Abstract
Study Objectives:
The high prevalence of obstructive sleep apnea (OSA) in the general population makes diagnosing OSA a high priority. Typically, patients receive in-person instructions to hook up the home sleep apnea test devices. Using recorded video instructions would save health care personnel time and improve access to OSA diagnostics for patients in remote areas. The aim of this study was to compare the quality of home sleep apnea test recordings when using in-person and video hookup instructions in a randomized study.
Methods:
A total of 100 patients aged 18 to 70 years with suspected OSA were randomized to receive either in-person or video hookup instructions for the Nox T3 device (Nox Medical, Reykjavik, Iceland). The overall quality of the resulting sleep studies was analyzed by determining the number of technically invalid studies. The recording quality of 4 sensors (pulse oximeter, nasal cannula, thorax and abdominal respiratory inductance plethysmography belts) was assessed by checking for signal artifacts.
Results:
No significant difference was found between the 2 groups in any quality index. Only 1 (2%) and 2 (3.9%) sleep studies were technically invalid in the in-person and video instructions group, respectively. The average ± standard deviation recording quality of the 4 sensors combined was 94.8% ± 13.6% for the in-person and 96.0% ± 11.0% for the video instructions group.
Conclusions:
This study found no difference in home sleep apnea test recording quality between the 2 groups. Video hookup instructions are therefore viable and an important step toward a telemedicine-based way of diagnosing OSA.
Citation:
Horne AF, Olafsdottir KA, Arnardottir ES. In-person vs video hookup instructions: a comparison of home sleep apnea testing quality. J Clin Sleep Med. 2022;18(8):2069–2074.
Keywords: obstructive sleep apnea, telemedicine, home sleep apnea test, video instructions
BRIEF SUMMARY
Current Knowledge/Study Rationale: The high prevalence of obstructive sleep apnea in the general population makes diagnosing obstructive sleep apnea a high priority, but home sleep apnea tests currently require patients to receive in-person instructions on hooking up home sleep apnea test devices. Using recorded video instructions would save health care personnel time and improve access to obstructive sleep apnea diagnostics for patients in remote areas.
Study Impact: This randomized double-blind study found no discernible difference in the quality of home sleep apnea test recordings when using in-person and video hookup instructions. Video hookup instructions are therefore a viable alternative and an important step toward a telemedicine approach to obstructive sleep apnea diagnosis.
INTRODUCTION
Obstructive sleep apnea (OSA) causes excessive daytime sleepiness and cardiometabolic problems.1 OSA may be prevalent in up to 1 billion people worldwide,2 making diagnosis and treatment a high priority. Traditionally, OSA is diagnosed by polysomnography in a sleep laboratory (type 1 sleep study3). However, there are several downsides to this. First, patients are less comfortable when sleeping in an unfamiliar environment,4 leading to reduced sleep efficiency.5 Second, capacities in the sleep laboratories are scarce, causing long patient waiting times.4 Third, it is difficult for people in rural or remote areas to reach a sleep laboratory.4
As an alternative method for diagnosing OSA, home sleep apnea tests (HSATs) (types 2–4 sleep studies3) are now officially accepted by the American Academy of Sleep Medicine.6 This resolves the first 2 downsides described above. However, the third downside still remains, requiring patients to receive in-person instructions on how to hook up the HSAT devices or have the devices set up by expert staff.7 To solve this, a fully telemedicine-based way of conducting HSATs is necessary.8 However, while previous studies about telemedicine in OSA have worked on improving different telemonitoring aspects of both type 29–11 and type 312 sleep studies, there has not been a focus on making the hookup procedure more telemedicine compatible.
To the authors’ knowledge, only 1 previous study compared in-person hookup instructions to a recorded video.13 In this study, the diagnosis and treatment of OSA was compared between 2 groups of veterans, 1 treated in a telemedicine-style and another in a traditional, in-person-style. For hooking up the HSAT devices, the telemedicine group received only an instructional DVD and brochure, whereas the in-person group received instructions from a trained professional at a clinic. In the telemedicine group, only 65% of the sleep tests were scoreable, compared to 83% in the in-person group.
Further research dedicated to the quality of video instructions in HSATs is needed. Therefore, the aim of this study was to perform a randomized double-blind study and compare the quality of type 3 sleep study recordings when using in-person and video hookup instructions. A priori, the authors expected no discernible difference in quality.
METHODS
Participants
The study participants were patients between 18 and 70 years, referred to Landspitali University Hospital in Iceland for HSAT because of suspected OSA. Participants were invited to participate in the study by continuously offering all incoming patients to participate until reaching n = 100. A total of 27 refused participation. The study was conducted with the consent of the Landspitali Bioethics Committee (22/2014). Written consent was obtained from all participants.
Procedure
All participants attended an interview at the hospital, during which they were randomly assigned to either the in-person or video instructions group by lottery. The in-person instructions group was shown how to hook up the HSAT device by a sleep technologist (not fully hooked up for the demonstration), while the video instructions group was given a hyperlink to an online instructional video to watch at home. Participants from both groups were sent home with a Nox T3 device (Nox Medical, Reykjavik, Iceland, for type 3 sleep studies), unattached, which they hooked up that night by themselves. All participants were given the option to call a sleep technologist for help, if necessary. The HSAT device contained the following sensors: a pulse oximeter, a nasal cannula, thorax and abdomen respiratory inductance plethysmography (RIP) belts, a microphone, and an accelerometer.
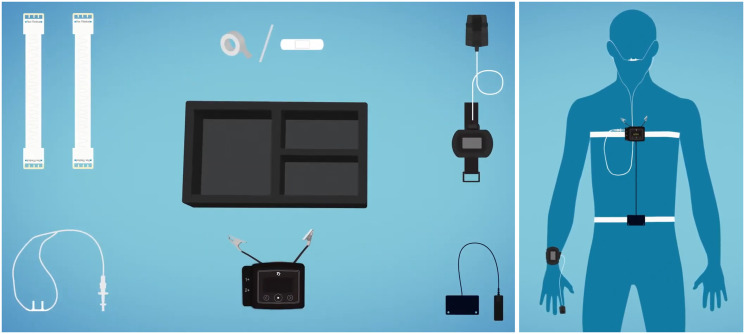
The instructional video14 (Figure 1), which had been translated from English to Icelandic, was almost 6 minutes long and used animations and voiceover to explain the contents of the HSAT kit, how to attach the device and different sensors, and how to start and stop the recording.
Figure 1. Instructional video for hooking up the Nox T3 device to perform an HSAT.14.
HSAT = home sleep apnea test.
Data analyses
The data recorded by the HSAT device was manually assessed by an expert sleep technologist, blinded to the study group of participants, according to the following criteria:
First, the total recording time of the sleep study was determined by detecting when the participant fell asleep for the first time and when he woke up for the last time (analysis start and stop time); only this period was relevant for all additional assessments. This was based on the self-report of the participant in a questionnaire and the manual review of the recording by the sleep technologist. Next, periods were detected in which the participant was considered awake within the total recording time, based on the participant’s body position, movements, and respiratory pattern. These periods were labeled as “invalid data,” so they would not count toward the index time for respiratory event index. Finally, artifacts were detected in the signals of 4 sensors (pulse oximeter, nasal cannula, thorax and abdomen RIP belts) according to the criteria listed in Table 1.
Table 1.
Criteria for determining artifacts for each HSAT sensor.
| Sensor | Artifacts |
|---|---|
| Pulse oximeter | No signal, signal with obviously invalid value or value of “127” (minimum 10 s) |
| Nasal cannula | Bad or flat signal (minimum 3 min) |
| Thorax RIP belt | Bad or flat signal (minimum 3 min) |
| Abdomen RIP belt | Bad or flat signal (minimum 3 min) |
HSAT = home sleep apnea test, RIP = respiratory inductance plethysmography.
Based on these preliminary steps, a study was considered technically invalid if it had fewer than 4 hours of monitoring time.15 The monitoring time was calculated by taking the total recording time and subtracting the time when the patient was awake or either the pulse oximeter or at least 2 of the 3 respiratory sensors (nasal cannula and thorax and abdomen RIP belts) had an artifact. An exception was made for 2 studies with monitoring time of 3.98 and 3.95 hours, respectively, considered extreme borderline cases that would normally not be rejected for OSA diagnosis.
For all technically valid sleep studies, the respiratory event index (apneas + hypopneas/total recording time) and oxygen desaturation index were scored manually in accordance with the latest American Academy of Sleep Medicine manual.16 Hypopneas were scored with 4% desaturations. The quality of the signals recorded by the 4 sensors (pulse oximeter, nasal cannula, thorax and abdomen RIP belts) was assessed by first subtracting the “invalid data” periods from the total recording time and then calculating the percentage of that time that was without artifacts for each sensor.
To statistically compare the values for the in-person and the video instruction group, a Mann-Whitney U test was performed for all continuous variables, since their values were not normally distributed, and a χ2 test for the nominal variables.
RESULTS
In total, 127 patients were invited to join the study, 27 of those refused. The patients who did on respond were of similar age (P = .48), body mass index (P = .11), and sex distribution (P = .75) as the study participants. When asked to give a reason for their refusal, 4 patients said they did not feel confident enough to follow a video instruction, 4 did not speak sufficient Icelandic, 2 refused due to disability, 2 did not have enough time to study the video, and 1 person did not have internet access at their home and was therefore unable to access the video. A total of 14 patients did not give a reason for their refusal.
The 100 study participants were randomly distributed by lottery, 49 to the in-person instructions group and 51 to the video instructions group. As Table 2 shows, participants in both groups were on average middle-aged and overweight to obese. The majority of participants in both groups were men. No significant difference was found between the 2 groups in demographic variables or OSA severity.
Table 2.
Comparison of participant characteristics between the in-person and video hookup instructions group.
| In-Person Instructions (n = 49) | Video Instructions (n = 51) | P | |
|---|---|---|---|
| Demographics | |||
| Age, y | 50.5 ± 10.3 | 48.4 ± 11.5 | .43 |
| Males, n (%) | 38 (77.6) | 33 (64.7) | .16 |
| BMI, kg/m2 | 29.6 ± 5.9 | 30.8 ± 6.3a | .36 |
| Sleep study | |||
| REI, events/h | 11.0 ± 12.1b | 16.9 ± 22.3c | .24 |
| ODI, events/h | 9.3 ± 11.2b | 14.3 ± 18.3c | .15 |
Values are mean ± standard deviation or n (%). an = 50. bn = 48. cn = 49. P values were calculated using Mann–Whitney U test, except for sex, where χ2 was used. BMI = body mass index, ODI = oxygen desaturation index, REI = respiratory event index.
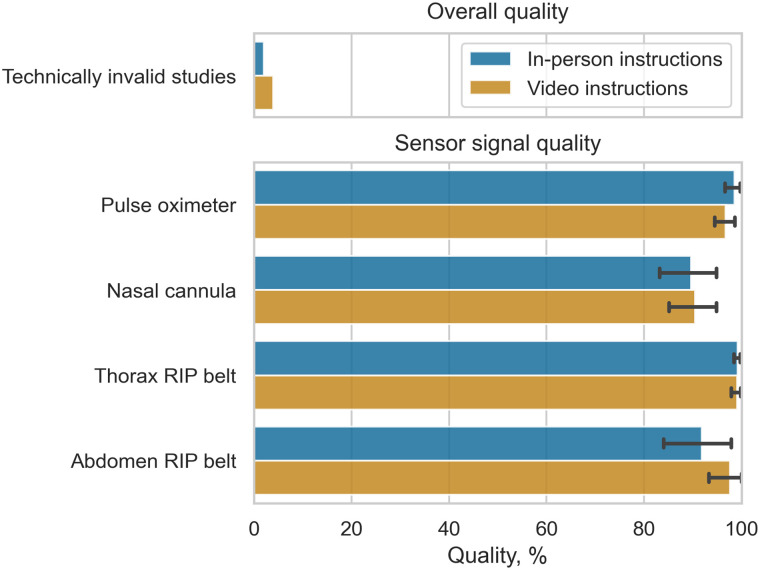
Table 3 illustrates that nearly all conducted sleep studies were valid. For the in-person instructions group, only 1 study was technically invalid. This participant had not put on the HSAT device at all. For the video instructions group, 2 studies were technically invalid: In one case, the pulse oximeter had failed to record any data. In the other case, the total recording time was above 4 hours (4.7 hours), but the monitoring time was only 2.5 hours, due to too many artifacts in the recordings. The amount of technically invalid studies was not significantly different between the 2 groups. The same was found for the total recording time and monitoring time.
Table 3.
Comparison of overall sleep study quality and sensor signal quality between the in-person and video hookup instructions group.
| In-Person Instructions (n = 49) | Video Instructions (n = 51) | P | ||
|---|---|---|---|---|
| Overall quality | ||||
| Technically invalid, n (%) | 1 (2.0) | 2 (3.9) | .58 | |
| TRT, h | 7.0 ± 1.1a | 7.0 ± 0.8b | .88 | |
| MT, h | 6.7 ± 1.2a | 6.7 ± 0.9b | .80 | |
| Sensor signal quality | ||||
| Pulse oximeter, % | Mean | 98.5 ± 6.0a | 96.8 ± 7.7b | .36 |
| Median | 99.9 (60.6, 100.0)a | 99.8 (60.9, 100.0)b | ||
| Nasal cannula, % | Mean | 89.6 ± 21.3a | 90.5 ± 18.0b | .70 |
| Median | 100.0 (25.5, 100.0)a | 100.0 (17.3, 100.0)b | ||
| Thorax RIP belt, % | Mean | 99.2 ± 2.4a | 99.1 ± 4.0b | .63 |
| Median | 100.0 (86.1, 100.0)a | 100.0 (72.0, 100.0)b | ||
| Abdomen RIP belt, % | Mean | 91.9 ± 24.8a | 97.5 ± 14.4b | .29 |
| Median | 100.0 (0.0, 100.0)a | 100.0 (0.0, 100.0)b | ||
Values are mean ± SD and median (minimum, maximum), or n (%). an = 48. bn = 49. P values were calculated using Mann–Whitney U test, except for number of technically invalid studies, where χ2 was used. MT = monitoring time, RIP = respiratory inductance plethysmography, SD = standard deviation, TRT = total recording time.
For the technically valid studies, the recordings of all 4 sensors (pulse oximeter, nasal cannula, thorax and abdomen RIP belts) were on average of high quality for both groups, with over 90% of the recording durations being artifact-free (mean quality > 90%, Table 3, Figure 2). Additionally, over half of the recordings in both groups were completely artifact-free for the RIP belts and nasal cannula (median quality = 100%, Table 3) and very nearly so for the pulse oximeter (median quality > 99%, Table 3). No significant differences were found between the groups in any quality assessment (Table 3).
Figure 2. Comparison of percentage of technically invalid studies and mean qualities for the different sensor recordings between the in-person and video hookup instructions group.
Bars without lines represent n (%). Bars with lines represent mean ± standard error (95% confidence interval). RIP = respiratory inductance plethysmography.
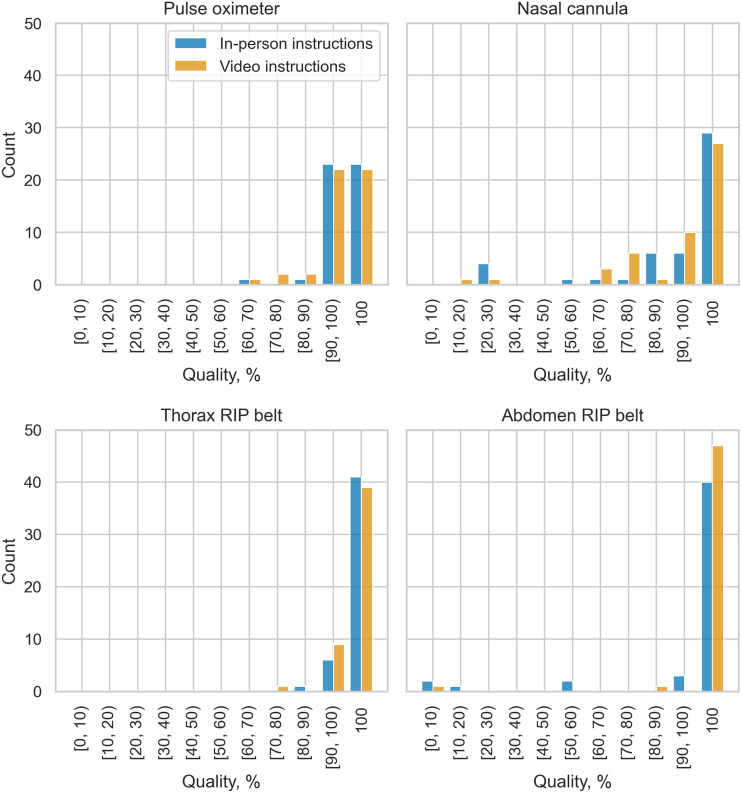
The distribution of sensor qualities and outliers was also similar between both groups (Figure 3). This was also found for the nasal cannula, whose recording quality was on average noticeably worse than for the other 3 sensors.
Figure 3. Comparison of quality distributions and outliers for the different sensor recordings between the in-person and video hookup instructions group.
RIP = respiratory inductance plethysmography.
No participants from either group took up the offer to call a sleep technologist for help.
DISCUSSION
This study found no discernible difference in the quality of HSAT recordings when using in-person and video hookup instructions. Neither the amount of technically invalid sleep studies varied significantly between the 2 groups nor the recording quality of any of the 4 sensors (pulse oximeter, nasal cannula, thorax and abdomen RIP belts).
Regarding sensor quality, these results support the findings of Fields et al,13 who had conducted the only previous study on this topic to date. While they did not actually test for significant differences in sensor quality between the groups, they reported that on average, at least 86% of the recording durations were artifact-free in both groups.13
However, in contrast to our study, Fields et al13 found that nearly 20% more of the sleep studies were technically invalid in their video instructions group than in their in-person instructions group. A possible explanation for this is that the video used in our study may be of higher quality, since the authors reported that some of their study participants found their instructional video confusing.13
The Fields et al13 study had a broad scope, exploring the feasibility of a telemedicine-based approach to OSA diagnosis and management by observing patients for several months. During this time span, their primary aim was to compare the functional outcome of automatic positive airway pressure treatment and the level of adherence between the 2 groups; comparing the quality of HSAT recording quality was only an additional, minor aspect.13 Our study, on the other hand, focused exclusively on this last aspect and performed a thorough statistical analysis comparing the results for both study groups (not performed in13). Furthermore, the study by Fields et al13 consisted of 60 participants, who were exclusively veterans, with less than 10% females. Our study included a larger sample size of 100 participants and was more demographically diverse. All in all, our study confirmed, strengthened, and generalized the results of Fields et al13 regarding HSAT recording quality for a wider part of the population and for a different HSAT device.
Additionally, those who did not respond were questioned about their reason for refusing to participate, which revealed a number of relevant insights: First, it is important to make instructional videos available in several languages. Second, patients’ self-confidence about learning how to hook up the HSAT device by watching a video needs to be boosted. Third, technological limitations need to be taken into account, eg, by providing alternative solutions to deliver instructional videos for patients without an internet connection at home.
A limitation of this study is that the demographics of the study participants, while more general than in Fields et al,13 still consisted, on average, of patients who were middle-aged and overweight to obese patients; two-thirds of them were men. While this is not representative of the general population, it is, however, representative of the average patient with OSA.17 Furthermore, while a sample size of 100 participants is not large, the participants covered a wide age range from 18 to 70 years and were both male and female, so that the study results should be seen as sufficiently representative. Nonetheless, this study is limited to 1 specific set of circumstances, which limits how much its findings can be generalized. Also, the study may not be powered to detect minor differences.
Future studies should therefore be conducted, eg, with different HSAT devices, in large populations of patients with suspected OSA in other centers to validate and generalize our findings. Finally, unlike Fields et al,13 the participants of our study were not interviewed after completing the HSAT about their experience with and opinion of the video hookup instructions. This should be added in future studies on this subject to gain more information about potential improvements to the instructional videos.
One of the strengths of this study is that an analysis of those who did not respond was conducted, since this provides valuable information about concerns patients have regarding video hookup instructions, which need to be addressed in the future. Further strengths include this study’s sole focus on evaluating HSAT recording quality between video and in-person hookup instructions, the thorough statistical analysis that was performed, and the fact that it is only the second study conducted on this topic.
In conclusion, providing hookup instructions for HSATs via recorded video is a viable alternative to providing them in-person. Video hookup instructions are an important step toward a telemedicine approach to OSA diagnosis, allowing patients in rural or remote areas to receive treatment easily and saving valuable health care personnel time.
ACKNOWLEDGMENTS
The authors thank sleep technologists Auður G. Sigurðardóttir, Marta Serwatko, Sigríður Sigurðardóttir, and Magdalena Ósk Sigurgunnarsdóttir, who assisted with the patient recruitment in this study, and Haraldur S. Þorsteinsson for his assistance with the data management. We also thank Aron Valgeir Gunnlaugsson, Birkir Björnsson, and Emil Þór Emilsson for their help in refining the text of this article.
ABBREVIATIONS
- HSAT
home sleep apnea test
- OSA
obstructive sleep apnea
- RIP
respiratory inductance plethysmography
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. Work for this study was performed at Landspitali University Hospital (data collection) and Reykjavik University (data analysis and writing). This study was funded by a grant from the Ministry of Health in Iceland. ESA discloses lecture fees from Nox Medical, Philips and ResMed. The other authors report no conflicts of interest.
EDITOR’S NOTE
The Emerging Technologies section focuses on new tools and techniques of potential utility in the diagnosis and management of any and all sleep disorders. The technologies may not yet be marketed, and indeed may only exist in prototype form. Some preliminary evidence of efficacy must be available, which can consist of small pilot studies or even data from animal studies, but definitive evidence of efficacy will not be required, and the submissions will be reviewed according to this standard. The intent is to alert readers of Journal of Clinical Sleep Medicine of promising technology that is in early stages of development. With this information, the reader may wish to (1) contact the author(s) in order to offer assistance in more definitive studies of the technology; (2) use the ideas underlying the technology to develop novel approaches of their own (with due respect for any patent issues); and (3) focus on subsequent publications involving the technology in order to determine when and if it is suitable for application to their own clinical practice. The Journal of Clinical Sleep Medicine and the American Academy of Sleep Medicine expressly do not endorse or represent that any of the technology described in the Emerging Technologies section has proven efficacy or effectiveness in the treatment of human disease, nor that any required regulatory approval has been obtained.
REFERENCES
- 1. Hughes BH, Polnitsky CA, Lee-Chiong T . Sleep-Related Breathing Disorders: Clinical Features and Evaluation . In: Avidan AY , ed. Review of Sleep Medicine E-Book. 4th ed. Philadelphia, PA: : Elsevier Health Sciences; ; 2017. : 150 – 163. [Google Scholar]
- 2. Benjafield AV, Ayas NT, Eastwood PR, et al . Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis . Lancet Respir Med. 2019. ; 7 ( 8 ): 687 – 698 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Arnardottir ES, Islind AS, Óskarsdóttir M . The future of sleep measurements: a review and perspective . Sleep Med Clin. 2021. ; 16 ( 3 ): 447 – 464 . [DOI] [PubMed] [Google Scholar]
- 4. Masa JF, Corral J, Pereira R, et al . Effectiveness of home respiratory polygraphy for the diagnosis of sleep apnoea and hypopnoea syndrome . Thorax. 2011. ; 66 ( 7 ): 567 – 573 . [DOI] [PubMed] [Google Scholar]
- 5. Bruyneel M, Sanida C, Art G, et al . Sleep efficiency during sleep studies: results of a prospective study comparing home-based and in-hospital polysomnography . J Sleep Res. 2011. ; 20 ( 1 Pt 2 ): 201 – 206 . [DOI] [PubMed] [Google Scholar]
- 6. Rosen IM, Kirsch DB, Carden KA, et al. ; American Academy of Sleep Medicine Board of Directors . Clinical use of a home sleep apnea test: an updated American Academy of Sleep Medicine position statement . J Clin Sleep Med. 2018. ; 14 ( 12 ): 2075 – 2077 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hoffman AG, Barnes D . Portable sleep apnea testing: an update . Can J Respir Ther. 2012. ; 48 ( 2 ): 7 – 14. [Google Scholar]
- 8. Bruyneel M . Telemedicine in the diagnosis and treatment of sleep apnoea . Eur Respir Rev. 2019. ; 28 ( 151 ): 180093 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kayyali HA, Weimer S, Frederick C, et al . Remotely attended home monitoring of sleep disorders . Telemed J E Health. 2008. ; 14 ( 4 ): 371 – 374 . [DOI] [PubMed] [Google Scholar]
- 10. Bruyneel M, Van den Broecke S, Libert W, Ninane V . Real-time attended home-polysomnography with telematic data transmission . Int J Med Inform. 2013. ; 82 ( 8 ): 696 – 701 . [DOI] [PubMed] [Google Scholar]
- 11. Coma-Del-Corral MJ, Alonso-Álvarez ML, Allende M, et al . Reliability of telemedicine in the diagnosis and treatment of sleep apnea syndrome . Telemed J E Health. 2013. ; 19 ( 1 ): 7 – 12 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Borsini E, Blanco M, Bosio M, Fernando DT, Ernst G, Salvado A . “Diagnosis of sleep apnea in network” respiratory polygraphy as a decentralization strategy . Sleep Sci. 2016. ; 9 ( 3 ): 244 – 248 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fields BG, Behari PP, McCloskey S, et al . Remote ambulatory management of veterans with obstructive sleep apnea . Sleep. 2016. ; 39 ( 3 ): 501 – 509 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nox Medical . Standard Nox T3 leidbeiningarmyndband handvirkt. https://noxmedical.com/about/news-press/article/video/standard-nox-t3-leidbeiningarmyndband-handvirkt/ . Published June 12, 2018. . Accessed February 27, 2021.
- 15. Arnardottir ES, Verbraecken J, Gonçalves M, et al .; The National Representatives as Study Collaborators . Variability in recording and scoring of respiratory events during sleep in Europe: a need for uniform standards . J Sleep Res. 2016. ; 25 ( 2 ): 144 – 157 . [DOI] [PubMed] [Google Scholar]
- 16. Berry RB, Quan SF, Abreu AR, et al. ; for the American Academy of Sleep Medicine . The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Version 2.6 . Darien, IL: : American Academy of Sleep Medicine; ; 2020. . [Google Scholar]
- 17. Franklin KA, Lindberg E . Obstructive sleep apnea is a common disorder in the population—a review on the epidemiology of sleep apnea . J Thorac Dis. 2015. ; 7 ( 8 ): 1311 – 1322 . [DOI] [PMC free article] [PubMed] [Google Scholar]