Abstract
Purpose of review
To describe root causes of health disparities by reviewing studies on incidence and outcomes of systemic lupus erythematosus (SLE) related to ethnic, race, gender, or socioeconomic differences and to propose solutions.
Recent findings
SLE outcomes have steadily improved over the past 40 years but are not uniformly distributed across various racial and ethnic groups. Belonging to racial and ethnic minority has been cited as a risk factor for more severe disease and poor outcome in SLE. Population-based registries have demonstrated that Black patients with SLE have significantly lower life expectancy compared to White patients. Lower socioeconomic status has been shown to be one of the strongest predictors of progression to end stage renal disease in lupus nephritis. An association between patient experiences of racial discrimination, increased SLE activity, and damage has also been described. The lack of representation of marginalized communities in lupus clinical trials further perpetuates these disparities. To that end, the goal of a rheumatology workforce that resembles the patients it treats has emerged as one of many solutions to current shortfalls in care.
Summary
Disparities in SLE incidence, treatment, and outcomes have now been well established. The root causes of these disparities are multifactorial including genetic, epigenetic, and socioeconomic. The underrepresentation of marginalized communities in lupus clinical trials further worsen these disparities. Efforts have been made recently to address disparities in a more comprehensive manner, but systemic causes of disparities must be acknowledged and political will is required for a sustained positive change.
Keywords: Clinical trials, Disparities, Epidemiology, SLE
Background
Health disparities are inequalities in health status among members of a given population [1•]. The centers for disease control and prevention (CDC) defines health disparities as “preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations.” Systemic lupus erythematosus (SLE) is a complex autoimmune disease that causes widespread organ damage and results in significant morbidity and mortality. The mortality among patients with SLE has improved significantly over the past decades, but these improved survival rates are not consistent among all ethnic and racial groups. Significant differences in mortality exist amongst various populations affected by SLE [2, 3•]. Healthcare disparities are observed at almost all levels in SLE such as in its incidence, prevalence, disease activity, damage accrual, severity of disease manifestations (lupus nephritis -LN), and disease outcomes (e.g., end-stage renal disease -ESRD). These observed differences have led to recognizing racial and ethnic minority as an independent predictor of worse disease outcome in SLE.
Epidemiologic data from various countries shows profound disparities. A meta-analysis by Izmirly et al. in the USA reported a higher incidence and prevalence of SLE in minority populations and women across all registries [4]. In another example, a San Francisco county cohort demonstrated a higher age-standardized incidence and prevalence of SLE among ethnic minorities like Black (15.5 per 100,000 person-years; 241.0 per 100,000 persons), Asian/Pacific islander (4.1 per 100,000 person-years; 90.5 per 100,000 persons), and Hispanic (4.2 per 100,000 person-years; 94.7 per 100,000 persons) compared to their White counterparts (2.8 per 100,000 person-years; 55.2 per 100,000 persons) [5]. In the UK, the incidence and prevalence of SLE were found to be higher in patients of Afro-Caribbean and Asian ethnicity [6]. Similarly, higher SLE prevalence rates were reported in Caribbean overseas areas of France [7].
Disparities are also found in age of disease onset and severity. In a cohort of patients at a tertiary care clinic, Sun et al. observed that Black patients have more active, severe SLE compared to their White counterparts [8]. This was reflected in the higher Safety of Estrogens in Systemic Lupus Erythematosus National Assessment-Systemic Lupus Erythematosus Disease Activity Index (SELENA-SLEDAI) scores [8]. A recent study from the Monash Lupus Clinic in Australia showed increased disease severity and serologic activity among Asian patients compared with White patients [9]. Other studies have found that Black patients develop disease earlier and have more severe disease [10] and hispanic patients accrue greater damage compared to other ethnic groups [11].
Considerable differences have been noted in incidence and prevalence of lupus nephritis across various ethnic groups. Data from cohorts like California Lupus Surveillance Project (CLSP), lupus in minorities: nature versus nurture (LUMINA), the Genetic Profile Predicting the Phenotype Cohort (PROFILE), and the Southern California Lupus Registry (SCOLR) have all found greater incidence and prevalence of renal disease in Black and Hispanic patients [5, 11, 12]. The Grupo Latino Americano De Estudio del Lupus (GLADEL) cohort reported a higher rate of renal involvement in Black and mestizo patients compared to White patients [13]. Similarly, a study conducted in Hong Kong reported higher rates of renal involvement in Asian patients [14].
Carter et al. observed that Black and Asian/Pacific Islander patients have increased hematologic manifestations, and Black patients have increased neurologic manifestations compared to their White counterparts [1•]. A recent study found that Black, Asian/Pacific Islander, and Hispanic patients are at increased risk of developing severe hematological manifestations of lupus like thrombocytopenia, and anti-phospholipid antibody syndrome (APS) than White patients following SLE diagnosis [15]. An analysis of SLE-related skin manifestations provides some interesting insights regarding disparities. Discoid lupus is most common in patients of African descent. Conversely, White patients are more likely to have photosensitivity and malar rash compared to those of African descent [1•].
Mortality rates experienced by minority populations continue to be disproportionately high. The data from Georgia Lupus Registry (GLR) demonstrated that cumulative mortality was significantly higher among Black patients for both incident and prevalent SLE [16]. Similarly, CLSP observed that Black patients died an average of 6.8 years earlier than White patients (p = 0.05) and Hispanic patients died 9.5 years earlier than did persons who were not of Hispanic/Latino ethnicity [17]. The highest and fastest increasing SLE mortality rates in the USA from 1979–1998 were observed among Black women aged 45–64 [3•]. Outside the USA, the GLADEL cohort reported that non-White patients died at a younger age [13] and a South African study noted that Black patients have a poor prognosis with 5-year survival rates between 57 and 72% [18].
Substantial disparities have been noted in the quality of care provided to marginalized populations, perhaps due to implicit bias among healthcare professionals. For example, healthcare professionals have been shown to withhold treatments based on preconceived notions about medication compliance in patients belonging to ethnic minorities. Many potential participants from ethnic minorities never receive information about clinical research studies due to these implicit biases which contributes to ongoing underrepresentation of minorities in clinical research [19]. A systematic review by Fitzgerald and Hurst showed that ethnic minority patients receive lower quality of care, lower rate of referral to specialist, and poor visit communication compared to White patients [20]. While physician implicit bias in SLE has not been adequately explored, it is expected that the same bias observed in other areas of medicine applies here.
Yet another form of disparity is found in the historic underrepresentation of ethnic minorities in SLE clinical trials. Nearly 40% of the US population identify as racial and ethnic minorities; however, research participation by such minority populations is estimated to be only 2–16% [21•]. A recent review found that only 14% of SLE trial participants were Black compared to 51% White participants [22]. Race can affect treatment response in SLE [23]; therefore, low participation of minority populations may lead to misleading or inconclusive results about the appropriateness of certain treatments in specific racial groups. For example, small sample sizes of Black and Hispanic patients in the belimumab clinical trials led to inconclusive results about the effectiveness of the drug in these ethnic groups [24].
Healthcare disparities are associated with significant social and economic costs to individuals and societies. Specifically in SLE, healthcare disparities can be associated with direct costs, indirect costs, and reduced health-related quality of life (HrQOL) [25].
In this review, we have summarized the current literature on causes of health disparities observed in SLE. Additionally, we have examined the challenges involved in overcoming these disparities and potential solutions to this important public health issue.
Causes and challenges in remedies
Mirroring the heterogeneity of systemic lupus erythematosus itself, numerous causes underpinning the disparities in lupus prevalence and outcomes have been identified (Table 1).
Table 1.
Causes of SLE disparities and future avenues of inquiry
| Gender | •Intersection of gender with marginalizing sociocultural norms (i.e., increased poverty in women, delay in diagnosis due to bias or reduced access to care)Further areas of research:oPossible sex related differences in interferon alpha regulationoPossible X chromosome dose effect |
| Race/ethnicity |
•Effects of systemic racism •Discrete acts of discrimination at the individual level Further areas of research: oElevated stress levels |
| Genetic |
•CKD risk alleles in patients of African ancestry •Unfavorable genetic risk gradient amongst patients of African ancestry Further areas of research: oGWAS/EWAS in heterogeneous populations |
| Socioeconomic status (SES) |
•Poverty linked with higher damage, exit from poverty halts this effect •Poverty amongst leading predictors of mortality •Medical costs higher in patients with lower SES Further areas of research: oEmployment that does not offer paid sick leave and/or accommodate chronically ill workers oElevated stress levels |
| Geospatial |
•Unequal distribution of specialty care to rural areas, low/middle income countries •Higher risk for inconsistent care due to barriers related to travel •Residence in areas with highly concentrated poverty and/or marginalized populations associated with decreased retention in care and worse outcomes •Association of quality of care with geographic regions Further areas of research: oLupus hotspots and environmental links oLongitudinal outcomes in areas with reduction in tertiary care centers |
| Education | •Lower educational levels translate to decreased access to telemedicine venues |
| Healthcare system |
•Fragmented health care systems that are difficult to navigate •Unequal access to healthcare for marginalized groups •Workforce not representative of most affected populations •Patient education materials designed for patients with higher educational attainment •Additional complexity for patients from linguistic minorities |
| Research |
•Lack of funding for female predominant diseases •Exclusion of marginalized groups from participation both in study design and presence of logistical barriers •Drug trials not representative of most affected populations •Genomic research not representative of most affected populations and lacking geographical context Further areas of research: oEpidemiologic studies and registries in low and middle income countries |
| Physician-specific |
•Limited exposure to rheumatology training for generalists tasked with caring for patients with SLE •Limited training in reproductive health and psychiatry for rheumatologists •Bias in patterns of diagnosis and management Further areas of research: oDevelopment of global guidelines for lupus care |
| Patient-specific |
•Stage of development in adolescents and young adults limits adherence •Childhood trauma history •Co-morbid depression •Medication beliefs that negatively influence adherence Further areas of research: oMultidisciplinary approach to research and care oQualitative research on treatment adherence in varied populations |
| Community and family supports |
•Worse outcomes for patients with limited family support •Positive impact of community based participatory research demonstrated but lack of resources and political will to sustain such efforts Further areas of research: oBuilding community supports, use of peer navigators, community health workers |
Sociopolitical causes
Poverty
Patients living in poverty face many obstacles to care including low-wage employment without sick leave, unreliable or costly transportation, lower rates of medical insurance, difficulties with childcare, and stressors associated with living in marginalized communities (e.g., crime, infestation, pollutants, poor access to healthy foods). Poverty was found to be the most important predictor of mortality in the multi-ethnic LUMINA cohort [26]. Lower socioeconomic status (SES) was found to associate strongly with reduced survival amongst patients with end-stage renal disease (ESRD) from lupus nephritis in multiple studies, and the survival disadvantage among Black lupus patients with ESRD was found to be significantly attenuated by household income [27–29]. Lower socioeconomic status combined with exposure to crime leads to increased damage accrual since stressors such as food and housing insecurity strain patients’ focus and attention leading to neglect of SLE symptoms [30].
Racism
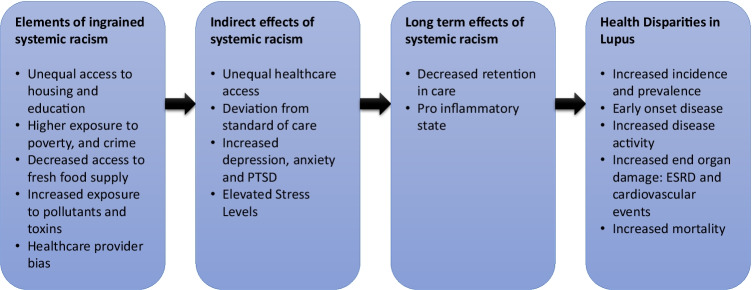
Structural racism perpetuates the cycle of poverty, with ongoing inequities in access to housing, education, and other environmental factors that lead to disparities in healthcare access, disease prevalence, and outcomes (Fig. 1). Race is frequently posited as a risk factor for more severe disease, and thus, the social construct of racial identity is conflated with an erroneous biologic (or genetic) construct of race. Illustrating this concept, the Systemic Lupus International Collaborating Clinics (SLICC) cohort showed higher damage in the US Black patients, but this difference was not seen in Black patients in ten other participating countries [31].
Fig. 1.
Overview of effects of systemic racism on disparities in SLE outcomes. Ingrained systemic racism in society involves a system where ethnic minorities have higher rates of poverty and unequal access to housing and education. This can have both indirect and long-term effects such as unequal healthcare access and elevated stress levels leading to a proinflammatory state. Figure 1 demonstrates how systemic racism can ultimately lead to disparities in SLE outcomes
Recent studies have identified patient reported experiences of racial discrimination as associated with increased SLE disease activity, end-organ damage and that experiences of vicarious racism via social media were associated with increased disease activity [32, 33].
Gendered disease
SLE is a disease of women, and women suffer gender-based disparities worldwide in part as a function of their subjugated role in societies. Funding for diseases that affect primarily women is less than non- or male-gendered diseases, putting SLE at a disadvantage relative to other chronic diseases. This may partially explain the slow drug development for this disease [34].
The biological reason behind the stark gender disparity in lupus remains elusive. Several putative mechanisms have been proposed, such as differences in the regulation of interferon alpha, potential dose effect of X chromosome, and differences in neutrophil biology, but more research is needed [35, 36].
Fertility preservation and pregnancy are important considerations for SLE patients who are predominantly diagnosed during reproductive age. Counseling patients about the short- and long-term effects of both SLE disease activity and associated treatments on reproductive health results in more favorable outcomes. However, rheumatologists may not discuss reproductive health issues with their patients, which was shown by only 40% of patients at risk for pregnancy reported receiving contraceptive counseling when starting teratogenic medications [37]. Adverse pregnancy outcomes in patients with SLE are more common than in the general population and lower socioeconomic status and belonging to Black race having the strongest association [38].
With respect to renal disease, women are more likely to donate a kidney but less likely to receive a transplant and have higher associated morbidity with renal replacement therapies [39, 40].
Occupational and environmental causes
Occupationally related environmental triggers have been identified by Cooper et al. as associated with an increased prevalence of SLE. Such triggers are more frequent with outdoor or industrial work (i.e., fine particulate air pollution, silica) and highly gendered workplaces in the case of solvent exposure in nail and hair salons [41]. Marginalized patients are more likely to be employed in these professions and hence more likely to be exposed to such environmental triggers of SLE. Additional exposure is related to housing that is grouped in proximity to large roadways, another source of fine particulate air pollution, which has been linked to gene hypomethylation in patients with SLE [42].
Unequal access to health care
Within the LUMINA cohort, Puerto Rican patients living in Puerto Rico distinguished themselves by their better outcomes compared with Hispanic and even with White and Black patients living in the USA [43]. One clear difference between the groups that could explain this difference was that Puerto Rican patients almost universally had medical insurance while the US patients did not. Puerto Rican patients likely also benefited from living in a relatively homogenous society where they were not marginalized as minorities unlike their US-based Black and Hispanic counterparts [44].
Patients with a lower SES are less likely to have a rheumatologist caring for their SLE and when they do have a rheumatologist, are more likely to have to travel long distances for care [45]. Ward found that patients who were uninsured or had Medicaid, had a younger age of onset for ESRD compared with patients with private insurance or Medicare; this was independent of race or ethnicity [28]. Patients with Medicaid can have difficulty finding specialty providers due to the difference in reimbursement which is lower than that of other publicly funded insurance coverage such as Medicare.
Genetic and epigenetic causes
Patients of African, Asian, and Amerindian descent have higher incidence of lupus nephritis (LN) and a younger age at onset which suggest a possible genetic component to this disparity [46]. The APOL 1 gene confers increased risk for chronic kidney disease and is selected in African populations. Patients who develop LN and are homozygous for APOL 1 are 2.5–11 times more likely to develop ESRD [47]. Additionally, variant TTC34 was found to confer elevated risk for LN in Hispanic patients [48].
A study examining epigenetic defects in B cells found in patients with SLE showed that Black patients had more transitional B cells and highly enriched methylated interferon regulated genes compared to White patients [49]. Exploring epigenetic processes, Lanata and colleagues identified clusters of disease phenotypes with more severe disease in non-White patients and differences in methylation between clusters, suggesting a role for environmental exposures perhaps modulated distinctly by ethnicity [50].
Geospatial causes
Neighborhood context with less hospitals and more Black residents correlated with worse individual outcomes for patients living in such areas, including less adherence to treatment [51]. This finding held true in a different context in the GLADEL cohort where rural residents were shown to have higher disease activity at diagnosis and higher rates of lupus nephritis during their disease course [52]. A population-based study looking at trends in SLE mortality in the USA over a 46-year period showed residence in Western US conferred a highest mortality risk in all racial/ethnic groups except for White patients who had the highest mortality if living in the South [53]. The reason for this difference in mortality based on region was thought to be multifactorial with higher mortality observed in the areas of concentrated poverty and/or higher concentration of Hispanic residents as well as due to regional differences in quality of care and access. Similarly, data from British Columbia revealed variability in incidence of lupus nephritis was attributable in part to the patient’s geographical residence [54].
Research causes
The earlier onset and more severe phenotype of lupus in Black, Hispanic, and Asian patients suggests there are genetic factors at play. The majority of participants in genome-wide association studies (GWAS) and epigenome-wide association studies (EWAS) were of European or Asian ancestry with disproportionately low participation from patients of African and Amerindian ancestry [55, 56].
Despite recognition of the racial and ethnic differences in the prevalence, severity, response to treatment, and overall outcomes in SLE, the current management guidelines for SLE are based on the data generated from randomized controlled trials (RCT) where majority of participants are White. The inclusion of racial minorities continues to be low, and this under representation of minorities in SLE clinical trials is most striking for Black patients. Multiple reasons have been identified for minority under-representation in RCTs such as limited knowledge about research, lack of resources, bias of healthcare provider in referring patients for research, and historical exploitation of minority communities in clinical research [19].
Health care system causes
Delays to specialty care and diagnosis
Global studies have cited complex systems for accessing specialty care, lack of awareness of SLE amongst frontline providers, and dearth of rheumatologists as reasons for delays in the initial SLE diagnosis [57, 58]. A US study found pediatric patients living in states with fewer rheumatologists led to longer delays in diagnosis [59].
Decreased access to specialty care
Patients without insurance or with Medicaid are likely to have inconsistent or delayed access to specialty rheumatology care which leads to preventable poor outcomes [60]. Medicaid beneficiaries were found to be more likely to use acute care settings for lupus care, and higher acute care users had up to 2.3 times higher odds ratio of mortality [61].
Other system causes
No references were found on the impact of native language on health disparities in patients with SLE, but there is literature in internal medicine that shows significant errors in communication with the use of ad hoc interpreters in place of trained interpreters as well as more poorly rated communication with language discordant patients and physicians independent of interpreter use [62, 63]
Health care provider specific causes
Poor screening patterns and prophylaxis use in marginalized patients
Mortality due to infection has improved in recent years, but is still one of the leading causes of death in lupus patients [64, 65]. Screening prior to immunosuppression, the use of appropriate prophylaxis, and judicious use of corticosteroid use are hallmarks of high-quality rheumatology care. Increased mortality from infections was identified in Black, Asian, and Native American patients living on the reservation when compared with White patients [66]. Children with SLE receiving Medicaid were found to have low rates of preventive care with only 3% receiving influenza vaccine and low rates of pneumocystis prophylaxis despite high rates of steroid use [67].
Health care bias in care and communication patterns
Health care providers including rheumatologists have shown to have implicit biases towards certain racial and ethnic groups. Black patients with lupus are less likely to receive standard of care treatment recommendations and received lower rates of antimalarial prescriptions in the first 5 years after diagnosis as compared to other races [43].
A comparison of Black and White patient adherence to medication found a significant disparity with Black patients being less adherent. This lower adherence was associated to fewer positive experiences of compassionate and respectful care [68]. Black patients were more likely to report feeling their rheumatologist was rushed when attending to their care [8]. Furthermore, patients are more likely to trust a provider from a similar racial background [69]. With the current rheumatology workforce being predominately White, minority patients are probably less likely to follow recommendations from their rheumatologist.
Patient-specific causes
Age at diagnosis
SLE has a significantly younger age of onset in Black, Hispanic, and Asian patients which has implications for medication adherence. Using national claims data, Feldman et al. found that Black and Hispanic patients were more likely to be nonadherent to hydroxychloroquine than White patients, a finding more pronounced in younger patients which also led to higher disease related morbidity [70]. Decreased medication adherence in younger patients with lupus has been found across many studies [71–73]
Depression
A study of patients with SLE and RA out of Iran showed an association between depression and medication non-adherence in both groups [74]. Medication adherence was studied in a group of Black and White patients with lupus and amongst Black patients depression was a factor in both medication non-adherence and missed appointments [75]. A recent study from China also found an association between depression and medication non-adherence [76].
Social network and support systems
An association between limited social supports and decreased health related quality of life has been found in patients with SLE [77]. This association has been noted in patients with higher levels of anxiety and/or depression in a binational study of patients from the Philippines and the USA (Southern California) [78]. Patients living in poverty and Black women are more likely to have limited social supports which contributes to increased damage accrual and mortality.
Limited health literacy
Study of health literacy in rheumatic diseases is sparse and is of interest given the association between limited health literacy and poor outcomes in other broader populations [79] Limited health numeracy was found to associate with higher disease activity in lupus patients [80]. Katz et al. found that patients with SLE and limited health literacy gave worse patient-reported outcome scores [81]. Interestingly, there were several studies which failed to show an association between medication non-adherence and health literacy [68, 73, 74]
Beliefs around medication use
Patients have differing beliefs and concerns around long-term medication use, and these beliefs may cluster in certain ethnic, socioeconomic, or other groups. Kumar and colleagues conducted a study of medication related health beliefs in British patients of South Asian and White ethnicities with RA or SLE using the Beliefs about Medications Questionnaire (BMQ). They found that South Asian patients scored significantly negatively on BMQ items for Specific Concern, General Overuse, and General Harm-related to medication use compared with White patients which indicated a higher risk for medication non-adherence [82]. However, a New Zealand study with an ethnically diverse patient population found that more highly rated BMQ measures of specific concern and general use associated with non-adherence and did not find significant associations by ethnic group [72]. In a group of mainland Chinese patients, positive scores on the BMQ scale associated with low to mild disease activity and there was generally high concern about medications and low self-reported medication adherence in this study [83]. A Canadian study with a diverse population of patients with lupus used the validated Medication Adherence Self Report Inventory (MASRI) to explore reasons for medication non-adherence and similar to the previously described studies measures on perceived harm of medications as well as disagreement on whether their condition would worsen without medications were associated with poorer adherence. There was not an association between race/ethnicity and MASRI measures in this study [84].
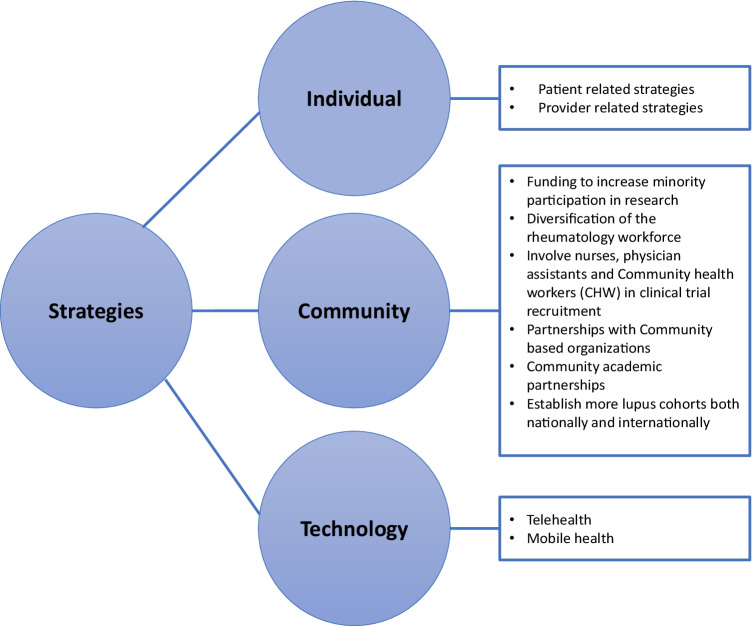
Suggestions and strategies
In recent years, significant work has been done to address healthcare disparities in SLE by employing both individual level and community level strategies (Fig. 2). While individual level strategies involving patients and healthcare providers are important, it is imperative to recognize that healthcare disparity is a systemic issue that requires structural change.
Fig. 2.
Solutions and strategies. Various strategies have been employed at both individual and community levels to address health disparities in SLE. Technology-based strategies are now increasingly being used for minority recruitment in clinical trials and in improving healthcare access
Individual level strategies
Patient-related strategies
Self-management is an effective individual level strategy to improve health disparities in minority populations. The Women Empowered to Live with Lupus (WELL) study demonstrated the effectiveness of the Chronic Disease Self-Management Program (CDSMP) among African American women with SLE [85]. Peer mentoring interventions have been successfully utilized in other chronic diseases that disproportionately affect minorities such as diabetes [86] and HIV [87] and are now being empirically tested for SLE. The Peer Approaches to Lupus Self-management (PALS) program involves Black women with SLE being paired together in a mentor–mentee relationship during a 12-week program. Mentees are guided by trained mentors in learning and regularly practicing disease self-management skills via weekly telephonic sessions [88]. Preliminary data from this cohort shows an improvement in self-management, reduction in disease activity and improvement in health-related quality of life (HRQOL) in the participants [88].
Provider-related strategies
It is important to acknowledge and overcome implicit bias amongst healthcare providers. Providers must acknowledge the legacy of exploitation of ethnic minorities by the healthcare system. Majority of the healthcare systems in the USA now mandate healthcare providers to attend workshops, conferences, and training modules on racial, cultural, religious, and linguistic sensitivities specific to minority communities. The impact of these educational endeavors on reducing healthcare disparities is yet to be seen.
The American College of Rheumatology (ACR) under the lupus initiative has undertaken several initiatives to educate non-rheumatologists about the healthcare disparities in lupus with the focus on early recognition and referral of patients suspected of lupus. This idea was successfully explored in the Lupus Education Assessment Program (LEAP) and Teaching Fellows in Lupus Project which involved Rheumatology fellows as educators and a presentation titled demystifying lupus by the ACR [89].
Pipeline programs are needed to attract and mentor more students from underrepresented minorities to health-related professions to diversify the medical workforce. Ethnic minority patients tend to listen to and trust health professionals that have similar ethnic background and are culturally competent and linguistically adept [69]. Amongst medical schools, Howard University has a “Young Doctors DC” program, and the University of North Carolina (UNC) has a “Minority Men in Medicine” program to enhance recruitment from minority populations. The Office of Minority Health and Health Equity (OMHHE) has collaborated with various institutions to establish training programs like the Project Imhotep (named after Imhotep, the world’s first doctor and architect who built Egypt’s first pyramid), the Future Public Health Leaders Program (FPHLP), and the US Centers for Disease Control and Prevention Undergraduate Public Health Scholars (CUPS) Program. These summer programs are designed to foster interest, provide educational, and research opportunities for minority students regarding public health [90].
Dedicated SLE clinics (involving internal medicine residents, postgraduate interns, and medical students) and post graduate SLE courses have also been arranged in the Philippines to foster an interest in rheumatology and to educate non-rheumatologists [91•].
Community level strategies
Disparities are systemic issues and require structural change and community level actions. Increasing minority participation in research is perhaps the most important strategy that can be implemented at the community level. Ensuring minority participation will ensure that therapy is guided by a representative population sample that reflects the unique genetic and epigenetic make up of minority patients, which should help address disparities and improve outcomes.
The ACR received a grant from the Office of Minority Health, Department of Health and Human Services, to develop strategies for increasing minority participation in lupus clinical trials. The ACR has developed a program to train healthcare providers and social workers to help enroll more lupus patients from ethnic minorities in clinical trials under the Materials to Increase Minority Involvement in Clinical Trials (MIMICT) and Community Health Worker Lupus Clinical Trials Training (LuCTT) initiatives. A peer-peer mentoring approach to increase minority participation in lupus clinical research is also currently underway at the Intramural Research Program at the National Institutes of Health in Bethesda, MD.
Outside of the physician–patient relationship, including other health professionals in the enrollment process, can increase minority participation in lupus clinical trials. Nurses, physician assistants, community health workers (CHWs), and patient advocates are all known to spend more time with patients. Such health professionals are trusted by patients and can play a significant role in patient education about lupus clinical trials [92].
Guidelines from the American College of Rheumatology can be adapted to meet local needs to educate non-rheumatologists. One such user-friendly primer was developed in the Philippines with a focus on early diagnosis, treatment, and prompt referral. Post-graduate SLE courses and dedicated SLE clinics involving trainees have also been arranged to educate non-rheumatologists [91•]. These strategies can help non-rheumatologists compensate for a lack of trained rheumatologists in a resource limited setting (Table 2).
Table 2.
Specific strategies to combat disparities in a resource-limited setting
| Patient-related strategies | •Patient and caregiver education•Patient empowerment with shared decision making and self-help programs•Peer to peer mentoring and support groups |
| Provider-related strategies |
•Incorporate SLE education in undergraduate, medical school and residency curriculums •Monthly (or more frequent) dedicated lupus clinics involving post graduate trainees and medical students to educate about SLE and foster a general interest in rheumatology •Post graduate SLE courses for the non-rheumatologist •Lupus education for the non-rheumatologist via a user friendly SLE primer developed by adapting ACR guidelines in accordance with local settings |
| Community social work |
•Multilingual CHWs/SWs to identify, educate, and refer SLE patients for dedicated care •Spread awareness in neighborhoods comprising communities of color •Community social work organizations to engage in advocacy to eliminate health disparities in SLE at various levels of government •Collaboration with health care organizations |
| Health care organizations |
•Recruitment for clinical trials •Setting up local SLE registries •Collaborations with community social work organizations for community outreach |
Community-based social work can act as a bridge for populations that are unable to access care. Multilingual outreach coordinators and CHWs can go to neighborhoods of marginalized populations and identify people with lupus. They can then help address biopsychosocial needs with healthcare referrals, housing, and education. Brochures can be distributed in settings that attract young women of color like salons, schools, shelters, and places of worship. Health fairs can be arranged in disadvantaged neighborhoods to create awareness about SLE. CHWs can also help arrange chronic disease self-management programs and peer to peer mentoring. Advocacy is needed at the local, state, and national level to adopt policies that allow affordable access to SLE care and medications. Collaboration with other community-based organizations and health care organizations is needed to serve potential patients, co-sponsor lupus-related programs, and conduct community-based research. The SLE Lupus foundation is an example of an organization that is involved in community-based social work, advocacy, and collaboration [93].
Life stressors have demonstrated a negative effect on SLE disease activity and outcomes. The American Psychological Association advocates “eliminating disparities in mental health status and mental health care through the use of psychological and behavioral research and services that are culturally and linguistically competent”. CHWs are trained to evaluate and address the biopsychosocial needs of patients. They can help implement the American Psychological Association recommendations by going disadvantaged neighborhoods, increasing awareness about mental health issues, and providing access to culturally and linguistically competent behavioral health services. A multidisciplinary approach to mental health is needed- this can involve increased partnerships physicians, behavioral health providers, government agencies, and families.
Population-based cohorts can play an important role in recognizing diverse disease phenotypes, identifying health disparities and outcomes, and providing data to help in disease management. Recognizing this, the CDC funded five population-based lupus registries in Georgia, Michigan, California, New York, and Indian Health Service (IHS). This is a step in the right direction, however, not all data are generalizable to the rest of the population. More national and international SLE cohorts are needed to understand the population at large better and to ultimately reduce health disparities.
Technology-based strategies
With the onset of the COVID-19 pandemic, telehealth has been successfully used to improve healthcare access to patients in general.
McDougall has discussed how this modality can also be leveraged to improve healthcare access to minorities in particular [94•]. The use of telehealth intervention focused on patient education and supervised non-pharmacological interventions such as physical exercise in SLE were found to be feasible in a recent review [95]. Using telehealth for such interventions can overcome some of the logistical challenges faced by minority populations. Many patients affected by SLE are young adults who are typically avid smartphone users and are adept at using mobile apps. Thus, mobile health (mHealth) can also play a significant role in recruiting participants [96] and collecting patient-reported outcomes (PRO) [97], especially due to ease of use and better accessibility. More studies regarding tele-health and mHealth are needed in SLE but early data is promising. Technology can, therefore, be used as a powerful tool to address prevalent heath disparities in SLE.
Conclusion
Most of the current work on health disparities in SLE has focused on identifying and exploring the causes behind health disparities. While it is certainly important to highlight disparities, this alone is not sufficient. As discussed above, different strategies to address disparities are now being implemented with variable success. It is important to recognize that disparities and racism are systemic issues. Therefore, we recommend advocacy, structural reform, and community level actions as more effective means to address this important public health issue.
Author contributions
All authors have made a substantial contribution to the conceptualization, drafting, and writing of this manuscript. All authors provide final approval for this version to be published and agree to be accountable for all aspects of the work. Individual contributions are as follows: BH was involved in the article concept and design, literature review, manuscript preparation, manuscript editing, and creating all figures and tables. AF was involved in the literature review, manuscript preparation, and editing figures and tables. SH was involved in the study concept and design, manuscript editing, and critical revision of this work.
Declarations
Disclosures
None.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bilal Hasan, Email: bilal.hasan@nih.gov.
Alice Fike, Email: alice.fike@nih.gov.
Sarfaraz Hasni, Email: Sarfaraz.hasni@nih.gov.
References
Papers of particular interest, published recently, have been highlighted as: •Of importance
- 1.Carter EE, Barr SG, Clarke AE. The global burden of SLE: prevalence, health disparities and socioeconomic impact. Nat Rev Rheumatol. 2016;12:605–620. doi: 10.1038/nrrheum.2016.137. [DOI] [PubMed] [Google Scholar]
- 2.Bernatsky S, et al. Mortality in systemic lupus erythematosus. Arthritis Rheum. 2006;54:2550–2557. doi: 10.1002/art.21955. [DOI] [PubMed] [Google Scholar]
- 3.Demas KL, Costenbader KH. Disparities in lupus care and outcomes. Curr Opin Rheumatol. 2009;21:102–109. doi: 10.1097/BOR.0b013e328323daad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Izmirly PM, et al. Prevalence of systemic lupus erythematosus in the united states: estimates from a meta-analysis of the centers for disease control and Prevention National Lupus Registries. Arthritis Rheumatol. 2021;73:991–996. doi: 10.1002/art.41632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dall'Era M, et al. The incidence and prevalence of systemic lupus erythematosus in San Francisco County, California: the California Lupus Surveillance Project. Arthritis Rheumatol. 2017;69:1996–2005. doi: 10.1002/art.40191. [DOI] [PubMed] [Google Scholar]
- 6.Rees F, et al. The incidence and prevalence of systemic lupus erythematosus in the UK, 1999–2012. Ann Rheum Dis. 2016;75:136–141. doi: 10.1136/annrheumdis-2014-206334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arnaud L, et al. Prevalence and incidence of systemic lupus erythematosus in France: a 2010 nation-wide population-based study. Autoimmun Rev. 2014;13:1082–1089. doi: 10.1016/j.autrev.2014.08.034. [DOI] [PubMed] [Google Scholar]
- 8.Sun K, et al. Racial differences in patient-provider communication, patient self-efficacy, and their associations with systemic lupus erythematosus-related damage: a cross-sectional survey. J Rheumatol. 2021;48:1022–1028. doi: 10.3899/jrheum.200682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golder V, et al. Association of Asian ethnicity with disease activity in SLE: an observational study from the Monash Lupus Clinic. Lupus. 2013;22:1425–1430. doi: 10.1177/0961203313500547. [DOI] [PubMed] [Google Scholar]
- 10.Lim SS, et al. The incidence and prevalence of systemic lupus erythematosus, 2002–2004: The Georgia lupus registry. Arthritis and Rheumatology. 2014;66:357–368. doi: 10.1002/art.38239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alarcón GS, et al. Systemic lupus erythematosus in three ethnic groups: IX. Differences in damage accrual. Arthritis Rheum. 2001;44:2797–2806. doi: 10.1002/1529-0131(200112)44:12<2797::AID-ART467>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 12.Alarcón GS, et al. Baseline characteristics of a multiethnic lupus cohort: PROFILE. Lupus. 2002;11:95–101. doi: 10.1191/0961203302lu155oa. [DOI] [PubMed] [Google Scholar]
- 13.Pons-Estel BA, et al. The GLADEL multinational Latin American prospective inception cohort of 1,214 patients with systemic lupus erythematosus: ethnic and disease heterogeneity among "Hispanics". Medicine (Baltimore) 2004;83:1–17. doi: 10.1097/01.md.0000104742.42401.e2. [DOI] [PubMed] [Google Scholar]
- 14.Mok CC, Lau CS. Lupus in Hong Kong Chinese. Lupus. 2003;12:717–722. doi: 10.1191/0961203303lu451xx. [DOI] [PubMed] [Google Scholar]
- 15.Maningding E, et al. Racial and ethnic differences in the prevalence and time to onset of manifestations of systemic lupus erythematosus: the california lupus surveillance project. Arthritis Care Res (Hoboken) 2020;72:622–629. doi: 10.1002/acr.23887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lim SS, et al. Racial disparities in mortality associated with systemic lupus erythematosus - Fulton and DeKalb Counties, Georgia, 2002–2016. MMWR Morb Mortal Wkly Rep. 2019;68:419–422. doi: 10.15585/mmwr.mm6818a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gianfrancesco MA, et al. Mortality among minority populations with systemic lupus erythematosus, including Asian and Hispanic/Latino persons—California, 2007–2017. Morb Mortal Wkly Rep. 2021;70:236. doi: 10.15585/mmwr.mm7007a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wadee S, Tikly M, Hopley M. Causes and predictors of death in South Africans with systemic lupus erythematosus. Rheumatology. 2007;46:1487–1491. doi: 10.1093/rheumatology/kem180. [DOI] [PubMed] [Google Scholar]
- 19.Yates I, et al (2020) Representation in clinical trials: a review on reaching underrepresented populations in research. Clin Res Retrieved from:https://acrpnet.org/2020/08/10/representation-in-clinical-trials-a-review-on-reaching-underrepresented-populationsin-research/
- 20.FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18:19. doi: 10.1186/s12910-017-0179-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lima K, et al. Factors associated with participation in rheumatic disease–related research among underrepresented populations: a qualitative systematic review. Arthritis Care Res. 2020;72:1481–1489. doi: 10.1002/acr.24036. [DOI] [PubMed] [Google Scholar]
- 22.Falasinnu T, et al. The representation of gender and race/ethnic groups in randomized clinical trials of individuals with systemic lupus erythematosus. Curr Rheumatol Rep. 2018;20:20. doi: 10.1007/s11926-018-0728-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Isenberg D, et al. Influence of race/ethnicity on response to lupus nephritis treatment: the ALMS study. Rheumatology (Oxford) 2010;49:128–140. doi: 10.1093/rheumatology/kep346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Furie R, et al. A phase III, randomized, placebo-controlled study of belimumab, a monoclonal antibody that inhibits B lymphocyte stimulator, in patients with systemic lupus erythematosus. Arthritis Rheum. 2011;63:3918–3930. doi: 10.1002/art.30613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barber MRW, Clarke AE. Socioeconomic consequences of systemic lupus erythematosus. Curr Opin Rheumatol. 2017;29:480–485. doi: 10.1097/bor.0000000000000416. [DOI] [PubMed] [Google Scholar]
- 26.Alarcón GSMGJ, Bartolucci AA, Roseman J, Lisse J, Fessler BJ, Bastian HM, Friedman AW, Reveille JD. Lupus in minority populations, nature versus nurture systemic lupus erythematosus in three ethnic groups IX Differences in damage accrual. Arthritis Rheum. 2001;44:2797–2806. doi: 10.1002/art.20409. [DOI] [PubMed] [Google Scholar]
- 27.Nee R, et al. Survival disparity of African American versus non-African American patients with ESRD due to SLE. Am J Kidney Dis. 2015;66:630–637. doi: 10.1053/j.ajkd.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 28.Ward MM. Medical insurance, socioeconomic status, and age of onset of endstage renal disease in patients with lupus nephritis. J Rheumatol. 2007;34:2024–2027. [PubMed] [Google Scholar]
- 29.Ward MM. Socioeconomic Status and the Incidence of ESRD. Am J Kidney Dis. 2008;51:563–572. doi: 10.1053/j.ajkd.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 30.Yelin ETL, Bunde J, Yazdany J. Poverty, neighborhoods, persistent stress, and systemic lupus erythematosus outcomes: a qualitative study of the patients' perspective. Arthritis Care Res. 2019;71:398–405. doi: 10.1002/acr.23599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bruce INOKA, Farewell V, Hanly JG, Manzi S, Su L, Gladman DD, Bae SC, Sanchez-Guerrero J, Romero-Diaz J, Gordon C, Wallace DJ, Clarke AE, Bernatsky S, Ginzler EM, Isenberg DA, Rahman A, Merrill JT, Alarcón GS, Fessler BJ, Fortin PR, Petri M, Steinsson K, Dooley MA, Khamashta MA, Ramsey-Goldman R, Zoma AA, Sturfelt GK, Nived O, Aranow C, Mackay M, Ramos-Casals M, van Vollenhoven RF, Kalunian KC, Ruiz-Irastorza G, Lim S, Kamen DL, Peschken CA, Inanc M, Urowitz MB. Factors associated with damage accrual in patients with systemic lupus erythematosus: results from the Systemic Lupus International Collaborating Clinics (SLICC) Inception Cohort. Ann Rheum Dis. 2015;74:1706–1713. doi: 10.1136/annrheumdis-2013-205171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chae DHMC, Fuller-Rowell TE, Spears EC, Smith TTG, Hunter EA, Drenkard C, Lim SS. Racial discrimination, disease activity, and organ damage: the Black Women's Experiences Living With Lupus (BeWELL) study. Am J Epidemiol. 2019;188:1434–1443. doi: 10.1093/aje/kwz105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martz CDAA, Fuller-Rowell TE, Spears EC, Lim SS, Drenkard C, Chung K, Hunter EA, Chae DH. Vicarious racism stress and disease activity: the Black Women's Experiences Living with Lupus (BeWELL) Study. J Racial Ethn Health Disparities. 2019;6:1044–1051. doi: 10.1007/s40615-019-00606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mirin AA. Gender disparity in the funding of diseases by the U.S. National Institutes of Health. J Womens Health. 2021;30:956–963. doi: 10.1089/jwh.2020.8682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scofield RHBG, Namjou B, Kimberly RP, Ramsey-Goldman R, Petri M, Reveille JD, Alarcón GS, Vilá LM, Reid J, Harris B, Li S, Kelly JA, Harley JB. Klinefelter's syndrome (47, XXY) in male systemic lupus erythematosus patients: support for the notion of a gene-dose effect from the X chromosome. Arthritis Rheumatol. 2008;58:2511–2517. doi: 10.1002/art.23701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gupta SNS, Blanco LP, O'Neil LJ, Wigerblad G, Goel RR, Mistry P, Jiang K, Carmona-Rivera C, Chan DW, Wang X, Pedersen HL, Gadkari M, Howe KN, Naz F, Dell'Orso S, Hasni SA, Dempsey C, Buscetta A, Frischmeyer-Guerrerio PA, Kruszka P, Muenke M, Franco LM, Sun HW, Kaplan MJ. Sex differences in neutrophil biology modulate response to type I interferons and immunometabolism. Proc Natl Acad Sci USA. 2020;117:16481–16491. doi: 10.1073/pnas.2003603117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yazdany J, et al. Quality of care in systemic lupus erythematosus: application of quality measures to understand gaps in care. J Gen Intern Med. 2012;27:1326–1333. doi: 10.1007/s11606-012-2071-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaplowitz ET, et al. Contribution of socioeconomic status to racial/ethnic disparities in adverse pregnancy outcomes among women with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2018;70:230–235. doi: 10.1002/acr.23263. [DOI] [PubMed] [Google Scholar]
- 39.Jindal RMRJ, Sajjad I, Murthy MH, Baines LS. Kidney transplantation and gender disparity. Am J Nephrol. 2005;25:474–483. doi: 10.1159/000087920. [DOI] [PubMed] [Google Scholar]
- 40.Adams SVRM, Streja E, Cheung AK, Arah OA, Kalantar-Zadeh K, Mehrotra R. Sex differences in hospitalizations with maintenance hemodialysis. J Am Soc Nephrol. 2017;28:2721–2728. doi: 10.1001/archinte.160.15.2349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cooper GSWJ, Bernatsky S, Claudio JO, Clarke A, Rioux JD. Occupational and environmental exposures and risk of systemic lupus erythematosus: silica, sunlight, solvents. Rheumatology. 2010;49:2172–2180. doi: 10.1093/rheumatology/keq214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lanata CNR, Nitiham J, Taylor K, Barcellos L, Chung S, Criswell L. Residential proximity to highways, DNA methylation and systemic lupus erythematosus. Arthritis Care Res. 2015;67:1604–1605. [Google Scholar]
- 43.Fernández M, et al. A multiethnic, multicenter cohort of patients with systemic lupus erythematosus (SLE) as a model for the study of ethnic disparities in SLE. Arthritis Rheum. 2007;57:576–584. doi: 10.1002/art.22672. [DOI] [PubMed] [Google Scholar]
- 44.Vilá LM, et al. Early clinical manifestations, disease activity and damage of systemic lupus erythematosus among two distinct US Hispanic subpopulations. Rheumatology. 2003;43:358–363. doi: 10.1093/rheumatology/keh048. [DOI] [PubMed] [Google Scholar]
- 45.Yazdany JGJ, Trupin L, Katz P, Panopalis P, Criswell LA, Yelin E. Association of socioeconomic and demographic factors with utilization of rheumatology subspecialty care in systemic lupus erythematosus. Arthritis Rheum. 2007;57:593–600. doi: 10.1002/art.22674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Feldman CHHL, Liu J, Fischer MA, Solomon DH, Alarcón GS, Winkelmayer WC, Costenbader KH. Epidemiology and sociodemographics of systemic lupus erythematosus and lupus nephritis among US adults with Medicaid coverage, 2000–2004. Arthritis Rheum. 2013;65:753–763. doi: 10.1002/art.37795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Limou SNG, Kopp JB, Winkler CA. APOL1 kidney risk alleles: population genetics and disease associations. Adv Chronic Kidney Dis. 2014;21:426–433. doi: 10.1053/j.ackd.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lanata CM NJ, Taylor KE, Chung SA, Torgerson DG, Seldin MF, Pons-Estel BA, Tusié-Luna T, Tsao BP, Morand EF, Alarcón-Riquelme ME, Criswell LA (2018) Genetic contributions to lupus nephritis in a multi-ethnic cohort of systemic lupus erythematous patients. PLoS One 13:e0199003. https://doi.org/10.1371/journal.pone.0199003. [DOI] [PMC free article] [PubMed]
- 49.Breitbach MERR, Roberts K, Kimberly RP, Absher D. Population-specific patterns of epigenetic defects in the B cell lineage in patients with systemic lupus erythematosus. Arthritis Rheum. 2020;72:282–291. doi: 10.1002/art.41083. [DOI] [PubMed] [Google Scholar]
- 50.Lanata CMPI, Nititham J, Taylor KE, Gianfrancesco M, Paranjpe M, Andrews S, Chung SA, Rhead B, Barcellos LF, Trupin L, Katz P, Dall'Era M, Yazdany J, Sirota M, Criswell LA. A phenotypic and genomics approach in a multi-ethnic cohort to subtype systemic lupus erythematosus. Nat Commun. 2019;10:1–13. doi: 10.1038/s41467-019-11845-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Feldman CHCK, Solomon DH, Subramanian SV, Kawachi I. Area-level predictors of medication nonadherence among US medicaid beneficiaries with lupus: a multilevel study. Arthritis Care Res. 2019;71:903–913. doi: 10.1002/acr.23721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pons-Estel GJ, et al. The impact of rural residency on the expression and outcome of systemic lupus erythematosus: data from a multiethnic Latin American cohort. Lupus. 2012;21:1397–1404. doi: 10.1177/0961203312458465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yen EY, et al. 46-year trends in systemic lupus erythematosus mortality in the United States, 1968 to 2013: a nationwide population-based study. Ann Intern Med. 2017;167:777–785. doi: 10.7326/m17-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Canney MID, McCandless LC, Reich HN, Barbour SJ. Disease-specific incident glomerulonephritis displays geographic clustering in under-serviced rural areas of British Columbia, Canada. Kidney Int. 2019;96:421–428. doi: 10.1016/j.kint.2019.02.032. [DOI] [PubMed] [Google Scholar]
- 55.Popejoy ABFS. Genomics is failing on diversity. Nature. 2016;538:161–164. doi: 10.1038/538161a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sirugo GWS, Tishkoff SA. The missing diversity in human genetic studies. Cell. 2019;177:26–31. doi: 10.1016/j.cell.2019.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lewandowski LB, et al. Missed opportunities for timely diagnosis of pediatric lupus in South Africa: a qualitative study. Pediatr Rheumatol. 2017;15:14. doi: 10.1186/s12969-017-0144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dey D, et al. Health disparities in rheumatic diseases: understanding global challenges in Africa, Europe, Latin America, and Asia and Proposing Strategies for Improvement. Rheum Dis Clin North Am. 2021;47:119–132. doi: 10.1016/j.rdc.2020.09.009. [DOI] [PubMed] [Google Scholar]
- 59.Rubinstein TB, et al. Delays to care in pediatric lupus patients: data from the childhood arthritis and rheumatology research alliance legacy registry. Arthritis Care Res. 2018;70:420–427. doi: 10.1002/acr.23285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yazdany JMB, Dean ML, Bardach NS, Duseja R, Ward MM, Dudley RA. Thirty-day hospital readmissions in systemic lupus erythematosus: predictors and hospital- and state-level variation. Arthritis Rheum. 2014;66:2828–2836. doi: 10.1002/art.38768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Feldman CH, et al. Patterns and predictors of recurrent acute care use among Medicaid beneficiaries with systemic lupus erythematosus. Semin Arthritis Rheum. 2020;50:1428–1436. doi: 10.1016/j.semarthrit.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nápoles AMS-OJ, Karliner LS, Gregorich SE, Pérez-Stable EJ. Inaccurate language interpretation and its clinical significance in the medical encounters of Spanish-speaking Latinos. Med Care. 2015;53:940–947. doi: 10.1097/MLR.0000000000000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sudore RLLC, Pérez-Stable EJ, Bibbins-Domingo K, Williams BA, Schillinger D. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns. 2009;75:398–402. doi: 10.1016/j.pec.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wu XYYM, Xie YS, Xiao WG, Lin J, Zhou B, Guan X, Luo CN, Che N, Liu XZ, Wang C, Teng JL, Cheng XB, Ye JN, Su YT, Shi H, Yin YF, Liu MR, Sun Y, Hu QY, Zhou ZC, Chi HH, Liu Y, Zhang X, Chen JW, Zhang MJ, Zhao DB, Yang CD, Wu LJ, Liu HL. Causes of death in hospitalized patients with systemic lupus erythematosus: a 10-year multicenter nationwide Chinese cohort. Clin Rheumatol. 2019;38:107–115. doi: 10.1007/s10067-018-4259-z. [DOI] [PubMed] [Google Scholar]
- 65.Bultink IEM, de Vreis F, van Vollenhoven RF, Lalmohamed A. Mortality, causes of death and influence of medication use in patients with systemic lupus erythematosus vs matched controls. Rheumatology. 2021;60:207–216. doi: 10.1093/rheumatology/keaa267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Falasinnu T, et al. Unraveling race, socioeconomic factors, and geographical context in the heterogeneity of lupus mortality in the United States. ACR Open Rheumatol. 2019;1:164–172. doi: 10.1002/acr2.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hiraki LTFC, Marty FM, Winkelmayer WC, Guan H, Costenbader KH. Serious infection rates among children with systemic lupus erythematosus enrolled in medicaid. Arthritis Care Res. 2017;69:1620–1626. doi: 10.1002/acr.23219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sun KEA, Criscione-Schreiber LG, Sadun RE, Rogers JL, Doss J, Corneli AL, Bosworth HB, Clowse MEB. Racial Disparities in medication adherence between African American and Caucasian patients with systemic lupus erythematosus and their associated factors. ACR Open Rheumatol. 2020;2:430–437. doi: 10.1002/acr2.11160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shen MJ, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018;5:117–140. doi: 10.1007/s40615-017-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Feldman CHCJ, Zhang Z, Subramanian SV, Solomon DH, Kawachi I, Costenbader KH. Dynamic patterns and predictors of hydroxychloroquine nonadherence among Medicaid beneficiaries with systemic lupus erythematosus. Semin Arthr Rheum. 2018;48:205–213. doi: 10.1016/j.semarthrit.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chehab GSG, Richter JG, Brinks R, Willers R, Fischer-Betz R, Winkler-Rohlfing B, Schneider M. Medical adherence in patients with systemic lupus erythematosus in Germany: predictors and reasons for non-adherence - a cross-sectional analysis of the LuLa-cohort. Lupus. 2018;27:1652–1660. doi: 10.1177/0961203318785245. [DOI] [PubMed] [Google Scholar]
- 72.Daleboudt GMBE, McQueen F, Kaptein AA. Intentional and unintentional treatment nonadherence in patients with systemic lupus erythematosus. Arthritis Care Res. 2011;63:342–350. doi: 10.1002/acr.20411. [DOI] [PubMed] [Google Scholar]
- 73.Flower CHI, Campbell M. The effect of psychosocial and neuropsychiatric factors on medication adherence in a cohort of women with systemic lupus erythematosus. J Clin Rheumatol. 2016;22:411–417. doi: 10.1097/RHU.0000000000000470. [DOI] [PubMed] [Google Scholar]
- 74.Shenavandeh SMA, Eazadnegahdar M, Nekooeian A. Medication adherence of patients with systemic lupus erythematosus and rheumatoid arthritis considering the psychosocial factors, health literacy and current life concerns of patients. Curr Rheumatol Rev. 2021;17:412–420. doi: 10.2174/1573397117666210301144651. [DOI] [PubMed] [Google Scholar]
- 75.Mosley-Williams ALM, Gillis M, Leisen J, Guice D. Barriers to treatment adherence among African American and white women with systemic lupus erythematosus. Arthritis Rheum. 2002;47:630–638. doi: 10.1002/art.10790. [DOI] [PubMed] [Google Scholar]
- 76.Du XCH, Zhuang Y, Zhao Q, Shen B. Medication adherence in Chinese patients with systemic lupus erythematosus. J Clin Rheumatol. 2020;26:94–98. doi: 10.1097/RHU.0000000000000952. [DOI] [PubMed] [Google Scholar]
- 77.Zheng YYD, Pan HF, Li WX, Li LH, Li J, Li XP, Xu JH. Influence of social support on health-related quality of life in patients with systemic lupus erythematosus. Clin Rheumatol. 2009;28:265–269. doi: 10.1007/s10067-008-1033-7. [DOI] [PubMed] [Google Scholar]
- 78.Zamora-Racaza GAD, Ishimori ML, Ormseth SR, Wallace DJ, Penserga EG, Sumner L, Ayeroff J, Draper T, Nicassio PM, Weisman MH. Role of psychosocial reserve capacity in anxiety and depression in patients with systemic lupus erythematosus. Int J Rheum Dis. 2018;21:850–858. doi: 10.1111/1756-185X.13033. [DOI] [PubMed] [Google Scholar]
- 79.Berkman NDSS, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 80.Maheswaranathan M, et al. Low health numeracy is associated with higher disease activity in systemic lupus erythematosus. Lupus. 2021;30:489–494. doi: 10.1177/0961203320979044. [DOI] [PubMed] [Google Scholar]
- 81.Katz P, et al. Impact of limited health literacy on patient-reported outcomes in systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2021;73:110–119. doi: 10.1002/acr.24361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kumar KGC, Toescu V, Buckley CD, Horne R, Nightingale PG, Raza K. Beliefs about medicines in patients with rheumatoid arthritis and systemic lupus erythematosus: a comparison between patients of South Asian and White British origin. Rheumatology. 2008;47:690–697. doi: 10.1093/rheumatology/ken050. [DOI] [PubMed] [Google Scholar]
- 83.Zhang L LW, Geng S, Ye S, Wang X, Qian L, Ding Y, Li T, Jiang A (2019) Lack of patient education is risk factor of disease flare in patients with systemic lupus erythematosus in China. BMC Health Serv Res 19:378. 10.1186/s12913-019-4206-y [DOI] [PMC free article] [PubMed]
- 84.Hardy CGD, Su J, Rozenbojm N, Urowitz MB. Barriers to medication adherence and degree of nonadherence in a systemic lupus erythematosus (SLE) outpatient population. Rheumatol Intl. 2021;41:1457–1464. doi: 10.1007/s00296-021-04898-0. [DOI] [PubMed] [Google Scholar]
- 85.Drenkard C, et al. Overcoming barriers to recruitment and retention of African-American women with SLE in behavioural interventions: lessons learnt from the WELL study. Lupus Science & Medicine. 2020;7:e000391. doi: 10.1136/lupus-2020-000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Heisler M, Piette JD. "I help you, and you help me": facilitated telephone peer support among patients with diabetes. Diabetes Educ. 2005;31:869–879. doi: 10.1177/0145721705283247. [DOI] [PubMed] [Google Scholar]
- 87.Rotheram-Borus MJ, et al. A cluster randomized controlled trial evaluating the efficacy of peer mentors to support South African women living with HIV and their infants. PLoS ONE. 2014;9:e84867. doi: 10.1371/journal.pone.0084867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Williams EM, et al. Peer approaches to self-management (PALS): comparing a peer mentoring approach for disease self-management in African American women with lupus with a social support control: study protocol for a randomized controlled trial. Trials. 2019;20:529. doi: 10.1186/s13063-019-3580-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gross D, et al. Lupus education advancement project (LEAP): Rheumatology fellows serving as educators increased knowledge and efficiency in lupus recognition and referral by providers in primary and emergency care. Arthritis Rheumatol. 2016;68:2595–2596. doi: 10.1002/art.39977. [DOI] [Google Scholar]
- 90.Bouye KE, McCleary KJ, Williams KB. Increasing diversity in the health professions: reflections on student pipeline programs. J Healthc Sci Humanit. 2016;6:67–79. [PMC free article] [PubMed] [Google Scholar]
- 91.Navarra SV, Zamora LD, Collante MTM. • Lupus education for physicians and patients in a resource-limited setting. Clin Rheumatol. 2020;39:697–702. doi: 10.1007/s10067-019-04795-9. [DOI] [PubMed] [Google Scholar]
- 92.Heller C, et al. Strategies addressing barriers to clinical trial enrollment of underrepresented populations: a systematic review. Contemp Clin Trials. 2014;39:169–182. doi: 10.1016/j.cct.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schudrich W, Gross D, Rowshandel J. Lupus and community-based social work. Soc Work Health Care. 2012;51:627–639. doi: 10.1080/00981389.2012.683694. [DOI] [PubMed] [Google Scholar]
- 94.McDougall J. Leveraging telemedicine as an approach to address rheumatic disease health disparities. Rheum Dis Clin North Am. 2021;47:97–107. doi: 10.1016/j.rdc.2020.09.008. [DOI] [PubMed] [Google Scholar]
- 95.Ritschl V, et al. Suitability for e-health of non-pharmacological interventions in connective tissue diseases: scoping review with a descriptive analysis. RMD Open. 2021;7:e001710. doi: 10.1136/rmdopen-2021-001710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Druce KL, et al. Recruitment and ongoing engagement in a UK smartphone study Examining the association between weather and pain: cohort study. JMIR Mhealth Uhealth. 2017;5:e168. doi: 10.2196/mhealth.8162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bell K, et al. Patient-reported outcome information collected from lupus patients using a mobile application: compliance and validation. ACR Open Rheumatol. 2021;4:99–109. doi: 10.1002/acr2.11370. [DOI] [PMC free article] [PubMed] [Google Scholar]