Abstract
Aim
To determine the impact of recurrent aphthous stomatitis on quality of life related to oral health, and then to determine the relationship between the observed impact and lesions characteristics.
Methods
In this prospective case-control study (n=62), patients were divided into a healthy group (people with no history of ulcers) and recurrent aphthous stomatitis (people who had an active ulcer at study entry). The latter were also evaluated when the lesion disappeared (remission stage). We record the quality of life in all groups using the impact profile of oral health in its abbreviated Spanish version (OHIP-14SP). Finally, we correlate the clinical characteristics of the lesions with the levels of quality of life.
Results
All the lesions were of the minor morphological type. Most of the lesions were located on the lining mucosa, primarily on the lips. Patients report a lower quality of life during ulcer episodes compared to ulcer-free periods, and this impact is positively related to the number and size of lesions.
Conclusion
We concluded that recurrent aphthous stomatitis increased the negative effects of oral health on the quality of life of patients. The number and size of ulcers are responsible for this impact. Our results suggest that, if intervened locally, general relief of the condition could be achieved.
Keywords: aphthous ulcers, quality of life, health-related quality of life, case-control studies
Introduction
Recurrent aphthous stomatitis (RAS) is the most common disease of the oral mucosa. It is characterized by recurrent, painful, single, or multiple ulcers, with erythematous margins.1
Aphthous ulcerations (or RAS-like ulcerations) have a systemic cause and should be treated as a separate medical condition. Autoinflammatory syndromes, immunodeficiency states, immune defects (such as human immunodeficiency virus infection), and neutrophil defects should be considered as differential diagnoses. RAS refers to ulceration that occurs in the absence of systemic disease.1
The disease sequence comprises several stages, including premonitory, pre-ulcerative, ulcerative, healing, and remission phases.2 The ulcerative phase (presence of active lesions) and remission (without evidence of lesions) are the stages that can be evaluated more objectively in the clinical examination.1
RAS can interfere with important functions such as talking, eating, swallowing, and consequently affect quality of life.3 Quality of life is a concept that refers to the general well-being of an individual, including physical, emotional, and psychological parameters. This concept is often used to describe the impact of a disease or the effects of a medical intervention on general health.4
Despite being a frequent disease, the low number of studies available evaluating the impact of ulcers on quality of life is surprising. In fact, there are only two investigations that evaluate this impact of disease activity, that is, when the lesions are present and then in an ulcer-free period.3,5 However, it is not known whether the local clinical characteristics of the lesions (eg number and size of lesions) could explain the observed impact levels. Therefore, the objective of this research is to determine the impact of RAS on quality of life related to oral health, and secondly to determine the correlation between the observed impact and lesions characteristics.
Materials and Methods
General Design
Our investigation corresponded to a case-control study. In it we evaluate the clinical characteristics of RAS and their impact on quality of life. For this, we record the quality of life reported in healthy people (without a history of ulcers) and people with RAS. Furthermore, in the latter we recorded the quality of life during the disappearance phase of the lesions. Finally, we correlate the clinical characteristics of the lesions with the levels of quality of life. All procedures followed the guidelines of the Declaration of Helsinki6 and Ethics committee/IRB of University of Antofagasta (an accredited committee according to the Chilean National Agency for Research and Development) gave ethical approval for this work (folio 156/2018, date 2018/11/19, https://doi.org/10.6084/m9.figshare.11225900). The informed consent from participants was obtained before starting the study.
Patients
We prospectively evaluated 62 patients in our clinical service (Center of Dental Clinics of the University of Talca) between March and October 2019. The patients were divided into a “healthy” group (n = 29, people with no history of ulcers) and “RAS” (N = 33, people who had an active ulcer at study entry). The latter were also evaluated when the lesion disappeared (n = 33, remission). We conducted a total of 95 clinical examinations.
Inclusion and Exclusion Criteria
To be included, the patients had to present ulcerative lesions with a history of no more than 3 days.7 Furthermore, these lesions must have had an anatomical location that allowed them to be photographed. Exclusion criteria were the use of medications to treat ulcers and the use of topical or systemic corticosteroids. Other exclusion criteria were the presence of other types of lesions of the oral mucosa, diseases that present with acute or chronic pain, smoking, excessive alcohol consumption (more than three times a week)8 and the presence of any of the following 28 conditions at the time of the examination: Behçet syndrome, folic acid deficiency, iron deficiency anemia, vitamin B-12 deficiency, Crohn’s disease, ulcerative colitis, lichen planus, pemphigus, pemphigoid, oral herpes, herpangina, iron deficiency, systemic lupus erythematosus, reactive arthritis, oral candidiasis, celiac disease, cyclic neutropenia, gluten-sensitive enteropathy, malabsorption, pernicious anemia, Sweet’s syndrome, Marshall syndrome, or PFAPA syndrome, trisomy 8, severe periodontal disease, erythema multiforme, syphilis and HIV-AIDS. We do not perform laboratory tests. When the examiners questioned the patients, they self-reported their diagnoses. For their inclusion as controls, volunteers should never have presented oral ulcers, and except for the absence of lesions, this group shared the same inclusion and exclusion criteria. We excluded 4 participants. Two for having herpes virus lesions and two for presenting traumatic ulcers.
Episode Characteristics
Diagnosis was established by a clinical examination by a doctor in oral medicine. We classify the lesions according to the standard pathological nomenclature (minor, major or herpetiform ulcer).9–12 In addition, we asked patients how many episodes of ulcers they suffered in the last year. We recorded the number of lesions present on examination, total ulcerated diameter, mean diameter of lesions, and pain associated with ulcers (using a visual analog scale, VAS).
Quality of Life
We determined the impact of the disease on the quality of life related to oral health in healthy controls and patients with RAS (during the injury and its remission) by applying the impact profile of oral health in its abbreviated Spanish version (OHIP-14SP).13 OHIP-14SP explores seven dimensions: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap. They are evaluated through questions of 5 levels (never, almost never, occasionally, frequently and very frequently) with a score from 0 to 4. The total OHIP score is between the ranges of 0 and 56 points (sum of all the answers). To view the OHIP-14SP questionnaire, see Supplementary Table S1.
Statistical Analysis
We perform a non-probability sampling (convenience sampling). To calculate the sample size, accepting an alpha risk of 0.05 and a beta risk of 0.2 in a two-sided test, a minimum of 28 subjects were necessary in each group to recognize as statistically significant a difference greater than or equal to 0.18 units in OHIP-14sp scores. The common standard deviation was assumed to be 0.2. We assume an eventual drop-out rate of 30%. Results were presented as frequencies and means ± standard deviation. We analyzed the differences between the groups using one-way ANOVA with post hoc Tukey and Games-Howell contrasts. To analyze the association between quantitative variables we used Spearman correlation coefficient. In all procedures we use a confidence level of 95% (p-value ≤ 0.05).
Results
Quality of Life
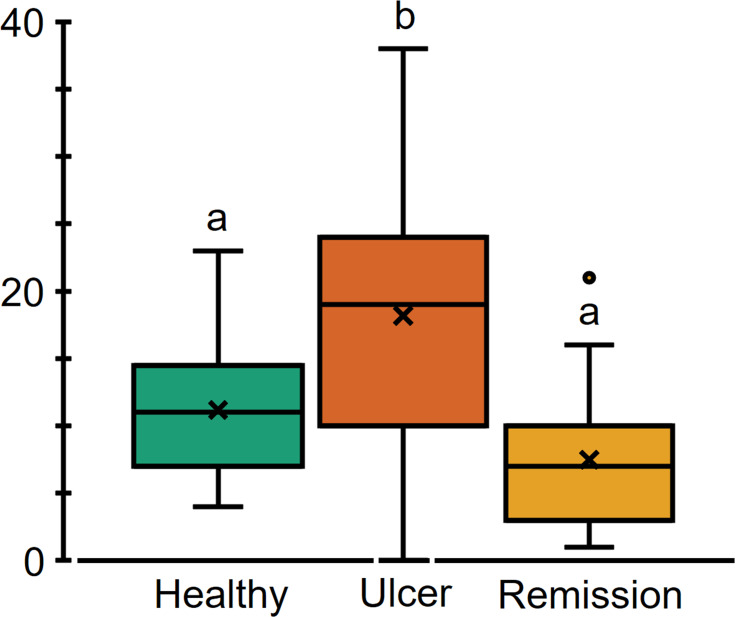
Demographic and clinical characteristics (database) are presented in Supplementary Table S2. We included 62 patients in our research. They were divided into two groups: healthy (n = 29) and RAS (n = 33). The mean age was 26 years for both, with women being the majority (24 and 27 respectively). All the lesions were of the minor morphological type. Most of the lesions were located on the lining mucosa, preferably on the lips. Table 1 shows clinicopathological characteristics associated with presence of ulcers. The RAS group was in turn divided into lesion (active ulcer presented at study entry) and remission (when the lesion disappeared completely). All the participants answered the quality of life questionnaire. The score was noticeably higher when there were lesions (Figure 1).
Table 1.
Characteristics of Recurrent Aphthous Stomatitis Episodes
| Variable | Magnitude |
|---|---|
| Ulcer episodes in the past year | 7.1±5.8 |
| Number of lesions on examination (n) | 1.4±0.7 |
| Total ulcerated diameter (mm) | 3.8±2.0 |
| Mean diameter (mm) | 3.3±1.4 |
| Reported pain (EVA) | 4.2±2.1 |
Notes: Numbers represent means ± standard deviation. Subjects without RAS reported no pain.
Figure 1.
Recurrent aphthous stomatitis affects quality of life. Total OHIP-14Sp score. On the box-and-whisker plot, the boxes represent quartile 1, median, and quartile 3. The x stands for the mean. The whiskers extend to the maximum and minimum values. Data outside of these limits represents outliers. The different letters indicate a statistically significant difference (p-value <0.05, one-way ANOVA with Tukey’s post hoc contrasts).
Distribution of OHIP-14Sp in the Presence and Absence of Oral Ulcers
Table 2 illustrates the distribution of OHIP-14Sp scores in the healthy and RAS groups. In general, the presence of lesions presents higher means when compared with subjects in healthy and in remission. It is striking that healthy patients have greater difficulty resting, which can be explained because they were mainly university students).
Table 2.
Scores of the OHIP-14SP Items
| OHIP-14Sp | Healthy | Ulcer | Remission |
|---|---|---|---|
| Functional limitation | |||
| Difficulty pronouncing words | 0.3±0.1 | 0.7±0.2a | 0.1±0.1b |
| Worst taste of food | 0.3±0.1 | 0.7±0.2a | 0.0b |
| Physical pain | |||
| Pain in the mouth | 0.3±0.1a | 3.0±0.2b | 0.3±0.2a |
| Discomfort when eating | 0.2±0.1a | 2.7±0.2b | 0.3±0.2a |
| Psychological distress | |||
| Concern for oral problems | 1.9±0.3 | 2.7±0.2 | 2.1±0.2 |
| Feel stress | 2.9±0.2 | 2.3±0.3 | 2.2±0.3 |
| Physical disability | |||
| Change foods | 0.9±0.2 | 0.9±0.2 | 0.5±0.2 |
| Interrupt food | 0.7±0.2 | 1.0±0.2a | 0.2±0.1b |
| Psychological disability | |||
| Difficulty resting | 2.3±0.2a | 1.3±0.2b | 0.9±0.2b |
| Shame about oral problems | 0.34±0.2 | 0.4±0.2 | 0.3±0.1 |
| Social disability | |||
| Irritable due to oral problems | 0.1±0.1a | 1.0±0.2b | 0.4±0.1a |
| Difficulty performing daily activities | 0.2±0.1 | 0.7±0.2a | 0.1±0.0b |
| Handicap | |||
| Less pleasant life | 0.6±0.2 | 0.8±0.2a | 0.2±0.1b |
| Unable to perform daily activities | 0.0 | 0.1±0.1 | 0.0 |
Notes: Numbers represent means ± standard deviation. Different letters a, bIndicate a statistical difference (p <0.05, one-way ANOVA with post hoc Games-Howell contrasts).
OHIP-14Sp Dimensions and Lesion Characteristics
Table 3 shows the relationship between the OHIP-14Sp items altered by the presence of RAS and the clinicopathological variables evaluated in the ulcers. The mean size of the lesions in the oral mucosa and the number of ulcers are the clinical variables that are best related to pain in the mouth, discomfort when eating and irritability.
Table 3.
Relationship between Affected Dimensions and Lesions' Clinical Features
| OHIP-14Sp | Spearman Correlation Coefficient | ||
|---|---|---|---|
| Number of Ulcers | Ulcerated Total Diameter | Mean Size | |
| Mouth pain | 0.8** | 0.5** | 0.8** |
| Discomfort when eating | 0.7** | 0.6** | 0.8** |
| Irritable due to oral problems | 0.4** | 0.4* | 0.5** |
Notes: Degree of relationship between dimensions affected by recurrent aphthous stomatitis and clinical characteristics of lesions. A coefficient equal to or greater than 0.8 indicates a good correlation. **Correlation is significant at p-value <0.01 and *p-value <0.05.
Discussion
Quality of life assessments have an important place in health care. In recent years, they have become an accepted end point in clinical research trials.5 Individual perceptions of the impact profile on oral health have grown in importance and may have a direct effect on people’s health-related quality of life.14 We are interested in evaluating the impact of RAS on the quality of life of those who suffer from it, to establish firstly whether the impact depends on the activity of the disease and secondly whether this effect may be associated with some local characteristic of injuries. In our study, we discovered that RAS has a negative impact on quality of life, causing pain that is primarily related to the number of ulcers and the mean size of lesions.
Patients reported presenting more than 7 episodes of ulcers per year. Considering that these lesions resolve in an approximate period of 2 weeks, a participant may be more than 27% of a current year with the discomforts that are associated with the disease. This emphasizes the need to pay attention to how ulcers compromise well-being.
Our sample is representative of the reality reported for this disease in the world. All of our participants presented minor lesions located on non-keratinized mucosa, mainly on the lips. This is the most frequent and least severe ulcer form.14 They are generally located on the lips, tongue, and oral vestibule.15 The fact that our patients correspond to the classically described pattern allows us to trust that the conclusions obtained from our data can be extrapolated to other populations.
RAS affected the quality of life of patients. To evaluate the effect of the lesions, we used the OHIP-14 scale. This is the most widely used instrument to assess the impact of oral health on quality of life.16 Along with examining healthy subjects as a basis, we applied the questionnaire in two disease periods, when lesions were present and then in the remission phase. Measuring the quality of life in different states of ulcer activity in the same subjects allowed us to have a better control of the design, since the changing condition is the presence or absence of the lesions. This provides a correct and isolated measure of the effects of ulcers.3
Notoriously, presence of RAS obtained much higher OHIP-14 scores, compared to healthy subjects and subjects whose ulcers disappeared. Five articles have previously evaluated the impact of RAS on quality of life, all finding a negative effect.3,5,17–19 Of these, 2 performed it in active lesions and in ulcer-free periods.3,5 Like us, they observed that the quality of life associated with oral health when ulcers are present is significantly lower. In this way, we went further in trying to understand what the impact is due to. Our findings showed that RAS caused pain, discomfort when eating, and irritability. This was positively associated with the number of ulcers present in the oral mucosa and average size of lesions. The impact was greater, while the number of ulcers and their size was also. This result shows that, if the condition caused by oral ulcers is to be improved, therapeutic measures must be focused on treating the local compromise of oral mucosa. Unfortunately, the evidence available today for the successful management of lesions is insufficient, both for topical and systemic treatments.20,21
Our results are limited to the fact that the impact of the lesions was essentially measured with self-reports obtained from an instrument that was designed for dental diseases and not for oral mucosa. New methods are being developed to evaluate the affection produced by mucosal lesions.22 However, its extension has not reached the use of OHIP-14. Another of our limitations was not performing blood tests to rule out systemic states. This leaves the door open for admission of RAS-like ulcerations, despite clinical examination.
Conclusion
We concluded in this study that RAS exacerbated the negative effects of oral health on patients’ quality of life. This effect is caused by the number and size of lesions. Intervening on these local characteristics could help affected patients with pain, eating difficulties, and irritability.
Acknowledgments
We want to thank all the volunteers who actively participated in this research, despite the national social context and the global pandemic, and the University Dental Clinic Center for hosting us. We would like to express our gratitude to Colgate-Palmolive Chile for providing oral hygiene kits to our volunteers. We also want to give special recognition to the TENS Yennifer Lemus. This research was funded by the Chilean National Agency for Research and Development (ANID) FONDECYT Iniciación grant number #11180170 (to C.R.) and Concurso de Proyectos de Investigación de Alto Nivel en Odontología, Red Estatal de Odontología grant number #REO19–012 (to C.R.).
Disclosure
All the authors declare that they have no conflicts of interest in relation to this work.
References
- 1.Rivera C. Essentials of recurrent aphthous stomatitis (Review). Biomed Rep. 2019;11(2):47–50. doi: 10.3892/br.2019.1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vucicevic Boras V, Savage NW. Recurrent aphthous ulcerative disease: presentation and management. Aust Dent J Mar. 2007;52(1):10–5; quiz 73. doi: 10.1111/j.1834-7819.2007.tb00459.x [DOI] [PubMed] [Google Scholar]
- 3.Al-Omiri MK, Karasneh J, Alhijawi MM, Zwiri AM, Scully C, Lynch E. Recurrent aphthous stomatitis (RAS): a preliminary within-subject study of quality of life, oral health impacts and personality profiles. J Oral Pathol Med. 2015;44(4):278–283. doi: 10.1111/jop.12232 [DOI] [PubMed] [Google Scholar]
- 4.Nature. Latest research and news by subject: quality of life; 2019. Avaialble from: https://www.nature.com/subjects/quality-of-life. Accessed November 22, 2019.
- 5.Mumcu G, Inanc N, Ergun T, et al. Oral health related quality of life is affected by disease activity in Behcet’s disease. Oral Dis. 2006;12(2):145–151. doi: 10.1111/j.1601-0825.2005.01173.x [DOI] [PubMed] [Google Scholar]
- 6.Mundial AM. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 7.Liu C, Zhou Z, Liu G, et al. Efficacy and safety of dexamethasone ointment on recurrent aphthous ulceration. Am J Med. 2012;125(3):292–301. doi: 10.1016/j.amjmed.2011.09.011 [DOI] [PubMed] [Google Scholar]
- 8.Bankvall M, Sjoberg F, Gale G, Wold A, Jontell M, Ostman S. The oral microbiota of patients with recurrent aphthous stomatitis. J Oral Microbiol. 2014;6:25739. doi: 10.3402/jom.v6.25739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bagan JV, Sanchis JM, Milian MA, Penarrocha M, Silvestre FJ. Recurrent aphthous stomatitis. A study of the clinical characteristics of lesions in 93 cases. J Oral Pathol Med. 1991;20(8):395–397. doi: 10.1111/j.1600-0714.1991.tb00952.x [DOI] [PubMed] [Google Scholar]
- 10.Porter SR, Scully C, Pedersen A. Recurrent aphthous stomatitis. Crit Rev Oral Biol Med. 1998;9(3):306–321. doi: 10.1177/10454411980090030401 [DOI] [PubMed] [Google Scholar]
- 11.Akintoye SO, Greenberg MS. Recurrent aphthous stomatitis. Dent Clin North Am. 2014;58(2):281–297. doi: 10.1016/j.cden.2013.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scully C, Gorsky M, Lozada-Nur F. The diagnosis and management of recurrent aphthous stomatitis: a consensus approach. J Am Dent Assoc. 2003;134(2):200–207. doi: 10.14219/jada.archive.2003.0134 [DOI] [PubMed] [Google Scholar]
- 13.Montero-Martin J, Bravo-Perez M, Albaladejo-Martinez A, Hernandez-Martin LA, Rosel-Gallardo EM. Validation the Oral Health Impact Profile (OHIP-14sp) for adults in Spain. Med Oral Patol Oral Cir Bucal. 2009;14(1):E44–E50. [PubMed] [Google Scholar]
- 14.Zucoloto ML, Maroco J, Campos JA. Impact of oral health on health-related quality of life: a cross-sectional study. BMC Oral Health. 2016;16(1):55. doi: 10.1186/s12903-016-0211-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edgar NR, Saleh D, Miller RA. Recurrent aphthous stomatitis: a review. J Clin Aesthet Dermatol. 2017;10(3):26–36. [PMC free article] [PubMed] [Google Scholar]
- 16.Bettie NF, Ramachandiran H, Anand V, Sathiamurthy A, Sekaran P. Tools for evaluating oral health and quality of life. J Pharm Bioallied Sci. 2015;7(Suppl 2):S414–9. doi: 10.4103/0975-7406.163473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang C, Liu L, Shi H, Zhang Y. Psychological problems and quality of life of patients with oral mucosal diseases: a preliminary study in Chinese population. BMC Oral Health. 2018;18(1):226. doi: 10.1186/s12903-018-0696-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zwiri AM. Anxiety, depression and quality of life among patients with recurrent aphthous ulcers. J Contemp Dent Pract. 2015;16(2):112–117. doi: 10.5005/jp-journals-10024-1646 [DOI] [PubMed] [Google Scholar]
- 19.Lopez-Jornet P, Camacho-Alonso F, Lucero Berdugo M. Measuring the impact of oral mucosa disease on quality of life. Eur J Dermatol. 2009;19(6):603–606. doi: 10.1684/ejd.2009.0762 [DOI] [PubMed] [Google Scholar]
- 20.Staines K, Greenwood M. Aphthous ulcers (recurrent). BMJ Clin Evid. 2015;2015:1303. [PMC free article] [PubMed] [Google Scholar]
- 21.Brocklehurst P, Tickle M, Glenny AM, et al. Systemic interventions for recurrent aphthous stomatitis (mouth ulcers). Cochrane Database Syst Rev. 2012;(9):Cd005411. doi: 10.1002/14651858.CD005411.pub2 [DOI] [PubMed] [Google Scholar]
- 22.Tappuni AR, Kovacevic T, Shirlaw PJ, Challacombe SJ. Clinical assessment of disease severity in recurrent aphthous stomatitis. J Oral Pathol Med. 2013;42(8):635–641. doi: 10.1111/jop.12059 [DOI] [PubMed] [Google Scholar]