., Leon Lucia A.De La Cruz De, Neira Yenny R., Rey Gloria J., Bowen Michael D. “Whole-Gene Analysis of Inter-Genogroup Reassortant Rotaviruses from the Dominican Republic: Emergence of Equine-like G3 Strains and Evidence of Their Reassortment with Locally-Circulating Strains”. Virology. 2019;534(August):114–131. doi: 10.1016/J.VIROL.2019.06.007. [DOI] [PubMed] [Google Scholar]
- Katz Eric M., Esona Mathew D., Gautam Rashi, Bowen Michael D. “Development of a Real-Time Reverse Transcription-PCR Assay To Detect and Quantify Group A Rotavirus Equine-Like G3 Strains”. Journal of Clinical Microbiology. 2021;59(11) doi: 10.1128/JCM.02602-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikuchi Wakako, Nakagomi Toyoko, Gauchan Punita, Ama Agbemabiese Chantal, Noguchi Atsuko, Nakagomi Osamu, Takahashi Tsutomu. “Detection in Japan of an Equine-like G3P[8]Reassortant Rotavirus A Strain That Is Highly Homologous to European Strains across All Genome Segments”. Archives of Virology. 2018;163(3):791–794. doi: 10.1007/s00705-017-3668-7. [DOI] [PubMed] [Google Scholar]
- Kirkwood Carl D., Boniface Karen, Barnes Graeme L., Bishop Ruth F. “Distribution of Rotavirus Genotypes after Introduction of Rotavirus Vaccines, Rotarix® and Rotateq®, into the National Immunization Program of Australia”. Pediatric Infectious Disease Journal. 2011;30(SUPPL. 1) doi: 10.1097/INF.0b013e3181fefd90. [DOI] [PubMed] [Google Scholar]
- Kirkwood Carl D., Steele A.Duncan. “Rotavirus Vaccines in China: Improvement Still Required”. JAMA Network Open. 2018 doi: 10.1001/jamanetworkopen.2018.1579. NLM (Medline) [DOI] [PubMed] [Google Scholar]
- Lartey Belinda L., Damanka Susan, Dennis Francis Ekow, Enweronu-Laryea Christabel C., Addo-Yobo Emmanuel, Ansong Daniel, Kwarteng-Owusu Sandra, et al. “Rotavirus Strain Distribution in Ghana Pre- and Post- Rotavirus Vaccine Introduction”. Vaccine. 2018;36(47):7238–7242. doi: 10.1016/j.vaccine.2018.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucien Mentor Ali Ber, Schaad Nicolas, Steenland Maria W., Mintz Eric D., Emmanuel Rossignol, Freeman Nicole, Boncy Jacques, Adrien Paul, Joseph Gerard A., Katz Mark A. “Identifying the Most Sensitive and Specific Sign and Symptom Combinations for Cholera: Results from an Analysis of Laboratory-Based Surveillance Data from Haiti, 2012-2013”. American Journal of Tropical Medicine and Hygiene. 2015;92(4):758–764. doi: 10.4269/ajtmh.14-0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthijnssens Jelle, Bilcke Joke, Ciarlet Max, Martella Vito, Bányai Krisztián, Rahman Mustafizur, Zeller Mark, Beutels Philippe, Van Damme Pierre, Van Ranst Marc. Future Microbiology. Future Medicine; London, UK: 2009. “Rotavirus Disease and Vaccination: Impact on Genotype Diversity”. [DOI] [PubMed] [Google Scholar]
- Mijatovic-Rustempasic Slavica, Tam Ka Ian, Kerin Tara K., Lewis Jamie M., Gautam Rashi, Quaye Osbourne, Gentsch Jon R., Bowen Michael D. “Sensitive and Specific Quantitative Detection of Rotavirus A by One-Step Real-Time Reverse Transcription-PCR Assay without Antecedent Double-Stranded-RNA Denaturation”. Journal of Clinical Microbiology. 2013;51(9):3047–3054. doi: 10.1128/JCM.01192-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MMWR. n.d. “Rotavirus Surveillance — Worldwide, 2001–2008”. Accessed March 10, 2021. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5746a3.htm.
- Payne Daniel C., Selvarangan Rangaraj, Azimi Parvin H., Boom Julie A., Englund Janet A., Staat Mary Allen, Halasa Natasha B., et al. “Long-Term Consistency in Rotavirus Vaccine Protection: RV5 and RV1 Vaccine Effectiveness in US Children, 2012-2013”. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America. 2015;61(12):1792–1799. doi: 10.1093/CID/CIV872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins Charity, Mijatovic-Rustempasic Slavica, Ward M.Leanne, Cortese Margaret M., Bowen Michael D. “Genomic Characterization of the First Equinelike G3P[8]Rotavirus Strain Detected in the United States”. Genome Announcements. 2017;5(47) doi: 10.1128/genomeA.01341-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman Mustafizur, Matthijnssens Jelle, Yang Xuelei, Delbeke Thomas, Arijs Ingrid, Taniguchi Koki, Iturriza-Gómara Miren, Iftekharuddin Nadia, Azim Tasnim, Van Ranst Marc. “Evolutionary History and Global Spread of the Emerging G12 Human Rotaviruses”. Journal of Virology. 2007;81(5):2382–2390. doi: 10.1128/jvi.01622-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roczo-Farkas, Susie, Carl D Kirkwood, Daniel Cowley, Graeme L Barnes, Ruth F Bishop, Nada Bogdanovic-Sakran, Karen Boniface, Celeste M Donato, and Julie E Bines.n.d. “The Impact of Rotavirus Vaccines on Genotype Diversity: A Comprehensive Analysis of 2 Decades of Australian Surveillance Data”. The Journal of Infectious Diseases546: 218. https://doi.org/10.1093/infdis/jiy197. [DOI] [PubMed]
- Roczo-Farkas, Susie, Carl D Kirkwood, Daniel Cowley, Graeme L Barnes, Ruth F Bishop, Nada Bogdanovic-Sakran, Karen Boniface, Celeste M Donato, and Julie E Bines. n.d. “The Impact of Rotavirus Vaccines on Genotype Diversity: A Comprehensive Analysis of 2 Decades of Australian Surveillance Data”. The Journal of Infectious Diseases546: 218. Accessed January 10, 2022. https://doi.org/10.1093/infdis/jiy197. [DOI] [PubMed]
- Sharma Sumit, Hagbom Marie, Svensson Lennart, Nordgren Johan. “The Impact of Human Genetic Polymorphisms on Rotavirus Susceptibility, Epidemiology, and Vaccine Take”. Viruses. 2020 doi: 10.3390/v12030324. MDPI AG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele Andrew D., Neuzil Kathleen M., Cunliffe Nigel A., Madhi Shabir A., Bos Pieter, Ngwira Bagrey, Witte Desiree, et al. “Human Rotavirus Vaccine RotarixTM Provides Protection against Diverse Circulating Rotavirus Strains in African Infants: A Randomized Controlled Trial”. BMC Infectious Diseases. 2012;12(September):213. doi: 10.1186/1471-2334-12-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tacharoenmuang Ratana, Komoto Satoshi, Guntapong Ratigorn, Upachai Sompong, Singchai Phakapun, Ide Tomihiko, Fukuda Saori, et al. “High Prevalence of Equine-like G3P[8]Rotavirus in Children and Adults with Acute Gastroenteritis in Thailand”. Journal of Medical Virology. 2020;92(2):174–186. doi: 10.1002/jmv.25591. [DOI] [PubMed] [Google Scholar]
- Taniguchi Koki, Urasawa Tomoko, Kobayashi Nobumichi, Gorziglia Mario, Urasawa Shozo. “Nucleotide Sequence of VP4 and VP7 Genes of Human Rotaviruses with Subgroup I Specificity and Long RNA Pattern: Implication for New G Serotype Specificity”. JOURNAL OF VIROLOGY. 1990;64 doi: 10.1128/jvi.64.11.5640-5644.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd Stacy, Page Nicola A., Duncan Steele A., Peenze Ina, Cunliffe Nigel A. “Rotavirus Strain Types Circulating in Africa: Review of Studies Published during 1997–2006”. The Journal of Infectious Diseases. 2010;202(S1):S34–S42. doi: 10.1086/653555. [DOI] [PubMed] [Google Scholar]
- Troeger Christopher, Khalil Ibrahim A., Rao Puja C., Cao Shujin, Blacker Brigette F., Ahmed Tahmeed, Armah George, et al. “Rotavirus Vaccination and the Global Burden of Rotavirus Diarrhea among Children Younger Than 5 Years”. JAMA Pediatrics. 2018;172(10):958–965. doi: 10.1001/jamapediatrics.2018.1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utsumi Takako, Wahyuni Rury Mega, Doan Yen Hai, Dinana Zayyin, Soegijanto Soegeng, Fujii Yoshiki, Juniastuti, et al. “Equine-like G3 Rotavirus Strains as Predominant Strains among Children in Indonesia in 2015–2016”. Infection, Genetics and Evolution. 2018;61(July):224–228. doi: 10.1016/j.meegid.2018.03.027. [DOI] [PubMed] [Google Scholar]
- Vinekar Kavita, Nicolas Schaad, Mentor Ali Ber Lucien, Eyal Leshem, Ikwo K.Oboho, Gerard Joseph, Stanley Juin, et al. “Hospitalizations and Deaths Because of Respiratory and Diarrheal Diseases among Haitian Children under Five Years of Age, 2011-2013”. Pediatric Infectious Disease Journal. 2015;34(10):e238–e243. doi: 10.1097/INF.0000000000000805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward Richard L., McNeal Monica M., Duncan Steele A. Therapeutics and Clinical Risk Management. Dove Press; 2008. “Why Does the World Need Another Rotavirus Vaccine?”. [DOI] [PMC free article] [PubMed] [Google Scholar]