Abstract
Study Objectives:
Social jetlag (SJL) measures the discrepancy between circadian and social clocks. Using accelerometry-derived data, our objective was to assess the prevalence of SJL in young healthy children and determine the association of SJL and sleep with temperament.
Methods:
Of 117 children participating in TARGet Kids!, a Canadian cohort of healthy preschool-aged children, 78 children (39 girls; 50%; mean age [SD]: 35.1 [20.5] months) were included. Sleep was measured objectively using accelerometry. Temperament dimensions (surgency, negative affectivity, and effortful control) were assessed with the very short forms of Rothbart’s child and infant behavior questionnaires. We examined associations of SJL and sleep with temperament using multivariable linear regression models adjusted for sex, age, ethnicity, and preschool/daycare attendance.
Results:
20 out of 78 (25.6%) experienced SJL of greater than 30 minutes. SJL was greater in children who attended preschool/daycare compared with children who did not (26.3[18.8] minutes vs 17.6 [14.8] minutes; P < .05). There was no evidence of an association between SJL and any temperament dimension. We found evidence of an association between increased sleep duration and increased negative affectivity scores (longer 24-hour sleep; β: 0.347; 95% confidence interval: 0.182, 0.512; P < .0001; and longer nighttime sleep duration: β: 0.413; 95% confidence interval: 0.163, 0.663; P = .002).
Conclusions:
In our cohort, 1 in 4 preschool-aged children experienced SJL. Increased sleep duration was associated with increased negative affect, which could have implications for children developing internalizing behavior such as depression or low self-esteem. We found that sleep duration, but not SJL, was associated with temperament and may impact daytime behavior of young children.
Citation:
Giannoumis M, Mok E, Borkhoff CM, et al. Association of accelerometry-derived social jetlag and sleep with temperament in children less than 6 years of age. J Clin Sleep Med. 2022;18(8):1993–1999.
Keywords: social jetlag, sleep, temperament
BRIEF SUMMARY
Current Knowledge/Study Rationale: Social jetlag (SJL) measures the discrepancy between circadian and social clocks. Sleep affects many aspects of a child’s life and may have an impact on temperament. Few studies have evaluated the effects of SJL and sleep on temperament in early life and no studies have examined SJL using objective accelerometer data in preschool children.
Study Impact: SJL is prevalent in 1 in 4 preschool-aged children and sleep duration, but not SJL, is associated with child temperament, highlighting sleep characteristics associated with daytime behavior. Our findings provide evidence of an association between sleep duration and behavioral problems in infants and preschool-aged children.
INTRODUCTION
Sleep is an important constituent of health in children and is associated with a child’s physical, mental, and neurobehavioral development.1–3 During the first year of life, sleep-wake regulation and sleep states evolve rapidly and continue to adapt with maturation throughout childhood.4,5 Sleep patterns in children are affected by the interplay between genetics, environmental, and social factors, such as parenting practices, expectations, family routines, and daycare and school schedules.4 Social jetlag (SJL) is defined as the absolute difference between sleep midpoints on school days and free days (often weekend days).6–8 It is rooted from conflicting biologically driven preferences and social obligations that result in circadian misalignment.7 For preschool children under 6 years old, free days would be days when their sleep-wake patterns are free from any influence of individual or family activities. Already at preschool age, delayed weekend sleep pattern, later sleep midpoint on free days, and SJL have been demonstrated using parent-reported sleep measures (eg, validated questionnaires).9–14 Therefore, the displacement of sleep-wake times for later hours on free days starts at an early age,9 suggesting that parental influence exists and has an impact on infant and child sleep-wake pattern (eg, delayed bedtime on weekends).13,15
The importance of SJL has been demonstrated in other populations. In school-aged children and adolescents, SJL is associated with sleep disorders and higher adiposity.16–18 In adults, SJL is associated with metabolic disorders and obesity.19,20 The relationship between SJL and emotional and behavioral problems is also well documented in children and adolescents.21,22 Moreover, preschool children of evening chronotype are vulnerable to higher SJL and more behavioral problems, including hyperactivity/inattention, conduct problems, peer problems, and sleep problems.10,23 Studies assessing SJL in young adolescents or adults used objective actigraphy monitoring for 5–7 days17,24–26 or validated questionnaires.19,27 In preschool children, studies assessing SJL relied exclusively on the parent’s report.9–12,14 To our knowledge, no studies assessed SJL using objective sleep measures (eg, actigraphy) in preschool-aged children.
Child temperament is defined as constitutionally based individual differences in self-regulation and reactivity that are apparent from infancy. Rothbart and colleagues28,29 define temperament using 3 dimensions: surgency, negative affectivity, and effortful control/orienting capacity to describe temperament in children. Surgency reflects motor and vocal activity, positive emotional reactions to high-intensity stimuli, and seeking closeness with others, and is associated with the development of externalizing problems.29 Negative affectivity reflects the tendency to experience negative emotions and distress; high negative affectivity is associated with developing internalizing problems. Effortful control, referred to as orienting capacity in infants, reflects self-control of behavior and positive reaction to low-intensity stimuli; high effortful control is associated with a positive development and lower behavioral problems.29–32 Few studies have evaluated the effects of SJL and sleep on temperament in early life and no studies have examined SJL with temperament in preschool children using objective accelerometer data.4,22,33
Vriend et al34 studied the impact of an imposed sleep schedule in a randomized trial where school-aged children slept for either 1 extra hour (long-sleep schedule) or with a 1-hour deficit (short-sleep schedule) and showed that participants demonstrated less positive affective response and poorer parent-reported emotion regulation directly after the short-sleep schedule compared with the long-sleep condition.
For the current study, we examined the relationship between accelerometry-derived sleep measures and temperament in infants and preschool-aged children. Our primary objective was to describe SJL in a cohort of healthy infants and young children under 6 years old and to determine the association between SJL and child temperament. Our primary hypothesis was that SJL is associated with temperament (ie, low surgency, high negative affectivity, and low effortful control). Our secondary objective was to examine the association between sleep duration (total 24-hour sleep duration, nighttime sleep duration) and temperament.
METHODS
Study design
This was a cross-sectional study with The Applied Research Group for Kids (TARGet Kids!), which is an ongoing, open, longitudinal cohort and is the largest cohort of children under 6 years of age in Canada recruited from primary health care settings.35 Healthy children under 6 years of age who attended well-child visits with a primary care physician in Toronto (a large urban city in Canada) between January 2013 and April 2014 and had ≥ 1 weekday and ≥ 1 weekend day of accelerometry were included in this study. The TARGet Kids! cohort excluded children with conditions affecting growth, severe developmental delay, chronic conditions (except for asthma), and children whose families were not able to complete questionnaires in English. For the present study, we also excluded children who had accelerometry data collected on days with time change affected by daylight savings (day of, or the days of the week that followed, since sleep timing may be affected by the time change). Children whose parents did not complete Rothbart’s child or infant behavior questionnaires30–32 were also excluded. This study was approved by the Research Ethics Board of the McGill University Health Centre, as well as the Research Ethics Board of the Hospital for Sick Children and St. Michael’s Hospital.
Baseline demographics
Parents completed standardized questionnaires on baseline characteristics and lifestyle (sex, age, ethnicity, daycare attendance, breastfeeding) sociodemographic information (maternal education, self-reported family income), health, and health-related behaviors. Child ethnicity was a composite variable derived from maternal and paternal self-reported ethnicity. The questionnaire completed by the parents had 2 separate questions to identify the ethnicity of each parent. Maternal and paternal ethnicity were classified into 1 of the following 9 categories: (1) “European,” (2) “East Asian,” (3) “South Asian,” (4) “Southeast Asian,” (5) “Arab,” (6) “African,” (7) “Latin American,” (8) “mixed ethnicity,” or (9) “other.” For the current study, child ethnicity was classified as European if both parents identified as European (category 1), or non-European if 1 or both parents identified as non-European ethnicity (categories 2 through 9, collapsed). Age groups were adapted from age group recommendations for sleep from the American Academy of Sleep Medicine (under 12 months of age, 12 months to under 36 months of age, 36 months to under 72 months of age).36
Exposure variables
The Actical accelerometer (Philips–Respironics, Oregon, USA), an omnidirectional accelerometer, was used to collect accelerometry data. The Actical senses high-energy and sedentary movements in 2-second epochs, which were combined into count values per minute. Parents were instructed to attach the Actical over their child’s right hip during 24 hours for 7 consecutive days. Actigraphy for 7 days has been shown to provide reliable measures of sleep in children.37,38 Parents kept a 7-day sleep log, recording sleep, wake, and nap times as well as any periods of time when the accelerometer was removed. We calculated SJL as a continuous variable (minutes) as the absolute difference between sleep midpoint on weekend days (or free days) and weekdays based on accelerometry data.6 Sleep midpoint was determined as the midpoint between sleep onset (sleep time) and sleep offset (wake time). Actigraphy data were corroborated with sleep diaries.39 We also defined SJL as a binary variable (≥ 30 minutes difference between weekend and weekday sleep midpoint) to assess the prevalence of SJL in children less than 6 years old. The choice of cutoff (SJL ≥30 minutes) was based on parent-reported SJL of 35 minutes for preschool children of evening chronotype and a weekday-to-weekend difference in sleep period of 30 minutes for evening chronotypes.10 In addition to higher SJL, evening chronotypes exhibit more sleep problems and behavioral problems relative to preschool children who are morning or intermediate chronotypes.10,23 We also derived sleep duration from accelerometry data, including nighttime sleep duration and total 24-hour sleep duration.
Outcome variables
We defined temperament dimensions using the very short forms of Rothbart’s child and infant behavior questionnaires. Parents completed the following questionnaires: for infants 3–12 months, the Infant Behavior Questionnaire (IBQ)31; for children 1–3 years old, the Early Childhood Behavior Questionnaire (ECBQ)32; and for children > 3 years old, the Children’s Behavior Questionnaire (CBQ).30 Parents reported how often their child performed a certain behavior “in the last 2 weeks” using a Likert scale ranging from 1 (never) to 7 (always). Rothbart scores for each dimension were calculated by the following method: (1) select items indicated on the items-by-dimension list were first reverse-scored, by subtracting the numerical response given by the caregiver from 8 (eg, a caregiver response of 7 becomes 1); (2) scores for the 3 dimensions were then computed by dividing the sum of the scores for items receiving a numerical response by the number of items answered to yield a mean score for each dimension.30–32
Data analysis
We described categorical variables as frequencies (percentages) and continuous variables as means (standard deviations [SDs]). We used t test and analysis of variance or nonparametric equivalent (Mann-Whitney U test or Kruskal-Wallis test), as appropriate, to assess the association between SJL and baseline characteristics. For the primary analysis to test the associations of SJL and temperament, we used multivariable linear regression models adjusting for age, sex, ethnicity, and daycare/school attendance. For the secondary analysis, we developed a similar model to examine the association between sleep duration (24-hour sleep and nighttime sleep) and temperament. Statistical significance level was set at P < .05.
RESULTS
Demographics
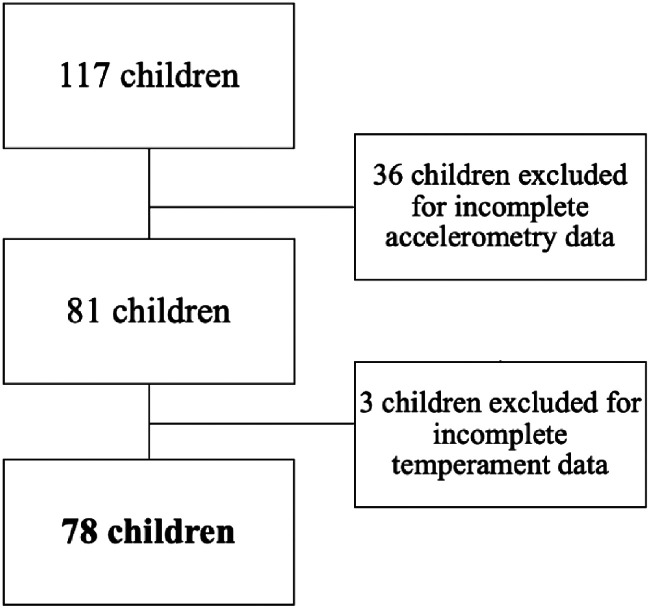
Among the 117 children younger than 6 years of age who had accelerometry performed, 34 were excluded due to incomplete accelerometry data (< 1 weekend and weekday), 2 children were excluded for incomplete accelerometry data with daylight savings time criteria applied, and 3 children were excluded due to temperament questionnaire completed not consistent with child’s age group at the time of accelerometry data collection (Figure 1). The demographic characteristics of the 78 children included in our study are presented in Table 1. Twenty (25.6%) children demonstrated ≥ 30 minutes of SJL. The mean SJL was 20 minutes (SD: 15.7 minutes) among children under 12 months of age, 19.9 minutes (SD: 19.8 minutes) for children aged 12 months to under 36 months, and 23 minutes for children 36 months to under 72 months of age (SD: 17.8 minutes).
Figure 1. Flowchart of children included in the study.
Table 1.
Baseline characteristics.
| Values | |
|---|---|
| Social jetlag in minutes, mean (SD) | 21.6 (17.8) |
| Sex, n (%) | |
| Female | 39 (50.0%) |
| Male | 39 (50.0%) |
| Age, n (%) | |
| < 12 months | 16 (20.5%) |
| 12–35.9 months | 21 (26.9%) |
| 36–72 months | 41 (52.6%) |
| Age in months, mean (SD) | 35.1 (20.5) |
| Family income (CAN$), n (%) | |
| < 60,000 | 4 (5.1%) |
| 60,000–99,999 | 12 (15.4%) |
| 100,000–149,999 | 24 (30.8%) |
| ≥ 150,000 | 38 (48.7%) |
| Siblings, n (%) | |
| No | 30 (38.5%) |
| Yes | 46 (59.0%) |
| Missing | 2 (2.5%) |
| School status, n (%) | |
| No school | 35 (44.9%) |
| Daycare/preschool | 37 (47.4%) |
| Missing | 6 (7.7%) |
| Child ethnicity, n (%) | |
| European | 46 (59.0%) |
| Non-European | 20 (25.6%) |
| Missing | 12 (15.4%) |
| Maternal ethnicity, n (%) | |
| European | 49 (59.3%) |
| Non-European | 20 (25.6%) |
| Missing | 9 (11.5%) |
| Maternal educational level, n (%) | |
| High school/apprenticeship/trade | 2 (2.6%) |
| College or university | 76 (97.4%) |
| Currently breastfeeding, n (%) | |
| No | 47 (60.3%) |
| Yes | 13 (16.7%) |
| Missing | 18 (23.0%) |
n = 78. CAN$ = Canadian dollars, SD = standard deviation.
Sleep characteristics and SJL
The mean duration of actigraphy data collection (number of valid days of actigraphy) was 5.7 days (SD: 0.9 days). Table 2 shows SJL stratified by baseline characteristics. Mean SJL was higher among families who reported their ancestry to be non-European (33.0 minutes; SD: 20.1 minutes; n = 20) compared with families who reported their ancestry to be European (17.7 minutes; SD: 15.6 minutes; n = 46). Mean SJL was higher in children who attended school or daycare (26.3 minutes; SD: 18.8 minutes; n = 37) vs children who did not attend school/daycare (17.6 minutes; SD: 14.5 minutes; n = 35; P < .05). The sleep features from the actigraphy data on weekdays and weekend days are presented in Table 3.
Table 2.
Social jetlag and baseline characteristics.
| n | Mean Social Jetlag (SD), min | |
|---|---|---|
| Age | ||
| < 12 months | 16 | 20.0 (15.7) |
| 12–35.9 months | 21 | 19.9 (19.8) |
| 36–72 months | 41 | 23.0 (17.8) |
| Sex | ||
| Female | 39 | 22.0 (20.3) |
| Male | 39 | 21.0 (15.3) |
| Family income (CAN$) | ||
| < 60,000 | 4 | 16.8 (10.6) |
| 60,000–99,999 | 12 | 21.6 (14.7) |
| 100,000–149,999 | 24 | 24.7 (23.4) |
| ≥ 150,000 | 38 | 20.1 (15.4) |
| Siblings | ||
| No | 30 | 21.6 (18.2) |
| Yes | 46 | 20.6 (17.6) |
| School status* | ||
| No school | 35 | 17.6 (14.5) |
| Daycare/preschool | 37 | 26.3 (18.8) |
| Child ethnicity* | ||
| European | 46 | 17.7 (15.6) |
| Non-European | 20 | 33.0 (20.1) |
| Maternal ethnicity* | ||
| European | 49 | 18.2 (2.1) |
| Non-European | 20 | 30.8 (5.02) |
| Currently breastfeeding | ||
| No | 47 | 20.6 (2.6) |
| Yes | 13 | 26.1 (5.5) |
n = 78. *P < .05, t test. CAN$ = Canadian dollars, SD = standard deviation.
Table 3.
Sleep features from actigraphy.
| Weekday | Weekend | |
|---|---|---|
| Wake time (hh:mm) | 07:32 (0:55) | 07:48 (1:04) |
| Sleep time (hh:mm) | 20:18 (0:50) | 20:25 (1:00) |
| Sleep midpoint (hh:mm) | 01:55 (0:45) | 02:07 (0:52) |
| Night sleep duration (h) | 11.2 (0.9) | 11.4 (1.1) |
Data are presented as mean (SD). n = 78. hh:mm = clock hour:minute, SD = standard deviation.
Associations of SJL and sleep with temperament
In the primary analysis using multivariable linear regression, there was no evidence of an association between SJL and temperament dimensions (Table 4). For the secondary analyses, we found evidence of an association between increased sleep duration (24-hour sleep and nighttime sleep) and increased negative affectivity scores (adjusted β coefficient [95% confidence interval]: 0.35 [0.18, 0.51] and 0.41 [0.16, 0.66], respectively).
Table 4.
Unadjusted and adjusted linear regression analysis.
| Surgency | Negative Affect | Effortful Control | ||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Social jetlag (min) | –0.02 (–0.01, 0.01) | 0.00 (–0.01, 0.02) | 0.10 (–0.01, 0.13) | –0.01 (–0.02, 0.01) | –0.13 (–0.02, 0.00) | –0.01 (–0.02, 0.01) |
| Total sleep in 24 hours (h) | 0.24 (0.01, 0.23) | –0.09 (–0.23, 0.05) | 0.13 (–0.05, 0.19) | 0.35** (0.18, 0.51) | –0.01 (–0.10, 0.09) | –0.14 (–0.28, 0.01) |
| Night sleep duration (h) | –0.09 (–0.34, 0.14) | –0.16 (–0.36, 0.04) | 0.28 (0.07, 0.56) | 0.41** (0.16, 0.66) | –0.08 (–0.26, 0.13) | –0.12 (–0.32, 0.10) |
Data are presented as β coefficients (95% confidence interval). n = 78. Adjusted and unadjusted linear regression analysis models for social jetlag, night sleep duration, total 24-hour sleep and temperament dimensions: surgency, negative affect, and effortful adjusted for sex, age, daycare/school attendance, and child ethnicity. **P < .005.
DISCUSSION
We found that increased sleep duration (24-hour and nighttime sleep duration), but not SJL, was associated with increased negative affectivity in preschool-aged children. Our study is the first study to examine the relationship between accelerometry-derived sleep measures and temperament in children less than 6 years old. Our findings suggest that SJL is prevalent in 1 in 4 children under 6 years old, with 25.6% of our cohort demonstrating ≥ 30 minutes of SJL, and even higher SJL among children attending daycare or preschool and in those of non-European ethnicity.
Doi et al10 conducted sleep surveys (self-reported measure of sleep) and similarly found that children aged 4–6 years old experience SJL at an average of 35 minutes in those with evening chronotypes (ie, a preference for later sleep and wake time). Our study further suggests that SJL may manifest in children younger than 4 years old (and as young as 6 months old) by demonstrating the prevalence of SJL with objective sleep measures.
Previous studies have evaluated sleep disparities among children of different ethnicities40,41; however, to our knowledge, no study has evaluated SJL directly among children of different ethnicities. Sleep habits and sleep quality vary among ethnicities; a review in the United States found that White children demonstrated more sufficient sleep, increased sleep duration, and fewer sleep/wake problems than Hispanic and Black youth.40 We observed a discrepancy in SJL between ethnicities, with more SJL observed in non-European compared with European children. We hypothesize that there may be a component of family routine, parenting practices, and environment that differs between ethnicities, which requires further investigation. Furthermore, we found that children attending daycare or school demonstrated greater mean SJL than children not attending either. This relationship suggests that SJL may be related to early start times in school or daycare resulting in circadian misalignment.
Doi et al10 studied the relationship between chronotype (individual’s preference in circadian rhythm) and behavior in Japanese children aged 4 to 6 years old and found that children with evening chronotypes were vulnerable to higher SJL and experienced greater behavioral problems such as hyperactivity and inattention. In contrast, we did not find that SJL was associated with temperament. This finding may be attributed to the differences in exposures since the study by Doi et al evaluated chronotype and not SJL directly using actigraphy. Moreover, our study included children aged 0 to just under 6 years old.
We found that increased sleep duration (24-hour and nighttime sleep) was associated with negative affectivity when adjusting for age, sex, ethnicity, and school status. A questionnaire-based study evaluating sleep duration and temperament among preterm infants at 2 years of age found that shorter nighttime sleep duration was associated with increased motor activity (surgency) and lower inhibition (effortful control).42 In contrast, we found that increased sleep duration was associated with increased negative affectivity, the latter of which can predispose children to developing internalizing behavior such as depression and low self-esteem. In adults, both short and long sleep duration is associated with increased risk of depression.43 Our findings may be an early manifestation of the relationship between sleep duration and depression risk in adults and adolescent populations.
Limitations of the current study include the cross-sectional design, which cannot provide strong evidence of a causal relationship between sleep and temperament (eg, directionality). Although temperament may affect sleep (eg, internalizing symptoms may lead to sleep problems), evidence from a randomized trial in school-aged children suggests that manipulating sleep duration alters temperament.16 We obtained participants from the TARGet Kids! cohort located in a large urban Canadian city (Toronto), which may not be representative of all preschool children. Moreover, many children were born to mothers of higher education, although higher education is frequent among women of childbearing age in Toronto. Although 7-day actigraphy provided only 1 weekend to assess SJL, actigraphy for 7 days has been shown to provide reliable measures of sleep in adolescents and school-aged and preschool children.37,38 Moreover, actigraphy permits noninvasive objective measurement of sleep and has been validated for use in preschool children.44 Further, we used established questionnaires to assess temperament. Questionnaire validity and reliability have been tested in this age group.30–32 Another limitation of the current study is that 30% of children had incomplete actigraphy data, which were unacceptable for analysis, because of illness, technical problems, and participant noncompliance.37 The children in our study were all under 6 years of age; as a result, compliance in wearing the accelerometer continuously over 1 week was difficult to obtain. Despite these challenges in young children, we managed to obtain complete objective and self- or parent’s reported data for 78 children (actigraphy and questionnaire data). Studies to date assessing SJL in preschool children (0–5 years of age) have only used self-reported sleep measures,9–12,14 despite discrepancies observed between parent reports and objective sleep measures,45,46 emphasizing the need for the use of complementary sleep assessment tools.39,47 No study has estimated SJL in this age group using objective sleep measures (actigraphy). The current study used both objective actigraphy data corroborated by sleep diaries to estimate sleep onset and sleep offset, capturing the different dimensions of sleep. Furthermore, 2 reviewers assessed actigraphy data with sleep diaries and consulted a third reviewer to resolve discrepancies. Finally, unmeasured confounding factors could have affected the results. Parenting/caregiving variables (eg, parental sleep patterns), family issues, or unforeseen circumstances might alter child sleep patterns, which also may affect behavior or child temperament. The measured variables and our sample size of 78 children allowed us to adjust for 4 important confounders (sex, age, child ethnicity, school/daycare attendance).12,41 Child ethnicity (European vs non-European) was a composite variable derived from maternal and paternal ethnicity, since the majority of parents identified as European. Furthermore, child school/daycare attendance also reflects parenting/caregiving characteristics. Future large longitudinal studies using objective sleep measures, such as > 7-day actigraphy data collection, are needed to confirm the current results. Further studies are also required to explore the effect of SJL with various outcomes as well as the underlying cause of the discrepancies in subpopulations to examine how sleep behaviors are patterned by ethnicity.
CONCLUSIONS
To our knowledge, this is the first study to investigate the associations between accelerometry-derived SJL and sleep duration with temperament in children less than 6 years old. Our study demonstrates that SJL varies in preschool-aged children by ethnicity and by daycare/preschool attendance. We did not find an association between SJL and temperament. Sleep duration was associated with negative affectivity, which could have implications for children developing behavioral problems such as depression or low self-esteem and can exacerbate pre-existing emotional and behavioral problems. Sleep duration and behavioral problems are related. Our findings highlight that this relationship may also be present in infants and preschool-aged children
SJL was present in young children less than 6 years of age. Understanding the impact of SJL on health and behavior is needed. Our study provides evidence that increased sleep duration was associated with negative affectivity. Large prospective longitudinal studies are required to confirm the observed association and to delineate the relationship of SJL and other sleep parameters with mental health to ensure optimal sleep habits and promote positive development and health.
ACKNOWLEDGMENTS
The authors thank Dr. MinGi Cho and Dr. Charlie Keown-Stoneman for their assistance with this study. They also thank the children and families who participated in this TARGetKids! study.
ABBREVIATIONS
- SD
standard deviation
- SJL
social jetlag
- TARGet Kids!
The Applied Research Group for Kids!
DISCLOSURE STATEMENT
The authors have reviewed and approved the submission of this manuscript. The authors report no conflicts of interest.
REFERENCES
- 1. Chaput JP, Gray CE, Poitras VJ, et al . Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth . Appl Physiol Nutr Metab. 2016. ; 41 ( 6 Suppl 3 ): 266 – 282 . [DOI] [PubMed] [Google Scholar]
- 2. Bathory E, Tomopoulos S . Sleep regulation, physiology and development, sleep duration and patterns, and sleep hygiene in infants, toddlers, and preschool-age children . Curr Probl Pediatr Adolesc Health Care. 2017. ; 47 ( 2 ): 29 – 42 . [DOI] [PubMed] [Google Scholar]
- 3. Rana M, Riffo Allende C, Mesa Latorre T, Rosso Astorga K, Torres AR . [Sleep in children: physiology and update of a literature review] . Medicina (B Aires). 2019. ; 79 ( Suppl 3 ): 25 – 28 . [PubMed] [Google Scholar]
- 4. Chaput JP, Gray CE, Poitras VJ, et al . Systematic review of the relationships between sleep duration and health indicators in the early years (0-4 years) . BMC Public Health. 2017. ; 17 ( Suppl 5 ): 855 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gruber R, Carrey N, Weiss SK, et al . Position statement on pediatric sleep for psychiatrists . J Can Acad Child Adolesc Psychiatry. 2014. ; 23 ( 3 ): 174 – 195 . [PMC free article] [PubMed] [Google Scholar]
- 6. Wittmann M, Dinich J, Merrow M, Roenneberg T . Social jetlag: misalignment of biological and social time . Chronobiol Int. 2006. ; 23 ( 1–2 ): 497 – 509 . [DOI] [PubMed] [Google Scholar]
- 7. Jankowski KS . Social jet lag: sleep-corrected formula . Chronobiol Int. 2017. ; 34 ( 4 ): 531 – 535 . [DOI] [PubMed] [Google Scholar]
- 8. Vetter C . Circadian disruption: what do we actually mean? Eur J Neurosci. 2020. ; 51 ( 1 ): 531 – 550 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Clara MI, Allen Gomes A . An epidemiological study of sleep-wake timings in school children from 4 to 11 years old: insights on the sleep phase shift and implications for the school starting times’ debate . Sleep Med. 2020. ; 66 : 51 – 60 . [DOI] [PubMed] [Google Scholar]
- 10. Doi Y, Ishihara K, Uchiyama M . Associations of chronotype with social jetlag and behavioral problems in preschool children . Chronobiol Int. 2015. ; 32 ( 8 ): 1101 – 1108 . [DOI] [PubMed] [Google Scholar]
- 11. Lan QY, Chan KC, Yu KN, et al . Sleep duration in preschool children and impact of screen time . Sleep Med. 2020. ; 76 : 48 – 54 . [DOI] [PubMed] [Google Scholar]
- 12. Muller D, Paine SJ, Wu LJ, Signal TL . Sleep timing and sleep problems of preschoolers in Aotearoa/New Zealand: relationships with ethnicity and socioeconomic position . Sleep Med. 2020. ; 76 : 1 – 9 . [DOI] [PubMed] [Google Scholar]
- 13. Randler C, Fontius I, Vollmer C . Delayed weekend sleep pattern in German infants and children aged 0–6 years . Biol Rhythm Res. 2012. ; 43 ( 3 ): 225 – 234 . [Google Scholar]
- 14. Randler C, Vollmer C, Kalb N, Itzek-Greulich H . Breakpoints of time in bed, midpoint of sleep, and social jetlag from infancy to early adulthood . Sleep Med. 2019. ; 57 : 80 – 86 . [DOI] [PubMed] [Google Scholar]
- 15. Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA . Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children . Sleep. 2005. ; 28 ( 12 ): 1568 – 1577 . [DOI] [PubMed] [Google Scholar]
- 16. Carissimi A, Dresch F, Martins AC, et al . The influence of school time on sleep patterns of children and adolescents . Sleep Med. 2016. ; 19 : 33 – 39 . [DOI] [PubMed] [Google Scholar]
- 17. Cespedes Feliciano EM, Rifas-Shiman SL, Quante M, Redline S, Oken E, Taveras EM . Chronotype, social jet lag, and cardiometabolic risk factors in early adolescence . JAMA Pediatr. 2019. ; 173 ( 11 ): 1049 – 1057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stoner L, Castro N, Signal L, et al . Sleep and adiposity in preadolescent children: the importance of social jetlag . Child Obes. 2018. ; 14 ( 3 ): 158 – 164 . [DOI] [PubMed] [Google Scholar]
- 19. Koopman ADM, Rauh SP, van’t Riet E, et al . The association between social jetlag, the metabolic syndrome, and type 2 diabetes mellitus in the general population: the New Hoorn Study . J Biol Rhythms. 2017. ; 32 ( 4 ): 359 – 368 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Parsons MJ, Moffitt TE, Gregory AM, et al . Social jetlag, obesity and metabolic disorder: investigation in a cohort study . Int J Obesity. 2015. ; 39 ( 5 ): 842 – 848 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Adan A, Archer SN, Hidalgo MP, Di Milia L, Natale V, Randler C . Circadian typology: a comprehensive review . Chronobiol Int. 2012. ; 29 ( 9 ): 1153 – 1175 . [DOI] [PubMed] [Google Scholar]
- 22. Schlarb AA, Sopp R, Ambiel D, Grünwald J . Chronotype-related differences in childhood and adolescent aggression and antisocial behavior—a review of the literature . Chronobiol Int. 2014. ; 31 ( 1 ): 1 – 16 . [DOI] [PubMed] [Google Scholar]
- 23. Jafar NK, Tham EK, Eng DZ, et al. ; Gusto Study Group . The association between chronotype and sleep problems in preschool children . Sleep Med. 2017. ; 30 : 240 – 244 . [DOI] [PubMed] [Google Scholar]
- 24. Larcher S, Gauchez AS, Lablanche S, Pépin JL, Benhamou PY, Borel AL . Impact of sleep behavior on glycemic control in type 1 diabetes: the role of social jetlag . Eur J Endocrinol. 2016. ; 175 ( 5 ): 411 – 419 . [DOI] [PubMed] [Google Scholar]
- 25. Malone SK, Zemel B, Compher C, et al . Social jet lag, chronotype and body mass index in 14-17-year-old adolescents . Chronobiol Int. 2016. ; 33 ( 9 ): 1255 – 1266 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wong PM, Hasler BP, Kamarck TW, Muldoon MF, Manuck SB . Social jetlag, chronotype, and cardiometabolic risk . J Clin Endocrinol Metab. 2015. ; 100 ( 12 ): 4612 – 4620 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Komada Y, Breugelmans R, Drake CL, et al . Social jetlag affects subjective daytime sleepiness in school-aged children and adolescents: a study using the Japanese version of the Pediatric Daytime Sleepiness Scale (PDSS-J) . Chronobiol Int. 2016. ; 33 ( 10 ): 1311 – 1319 . [DOI] [PubMed] [Google Scholar]
- 28. Rothbart MK, Ahadi SA, Hershey KL, Fisher P . Investigations of temperament at three to seven years: the Children’s Behavior Questionnaire . Child Dev. 2001. ; 72 ( 5 ): 1394 – 1408 . [DOI] [PubMed] [Google Scholar]
- 29. Rothbart MK . Becoming Who We Are: Temperament and Personality in Development. New York: ; Guilford Press; ; 2011. . [Google Scholar]
- 30. Putnam SP, Rothbart MK . Development of short and very short forms of the Children’s Behavior Questionnaire . J Pers Assess. 2006. ; 87 ( 1 ): 102 – 112 . [DOI] [PubMed] [Google Scholar]
- 31. Putnam SP, Helbig AL, Gartstein MA, Rothbart MK, Leerkes E . Development and assessment of short and very short forms of the Infant Behavior Questionnaire-revised . J Pers Assess. 2014. ; 96 ( 4 ): 445 – 458 . [DOI] [PubMed] [Google Scholar]
- 32. Putnam SP, Gartstein MA, Rothbart MK . Measurement of fine-grained aspects of toddler temperament: the early childhood behavior questionnaire . Infant Behav Dev. 2006. ; 29 ( 3 ): 386 – 401 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Roberts RE, Duong HT . Is there an association between short sleep duration and adolescent anxiety disorders? Sleep Med. 2017. ; 30 : 82 – 87 . [DOI] [PubMed] [Google Scholar]
- 34. Vriend JL, Davidson FD, Corkum PV, Rusak B, Chambers CT, McLaughlin EN . Manipulating sleep duration alters emotional functioning and cognitive performance in children . J Pediatr Psychol. 2013. ; 38 ( 10 ): 1058 – 1069 . [DOI] [PubMed] [Google Scholar]
- 35. Carsley S, Borkhoff CM, Maguire JL, et al. ; TARGet Kids! Collaboration . Cohort profile: The Applied Research Group for Kids (TARGet Kids!) . Int J Epidemiol. 2015. ; 44 ( 3 ): 776 – 788 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Paruthi S, Brooks LJ, D’Ambrosio C, et al . Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine . J Clin Sleep Med. 2016. ; 12 ( 6 ): 785 – 786 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Acebo C, Sadeh A, Seifer R, et al . Estimating sleep patterns with activity monitoring in children and adolescents: how many nights are necessary for reliable measures? Sleep. 1999. ; 22 ( 1 ): 95 – 103 . [DOI] [PubMed] [Google Scholar]
- 38. Lam JC, Mahone EM, Mason TB, Scharf SM . Defining the roles of actigraphy and parent logs for assessing sleep variables in preschool children . Behav Sleep Med. 2011. ; 9 ( 3 ): 184 – 193 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kushnir J, Sadeh A . Correspondence between reported and actigraphic sleep measures in preschool children: the role of a clinical context . J Clin Sleep Med. 2013. ; 9 ( 11 ): 1147 – 1151 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Guglielmo D, Gazmararian JA, Chung J, Rogers AE, Hale L . Racial/ethnic sleep disparities in US school-aged children and adolescents: a review of the literature . Sleep Health. 2018. ; 4 ( 1 ): 68 – 80 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Vaipuna TFW, Williams SM, Farmer VL, et al . Sleep patterns in children differ by ethnicity: cross-sectional and longitudinal analyses using actigraphy . Sleep Health. 2018. ; 4 ( 1 ): 81 – 86 . [DOI] [PubMed] [Google Scholar]
- 42. Caravale B, Sette S, Cannoni E, et al . Sleep characteristics and temperament in preterm children at two years of age . J Clin Sleep Med. 2017. ; 13 ( 9 ): 1081 – 1088 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zhai L, Zhang H, Zhang D . Sleep duration and depression among adults: a meta-analysis of prospective studies . Depress Anxiety. 2015. ; 32 ( 9 ): 664 – 670 . [DOI] [PubMed] [Google Scholar]
- 44. Bélanger MÈ, Bernier A, Paquet J, Simard V, Carrier J . Validating actigraphy as a measure of sleep for preschool children . J Clin Sleep Med. 2013. ; 9 ( 7 ): 701 – 706 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Aili K, Åström-Paulsson S, Stoetzer U, Svartengren M, Hillert L . Reliability of actigraphy and subjective sleep measurements in adults: the design of sleep assessments . J Clin Sleep Med. 2017. ; 13 ( 1 ): 39 – 47 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Girschik J, Fritschi L, Heyworth J, Waters F . Validation of self-reported sleep against actigraphy . J Epidemiol. 2012. ; 22 ( 5 ): 462 – 468 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Buysse DJ, Hall ML, Strollo PJ, et al . Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample . J Clin Sleep Med. 2008. ; 4 ( 6 ): 563 – 571 . [PMC free article] [PubMed] [Google Scholar]