Abstract
Objective:
In Africa, there is up to 316 per 100,000 annual incidence rate of stroke, a prevalence of up to 1460 per 100,000, and a 3-year mortality rate higher than 80%. The incidence of stroke mortality in Ethiopia is 19.2%. Stroke is a major cause of disability and death worldwide. Early mortality in-hospital and deprived functional outcomes are common in acute stroke. This study aims to assess survival status and predictors of mortality among adult stroke patients.
Methods:
Institution-based retrospective cohort was conducted on patients who were admitted to Saint Paul’s Hospital Millennium Medical College. A simple random sampling technique was used. Bivariate and multivariable cox regression analysis were used to identify predictors of stroke mortality. For multivariable cox regression analysis statistically, significance was declared at p-value <0.05 and 95% CI.
Results:
A total of 251 adult stroke patient charts were included in the study. The overall Kaplan–Meier estimate showed that the probability of in-hospital stroke patients’ survival on the 41st day was nearly 50%. In this study, 77 (30.7%) of the study participants died. Decreased Glasgow Coma Scale (GCS) with adjusted hazard ratio (AHR) 4.26 (95% CI: 2.25–8.07) and p-value ⩽ 0.01 and presence of pneumonia with AHR 3.05 (95% CI: 1.29–7.21) and p-value ⩽ 0.01 are the predictor of mortality.
Conclusion:
The probability of survival relatively falls as follow-up time increases. The overall incidence of mortality among adult stroke patients was high. The decreased GCS and the presence of pneumonia are predictors of mortality among adult stroke patients.
Keywords: Stroke, survival, event, predictor of mortality, cardiovascular, neurology
Introduction
Africa had nearly 2–3 times higher rates of stroke incidence and greater stroke prevalence than Western Europe and the United States. In Africa, there is up to 316 per 100,000 annual incidence rate of stroke, a prevalence of up to 1460 per 100,000, and a 3-year mortality rate higher than 80%. 1 Almost 85% of the participants with stroke had ischemic stroke. 2 Stroke is highly increased in Africa in the last 20 years. 3 The burden of stroke is high in sub-Saharan African countries. 4
Early mortality in-hospital and deprived functional outcomes are common in acute stroke. 4 There were 58,010 deaths in Addis Ababa from 2006 to 2009. Among these, stroke was attributed to 11% of the total deaths. 5 The incidence of stroke mortality in Ethiopia’s Tikur Anbesa Specialized Hospital (TASH) was 19.2%. 6
Stroke is a major cause of disability and death worldwide.7 –9 Stroke mortality and disabled survivors increased due to a lack of health care facilities. 10 Stroke accounts for the fifth among all causes of death, next to heart diseases, cancer, chronic lower respiratory disease, and unintentional injuries/accidents. 7 The most commonly recognized risk factors for stroke are hypertension, dyslipidemia, and diabetes 11 which are followed by an unhealthy diet, tobacco use, alcohol drinking, and physical inactivity. 12 The warning signs of stroke are sudden unilateral weakness, sudden trouble with speaking, sudden trouble with walking, loss of balance, and dizziness. 11
To reduce the risk of stroke is adherence to a diet higher in nuts and olive oil. 7 Cardiovascular risk factor control interventions are important to decrease the risk of stroke and achieve better improvements in stroke outcomes. 13 Emergency medical service (EMS) is important for pre-hospital stroke care and transfer to stroke centers, which decreases stroke mortality. 14
The survival status and predictor of mortality among stroke patients are not assessed yet in Ethiopia. This study aims to assess survival status and predictors of mortality among adult stroke patients.
Methods
Study area
The study was conducted at Saint Paul’s Hospital Millennium Medical College (SPHMMC), Addis Ababa capital city of Ethiopia.
Study design and period
An institution-based retrospective cohort study was conducted. Adult patients admitted to SPHMMC from 1 January 2016 to 30 December 2018, with a primary diagnosis of stroke ischemic stroke (IS) or hemorrhage stroke (HS) confirmed by CT scan (computed tomography) or MRI (magnetic resonance imaging) included.
Size calculation and sampling procedure
Sample size was calculated by using Epi Info Version 7 statistical software by two population proportion formulas with 95% CI, power 80%, unexposed to exposed case ratio 1, percent of outcome in the unexposed group for heavy alcohol drinking was 6%, and percent of outcome in the exposed group for heavy alcohol drinking = 19% with an adjusted hazard ratio = 3.16. 15 Accordingly, the total sample size with a 10% incomplete chart becomes 256.
The medical record numbers (MRN) of stroke patients were taken from the Health Management Information System (HMIS). There were a total of 562 admitted stroke patients in SPHMMC from 1 January 2016 to 30 December 2018. By using a simple random sampling technique (a computer-generated method), 256 patient charts were recruited.
Inclusion and exclusion criteria
Inclusion criteria: age greater than or equal to 18 years old and the patient’s primarily diagnosed with ischemic stroke or hemorrhagic stroke.
Exclusion criteria: age less than 18 years old and incomplete chart.
Statistical analysis
Data were entered into Epidata 4.4 and analyzed using Stata14 statistical software. The outcome of each participant was dichotomized into censored or death. Kaplan–Meier was used to estimate the mean survival time and cumulative probability of survival. The cox-proportional hazard regression model assumption was checked using the Schoenfeld residual test, and variables having a p-value > 0.05 were considered as fulfilling the assumption. A bivariate cox-proportional hazards regression model was fitted for each explanatory variable. Those variables having a p-value ⩽ 0.25 in the bivariate analysis were entered into the multivariable cox-proportional hazards regression. The strength of association was measured by using the Adjusted Hazard ratio. The p-value with a 95% CI was used to assess the presence of statistical significance. Variables that have p-value ⩽ 0.05 were independent predictors of stroke mortality.
Operational definition
Event: Death of patient due to stroke during the hospital stay.
Censored: If a patient experienced either of the following (referred to other hospitals, against medical advice, or discharged from the hospital).
Results
Characteristics of adult stroke patients
Among a total of 256 study participant charts, 251 (98%) were included in the study while the rest of 5 (2%) were incomplete. The mean age of the patients was 57.6 years, with a standard deviation of ± 17.8. See Table 1.
Table 1.
Patients characteristics of survival status and predictors of mortality among adult stroke patients admitted to SPHMMC, Addis Ababa, Ethiopia, 1 January 2016 to 30 December 2018.
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Sex | Male | 123 | 49 |
| Female | 128 | 51 | |
| Age | ⩽50 | 87 | 34.7 |
| 51–60 | 54 | 21.5 | |
| 61–70 | 50 | 19.9 | |
| ⩾71 | 60 | 23.3 | |
| Types of stroke | Hemorrhagic stroke | 135 | 53.8 |
| Ischemic stroke | 116 | 46.2 | |
| Presence of pneumonia | Yes | 144 | 57.3 |
| No | 107 | 42.7 |
Patient baseline data
Among the total participants, 156 (62.3%) had SBP ⩾ 130 mmHg. Of the total participants, 161 (64.2%) had DBP ⩾ 80 mmHg. Fifty-five (21.9%) of the study participants had a GCS of less than nine. See Table 2.
Table 2.
Patients baseline data for survival status and predictors of mortality among adult stroke patients admitted in SPHMMC, Addis Ababa, Ethiopia, 1 January 2016 to 30 December 2018.
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Body temperature | <37.5°C | 191 | 76 |
| ⩾37.5°C | 60 | 24 | |
| SBP | <130 | 95 | 37.8 |
| ⩾130 | 156 | 62.3 | |
| DBP | <80 | 90 | 35.8 |
| ⩾80 | 161 | 64.2 | |
| Respiratory rate | ⩽20 | 135 | 53.8 |
| >20 | 116 | 46.2 | |
| pulse rate | ⩽100 | 197 | 78.5 |
| >100 | 54 | 21.5 | |
| GCS level | <9 | 55 | 21.9 |
| ⩾9 | 196 | 78.1 |
SBP: systolic blood pressure; DBP: diastolic blood pressure; GCS: Glasgow Coma Scale.
Pre-existing risk factors for stroke
From the total patients, 178, 173, and 110 of them had a previous history of hypertension, alcohol drinking, and diabetes mellitus, respectively. See Table 3.
Table 3.
A pre-existing risk factor of stroke for survival status and predictors of mortality among adult stroke patients admitted in SPHMMC, Addis Ababa, Ethiopia, 1 January 2016 to 30 December 2018.
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| History of stroke | No | 202 | 80.5 |
| Yes | 49 | 19.5 | |
| History of hypertension (HTN) | No | 73 | 29.1 |
| Yes | 178 | 70.9 | |
| History of Diabetic Mellitus (DM) | No | 141 | 56.2 |
| Yes | 110 | 43.8 | |
| Total | 251 | 100.0 | |
| History of cardiovascular diseases (CVD) | No | 155 | 61.8 |
| Yes | 96 | 38.2 | |
| History of alcohol drinking | No | 173 | 68.9 |
| Yes | 78 | 31.1 | |
| History of smoking | No | 195 | 77.7 |
| Yes | 56 | 22.3 |
Status of the study participants
From the total patients, 174 (69.3%) were censored. See Figure 1.
Figure 1.
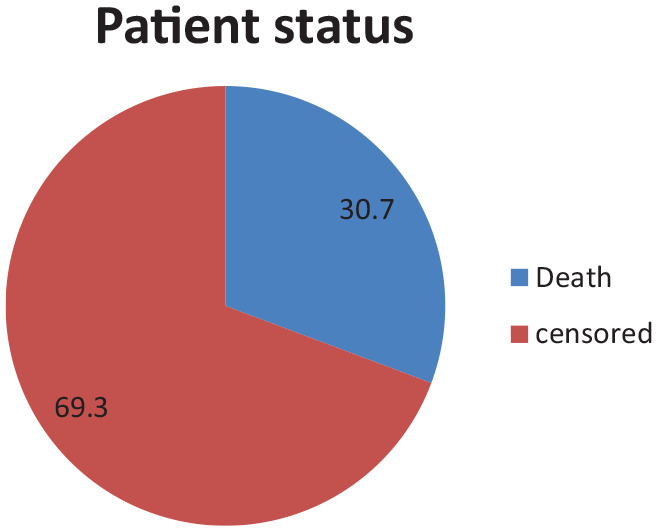
Status of adult stroke patients admitted to SPHMMC, Addis Ababa, Ethiopia, 1 January 2016 to 30 December 2018.
Overall survival function
The overall Kaplan–Meier estimate showed that the overall mean and median survival were 35.99 (95% CI: 32.97–39.01) and 41.00 (95% CI: 34.55–47.45) days, respectively. The probability of in-hospital adult stroke patients’ survival on the 1st, 4th, and 41st days was 99.6%, 95.6%, and nearly 50%, respectively. The probability of survival relatively falls as follow-up time increases. See Figure 2.
Figure 2.
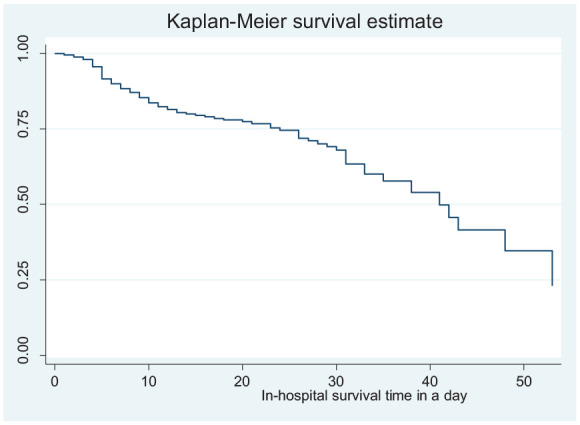
Overall Kaplan–Meier survival status among adult stroke patients admitted in SPHMMC, Addis Ababa, Ethiopia, 1 January 2016 to 30 December 2018.
Survival function and comparison of different categorical variables
In this study, an adult stroke patient who had a GCS level of less than nine had a lower survival time with a mean survival time of 15.89 (95% CI: 12.13–19.65) as compared to those who had a GCS level greater than nine with a mean survival time of 44.46 (95% CI: 40.99–47.94) and an adult stroke patient who developed pneumonia had a lower survival time of 24.93 (95% CI: 21.38–28.48) as compared to those who did not develop pneumonia with a survival time of 48.72 with (95% CI: 46.40–51.04).
Predictors of mortality among adult stroke patients
In bivariate cox regression analysis, the presence of pneumonia, level of GCS, respiratory rate, body temperature, previous history of cardiovascular diseases, previous history of diabetes mellitus, previous history of alcohol drinking, and previous history of smoking were candidates for multivariable cox regression analysis.
The result of the multivariable analysis showed that stroke patients who had GCS levels less than nine were more than four times more likely to die compared to those who had GCS levels greater than or equal to nine (AHR: 4.26 (95% CI: 2.25–8.07) with p-value ⩽ 0.01). Adult stroke patients who had pneumonia were three times more likely to die compared to those adult stroke patients who had no pneumonia (AHR: 3.05 (95% CI: 1.29–7.21) with a p-value ⩽ 0.01). See Table 4.
Table 4.
Results of Bivariate and Multivariable Cox regression analysis for survival status and predictors of mortality among adult stroke patients admitted in SPHMMC, Addis Ababa, Ethiopia, 1 January 2016 to 30 December 2018.
| Variable | Category | Dead n/N (%) | Censored | crude HR 95% CI | Adjusted HR 95% CI |
|---|---|---|---|---|---|
| Sex | Male | 46/123(37.3) | 77/123(62.7) | 1.48(0.93–2.35) | 0.86(0.49–1.50) |
| Female | 31/128(25.2) | 97/128(74.8) | 1 | 1 | |
| GCS Level | GCS < 9 | 52/55(94.5) | 3/55(5.4%) | 11.29(6.97–18.27) ** | 4.26(2.25–8.07) ** |
| GCS ⩾ 9 | 25/196(12.7) | 171/196(87.3) | 1 | ||
| Has Pneumonia | Yes | 65/107(60.7) | 42/107(39.3) | 8.92(4.814–16.55) ** | 3.05(1.29–7.21) ** |
| No | 12/144(8.3) | 132/144(91.7) | 1 | ||
| History of stroke | Yes | 21/49(42.8) | 28/49(57.2) | 1.57(0.95–2.61) | 0.96(0.51–1.80) |
| No | 56/202(27.7) | 146/202(72.3) | 1 | ||
| History of CVD | Yes | 42/96(43.7) | 54/96(56.3) | 2.13(1.35–3.35) ** | 1.42(0.62–2.08) |
| No | 35/155(22.6) | 120/155(77.4) | 1 | ||
| History of HTN | Yes | 63/178(35.4) | 115/178(64.6) | 1.58(0.88–2.84) | 0.82(0.40–1.71) |
| No | 14/73(19.2) | 59/73(90.8) | 1 | ||
| History of DM | Yes | 48/110(43.6) | 62/110(56.4) | 2.25(1.41–3.59) ** | 1.13(0.64–2.00) |
| No | 29/141(20.6) | 112/141(79.4) | 1 | ||
| History of drinking | Yes | 37/78(47.4) | 41/78(52.6) | 2.25(1.43–3.53) ** | 0.96(0.46–2.00) |
| No | 40/173(23.1) | 133/173(76.9) | 1 | ||
| History of smoking | Yes | 35/56(62.5) | 21(37.5%) | 3.14(2.00–4.94) ** | 1.34(0.63–2.84) |
| No | 42/195(21.5) | 153(88.5) | 1 | ||
| Temperature | < 37.5 °C | 35/191(18.3) | 156/191(81.7) | 1 | |
| ⩾ 37.5 °C | 42/60(70) | 18/60(30) | 5.21(3.30–8.25) ** | 1.43(0.78–2.61) | |
| Respiratory rate | ⩽ 20 | 18/135(13.3) | 117/135(86.6) | 1 | |
| > 20 | 59/116(50.9) | 57/116(49.1) | 4.28(2.52–7.27) ** | 1.12(0.57–2.18) | |
| Pulse rate | ⩽ 100 | 48/197(24.4) | 149/197(75.6) | 1 | |
| > 100 | 29/54(53.7) | 25/54(46.3) | 2.35(1.48–3.74) ** | 1.57(0.95–2.59) |
CHR: crude hazard ratio; AHR: adjusted hazard ratio; CVD: cardiovascular diseases; DM: diabetic mellitus.
(0.05 > p-value > 0.01) and **(p ⩽ 0.01).
Discussion
In this study, the overall median survival was 41.00 (95% CI: 34.55–47.45) days, which is lower than the study conducted at Ayder Comprehensive Specialized Hospital, which was 48 days, 16 and which is higher than the study conducted at Felege Hiwot Comprehensive Specialized Hospital, which was 7.8 days. 17
This study shows that the overall mortality of adult stroke patients admitted to SPHMMC during the study period was 77 (30.7%). This finding is higher than the study conducted in Zimbabwe which was 25%, 18 Nigerian teaching hospitals 35%, 19 Uganda 26.8%, 7 and Azerbaijan province 22%. 20 Justification those countries with better economies had advanced equipment and well-trained and adequate health professional which are used to deliver the appropriate care and medical management for their patients. 1
In this study, the presence of pneumonia was a predictor of mortality among stroke patients. It is consistent with a study conducted in Zimbabwe 18 and Nigeria. 19 The justification is that those patients who had pneumonia had developed abnormal lip closure, lingual incoordination, delay or absence of swallowing trigger reflex, and stroke patients can’t feed by themselves, which means they develop aspiration, which causes mortality.21,22
A decreased level of GCS has a strong association with adult stroke patients’ mortality with an adjusted hazard ratio. GCS level and stroke survival are inversely proportional. This finding is consistent with a study conducted in Uganda 4 and Nigeria. 19 The reason might be that decreased GCS level can’t survive compared to a patient with a normal GCS level because the brain controls all activity of the body, so they may develop airway obstruction and they can’t control hunger. 23
Limitations
Since the data was collected from a secondary source, some important predictors such as fasting blood sugar and cholesterol level (high-density lipoprotein (HDL)/low-density lipoprotein (LDL)) were not assessed.
Conclusion
The probability of survival relatively falls as follow-up time increases. The overall incidence of mortality among adult stroke patients was high. Decreased levels of the GCS and the presence of pneumonia are predictors of mortality among adult stroke patients. Health professionals should be able to assess early to manage pneumonia among adult patients admitted with stroke.
Acknowledgments
We would like to express our heartfelt appreciation to the data collector and staff of SPHMMC for their collaboration and support of the study process.
Footnotes
Author contributions: T.S.A. designed the study, was involved in data collection, did the analysis and interpretation of the result and drafted the paper, and participated in preparing all versions of the manuscript. H.M., T.A., T.A., and T.M. assisted in the design, proposal development, monitoring during data collection, assisted during analysis, and revised subsequent drafts of the paper. All authors read and approved the final manuscript.
Data availability: The data sets used/or analyzed during the current study available to all authors on reasonable request.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors declare that they have no conflict of interest. This paper is part of H.M.’s thesis in school of graduate studies at Addis Ababa University in partial fulfillment of a Master of Science degree in adult health nursing.
Ethical approval: Ethical approval for this study was obtained from Addis Ababa University College of health sciences Institutional Ethical Review Board with protocol number 040/19/SNM then formal letter was written to the study hospital (SPHMMC).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Informed consent was not sought for the present study because The Independent Ethics committee of SPHMMC exempts the requirement for informed consent to use the patients’ medical records to conduct the research. To ensure confidentiality, the name of the clients was not recorded and medical records were immediately returned to the record room after collecting the necessary information.
Trial registration: Not applicable because this is not a clinical trial.
ORCID iDs: Tadesse Sahle Adeba  https://orcid.org/0000-0003-2727-328X
https://orcid.org/0000-0003-2727-328X
Tamirat Melis  https://orcid.org/0000-0001-5536-8169
https://orcid.org/0000-0001-5536-8169
References
- 1. Akinyemi RO. Stroke in Africa: the profile, progress, prospects, and priorities. Nat Rev Neurol 2021;17: 634–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics — 2015 update. A report from the American Heart Association. Circulation 2015; 131: e29–e322. [DOI] [PubMed] [Google Scholar]
- 3. Owolabi MO, Akarolo-Anthony S, Akinyemi R, et al. The burden of stroke in Africa: a glance at the present and a glimpse into the future. Cardiovasc J Afr 2015; 26(2 Suppl. 1): S27–S38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nakibuuka J, Sajatovic M, Nankabirwa J, et al. Early mortality and functional outcome after acute stroke in Uganda: a prospective study with 30 days follow-up. Springerplus 2015; 4: 450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Misganaw A, Mariam DH, Araya T. The double mortality burden among adults in Addis Ababa, Ethiopia, 2006-2009. Prev Chronic Dis 2012; 9: E84–E89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sultan M, Debebe F, Azazh A, et al. Epidemiology of stroke patients in Tikur Anbessa specialized hospital: emphasizing clinical characteristics of hemorrhagic stroke patients. Ethiop J Heal Dev 2017; 31: 13–17. [Google Scholar]
- 7. Fornage M, Gillespie C, Isasi CR, et al. Heart disease and stroke statistics—2017 update: a report from the American Heart association. Circulation 2017; 135: e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. On U, Global THE and Of B. Update on the global burden of ischaemic and haemorrhagic stroke in 1990–2013: the GBD 2013 study. Neuroepidemiology 2016; 45(3): 161–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century. Stroke 2013; 44: 2064–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Venketasubramanian N, Yoon W, Pandian J, et al. Stroke epidemiology in South, East, and South-East Asia: a review. J Stroke 2017; 19(3): 286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Saengsuwan J, Suangpho P, Tiamkao S. Knowledge of stroke risk factors and warning signs in patients with recurrent stroke or recurrent transient ischaemic attack in Thailand. Neurol Res Int 2017; 19: 286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res 2017; 120: 439–448. [DOI] [PubMed] [Google Scholar]
- 13. Lackland DT, Roccella EJ, Deutsch AF, et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke 2014; 45: 315–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Adams HP, Bruno A, Connors JJB, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019; 50: e344–e418. [DOI] [PubMed] [Google Scholar]
- 15. Putaala J, Curtze S, Hiltunen S, et al. Causes of death and predictors of 5-year mortality in young adults after first-ever ischemic stroke. Stroke 2009; 40(8): 2698–2703. [DOI] [PubMed] [Google Scholar]
- 16. Hagos Gufue Z, Gizaw NF, Ayele W, et al. Survival of stroke patients according to hypertension status in Northern Ethiopia: seven years retrospective cohort study. Vasc Health Risk Manag 2020; 16: 389–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Walelgn N, Abyu GY, Seyoum Y, et al. The survival status and predictors of mortality among stroke patients at North West Ethiopia. Risk Manag Healthc Policy 2021; 14: 2983–2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kaseke F, Stewart A, Gwanzura L, et al. Clinical characteristics and outcomes of patients with stroke admitted to three tertiary hospitals in Zimbabwe: a retrospective one-year study. Malawi Med J 2017; 29(2): 177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ekeh B, Ogunniyi A, Isamade E, et al. Stroke mortality and its predictors in Nigerian teaching hospital. African Heal Sci 2015; 15(1): 74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shamshirgaran SM, Barzkar H, Savadi-Oskouei D, et al. Predictors of short-term mortality after acute stroke in East Azerbaijan province, 2014. J Cardiovasc Thorac Res 2018; 10(1): 36–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yoon H, Shim SS, Jung S, et al. Long-term mortality and prognostic factors in aspiration pneumonia. J Am Med Dir Assoc 2019; 20: 1098–1104.e4. [DOI] [PubMed] [Google Scholar]
- 22. Chang C, Cheng T, Lin C. Reporting of aspiration pneumonia or choking as a cause of death in patients who died with stroke. Stroke 2015(1): 1182–1186. [DOI] [PubMed] [Google Scholar]
- 23. Jain SIL. Glasgow Coma Scale. Treasure Island, FL: StatPearls, https://www.ncbi.nlm.nih.gov/books/NBK513298/ [Google Scholar]


