ABSTRACT
The need for adherence to a healthy and sustainable dietary pattern in the pediatric stage is discussed worldwide, being linked to a progressive incidence of noncommunicable diseases in adulthood. The aims of this systematic review were to summarize the healthy and/or sustainable dietary patterns, defined a priori, described in the literature for use during the pediatric stage; to evaluate the adherence to these dietary patterns; and identify the health-related benefits associated with adherence to these patterns. A literature search was carried out on Medline, Scopus, and Web of Science from 2010 up to 2021, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A total of 128 articles were included according to the following criteria: participants 2–17 y old, healthy and/or sustainable dietary patterns defined by an a priori methodology; articles written in English or Portuguese; and published since 2010. Fifty instruments with 14 adaptations that measure adherence to healthy and/or sustainable dietary patterns in children and adolescents were found. The Mediterranean Diet was the most studied dietary pattern. Adherence to healthy and/or sustainable dietary patterns has wide variations worldwide. Most of the instruments described have been little studied at pediatric ages, reducing the ability to extrapolate results. Higher adherence to these dietary patterns was associated with lower body fat, waist circumference, blood pressure, and metabolic risk. There is no consensus regarding the association with BMI. No studies have proofs of the sustainability characteristics of these instruments, it being necessary to produce a new sustainable instrument or test the association of the previous ones with, for example, the ecological footprint. Further validations of these instruments in each country and more prospective studies are needed to establish temporal relations with health-related outcomes.
This systematic review was registered at www.crd.york.ac.uk/prospero/ as CRD42020221788.
Keywords: feeding behaviors, diet, children, adolescent, health, sustainability, systematic review
Statement of Significance: This is the first article to systematically search and review the scientific literature available on healthy and sustainable dietary patterns in children and adolescents.
Introduction
According to the FAO, a dietary pattern is defined as “the quantities, proportions, and combinations of different foods and beverages in diets and the frequency of how they are habitually consumed” (1). It is estimated that diets are connected to around one-third of the human influence on climate change and land use (2). The increase of the world population as well as the changes in food consumption patterns, in particular the increase of meat consumption (3), disturb climate, food security, ecosystem health, and populations’ health and nutrition (4, 5). Therefore, it is urgent to face the existence of a global unsustainable food system that produces climatic, socioeconomic, political, and financial crises (5). The world needs sustainable diets, with low-input, local, and seasonal food production and a short production–consumption distance. Although there is currently no universally agreed-upon definition of a “sustainable diet,” FAO experts, in 2010, agreed that:
Sustainable diets are those diets with low environmental impacts which contribute to food and nutrition security and to healthy life for present and future generations. Sustainable diets are protective and respectful of biodiversity and ecosystems, culturally acceptable, accessible, economically fair and affordable; nutritionally adequate, safe and healthy; while optimizing natural and human resources. (6)
Globally, there has been a reduction in the adherence to these sustainable dietary patterns over the decades, such as the Mediterranean dietary pattern (7). This dietary pattern is widely known in the literature to be sustainable on account of having a low ecological footprint, because it is rich in fruits and vegetables and low in meat. Besides, its characterization by biodiverse, eco-friendly, and traditional consumption helps benefit future generations (8). Lower adherence to the Mediterranean Diet (MD) appears to be more prevalent among the young, and children and adolescents (<18 y old) seem to be a particular cause of concern (9, 10).
A healthy dietary pattern can be defined as one which complies with dietary guidelines’ recommendations in relation to food group consumption. Adherence to healthy dietary patterns reflects achieving all nutrient and energy requirements. Nonadherence to healthy diets is linked to a progressive incidence of noncommunicable diseases such as the rise of pediatric obesity (11) and cardiovascular diseases (12). The assessment of healthy dietary patterns in children and adolescents, as well as the identification of their main modifiable determinants, are extremely important because food habits and behaviors developed in childhood and adolescence tend to track into adulthood (13, 14) and can predict adults’ diet-related diseases (15).
For all these reasons, nutrition and health education regarding healthy and sustainable dietary patterns is demanded everywhere, particularly from childhood (16). It is urgent to profoundly change the world's current dietary pattern and promote culturally appropriate, biodiversity-based, ecofriendly, sustainable, and healthy diets starting in childhood (5, 6). As such, we require the ability to measure the adherence to healthy and sustainable dietary patterns. Commonly, 2 analytical approaches are used to derive dietary patterns: a posteriori and a priori. The a posteriori approach is based on statistical methods and uses dietary information collected from the sample under study. This kind of approach is occasionally difficult because different samples are expected to lead to the extraction of different components, hampering straight comparisons among populations. The a priori approach is defined based on previously established evidence/data which creates predefined dietary patterns (17). The Mediterranean Diet Score (MDS) and the Southern European Atlantic Diet (SEAD) are examples of a priori indexes that measure adherence to the MD and to the Atlantic Diet, respectively (18, 19). However, their utility and validity in pediatric populations worldwide are relatively understudied. The several adaptations of these instruments performed over time also make difficult their evaluation.
Adherence to healthy and sustainable dietary patterns, especially in adults, using a single focus (e.g., MD adherence) has been reviewed previously (20, 21). However, less has been compiled about these dietary patterns in children and adolescents. In 2011, 2 reviews explored diet quality measures in this age range (but only from developed countries) and concluded that research establishing the predictive validity of dietary pattern methods in childhood is needed (22, 23). In 2014 and recently, in 2020, 2 more systematic reviews were conducted regarding this issue (24, 25). However, none of them took into account the sustainability of the instruments found. The present study expands on the information presented in these reviews by incorporating additional studies, as well as investigating the existence of a sustainability factor in the pediatric instruments under review, thereby providing a more thorough and updated summary of the sustainable dietary pattern instruments’ characteristics and uses in children and adolescents.
As such, the objectives of this systematic review are 1) to identify and characterize the healthy and sustainable dietary patterns (defined a priori) used in children and adolescents and described in the literature, also identifying the methodology used for their construction (food items/nutrients included and scoring methods, or others); 2) to evaluate the adherence to the healthy and sustainable dietary patterns studied in children and adolescents; and 3) to identify the benefits associated with adherence to the studied dietary patterns. Supplemental Table 1 presents the answers to the Population, Indicator, Comparator, Outcomes, and Study design (PICOS) question.
Methods
Study design
This systematic review was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (26), using the PRISMA guidelines (27), and is registered prospectively with the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020221788).
Search strategy
The search to respond to the systematic review objectives was performed from October to December 2021 in 3 databases, namely Medline, Scopus, and Web of Science.
Search terms were developed by a reviewerwith inputs from the research team. In PubMed, the final search results were identified by using the following expression: (“sustainable diet*” OR “healthy diet*” OR “dietary pattern” OR “food pattern” OR “healthy dietary pattern” OR “diet quality” OR “diet variety” OR “food variety” OR (behaviors, feeding[MeSH Terms])) AND (children[MeSH Terms] OR “young people” OR adolescent[MeSH Terms]) AND (“score” OR index* OR (abstracting and indexing[MeSH Terms]) OR “instrument” OR “indicator” OR “diet quality index” OR “diet quality indices”). A similar expression was used for the other 2 databases. Keywords were identified through the existing knowledge of the research team.
Eligibility criteria
Supplemental Table 1 presents the eligibility criteria used to identify studies of interest. In addition, only articles written in English and Portuguese and published since 2010 were included in the systematic review. Specifically in the Medline database, it was possible to search expressions in the abstract. No study design was imposed on the search. However, reviews, abstracts-only, case studies of 1 individual, books, and conference papers were not included. It is important to note that for the inclusion criteria 2 options were considered regarding the inclusion of instruments. At first, only instruments with evidence of being both healthy and sustainable, for example regarding their environmental impact through their association with the ecological footprint or water footprint, were deemed to be targeted. However, owing to the impossibility of fulfilling this criterion (because none of the instruments accomplished the sustainability criterion), this review ultimately considered all healthy instruments for use in those 2–17 y old, indicating that there is no evidence of sustainable instruments to assess dietary patterns in children and adolescents.
After the definition of the exclusion and inclusion criteria, all the references of the selected articles were checked in order to find more relevant information, using the snowballing technique procedure (28).
Study selection and data extraction
Two independent reviewers applied the eligibility criteria and selected the studies of interest for inclusion in this systematic review firstly by reading the titles and the respective abstracts. The other members of the research team confirmed the process. Two reviewers extracted the data and the others checked. Reviewers screened the full-text reports and decided whether these met the inclusion criteria. A third reviewer participated when disagreement in the selection of studies occurred. The reasons for excluding studies were reported in the PRISMA fluxogram (Figure 1). Neither the reviewers nor the other authors were blinded to the journal titles or to the study authors. All the necessary information to answer the study objectives had already been published within the articles, so no additional contact with authors was needed. After a full-text reading, a study was included in this review if it could answer ≥1 of the proposed objectives, despite having no data to answer the other ones. This means that an article was included if it had information on 1) instrument structure and characteristics of a healthy and/or sustainable dietary pattern or 2) population adherence level to the dietary pattern or 3) health-related outcomes.
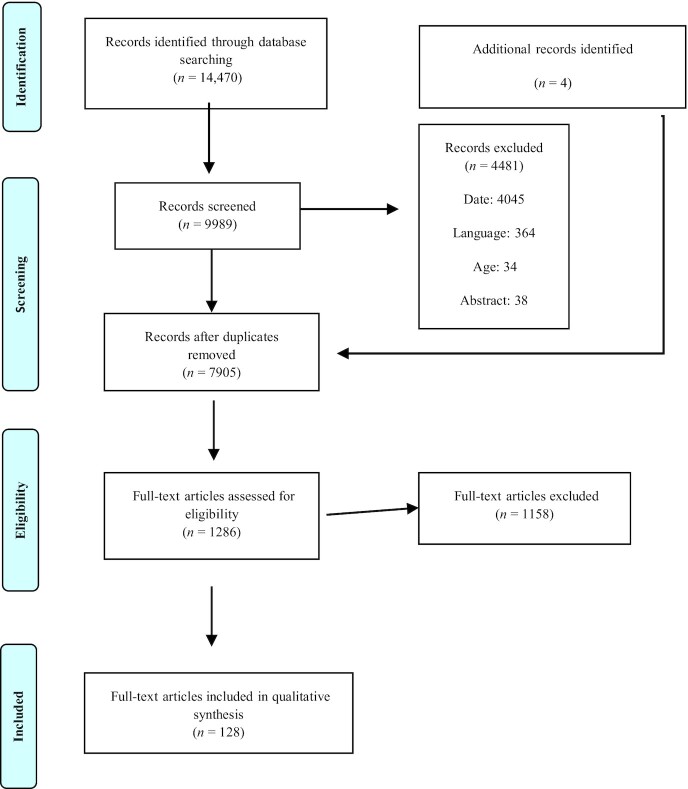
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) fluxogram.
Two tables were designed to summarize the eligible studies. Table 1 describes the adherence level to the different healthy and/or sustainable dietary patterns and the respective health-related outcomes. Table 2 presents all the instruments included in this systematic review and their respective and detailed methodology.
TABLE 1.
Characteristics of the studies included, evaluating the adherence to healthy and/or sustainable dietary patterns and associated outcomes in children and adolescents1
| Instrument | Authors (reference) | Country | Study design | Sample size, age, and sex | Adherence level | Health outcomes associated with adherence level | Quality assessment score |
|---|---|---|---|---|---|---|---|
| KIDMED | Bonaccorsi et al. (85) | Italy | Cross-sectional study | n = 3146 14 y old 47.8% males | Score range: −4 to 12. Mean ± SD: 5.91 ± 2.40.High adherence: 24.8%.Medium adherence: 56.4%.Poor adherence: 18.8% | Less adherence to the KIDMED was related to preobesity and obesity. | 62 |
| Grassi et al. (127) | Italy | Cross-sectional study | n = 2826 8 y old 55.7% males | Score range: −4 to 12.Mean ± SD: 4.93 ± 2.30.High adherence: 13.5%.Medium adherence: 59.6%.Poor adherence: 27% | — | 32 | |
| Ríos-Hernández et al. (117) | Spain | Case–control study | n = 1306 16 y old 56.7% males | Score range: −4 to 12.ADHD cases:Mean ± SD: 6.2 ± 2.0.High adherence: 30%.Medium adherence: 58.3%.Poor adherence: 11.7%.Control cases:Mean ± SD: 8.1 ± 1.8.High adherence: 63.3%.Medium adherence: 36.7%.Poor adherence: 0.0% | Lower adherence to the KIDMED index was associated with ADHD diagnosis. | 63 | |
| Rosi et al. (128) | Italy | Cross-sectional study | n = 40911 14 y old 54% males | Score range: −4 to 12.Mean ± SD: 6.0 ± 2.3.High adherence: 12%.Medium adherence: 60%.Poor adherence: 28% | — | 52 | |
| Ojeda-Rodríguez et al. (74) | Spain | RCT 2 months follow-up | n = 1077 16 y old 37% males | Score range: −4 to 12.Mean ± SD at baseline: 5.2 ± 1.8 (usual care group); 7.2 ± 1.6 (intensive care group).Mean (95% CI) changes within group after 8 wk: 2.0 (0.9, 3.0) (usual care group); 3.0 (2.5, 3.5) (intensive care group) | — | High risk of bias4 | |
| Grao-Cruces et al. (129) | Spain | Cross-sectional study | n = 180812 16 y old 51.3% males | Score range: −4 to 12.Mean ± SD: 6.44 ± 2.38 (male); 5.95 ± 2.42 (female) | — | 72 | |
| Yüksel et al. (56) | Turkey | Cross-sectional study | n = 85915 9 ± 1.3 y old 81.4% male | High adherence: 13%.Medium adherence: 54.6%.Poor adherence: 32.4% | There was no statistically significant relation between adherence to the KIDMED index and obesity and Night Eating Syndrome.5 | 42 | |
| Arriscado et al. (97) | Spain | Cross-sectional study | n = 32111 12 y old 50.8% male | Score range: −4 to 12.Mean ± SD: 7.2 ± 1.9.High adherence: 46.8%.Medium adherence: 48.6%.Poor adherence: 4.7% | There was no statistically significant relation between KIDMED index and BMI.5 | 42 | |
| Gómez et al. (70) | Spain | RCT 15 months follow-up | n = 22508 10 y old 48.2% male | Score range: −4 to 12.Mean ± SD at baseline: 6.7 ± 2.5 (intervention); 7.0 ± 2.3 (control).Mean ± SD at follow-up: 6.7 ± 2.4 (intervention); 6.6 ± 2.4 (control) | Promoting adherence to the KIDMED index had no significant effect on the BMI z score, and incidence of general and abdominal obesity. | High risk of bias4 | |
| Muros et al. (73) | Chile | Cross-sectional study | n = 51510 6 ± 0.5 y old 50.5% male | Score range: −4 to 12.Mean ± SD: 6.1 ± 2.5.High adherence: 22.9%.Medium adherence: 67.6%.Poor adherence: 9.5% | Adherence to the KIDMED index was consistently and negatively associated with BMI, percentage of body fat, subscapular skinfold thickness, and WC.5 | 52 | |
| Monjardino et al. (55) | Portugal | Cohort study 4 y follow-up | n = 1023 13 and 17 y old (KIDMED adherence at age 13 y and association with bone mineral density at age 17 y) 46.3% male | Score range: −4 to 12.Mean ± SD at 13 y: 5.2 ± 2.0 (male); 5.1 ± 2.1 (female) | Only among 13-y-old males, KIDMED index was significantly associated with higher bone mineral density at 17 y. No associations were found in relation to BMI at both ages. | 76 | |
| Rosi et al. (76) | Italy | Cross-sectional study | n = 6909 11 y old 48.3% males | Mean ± SD: 6.5 ± 2.2High adherence: 35.5%.Medium adherence: 55.2%.Poor adherence: 9.3% | No evidence was found of an association between the KIDMED index and BMI.5 | 52 | |
| Grigoropoulou et al. (116) | Greece | Cross-sectional study | n = 112510 12 y old 47% males | Score range: −4 to 12.Mean ± SD: 4.7 ± 1.9 (urban areas); 5.3 ± 2.0 (rural areas) | A 1-unit increase in the KIDMED index was associated with 16% lower likelihood of having asthma symptoms. | 62 | |
| Torres-Luque et al. (130) | Spain | Cross-sectional study | n = 3633 5 y old 54% males | Male:High adherence: 51.3%.Medium adherence: 48.7%.Poor adherence: 0.0%.Female:High adherence: 44.8%.Medium adherence: 50.0%.Poor adherence: 5.2% | — | 42 | |
| Korkmaz and Kabaran (86) | Turkey | Cross-sectional study | n = 9006 9 y old 60.5% males | Score range: −4 to 12.Mean ± SD: 5.0 ± 2.45.High adherence: 18.7%.Medium adherence: 45.7%.Poor adherence: 35.7% | An inverse correlation was found between KIDMED index and body weight, BMI, and waist and neck circumferences.5 | 72 | |
| Obradovic Salcin et al. (131) | Croatia | Cross-sectional study | n = 2605 6 y old 51.5% males | High adherence: 70.0%.Medium adherence: 24.0%.Poor adherence: 6.0% | — | 72 | |
| Bacopoulou et al. (50) | Greece | Cross-sectional study | n = 161012 17 y old 41.7% males | Score range: −4 to 12.Mean ± SD: 5.6 ± 2.4 (baseline); 5.8 ± 2.4 (follow-up) | Waist of circumference decreased as the KIDMED score increased.5 | 72 | |
| Mistretta et al. (87) | Italy | Cross-sectional study | n = 164311 16 y old 53.9% males | Score range: −4 to 12.Mean ± SD: 4.3 ± 2.1.High adherence: 9.1%.Medium adherence: 61.0%.Poor adherence: 29.9% | An inverse correlation was found between the KIDMED index and BMI, WC, and fat mass. No relation with blood pressure was found. | 62 | |
| Magriplis et al. (75) | Greece | Cross-sectional study | n = 45810 12 y old 49% males | Score range: −4 to 12.Mean ± SD: 3.78 ± 2.20 | — | 72 | |
| Calmeiro and Pereira (132) | Portugal | Cross-sectional study | n = 7827 9 ± 1.4 y old 51.8% males | Score range: −4 to 12.Mean ± SD: 5.88 ± 2.23 | — | 62 | |
| López-Gil et al. (88) | Spain | Cross-sectional study | n = 3706 13 y old 55.1% males | Score range: −4 to 12.Mean ± SD: 6.1 ± 2.1 (male); 6.3 ± 2.0 (female) | KIDMED < 3.8: positive association with adiposity. KIDMED > 9.3: negative association with adiposity | 62 | |
| Garcia-Hermoso et al. (115) | Colombia | Cross-sectional study | n = 11408 12 y old69.6% males | Score range: −4 to 12.Mean ± SD: 6.42 ± 0.12 (male); 6.39 ± 0.16 (female) | Adherence to the KIDMED index was negatively associated with systolic and diastolic arterial pressure.5 | 62 | |
| Grosso et al. (89) | Italy | Cross-sectional study | n = 113513 16 y old 45% males | Score range: −4 to 12.Mean ± SD: 4.9 ± 2.3 (male); 5.0 ± 2.1 (female) | Lower adherence to the KIDMED index was associated with being obese. | 72 | |
| López-Gil et al. (133) | Spain | Cross-sectional study | n = 3706 13 y old 55.1% males | High adherence: 25.9%.Medium adherence: 65.1%.Poor adherence: 8.9% | — | 72 | |
| Archero et al. (98) | Italy | Cross-sectional study | n = 6696 16 y old 48.4% males | High adherence: 19.6%.Medium adherence: 63.7%.Poor adherence: 16.7% | KIDMED score was positively associated with height. Adherence to the KIDMED index was not associated with the risk of overweight/obesity. | 72 | |
| Esteban-Cornejo et al. (134) | Spain | Cross-sectional study | n = 137112.0 ± 2.5 y old 50% males | Score range: −4 to 12.Mean ± SD: 6.66 ± 2.29.High adherence: 37%.Medium adherence: 55%.Poor adherence: 8% | — | 62 | |
| Mazaraki et al. (51) | Greece | Cross-sectional study | n = 36512 17 y old 58% males | High adherence: 6.8%.Medium adherence: 51.2%.Poor adherence: 42% | Adherence to the KIDMED index was positively related to BMI, WC, and systolic blood pressure and negatively associated with albuminuria.5 | 62 | |
| Costarelli et al. (36) | Greece | Cross-sectional study | n = 3962 12 y old 47.5% males | Score range: −4 to 12.Mean ± SD: 6.54 ± 2.44.High adherence: 34.8%.Medium adherence: 56.5%.Poor adherence: 8.6% | — | 72 | |
| Marques et al. (77) | Portugal | Cross-sectional study | n = 8919 11 y old 51% males | High adherence: 77.6%.Medium adherence: 13.7%.Poor adherence: 0.4% | — | 52 | |
| Roccaldo et al. (99) | Italy | Cross-sectional study | n = 17408 9 y old 51.7% males | High adherence: 5%.Medium adherence: 62.5%.Poor adherence: 32.8% | The KIDMED index did not differ significantly according to BMI. 5 | 52 | |
| Chacón-Cuberos et al. (135) | Spain | Cross-sectional study | n = 105914 16 y old 49.4% males | High adherence: 76.8%.Medium adherence: 22.7%.Poor adherence: 0.6% | — | 62 | |
| Azekour et al. (100) | Morocco | Cross-sectional study | n = 36849 8 ± 2.1 y old 48.7% males | High adherence: 40%.Medium adherence: 57.9%.Poor adherence: 2.1% | No relation was found between the KIDMED index and BMI. | 72 | |
| Martin-Calvo et al. (71) | Spain | Cohort study 2–3 y of follow-up | n = 10,9188 15 y old 45% males | At baseline:High adherence: 0.8%.Medium adherence: 17.8%.Poor adherence: 81.4%.Follow-up: 2-point increase in the score. | A 2-point increase in the KIDMED index was negatively associated with BMI. | 66 | |
| Bawaked et al. (72) | Spain | Cohort study 15 months follow-up | n = 16398 10 y old 51.8% males | Score range: −4 to 12.At baseline:Mean ± SD: 6.8 ± 2.4.High adherence: 40.4%.Medium adherence: 50.0%.Poor adherence: 9.6% | — | 66 | |
| Labayen Goñi et al. (101) | Spain | Cross-sectional study | n = 6194 7 ± 0.8 y old 51.4% males | High adherence: 62% | Higher KIDMED index was significantly related to lower WC.No significant association was observed between KIDMED index and BMI. | 62 | |
| Sahingoz and Sanlier (136) | Turkey | Cross-sectional study | n = 89010 14 y old 52.1% males | High adherence: 22.9%.Medium adherence: 59.2%.Poor adherence: 17.9% | — | 52 | |
| del Mar Bibiloni et al. (52) | Spain | Cross-sectional study | n = 123112 17 y old 43.4% males | High adherence: 28.4%.Medium adherence: 55.9%.Poor adherence: 15.7% | — | 72 | |
| Zervaki et al. (57) | Greece | Cross-sectional study | n = 40014 17 y old 49.5% males | Score range: −4 to 13.Mean ± SD: 5.1 ± 1.8 | — | 52 | |
| Krece Plus test | Delgado Floody et al. (137) | Chile | Cross-sectional study | n = 634Female: 11.9 ± 0.8 y old Male: 12.0 ± 0.9 y old 55.5% males | High adherence: 35%.Medium adherence: 47.5%.Poor adherence: 15.9% | — | 62 |
| MDS | Arouca et al. (58) | European countries (Austria, Belgium, France, Germany, Greece Hungary, Italy, Spain, and Sweden) | Cross-sectional study | n = 56213 17 y old 46.8% males | Score range: 0–8.Mean ± SD: 4.15 ± 1.45 | Greater adherence to the MDS was associated with lower blood C-reactive protein concentrations. | 62 |
| Winpenny et al. (54) | United Kingdom | Cohort study 3 y follow-up | n = 60314 and 17 y old 40% males | Score range: 0–8.Mean ± SD at 14 y: 4.88 ± 1.78 | The MDS was not associated with depressive symptoms. | 76 | |
| Martínez et al. (53) | Spain | Cross-sectional study | n = 1231 12–17 y old 56.9% males | Low adherence: 44.1% (% of adherence below the lower quartile).High adherence: 5.4% (% of adherence above the upper quartile). | — | 72 | |
| Jennings et al. (78) | England | Cross-sectional study | n = 17009 10 y old 43.8% males | Score range: 0–8.Mean ± SD: 4.1 ± 1.6. | The MDS was not associated with BMI, WC, and waist-to-height ratio. | 52 | |
| Rivas et al. (68) | Spain | Cross-sectional study | n = 1326 8 y old43% males | Score range: 1–13.Mean: 8.24. | — | 42 | |
| fMDS | Tognon et al. (37) | European countries (Sweden, Germany, Hungary, Italy, Cyprus, Spain, Belgium, and Estonia) | Cohort study 2 y follow-up | n = 16,2202 9 y old 50.9% males | fMDS>3:Sweden: 56.7%.Italy: 37.5%.Germany: 35.1%.Spain: 31.8%.Hungary: 32.2%.Belgium: 32.7%.Estonia: 26.3%.Cyprus: 24.2% | In a pooled analysis, higher scores of the fMDS were inversely associated with overweight, obesity, and percentage of fat mass | 76 |
| Mediterranean Adequacy Index (MAI) | Pastor et al. (138) | Spain | Cross-sectional study | n = 1306 12 y old 53% males | Score ≥ 0.Mean ± SD: 0.87 ± 0.4666 | — | 72 |
| Italian Mediterranean Index (IMI) | Zani et al. (139) | Italy | Cross-sectional study | n = 11646 8 y old 50.8% males | High adherence: 10.9%.Medium adherence: 30.1%.Poor adherence: 59% | — | 42 |
| Mediterranean-Style Dietary Pattern Score (MSDPS) | Neshatbini Tehrani et al. (49) | Iran | Cross-sectional study | n = 29716.1 ± 0.9 y old 100% females | Score: 0–100.Median [IQR]: 15.2 [11.9–19.5].High adherence: 51.2%.Low adherence: 48.8% | — | 72 |
| DQI-I adapted to Mediterranean Diet | Mariscal-Arcas et al. (69) | Spain | Cross-sectional study | n = 31908 15 y old 49.4% males | Score range: 0–100.Mean ± SD: 58.37 ± 7.74 | — | 52 |
| Silva et al. (66) | Portugal | Cross-sectional study | n = 66910 17 y old 50% males | Score range: 0–100.Mean ± SD: 49.7 ± 7.0 | — | 52 | |
| BSDS | Eloranta et al. (81) | Finland | Cross-sectional study | n = 4026 8 y old 50.7% males | Score range: 0–25.Mean ± SD: 11.5 ± 4.4 (male); 12.0 ± 4.3 (female). | BSDS was not associated with cardiometabolic risk. Higher BSDS score was associated with lower concentration of plasma HDL cholesterol in females. | 52 |
| SEAD score | Moreira et al. (47) | Portugal | Cross-sectional study | n = 46816.5 ± 0.9 y old 41.7% males | High adherence: 57.1%.Low adherence: 42.9% | Low adherence to the SEAD was associated with higher values of a metabolic risk score. Fit adolescents with high adherence to the SEAD showed the lowest prevalence of high metabolic risk score | 52 |
| Agostinis-Sobrinho et al. (113) | Portugal | Cross-sectional study | n = 437 Mean: 16.5 y old 41.1% males | Score range: 0–8.Mean ± SD: 4.74 ± 1.88 | Adolescents with low adherence to the SEAD had the highest odds of having a high cardiometabolic risk score. | 72 | |
| Diet Score based on the Norwegian Health Directorate | Handeland et al. (140) | Norway | Cross-sectional study | n = 47214 15 y old 47.5% males | High adherence: 24.8%.Medium adherence: 47.9%.Poor adherence: 26.9% | — | 62 |
| HuSKY | Truthmann et al. (46) | Germany | Cross-sectional study | n = 519812 17 y old 50.9% males | Score range: 0–100.Mean: 53.1 | A negative association was found between the HuSKY and homocysteine concentrations. | 72 |
| Egmond-Fröhlich et al. (62) | Germany | Cross-sectional study | n = 11,6766 17 y old No information on sex % | Score range: 0–100.Mean ± SD: 55.0 ± 11.0 | The HuSKY score had a negative association with ADHD symptoms. | 72 | |
| Diet Quality Index for Children | Huybrechts et al. (141) | Belgium | Cross-sectional study | n = 1692 5–6.5 y old No information on sex % | Score range: −25 to 100.Mean ± SD: 72.0 ± 11.0 | — | 52 |
| DQI-A | Vyncke et al. (41) | European countries (Austria, Belgium, France, Germany, Greece, Italy, Spain, and Sweden) | Cross-sectional study | n = 180712.5–17.5 y old 47.4% males | Score range: 0–100.Mean ± SD: 49.0 ± 17.0 (male); 53.3 ± 15.9 (female) | — | 72 |
| DQI-A adapted to Brazil | Ronca et al. (65) | Brazil | Cross-sectional study | n = 71,533 12–17 y old 50.2% males | Score range: −33 to 100.Mean ± SD: 19.0% ± 6.3% (male); 14.8% ± 6.1% (female) | — | 72 |
| Dietary Quality Score for Ireland | Keane et al. (142) | Ireland | Cross-sectional study | n = 85619 y old 51.2% males | Score range: −5 to 25.Mean ± SD: 9.4 ± 4.2 | — | 72 |
| CIDQ | Röytiö et al. (40) | Finland | Cohort study, cross-sectional analysis | n = 4002 6 y old 48% males | High adherence: 19.8%.Medium adherence: 58.0%.Poor adherence: 22.2% | The CIDQ score was associated with lower total cholesterol concentrations.5 | 66 |
| SHEIA 2015 | Moraeus et al. (94) | Sweden | Cross-sectional study | n = 2905Mean 12 y old 44% males | High adherence: 30.0%.Medium adherence: 48.8%.Poor adherence: 24.4% | No association was found between the SHEIA 2015 and BMI. | 72 |
| RADDS | Moraeus et al. (94) | Sweden | Cross-sectional study | n = 2905Mean: 12 y old 44% males | High adherence: 17.9%.Medium adherence: 56.8%.Poor adherence: 25.3% | RADDS score was inversely associated with BMI | 72 |
| Finish Children Healthy Eating Index (FCHEI) | Eloranta et al. (143) | Finland | Cross-sectional study | n = 3676 8 y old 51.2% males | Score range: 5–40.Mean ± SD: 23.0 ± 7.0 | — | 72 |
| DASH | Robson et al. (80) | San Diego | Cross-sectional study | n = 6986 12 y old 49.3% males | Score range: 0–80.Mean ± SD: 43.4 ± 9.0 | — | 72 |
| Monjardino et al. (55) | Portugal | Cohort study 4 y follow-up | n = 1023 13 and 17 y old 46.3% males | Score range: 8–40.Mean ± SD: 23.7 ± 4.5 (male); 23.7 ± 4.5 (female) | No association was found between the DASH score and BMI and bone mineral density. | 76 | |
| Bricarello et al. (59) | Brazil | Cross-sectional study | n = 71,553 12–17 y old 44.5% males | Score range: 8–40.Mean: 15.7.Minimum: 5.4.Maximum: 34.5 | No associations were found between the DASH score and hypertension. | 72 | |
| Asghari et al. (60) | Iran | Cohort study 3.6 y follow-up | n = 425 10–17 y old 42% males | Score range: 8–40.Baseline mean ± SD: 24.1 ± 4.3 | High adherence to the DASH diet was associated with lower levels of metabolic syndrome, hypertension, high fasting plasma glucose, and abdominal obesity. | 56 | |
| Eloranta et al. (81) | Finland | Cross-sectional study | n = 4026 8 y old 50.7% males | Score range: 0–80.Mean ± SD: 20.3 ± 4.4 (male); 21.8 ± 4.2 (female) | High adherence to the DASH diet was associated with lower concentrations of serum insulin and triglyceride in males and a lower concentration of plasma HDL cholesterol in females. | 52 | |
| Rostami et al. (48) | Iran | Cross-sectional study | n = 488 12–17 y old No information on sex % | 20% was in the first quintile of adherence to the DASH diet. | High adherence to the DASH diet was associated with lower levels of insomnia. | 72 | |
| Najafi et al. (79) | Iran | Cross-sectional study | n = 4076 12 y old 47.4% males | 33.4%: lowest tertile.33.2%: highest tertile | A higher adherence (highest tertile) to the DASH score was significantly related to lower levels of systolic blood pressure. | 72 | |
| Pérez-Gimeno et al. (82) | Spain | Cross-sectional study | n = 6875 16 y old No information on sex % | Score range: 7–35.Males:Mean ± SD: 17.3 ± 4.7 (prepubertal); 17.8 ± 5.3 (pubertal).Females:Mean ± SD: 18.5 ± 5.1 (prepubertal); 19.4 ± 4.7 (pubertal) | — | 72 | |
| HLD Index | Manios et al. (114) | Greece | Cross-sectional study | n = 72910–12 y old No information on sex % | Score range: 0–40.Mean ± SD: 20.0 ± 4.4. | <3.16 points → 20.9% of participants were found to be insulin resistant. | 52 |
| Manios et al. (90) | Greece | Cross-sectional study | n = 2660 9–13 y old 50.6% males | Score range: 0–48.Mean ± SD: 17.12 ± 4.50. | A 1-unit increase in the HLD Index score was associated with 6% lower odds of obesity. | 72 | |
| PDL-Index | Manios et al. (38) | Greece | Cross-sectional study | n = 2287 2–5 y old 51.5% males | Score range: 0–44.Mean ± SD: 18.2 ± 4.8. | Participants in the third tertile of the PDL-Index were less likely to be overweight than those in the first tertile. | 52 |
| E-KINDEX | Lazarou et al. (92) | Greece | Cross-sectional study | n = 63410–13 y old No information on sex % | Score range: 1–87.Mean ± SD: 58.2 ± 7.8. | The highest E-KINDEX category (>60 points) was associated with 85% less likelihood of a child being obese or overweight and 86% less likelihood of having a WC >75th percentile.5 | 52 |
| HEI-1995 | Azadbakht et al. (84) | Iran | Cross-sectional study | n = 265 11–13 y old 100% females | Score range: 0–100.Mean ± SD: 63.90 ± 19.86. | HEI-1995 was not associated with BMI and blood pressure.5 | 62 |
| Drenowatz et al. (111) | USA | Cross-sectional study | n = 354Mean ± SD: 10.4 ± 0.4 y old 41.5% males | Score range: 0–100.Mean ± SD: 62.0 ± 8.9 | HEI-1995 was not associated with HDL cholesterol, blood pressure, and body fat. | 72 | |
| HEI-2005 | Loprinzi et al. (61) | USA | Cross-sectional study | n = 26296–17 y old No information on sex % | Score range: 0–100.Mean: 50.2 (children); 49.8 (adolescents) | A higher HEI-2005 score was associated with lower WC, C-reactive protein concentrations, and triglyceride concentrations. | 72 |
| Rydén and Hagfors (144) | Sweden | Cross-sectional study | n = 24944, 8, and 11 y old 51% males | Score range: 0–100.Mean ± SD: 59.99 ± 7.80 | — | 72 | |
| Torres et al. (145) | Puerto Rico | Cross-sectional study | n = 115012 y old 45.5% males | Score range: 0–100.Mean ± SD: 40.9 ± 0.9 | — | 72 | |
| He et al. (146) | Canada | Cross-sectional study | n = 81011–14 y old 49% males | Score range: 0–100.Mean ± SD: 39.1 ± 7.8 | — | 72 | |
| Burke et al. (147) | South Carolina | Cross-sectional study | n = 1719–15 y old 49.1% males | Score range: 0–100.Mean ± SD: 52.4 ± 0.85 | — | 62 | |
| HEI-2010 | Anderson Steeves et al. (148) | USA | Cross-sectional study | n = 2789–15 y old 47% males | Score range: 0–100.Mean ± SD: 55.5 ± 9.6 | — | 62 |
| Mellendick et al. (63) | USA | Cross-sectional study | n = 16316–17 y old 40% males | Score range: 0–100.Mean ± SD: 49.2 ± 12.0 | HEI-2010 had no association with BMI, WC, blood pressure, and lipid profile. | 72 | |
| Dave et al. (104) | USA | RCT 6 wk follow-up | n = 1209–12 y old 40.8% males | Score range: 0–100.Mean ± SD: 55.72 ± 1.98 (baseline intervention); 57.34 ± 1.79 (baseline control); 56.54 ± 1.99 (posttest cases); 53.74 ± 1.80 (posttest control) | No differences were found between the intervention group and the control group with regard to BMI after 6 wk of follow-up. | Low risk of bias4 | |
| Au et al. (149) | San Diego | Cross-sectional study | n = 3944 9.8 ± 0.7 y old 49.3% males | Score range: 0–100.Mean ± SD: 47.4 ± 11.9 | — | 72 | |
| Santiago-Torres et al. (150) | Spain | Cross-sectional study | n = 187 10–14 y old 47% males | Score range: 0–100.Mean ± SD: 59.4 ± 8.8 | — | 52 | |
| Arandia et al. (151) | Spain | Cross-sectional study | n = 14668–16 y old 50.7% males | Score range: 0–100.Mean: 53.8 | — | 72 | |
| Arcan et al. (152) | USA | RCT | n = 1608–12 y old 85% males | Score range: 0–100.Mean ± SD: 53.7 ± 11.3 | After the intervention, parents reported their children had half their plates filled with fruit and vegetables at dinner on average 2.7 times in the past week (although not related to the aims of this article). | High risk of bias4 | |
| Clennin et al. (83) | USA | Cross-sectional study | n = 828Mean ± SD: 10.6 ± 0.05 y old 45.3% males | Score range: 0–100.Mean ± SD: 30.1 ± 5.38 | — | 62 | |
| HEI-2010 adapted to Brazil | Horta et al. (153) | Brazil | Cross-sectional study | n = 1357 8–12 y old 51% males | Score range: 0–100.Mean: 51.8 | — | 72 |
| HEI-2010 adapted to Singapore Health Promotion Board | Brownlee et al. (105) | Malaysia | Cross-sectional study | n = 5616–12 y old 47.4% males | Score range: 0–100.Median (IQR) 65.4 (57.1; 73.0) | HEI had no association with BMI.5 | 42 |
| HEI-2015 | Hayuningtyas et al. (109) | Indonesia | Cross-sectional study | n = 85 3–5 y old 48.2% males | Score range: 0–100.Mean ± SD: 33.2 ± 8.3 | A 1-point increase in the HEI-2015 was associated with an increase in serum adiponectin. | 52 |
| Khan et al. (154) | USA | Cross-sectional study | n = 574 and 5 y old 59.6% males | Score range: 0–100.Mean ± SD: 54.2 ± 14.2 | — | 52 | |
| Hopkins et al. (155) | USA | Cohort study 4 months follow-up | n = 100 3–12 y old 53% males | Score range: 0–100.Mean ± SD: 46.51 ± 1.72 (baseline); 46.51 ± 1.27 (first phase); 51.13 ± 1.46 (second phase) | — | 66 | |
| YHEI | Gingras et al. (45) | USA | Cohort study 7.9 y follow-up | n = 10512 y old 50.3% males | Score range: 0–85.Mean ± SD: 55.4 ± 9.4 | — | 86 |
| Protudjer et al. (118) | Canada | Case–control study | n = 47612.6 ± 0.5 y old 56.7% males | Score range: 0–85.Median (IQR)33.85 (29.85; 38.12) | YHEI had no association with asthma. | 93 | |
| Diet Quality Index Canadian (DQI-C) | Jarman et al. (156) | Canada | Cross-sectional study | n = 12603 y old 52% males | Score range: 0–6.Mean ± SD: 3.69 ± 0.6 | — | 72 |
| Healthy Dietary Variety Index | Barros et al. (96) | Portugal | Cohort study | n = 3962 4 y old 51.5% males | Score range: 0–1.Mean ± SD: 0.78 ± 0.11 | The score was inversely related to BMI. | 86 |
| School Child Diet Index (ALES) | Molina et al. (157) | Brazil | Cross-sectional study | n = 12827–10 y old 42% males | Score range: −10 to 10.Mean ± SD: 4.3 ± 3.5.Low adherence/diet quality: 41% | — | 62 |
| Brazilian Healthy Eating Index Revised (BHEI-R) | Toffano et al. (158) | Brazil | Cross-sectional study | n = 1679–13 y old 47.3% males | Score range: 0–100.Median (IQR): 54.3 (31.0–81.0) | — | 52 |
| Wendpap et al. (110) | Brazil | Cross-sectional study | n = 1326 10–14 y old 50% males | Score range: 0–100.Median (IQR): 75.1 (74.8–75.5) | There was a positive association between the score and BMI.5 | 72 | |
| Prado et al. (159) | Brazil | Cross-sectional study | n = 2017–10 y old 43.5% males | Score range: 0–100.Mean ± SD: 62.4 ± 8.68 | — | 62 | |
| Recommended Food Score | Coelho et al. (103) | Brazil | Cross-sectional study | n = 6616–14 y old 52.2% males | Score range: 0–50.Mean ± SD: 16.00 ± 6.82.Low adherence: 77.2% (<80th percentile) | The score had no association with BMI. | 72 |
| Healthy Eating Index (Brazil) | Leal et al. (39) | Brazil | Cross-sectional study | n = 5562–5 y old 53.6% males | Score range: 0–100.Mean ± SD: 74.4 ± 0.4 | — | 62 |
| ACARFS | Marshall et al. (102) | Australia | Cross-sectional study | n = 69111.0 ± 1.1 y old 43.8% males | Score range: 0–73.Mean ± SD: 25 ± 13 | ACARFS was not related to BMI. | 72 |
| DGI-CA | Ping-Delfos et al. (64) | Australia | Cohort study 3 y follow-up | 14 y old n = 1419 51.4% males 17 y old n = 843 46.5% males | Score range: 0–100.Mean ± SD: 47.1 ± 10.4 (14 y); 47.7 ± 11.0 (17 y) | From baseline at 14 y to the follow-up at 17 y, DGI-CA was positively related to BMI and negatively related to waist-to-height ratio and triglyceride concentrations. No relation with blood pressure was found. | 86 |
| Golley et al. (123) | Australia | Cross-sectional study | n = 34164–16 y old No information on sex % | Score range: 0–100.Mean ± SD: 53.6 ± 0.4. | 8–11 y: There was no relation between the score and body mass and WC.4–10, 12–16 y: A positive relation was found between the score and BMI and WC. | 72 | |
| Prior derived Diet Quality Index | Lioret et al. (93) | Australia | Cohort study 3 y follow-up | n = 2165–12 y old 44% males | Score range: 0–100.Mean ± SD: 64.2 ± 10.3 (baseline); 59.7 ± 12.4 (posttest) | The score was inversely related to BMI only in children with overweight at baseline. | 86 |
| Australian Recommended Food Scores for Pre-Schoolers (ARFS-P) | Burrows et al. (160) | Australia | Cross-sectional study | n = 1462–5 y old 54% males | Score range: 0–73.Median (IQR)32.0 (22.9–42.0) | — | 62 |
| Revised Children's Diet Quality Index (RC-DQI) | Collins et al. (161) | Australia | RCT 3.5 y follow-up | n = 244 3.5 y old 50.4% males | Score range: 0–85.Mean ± SD: 62.8 ± 8.3 | — | High risk of bias4 |
| Dietary Index for a Child's Eating (DICE) | Delshad et al. (42) | New Zealand | Cross-sectional study | n = 65 2–8 y old 44.6% males | Score range: 0–100.Mean ± SD: 78.2 ± 11.5 | — | 42 |
| Modified version of Revised Children's Diet Quality Index (M-RCDQI) | Keshani et al. (162) | Iran | Cross-sectional study | n = 112413–15 y old 53.3% males | Score range: 0–90.Mean ± SD: 58.91 ± 8.58 | — | 72 |
| Diet Quality Index for Indian Children (DQIIC) | Chamoli et al. (163) | India | Cross-sectional study | n = 1007–9 y old 53% males | Unhealthy diet: 33%.Moderate diet quality: 41%.Healthy diet: 26% | — | 62 |
| Chinese's Children's Dietary Index (CCDI) | Zhang et al. (67) | China | Cross-sectional study | n = 20437–15 y old 51.6% males | Score range: 0–160.Mean ± SD: 88.9 ± 15.1 (adherence was positively associated with energy adjusted for diet cost) | — | 72 |
| Duan et al. (164) | China | Cohort study 4.2 y follow-up | n = 3983 Mean: 7 y old 56% males | Score range: 0–160.Male range: 56.2–136.3.Female range: 46.1–131.5 | — | 76 | |
| Japanese Food Guide Spinning Top Score (JFGST) | Shinsugi et al. (112) | Japan | Cross-sectional study | n = 110Mean ± SD: 4.8 ± 0.4 y old 51.6% males | Score range: 0–70.Mean ± SD: 55.7 ± 7.5 | There was no association between the score and waist-to-height ratio. | 72 |
| Malaysian Healthy Eating Index | Appannah et al. (106) | Malaysia | Cross-sectional study | n = 33713 y old 29% males | Score range: 0–100.Mean ± SD: 49.1 ± 14.5 | There was no association between the index and BMI, WC, or fasting blood glucose, cholesterol, and insulin concentrations. | 62 |
| Rezali et al. (165) | Malaysia | Cross-sectional study | n = 37613–16 y old 35.1% males | Score range: 0–100.Mean ± SD: 37.9 ± 9.1 | — | 72 | |
| OPLS | Papoutsakis et al. (91) | Greece | Cross-sectional study | n = 5145–11 y old No information on sex % | Score range: 0–18.Mean ± SD: 8.6 ± 2.9 (asthma cases); 9.3 ± 2.7 (control cases) | OPLS was negatively associated with BMI, WC, and hip circumference.A high OPLS was protective against diagnosed asthma. | 72 |
| HEI based on WHO guidelines | da Costa et al. (166) | Portugal | Cohort study 3 y follow-up | n = 50134 and 7 y old No information on sex % | Score range: 8–32.Mean ± SD: 21.4 ± 3.53 (4 y); 20.3 ± 3.36 (7 y) | — | 86 |
| DQI-I | Tur et al. (108) | Italy | Cross-sectional study | n = 164312.4 ± 0.4 y old 53.9% males | Score range: 0–100.Mean ± SD: 52.31 ± 8.89 | DQI-I was positively related to BMI. | 72 |
| Healthy Dietary Adherence Score | Arvidsson et al. (43) | European countries (Belgium, Cyprus, Estonia, Germany, Hungary, Italy, Spain, and Sweden) | Cohort study 2 y follow-up | n = 76752–9 y old 51% males | High adherence: 52% | — | 56 |
| DDS | Jiang et al. (167) | China | Cross-sectional study | n = 6973–7 y old 50.6% males | Score range: 0–9.Mean ± SD: 7.0 ± 1.3 | — | 62 |
| Mak et al. (168) | Philippines | Cross-sectional study | n = 64606–12 y old 48.5% males | Score range: 0–9.Mean ± SD: 4.1 ± 1.3 | — | 62 | |
| Bi et al. (169) | China | Cross-sectional study | n = 1328 3 or 5 y old 51.6% males | Score range: 0–9.Median (IQR)5.77 (5.70–5.83). | — | 72 | |
| Zhao et al. (107) | China | Cross-sectional study | n = 1694 3–12 y old 51.8% males | Score range: 0–9.Mean ± SD: 6.3 ± 1.6 | There was no relation between DDS and BMI.5 | 52 | |
| Miller et al. (170) | Nepal | Case–control study | n = 26955.9 ± 6.5 months 46.8% males | Score range: 0–48.Mean: 26 points | — | 83 | |
| Cabalda et al. (44) | Philippines | Cross-sectional study | n = 200 2–6 y old No information on sex % | Score range: 0–10.Mean ± SD: 6.12 ± 0.17 (with garden); 5.62 ± 0.17 (without garden) | — | 62 | |
| HDS | Shang et al. (95) | China | Cross-sectional study | n = 56766–13 y old 46.6% males | HDS ≥ 8: 5.3%.HDS ≤ 3: 15.2% | An HDS ≥ 8 was inversely related to BMI, blood pressure, mean arterial pressure, fasting glucose and insulin concentrations, and HOMA values compared with HDS ≤ 3. | 72 |
ACARFS, Australian Child and Adolescent Recommended Food Score; ADHD, attention deficit hyperactivity disorder; BSDS, Baltic Sea Diet Score; CIDQ, Children's Index of Diet Quality; DASH, Dietary Approaches to Stop Hypertension; DDS, Dietary Diversity Score; DGI-CA, Dietary Guideline Index for Children and Adolescents; DQI-A, Diet Quality Index for Adolescents; DQI-I, Diet Quality Index International; E-KINDEX, Electronic Kids Dietary Index; fMDS, food frequency–based Mediterranean Diet Score; HDS, Healthy Diet Score; HLD Index, Healthy Lifestyle–Diet Index; HuSKY, Healthy Nutrition Score for Kids and Youth; KIDMED, Mediterranean Diet Quality Index for Children and Adolescents; MDS, Mediterranean Diet Score; NOS, Newcastle-Ottawa Scale; OPLS, Obesity-Preventive Lifestyle Score; PDL-Index, Preschoolers Diet–Lifestyle Index; RADDS, Riskmaten Adolescents Diet Diversity Score; SEAD, Southern European Atlantic Diet; SHEIA, Swedish Healthy Eating Index for Adolescents; WC, waist circumference; YHEI, Youth Healthy Eating Index.
The NOS for cross-sectional studies (varying from 0 to 8 stars).
The NOS for case–control studies (varying from 0 to 9 stars).
Tool of the Cochrane Collaboration for randomized control trials (low, medium, or high risk of bias).
Associations with outcomes obtained only by correlations.
The NOS for cohort studies (varying from 0 to 9 stars).
TABLE 2.
Description of the instruments identified in the literature and detailed methodology for assessment of healthy and/or sustainable dietary patterns in children and adolescents1
| Instrument | Method for food assessment | Quantitative portions of food | Consumption frequency | Components in analysis | Scoring methods | Score penalty | Score range | Adherence level | References |
|---|---|---|---|---|---|---|---|---|---|
| Based on the principles of the MD | |||||||||
| Mediterranean Diet Quality Index for Children and Adolescents (KIDMED) | 16 items of “yes or no” questions | No | Yes | 1) Fruit, 2) vegetables, 3) fish/seafood, 4) fast-food restaurants, 5) pulses, 6) pasta/rice, 7) cereal products, 8) nuts, 9) olive oil, 10) breakfast, 11) dairy products for breakfast, 12) commercially baked goods or pastries for breakfast, 13) yogurts/cheese, 14) sweets/candies. | Positive answers to questions with a negative connotation with MD adherence (n = 4) are scored −1 point, whereas questions with a positive connotation (n = 12) are scored +1 point. | No | Sum of the components, ranging from −4 to 12. | High adherence: ≥8 points; medium adherence: 4–7 points; poor adherence: ≤3 points | (36, 50–52, 56, 57, 70–77, 85–89, 97–101, 115, 116, 127–136) |
| KIDMED adaptation | FFQ | No | Yes | Removal of the breakfast component. | 24-h dietary recall | 24-h dietary recall | −4 to 13 | Use of the 33rd percentile | (55) |
| Krece Plus test | 15 “yes or no” questions | No | Yes | 1) Olive oil, 2) having breakfast, 3) vegetables, 4) pasta/rice, 5) fish, 6) fruits, 7) cereals at breakfast, 8) yogurts/cheese, 9) nuts, 10) commercially baked goods or pastries for breakfast, 11) sweets/candies, 12) takeaway. | Each item has a score of +1 or −1, depending on whether or not one follows the principles of the MD. | No | Sum of the components, ranging from −15 to 15. | Low nutritional level: ≤5 points; moderate nutritional level: 6–8 points; high nutritional level: ≥9 points | (137) |
| MDS | FFQ, dietary records, or 24-h recalls | No | No | 1) Ratio of MUFAs to SFAs (mainly olive oil), 2) vegetables, 3) fruits and nuts, 4) fish, 5) cereals, 6) pulses, 7) meat and meat products, 8) dairy products, 9) alcohol. | Score of 0 or 1 using the sex-specific sample medians as cutoffs.1–6): < median: 0 points; ≥ median: 1 point.7–8): ≥ median: 0 points; < median: 1 point.9) 0 g: 1 point; >0 g: 0 points. | No | Sum of the components, ranging from 0 to 8. | Higher scores indicate greater adherence. Participants can be categorized into 2 groups: low (<4 points) and high (≥4 points) adherence. | (58) |
| MDS adaptation | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | Alcohol intake was removed. | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | (54) |
| 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | Dairy products are scored as a beneficial component. | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | (53, 78) | |
| 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | MDS is calculated as a continuous variable using standardized z scores. | 24-h dietary recall | Use of quartiles. | 24-h dietary recall | (53) | |
| Semiquantitative questionnaire applied by face-to-face interview | Yes | Yes | 1) Olive oil, 2) butter, margarine, or cream, 3) sweet or carbonated beverages, 4) commercial sweets or pastries, 5) preference of lean meat over red meat, 6) sofrito (sauce with tomato and onion, leek, or garlic simmered in olive oil). | According to the MD recommendations 1 or 0 points. | 24-h dietary recall | Sum of the components, 1–13. | Higher scores indicate greater adherence. | (68) | |
| fMDS | FFQ | No | No | 1) Vegetables and legumes, 2) fruit and nuts, 3) cereals, 4) fish, 5) dairy products, 6) meat products. | Score of 0 or 1 using the sex-specific medians as cutoffs.1–4): < median: 0 points; > median: 1 point.5–6): > median: 0 points; < median: 1 point. | No | Sum of the components, 0–6. | High adherence levels to the fMDS when fMDS > 3. | (37) |
| MAI | Three 24-h dietary recalls | No | No | 1) Bread, 2) whole cereals, 3) pulses, 4) potatoes, 5) vegetables, 6) fresh fruit, 7) nuts, 8) fish, 9) olive oil, 10) wine, 11) milk, 12) cheese, 13) meat, 14) eggs, 15) animal fats and seed oils, 16) sweetened beverages, 17) cakes and cookies, 18) sugar, 19) other dairies, 20) ready or prepared meals. | MAI is obtained by dividing the sum of the percentage of total energy from typical Mediterranean food groups (bread + whole cereals + pulses + potatoes + vegetables + fresh fruit + nuts + fish + olive oil + wine) by the sum of the percentage of total energy from nontypical Mediterranean food groups (milk + cheese + meat + eggs + animal fats and seed oils + sweetened beverages + cakes and cookies + sugar + other dairies + ready or prepared meals). | No | Score ≥ 0. | The higher the score, the greater the adherence to the MAI. | (138) |
| Italian Mediterranean Index (IMI) | FFQ | No | No | 1) Pasta, 2) vegetables, 3) fruit, 4) pulses, 5) olive oil, 6) fish, 7) sugar-sweetened beverages, 8) butter, 9) red meat, 10) potatoes. | 1–6) 3rd tertile: 1 point; all other intakes received 0 points.7–10) 1st tertile: 1 point; all other intakes received 0 points. | No | Sum of the components, 0–10. | MD adherence was classified as low (≤3), medium (4–5), and high (≥6). | (139) |
| MSDPS | FFQ | Yes | Yes | 1) Whole-grain cereals, 2) fruits, 3) vegetables, 4) dairy products, 5) fish/seafood, 6) poultry, 7) olives, legumes, and nuts, 8) potatoes and other starchy roots, 9) eggs, 10) sweets, 11) meat, 12) olive oil. | Based on daily/weekly recommendations presented by the food guide pyramid.Except for olive oil, other MSDPS components are scored continuously from 0 to 10.Exclusive olive oil intake has a score of 10, olive oil besides other vegetable oils scores 5, and no olive oil intake scores 0. | For participants with the number of consumed servings above recommendation, a penalty score was assigned. A 0 score was considered for those who had a negative total MSDPS because of the overconsumption penalty. | 0–100.Equation based on the total score of the MSDPS components dividing by 120, multiplying by 100%, and, finally, multiplying by the proportion of total energy intake in the MD pyramid. | MD adherence was classified as low (15) and high (≥15). | (49) |
| DQI-I adaptedto MD | FFQ | Yes | Yes | 1) Variety (overall food group variety; within-group variety for protein sources), 2) adequacy (vegetable group, fruit group, cereal group, fiber, protein, iron, calcium, vitamin C), 3) moderation (total fat, saturated fat, cholesterol, sodium, empty calorie foods), 4) overall balance (macronutrient ratio, fatty acid ratio). | According to the MD recommendations.Variety: 0–15 or 0–5 each itemAdequacy: 0–5 each itemModeration: 0–6 each itemOverall balance: 0–4 or 0–6 each item | No | Sum of the components, 0–100 points.Variety: 0–20 pointsAdequacy: 0–40 pointsModeration: 0–30 pointsOverall balance: 0–10 points | Higher scores indicate greater adherence. | (66, 69) |
| Based on European recommendations and/or applied in European countries | |||||||||
| BSDS | Food records | No | No | 1) Fruits and Nordic berries, 2) vegetables (including legumes and roots; potatoes excluded), 3) cereals, 4) low-fat milk, 5) fish (salmon, Baltic herring, and mackerel), 6) meat and processed meat products, 7) diet total fat, 8) ratio of PUFA:SFA. | Use of quartiles.(1)–(5) and (8): 1st quartile: 0; 4th quartile: 3.(6)–(7): 1st quartile: 3; 4th quartile: 0. | No | Sum of the components, 0–25. | Higher points indicate higher adherence to the BSDS. | (81) |
| Southern European Atlantic Diet (SEAD) score | FFQ | No | No | 1) Fresh fish (excluding cod), 2) cod, 3) red meat/meat products, 4) dairy products, 5) vegetables and legumes, 6) vegetables soup, 7) potatoes, 8) bread. | Each component is measured as grams per 1000 kcal per day. Score of 0 or 1 using the sex-specific medians as cutoffs: < = 0 points; ≥ = 1 point. | No | Sum of the components, 0–8 points. | Higher points indicate higher adherence. Split into 2 groups: low (≤4 points) and high (≥5 points). | (47, 113) |
| Diet Score based on the Norwegian Health Directorate | FFQ | No | Yes | 1) Fruit and vegetables, 2) fish, 3) lean meat and meat products, 4) low-fat dairy products, 5) sugar, 6) water, 7) physical activity, 8) whole products. | When the Norwegian Health Directorate recommendation is fulfilled, 1 point is given; when it is not, 0 points. | No | Sum of the components, 0–8. | Low (0–3 points), moderate (4–5 points), or high (6–8 points) adherence to the dietary recommendations. | (140) |
| HuSKY | FFQ | No | Yes | 1) Beverages, 2) fruit, 3) vegetables, 4) pasta, rice, potatoes, 5) bread/cereals, 6) dairy products, 7) eggs, 8) meat, 9) fish, 10) fats, 11) sweets/fatty snacks/sugar-rich soft drinks. | For most food groups an intake below the Optimized Mixed Diet for German Children and Adolescents recommendation is assessed proportionally (0–10). Only for meat, fats, and sweets/fatty snacks/sugar-rich soft drinks, 10 points are given when the intake is below or equal to the tolerable consumption. | When more than twice the recommended amount was consumed, points were proportionally subtracted from 100. For meat, fats, and sweets/fatty snacks/sugar-rich soft drinks points were proportionally subtracted from 100 if consumption exceeded the recommendations. | Single points were added together and standardized to a scale from 0 to 100 (HuSKY = Σscorex/number of scorex). | A higher score implies a better overall dietary quality. | (46, 62) |
| Diet Quality Index for Children | FFQ | Yes | Yes | Dietary 1) diversity, 2) quality, 3) equilibrium, and 4) moderation are evaluated by the main food groups:
|
The sum of the 4 scores dividing by 4. According to the Belgium Health Council. | No | −25 to 100 | A higher score implies a better overall dietary quality. | (141) |
| DQI-A | 24-h dietary recall | Yes | Yes | 1) Water, 2) bread and cereals, 3) grains and potatoes, 4) vegetables, 5) fruits, 6) milk products, 7) cheese, 8) meat, fish, eggs, and substitutes, 9) fats and oils. | According to the Belgium Health Council and WHO (0–9 for each component). | No | 0–100 | A higher score implies a better overall dietary quality. | (41) |
| DQI-A in Brazil adaptation | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | In relation to the DQI-A, addition of:
|
According to the Brazilian Ministry of Health. | 24-h dietary recall | −33% to 100% | 24-h dietary recall | (65) |
| Dietary Quality Score for Ireland | 20-item FFQ reported by parents | No | Yes | According to the Irish dietary guidelines, each food item was defined as “healthy” or “unhealthy.” Healthy items: 1) fresh fruit, 2) vegetables, 3) meat, 4) eggs, 5) bread, 6) cereals, 7) potatoes, 8) dairy products, and 9) water. Unhealthy items: 1) meat pie, 2) hot chips, 3) crisps, 4) biscuits, and 5) soft drinks. | For each component a score of 1 = one; 2 = more than one; 3 = not at all; 4 = don't know. For consumption of each healthy item, a value of 0 for not eaten at all, 1 for eaten 1 portion, and 2 for eaten more than once were assigned. Unhealthy items were given a value of −2 for eaten more than once, −1 for eaten once, and 0 for not eaten at all. | No | −5 to 25 | A higher score value implies a better overall dietary quality. | (142) |
| Children's Index of Diet Quality (CIDQ) | 7-d food records + original questionnaire | Yes | No | 1) Cereals and fiber, 2) SFA, 3) MUFA, 4) PUFA, 5) sucrose, 6) vegetables and fruits, 7) calcium. | According to the Nordic Nutrition recommendations | No | Standardized for 0–21 | Low adherence: 0–2 components fulfilled. Medium adherence: 3 or 4 components fulfilled. High adherence: ≥5 components fulfilled. | (40) |
| Swedish Healthy Eating Index for Adolescents 2015 (SHEIA2015) | 24-h dietary recall | Yes | No | 1) Vegetables, 2) pulses, 3) fruits, 4) fiber, 5) whole meal, 6) fish and shellfish, 7) PUFA, MUFA, and SFA, 8) red and processed meat, 9) added sugar. | According to the Nordic Nutrition recommendations. 0 or 1 for each component. | No | 0–9 | A higher score implies a better overall dietary quality. Use of tertiles for adherence. | (94) |
| Riskmaten Adolescents Diet Diversity Score (RADDS) | 24-h dietary recall | Yes | No | 1) Vegetables, 2) pulses, 3) fruits, 4) pasta, rice, grains, and bread, 5) red meat, 6) poultry, 7) eggs, 8) white fish, 9) oil fish, 10) shellfish, 11) dairy products. | Each component varies between 1 and 17 points; 1 point is given if consumption is <5 g and proportionally until the recommendation is reached (17 points). According to the Nordic Nutrition recommendations. | No | Standardized for 1–17 | A higher score value implies a better overall dietary quality. Use of tertiles. | (94) |
| Finnish Children Healthy Eating Index (FCHEI) | Food records | Yes | No | 1) Vegetables, 2) fruits and berries, 3) oils and vegetable oils, 4) fish and skimmed milk, 5) foods with high amounts of sugar. | Consumption is divided by energy intake and categorized according to its variation (deciles), according to the Finnish dietary guidelines for children. | No | 5–40 | A higher score implies a better overall dietary quality. | (143) |
| Based on US recommendations | |||||||||
| DASH score | FFQ, food records, or 24-h dietary recall | No | Yes | 1) Grains, 2) vegetables, 3) fruits, 4) dairy products, 5) nuts, seeds, legumes, 6) red and processed meat, 7) fats/oils, 8) sweets. | There is a maximum component score of 10 for each food group when intake meets recommendations, with lower intakes scored proportionately. Reverse scoring is used when lower intakes are favored. | No | Sum of the components, 0–80 | Higher scores indicate greater adherence. | (80, 81) |
| DASH score adaptation | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall |
|
Use of quintiles. (1) to (5): quintile 1 is assigned 1 point and quintile 5, 5 points. Other components: low intake was desired. | 24-h dietary recall | Sum of the components, 8–40 | Higher scores indicate greater adherence OR Use of centiles (tertiles, quartiles, quintiles). | (48, 55, 59, 60, 79) |
| 24-h dietary recall | 24-h dietary recall | 24-h dietary recall |
|
Use of quintiles | 24-h dietary recall | Sum of the components, 7–35 | 24-h dietary recall | (82) | |
| HLD Index | 24-h dietary recalls | No | Yes | 1) Fruits, 2) vegetables, 3) grains, 4) dairy products, 5) meat, 6) fish/seafood, 7) soft drinks, 8) sweets, 9) watch TV/play computer, 10) moderate to vigorous physical activity. | A 0–4 scoring system is used to assign the appropriate score to each index component according to the USDA recommendations. | No | Sum of the components, 0–40 | Tertiles could be considered (a) “unhealthy diet–lifestyle pattern” (first tertile); (b) “moderate healthy diet–lifestyle pattern” (second tertile); (c) a “healthy diet–lifestyle pattern” (third tertile). | (114) |
| HLD Index adaptation | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | Two components were added to the original HDL index: legumes and eggs. | 24-h dietary recall | 24-h dietary recall | Sum of the components, 0–48 | 24-h dietary recall | (90) |
| Preschoolers Diet–Lifestyle Index (PDL-Index) | 24-h dietary recall or food diaries | No | Yes | 1) Fruits, 2) vegetables, 3) total grains, 4) dairy products, 5) red meat, 6) white meat/legumes, 7) fish and seafood, 8) unsaturated fats, 9) sweets, 10) time spent watching TV/vídeo, 11) moderate-to-vigorous physical activity. | A 0–4 scoring system was used to assign the appropriate score to each index component according to USDA recommendations. | 24-h dietary recall | Sum of the components, 0–44 | Use of tertiles. | (38) |
| Electronic Kids Dietary Index (E-KINDEX) | FFQ and supplementary questions | No | Yes | 1) Bread, 2) cereals (excluding bread), 3) fruits and fruit juices, 4) vegetables, 5) legumes, 6) milk, 7) fish, seafood, 8) meats, 9) salted and smoked meat foods, 10) sweets and junk food, 11) soft drinks, 12) grilled foods, 13) fried foods, 14) breakfast, 15) fast food, 16) number of main meals and snacks, 17) frequency of school meals in the afternoon. | A 4-point scoring system (0–3 or the reverse) is used for most components of the index according to the 1990 USDA recommendations. | No | Sum of the components, 1–87 | Higher values indicate higher adherence. | (92) |
| HEI-1995 | FFQ | Yes | Yes | 1) Grains, 2) vegetables, 3) fruits, 4) milk, 5) meat, 6) total fat, 7) SFA, 8) cholesterol, 9) diet variety, 10) sodium. | Each component scores 0–10 points according to the Food Guide Pyramid (USDA) recommendations. | No | 0–100 | Higher values indicate higher adherence.>80: “good”; 51–80: “needs improvement”; ≤50: “poor”. | (84, 111) |
| HEI-2005 | 24-h dietary recall or 4-d food records | Yes | Yes | 1) Total fruit, 2) whole fruit, 3) total vegetables, 4) dark and orange vegetables and legumes, 5) total grain, 6) whole grain, 7) milk, 8) meat and beans, 9) oil, 10) saturated fats, 11) sodium, 12) calories from solid fats, alcoholic beverages, and added sugar. | Depending on the components, a score of 0–5, 0–10, or 0–20 points is given, according to the USDA recommendations.All components are calculated per 4184 kJ (1000 kcal). | No | 0–100 | Higher values indicate higher adherence.>80: “good”; 51–80: “needs improvement”; ≤50: “poor”. | (61, 144–147) |
| HEI-2010 | 24-h dietary recall | Yes | Yes | 1) Total fruits, 2) whole fruit, 3) total vegetables, 4) greens and beans, 5) whole grains, 6) dairy, 7) total protein foods, 8) seafood and plant proteins, 9) fatty acids, 10) refined grains, 11) sodium, 12) empty calories. | Each component can receive a score ranging from 0 to 20 points, depending on the assigned maximum point total according to the 2010 Dietary Guidelines for Americans.Each average intake is standardized to an intake per 1000 kcal. | 0 | 0–100 | Higher values indicate higher adherence.>80: “good”; 51–80: “needs improvement”; ≤50: “poor”. | (63, 83, 104, 148–152) |
| HEI-2010 adapted to Brazil adaptation | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | According to the Brazilian Ministry of Health recommendations. | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | (153) |
| HEI-2010 adapted for Singapore Health Promotion Board adaptation | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 1) Rice, 2) whole grains, 3) fruits, 4) vegetables, 5) meats and alternatives, 6) dairy products, 7) sodium, 8) energy and total fat, 9) saturated fat, 10) added sugar. | Each component is given 0–10 points according to the Singapore dietary recommendations. | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | (105) |
| HEI-2015 | 24-h dietary recall | Yes | Yes | 1) Total fruits, 2) whole fruits, 3) total vegetables, 4) greens and beans, 5) whole grains, 6) dairy, 7) total protein fruits, 8) seafood and plant proteins, 9) fatty acids, 10) refined grains, 11) sodium, 12) added sugar, 13) saturated fats. | Depending on the components, a score of 0–5 or 0–10 points is given, according to the 2015–2020 Dietary Guidelines for Americans recommendation.The amounts are adjusted per 1000 kcal. | No | 0–100 | Higher values indicate higher adherence. | (109, 154, 155) |
| Youth Healthy Eating Index (YHEI) | FFQ + questionnaire | No | Yes | 1) Whole grains, 2) vegetables, 3) fruits, 4) dairy, 5) meat ratio, 6) snack foods, 7) soda and drinks, 8) multivitaminic use, 9) margarine and butter, 10) fried foods outside home, 11) visible animal fat, 12) dinner with family, 13) fish. | Depending on the components, a score of 0–5 or 0–10 points is given, according to USDA recommendations. | No | 0–85 | Higher values indicate higher adherence. | (45, 118) |
| Diet Quality Index Canadian (DQI-C) | FFQ | Yes | Yes | 1) Vegetables and fruits, 2) grain, 3) milk and alternatives, 4) meat and alternatives, 5) candy and snacks, 6) sugar-sweetened beverages. | Each component is given a score of 0 or 1 according to the Canada's Food Guide recommendations. | No | 0–6 | Higher values indicate higher adherence.≤72: unhealthy diet; 73–77: moderate diet quality; ≥78: healthy diet. | (156) |
| Healthy Dietary Variety Index | FFQ | No | Yes | 1) Starchy food (including potatoes), 2) fruits, 3) vegetables, 4) meat, fish, and alternatives, 5) dairy foods. | Foods are allocated into 1 of the 5 groups according to similar composition.Within each group the contribution of a particular food is truncated at 33%. The recommended number of servings is multiplied by 33%.Considering the USDA recommendations. | No | 0–1 | Higher values indicate higher adherence. | (96) |
| Based on Brazilian recommendations | |||||||||
| School Child Diet Index (ALES) | FFQ | No | Yes | 1) Fruits, 2) vegetables, 3) beans, 4) milk, 5) candies, 6) soft drinks, 7) fried foods, 8) instant noodles, 9) hamburgers, 10) mayonnaise. | According to the recommendations of the Brazilian Ministry of Health.Scores of +1 or −1 to each food component. | No | −10 to 10 | Use of tertiles.<3, poor quality; 3–6, average quality; ≥6, good quality. | (157) |
| Brazilian Healthy Eating Index Revised (BHEI-R) | 24-h dietary recall | Yes | Yes | 1) Total grains, 2) whole grains, 3) total vegetables and legumes, 4) dark and yellow vegetables and legumes, 5) fruits, 6) meat, eggs, and legumes, 7) dairy, 8) oils, 9) saturated fat, 10) sodium, 11) calories from solid fat, alcohol, and added sugar. | Depending on the components, a score of 0–5, 0–10, or 0–20 points is given, according to the Brazilian recommendations. | No | 0–100 | Higher values indicate higher adherence. | (110, 158, 159) |
| Recommended Food Score | FFQ | No | Yes | 1) Vegetables, 2) fruits, 3) lean meat, 4) cereals, 5) dairy products. | Selection of 50 foods from 120 of the FFQ to compose the index groups. The score is calculated by adding 1 point for each food that complied with the recommendations of the Brazilian Ministry of Health. When the recommendation was not fulfilled, the component has 0 points. | No | 0–50 | Higher values indicate higher adherence.>80th percentile: high adherence; <80th percentile: low adherence. | (103) |
| Healthy Eating Index (Brazil) | FFQ | Yes | Yes | 1) Cereals, 2) vegetables, 3) fruits and fruit juices, 4) dairy products, 5) meat and eggs, 6) legumes, 7) oils and fats, 8) sugar, candies, chocolates, and snacks, 9) total fat, 10) saturated fat, 11) cholesterol, 12) sodium, 13) diet variety. | Each component is scored from 1 to 10 according to the recommendations of the Brazilian Ministry of Health. Components 1–8) contribute 50% of the total score and 9–13) the other 50%. | No | Standardized, 0–100 | Higher values indicate higher dietary quality.>80: “good”; 51–80: “needs improvement”; ≤50: “poor”. | (39) |
| Based on Oceania (Australia and New Zealand) recommendations | |||||||||
| Australian Childand Adolescent Recommended Food Score (ACARFS) | 70 questions | No | Yes | 1) Vegetables, 2) fruits, 3) protein food (meat and nonmeat protein), 4) cereals, 5) dairy products, 6) water, 7) spreads/sauce. | The maximum possible score for each component was determined by the number of suitable FFQ items.Score according to the Australian Guide to Healthy Eating | No | Sum of the components, 0–73 | Higher values indicate higher adherence. | (102) |
| Dietary Guideline Index for Children and Adolescents (DGI-CA) | 24-h dietary recalls, FFQ | No | Yes | 1) Variety, 2) fruits, 3) vegetables, 4) bread and cereals, 5) whole-grain cereals, 6) meat and alternatives, 7) dairy, 8) water, 9) extra foods (moderation of salt and sugar), 10) healthy fats (ex. olive oil, nuts). | Depending on the components, a score of 0–5, 0–10, or 0–20 points is given, according to the 2003 Australian Dietary Guidelines for Children and Adolescents. | No | 0–100 | Higher values indicate higher adherence. | (64, 123) |
| Prior derived Diet Quality Index adaptation | FFQ | 24-h dietary recall | 24-h dietary recall | Instead of 10) healthy fats, it includes a “Saturated fats” component. | Each component was scored from 1 to 10. | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | (93) |
| Australian Recommended Food Scores for Pre-Schoolers (ARFS-P) | FFQ for parents | No | Yes | 1) Vegetables, 2) fruits, 3) meat, 4) meat alternatives, 5) grains, 6) dairy products, 7) condiments. | According to the Australian Recommended Food Score.The component scores vary from 0 to the number of questions in that component, plus 1 more possible for vegetables, low-fat dairy, and whole grains. | No | 0–73 | Higher values indicate higher adherence. | (160) |
| Revised Children's Diet Quality Index (RC-DQI) | 24-h recall | Yes | Yes | 1) Total fat, 2) linoleic acid, 3) α-linolenic acid, 4) EPA and DHA, 5) iron, 6) total grains, 7) whole grains, 8) dairy, 9) fruits, 10) vegetables, 11) electronic media use and energy intake interaction. | Depending on the components, a score of 0–2.5, 0–5, or 0–10 points is given, according to the Nutrient Reference Values for Australia and New Zealand. | No | 0–85 | Higher values indicate higher adherence. | (161) |
| Dietary Index for a Child's Eating (DICE) | Original questionnaire to parents | No | Yes | 1) Fruits, 2) vegetables, 3) dairy products, 4) meat and alternatives, 5) bread, 6) cereals. | Each component was scored from 1 to 10 according to the New Zealand Ministry of Health Food and Nutrition Guidelines for 2–18 y. | No | 0–100 | Higher values indicate higher adherence. | (42) |
| Based on Asian recommendations | |||||||||
| Modified version of Revised Children's Diet Quality Index (M-RCDQI) | FFQ | Yes | No | 1) Added sugar, 2) total fat, 3) linoleic acid, 4) α-linolenic acid, 5) EPA and DHA, 6) total grains, 7) fiber, 8) fruits, 9) vegetables, 10) dairy, 11) salty snacks, 12) iron, 13) energy. | According to Iranian recommendations (children consuming within the recommended amounts receive full points, varying from 2.5 to 10 points depending on the component). | No | 0–90 | Higher values indicate higher adherence. | (162) |
| Diet Quality Index for Indian Children (DQIIC) | 21 questions | Yes | Yes | 1) Cereals, 2) pulses, 3) meat and meat products, 4) dairy, 5) vegetables, 6) fruits, 7) sugar, 8) roots and tubers, 9) empty calories foods, 10) frequency of breakfast consumption, 11) frequency of meal given in lunch box, 12) number of meals per day, 13) frequency of consumption of favorite meal, 14) eat out of home in the past 2 d, 15) dietary behavior regarding consumption of advertised foods, 16) consumption of home-food, 17) sodium, 18) total energy from fat. | Depending on the components, a score of 0–4, 0–6, 0–2, 0–10, or 0–8 points is given, according to the Dietary Guidelines for Indian Children. | No | Standardized, 0–90 | Higher values indicate higher adherence.≤72: unhealthy diet; 73–77: moderate diet quality; ≥78: healthy diet. | (163) |
| Chinese's Children's Dietary Index (CCDI) | 24-h dietary recall | Yes | Yes | 1) Grains, 2) vegetables, 3) fruits, 4) dairy products, 5) soybeans and soy products, 6) meat, 7) fish and shrimp, 8) eggs, 9) water, 10) sugar-sweetened beverages, 11) vitamin A, 12) fatty acids, 13) fiber, 14) dietary variety, 15) energy balance, 16) regularly eating breakfast or dinner with parents. | Each component was scored from 1 to 10 according to the Chinese healthy recommendations. | 0 | 0–160 | Higher values indicate higher adherence. | (67, 164) |
| Japanese FoodGuide Spinning Top Score (JFGST) | FFQ | Yes | Yes | 1) Grain dishes, 2) vegetable dishes, 3) fish and meat dishes, 4) milk, 5) fruits, 6) total energy, 7) snacks and beverages. | Each component was scored from 1 to 10 according to the 2000 Dietary Guidelines for Japanese. | No | 0–70 | Higher values indicate higher adherence.Use of tertiles. | (112) |
| Malaysian Healthy Eating Index | FFQ or 2-d dietary record | Yes | Yes | 1) Cereals and grains, 2) vegetables, 3) fruits, 4) dairy products, 5) poultry, meat, and eggs, 6) fish, 7) legumes, 8) energy from total fat, 9) sodium. | Each component was scored from 1 to 10 according to the Malaysian Dietary Guidelines for Children and Adolescents. | No | 0–100 (total score of 9 components/9 × 10) × 100% | Higher values indicate higher adherence.≤46: high risk of a poor dietary quality; ≥47: low risk of a poor dietary quality | (106, 165) |
| Based on the principles of international entities or others | |||||||||
| Obesity-Preventive Lifestyle Score (OPLS) | FFQ | No | Yes | 1) Fruits, 2) vegetables, 3) sugar-sweetened beverages, 4) breakfast, 5) restaurants/fast food, 6) screen time, 7) moderate/ intense physical activity, 8) school sport physical activity, 9) active commuting. | Tertiles and assigned ascending values (0, 1, 2) for favorable behaviors and descending values (2, 1, 0) for unfavorable behaviors. | No | Sum of the components, 0–18 | Higher values indicate healthier lifestyles. | (91) |
| HEI based on WHO recommendation | FFQ | No | Yes | 1) Fruits, 2) vegetables, 3) dairy products, 4) fish, 5) eggs, 6) meat and meat products, 7) salty snacks, 8) sweet foods and soft drinks. | Each food group is assigned 1–4 points.(1) to (5) components: 1st quartile: 1 point; 4th quartile: 4 points.(6) to (8) components: 1st quartile: 4 points; 4th quartile: 1 point. | No | 8–32 | Higher values indicate higher adherence.Use of quartiles. | .(166) |
| DQI-I | FFQ | Yes | Yes | 1) Variety (overall food group variety; within-group variety for protein sources), 2) adequacy (vegetables, fruits, grains, fiber, iron, protein, calcium, vitamin C), 3) moderation (total fat, saturated fat, cholesterol, sodium, empty calories food), 4) overall balance (macronutrient ratio, fatty acid ratio). | Depending on the components, a score of 0–10, 0–20, 0–30, or 0–40 points is given, according to the USDA Dietary Guidelines and 1996 WHO recommendations, | No | 0–100 | Higher values indicate higher adherence.<50: poor diet; 50–70: moderate diet quality; >70: high diet quality. | (108) |
| Healthy Dietary Adherence Score (HDAS) | FFQ | Yes | Yes | 1) Refined sugars, 2) fat intake, 3) whole meal, 4) fruits, 5) vegetables, 6) fish. | Each component was scored from 1 to 10 according to the guidelines common to all 8 countries participating in the study. | No | 0–50 | Higher values indicate higher adherence. | (43) |
| DDS | 24-h dietary recall | Yes | No | 1) Cereals, roots, and tubers, 2) vitamin A–rich fruits and vegetables, 3) other fruits and vegetables, 4) legumes, pulses, and nuts, 5) oils and fats, 6) dairy, 7) meat and fish, 8) eggs, 9) foods rich in sugar. | 0 or 1 point for each component according to the guidelines of the FAO. | No | 0–9 | Higher values indicate higher adherence. | (107, 167–169) |
| DDS adaptation | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 0–48 | 24-h dietary recall | (170) |
| DDS adaptation | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 24-h dietary recall | 0–10 | 24-h dietary recall | (44) |
| Healthy Diet Score (HDS) | 24-h recall or record diaries | No | No | 1) Refined grains, 2) seafood, 3) fried foods, 4) sugar-sweetened beverages, 5) meat, 6) rice, 7) fungi and algae, 8) roots and tubers, 9) wheat. | Computed by summing subscores with each of the leading dietary predictors as 1 point according to the association with cardiometabolic risk. Example: for ≥ median intake of fruit a score of 1 is given and 0 for < median, if fruit intake is inversely related to cardiometabolic risk. | No | 0–9 | Higher values indicate healthier lifestyles. | (45) |
BSDS, Baltic Sea Diet Score; DASH, Dietary Approaches to Stop Hypertension; DDS, Dietary Diversity Score; DQI-A, Diet Quality Index for Adolescents; DQI-I, Diet Quality Index International; FAO, Food and Agriculture Organization of the United Nations; fMDS, food frequency–based Mediterranean Diet Score; HEI, Healthy Eating Index; HLD Index, Healthy Lifestyle–Diet Index; HuSKY, Healthy Nutrition Score for Kids and Youth; MAI, Mediterranean Adequacy Index; MD, Mediterranean Diet; MDS, Mediterranean Diet Score; MSDPS, Mediterranean-Style Dietary Pattern Score.
The identified records were de-duplicated using Systematic Review Assistant-Deduplication (29) followed by a manual search in Endnote (30). A total of 1286 full-text studies were assessed for eligibility according to the inclusion criteria and 128 were included in the qualitative synthesis (Figure 1). In April 2021, the most recent articles from 2021 were assigned to “Additional records identified” (Figure 1), which data were important to include in this systematic review.
Quality assessment
The Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of all included cohort and case–control studies (31), with an overall quality score ranging from 0 to 9 stars. The adapted NOS for cross-sectional studies was also used in this review, ranging from 0 to 8 stars (32). This adapted version has been used to analyze the quality of previous systematic reviews (33, 34). In addition, the methodological quality and risk of biases of randomized control trials (RCTs) were assessed using the Cochrane Collaboration revised tool for assessing the quality and bias of RCTs (35). Any disagreements among reviewers were resolved by consensus.
Results
Figure 1 summarizes the selection procedure. We analyzed 128 final full-text articles, which are summarized in Tables 1 and 2 (105 cross-sectional studies, 15 cohort studies, 3 case–control studies, and 5 RCTs). As a whole, the studies involved 329,898 subjects with samples varying from 2 (36–45) to 17 y old (41, 46–66). Forty-two articles were published between 2010 and 2015 and 86 between 2016 and 2021. Regarding the geographical distribution, 70 studies were conducted in Europe, followed by America (29 studies), Asia (21 studies), Oceania (7 studies), and Africa (1 study). It is important to highlight that 50 of the articles were from Mediterranean countries, in which Spain stands out, as can be seen in Figure 2. Thirty-four and 47 articles provided data on the first (children) or the second decade of life (adolescents), respectively, and 47 presented data regarding both children and adolescents (Table 1).
FIGURE 2.
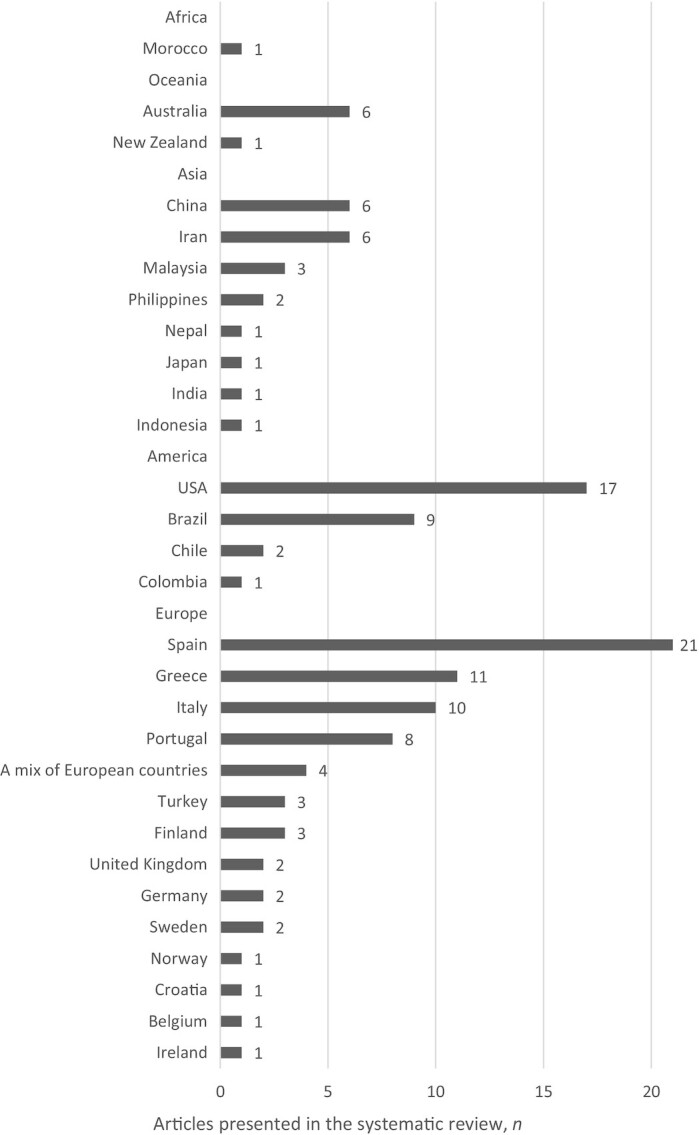
Geographical distribution of the studies included.
Regarding quality assessment, the mean ± SD quality score was 6.10 ± 1.01 (min: 3; max: 7) for the cross-sectional studies, 7.67 ± 1.53 (min: 5; max: 8) for the cohort studies, and 6.81 ± 1.08 (min: 6; max: 9) for the case–control studies. With respect to the RCTs, 1 study presented a low risk of bias and 3 articles a high risk of bias.
In this systematic review, 50 instruments plus 14 adaptations were identified, making a total of 64 instruments measuring adherence to healthy dietary patterns, which are presented in Table 1. It is important to consider that none of the instruments found proved to be assessing a sustainable dietary pattern, in relation to the environmental impact. Geographically, concerning the 50 instruments, this systematic review presents 12 instruments that are based on recommendations from European countries, 10 based on North American recommendations, 8 based on the principles of the MD, 6 based on international recommendations such as those of the FAO and WHO, 5 based on recommendations from Oceania (Australia, New Zealand), 5 based on recommendations from Asia, and 4 based on Brazilian recommendations. The healthy and/or sustainable dietary pattern most studied in children and adolescents was the MD, with 8 different instruments and 50 articles found in this systematic review. Within these instruments, the Mediterranean Diet Quality Index for Children and Adolescents (KIDMED) was the index most often used to assess the adherence of the pediatric population to this dietary pattern, with 38 full-text articles published. It should be noted that none of these instruments have presented objective data on their sustainability, for example through the analysis of their ecological or water footprint and emission of greenhouse gases. In fact, the Chinese Children Dietary Index presented a positive association between diet quality and energy-adjusted diet cost, the economic dimension being one of the pillars of sustainability (67). Table 2 presents all instruments and the respective detailed methodologies.
In general, these scores/indexes were defined based on previous application of a dietary intake assessment method: FFQs, food records, or 24-h dietary recalls (58 out of 65 instruments). However, some instruments such as the KIDMED had already a predefined list of “yes or no” questions to measure the adherence to the dietary pattern. More than half (53.1%; 34 out of 64 instruments) did not take into account quantitative data (e.g., portions, amounts) of the included components and 73.4% (47 out of 64 instruments) considered recommended food consumption frequencies. In Figure 3, it can be observed that the components that were present in at least half of the revised instruments were the following, in descending order: vegetables, fruit, dairy products, meat and meat products, cereal products, and fish. Revised instruments were based on national recommendations or principles of dietary patterns known a priori (e.g., MD, national and international recommendations). Only 2 instruments took into account the penalty for exceeding the recommended values (46, 49). For the scoring method, several methodologies were followed such as the determination of cutoffs or z scores. The instruments had very different boundaries and, in all of them, the higher the final score (usually the sum of all individual components’ scores), the greater the adherence to the dietary pattern. In addition, some instruments made use of percentiles (medians, quintiles, quartiles, or tertiles) or other specific cutoffs to determine the adherence level (e.g., low, moderate, high) (Table 2).
FIGURE 3.

Food components identified in at least half of the 50 instruments identified in the literature to measure the adherence to healthy and/or sustainable a priori dietary patterns.
Adherence to the a priori dietary patterns identified
In this systematic review it was found that the adherence to the MD in children and adolescents was measured by 8 different instruments plus 6 adaptations. Of these, only 3 took into account the recommended quantitative portions (49, 68, 69) (Table 2). Table 1 shows the results on MD adherence (as mean and/or categories of poor compared with high adherence) that were collected from the selected articles. The KIDMED index, ranging in general from −4 to 12 points, was used in 38 studies with participants ranging between 2 and 17 y old. Of these, 32 studies were cross-sectional, 5 were cohort studies (55, 70–73), and 1 was an RCT (74). Twelve studies expressed the results as mean values and categorical values; 12 studies stated the results only as mean ± SD values which varied from 3.78 ± 2.20 in Greek adolescents (75) to 7.2 ± 1.9 in Spanish adolescents (76). In 24 studies the distribution of the KIDMED score into categories (high, medium, and poor adherence) was reported. High adherence varied from 0.8% in Spanish individuals at baseline (71) to 77.6% in Portuguese individuals (77). The MDS, ranging in general from 0 to 8 points and used in 5 studies, varied in terms of mean scores from 4.1 in English participants 9–10 y of age (78) to 8.24 in Spanish children (68) (Table 1).
With participants ranging from 5 to 17 y of age, the Dietary Approaches to Stop Hypertension (DASH) score, ranging in general from 0 to 80 points, was used in 8 studies and often in Iran (48, 60, 79), 6 of which were cross-sectional (48, 59, 79–82) and 2 cohort studies (55, 60). Six studies expressed the results as mean ± SD values, which varied from 15.7 ± 50.0 in Brazilian adolescents (59) to 43.4 ± 49.0 in San Diego individuals 6–12 y of age (80). Most of these studies showed levels of adherence according to tertile (48, 55, 59, 60, 79, 81) or continuous scores (80–82). Regarding the Healthy Eating Index (HEI) from 1995 to 2015, ranging in general from 0 to 100 points, the mean ± SD adherence varied from 30.1 ± 5.38 in American adolescents (83) to 63.90 ± 19.86 in Iranian adolescents (84). In relation to the other instruments, it was not possible to make an analysis of adherence to each instrument because each had been applied in only a few studies. However, most of these instruments were applied in cross-sectional studies, in which the higher the score, the greater the level of adherence to the dietary pattern under study (Table 1).
Associations between the dietary patterns identified and the health-related outcomes
Relations with clinical outcomes were found in 62 articles. In most of them (40%), body fat, waist circumference (WC), blood pressure, and metabolic risk were negatively related with adherence to healthy and/or sustainable dietary patterns. Of these, 29 included only adolescents, whereas the rest contained children or children and adolescents. Fifteen only used crude correlations to describe the associations found.
Anthropometric/clinical factors
Seventeen studies showed a significant negative association between BMI and the following dietary patterns: the KIDMED index (71, 73, 85–89), the food frequency–based Mediterranean Diet Score (fMDS) (37), the DASH score (60), the Healthy Lifestyle–Diet Index (HLD Index) (90), the Preschoolers Diet–Lifestyle Index (PLD-Index) (38), the Obesity-Preventive Lifestyle Score (OPLS) (91), the Electronic Kids Dietary Index (E-KINDEX) (92), the Prior Derived Diet Quality Score (93), the Riskmaten Adolescents Diet Diversity Score (94), the Healthy Diet Score (HDS) (95), and the Healthy Dietary Variety Index (96). However, 20 studies found no significant relation of BMI with the KIDMED index (55, 56, 70, 76, 97–101), MDS (78), DASH diet (55), Australian Child and Adolescent Recommended Food Score (ACARFS) (102), Recommended Food Score (103), HEI-1995 (84), HEI-2010 (63, 104, 105), Malaysia Healthy Eating Index Score (106), Swedish Healthy Eating Index for Adolescents (94), and the Dietary Diversity Score (107). Finally, 5 articles described a positive association of BMI with the KIDMED index (51), Diet Quality Index International (DQI-I) (108), HEI-2015 (109), Brazilian Healthy Eating Index Revised (110), and Dietary Guideline Index for Children and Adolescents (64); within these articles, 4 were cross-sectional and 1 was a cohort study in which no adjustments were made for multiple comparisons (Table 1).
The KIDMED index was negatively related to body fat mass in 2 studies (73, 87), to WC in 5 studies (50, 73, 86, 87, 101), to subscapular skinfold thickness (73), and to neck circumference (86). The KIDMED index was positively related to height in 1 article (98), to WC in 1 article (51), and had no association with waist-to-height ratio (78). Fat mass was also negatively related with the fMDS (37), but it was not associated with the HEI-1995 (111). WC was also negatively related to the E-KINDEX (92), OPLS (91), and HEI-2005 (61). No association was found between the WC and the MDS (78), HEI-2010 (63), and Malaysia Healthy Eating Index Score (106). Hip circumference was negatively related to OPLS in 1 study (91). Waist-to-height ratio was negatively associated with the Japanese Food Guide Spinning Top Score (112), but did not have a significant relation with the Dietary Guideline Index for Children and Adolescents (64) (Table 1).
Cardiometabolic risk was negatively associated with the DASH score (60) and the SEAD (47, 113). On the other hand, the Baltic Sea Diet Score was not related to cardiometabolic risk (81). The DASH score, Baltic Sea Diet Score, and Children's Index of Diet Quality were associated with lower concentrations of blood cholesterol (40, 81), whereas the HEI-2005 (19) and Malaysia Healthy Eating Index Score (106) did not present any association. The HLD Index (114), DASH score (60, 81), and HDS (95) were suggested to be protective in relation to insulin resistance and, as such, to an adequate concentration of glucose and insulin in the blood, unlike the Malaysia Healthy Eating Index Score (106) which had no relation. The concentration of triglycerides was negatively associated with the HEI-2005 (61) and the Dietary Guideline Index for Children and Adolescents (64), despite not having any relation with the HEI-2010 (63). The KIDMED index and the Healthy Nutrition Score for Kids and Youth were negatively related to albuminuria (51) and homocysteine concentrations (46), respectively. Greater scores on the KIDMED index (58) and the HEI-2005 (61) were associated with a lower C-reactive protein blood concentration (Table 1).
Concerning blood pressure individually, a negative relation was reported with the DASH score in 2 articles (60, 79), KIDMED index in 1 article (115), and HDS in another 1 (95). However, no associations were found of blood pressure with the DASH score in 1 article (59), KIDMED index in 1 article (87), HEI-2010 (63), HEI-1995 (84, 111), and Dietary Guideline Index for Children and Adolescents (64). However, 1 article correlated positively the KIDMED index with blood pressure (article quality: 6 points) (51) (Table 1).
Regarding diagnosed disease occurrence, the KIDMED index was negatively associated with asthma (116) and attention deficit hyperactivity disorder (ADHD) (117) and positively with bone mineral density (55). Asthma was also negatively related to the OPLS (91) and had no relation with the Youth Healthy Eating Index (118). ADHD diagnosis was also negatively associated to the Healthy Nutrition Score for Kids and Youth (62). The DASH score did not present any association with bone mineral density (55), but it was negatively related to insomnia (48). Depression and Night Eating Syndrome had no association with the MDS (54) and the KIDMED index (56) (Table 1).
Discussion
In the present study, a systematic review was carried out, which, to our knowledge, is the first to combine the search for simultaneously healthy and sustainable a priori dietary patterns used in children and adolescents with the additional purpose of combining benefits and health outcomes associated with them. In this review, 50 instruments plus 14 adaptations were identified. In general, the articles included a high-quality average score, which is extremely important for the discussion of results.
The MD pattern is the dietary pattern most described in this systematic review (50 out of 128 articles), followed by the HEI-2010 (9 of 128) and the DASH diet (8 of 128). Among the instruments described for evaluating MD adherence among children/adolescents, the KIDMED index is the most used in Mediterranean countries, such as Spain, Italy, Greece, Portugal, and Turkey. The MDS is also used in non-Mediterranean countries (3 out of 5 articles). Geographically, adherence to the MD is studied in all the continents of the world, which highlights its global importance, being more studied over the last decade in the European and American continents. Some of the instruments described were developed specifically for children and adolescents as is the case of the KIDMED index (119), whereas others were modified from those used in adults (19, 120–122).
All of the dietary patterns identified are based on a priori criteria supported by scientific knowledge and differ between themselves with regard to the number of items, included components, cutoffs for scoring, and inclusion of quantitative food portions or food frequencies, which hampers straight comparisons between them. Most of them have in common the characteristics of a healthy and sustainable diet, stated by the EAT–Lancet Commission (5). However, none of these instruments has been proven to have sustainable characteristics, so instruments are only considered sustainable owing to their a priori classification in the literature or based on the inclusion of specific food groups that are known to have a lower ecological footprint, such as fruit and vegetables. The need to adhere to more sustainable diets is urgently growing. According to the EAT–Lancet Commission, these diets must have an adequate caloric intake and consist of consumption of a diversity of plant foods, low amounts of animal source foods, unsaturated fats instead of saturated fats, and small amounts of refined grains, highly processed foods, and added sugars (5). It is crucial to develop strategies for increasing adherence to healthy and sustainable dietary patterns all around the world. In fact, this transformation for 2050 will require a >50% reduction in global consumption of unhealthy foods, such as red meat and sugar, and a >100% increase in consumption of healthy foods, such as vegetables, fruit, nuts, and pulses (5). As such, it becomes relevant and essential to produce evidence that instruments that measure adherence to dietary patterns for children and adolescents are also sustainable, for example through associations of the dietary pattern represented with greenhouse gas emissions, land use, or a water footprint. Future research could produce a new instrument that sets at the same time a healthy and sustainable dietary pattern for children and adolescents.
Adherence to the dietary patterns identified
A narrative review suggested that MD adherence is poor in children and adolescents living in the Mediterranean countries (10). In this research, data on MD adherence were mainly provided by studies using the KIDMED index. MD adherence, in this study, even using the same index and concerning the same country, suffers great fluctuations, as already described in a systematic review (9). MD adherence cannot be directly compared across the different instruments identified. The pediatric population's adherence to the DASH score and the different instruments also vary widely in this review. According to our knowledge, this is the first time that adherence to other dietary patterns (beyond the MD) has been summarized in children and adolescents aged 2–17 y and, therefore, adherence data to be discussed are scarce.
There is no consensual and easy explanation for the wide variations in adherence to healthy and/or sustainable dietary patterns, even within the same country. These variations may be due to methodological constraints, namely different characteristics in terms of sample size, age range, percentage of males compared with females, method of food consumption assessment (questionnaire application, food diaries, FFQs, 24-h dietary recalls), the cutoffs used for scoring (based on different recommendations or different percentiles), and the study type (cross-sectional, cohort, case control, and RCT). Finally, the fact that most instruments are not adapted/validated for the countries in use makes adherence results found in the literature less reliable.
Health-related outcomes associated with the dietary patterns identified
Pediatric dietary patterns can predict adults’ diet-related disease (15) and it is known that unhealthy and unsustainable diets are related to noncommunicable diseases, including cardiovascular diseases, obesity, and diabetes, among adults (5). However, our article showed conflicting results: 17 articles showed a negative association between adherence to these dietary patterns and BMI, whereas 20 did not find any association and 5 reported a positive relation with children's BMI. These inconsistent associations have been previously described in a review regarding the MD in children and adolescents (9). Firstly, it should be underlined that, in this systematic review, 33 out of the 40 articles that studied BMI were cross-sectional, which makes less accurate the assessment of cause–effect associations. With respect to the 7 prospective studies which studied BMI, 5 of them reported a negative association (37, 60, 71, 93, 96). Secondly, different criteria for obesity definition were taken into account in this review, for example from the WHO (70), International Obesity Task Force gender- and age-related cutoffs (76), and British Growth Reference (102). Thirdly, some of the articles from this review that analyzed BMI effects used instruments that did not consider quantitative food data, which we know will influence individuals’ weight. Fourthly, the use of z scores of BMI (70) or not (85) can also explain discrepancies between results. Finally, associations with BMI also depend on the variables for which the analyses were adjusted. In general, the studies that analyzed BMI adjusted for multiple confounders; however, there is always a minority that only make simple correlations. In addition, in this review, a study showed different results (no association compared with a positive association between BMI and adherence to the Dietary Guideline Index for Children and Adolescents) according to stratification by the ages of the participants (123).
Other anthropometric indicators have been studied, such as WC for which a negative association with adherence to dietary patterns was found in all the 7 studies reported, but they are scarcer and limited. In 2 prospective studies it was possible to observe a decrease in WC and an improvement in body composition when adhering to healthier dietary patterns in children and adolescents (124, 125), meeting the main results obtained in this review in relation to these variables. Also, for cardiometabolic risk some evidence seems to support better cardiometabolic health being an effect of these dietary patterns, particularly when considering the KIDMED index and the DASH score. Indeed, some dietary patterns such as the MD, DASH, and the Nordic Diet are being related to reduced risks of cardiovascular disease in the literature (126). Regarding diagnostic diseases, a reduced number of articles were conducted, hampering further conclusions. It is also worthy of note that because many of the studies focused on adherence to the MD (50 of 128), it is important to consider a possible data bias with regard to the described associations with health outcomes.
Final remarks
To the best of our knowledge, this is the first article that has systematically searched and reviewed the scientific literature available on healthy and/or sustainable dietary patterns in children and adolescents, all over the world. To make this review more comprehensive, instruments were examined in detail at the methodology level, for example by performing analysis of the number of items, food and nonfood components included, cutoffs used in the scoring method, and categorization criteria for adherence classification. This work is also the first review which aimed to investigate the health-related outcomes associated with healthy and/or sustainable dietary patterns in children and adolescents. This systematic review scientifically supports the need to promote adherence to these dietary patterns from an early age and to understand how health education may benefit in the future these children and adolescents. In addition, this work upholds the need to consider the penalty for exceeding the recommended values, in order to measure more accurately adherence to dietary recommendations. Finally, none of the instruments have been duly proven to be sustainable, so the creation of a new instrument with sustainable characteristics or showing the associations of previous dietary patterns with, for example, the ecological and water footprints is highly demanded.
This systematic review has also some limitations. Firstly, most of the studies found were cross-sectional, which makes it impossible to establish temporal relations, which reduces the robustness of the results on the associations between the dietary patterns and the health-related outcomes. For this reason, more prospective cohorts and intervention studies are necessary to better understand the relation between adherence to these dietary patterns and health. Secondly, only MD instruments have several studies focused on the pediatric population. All the other studies identified instruments that need further application and investigation. Thirdly, most of the instruments described were not validated/adapted for the countries under study, which compromises the internal consistency of the described results, making validation/adaptation of these instruments in each country truly recommended and needed.
Conclusions
In this systematic review, 50 instruments measuring the adherence to healthy/or sustainable dietary patterns in children and adolescents were found: KIDMED, Krece Plus Test, MDS, fMDS, Mediterranean Adequacy Index, Italian Mediterranean Index, Mediterranean-Style Dietary Pattern Score, DQI-I adapted to MD, DASH score, Baltic Sea Diet Score, SEAD score, HLD Index, PLD-Index, OPLS, E-KINDEX, School Child Diet Index, HEI-1995, HEI-2005, HEI-2010, HEI-2015, HEI based on WHO recommendation, HDS, Healthy Dietary Adherence Score, Healthy Nutrition Score for Kids and Youth, Healthy Eating Index (Brazil), Malaysia Healthy Eating Index Score, Finnish Children Healthy Eating Index, Swedish Healthy Eating Index for Adolescents, Diet Quality Index for Adolescents, Riskmaten Adolescents Diet Diversity Score, Healthy Dietary Variety Index, Brazilian Healthy Eating Index Revised, Chinese's Children's Dietary Index, Children's Index of Diet Quality, Dietary Index for a Child's Eating, Youth Healthy Eating Index, modified version of Revised Children's Diet Quality Index, Dietary Diversity Score, Diet Score based on the Norwegian Health Directorate, DQI-I, Diet Quality Index for Children, Diet Quality Score for Ireland, Diet Quality Index Canadian, Diet Quality Index for Indian Children, Japanese Food Guide Spinning Top Score, Dietary Guideline Index for Children and Adolescents, Revised Children's Diet Quality Index, Recommended Food Score, ACARFS, and Australia Recommended Food Score for Pre-Schoolers. Of these, 14 adaptations were found.
Concerning the methodological approach, most of the instruments were based on previous application of an FFQ, food records, or 24-h dietary recalls. Out of the total instruments found (64 = 50 + 14), 29 took into account the quantitative consumption data of the included components and 47 considered the recommended food consumption frequencies. Vegetables, fruit, dairy products, meat and meat products, cereal products, and fish were the components presented in at least half of the revised instruments. Scoring was based on different methods such as national recommendations or principles of dietary patterns known a priori. The scoring methods were based on percentiles (medians, quintiles, quartiles, tertiles) or z scores. Only 2 instruments took into account the penalty for exceeding the recommended values.
The MD was the most studied dietary pattern among those aged 2–17 y (50 of 128 articles). This review shows that adherence to the dietary patterns exhibits wide variation all over the world, and ultimately depends on subjective factors, reflected in the food habits of a country. Moreover, most of the instruments described have still been little studied in children and adolescents, reducing the external validity of the results.
The dietary patterns described have primarily been associated with BMI, for which no consistent associations have been found. Other inverse relations were described, for instance with body fat, WC, and blood pressure, but evidence is still scarce.
Supplementary Material
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—BT, CA, and AO: designed the research, drafted the manuscript, conducted the research, and analyzed the data; BT: wrote the paper and had primary responsibility for the final content; CA, SR, and AO: reviewed and edited the paper; and all authors: read and approved the final manuscript.
Notes
BT was supported by PhD grant 2021.05133.BD, cofunded by the Foundation for Science and Technology (FCT—(Portuguese Ministry of Education and Science) and the FSE (Fundo Social Europeu) Program. AO was supported by FCT Investigator contract IF/01350/2015. This study had support from national funds from the Foundation for Science and Technology, I.P. – FCT (Portuguese Ministry of Education and Science) through the projects UIDB/04750/2020 and LA/P/0064/2020.
Author disclosures: The authors report no conflicts of interest.
Supplemental Table 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances/.
Abbreviations used: ACARFS, Australian Child and Adolescent Recommended Food Score; ADHD, attention deficit hyperactivity disorder; DASH, Dietary Approaches to Stop Hypertension; DQI-I, Diet Quality Index International; E-KINDEX, Electronic Kids Dietary Index; FAO, Food and Agriculture Organization of the United Nations; fMDS, food frequency–based Mediterranean Diet Score; HDS, Healthy Diet Score; HEI, Healthy Eating Index; HLD Index, Healthy Lifestyle–Diet Index; KIDMED, Mediterranean Diet Quality Index for Children and Adolescents; MD, Mediterranean Diet; MDS, Mediterranean Diet Score; NOS, Newcastle-Ottawa Scale; OPLS, Obesity-Preventive Lifestyle Score; PLD-Index, Preschoolers Diet–Lifestyle Index; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; RCT, randomized control trial; SEAD, Southern European Atlantic Diet; WC, waist circumference.
Contributor Information
Beatriz Teixeira, Faculty of Nutrition and Food Sciences, University of Porto, Porto, Portugal; EPIUnit - Instituto de Saúde Pública, Universidade do Porto [Institute of Public Health, University of Porto], Porto, Portugal; Laboratório para a Investigação Integrativa e Translacional em Saúde Populacional (ITR), [Laboratory for Integrative and Translational Research in Population Health (ITR)], Porto, Portugal.
Cláudia Afonso, Faculty of Nutrition and Food Sciences, University of Porto, Porto, Portugal; EPIUnit - Instituto de Saúde Pública, Universidade do Porto [Institute of Public Health, University of Porto], Porto, Portugal; Laboratório para a Investigação Integrativa e Translacional em Saúde Populacional (ITR), [Laboratory for Integrative and Translational Research in Population Health (ITR)], Porto, Portugal.
Sara Rodrigues, Faculty of Nutrition and Food Sciences, University of Porto, Porto, Portugal; EPIUnit - Instituto de Saúde Pública, Universidade do Porto [Institute of Public Health, University of Porto], Porto, Portugal; Laboratório para a Investigação Integrativa e Translacional em Saúde Populacional (ITR), [Laboratory for Integrative and Translational Research in Population Health (ITR)], Porto, Portugal.
Andreia Oliveira, EPIUnit - Instituto de Saúde Pública, Universidade do Porto [Institute of Public Health, University of Porto], Porto, Portugal; Laboratório para a Investigação Integrativa e Translacional em Saúde Populacional (ITR), [Laboratory for Integrative and Translational Research in Population Health (ITR)], Porto, Portugal; Faculty of Medicine, University of Porto, Porto, Portugal.
Data Availability
Supllementary Data are freely available without restriction at https://doi.org/10.1093/advances/nmab148.
References
- 1. Food and Agriculture Organization . Terminology at FAO. [Internet]. Rome, Italy: FAO; 2021. [cited September 2021] Available from: https://www.fao.org/faoterm/terminology-at-fao/en/. [Google Scholar]
- 2. Garnett T. Where are the best opportunities for reducing greenhouse gas emissions in the food system (including the food chain)?. Food Policy. 2011;36:S23–32. [Google Scholar]
- 3. Alexandratos N, Bruinsma J. World agriculture towards 2030/2050: the 2012 revision. ESA Working Paper No. 12-03. Rome, Italy: FAO; 2012. [Google Scholar]
- 4. European Environment Agency (EEA) . The European environment: state and outlook 2015: synthesis report. Copenhagen, Denmark: EEA; 2015. [Google Scholar]
- 5. Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, Garnett T, Tilman D, DeClerck F, Wood Aet al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;393(10170):447–92. [DOI] [PubMed] [Google Scholar]
- 6., Burlingame B, Dernini S, Nutrition and Consumer Protection Division, FAO , editors. Sustainable diets and biodiversity: directions and solutions for policy, research and action. Rome, Italy: FAO; 2012. [Google Scholar]
- 7. Vilarnau C, Stracker DM, Funtikov A, da Silva R, Estruch R, Bach-Faig A. Worldwide adherence to Mediterranean Diet between 1960 and 2011. Eur J Clin Nutr. 2019;72(S1):83–91. [DOI] [PubMed] [Google Scholar]
- 8. Dernini S, Berry EM. Mediterranean diet: from a healthy diet to a sustainable dietary pattern. Front Nutr. 2015;2:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Iaccarino Idelson P, Scalfi L, Valerio G. Adherence to the Mediterranean Diet in children and adolescents: a systematic review. Nutr Metab Cardiovasc Dis. 2017;27(4):283–99. [DOI] [PubMed] [Google Scholar]
- 10. Grosso G, Galvano F. Mediterranean diet adherence in children and adolescents in southern European countries. NFS J. 2016;3:13–19. [Google Scholar]
- 11. Liberali R, Kupek E, Assis MAA. Dietary patterns and childhood obesity risk: a systematic review. Child Obes. 2020;16(2):70–85. [DOI] [PubMed] [Google Scholar]
- 12. Rocha NP, Milagres LC, Longo GZ, Ribeiro AQ, Novaes JF. Association between dietary pattern and cardiometabolic risk in children and adolescents: a systematic review. J Pediatr (Rio J). 2017;93(3):214–22. [DOI] [PubMed] [Google Scholar]
- 13. Movassagh EZ, Baxter-Jones ADG, Kontulainen S, Whiting SJ, Vatanparast H. Tracking dietary patterns over 20 years from childhood through adolescence into young adulthood: the Saskatchewan Pediatric Bone Mineral Accrual Study. Nutrients. 2017;9(9):990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ambrosini GL, Emmett PM, Northstone K, Jebb SA. Tracking a dietary pattern associated with increased adiposity in childhood and adolescence. Obesity. 2014;22(2):458–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas. 2011;70(3):266–84. [DOI] [PubMed] [Google Scholar]
- 16. Taddei JA, Longo-Silva G, Lang RMF, de Aguiar Toloni MH, Vega JB. Nutrição em saúde pública. 2nd ed. Rio de Janeiro, Brazil: Rubio; 2016. [Google Scholar]
- 17. Kastorini CM, Papadakis G, Milionis HJ, Kalantzi K, Puddu PE, Nikolaou V, Vemmos KN, Goudevenos JA, Panagiotakos DB. Comparative analysis of a-priori and a-posteriori dietary patterns using state-of-the-art classification algorithms: a case/case-control study. Artif Intell Med. 2013;59(3):175–83. [DOI] [PubMed] [Google Scholar]
- 18. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–608. [DOI] [PubMed] [Google Scholar]
- 19. Oliveira A, Lopes C, Rodríguez-Artalejo F. Adherence to the Southern European Atlantic Diet and occurrence of nonfatal acute myocardial infarction. Am J Clin Nutr. 2010;92(1):211–7. [DOI] [PubMed] [Google Scholar]
- 20. Martinez-Lacoba R, Pardo-Garcia I, Amo-Saus E, Escribano-Sotos F. Mediterranean diet and health outcomes: a systematic meta-review. Eur J Public Health. 2018;28(5):955–61. [DOI] [PubMed] [Google Scholar]
- 21. Kelly JT, Palmer SC, Wai SN, Ruospo M, Carrero J-J, Campbell KL, Strippoli GFM. Healthy dietary patterns and risk of mortality and ESRD in CKD: a meta-analysis of cohort studies. Clin J Am Soc Nephrol. 2017;12(2):272–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smithers LG, Golley RK, Brazionis L, Lynch JW. Characterizing whole diets of young children from developed countries and the association between diet and health: a systematic review. Nutr Rev. 2011;69(8):449–67. [DOI] [PubMed] [Google Scholar]
- 23. Lazarou C, Newby PK. Use of dietary indexes among children in developed countries. Adv Nutr. 2011;2(4):295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dalwood P, Marshall S, Burrows TL, McIntosh A, Collins CE. Diet quality indices and their associations with health-related outcomes in children and adolescents: an updated systematic review. Nutr J. 2020;19(1):118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Marshall S, Burrows T, Collins CE. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J Hum Nutr Diet. 2014;27(6):577–98. [DOI] [PubMed] [Google Scholar]
- 26. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group . Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- 28. Wohlin C. Guidelines for snowballing in systematic literature studies and a replication in software engineering. In: Proceedings of the 18th International Conference on Evaluation and Assessment in Software Engineering; 13–14 May, 2014; London, United Kingdom. New York: Association for Computing Machinery; 2014. Article 38. [Google Scholar]
- 29. Rathbone J, Carter M, Hoffmann T, Glasziou P. Better duplicate detection for systematic reviewers: evaluation of Systematic Review Assistant-Deduplication Module. Syst Rev. 2015;4(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Clarivate Analytics . Endnote. Boston, MA: Clarivate Analytics; 2019. [Google Scholar]
- 31. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [Internet]. Ottawa, Canada: The Ottawa Hospital Research Institute; 2000.[cited April 2021] Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Google Scholar]
- 32. Moskalewicz A, Oremus M. No clear choice between Newcastle–Ottawa Scale and Appraisal Tool for Cross-Sectional Studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J Clin Epidemiol. 2020;120:94–103. [DOI] [PubMed] [Google Scholar]
- 33. Alshabanat A, Zafari Z, Albanyan O, Dairi M, FitzGerald JM. Asthma and COPD Overlap Syndrome (ACOS): a systematic review and meta analysis. PloS One. 2015;10(9):e0136065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, Perruolo E, Parati G, ESH Working Group on CV Risk in Low Resource Settings . Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PloS One. 2016;11(1):e0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SMet al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 36. Costarelli V, Michou M, Panagiotakos DB, Lionis C. Adherence to the Mediterranean diet and weight status in children: the role of parental feeding practices. Int J Food Sci Nutr. 2021;72(1):112–22. [DOI] [PubMed] [Google Scholar]
- 37. Tognon G, Hebestreit A, Lanfer A, Moreno LA, Pala V, Siani A, Tornaritis M, Henauw S, Veidebaum T, Molnár Det al. Mediterranean diet, overweight and body composition in children from eight European countries: cross-sectional and prospective results from the IDEFICS study. Nutr Metab Cardiovasc Dis. 2014;24(2):205–13. [DOI] [PubMed] [Google Scholar]
- 38. Manios Y, Kourlaba G, Grammatikaki E, Androutsos O, Moschonis G, Roma-Giannikou E. Development of a diet–lifestyle quality index for young children and its relation to obesity: the Preschoolers Diet–Lifestyle Index. Public Health Nutr. 2010;13(12):2000–9. [DOI] [PubMed] [Google Scholar]
- 39. Leal KK, Schneider BC, França GVA, Gigante DP, dos Santos I, Assunção MCF. Diet quality of preschool children aged 2 to 5 years living in the urban area of Pelotas, Brazil. Rev Paul Pediatr. 2015;33(3):310–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Röytiö H, Jaakkola J, Hoppu U, Poussa T, Laitinen K. Development and evaluation of a stand-alone index for the assessment of small children's diet quality. Public Health Nutr. 2015;18(11):1941–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Vyncke K, Cruz Fernandez E, Fajó-Pascual M, Cuenca-García M, De Keyzer W, Gonzalez-Gross M, Moreno LA, Beghin L, Breidenassel C, Kersting Met al. Validation of the Diet Quality Index for Adolescents by comparison with biomarkers, nutrient and food intakes: the HELENA study. Br J Nutr. 2013;109(11):2067–78. [DOI] [PubMed] [Google Scholar]
- 42. Delshad M, Beck KL, von Hurst PR, Mugridge O, Conlon CA. The validity and reliability of the Dietary Index for a Child's Eating in 2–8-year old children living in New Zealand. Matern Child Nutr. 2019;15(3):e12758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Arvidsson L, Eiben G, Hunsberger M, De Bourdeaudhuij I, Molnar D, Jilani H, Thumann B, Veidebaum T, Russo P, Tornatitis Met al. Bidirectional associations between psychosocial well-being and adherence to healthy dietary guidelines in European children: prospective findings from the IDEFICS study. BMC Public Health. 2017;17(1):926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cabalda AB, Rayco-Solon P, Solon JA, Solon FS. Home gardening is associated with Filipino preschool children's dietary diversity. J Am Diet Assoc. 2011;111(5):711–5. [DOI] [PubMed] [Google Scholar]
- 45. Gingras V, Switkowski KM, Rifas-Shiman SL, Faleschini S, Oken E, Hivert MF. Associations of early parental concerns and feeding behaviors with child's diet quality through mid-childhood. Nutrients. 2020;12(11):3231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Truthmann J, Richter A, Thiele S, Drescher L, Roosen J, Mensink GB. Associations of dietary indices with biomarkers of dietary exposure and cardiovascular status among adolescents in Germany. Nutr Metab. 2012;9(1):92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Moreira C, Santos R, Moreira P, Lobelo F, Ruiz JR, Vale S, Santos PC, Abreu S, Mota J. Cardiorespiratory fitness is negatively associated with metabolic risk factors independently of the adherence to a healthy dietary pattern. Nutr Metab Cardiovasc Dis. 2013;23(7):670–6. [DOI] [PubMed] [Google Scholar]
- 48. Rostami H, Khayyatzadeh SS, Tavakoli H, Bagherniya M, Mirmousavi SJ, Farahmand SK, Tayefi M, Ferns GA, Ghayour-Mobarhan M. The relationship between adherence to a Dietary Approach to Stop Hypertension (DASH) dietary pattern and insomnia. BMC Psychiatry. 2019;19(1):234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Neshatbini Tehrani A, Farhadnejad H, Salehpour A, Beyzai B, Hekmatdoost A, Rashidkhani B. The association between nutrition knowledge and adherence to a Mediterranean dietary pattern in Iranian female adolescents. Int J Adolesc Med Health. 2019;33(4):2018–0188. [DOI] [PubMed] [Google Scholar]
- 50. Bacopoulou F, Landis G, Rentoumis A, Tsitsika A, Efthymiou V. Mediterranean diet decreases adolescent waist circumference. Eur J Clin Invest. 2017;47(6):447–55. [DOI] [PubMed] [Google Scholar]
- 51. Mazaraki A, Tsioufis C, Dimitriadis K, Tsiachris D, Stefanadi E, Zampelas A, Richter D, Mariolis A, Panagiotakos D, Tousoulis Det al. Adherence to the Mediterranean diet and albuminuria levels in Greek adolescents: data from the Leontio Lyceum Albuminuria (3L study). Eur J Clin Nutr. 2011;65(2):219–25. [DOI] [PubMed] [Google Scholar]
- 52. del Mar Bibiloni M, Pons A, Tur JA. Compliance with the Mediterranean Diet Quality Index (KIDMED) among Balearic Islands’ adolescents and its association with socioeconomic, anthropometric and lifestyle factors. Ann Nutr Metab. 2016;68(1):42–50. [DOI] [PubMed] [Google Scholar]
- 53. Martínez E, Llull R, Del Mar Bibiloni M, Pons A, Tur JA. Adherence to the Mediterranean dietary pattern among Balearic Islands adolescents. Br J Nutr. 2010;103(11):1657–64. [DOI] [PubMed] [Google Scholar]
- 54. Winpenny EM, van Harmelen AL, White M, van Sluijs EM, Goodyer IM. Diet quality and depressive symptoms in adolescence: no cross-sectional or prospective associations following adjustment for covariates. Public Health Nutr. 2018;21(13):2376–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Monjardino T, Lucas R, Ramos E, Barros H. Associations between a priori-defined dietary patterns and longitudinal changes in bone mineral density in adolescents. Public Health Nutr. 2014;17(1):195–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yüksel A, Önal HY, Kurt KG, Adherence to the Mediterranean Diet and factors affecting obesity in high school students. Int J Med Res Health Sci. 2017;6(12):78–86. [Google Scholar]
- 57. Zervaki K, Yiannakouris N, Sdrali D, Costarelli V. Diet quality, disordered eating and health-related quality of life in Greek adolescents. Nutr Food Sci. 2017;47(4):511–21. [Google Scholar]
- 58. Arouca AB, Meirhaeghe A, Dallongeville J, Moreno LA, Lourenço GJ, Marcos A, Huybrechts I, Manios Y, Lambrinou CP, Gottrand Fet al. Interplay between the Mediterranean diet and C-reactive protein genetic polymorphisms towards inflammation in adolescents. Clin Nutr. 2020;39(6):1919–26. [DOI] [PubMed] [Google Scholar]
- 59. Bricarello LP, de Moura Souza A, de Almeida Alves M, Retondario A, Fernandes R, Trindade E, Zeni L, Vasconcelos F. Association between DASH diet (Dietary Approaches to Stop Hypertension) and hypertension in adolescents: a cross-sectional school-based study. Clin Nutr ESPEN. 2020;36:69–75. [DOI] [PubMed] [Google Scholar]
- 60. Asghari G, Yuzbashian E, Mirmiran P, Hooshmand F, Najafi R, Azizi F. Dietary Approaches to Stop Hypertension (DASH) dietary pattern is associated with reduced incidence of metabolic syndrome in children and adolescents. J Pediatr. 2016;174:178–84.e1. [DOI] [PubMed] [Google Scholar]
- 61. Loprinzi PD, Lee IM, Andersen RE, Crespo CJ, Smit E. Association of concurrent healthy eating and regular physical activity with cardiovascular disease risk factors in U.S. youth. Am J Health Promot. 2015;30(1):2–8. [DOI] [PubMed] [Google Scholar]
- 62. van Egmond-Fröhlich AWA, Weghuber D, de Zwaan M. Association of symptoms of attention-deficit/hyperactivity disorder with physical activity, media time, and food intake in children and adolescents. PloS One. 2012;7(11):e49781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mellendick K, Shanahan L, Wideman L, Calkins S, Keane S, Lovelady C. Diets rich in fruits and vegetables are associated with lower cardiovascular disease risk in adolescents. Nutrients. 2018;10(2):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ping-Delfos WLCS, Beilin LJ, Oddy WH, Burrows S, Mori TA. Use of the Dietary Guideline Index to assess cardiometabolic risk in adolescents. Br J Nutr. 2015;113(11):1741–52. [DOI] [PubMed] [Google Scholar]
- 65. Ronca DB, Blume CA, Cureau FV, Camey SA, Leotti VB, Drehmer M, Schaan BD, Baiocchi de Carvalho K. Diet quality index for Brazilian adolescents: the ERICA study. Eur J Nutr. 2020;59(2):539–56. [DOI] [PubMed] [Google Scholar]
- 66. Silva AL, Fragoso I, Barrigas C, Teles J. Portuguese adolescents diet quality, lifestyle variables and body composition, in relation to precise measures of maturity. Med J Nutrition Metab. 2020;13(1):29–41. [Google Scholar]
- 67. Zhang X, Gong Y, Jia P, Zhang J, Xue H, Quan L, Tian G, Xiong J, Zhang L, Wang Yet al. Monetary diet cost is positively associated with diet quality and obesity: an analysis of school-aged children in Southwest China. J Public Health (Oxf). 2019;41(2):250–8. [DOI] [PubMed] [Google Scholar]
- 68. Rivas A, Monteagudo C, Heras-Gonzalez L, Mariscal-Arcas M, Lorenzo-Tovar ML, Olea-Serrano F. Association of bisphenol A exposure with dietary quality indices in Spanish schoolchildren. Food Chem Toxicol. 2016;94:25–30. [DOI] [PubMed] [Google Scholar]
- 69. Mariscal-Arcas M, Velasco J, Monteagudo C, Caballero-Plasencia MA, Lorenzo-Tovar ML, Olea-Serrano F. Comparison of methods to evaluate the quality of the Mediterranean diet in a large representative sample of young people in Southern Spain. Nutr Hosp. 2010;25(6):1006–13. [PubMed] [Google Scholar]
- 70. Gómez SF, Casas Esteve R, Subirana I, Serra-Majem L, Fletas Torrent M, Homs C, Bawaked RA, Estrada L, Fíto M, Schröder H. Effect of a community-based childhood obesity intervention program on changes in anthropometric variables, incidence of obesity, and lifestyle choices in Spanish children aged 8 to 10 years. Eur J Pediatr. 2018;177(10):1531–9. [DOI] [PubMed] [Google Scholar]
- 71. Martin-Calvo N, Chavarro JE, Falbe J, Hu FB, Field AE. Adherence to the Mediterranean dietary pattern and BMI change among US adolescents. Int J Obes. 2016;40(7):1103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Bawaked RA, Gomez SF, Homs C, Casas Esteve R, Cardenas G, Fíto M, Helmut S. Association of eating behaviors, lifestyle, and maternal education with adherence to the Mediterranean diet in Spanish children. Appetite. 2018;130:279–85. [DOI] [PubMed] [Google Scholar]
- 73. Muros JJ, Cofre-Bolados C, Arriscado D, Zurita F, Knox E. Mediterranean diet adherence is associated with lifestyle, physical fitness, and mental wellness among 10-y-olds in Chile. Nutrition. 2017;35:87–92. [DOI] [PubMed] [Google Scholar]
- 74. Ojeda-Rodríguez A, Zazpe I, Morell-Azanza L, Chueca MJ, Azcona-Sanjulian MC, Marti A. Improved diet quality and nutrient adequacy in children and adolescents with abdominal obesity after a lifestyle intervention. Nutrients. 2018;10(10):1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Magriplis E, Farajian P, Pounis GD, Risvas G, Panagiotakos DB, Zampelas A. High sodium intake of children through ‘hidden’ food sources and its association with the Mediterranean diet: the GRECO study. J Hypertens. 2011;29(6):1069–76. [DOI] [PubMed] [Google Scholar]
- 76. Rosi A, Calestani MV, Parrino L, Milioli G, Palla L, Volta E, Brighenti F, Scazzina F. Weight status is related with gender and sleep duration but not with dietary habits and physical activity in primary school Italian children. Nutrients. 2017;9(6):579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Marques GFS, Pinto SMO, Reis A, Martins TDB, Conceição APD, Pinheiro ARV. Adherence to the Mediterranean diet in elementary school children (1st cycle). Rev Paul Pediatr. 2021;39:e2019259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Jennings A, Welch A, van Sluijs EM, Griffin SJ, Cassidy A. Diet quality is independently associated with weight status in children aged 9–10 years. J Nutr. 2011;141(3):453–9. [DOI] [PubMed] [Google Scholar]
- 79. Najafi A, Faghih S, Hojhabrimanesh A, Najafi M, Tangestani H, Atefi M, Teymouri M, Salehi M, Kamali M, Amanat Set al. Greater adherence to the dietary approaches to stop hypertension (DASH) dietary pattern is associated with lower blood pressure in healthy Iranian primary school children. Eur J Nutr. 2018;57(4):1449–58. [DOI] [PubMed] [Google Scholar]
- 80. Robson SM, Couch SC, Peugh JL, Glanz K, Zhou C, Sallis JF, Saelens BE. Parent diet quality and energy intake are related to child diet quality and energy intake. J Acad Nutr Diet. 2016;116(6):984–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Eloranta AM, Schwab U, Venäläinen T, Kiiskinen S, Lakka HM, Laaksonen DE, Lakka TA, Lindi V. Dietary quality indices in relation to cardiometabolic risk among Finnish children aged 6–8 years – the PANIC study. Nutr Metab Cardiovasc Dis. 2016;26(9):833–41. [DOI] [PubMed] [Google Scholar]
- 82. Pérez-Gimeno G, Rupérez AI, Vázquez-Cobela R, Herráiz-Gastesi G, Gil-Campos M, Aguilera CM, Moreno LA, Trabazo M, Bueno-Lozano G. Energy dense salty food consumption frequency is associated with diastolic hypertension in Spanish children. Nutrients. 2020;12(4):1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Clennin M, Brown A, Lian M, Dowda M, Colabianchi N, Pate RR. Neighborhood socioeconomic deprivation associated with fat mass and weight status in youth. Int J Environ Res Public Health. 2020;17(17):6421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Azadbakht L, Akbari F, Esmaillzadeh A. Diet quality among Iranian adolescents needs improvement. Public Health Nutr. 2015;18(4):615–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Bonaccorsi G, Furlan F, Scocuzza M, Lorini C. Adherence to Mediterranean diet among students from primary and middle school in the Province of Taranto, 2016–2018. Int J Environ Res Public Health. 2020;17(15):5437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Korkmaz GÖ, Kabaran S. Protective effects of a Mediterranean-like dietary pattern on obesity, abdominal obesity and large neck circumference in a cohort of Turkish children aged 6-9 years. Asia Pac J Clin Nutr. 2020;29(2):363–71. [DOI] [PubMed] [Google Scholar]
- 87. Mistretta A, Marventano S, Antoci M, Cagnetti A, Giogianni G, Nolfo F, Rametta S, Pecora G, Marranzano M. Mediterranean diet adherence and body composition among Southern Italian adolescents. Obes Res Clin Pract. 2017;11(2):215–26. [DOI] [PubMed] [Google Scholar]
- 88. López-Gil JF, García-Hermoso A, Gomes Sentone R, Israel Caetano C, Renato Cavichiolli F, Yuste Lucas JL. Influence of adiposity on physical activity in schoolchildren: the moderator role of adherence to the Mediterranean diet. Sustainability. 2020;12(16):6474. [Google Scholar]
- 89. Grosso G, Marventano S, Buscemi S, Scuderi A, Matalone M, Platania A, Giorgianni G, Rametta S, Nolfo F, Galvano Fet al. Factors associated with adherence to the Mediterranean diet among adolescents living in Sicily, Southern Italy. Nutrients. 2013;5(12):4908–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Manios Y, Moschonis G, Papandreou C, Politidou E, Naoumi A, Peppas D, Mavrogianni C, Lionis C, Chrousos GP, ‘Healthy Growth Study’ group . Revised Healthy Lifestyle-Diet Index and associations with obesity and iron deficiency in schoolchildren: The Healthy Growth Study. J Hum Nutr Diet. 2015;28:50–8. [DOI] [PubMed] [Google Scholar]
- 91. Papoutsakis C, Papadakou E, Chondronikola M, Antonogeorgos G, Matziou V, Drakouli M, Konstantaki E, Priftis KN. An obesity-preventive lifestyle score is negatively associated with pediatric asthma. Eur J Nutr. 2018;57(4):1605–13. [DOI] [PubMed] [Google Scholar]
- 92. Lazarou C, Panagiotakos D, Spanoudis G, Matalas AL. E-KINDEX: a dietary screening tool to assess children's obesogenic dietary habits. J Am Coll Nutr. 2011;30(2):100–12. [DOI] [PubMed] [Google Scholar]
- 93. Lioret S, McNaughton SA, Cameron AJ, Crawford D, Campbell KJ, Cleland VJ, Ball K. Three-year change in diet quality and associated changes in BMI among schoolchildren living in socio-economically disadvantaged neighbourhoods. Br J Nutr. 2014;112(2):260–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Moraeus L, Lindroos AK, Warensjö Lemming E, Mattisson I. Diet diversity score and healthy eating index in relation to diet quality and socio-demographic factors: results from a cross-sectional national dietary survey of Swedish adolescents. Public Health Nutr. 2020;23(10):1754–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Shang X, Li Y, Xu H, Zhang Q, Liu A, Du S, Guo H, Ma G. Leading dietary determinants identified using machine learning techniques and a healthy diet score for changes in cardiometabolic risk factors in children: a longitudinal analysis. Nutr J. 2020;19(1):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Barros L, Lopes C, Oliveira A. Child and family characteristics are associated with a dietary variety index in 4-year-old children from the Generation XXI cohort. Nutr Res. 2019;63:76–85. [DOI] [PubMed] [Google Scholar]
- 97. Arriscado D, Muros JJ, Zabala M, Dalmau JM. Factors associated with low adherence to a Mediterranean diet in healthy children in northern Spain. Appetite. 2014;80:28–34. [DOI] [PubMed] [Google Scholar]
- 98. Archero F, Ricotti R, Solito A, Carrera D, Civello F, Di Bella R, Bellone S, Prodamet F. Adherence to the Mediterranean diet among school children and adolescents living in Northern Italy and unhealthy food behaviors associated to overweight. Nutrients. 2018;10(9):1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Roccaldo R, Censi L, D'Addezio L, Toti E, Martone D, D'Addesa D, Cernigliaro A, ZOOM8 Study group . Adherence to the Mediterranean diet in Italian school children (The ZOOM8 Study). Int J Food Sci Nutr. 2014;65(5):621–8. [DOI] [PubMed] [Google Scholar]
- 100. Azekour K, Outaleb Z, Eddouks M, Khallouki F, El Bouhali B. Adherence to the Mediterranean diet of school-age children in Moroccan oases, Draa-Tafilalet Region. East Mediterr Health J. 2020;26(9):1070–7. [DOI] [PubMed] [Google Scholar]
- 101. Labayen Goñi I, Arenaza L, Medrano M, García N, Cadenas-Sanchez C, Ortega FB. Associations between the adherence to the Mediterranean diet and cardiorespiratory fitness with total and central obesity in preschool children: the PREFIT project. Eur J Nutr. 2018;57(8):2975–83. [DOI] [PubMed] [Google Scholar]
- 102. Marshall S, Watson J, Burrows T, Guest M, Collins CE. The development and evaluation of the Australian child and adolescent recommended food score: a cross-sectional study. Nutr J. 2012;11(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Coelho LG, Cândido APC, Machado-Coelho GLL, de Freitas SN. Association between nutritional status, food habits and physical activity level in schoolchildren. J Pediatr (Rio J). 2012;88(5):406–12. [DOI] [PubMed] [Google Scholar]
- 104. Dave JM, Liu Y, Chen T-A, Thompson DI, Cullen KW. Does the Kids Café Program's nutrition education improve children's dietary intake? A pilot evaluation study. J Nutr Educ Behav. 2018;50(3):275–82.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Brownlee IA, Low J, Duriraju N, Chun M, Ong JXY, Tay ME, Hendrie GA, Santos-Merx L. Evaluation of the proximity of Singaporean children's dietary habits to food-based dietary guidelines. Nutrients. 2019;11(11):2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Appannah G, Emi NA, Yusin NAA, Gan WY, Shariff ZM, Shamsuddin NH, Zaini AA, Appukutty M. Evaluation of dietary quality using Malaysian Healthy Eating Index and its relationships with cardiometabolic risk factors in Malaysian adolescents. Mal J Med Health Sci. 2020;16(SUPP6):46–55. [Google Scholar]
- 107. Zhao W, Yu K, Tan S, Zheng Y, Zhao A, Wang P, Zhang Y. Dietary diversity scores: an indicator of micronutrient inadequacy instead of obesity for Chinese children. BMC Public Health. 2017;17(1):440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Tur JA, Romaguera D, Pons A. The Diet Quality Index-International (DQI-I): is it a useful tool to evaluate the quality of the Mediterranean diet?. Br J Nutr. 2005;93(3):369–76. [DOI] [PubMed] [Google Scholar]
- 109. Hayuningtyas A, Dewi YA, Octavia L, Pulungan A, Agustina R. Dietary quality score is positively associated with serum adiponectin level in Indonesian preschool-age children living in the urban area of Jakarta. PloS One. 2021;16(2):e0246234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Wendpap LL, Ferreira MG, Rodrigues PRM, Pereira RA, Loureiro ADS, Gonçalves-Silva RMV. Qualidade da dieta de adolescentes e fatores associados. Cad Saude Publica. 2014;30(1):97–106. [DOI] [PubMed] [Google Scholar]
- 111. Drenowatz C, Carlson JJ, Pfeiffer KA, Eisenmann JC. Joint association of physical activity/screen time and diet on CVD risk factors in 10-year-old children. Front Med. 2012;6(4):428–35. [DOI] [PubMed] [Google Scholar]
- 112. Shinsugi C, Tani Y, Kurotani K, Takimoto H, Ochi M, Fujiwara T. Change in growth and diet quality among preschool children in Tokyo, Japan. Nutrients. 2020;12(5):1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Agostinis-Sobrinho C, Abreu S, Moreira C, Lopes L, García-Hermoso A, Ramírez-Vélez R, Correa-Bautista JE, Mota J, Santoset R. Muscular fitness, adherence to the Southern European Atlantic Diet and cardiometabolic risk factors in adolescents. Nutr Metab Cardiovasc Dis. 2017;27(8):695–702. [DOI] [PubMed] [Google Scholar]
- 114. Manios Y, Kourlaba G, Grammatikaki E, Koubitski A, Siatitsa PE, Vandorou A, Kyriakou K, Dede V, Moschonis G. Development of a lifestyle–diet quality index for primary schoolchildren and its relation to insulin resistance: the Healthy Lifestyle–Diet Index. Eur J Clin Nutr. 2010;64(12):1399–406. [DOI] [PubMed] [Google Scholar]
- 115. Garcia-Hermoso A, Vegas-Heredia ED, Fernández-Vergara O, Ceballos-Ceballos R, Andrade-Schnettler R, Arellano-Ruiz P, Ramírez-Vélez R. Independent and combined effects of handgrip strength and adherence to a Mediterranean diet on blood pressure in Chilean children. Nutrition. 2019;60:170–4. [DOI] [PubMed] [Google Scholar]
- 116. Grigoropoulou D, Priftis K, Yannakoulia M, Papadimitriou A, Anthracopoulos M, Yfanti K, Panagiotakos DB. Urban environment adherence to the Mediterranean diet and prevalence of asthma symptoms among 10- to 12-year-old children: the Physical Activity, Nutrition, and Allergies in Children Examined in Athens study. Allergy Asthma Proc. 2011;32(5):351–8. [DOI] [PubMed] [Google Scholar]
- 117. Ríos-Hernández A, Alda JA, Farran-Codina A, Ferreira-García E, Izquierdo-Pulido M. The Mediterranean diet and ADHD in children and adolescents. Pediatrics. 2017;139(2):e20162027. [DOI] [PubMed] [Google Scholar]
- 118. Protudjer JL, Sevenhuysen GP, Ramsey CD, Kozyrskyj AL, Becker AB. Low vegetable intake is associated with allergic asthma and moderate-to-severe airway hyperresponsiveness. Pediatr Pulmonol. 2012;47(12):1159–69. [DOI] [PubMed] [Google Scholar]
- 119. Cabrera SG, Fernández NH, Hernández CR, Nissensohn M, Román-Viñas B, Serra-Majem L. KIDMED test; prevalence of low adherence to the Mediterranean diet in children and young; a systematic review. Nutr Hosp. 2015;32(6):2390–9. [DOI] [PubMed] [Google Scholar]
- 120. SooHoo NF, McDonald AP, Seiler JG, McGillivary GR. Evaluation of the construct validity of the DASH questionnaire by correlation to the SF-36. J Hand Surg Am. 2002;27(3):537–41. [DOI] [PubMed] [Google Scholar]
- 121. Kanerva N, Kaartinen NE, Schwab U, Lahti-Koski M, Männistö S. The Baltic Sea Diet Score: a tool for assessing healthy eating in Nordic countries. Public Health Nutr. 2014;17(8):1697–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, Vassilakou T, Lipworth L, Trichopoulos D. Diet and overall survival in elderly people. BMJ. 1995;311(7018):1457–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Golley RK, Hendrie GA, McNaughton SA. Scores on the Dietary Guideline Index for Children and Adolescents are associated with nutrient intake and socio-economic position but not adiposity. J Nutr. 2011;141(7):1340–7. [DOI] [PubMed] [Google Scholar]
- 124. Poeta M, Lamberti R, Di Salvio D, Massa G, Torsiello N, Pierri L, Bovi A, Michele LD, Nuzio SG, Pietro Vajro P. Waist circumference and healthy lifestyle preferences/knowledge monitoring in a preschool obesity prevention program. Nutrients. 2019;11(9):2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Fernández-Alvira JM, Bammann K, Eiben G, Hebestreit A, Kourides YA, Kovacs E, Michels N, Pala V, Reisch L, Russo Pet al. Prospective associations between dietary patterns and body composition changes in European children: the IDEFICS study. Public Health Nutr. 2017;20(18):3257–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Cena H, Calder PC. Defining a healthy diet: evidence for the role of contemporary dietary patterns in health and disease. Nutrients. 2020;12(2):334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Grassi T, Bagordo F, Panico A, De Giorgi M, Idolo A, Serio F, Tumolo MR, Donnoet A. Adherence to Mediterranean diet of children living in small Southern Italian villages. Int J Food Sci Nutr. 2020;71(4):490–9. [DOI] [PubMed] [Google Scholar]
- 128. Rosi A, Giopp F, Milioli G, Melegari G, Goldoni M, Parrino L, Scazzina F. Weight status, adherence to the Mediterranean Diet, physical activity level, and sleep behavior of Italian junior high school adolescents. Nutrients. 2020;12(2):478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Grao-Cruces A, Nuviala A, Fernández-Martínez A, Pérez-Turpin JA. Association of physical self-concept with physical activity, life satisfaction and Mediterranean diet in adolescents. Kinesiology. 2014;46(1):3–11. [Google Scholar]
- 130. Torres-Luque G, Hernández-García R, Ortega-Toro E, Nikolaidis PT. The effect of place of residence on physical fitness and adherence to Mediterranean Diet in 3–5-year-old girls and boys: urban vs. rural. Nutrients. 2018;10(12):1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Obradovic Salcin L, Karin Z, Miljanovic Damjanovic V, Ostojic M, Vrdoljak A, Gilic B, Sekulic D, Lang-Morovic M, Markic J, Sajber D. Physical activity, body mass, and adherence to the Mediterranean diet in preschool children: a cross-sectional analysis in the Split-Dalmatia County (Croatia). Int J Environ Res Public Health. 2019;16(18):3237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Calmeiro L, Pereira C. Healthy lifestyles and BMI as correlates of body image dissatisfaction in primary school children. Acta Gymnica. 2019;49(4):189–96. [Google Scholar]
- 133. López-Gil JF, Brazo-Sayavera J, García-Hermoso A, Yuste Lucas JL. Adherence to Mediterranean Diet related with physical fitness and physical activity in schoolchildren aged 6–13. Nutrients. 2020;12(2):567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Esteban-Cornejo I, Izquierdo-Gomez R, Gómez-Martínez S, Padilla-Moledo C, Castro-Piñero J, Marcos A, Veiga OL. Adherence to the Mediterranean diet and academic performance in youth: the UP&DOWN study. Eur J Nutr. 2016;55(3):1133–40. [DOI] [PubMed] [Google Scholar]
- 135. Chacón-Cuberos R, Zurita-Ortega F, Martínez-Martínez A, Olmedo-Moreno EM, Castro-Sánchez M. Adherence to the Mediterranean diet is related to healthy habits, learning processes, and academic achievement in adolescents: a cross-sectional study. Nutrients. 2018;10(11):1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Sahingoz SA, Sanlier N. Compliance with Mediterranean Diet Quality Index (KIDMED) and nutrition knowledge levels in adolescents. A case study from Turkey. Appetite. 2011;57(1):272–7. [DOI] [PubMed] [Google Scholar]
- 137. Delgado Floody PA, Caamaño Navarrete F, Jerez Mayorga D, Cofré-Lizama A, Guzmán-Guzmán IP. The association between children's food habits, anthropometric parameters and health-related quality of life in Chilean school-age children. Nutr Hosp. 2019;36(5):1061–6. [DOI] [PubMed] [Google Scholar]
- 138. Pastor R, Pinilla N, Tur JA. The economic cost of diet and its association with adherence to the Mediterranean diet in a cohort of Spanish primary schoolchildren. Int J Environ Res Public Health. 2021;18(3):1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Zani C, Ceretti E, Grioni S, Viola GCV, Donato F, Feretti D, Festa A, Bonizzoni S, Bonetti A, Monarca Set al. Are 6-8 year old Italian children moving away from the Mediterranean diet?. Ann Ig. 2016;28(5):339–48. [DOI] [PubMed] [Google Scholar]
- 140. Handeland K, Kjellevold M, Markhus MW, Graff IE, Frøyland L, Lie Ø, Skotheim S, Stormark KM, Dahl L, Øyen J. A diet score assessing Norwegian adolescents’ adherence to dietary recommendations—development and test-retest reproducibility of the score. Nutrients. 2016;8(8):467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Huybrechts I, Vereecken C, De Bacquer D, Vandevijvere S, Van Oyen H, Maes L, Vanhauwaert E, Temme L, Backer G, Henauw S. Reproducibility and validity of a diet quality index for children assessed using a FFQ. Br J Nutr. 2010;104(1):135–44. [DOI] [PubMed] [Google Scholar]
- 142. Keane E, Cullinan J, Perry CP, Kearney PM, Harrington JM, Perry IJ, Layte R. Dietary quality in children and the role of the local food environment. SSM Popul Health. 2016;2:770–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Eloranta AM, Jääskeläinen J, Venäläinen T, Jalkanen H, Kiiskinen S, Mäntyselkä A, Schwab U, Lindi V, Lakka TA. Birth weight is associated with dietary factors at the age of 6–8 years: the Physical Activity and Nutrition in Children (PANIC) study. Public Health Nutr. 2018;21(7):1278–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Rydén PJ, Hagfors L. Diet cost, diet quality and socio-economic position: how are they related and what contributes to differences in diet costs?. Public Health Nutr. 2011;14(9):1680–92. [DOI] [PubMed] [Google Scholar]
- 145. Torres R, Santos E, Orraca L, Elias A, Palacios C. Diet quality, social determinants, and weight status in Puerto Rican children aged 12 years. J Acad Nutr Diet. 2014;114(8):1230–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. He M, Tucker P, Irwin JD, Gilliland J, Larsen K, Hess P. Obesogenic neighbourhoods: the impact of neighbourhood restaurants and convenience stores on adolescents’ food consumption behaviours. Public Health Nutr. 2012;15(12):2331–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Burke MP, Jones SJ, Frongillo EA, Blake CE, Fram MS. Parenting styles are associated with overall child dietary quality within low-income and food-insecure households. Public Health Nutr. 2019;22(15):2835–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Anderson Steeves E, Jones-Smith J, Hopkins L, Gittelsohn J. Perceived social support from friends and parents for eating behavior and diet quality among low-income, urban, minority youth. J Nutr Educ Behav. 2016;48(5):304–10.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Au LE, Rosen NJ, Fenton K, Hecht K, Ritchie LD. Eating school lunch is associated with higher diet quality among elementary school students. J Acad Nutr Diet. 2016;116(11):1817–24. [DOI] [PubMed] [Google Scholar]
- 150. Santiago-Torres M, Adams AK, Carrel AL, LaRowe TL, Schoeller DA. Home food availability, parental dietary intake, and familial eating habits influence the diet quality of urban Hispanic children. Child Obes. 2014;10(5):408–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Arandia G, Sotres-Alvarez D, Siega-Riz AM, Arredondo EM, Carnethon MR, Delamater AM, Gallo LC, Isasi CR, Marchante AN, Pritchard Det al. Associations between acculturation, ethnic identity, and diet quality among U.S. Hispanic/Latino youth: findings from the HCHS/SOL Youth Study. Appetite. 2018;129:25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Arcan C, Friend S, Flattum CF, Story M, Fulkerson JA. Fill "half your child's plate with fruits and vegetables": correlations with food-related practices and the home food environment. Appetite. 2019;133:77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Horta PM, Verly E Jr, Dos Santos LC. Usual diet quality among 8- to 12-year-old Brazilian children. Cad Saude Publica. 2019;35(2):e00044418. [DOI] [PubMed] [Google Scholar]
- 154. Khan NA, Cannavale C, Iwinski S, Liu R, McLoughlin GM, Steinberg LG, Walk AM. Visceral adiposity and diet quality are differentially associated with cognitive abilities and early academic skills among preschool-age children. Front Pediatr. 2020;7(7):548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Hopkins LC, Tiba S, Westrick M, Gunther C. The diet quality of a sample of predominantly racial minority children from low-income households is lower during the summer vs school year: results from the Project Summer Weight and Environmental Assessment Trial substudy. J Acad Nutr Diet. 2021;121(1):112–20. [DOI] [PubMed] [Google Scholar]
- 156. Jarman M, Vashi N, Angus A, Bell RC, Giesbrecht GF. Development of a diet quality index to assess adherence to Canadian dietary recommendations in 3-year-old children. Public Health Nutr. 2020;23(3):385–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Molina MdCB, Lopéz PM, de Faria CP, Cade NV, Zandonade E. Socioeconomic predictors of child diet quality. Rev Saude Publica. 2010;44(5):785–92. [DOI] [PubMed] [Google Scholar]
- 158. Toffano RBD, Hillesheim E, Mathias MG, Coelho-Landell CA, Salomão RG, Almada M, Camarneiro JM, Barros TT, Camelo-Junior J, Rezzi Set al. Validation of the Brazilian Healthy Eating Index-Revised using biomarkers in children and adolescents. Nutrients. 2018;10(2):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Prado BG, Hinnig PdF, Tanaka LF, Latorre M. Qualidade da dieta de escolares de 7 a 10 anos do município de São Paulo: associação com o número e os locais de refeições. Rev de Nutr. 2015;28(6):607–18. [Google Scholar]
- 160. Burrows TL, Collins K, Watson J, Guest M, Boggess MM, Neve M, Rollo M, Duncanson K, Collins CE. Validity of the Australian Recommended Food Score as a diet quality index for pre-schoolers. Nutr J. 2014;13(1):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Collins LJ, Lacy KE, Campbell KJ, McNaughton SA. The predictors of diet quality among Australian children aged 3.5 years. J Acad Nutr Diet. 2016;116(7):1114–26.e2. [DOI] [PubMed] [Google Scholar]
- 162. Keshani P, Salehi M, Kaveh MH, Faghih S. Self-efficacy and cues to action: two main predictors of modified version of diet quality index in Iranian adolescents. Progr Nutr. 2018;20(2):197–204. [Google Scholar]
- 163. Chamoli R, Jain M, Tyagi G. Reliability and validity of the Diet Quality Index for 7–9-year-old Indian children. Pediatr Gastroenterol Hepatol Nutr. 2019;22(6):554–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Duan R, Qiao T, Chen Y, Chen M, Xue H, Zhou X, Yang M, Liu Y, Zhao L, Libuda Let al. The overall diet quality in childhood is prospectively associated with the timing of puberty. Eur J Nutr. 2021;60(5):2423–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Rezali FW, Chin YS, Mohd Shariff Z, Mohd Yusof BN, Sanker K, Woon FC. Evaluation of diet quality and its associated factors among adolescents in Kuala Lumpur, Nutr Res Pract. 2015;9(5):511–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. da Costa MP, Durão C, Lopes C, Vilela S. Adherence to a healthy eating index from pre-school to school age and its associations with sociodemographic and early life factors. Br J Nutr. 2019;122(2):220–30. [DOI] [PubMed] [Google Scholar]
- 167. Jiang H, Zhao A, Zhao W, Tan S, Zhang J, Zhang Y, Wang P. Do Chinese preschool children eat a sufficiently diverse diet? A cross-sectional study in China. Nutrients. 2018;10(6):794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Mak T-N, Angeles-Agdeppa I, Lenighan YM, Capanzana MV, Montoliu I. Diet diversity and micronutrient adequacy among Filipino school-age children. Nutrients. 2019;11(9):2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Bi J, Liu C, Li S, He Z, Chen K, Luo R, Wang Z, Yu Y, Xu H. Dietary diversity among preschoolers: a cross-sectional study in poor, rural, and ethnic minority areas of Central South China. Nutrients. 2019;11(3):558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Miller LC, Neupane S, Joshi N, Shrestha M, Lohani M, Thorne-Lyman AL. Diet quality over time is associated with better development in rural Nepali children. Matern Child Nutr. 2020;16(3):e12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Supllementary Data are freely available without restriction at https://doi.org/10.1093/advances/nmab148.