Introduction
Patients with long-standing inflammatory bowel diseases (IBDs) have an increased risk of colorectal cancer and undergo frequent dysplasia surveillance with colonoscopy.1 Early guidelines recommended obtaining 4 mucosal biopsies every 10 cm throughout the colon.2 With high-definition white light colonoscopy (HDWLC), it is now believed that most dysplastic lesions are visible.3 Moreover, dye-based chromoendoscopy (DCE) and virtual chromoendoscopy (VCE) have been proposed to improve dysplasia detection.
Since 2015, several high-profile position statements have addressed approaches to colorectal cancer surveillance in IBD.3-6 Each endorsed DCE for those skilled in the method, while the American College of Gastroenterology and American Gastroenterological Association documents endorsed VCE as well. However, a recent meta-analysis questions the superiority of any of these methods.7 Additionally, there was little agreement on the role of obtaining 4 random biopsies every 10 cm throughout the colon during surveillance colonoscopy.3-6 For example, the SCENIC consensus and American College of Gastroenterology guidelines neither endorsed nor refuted the role of random biopsies with HDWLC, while the European Crohn’s and Colitis Organization guidelines and an American Gastroenterological Association expert review both endorsed use of random biopsies with HDWLC, although the latter recognized that this practice is being questioned. The lack of clarity on the role of random biopsies likely stems in part from the wide range of reported rates of detection of dysplasia in random biopsies and the value that clinicians and patients place on the risk of missed dysplasia. For example, van den Broek et al8 reported that dysplasia was detected only with random biopsies in 5 out of 1010 colonoscopies (0.2%). In contrast, Hu et al9 described that among 442 colonoscopies for IBD with dysplasia detected in the Partners HealthCare system from 2011 to 2019, 18.1% had dysplasia detected on random biopsies, and in 11.8% the only dysplasia detected was with random biopsies. Given these inconsistent position statements and primary data, we surveyed expert IBD clinicians in the United States to describe their opinions and practice patterns.
Methods
We conducted a survey of IBD expert clinicians linked to the Crohn’s & Colitis Foundation via the Clinical Research Alliance, IBD Qorus, a quality improvement network of more than 40 clinical sites, or the SPARC IBD (Study of a Prospective Adult Research Cohort with IBD) study, multicenter cohort study being conducted at 18 centers across the United States. The survey was implemented using REDCap (Research Electronic Data Capture) in July 2022. Invitations and reminders to complete the survey were sent via email.
The survey addressed the following domains: provider demographics, training, and practice setting; belief that one imaging modality is superior to another for detection of cancer, polypoid dysplasia, and flat dysplasia; belief that random biopsies increase the detection of flat dysplasia; reasons for not using different methods for dysplasia detection; and frequency of use of different methods in special populations.
The following definitions were provided to respondents to use when answering questions:
It is assumed that all colonoscopies are performed with high-definition colonoscopy equipment.
Chromoendoscopy refers to the topical application of indigo carmine or methylene blue throughout the entire colon at the time of colonoscopy. This does not refer to focal application to better visualize a previously detected or suspected lesion.
Narrow-band imaging (NBI) refers to using NBI or similar technologies as the primary modality to detect dysplasia during withdrawal of the scope, not to better visualize a previously detected or suspected lesion. References to NBI can be assumed to apply to other advanced imaging methods for computerized image enhancement or virtual chromoendoscopy, such as flexible spectral imaging color Enhancement or i-scan.
All statements refer to the use of colonoscopy to detect dysplasia and cancer in patients with >8 years of IBD, affecting at least 33% of the colon.
Questions were phrased in the following pattern: technique A is more effective than technique B to detect dysplastic polyps, flat dysplasia, or colon cancer. Questions regarding random biopsies obtained every 10 cm to detect dysplasia were phrased, “When using high-definition white light colonoscopy, obtaining 4 random biopsies per 10 cm improves the detection of dysplasia when there is endoscopic remission.” The corollary question addressed when there is not endoscopic remission and with VCE. Response options were on a 5-point Likert-type scale ranging from strongly agree to strongly disagree, with 3 being neutral.
Although the terms chromoendoscopy and NBI were used as defined previous in the survey, they are referred to as DCE and VCE, respectively, hereafter.
Statistical Analysis
Providers were defined as a “regular user” of a technique if they reported that they used the technique in 50% or more of their last 10 IBD surveillance colonoscopies. Categorical data were compared across groups using Fisher’s exact test. Continuous variables were compared across groups using 1-way analysis of variance. The study was approved by the University of Pennsylvania’s Institutional Review Board.
Results
Responses were received from 55 providers who currently perform colonoscopy as part of their practice. Responses were received from 9 of 16 SPARC principal investigators contacted, 40 of an estimated 50 to 60 active Clinical Research Alliance Members, and 30 QORUS members; many were members of multiple groups. Overall, 76% worked in an academic medical center and reported performing approximately 12 ± 9.5 IBD surveillance colonoscopies in a 2-week period (Supplemental Table 1). One (1.8%) was a regular user of both DCE and VCE, 10 (18.2%) were regular users of DCE, and 14 (25.5%) were regular users of NBI. The remaining 30 (56.4%) regularly used HDWLC without DCE or VCE. Regular use of random biopsies for dysplasia detection was reported by 32 (54.5%) providers and was strongly inversely associated with the use of DCE (P < .001) (Supplemental Table 2).
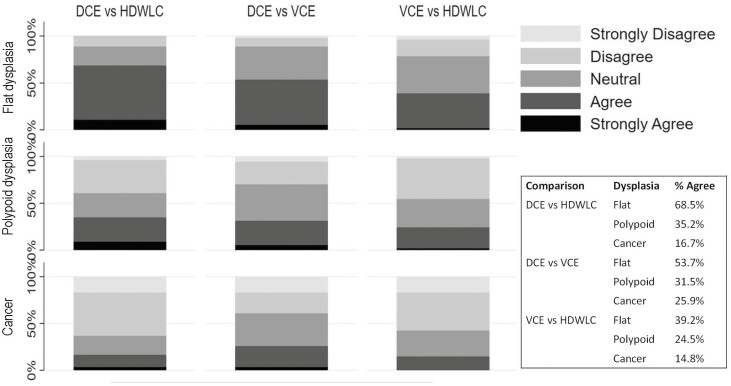
When considering the relative effectiveness of the different imaging modalities to identify dysplasia, belief that DCE was superior to HDWLC to detect flat dysplasia was reported by 68.5% of respondents (Figure 1). Only 53.7% believed that DCE was more effective than VCE to detect flat dysplasia. The 7 other comparisons all had <50% of respondents stating agree or strongly agree (Figure 1).
FIGURE 1.
Inflammatory bowel disease providers’ belief in the relative effectiveness of different imaging modalities to detect dysplasia and cancer. Statements were worded such that the first modality was superior to the second listed modality. Responses ranged from strongly agree to strongly disagree. Responses of strongly agree or agree were considered to be in agreement with the statement as reported in the table. DCE, dye-based chromoendoscopy; HDWLC, high-definition white light colonoscopy; VCE, virtual chromoendoscopy.
The most common reasons reported for not using DCE (54.6%) and VCE (40.0%) was not being convinced that the yield for dysplasia was higher with that technique (Supplemental Table 1).
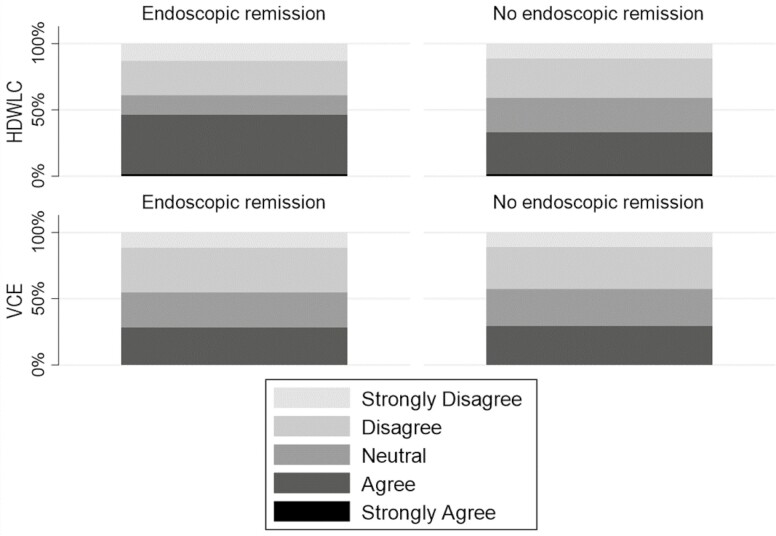
Less than 50% of providers agreed or strongly agreed that random biopsies increase the detection of dysplasia when using HDWLC, regardless of whether there was endoscopic remission (Figure 2).
FIGURE 2.
Inflammatory bowel disease providers’ beliefs about the effectiveness of random biopsies to detect dysplasia when using high-definition white light colonoscopy (HDWLC). VCE, virtual chromoendoscopy.
There were several conditions in which DCE and random biopsies were used most of the time by most of the respondents. These included patients with primary sclerosing cholangitis and patients with a history of dysplasia (Supplemental Table 4).
Discussion
Providers must make 2 main decisions when performing dysplasia surveillance, what imaging modality to use and whether to obtain random biopsies. Current guidelines and position statements on IBD dysplasia surveillance are inconsistent3-6. This survey of high-volume IBD providers demonstrated substantial heterogeneity in beliefs and self-reported practice patterns for dysplasia surveillance in IBD. In selected high-risk populations, most providers frequently use DCE and random biopsies. However, uptake of DCE for most patients with IBD has been limited, even among high-volume IBD clinicians. Rather, HDWLC with random biopsies remains the most used modality. Despite this, <50% of respondents agreed that random biopsies used in conjunction with HDWLC effectively increased flat dysplasia detection, and nearly as many disagreed with this concept.
Despite multiple guidelines and position statements that endorse DCE and to some extent VCE over HDWLC,3-6 a recent meta-analysis observed similar effectiveness of DCE, VCE, and HDWLC to detect dysplasia.7 There are far fewer head to head comparisons of random biopsies. A small clinical trial demonstrated numerically, although not statistically, higher rates of dysplasia detection when only targeted biopsies were obtained as compared with obtaining random and targeted biopsies.10 Thus, uncertainty regarding the best method for dysplasia surveillance and practice variability is anticipated.
In selected patients such as those with prior dysplasia or primary sclerosing cholangitis, most providers reported using both DCE and random biopsies. This suggests some belief in the incremental effectiveness of both DCE and random biopsies, at least in the highest-risk patients.
The respondents to our survey were experienced, high-volume providers, performing a mean of 12 dysplasia surveillance colonoscopies in the prior 2 weeks. Thus, these were experienced providers who likely have knowledge of the existing data and recommendations related to dysplasia surveillance. It is unknown if providers who have fewer patients with IBD would have similar beliefs and practices.
In summary, multiple clinical trials have demonstrated minimal difference in effectiveness of available imaging modalities. Perhaps as a result, HDWLC and random biopsies were the most used modalities for dysplasia surveillance in this cohort of physicians caring for patients with IBD. However, substantial uncertainty exists regarding the effectiveness of random biopsies. Additional clinical trials of random biopsies when using HDWLC are needed to inform evidence-based guidelines.
Supplementary Material
Contributor Information
James D Lewis, Division of Gastroenterology and Hepatology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA; Department of Biostatistics, Epidemiology and Informatics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA; Center for Clinical Epidemiology and Biostatistics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
Raymond K Cross, Department of Medicine, Division of Gastroenterology and Hepatology, University of Maryland, Baltimore, MD, USA.
Millie Long, Department of Medicine, Division of Gastroenterology and Hepatology, University of North Carolina, Chapel Hill, NC, USA.
Siddharth Singh, Department of Medicine, Division of Gastroenterology, University of California San Diego, San Diego, CA, USA.
Hans Herfarth, Department of Medicine, Division of Gastroenterology and Hepatology, University of North Carolina, Chapel Hill, NC, USA.
Alexandra Weiss, Division of Gastroenterology and Hepatology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
Anna Buchner, Division of Gastroenterology and Hepatology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
Author Contributions
J.D.L., R.K.C., M.L., S.S., H.H., A.W., A.B.: conceptualization and design, data interpretation, critical editing of the manuscript. J.D.L.: data collection, data analysis, drafting of the manuscript.
Funding
This work was supported in part by National Institutes of Health grants K23-DK117058, R03-DK129631, and P30-DK050306.
Conflicts of Interest
No authors report potential conflict of interest related to this work.
References
- 1. Clarke WT, Feuerstein JD.. Colorectal cancer surveillance in inflammatory bowel disease: practice guidelines and recent developments. World J Gastroenterol. 2019;25:4148-4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alexandersson B, Hamad Y, Andreasson A, et al. High-definition chromoendoscopy superior to high-definition white-light endoscopy in surveillance of inflammatory bowel diseases in a randomized trial. Clin Gastroenterol Hepatol. 2020;18:2101-2107. [DOI] [PubMed] [Google Scholar]
- 3. Rubin DT, Ananthakrishnan AN, Siegel CA, et al. ACG clinical guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019;114:384-413. [DOI] [PubMed] [Google Scholar]
- 4. Magro F, Gionchetti P, Eliakim R, et al.; European Crohn’s and Colitis Organisation [ECCO]. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. 2017;11:649-670. [DOI] [PubMed] [Google Scholar]
- 5. Laine L, Kaltenbach T, Barkun A, et al.; SCENIC Guideline Development Panel. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015;148:639-651.e28. [DOI] [PubMed] [Google Scholar]
- 6. Murthy SK, Feuerstein JD, Nguyen GC, Velayos FS.. AGA clinical practice update on endoscopic surveillance and management of colorectal dysplasia in inflammatory bowel diseases: expert review. Gastroenterology. 2021;161:1043-1051.e4. [DOI] [PubMed] [Google Scholar]
- 7. El-Dallal M, Chen Y, Lin Q, et al. Meta-analysis of virtual-based chromoendoscopy compared with dye-spraying chromoendoscopy standard and high-definition white light endoscopy in patients with inflammatory bowel disease at increased risk of colon cancer. Inflamm Bowel Dis. 2020;26:1319-1329. [DOI] [PubMed] [Google Scholar]
- 8. van den Broek FJ, Stokkers PC, Reitsma JB, et al. Random biopsies taken during colonoscopic surveillance of patients with longstanding ulcerative colitis: low yield and absence of clinical consequences. Am J Gastroenterol. 2014;109:715-722. [DOI] [PubMed] [Google Scholar]
- 9. Hu AB, Burke KE, Kochar B, Ananthakrishnan AN.. Yield of random biopsies during colonoscopies in inflammatory bowel disease patients undergoing dysplasia surveillance. Inflamm Bowel Dis. 2021;27:779-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Watanabe T, Ajioka Y, Mitsuyama K, et al. Comparison of targeted vs random biopsies for surveillance of ulcerative colitis-associated colorectal cancer. Gastroenterology. 2016;151:1122-1130. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.