Abstract
Background and Purpose—
African Americans suffer disproportionately higher cardiovascular disease mortality rates than do whites. Psychosocial stress influences the development and progression of atherosclerosis. Carotid intima-media thickness (IMT) is a valid surrogate measure for coronary atherosclerosis, is a predictor of coronary outcomes and stroke, and is associated with psychosocial stress factors. Stress reduction with the Transcendental Meditation (TM) program decreases coronary heart disease risk factors and cardiovascular mortality in African Americans. B-mode ultrasound is useful for the noninvasive evaluation of carotid atherosclerosis.
Methods—
This randomized controlled clinical trial evaluated the effects of the TM program on carotid IMT in hypertensive African American men and women, aged >20 years, over a 6- to 9-month period. From the initially enrolled 138 volunteers, 60 subjects completed pretest and posttest carotid IMT data. The assigned interventions were either the TM program or a health education group. By use of B-mode ultrasound, mean maximum IMT from 6 carotid segments was used to determine pretest and posttest IMT values. Regression analysis and ANCOVA were performed.
Results—
Age and pretest IMT were found to be predictors of posttest IMT values and were used as covariates. The TM group showed a significant decrease of −0.098 mm (95% CI −0.198 to 0.003 mm) compared with an increase of 0.054 mm (95% CI −0.05 to 0.158 mm) in the control group (P=0.038, 2-tailed).
Conclusions—
Stress reduction with the TM program is associated with reduced carotid atherosclerosis compared with health education in hypertensive African Americans. Further research with this stress-reduction technique is warranted to confirm these preliminary findings.
Keywords: atherosclerosis, blacks, carotid arteries, stress, ultrasonography
African Americans suffer disproportionately higher total mortality rates than do whites.1,2 Cardiovascular diseases (CVDs), in particular, coronary heart disease (CHD) and stroke, are the major contributors to this differential. Prevalence of CHD is ≈50% higher3–5 and mortality rates for stroke6,7 are 4 to 5 times higher in African Americans than in whites. Hypertension is also disproportionately high in African Americans and is a major contributor to their risk for atherosclerotic CVD mortality.8,9 Psychosocial stress has been reported to influence the development and progression of atherosclerosis in the general population,10–13 as well as in African Americans,14 and may explain part of the differential cardiovascular and cerebrovascular mortality rates.15 In general, studies on a range of stress-reduction techniques in whites have demonstrated significant decrease in cardiac events in patients with myocardial ischemia,16 but they do not report effects on prevalent or incident stroke nor do they evaluate the high-risk African American population. However, the Transcendental Meditation (TM) program has been found to decrease CHD risk factors, including hypertension, and associated cardiovascular morbidity and mortality in African Americans17,18 and in the general population.19,20
Population-based21–23 and intervention studies24–26 have shown that carotid intima-media thickness (IMT) measured by B-mode ultrasound is a valid and reliable surrogate measure of coronary atherosclerosis.27 Carotid IMT is a significant predictor of coronary outcome28–30 and of prevalent31 and incident stroke29 and correlates with traditional32–34 and psychosocial cardiovascular risk factors in the general population.13,35–37 Carotid IMT is higher in African Americans than in whites38–40; this finding represents an increased risk for clinical CHD, stroke,29 and death.29,32 There are several demonstrated advantages of B-mode ultrasound over angiography: (1) being noninvasive, B-mode ultrasound is especially suitable for stress-reduction studies; (2) it provides information in asymptomatic individuals; (3) it allows evaluation of early stages of the arterial disease process; (4) it provides a continuous measure for statistical analysis; and (5) compared with angiography, B-mode ultrasound requires a smaller sample size.27,41
The present study hypothesizes that stress reduction through use of the TM program compared with a health education comparison group will regress or slow progression of carotid atherosclerosis as measured by B-mode ultrasound in a population of high-risk hypertensive urban African Americans.
Subjects and Methods
The present study was an ancillary study to a larger randomized clinical trial comparing a stress-reduction intervention, the TM technique, with a heart disease education comparison group for the treatment of hypertensive heart disease in African Americans. Subjects were tested for primary and secondary outcomes at baseline and had an intervention period after randomization of 6 to 9 months. One hundred thirty-eight men and women aged >20 years, self-identified as African American and residing in Los Angeles, with high normal blood pressure (130 to 139 mm Hg systolic blood pressure [SBP] and 80 to 85 mm Hg diastolic blood pressure [DBP]), stage 1 hypertension (140 to 159 mm Hg SBP and 90 to 99 mm Hg DBP), or stage II hypertension (160 to 179 mm Hg SBP and 100 to 109 mm Hg DBP) were recruited through local radio and press advertising and from community organizations. They were eligible whether or not they were taking antihypertensive medication and independent of the duration of hypertension. Candidates were excluded if they had evidence of complications due to CVD (eg, personal history of myocardial infarction, stroke, coronary artery bypass graft, or percutaneous transluminal coronary angiography) or other life-threatening or disabling illnesses. All subjects gave informed consent and had the approval of their primary care physicians. The study was approved by institutional review boards at King/Drew Medical Center and Maharishi University of Management.
B-mode carotid ultrasound scanning for all subjects was performed with a Toshiba 140 transducer by one of the coauthors (R.C.) after a modification of the Asymptomatic Carotid Artery Progression Study (ACAPS) protocol for carotid evaluation.41,42 Measurements of IMT were taken from the far wall at the level of the distal 2 cm of the common carotid, the bulb, and the proximal 1 cm of the internal carotid arteries on both sides. Far wall measurements were chosen in accordance with methodological recommendations and their reported use in clinical trials because the far wall is more easily and consistently visualized than the near wall.28,43 The primary outcome was IMT, defined as the distance between the intima-lumen and media-adventitia interfaces at end diastole. IMT was observed and manually marked for 5 to 8 cycles, controlled by ECG. Three measurements were taken from each segment, and the average value was included as the maximum IMT score for that carotid segment. Whenever plaque was identified, 3 measurements were taken, and the mean value was included as the maximum IMT score for that particular carotid segment. Reading of these data was done on-line by the radiologist performing the scanning, and images were stored on S-VHS tape. The mean maximum IMT of the 6 segments was used for data analysis, which has been found to give less variability than single maximum measures.44 These combined measures of common and internal carotid IMT are also as strong predictors of cardiovascular events as traditional risk factors.29
Secondary outcomes included blood pressure, weight, and lipids. Clinic blood pressure taken with a random-zero sphygmomanometer was measured 3 times per visit during 3 consecutive baseline visits, and the average of the last 2 visits was recorded. Blood pressure evaluations were performed at approximately the same time of day whenever possible. Weight was taken during 2 different baseline visits, and the average of the 2 measurements was recorded. After 12-hour overnight fasting blood samples were drawn, they were stored under freezing conditions for lipid analysis. No evaluation of blood glucose was performed. Other behavioral factors, such as exercise (hours per week) and the number of cigarettes smoked per day, were evaluated at pretest and posttest as part of the major ongoing trial.
Interventions
After baseline evaluations were performed, the participants were randomly assigned to 1 of 2 treatment groups: (1) the TM program and (2) a CVD risk factor prevention education program. The TM technique is a simple, natural, and effortless mental technique practiced 20 minutes twice a day with the participant sitting comfortably with eyes closed. The TM technique is considered the principal approach for stress reduction and self-development of Maharishi Vedic Medicine,45 a comprehensive, prevention-oriented system of natural health care traditionally derived from the ancient Vedic approach to health. During the TM technique, the ordinary thinking process becomes less active or quiescent, and a distinctive psychophysiological state of “restful alertness” appears to be gained.46–49 The prevention education program was modeled after the Treatment of Mild Hypertension Study protocol.50 Both groups were matched for teaching format, instructional time, home practice (20 minutes twice a day), and expectancy of beneficial outcomes. Neither group required change in personal beliefs. Number and length of meetings were similar in both groups. Initial instruction occurred over 1 week. Follow-up meetings after instruction were set up 1 week later, then every 2 weeks for 2 months, and then once a month for 3 months. Instruction in both programs was given by certified instructors from the African American community. The TM program involved an introductory lecture to discuss the benefits and mechanics of the technique, a brief interview, and a session of personal instruction, after which the participant joined small group meetings. These meetings were not designed to generate social support but to evaluate and clarify different aspects of the TM practice. For the health education group, participants received didactic instruction and group support for modifying major cardiovascular risk factors through nonpharmacological means. Their 20-minute home practice involved personal time dedicated to any leisure activity (eg, reading and exercising). The format involved materials and structured presentations specifically implemented for African Americans.
Data Analysis
Baseline characteristics of the 2 groups were compared by ANOVA. Baseline factors included age, sex, weight, blood pressure, pulse, pulse pressure, medication status, total cholesterol, HDL, LDL, smoking (cigarettes per day), exercise (hours per week), and carotid IMT. The mean IMT of 6 carotid segments was used to determine pretest and posttest IMT values. Change in IMT (posttest minus pretest) was used for data analysis. Regression analysis was performed for all variables. ANCOVA for change in IMT scores was performed by using as covariates those variables found to be predictors of IMT change—age and pretest IMT. A separate ANCOVA was performed by using antihypertensive medication and smoking status to account for possible effects of these variables on IMT change. Intent-to-treat analysis was performed by using the group mean change for all missing values. The significance level was set at P<0.05 (2-tailed).
Randomization
Volunteer subjects from the parent trial were consecutively included in the carotid atherosclerosis study until the end of the recruitment phase. Subjects in the parent trial were randomly assigned to the 2 treatment groups with stratification by age, sex, mean arterial pressure, left ventricular mass index, and use of antihypertensive medication at baseline. Randomization was performed according to a computer-generated table, which randomly assigned consecutive pairs of subjects in each stratum in order to place members of a pair into different treatment groups. This ensured that the strata were evenly distributed between the 2 groups. Blinding of the participants’ treatment assignments was maintained during scanning and reading of the B-mode ultrasound. All data collection staff were blinded to the treatment status of the participants. The project manager notified the participants of their treatment assignment.
Results
Of the 170 subjects randomized into the parent trial, 138 volunteered to participate in the ancillary IMT study, and after an average intervention period of 6.8±1.3 months, 62 subjects completed posttest B-mode ultrasound evaluations. Two subjects were excluded because of unreadable scannings. Results are described for 60 subjects with complete pretest and posttest data on carotid IMT. There was no significant difference in the intervention period between the 2 treatment groups. Fiscal restrictions precluded completion of posttest evaluation for all subjects, with ≈56.5% of subjects not completing posttest measures. The measurements of carotid IMT, blood pressure, and other variables were obtained simultaneously at baseline and the end of the treatment phase. No differences were found between those not completing the study (attriters) and nonattriters in baseline characteristics. No differences before the start of the treatment regimen were found in demographics, blood pressure, pulse, pulse pressure, and weight between treatment and health education groups (see Table 1).
TABLE 1.
Baseline Characteristics
| Variable | TM Group (n = 31) | Health Education Group (n = 29) | P * |
|---|---|---|---|
|
| |||
| Age, y | 55.2±9.2 | 52.5±10.9 | 0.30 |
| Sex, % male | 29.03 | 34.48 | 0.1† |
| SBP, mm Hg | 145.5±13.2 | 149.9±13.7 | 0.20 |
| DBP, mm Hg | 83.4±9.9 | 87.6±12.2 | 0.15 |
| Pulse, bpm | 76.98±10.6 | 75.14±10.7 | 0.51 |
| Pulse pressure, mm Hg | 62.13±17.1 | 62.36±17.2 | 0.96 |
| Antihypertensive medication, % | 67.7 | 72.4 | 0.1† |
| Weight, lb | 196.6±33.6 | 194.2±40.4 | 0.8 |
| Total cholesterol, mg/dL | 216.6±41.7 | 220.6±47.82 | 0.76 |
| HDL-C, mg/dL | 55.24±18.5 | 49.55±11.4 | 0.23 |
| LDL-C, mg/dL | 136.76±37.1 | 142.98±38.2 | 0.58 |
| Smoking, cigarettes/d | 1.37±4.6 | 0.73±3.7 | 0.56 |
| Exercise, h/wk | 6.97±4.5 | 8.0±4.5 | 0.38 |
| Carotid IMT, mm | 1.57±0.35 | 1.52±0.38 | 0.64 |
Values are mean±SD and percentage (as indicated). HDL-C indicates HDL cholesterol; LDL-C, LDL cholesterol.
Level of significance is P<0.05.
Based on χ2 analysis.
ANCOVA for IMT-change scores, with pretest IMT and age used as covariates, indicated that the TM group showed a significant decrease in IMT compared with the health education control group. The TM group showed an adjusted mean change of −0.098 mm (95% CI −0.198 to 0.003 mm) compared with 0.05 mm (95% CI −0.05 to 0.158 mm) (P=0.038), giving a relative mean adjusted difference of −0.15 mm between groups (see Figure). Thirty-seven subjects (61.7%) were receiving antihypertensive medication at pretest, and 18 reported changes in their medication status. Differences between the 2 groups were not significant. Results remained significant when covarying for changes in antihypertensive medication and smoking (P=0.027). Only 2 subjects from the health education group reported use of lipid-lowering medication at pretest and posttest. No differences between groups were found in other measures, including blood pressure, pulse, pulse pressure, lipids, total cholesterol/HDL ratio, weight, smoking (cigarettes per day), and exercise (hours per week). Intent-to-treat analysis using the mean change for the whole group (−0.02±0.3 mm) in place of missing values confirmed differences in change in IMT between the 2 groups (P=0.049). The number of intervention meetings attended was significantly higher in the TM group (78.9%) than in the health education group (61.9%) (P=0.025). Correlation between attendance to meetings and change in IMT scores was significant for the TM group (r=−0.42, P=0.018) but not for the health education group (r=−0.11, P=0.56).
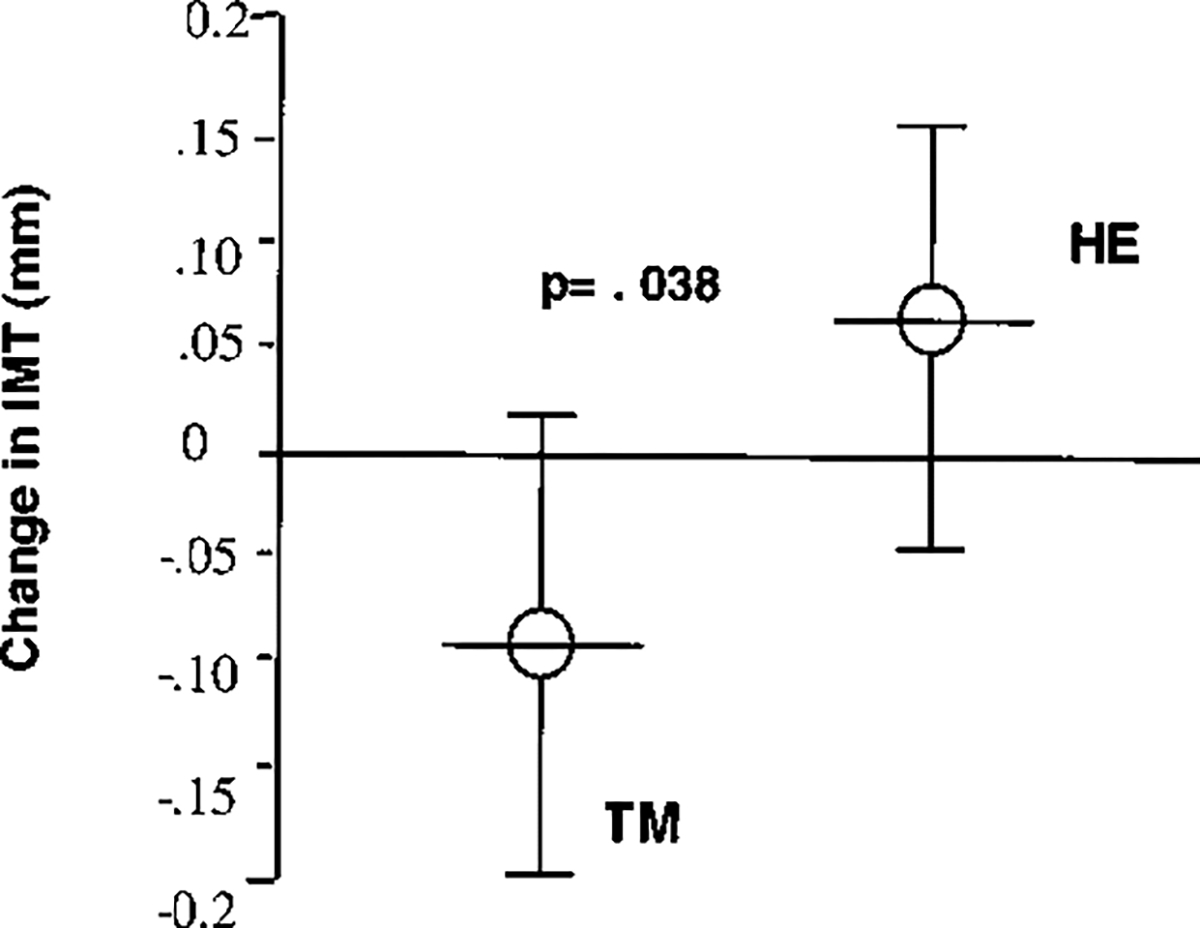
Comparative effects of TM and health education (HE) on carotid IMT in hypertensive African Americans. Graph shows mean change in IMT scores and 95% CI.
As seen on Table 2, the TM group showed statistically significant within-group changes in SBP, DBP, pulse, and pulse pressure. The health education group showed significant reduction in SBP and DBP.
TABLE 2.
Changes in Intermediate Variables
|
P
|
||||
|---|---|---|---|---|
| Variable | Groups | Within-Group–Change Scores | Within Group | Between Group |
|
| ||||
| SBP, mm Hg | TM | −7.77 ±10.34 | 0.0003* | 0.25 |
| HE | −6.74 ±12.8 | 0.01* | ||
| DBP, mm Hg | TM | −3.5 ±7.6 | 0.02* | 0.5 |
| HE | −5.9 ±8.6 | 0.001* | ||
| Pulse, bpm | TM | −3.88 ±10.97 | 0.01* | 0.59 |
| HE | −3.0 ±11.24 | 0.16 | ||
| Pulse pressure, mm Hg | TM | −4.26 ±9.02 | 0.02* | 0.13 |
| HE | −0.84 ±9.5 | 0.63 | ||
| Total cholesterol, mg/dL | TM | 2.8 ±25.16 | 0.58 | 0.69 |
| HE | 5.36 ±38.1 | 0.53 | ||
| HDL-C, mg/dL | TM | −1.64 ±7.9 | 0.31 | 0.28 |
| HE | 2.74 ±12.0 | 0.31 | ||
| LDL-C, mg/dL | TM | 2.14 ±20.3 | 0.6 | 0.86 |
| HE | 1.79 ±36.46 | 0.82 | ||
| Weight, lb | TM | −1.02 ±7.98 | 0.48 | 0.48 |
| HE | −3.34 ±17.7 | 0.32 | ||
| Smoking, cigarettes/d | TM | −0.5 ±2.74 | 0.33 | 0.35 |
| HE | 0.17 ±1.7 | 0.59 | ||
| Exercise, h/wk | TM | −0.44 ±4.47 | 0.63 | 0.3 |
| HE | −2.39 ±6.38 | 0.05* | ||
Values are mean±SD.
All coefficients significant at P<0.05.
Discussion
This preliminary randomized controlled trial suggests that stress reduction with the TM program is associated with reduced carotid atherosclerosis in African Americans with hypertension compared with a health education comparison group. Fiscal constraints on posttesting, high residential mobility, and scheduling conflicts were the main reasons for a high attrition rate. Although the generalizability of our findings may appear to be compromised by the attrition rate, attriters and completers were not found to be different in baseline characteristics that would systematically bias treatment outcomes. Moreover, both the TM group (56.3%) and the health education group (56.7%) (P=0.94 for difference between groups) were equally affected by attrition, reducing potential subject bias in the final sample. Given the change in IMT, the number of subjects in our pilot study was sufficient to indicate differences between the 2 groups.
The parent trial from which the present study drew its subjects did not include evaluation of diabetes as a risk factor or lipid peroxidation in the progression of carotid atherosclerosis; therefore, these factors cannot be ruled out. Future studies will address these issues.
The sex distribution in the present study sample reflects the population of other clinical trials with African Americans.17,18 A low proportion of male participants may limit the generalizability of our findings, but they were equally distributed in the TM group (n=9) and the health education group (n=10) without affecting the observed IMT difference between groups. The analysis by sex strengthened the difference in change in IMT scores between groups (P=0.017). The effect of hormonal replacement therapy in the women’s subgroup was minimal because only 3 women in the TM group and 2 in the health education group were receiving estrogen.
Conceivably, observed differences in outcomes may have been due to differing compliance rates rather than the effect of the experimental treatment per se. Compliance is considered an outcome of treatment, because patients will naturally tend to comply with a behavioral intervention if they perceive that it is beneficial to them. With regard to the interventions in this trial, the TM technique has been shown in previous studies to reduce stress and to deliver perceivable improvements in physical health.17,51–53 On the other hand, the health education comparison group did not practice any stress-reduction technique and received only didactic instruction in the benefits of lifestyle changes. Higher compliance rates in the experimental group may therefore be due to the intrinsic nature of the treatments rather than differences in motivation of subjects in the groups. Moreover, examining correlations between attendance at meetings and change in IMT scores revealed that a significant dose-response relation existed within the TM group but not within the health education group. Therefore, it is unlikely that had compliance rates been higher in the health education group, more favorable outcomes would have been obtained in that group. More likely, differences in treatment outcomes are not reflecting differences in compliance levels. The dose-response relation found in the TM group is consistent with the hypothesis that changes were due to TM practice rather than nonspecific treatment effects, such as subjects’ expectations or experimenter influences.
The manual IMT measurements and readings used in the present study have been replaced recently by more precise computerized tracking.24,54 We made all attempts to preserve the consistency of our readings, but this difference may explain relatively higher IMT values in the present study compared with computerized measurements in clinical trials.24,26,55 B-mode ultrasound is a valuable tool for noninvasive assessment of carotid atherosclerosis even in its early stages of development.24,55 Carotid IMT measured by B-mode ultrasonography is widely used in clinical trials because of its associations with prevalence and incidence of CVD and stroke28–30 and with traditional cardiovascular risk factors, including hypertension, hyperlipidemia, obesity, and diabetes.32–34 In our protocol, we used a summary outcome measure of 6 different segments of the carotid wall similar to that used in ACAPS.42 To maintain reproducibility and decrease variability throughout the study, we retained the same sonographer, and we used mean maximum IMT as our primary outcome measure. Using the same sonographer minimizes interrater variability, which is considered to be the main cause of measurement variation.56 Reported intraobserver reproducibility is 0.97.57 Mean maximum IMT is considered more reliable than single maximum measure because it also reduces intrarater variability and increases statistical power, whereas single maximum IMT differs according to the various carotid locations, thus decreasing reproducibility.44 Compared with individual measures, mean maximum IMT is also a stronger predictor for CVD outcome.29,58
Our mean IMT baseline value is in the same range as the baseline IMT reported for the Northern Manhattan Stroke Study (NOMASS) African American subgroup.59 The annual progression rate found in our comparison group is similar to that of the placebo group of the Pravastatin, Lipids, and Atherosclerosis in the Carotid Arteries (PLAC-II) study involving coronary artery disease patients.26 The reduction of 0.098 mm in our stress-reduction group, practicing the TM technique, is within the range of reduction shown by lipid-lowering medications27 and intensive lifestyle modification programs.60 Based on the observation of Salonen and Salonen56 that a 0.1-mm increase in IMT would raise the risk of acute myocardial infarction by 11%, the change in our treatment group of −20.098 mm would indicate a decrease in the risk of myocardial infarction by approximately the same percentage. Similarly, based on the observation of O’Leary et al29 of the correlation between IMT and incidence of stroke, a reduction of 0.1-mm IMT would represent a 7.7% to 15% reduction in risk of stroke. With the use of different approaches, recent studies on stress-reduction programs with behaviorally oriented interventions in white populations have found a positive impact on cardiovascular morbidity and mortality.16 These studies have focused on tertiary prevention of atherosclerotic disease and have used cardiac events, including CVD mortality, as end points. Studies on the effects of stress reduction on stroke have not been reported.
Our results are consistent with other findings that describe the effects of TM on the cardiovascular system. The changes found in the present study may be related to several accelerated homeostatic and self-repair processes acting in concert to halt early atherosclerotic pathological mechanisms. A likely mechanism explaining the reduction of IMT of the carotid wall is the decrease in excessive sympathetic nervous system activation. Evidence indicates that chronic psychosocial stress induces excessive adrenergic activation and sympathetic hyperresponsivity, leading to carotid atherosclerosis.61–63 In the present study, stress reduction with either TM or changes in diet and exercise led to statistically significant declines in blood pressure within each group. Decrease in blood pressure in the control group, however, was not associated with a corresponding decrease in IMT. In the TM group, improved arterial compliance reflected in the reduction of pulse pressure together with changes in blood pressure and heart rate may have had hemodynamic effects that influenced the observed IMT reduction. These results support previous findings that describe pulse pressure as a strong predictor of carotid atherosclerosis23 and suggest a reduction in sympathetic activation with the practice of the TM program.64,65
From the perspective of Maharishi Vedic Medicine, stress and disease arise from a lack of integration of the various physiological systems with the holistic “inner intelligence” of the body.45 This may result in loss of homeostasis in the cardiovascular system that could be expressed as higher blood pressure or increased atherosclerosis. The practice of the TM technique may involve a set of adaptive responses at the cortical, autonomic, neuroendocrine, and cardiovascular levels that would restore homeostatic and self-repair mechanisms.20,47,64 Further research on the effects of TM and the regression of atherosclerosis may help verify the proposed mechanistic hypotheses.
The present study evaluated the effects of a stress-reduction technique on atherosclerosis in African Americans at high risk of cardiovascular complications. The results have potentially important implications for the prevention and treatment of atherosclerosis and its clinical and epidemiological consequences. These preliminary findings are followed up by a larger National Institutes of Health–funded randomized controlled trial in African Americans currently in progress that will further evaluate these results and address questions concerning the long-term efficacy of stress-reduction techniques.
Acknowledgments
This study was supported by National Heart, Lung, and Blood Institute grants HL-51519 to Drs Schneider, Alexander, and Myers and HL-51519-S2 to Dr Castillo-Richmond. We thank Elizabeth Barrett-Connor, MD, and Paul McGovern, PhD, for their valuable comments on a previous version of this manuscript.
Contributor Information
Amparo Castillo-Richmond, Center for Natural Medicine and Prevention, Maharishi University of Management, College of Maharishi Vedic Medicine, Fairfield, Iowa.
Robert H. Schneider, Center for Natural Medicine and Prevention, Maharishi University of Management, College of Maharishi Vedic Medicine, Fairfield, Iowa.
Charles N. Alexander, Center for Natural Medicine and Prevention, Maharishi University of Management, College of Maharishi Vedic Medicine, Fairfield, Iowa.
Robert Cook, Department of Radiology, Charles Drew University of Medicine and Science, Los Angeles, Calif.
Hector Myers, Biobehavioral Research Center, Charles Drew University of Medicine and Science, Los Angeles, Calif; Department of Psychology, University of California at Los Angeles, Los Angeles, Calif..
Sanford Nidich, Center for Natural Medicine and Prevention, Maharishi University of Management, College of Maharishi Vedic Medicine, Fairfield, Iowa.
Chinelo Haney, Biobehavioral Research Center, Charles Drew University of Medicine and Science, Los Angeles, Calif.
Maxwell Rainforth, Center for Natural Medicine and Prevention, Maharishi University of Management, College of Maharishi Vedic Medicine, Fairfield, Iowa.
John Salerno, Center for Natural Medicine and Prevention, Maharishi University of Management, College of Maharishi Vedic Medicine, Fairfield, Iowa.
References
- 1.Keil JE, Sutherland SE, Knapp RG, Lackland DT, Gazes PC, Tyroler HA. Mortality rates and risk factors for coronary disease in black as compared with white men and women. N Engl J Med. 1993;329:73–78. [DOI] [PubMed] [Google Scholar]
- 2.Cooper R, Ford E. Coronary heart disease among blacks and whites in the NHANES-1 Epidemiologic Follow-up Study: incidence of new events and risk factor prediction. Ann Epidemiol. 1992;2:637–645. [DOI] [PubMed] [Google Scholar]
- 3.American Heart Association. 1997 Heart & Stroke Facts: Statistical Update. Dallas, Tex: American Heart Association; 1996. [Google Scholar]
- 4.NHLBI. Report of the Working Group on Research in Coronary Heart Disease in Blacks. Washington, DC: National Institutes of Health, National Heart, Lung, and Blood Institute; 1994. [Google Scholar]
- 5.NIH-National Heart, Lung, and Blood Institute. Morbidity and Mortality: 1996 Chartbook of Cardiovascular, Lung, and Blood Diseases. Washington, DC: National Institutes of Health; 1996. [Google Scholar]
- 6.Howard G, Anderson R, Sorlie P, Andrews V, Backlund E, Burke GL. Ethnic differences in stroke mortality between non-Hispanic whites, Hispanic whites, and blacks: the National Longitudinal Mortality Study. Stroke. 1994; 25:2120–2125. [DOI] [PubMed] [Google Scholar]
- 7.Gillum RF. Stroke in blacks. Stroke. 1988;19:1–9. [DOI] [PubMed] [Google Scholar]
- 8.Deubner DC, Tyroler HA, Cassel JC, Hames CG, Becker C. Attributable risk, population attributable risk and population attributable fraction of death associated with hypertension in a biracial population. Circulation. 1975;52:901–908. [DOI] [PubMed] [Google Scholar]
- 9.Langford HG, Oberman A, Borhani NO, Entwisle G, Tung B. Black-white comparison of indices of coronary heart disease and myocardial infarction in the stepped-care cohort of the Hypertension Detection and Follow-up Program. Am Heart J. 1984;104:797–801. [DOI] [PubMed] [Google Scholar]
- 10.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan J, Manuck S, Clarkson T, Lusso FM, Taub DM. Social status, environment, and atherosclerosis in cynomolgus monkeys. Arteriosclerosis. 1982;2:359–368. [DOI] [PubMed] [Google Scholar]
- 12.Julkunen J, Salonen R, Kaplan G, Chesney M, Salonen J. Hostility and the progression of carotid atherosclerosis. Psychosom Med. 1994;56:519–525. [DOI] [PubMed] [Google Scholar]
- 13.Everson S, Lynch J, Chesney M, Kaplan G, Goldberg D, Shade S, Cohen R, Salonen R, Salonen J. Interaction of workplace demands and cardiovascular reactivity in progression of carotid atherosclerosis: a population based study. BMJ. 1997;314:553–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muntaner C, Nieto FJ, Cooper L, Meyer J, Szklo M, Tyroler HA. Work organization and atherosclerosis: findings from the ARIC study: Atherosclerosis Risk in Communities. Am J Prev Med. 1998;14:9–18. [DOI] [PubMed] [Google Scholar]
- 15.Otten MW, Teutsch SM, Williamson DF, Marks JS. The effect of known risk factors on the excess mortality of black adults in the United States. JAMA. 1990;263:845–850. [PubMed] [Google Scholar]
- 16.Blumenthal J, Jiang W, Babyak M, Krantz D, Frid D, Coleman R, Waugh R, Hanson M, Appelbaum M, O’Connor C, Morris J. Stress management and exercise training in cardiac patients with myocardial ischemia. Arch Intern Med. 1997;157:2213–2223. [PubMed] [Google Scholar]
- 17.Schneider RH, Staggers F, Alexander C, Sheppard W, Rainforth M, Kondwani K, Smith S, King CG. A randomized controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995; 26:820–827. [DOI] [PubMed] [Google Scholar]
- 18.Alexander CN, Schneider R, Claybourne M, Sheppard W, Staggers F, Rainforth M, Salerno J, Kondwani K, Smith S, Egan B. A trial of stress reduction for hypertension in older African Americans, II: sex and risk factor subgroup analysis. Hypertension. 1996;28:228–237. [DOI] [PubMed] [Google Scholar]
- 19.Alexander CN, Barnes VA, Schneider RH, Langer EJ, Newman RI, Chandler HM, Davies JL, Rainforth M. A randomized controlled trial of stress reduction on cardiovascular and all-cause mortality in the elderly: results of 8 and 15 year follow-ups. Circulation. 1996;93:629. Abstract. [Google Scholar]
- 20.Alexander CN, Robinson P, Orme-Johnson DW, Schneider RH, Walton KG. Effects of Transcendental Meditation compared to other methods of relaxation and meditation in reducing risk factors, morbidity and mortality. Homeostasis. 1994;35:243–264. [Google Scholar]
- 21.Bond MG, Barnes RW, Riley WA, Wilmoth SK, Chambless LE, Howard G, Owens B. High-resolution B-mode ultrasound scanning methods in the Atherosclerosis Risk in Communities Study (ARIC). J Neuroimaging. 1991;1:68–73. [PubMed] [Google Scholar]
- 22.O’Leary DH, Polak JF, Wolfson SK, Bond MG, Bommer W, Sheth S, Psaty BM, Sharret AR, Manolio TA. Use of sonography to evaluate carotid atherosclerosis in the elderly: the Cardiovascular Health Study. Stroke. 1991; 22:1155–1163. [DOI] [PubMed] [Google Scholar]
- 23.Salonen J, Salonen R. Determinants of carotid-intima media thickness: a population based ultrasonography study in eastern Finnish men. J Intern Med. 1991;229:225–231. [DOI] [PubMed] [Google Scholar]
- 24.Blankenhorn DH, Selzer RH, Crawford DW, Barth JD, Liu CR, Liu CH, Mack WJ, Alaupovic P. Beneficial effects of colestipol-niacin therapy on the common carotid artery: two- and four-year reduction of intima-media thickness measured by ultrasound. Circulation. 1993;88:20–28. [DOI] [PubMed] [Google Scholar]
- 25.Furberg CD, Adams HP Jr, Applegate WB, Byington RP, Espeland MA, Hartwell T, Hunninghake DB, Lefkowitz DS, Probstfield J, Riley WA, et al. Effect of lovastatin on early carotid atherosclerosis and cardiovascular events: Asymptomatic Carotid Artery Progression Study (ACAPS) Research Group. Circulation. 1994;90:1679–1687. [DOI] [PubMed] [Google Scholar]
- 26.Byington RP, Furberg CD, Crouse JR III, Espeland MA, Bond MG. Pravastatin, Lipids, and Atherosclerosis in the Carotid Arteries (PLAC-II). Am J Cardiol. 1995;76:54C–59C. [DOI] [PubMed] [Google Scholar]
- 27.Blankenhorn DH, Hodis HN. Arterial imaging and atherosclerosis reversal: George Lyman Duff Memorial Lecture. Arterioscler Thromb. 1994;14: 177–192. [DOI] [PubMed] [Google Scholar]
- 28.Salonen JT, Salonen R. Ultrasonographically assessed carotid morphology and the risk of coronary heart disease. Arterioscler Thromb. 1991;11: 1245–1249. [DOI] [PubMed] [Google Scholar]
- 29.O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults: Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22. [DOI] [PubMed] [Google Scholar]
- 30.Hodis HN, Mack WJ, LaBree L, Selzer RH, Liu CR, Liu CH, Azen SP. The role of carotid arterial intima-media thickness in predicting clinical coronary events. Ann Intern Med. 1998;128:262–269. [DOI] [PubMed] [Google Scholar]
- 31.Burke GL, Evans GW, Riley WA, Sharrett AR, Howard G, Barnes RW, Rosamond W, Crow RS, Rautaharju PM, Heiss G. Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults: the Atherosclerosis Risk in Communities (ARIC) Study. Stroke. 1995;26: 386–391. [DOI] [PubMed] [Google Scholar]
- 32.Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, Clegg LX. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. Am J Epidemiol. 1997;146:483–494. [DOI] [PubMed] [Google Scholar]
- 33.Crouse JR, Goldbourt U, Evans G, Pinsky J, Sharrett AR, Sorlie P, Riley W, Heiss G. Risk factors and segment-specific carotid arterial enlargement in the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1996;27:69–75. [DOI] [PubMed] [Google Scholar]
- 34.Howard G, Manolio TA, Burke GL, Wolfson SK, O’Leary DH. Does the association of risk factors and atherosclerosis change with age?: an analysis of the combined ARIC and CHS cohorts: the Atherosclerosis Risk in Communities (ARIC) and Cardiovascular Health Study (CHS) investigators. Stroke. 1997;28:1693–1701. [DOI] [PubMed] [Google Scholar]
- 35.Diez-Roux AV, Nieto FJ, Tyroler HA, Crum LD, Szklo M. Social inequalities and atherosclerosis: the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 1995;141:960–972. [DOI] [PubMed] [Google Scholar]
- 36.Matthews K, Owens J, Kuller L, Sutton-Tyrrell K, Jansen-McWilliams L. Are hostility and anxiety associated with carotid atherosclerosis in healthy postmenopausal women? Psychosom Med. 1998;60:633–638. [DOI] [PubMed] [Google Scholar]
- 37.Lynch J, Krause N, Kaplan GA, Salonen JT. Workplace demands, economic reward, and progression of carotid atherosclerosis. Circulation. 1997;96:302–307. [DOI] [PubMed] [Google Scholar]
- 38.Howard G, Sharrett R, Heiss G, Evans G, Chambless L, Riley W, Burke G. Carotid artery intima-media thickness distribution in general populations as evaluated by B-mode ultrasound. Stroke. 1993;24:1297–1304. [DOI] [PubMed] [Google Scholar]
- 39.Arnett DK, Tyroler HA, Burke G, Hutchinson R, Howard G, Heiss G. Hypertension and subclinical carotid artery atherosclerosis in blacks and whites: the Atherosclerosis Risk in Communities Study: ARIC Investigators. Arch Intern Med. 1996;156:1983–1989. [PubMed] [Google Scholar]
- 40.D’Agostino RB Jr, Burke G, O’Leary D, Rewers M, Selby J, Savage PJ, Saad MF, Bergman RN, Howard G, Wagenknecht L, Haffner SM. Ethnic differences in carotid wall thickness: the Insulin Resistance Atherosclerosis Study. Stroke. 1996;27:1744–1749. [DOI] [PubMed] [Google Scholar]
- 41.Probstfield J, Byington R, Egan D. Methodogical issues facing studies of atherosclerotic change. Circulation. 1993;87(suppl II):II-74–II-81. [PubMed] [Google Scholar]
- 42.Riley WA, Barnes R, Applegate WB, Dempsey R, Hartwell T, Davis V, Bond M, Furberg C. Reproducibility of noninvasive ultrasonic measurement of carotid atherosclerosis: the Asymptomatic Carotid Artery Plaque Study. Stroke. 1992;23:1062–1068. [DOI] [PubMed] [Google Scholar]
- 43.Devereux RB, Waeber B, Roman MJ. Conclusions on the measurement of arterial wall thickness: anatomic, physiologic and methodologic considerations. J Hypertens. 1992;10:S119–S121. [PubMed] [Google Scholar]
- 44.Furberg C, Byington R, Craven T. Lessons learned from clinical trials with ultrasound end-points. J Intern Med. 1994;236:575–580. [DOI] [PubMed] [Google Scholar]
- 45.Nader T Human Physiology-Expression of Veda and the Vedic Literature. Vlodrop, Holland: Maharishi University Press; 1995. [Google Scholar]
- 46.Wallace RK, Benson H, Wilson AF. A wakeful hypometabolic physiologic state. Am J Physiol. 1971;221:795–799. [DOI] [PubMed] [Google Scholar]
- 47.Jevning R, Wallace RK, Biedebach M. The physiology of meditation: a review: a wakeful hypometabolic integrated response. Neurosci Biobehav Rev. 1992;16:415–424. [DOI] [PubMed] [Google Scholar]
- 48.Dillbeck MC, Orme-Johnson DW. Physiological differences between Transcendental Meditation and rest. Am Psychol. 1987;42:879–881. [Google Scholar]
- 49.Travis F, Wallace RK. Autonomic patterns during respiration suspensions: possible markers of transcendental consciousness. Psychophysiology. 1997; 34:39–46. [DOI] [PubMed] [Google Scholar]
- 50.The Treatment of Mild Hypertension Research Group. The Treatment of Mild Hypertension Study: a randomized, placebo-controlled trial of nutritional-hygienic regimen along with various drug monotherapies. Arch Intern Med. 1991;151:1413–1423. [DOI] [PubMed] [Google Scholar]
- 51.Zamarra JW, Schneider RH, Besseghini I, Robinson DK, Salerno JW. Usefulness of the Transcendental Meditation program in the treatment of patients with coronary artery disease. Am J Cardiol. 1996;78:77–80. [DOI] [PubMed] [Google Scholar]
- 52.Wenneberg SR, Schneider RH, MacLean C, Walton KG, MacLean CRK, Levitsky DK, Mandarino JV, Rainforth MV, Salerno JW, Waziri R, Wallace RK. A controlled study on the effects of Transcendental Meditation on cardiovascular reactivity and ambulatory blood pressure. Int J Neurosci. 1997;89:15–28. [DOI] [PubMed] [Google Scholar]
- 53.Alexander CN, Langer EJ, Newman RI, Chandler HM, Davies JL. Transcendental Meditation, mindfulness, and longevity: an experimental study with the elderly. J Pers Soc Psychol. 1989;57:950–964. [DOI] [PubMed] [Google Scholar]
- 54.Dwyer JH, Sun P, Kwong-Fu H, Dwyer KM, Selzer RH. Automated intima-media thickness: the Los Angeles Atherosclerosis Study. Ultrasound Med Biol. 1997;24:981–987. [DOI] [PubMed] [Google Scholar]
- 55.Mack WJ, Seltzer RH, Hodis HN, Erickson JK, Liu C, Liu C, Crawford DW, Blankenhorn DH. One-year reduction and longitudinal analysis of carotid intima-media thickness associated with colestipol/niacin therapy. Stroke. 1993;24:1779–1783. [DOI] [PubMed] [Google Scholar]
- 56.Salonen JT, Salonen R. Ultrasound B-mode imaging in observational studies of atherosclerotic progression. Circulation. 1993;87(suppl II):II-56–II-65. [PubMed] [Google Scholar]
- 57.Salonen R, Haapanen A, Salonen JT. Measurement of intima-media thickness of common carotid arteries with high-resolution B-mode ultrasonography: inter- and intra-observer variability. Ultrasound Med Biol. 1991; 17:225–230. [DOI] [PubMed] [Google Scholar]
- 58.Crouse J, Craven T, Hagaman A, Bond M. Associations of coronary disease with segment-specific intimal-medial thickening of the extracranial carotid artery. Circulation. 1995;92:1141–1147. [DOI] [PubMed] [Google Scholar]
- 59.Sacco R, Roberts K, Boden-Albala B, Gu Q, Lin I, Kargman D, Berglund L, Hauser W, Shea S, Paik M. Race-ethnicity and determinants of carotid atherosclerosis in a multiethnic population: the Northern Manhattan Stroke Study. Stroke. 1997;28:929–935. [DOI] [PubMed] [Google Scholar]
- 60.Markus RA, Mack WJ, Azen SP, Hodis HN. Influence of lifestyle modification on atherosclerotic progression determined by ultrasonographic change in the common carotid intima-media thickness. Am J Clin Nutr. 1997;65:1000–1004. [DOI] [PubMed] [Google Scholar]
- 61.Kaplan JR, Manuck SB, Clarkson TB, Lusso FM, Taub D, Miller EW. Social stress and atherosclerosis in normocholesterolemic monkeys. Science. 1983; 220:733–735. [DOI] [PubMed] [Google Scholar]
- 62.Kamarck TW, Everson SA, Kaplan GA, Manuck SB, Jennings JR, Salonen R, Salonen JT. Exaggerated blood pressure responses during mental stress are associated with enhanced carotid atherosclerosis in middle-aged Finnish men: findings from the Kuopio Ischemic Heart Disease Study. Circulation. 1997; 96:3842–3848. [DOI] [PubMed] [Google Scholar]
- 63.Barnett PA, Spence JD, Manuck SB, Jennings JR. Psychological stress and the progression of carotid artery disease. J Hypertens. 1997;15:49–55. [DOI] [PubMed] [Google Scholar]
- 64.Schneider RH, Alexander CN, Wallace RK. In search of an optimal behavioral treatment for hypertension: a review and focus on Transcendental Meditation. In: Johnson EH, Gentry WD, Julius S, eds. Personality, Elevated Blood Pressure, and Essential Hypertension. Washington DC: Hemisphere Publishing Corp; 1992:291–312. [Google Scholar]
- 65.Mills PJ, Schneider RH, Hill D, Walton KG, Wallace RK. Beta-adrenergic receptor sensitivity in subjects practicing Transcendental Meditation. J Psychosom Med. 1990;34:29–33. [DOI] [PubMed] [Google Scholar]


