Abstract
Background:
Unit cohesion may protect service member mental health by mitigating effects of combat exposure; however, questions remain about the origins of potential stress-buffering effects. We examined buffering effects associated with two forms of unit cohesion (peer-oriented horizontal cohesion and subordinate-leader vertical cohesion) defined as either individual-level or aggregated unit-level variables.
Methods:
Longitudinal survey data from US Army soldiers who deployed to Afghanistan in 2012 were analyzed using mixed-effects regression. Models evaluated individual- and unit-level interaction effects of combat exposure and cohesion during deployment on symptoms of posttraumatic stress disorder (PTSD), depression, and suicidal ideation reported at 3 months post-deployment (model n’s=6,684 to 6,826). Given the small effective sample size (k=89), significance of unit-level interactions was evaluated at a 90% confidence level.
Results:
At the individual-level, buffering effects of horizontal cohesion were found for PTSD symptoms (B=−0.11, 95% CI [−0.18, −0.04], p<.01) and depressive symptoms (B=−0.06, 95% CI [−0.10, −0.01], p<0.05); while a buffering effect of vertical cohesion was observed for PTSD symptoms only (B=−0.03, 95% CI [−0.06, −0.0001], p<.05). At the unit-level, buffering effects of horizontal (but not vertical) cohesion were observed for PTSD symptoms (B=−0.91, 90% CI [−1.70, −0.11], p=.06), depressive symptoms (B=−0.83, 90% CI [−1.24, −0.41], p<.01), and suicidal ideation (B=−0.32, 90% CI [−0.62, −0.01], p=.08).
Conclusions:
Policies and interventions that enhance horizontal cohesion may protect combat-exposed units against post-deployment mental health problems. Efforts to support individual soldiers who report low levels of horizontal or vertical cohesion may also yield mental health benefits.
Introduction
Service members who have deployed in support of combat operations are at risk of developing posttraumatic stress disorder (PTSD), depression, and other mental health problems, with vulnerability generally increasing with the degree of combat exposure (e.g., Hines et al., 2014, Hoge et al., 2006, Hoge et al., 2004, Smith et al., 2008). Combat exposure has also been associated with suicide-related outcomes (e.g., Bryan et al., 2015), which are of great concern to military leadership and society as a whole. Identifying factors that buffer the effects of combat exposure can inform efforts to reduce a range of mental health morbidities among service members.
One potential buffering factor is unit cohesion, or the “shared identity and mutually supportive relationships” that develop among members of the same military unit (Griffith, 2015, p. 99). Service members who report high unit cohesion exhibit fewer mental health problems including PTSD (e.g., Anderson et al., 2019, Jones et al., 2012, Kanesarajah et al., 2016, Pietrzak et al., 2010), depression (Anderson et al., 2019, Pietrzak et al., 2010), and suicidal ideation (Anderson et al., 2019, Griffith, 2015, Kanesarajah et al., 2016, Mitchell et al., 2012). However, few studies have specifically investigated stress-buffering effects of unit cohesion, and those that have done so have yielded mixed results (Anderson et al., 2019, Armistead-Jehle et al., 2011, Griffith, 2015, Mitchell et al., 2012).
The evidence linking unit cohesion to mental health outcomes is also limited by the common practice of measuring and modeling cohesion at the individual level. Perceptions of cohesion captured by raw individual-level measures are likely influenced not only by the cohesion of the respondent’s unit (a group characteristic), but also by the respondent’s personality, mental health, and idiosyncratic experiences within that unit (individual characteristics). Without further analyses, the extent to which relationships between raw measures of unit cohesion and mental health outcomes are explained by individual versus group factors is unknown and, consequently, the policy and intervention implications of such associations remain unclear.
Mixed effects modeling can disaggregate individual- and group-level effects and yield more actionable findings. Here, the use of mixed-effect models entails deriving group-level measures of the constructs of interest, and fitting a series of models to isolate individual-level, unit-level, and cross-level interaction effects of combat exposure and cohesion on mental health outcomes. An individual-level interaction would signify that personal perceptions of cohesion, shaped by factors such as personality and idiosyncratic experiences, moderate the effect of an individual’s reported combat exposure on his or her mental health outcomes. In contrast, a cross-level interaction would imply that a shared group property of cohesion moderates the relationship between an individual’s reported level of combat exposure and his or her mental health outcomes. Finally, a pure unit-level interaction would suggest that a shared group property of cohesion moderates the relationship between a unit’s collective combat exposure and the overall mental health outcomes of that unit.
Parsing effects in this manner is important because it provides insight into the mechanisms underlying cohesion’s presumed buffering effects and the level at which intervention should occur. Significant cross- or unit-level interactions would imply that group-level processes are key and suggest that policies or interventions that enhance overall unit cohesion could help protect members against adverse psychological effects of combat exposure. In contrast, individual-level interactions would imply that individual perceptions are primary and that risk mitigation programs should target individuals who report low cohesion, irrespective of the overall level of cohesion in their unit. To our knowledge, only two prior studies have used mixed-effect models to evaluate cohesion and mental health outcomes (Breslau et al., 2016, Griffith, 2015). While these provided important insights, only one examined potential buffering effects (Griffith, 2015); and neither sought to fully disentangle individual- and unit-level effects of cohesion, which are inherently confounded in survey-based measures.
Another concern is that prior studies have not consistently differentiated two types of cohesion: bonds among peers (“horizontal cohesion”) and bonds between subordinates and leaders (“vertical cohesion”). Some studies have employed measures of unit cohesion that simultaneously assess bonds with peers, leaders, and/or the service branch as a whole (e.g., Anderson et al., 2019, Breslau et al., 2016, Griffith, 2015). This approach may fail to identify unique effects of horizontal and vertical cohesion, which can impact health outcomes in distinct ways (e.g., Browne et al., 2008). Research parsing these constructs also has the potential to yield more specific recommendations for intervention (e.g., policies to promote bonding of peers versus training programs for unit leaders).
Given the limitations of existing literature, we sought to conduct a study that would provide further insights into cohesion’s buffering effects and yield more specific actionable findings for the US Army. Data were drawn from the Pre/Post Deployment Study (PPDS), a prospective component of the Army Study to Assess Risk and Resilience in Servicemembers [Army STARRS; (Ursano et al., 2014)]. The PPDS surveyed soldiers shortly before, and at multiple points after, their deployment to Afghanistan. By combining PPDS survey data with Army administrative data, we developed individual- and unit-level measures of horizontal cohesion, vertical cohesion, combat exposure, and mental health outcomes. Using mixed-effects modeling, we evaluated whether horizontal and vertical unit cohesion during deployment buffered the effects of combat exposure on symptoms of PTSD, depression, and suicidal ideation assessed 3 months after return from deployment. By comparing the results of individual-level, cross-level, and unit-level models, we examined whether any stress-buffering effects of cohesion were attributable to differences in individual characteristics or differences in units.
Method
The PPDS (Kessler et al., 2013, Ursano et al., 2014) is a multi-wave panel survey of members of 3 Brigade Combat Teams (BCTs) that deployed to Afghanistan in 2012 for an average of 10 months. Baseline (T0) data were collected 1-2 months before the index deployment. Follow-up data were collected within 1 month of return from deployment (T1), and approximately 3 months (T2) and 9 months (T3) after return from deployment. Respondents provided written informed consent to participate in the surveys, and were asked separately for consent to link survey responses to their Army/Department of Defense administrative records. Study procedures were approved by the Human Subjects Committees of the Army STARRS collaborating institutions.
At baseline, 9949 soldiers were present for duty in the 3 BCTs. Supplementary Figure S1 depicts selection of participants for the study. To be included, soldiers must have: participated in the T1 and T2 surveys, consented to administrative data linkage at T1 and T2, belonged to the same unit at T1 and T2, completed items from the combat exposure and cohesion measures at T1, and completed items for at least 1 of the 3 dependent variables at T2. Available unit membership data consisted of de-identified unit identification codes for each soldier’s “parent unit” and “child unit”. Because the concept of unit cohesion is typically applied to smaller groups (squads, platoons, companies) as opposed to larger ones (battalions, brigades, divisions), we constrained the analytic samples to soldiers who belonged to child units represented by between 10 and 299 soldiers (e.g., company-sized units). There are 3 analytic samples, one for each dependent variable: past-30-day depressive symptoms (n=6,712), past-30-day PTSD symptoms (n=6,684), and past-30-day suicidal ideation (n=6,826). The soldiers included in each analytic sample belonged to a total of k=89 units.
Measures
Unit Cohesion.
The T1 survey included items assessing soldiers’ unit experiences, some of which were adapted from prior instruments (Joint Mental Health Advisory Team 7 (J-MHAT 7), 2011, Mental Health Advisory Team (MHAT) 6, 2009) and others that were developed for Army STARRS. Six items were considered appropriate for measuring cohesion at both the individual and group levels. These items were rated on Likert-style scales, which were converted to scores ranging from 0 (strongly disagree) to 4 (strongly agree). We derived 2 scales that measured horizontal cohesion (2 items: I can rely on my battle buddy for help if I need it, I can rely on other members of my unit for help if I need it) and vertical cohesion (4 items: I can open up and talk to my first line leaders if I need help, I respect the Non-Commissioned Officers in my unit, I respect the Officers in my unit, My leaders take a personal interest in the well-being of the Soldiers in my unit). Items for each scale were selected based on face validity. The ratings of each set of items were summed to yield a Horizontal Cohesion score (theoretical range=0-8; Cronbach’s α=0.79) and a Vertical Cohesion score (theoretical range=0-16; Cronbach’s α=0.88), with higher scores indicating a higher level of cohesion perceived by the respondent. We then aggregated the Horizontal Cohesion and Vertical Cohesion scores as unit-level averages for the 89 units in each of the 3 analytic samples (based only on data from soldiers in that particular sample). The average intraclass correlation coefficients [ICC(1)s] for Horizontal Cohesion and Vertical Cohesion were 0.04 and 0.05, respectively, across the three analytic samples. Values indicate that the measures of cohesion demonstrated low (but not atypical) levels of clustering by unit. The average ICC(2) values for Horizontal Cohesion and Vertical Cohesion (0.76 and 0.80, respectively) indicate reliable group-mean differences which facilitate detecting group-level effects (Bliese et al., 2018).
Combat Exposure.
The T1 survey contained 10 items adapted from the Deployment Risk and Resilience Inventory (King, 2006, Vogt et al., 2008) and the Joint Mental Health Advisory Team 7 survey (Joint Mental Health Advisory Team 7 (J-MHAT 7), 2011) that assessed frequency of exposure to combat situations (e.g., During your deployment, how many times did you… fire rounds at the enemy or take enemy fire?… have members of your unit who were seriously wounded or killed?). Two items assessing responsibility for the death of a non-combatant and responsibility for the death of US or ally personnel were excluded due to low incidence (<2%). Responses to the remaining 8 items were recoded 0/1 or 0/1/2 based on the optimal functional form in association with mental health outcomes (for scoring details, see Campbell-Sills et al., 2018). Item-level scores were then summed to quantify overall combat exposure, with higher scores suggesting a higher level of exposure (theoretical range=0-9). The ICC(1) for Combat Exposure was 0.34 in each of the analytic samples indicating a high degree of clustering at the unit-level and the ICC(2) was 0.98 indicating highly reliable group mean differences.
Demographic and Service Characteristics.
Demographic and service-related variables were obtained from administrative data linked to surveys at T1. Administrative data were compiled from multiple databases provided by the Defense Manpower Data Center; prior reports from the Army STARRS Historical and Administrative Data Study provide the list of databases (Kessler et al., 2017, Ursano et al., 2018). The covariates included in the models were gender, age, race, education level, marital status, age of entry to the Army, and years of Army service.
Mental Health Outcomes.
The T2 survey contained items adapted from the Composite International Diagnostic Interview Screening Scales (CIDI-SC; Kessler and Ustun, 2004), the civilian PTSD Checklist for DSM-IV (PCL-C; Weathers et al., 1993), and the Columbia-Suicide Severity Rating Scale (Posner et al., 2011). We selected CIDI-SC items that corresponded to items from validated dimensional measures of depression (e.g., Kroenke et al., 2001) to measure past-30-day depressive symptoms (theoretical range=0-36; Cronbach’s α=0.88), PCL-C items to measure past-30-day PTSD symptoms (theoretical range=17-85; Cronbach’s α=0.94), and two items that assessed past-30-day thoughts of suicide and wishing to be dead (“no” to both items=0; “yes” to either item=1) to construct the 3 dependent variables, respectively. Past 30-day PTSD symptoms were rated in reference to “any stressful experience that ever happened to you.”
If responses were missing due to survey skip patterns, these were assigned the null value and included in the analysis. For the purpose of constructing the measure of depressive symptoms, if more than one CIDI-SC item could be mapped onto a single depression criterion (e.g., feeling tired out and easily fatigued), the response indicating higher symptom severity was chosen. The ICC(1)s for post-deployment PTSD symptoms, depressive symptoms, and suicidal ideation, were 0.03, 0.02, and 0.00, respectively with ICC(2) values of 0.69, 0.60 and 0.20. The ICC(1) values (while low) are typical for mental health outcomes (Bliese et al., 2018). The ICC(2) values are also relatively low, but do not preclude detecting meaningful group-level effects (Bliese et al., 2018).
Data Analysis
We conducted our analyses using the lme4 (Bates et al., 2015) and nlme (Pinheiro et al., 2019) packages in the R statistical software program. Hypotheses were tested in two-level models with random intercepts to account for clustering (Raudenbush & Bryk, 2002). Level-1 in the analyses reflects individual soldiers nested within units (level-2). Mixed-effects models are well-suited for evaluating cross-level interactions when level-2 units differ with respect to size (Raudenbush and Bryk, 2002), as in our sample. Models examining post-deployment PTSD and depressive symptoms were estimated using linear mixed-effects models. In contrast, a generalized linear mixed-effects model with a binomial link function was used to examine suicidal ideation because the outcome was dichotomous.
We fit several models for each outcome to decompose the origin of the variance (individual-level, cross-level, or unit-level) for interactions involving combat exposure and cohesion variables. The Raw Interaction Model (e.g., Model 1.2 in Table 1) tests interactions at the individual level where all variables (combat exposure, horizontal/vertical unit cohesion, mental health outcomes) reflect individual responses. The Cross-Level Interaction Model (e.g., Model 1.3) tests whether an individual’s level of combat exposure, relative to others in the same unit, interacts with his or her unit’s average cohesion in predicting individual mental health outcomes. In the cross-level interaction model we group-mean center (e.g., demean) individual reports of combat exposure to obtain an unbiased estimate of level-1 slope (Hofmann and Gavin, 1998). The Group-Mean Model (e.g., Model 1.4) examines unit-level effects by examining whether the interaction of a unit’s average combat exposure and average cohesion predicts unit-average mental health outcomes. The Simultaneous Model (e.g., Model 1.5) includes both the raw individual interaction and the group-mean interaction terms. Note that parameters from models with main effects at both levels (e.g., combat exposure as both an individual rating and a unit estimate) have a clear interpretation. For instance, when level-1 variables are in the raw form, the level-2 parameter represents the difference between level-1 and level-2 slope (Hofmann and Gavin, 1998). In contrast, models with simultaneous interaction terms are more complex and are simply used here to examine whether effects persist when adjusting for effects at the other level (Shaver, 2019).
Table 1.
Effects of combat exposure and horizontal cohesion on post-deployment PTSD symptoms (N=6,684 soldiers in k=89 units)
| Model 1.1 | Model 1.2 | Model 1.3 | Model 1.4 | Model 1.5 | |
|---|---|---|---|---|---|
|
|
|||||
| Constant | 28.44***(3.24) | 24.96***(1.00) | 22.43***(3.76) | 14.45†(7.85) | 13.94†(7.89) |
| Combat Exposure | 1.45***(0.08) | 2.04***(0.23) | 2.06***(0.24) | ||
| Combat Exposure (group mean centered) | 1.29(1.23) | ||||
| Unit Average Combat Exposure | −0.28(0.19) | 6.78*(2.96) | 5.09†(2.99) | ||
| Horizontal Cohesion | −1.00***(0.07) | −0.71***(0.13) | −0.72***(0.13) | ||
| Unit Average Horizontal Cohesion | −0.18(0.55) | 0.32(0.61) | 1.11(1.29) | 1.90 (1.30) | |
| Combat Exposure X Horizontal Cohesion | −0.11**(0.04) | −0.10**(0.04) | |||
| Combat Exposure (group mean centered) X Unit Average Horizontal Cohesion |
0.02(0.20) | ||||
| Unit Average Combat Exposure X Unit Average Horizontal Cohesion |
−0.91†(0.48) | −0.86†(0.48) | |||
Note. Unstandardized regression coefficients reported (standard errors in parentheses). Models controlled for gender, age, race, education level, marital status, age of entry to the Army, and years of Army service.
p<0.1,
p<0.05,
p<0.01,
p<0.001.
It is important to note that the effective sample size for the group-mean models is based on the number of units (k=89) rather than respondents (N=6,684 to 6,826 based on the dependent variable). As such, the standard errors for group-mean effects will be much larger than individual-level standard errors, requiring a substantially larger effect to reach statistical significance. Thus, for group-mean models we interpret interaction effects as significant at a 90% confidence level.
Finally, we ran a series of models that included pre-deployment (T0) measures of the outcomes as controls. In addition to providing a robustness check of our primary findings, these models offer insight into whether the patterns we observed with respect to understanding the key source of variance across levels would generalize to models that explicitly examine change over time. Sample sizes for these models were smaller (N=5,197 to 5,311 based on the dependent variable), because some of the soldiers that were included in the primary analysis had not completed the measures at T0. For models evaluating buffering effects found to be significant in the primary analysis, we used one-tailed tests based on the expectation that the forms of the relationships would be similar; two-tailed tests were used to evaluate all other interactions involving the cohesion variables.
In sum, by contrasting results across a series of complementary models we can draw inferences about the sources of variance in a complex multilevel situation where relationships at one level are often mirrored at other levels (Bliese et al., 2018). In so doing, we can gain theoretical and practical insights into whether effects occurring at the individual-level are reflected in group means or vice versa.
Results
The demographic and Army service characteristics of soldiers included in the PTSD, depression, and suicidal ideation analyses are presented in Supplementary Table S1. The composition of the three analytic samples was nearly identical. Soldiers in the analytic samples were predominantly male (94%). Approximately two-thirds were White (68%) and more than half were married (56%). The majority had a high school diploma and no college education (73%), and had entered the Army between the ages of 17-20 (58%). At the time of the PPDS T0 survey, most were E3/E4 enlisted soldiers (71%) who were 21-29 years old (65%) and had served in the Army for 3-10 years (68%).
Buffering effects of horizontal cohesion
The results of the models of post-deployment PTSD symptoms are shown in Table 1.
Raw Interaction Model.
Model 1.2 results show that the interaction between an individual soldier’s level of combat exposure and his or her perceptions of horizontal cohesion was significantly associated with PTSD symptoms (B= −0.11, 95% CI [−0.18, −0.04], p< 0.01). A predicted plot (Figure 1A; dotted lines) shows that the relationship between individual-level combat exposure and PTSD symptoms was attenuated for individuals who perceived their units as having high horizontal cohesion. As noted earlier, a limitation of this model is that the interaction of raw scores can stem from either individual- or group-level effects; thus, additional models were fit to identify the source of variation underlying the interaction.
Figure 1.
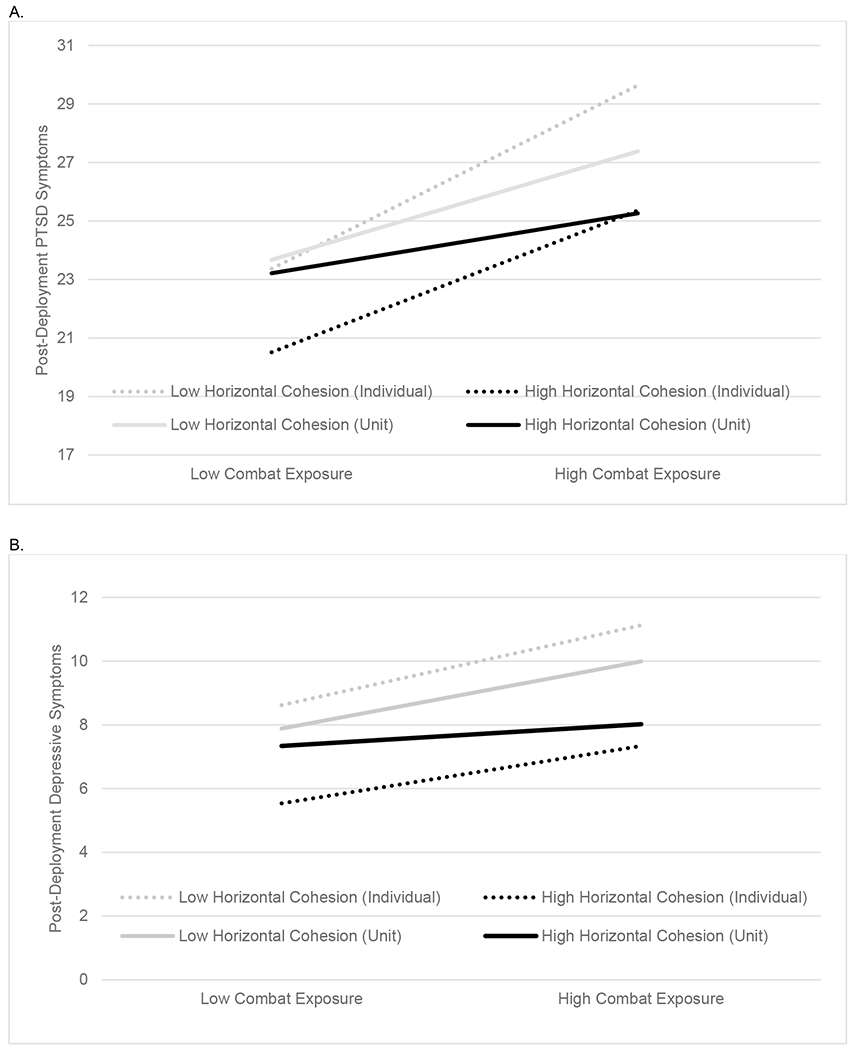
Illustration of the individual-level and unit-level interaction effects of combat exposure and horizontal cohesion on symptoms of PTSD (panel A) and depression (panel B) at 3 months post-deployment. Dotted lines show the predicted levels of symptoms for individuals scoring 1 SD below the mean (gray line) and 1 SD above the mean black line) on the horizontal cohesion scale. Solid lines show the predicted unit-average symptom scores for units with average horizontal cohesion scores that were 1 SD below the mean (gray line) and 1 SD above the mean (black line) for the 89 units represented in the analytic samples. At the individual level, low combat exposure is defined as 1 SD below the mean and high combat exposure as 1 SD above the mean level of combat exposure reported by the soldiers in each analytic sample. At the unit level, low combat exposure is defined as a unit-average combat exposure score 1 SD below the mean and high combat exposure as a unit-average combat exposure score 1 SD above the mean combat exposure score for all 89 units. Estimates are based on Models 1.2 and 1.4 (panel A) and Models 2.2 and 2.4 (panel B). Subsequent models showed that both the individual- and unit-level interactions were unique predictors of post-deployment PTSD symptoms (panel A) and depressive symptoms (panel B).
Cross-Level Interaction Model.
Model 1.3 results revealed that the cross-level interaction between an individual’s combat exposure, relative to others in the same unit, and his or her unit’s average horizontal cohesion was not significantly associated with PTSD symptoms (B= 0.02, 95% CI [−0.48, 0.42], p= 0.93). This suggests that the relationship between a soldier’s individual reports of combat exposure and PTSD symptoms is not moderated by the average level of horizontal cohesion in his or her unit.
Group-Mean Model.
Model 1.4 examined the interaction between a unit’s average combat exposure and average horizontal cohesion on unit-average PTSD symptoms. The estimated slope (B= −0.91, 90% CI [−1.70, −0.11], p=0.06) was substantially larger in absolute magnitude than the estimate from the raw interaction model (B= −0.11), and was significant at the 90% confidence level. A plot based on predicted values (Figure 1A; solid lines) shows that the relationship between units’ average levels of combat exposure and PTSD symptoms was attenuated in units with high levels of horizontal cohesion.
Simultaneous Model.
Model 1.5 included combat exposure x horizontal cohesion interactions at both levels. Both the individual-level (B= −0.10, 95% CI [−0.17, −0.10], p< 0.01) and unit-level (B= −0.86, 90% CI [−1.67, −0.06], p= 0.08) interaction effects remained significant, but their magnitude was slightly attenuated relative to the models that estimated these effects separately.
The results of the models of post-deployment depressive symptoms are shown in Table 2.
Table 2.
Effects of combat exposure and horizontal cohesion on post-deployment depressive symptoms (N=6,712 soldiers in k=89 units)
| Model 2.1 | Model 2.2 | Model 2.3 | Model 2.4 | Model 2.5 | |
|---|---|---|---|---|---|
|
|
|||||
| Constant | 15.20***(1.90) | 12.13***(0.63) | 12.22***(2.03) | 1.97(4.29) | 2.49(4.30) |
| Combat Exposure | 0.56***(0.05) | 0.88***(0.15) | 0.86***(0.15) | ||
| Combat Exposure (group mean centered) | 1.46†(0.78) | ||||
| Unit Average Combat Exposure | −0.08(0.12) | 5.61***(1.56) | 4.75**(1.58) | ||
| Horizontal Cohesion | −0.98***(0.05) | −0.83***(0.08) | −0.84***(0.08) | ||
| Unit Average Horizontal Cohesion | −0.33(0.32) | −0.64†(0.32) | 0.78(0.70) | 1.57*(0.71) | |
| Combat Exposure X Horizontal Cohesion | −0.06*(0.02) | −0.05*(0.02) | |||
| Combat Exposure (group mean centered) X Unit Average Horizontal Cohesion |
−0.15(0.13) | ||||
| Unit Average Combat Exposure X Unit Average Horizontal Cohesion |
−0.83**(0.25) | −0.78**(0.25) | |||
Note. Unstandardized regression coefficients reported (standard errors in parentheses). Models controlled for gender, age, race, education level, marital status, age of entry to the Army, and years of Army service.
p<0.1,
p<0.05,
p<0.01,
p<0.001.
Raw Interaction Model.
Model 2.2 revealed that the interaction between an individual soldier’s level of combat exposure and his or her perceptions of horizontal cohesion was significantly associated with his or her depressive symptoms (B= −0.06, 95% CI [−0.10, −0.01], p< 0.05). A predicted plot (Figure 1B; dotted lines) shows that the relationship between individual reports of combat exposure and depressive symptoms was attenuated for individuals who perceived their units as having high horizontal cohesion.
Cross-Level Interaction Model.
Model 2.3 results show that the cross-level interaction between an individual’s combat exposure, relative to others in the same unit, and his or her unit’s average level of horizontal cohesion, was not a significant predictor of depressive symptoms (B= −0.15, 95% CI [−0.41, 0.10], p= 0.23). Results from this model suggest that the relationship between a soldier’s individual reports of combat exposure and depression is not moderated by the average level of horizontal cohesion in his or her unit.
Group-Mean Model.
Model 2.4 examined the interaction effect of a unit’s average combat exposure and average horizontal cohesion on unit-average depressive symptoms. The estimate of the slope (B= −0.83, 90% CI [−1.24, −0.41], p< 0.01) was substantially larger in absolute magnitude than the raw estimate (B= −0.06). A predicted plot (Figure 1B; solid lines) shows that the relationship between units’ average levels of combat exposure and depressive symptoms was attenuated in units with high levels of horizontal cohesion.
Simultaneous Model.
Model 2.5 included combat exposure x horizontal cohesion interactions at both levels. Both the individual-level (B= −0.05, 95% CI [−0.10, −0.01], p< 0.05) and unit-level (B= −0.78, 90% CI [−1.20, −0.35], p< 0.01) interaction effects remained significant, although both were slightly attenuated relative to the models that estimated these effects separately.
The results of the models of post-deployment suicidal ideation are shown in Table 3.
Table 3.
Effects of combat exposure and horizontal cohesion on post-deployment suicidal ideation (N=6,826 soldiers in k=89 units)
| Model 3.1 | Model 3.2 | Model 3.3 | Model 3.4 | Model 3.5 | |
|---|---|---|---|---|---|
|
|
|||||
| Constant | −4.70***(1.37) | −1.97***(0.49) | −5.13*(2.08) | −9.95**(3.29) | −9.98**(3.34) |
| Combat Exposure | 0.04(0.04) | 0.11(0.10) | 0.06(0.11) | ||
| Combat Exposure (group mean centered) | −0.56(0.69) | ||||
| Unit Average Combat Exposure | 0.06(0.09) | 2.09†(1.15) | 2.08†(1.17) | ||
| Horizontal Cohesion | −0.20***(0.04) | −0.16*(0.06) | −0.19**(0.07) | ||
| Unit Average Horizontal Cohesion | 0.06(0.09) | 0.38†(0.21) | 1.11*(0.53) | 1.31*(0.55) | |
| Combat Exposure X Horizontal Cohesion | −0.01(0.02) | 0.00(0.02) | |||
| Combat Exposure (group mean centered) X Unit Average Horizontal Cohesion |
0.10(0.11) | ||||
| Unit Average Combat Exposure X Unit Average Horizontal Cohesion |
−0.32†(0.18) | −0.32†(0.19) | |||
Note. Unstandardized regression coefficients reported (standard errors in parentheses). Models controlled for gender, age, race, education level, marital status, age of entry to the Army, and years of Army service.
p<0.1,
p<0.05,
p<0.01,
p<0.001.
Raw Interaction Model.
Model 3.2 results revealed that the interaction between an individual’s combat exposure and perceptions of horizontal cohesion was not associated with suicidal ideation (B= −0.01, 95% CI [−0.04, 0.03], p= 0.68). The results suggest that the relationship between a soldier’s individual reports of combat exposure and suicidal ideation is not moderated by his or her perceptions of horizontal cohesion.
Cross-Level Interaction Model.
Model 3.3 results showed that the cross-level interaction between an individual’s combat exposure, relative to others in the same unit, and his or her unit’s average level of horizontal cohesion, was not associated suicidal ideation (B= 0.10, 95% CI [−0.12, 0.31], p= 0.39). Results from this model suggest that the link between a soldier’s individual reports of combat exposure and suicidal ideation is not moderated by the average level of horizontal cohesion in his or her unit.
Group-Mean Model.
Model 3.4 examined the interaction between a unit’s average combat exposure and average horizontal cohesion. Results show that the interaction was a significant predictor of unit-average suicidal ideation at the 90% confidence level (B= −0.32, 90% CI [−0.62, −0.01], p= 0.08). A predicted plot (Figure 2) shows that the relationship between a unit’s average levels of combat exposure and suicidal ideation was attenuated in units with high horizontal cohesion. However, because the results also suggested higher overall levels of suicidal ideation in units with higher cohesion (as indicated by the significant main effect of unit-average horizontal cohesion on suicidal ideation in Model 3.4), the results are not entirely congruent with a stress-buffering interpretation.
Figure 2.
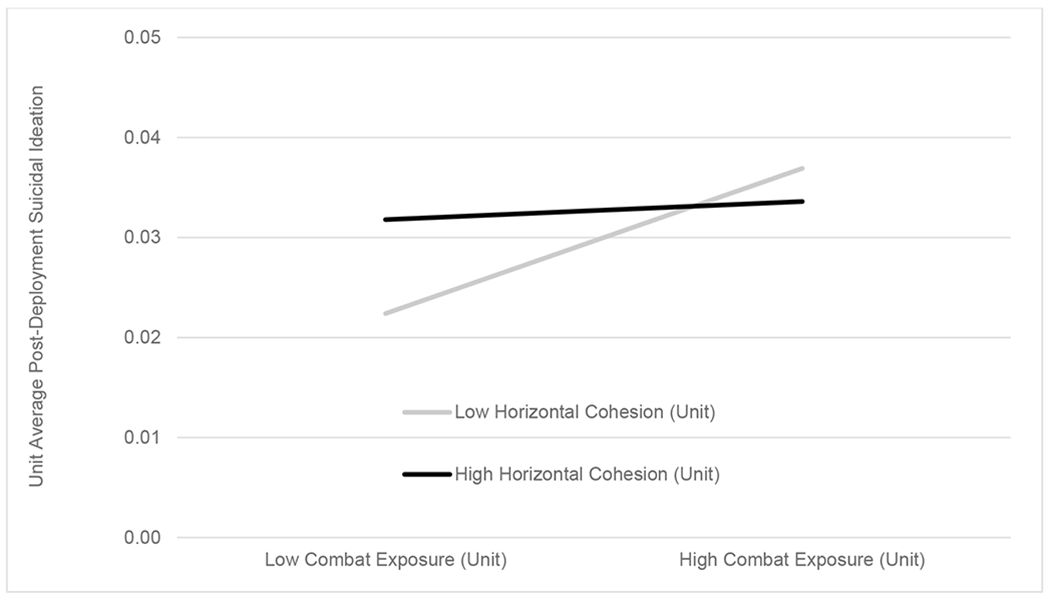
Illustration of the unit-level interaction effect of combat exposure and horizontal cohesion on unit-average suicidal ideation at 3 months post-deployment. The plot shows the predicted unit-average rate of suicidal ideation for units with average horizontal cohesion scores that were 1 SD below (low; gray line) and 1 SD above (high; black line) the mean horizontal cohesion score for all 89 units. Estimates are based on Model 3.4. At the unit level, low combat exposure is defined as a unit-average combat exposure score that is 1 SD below the mean and high combat exposure as a unit-average combat exposure score that is 1 SD above the mean combat exposure score for all 89 units.
Simultaneous Model.
Model 3.5 included combat exposure x horizontal cohesion interactions at both levels. The estimates from the simultaneous model were nearly identical to those from the models in which the individual-level and unit-level interactions were estimated separately.
Figure 3 provides a summary of the mixed-effects models used to examine the interactive effects of combat exposure and horizontal cohesion (panel A) and the results of those models (panel B).
Figure 3.
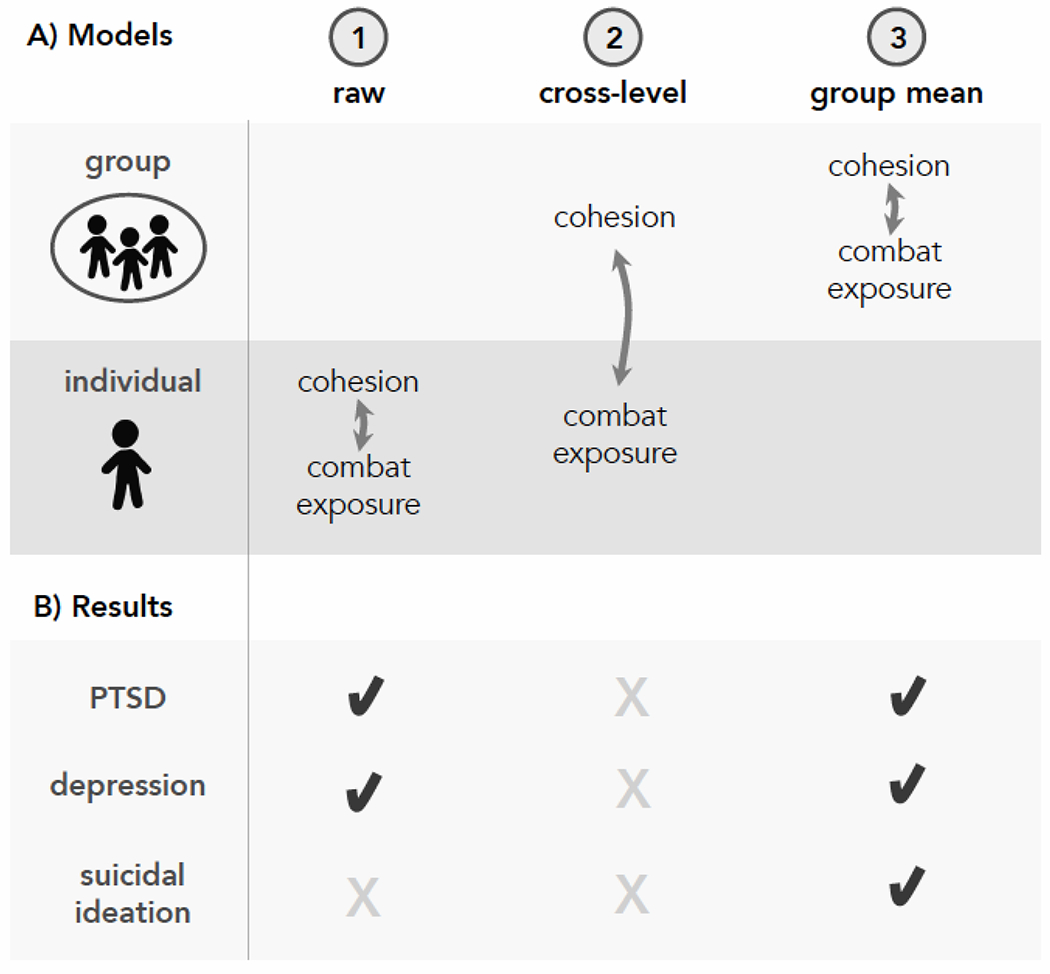
Summary of analytic models and results of analyses of the interactive effects of horizontal cohesion and combat exposure. The statistical interaction between horizontal cohesion and combat exposure was examined in a series of models (Panel A), which varied based on the levels at which cohesion and combat exposure were considered (i.e., group or individual). Results of each model of PTSD symptoms, depressive symptoms, and suicidal ideation are shown in Panel B. X = not statistically significant. ✔ = statistically significant; due to a large discrepancy in effective sample size for individual-level (ns=6,684 to 6,826) and unit-level (k=89) models, alpha was set at p<.05 for raw interaction and cross-level models and at p<.10 for group-mean models.
Buffering effects of vertical cohesion
Analogous models evaluated whether vertical cohesion moderated the relationships between combat exposure and post-deployment symptoms of PTSD (Supplementary Table S2), depression (Supplementary Table S3), and suicidal ideation (Supplementary Table S4). The Raw Interaction model of PTSD symptoms revealed that the relationship between individual reports of combat exposure and PTSD symptoms was attenuated for individuals who perceived high vertical cohesion (B= −0.03, p< 0.05; Model 2.2S). None of the other interactions involving vertical cohesion were statistically significant.
Accounting for pre-deployment symptoms
To evaluate the robustness of our results, we also examined whether horizontal and vertical cohesion moderated the relationships between combat exposure and post-deployment symptoms of PTSD, depression, and suicidal ideation, controlling for pre-deployment (T0) levels of these outcomes. Consistent with the primary findings, the models revealed individual-level interaction effects of combat exposure and horizontal cohesion on PTSD symptoms (B= −0.07, one-tailed p< 0.05; Supplementary Table S5, Model 5.2S) and depressive symptoms (B= −0.05, one-tailed p< 0.01; Supplementary Table S6, Model 6.2S). Group-mean models also showed unit-level interaction effects of combat exposure and horizontal cohesion on PTSD symptoms (B= −0.76, one-tailed p= 0.07; Supplementary Table S5, Model 5.4S) and suicidal ideation (B= −0.31, one-tailed p= 0.09; Supplementary Table S7, Model 7.4S), which were significant at a 90% confidence level with slope values in the same direction as those in the main analysis. Additionally, a robust buffering effect of horizontal cohesion was observed in the group-mean model of depressive symptoms (B= −0.65, one-tailed p< 0.01; Supplementary Table S6, Model 6.4S). None of the other interactions involving horizontal cohesion were statistically significant.
With respect to vertical cohesion, the individual-level interaction effect of combat exposure and vertical cohesion on PTSD symptoms failed to replicate when T0 PTSD symptoms were included as a control (B= 0.00, p= 0.96). The other interactions involving vertical cohesion were also non-significant.
Discussion
The current study provides evidence that unit cohesion buffers effects of combat exposure on post-deployment mental health. Our analysis was novel in that it prospectively examined interaction effects of combat exposure and unit cohesion, differentiated between horizontal (peer-to-peer) and vertical (subordinate-to-leader) cohesion, and utilized methods that disaggregated individual- and unit-level effects. Results suggest that cohesion among peers in a military unit, as well as individual factors that influence perceptions of horizontal and vertical cohesion, operate to protect soldiers from some of the adverse psychological effects of combat.
At the unit level, buffering effects of horizontal cohesion were found for all three outcomes: PTSD symptoms, depressive symptoms, and suicidal ideation. However, the buffering effects of unit-level horizontal cohesion were strongest for post-deployment depression, even when pre-deployment unit-average depression was controlled. Interpersonal mechanisms have been theorized as central to the development and maintenance of depression (Markowitz and Weissman, 2004; Panzarella, Alloy, and Whitehouse, 2006); and evidence suggests that social support may protect against depression in particular by increasing positive reinforcement and coping processes that may be disrupted in mood disorders (Carvalho and Hopko, 2011). Consistent with this theoretical framework and empirical evidence, our analysis suggests that strong bonds among peers in a military unit may protect combat-exposed units from depression during the post-deployment period.
Overall, the unit-level results imply that policies and interventions that enhance horizontal cohesion may protect unit-wide mental health. It is not entirely clear why interactive effects involving group means were greater in magnitude than interactive effects involving individual-level perceptions. Among potential theoretical mechanisms, evidence suggests that social support may buffer impacts of stress on mental health by providing interpersonal sources of emotion regulation (Marroquin, 2011) as well as external feedback to counteract maladaptive thinking (Liu et al., 2015). Perhaps units with high horizontal cohesion provide an environment that benefits members broadly, regardless of whether a specific unit member actually perceives the unit as cohesive. Future studies could evaluate the effects of policies and interventions that promote horizontal cohesion, to determine whether these lead to improved mental health of units following combat deployments and other major stressors. Routine surveys of horizontal cohesion may also be worthwhile, as these assessments could identify units that might benefit from efforts to strengthen peer support and bonding.
Interestingly, we found no buffering effects of unit-level vertical cohesion. While our results did not demonstrate that bonds between subordinates and leaders mitigate the psychological effects of combat exposure, it is important to note that other evidence suggests that leaders play important roles in promoting the mental health of their units (e.g., facilitating care for mental health concerns; Hom et al., 2017). It is also possible that more fine-grained measures of vertical cohesion might reveal buffering effects. For instance, Bliese, Adler and Castro (2011) reported cross-level interaction effects involving platoon-level perceptions of junior officer leadership and combat exposure on PTSD symptoms, where the buffering effects were unique to shared perceptions of officers. This finding suggests that buffering effects involving vertical cohesion may depend on the type of unit leader (i.e., officers versus NCOs).
At the individual-level, our analysis revealed buffering effects of horizontal cohesion (for PTSD and depressive symptoms) and vertical cohesion (for PTSD symptoms only); however, the size of these effects was modest. Nevertheless, the individual-level results suggest that combat-exposed soldiers who personally view high levels of horizontal or vertical cohesion may be protected from mental health difficulties, irrespective of the overall levels of horizontal and vertical cohesion in their units. Efforts to help soldiers who perceive low cohesion to bond with peers and leaders may be beneficial, and are supported by the broader literature linking perceived social support to the physical, mental, and social well-being of service members (Brooks and Greenberg, 2018, Keane et al., 2006, Nock et al., 2013).
Results of this study must be considered in light of several limitations. First, the cohesion and depression scales were developed for this study and have not been validated against established measures. The PTSD measure captured past 30-day symptoms related to any stressful experience in the respondent’s life, and the survey did not permit differentiation of symptoms related to events experienced during the index deployment versus events experienced before or after that deployment. Future studies could investigate the effects of unit cohesion on PTSD symptoms attributed to events that occurred while the unit was deployed. Second, the study outcome measures were not available at T1 (upon return from deployment); thus, we did not fit models that controlled for T1 levels of PTSD symptoms, depression, and suicidal ideation. However, we were able to incorporate T0 measures of PTSD symptoms, depression, and suicidal ideation, which allowed us to test the robustness of our primary results and evaluate buffering effects of cohesion on change in symptoms from pre- to post-deployment. Future studies should also incorporate information about mental health during deployment, to investigate the effects of cohesion on post-deployment adjustment.
Third, the results may not generalize to Army units with different characteristics (e.g., units comprised of Reserve/Guard members) than the units surveyed in the PPDS. The size of units included in the study varied considerably, and we had inadequate power to examine whether buffering effects of horizontal and vertical cohesion varied based on unit size. Fourth, cohesion variables were measured upon return from deployment, which we assume predominantly captured soldiers’ impressions of cohesion during deployment. However, cohesion during the weeks and months after return from deployment may also affect mental health during the post-deployment period; this is an important avenue for future study. Finally, group cohesion is not static, and future studies should aim to incorporate information about changes in cohesion over time (e.g., across the deployment cycle) and how such changes relate to mental health outcomes.
In conclusion, we found that horizontal cohesion buffers effects of combat exposure on mental health and that effects are strongest when modeled as shared unit properties. Units that faced more combat in Afghanistan, but also had strong horizontal cohesion, exhibited lower average levels of PTSD and depressive symptoms after return from deployment. Additionally, the association between a unit’s average combat exposure and suicidal ideation was attenuated in units with high horizontal cohesion. Finally, individual soldiers who perceived high horizontal or vertical cohesion (regardless of their unit’s overall level of cohesion) were less susceptible to PTSD and depressive symptoms following high combat exposure, although individual-level buffering effects were substantially weaker than the corresponding unit-level effects. In terms of practical implications, our findings provide guidance for efforts to reduce the mental health burden of soldiers who deploy in support of combat operations. Efforts to support combat-exposed soldiers who report low horizontal or vertical cohesion may help reduce posttraumatic stress and depression. Moreover, policies and interventions that strengthen cohesion among peers may promote resilience of the unit as a whole. Routine monitoring of horizontal cohesion at the unit level, and further development and evaluation of programs designed to enhance bonds between soldiers, may help prevent adverse mental health outcomes following combat exposure.
Supplementary Material
Acknowledgments
The Army STARRS Team consists of Co-Principal Investigators: Robert J. Ursano, MD (Uniformed Services University of the Health Sciences) and Murray B. Stein, MD, MPH (University of California San Diego and VA San Diego Healthcare System)
Site Principal Investigators: Steven Heeringa, PhD (University of Michigan), James Wagner, PhD (University of Michigan) and Ronald C. Kessler, PhD (Harvard Medical School)
Army liaison/consultant: Kenneth Cox, MD, MPH (US Army Public Health Center)
Other team members: Pablo A. Aliaga, MA (Uniformed Services University of the Health Sciences); COL David M. Benedek, MD (Uniformed Services University of the Health Sciences); Laura Campbell-Sills, PhD (University of California San Diego); Carol S. Fullerton, PhD (Uniformed Services University of the Health Sciences); Nancy Gebler, MA (University of Michigan); Robert K. Gifford, PhD (Uniformed Services University of the Health Sciences); Meredith House, BA (University of Michigan); Paul E. Hurwitz, MPH (Uniformed Services University of the Health Sciences); Sonia Jain, PhD (University of California San Diego); Tzu-Cheg Kao, PhD (Uniformed Services University of the Health Sciences); Lisa Lewandowski-Romps, PhD (University of Michigan); Holly Herberman Mash, PhD (Uniformed Services University of the Health Sciences); James E. McCarroll, PhD, MPH (Uniformed Services University of the Health Sciences); James A. Naifeh, PhD (Uniformed Services University of the Health Sciences); Tsz Hin Hinz Ng, MPH (Uniformed Services University of the Health Sciences); Matthew K. Nock, PhD (Harvard University); Nancy A. Sampson, BA (Harvard Medical School); CDR Patcho Santiago, MD, MPH (Uniformed Services University of the Health Sciences); LTC Gary H. Wynn, MD (Uniformed Services University of the Health Sciences); and Alan M. Zaslavsky, PhD (Harvard Medical School).
Funding/Disclaimer:
Army STARRS was sponsored by the Department of the Army and funded under cooperative agreement number U01MH087981 (2009-2015) with the U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health (NIH/NIMH). Subsequently, STARRS-LS was sponsored and funded by the Department of Defense (USUHS grant number HU0001-15-2-0004). The contents are solely the responsibility of the authors and do not necessarily represent the views of the Department of Health and Human Services, NIMH, the Department of the Army, the Department of Veterans Affairs, or the Department of Defense.
Disclosures:
Dr. Stein has in the past three years been a consultant for Actelion, Aptinyx, Bionomics, Dart Neuroscience, Healthcare Management Technologies, Janssen, Oxeia Biopharmaceuticals, Pfizer, and Resilience Therapeutics. In the past 3 years, Dr. Kessler received support for his epidemiological studies from Sanofi Aventis; was a consultant for Johnson & Johnson Wellness and Prevention, Sage Pharmaceuticals, Shire, Takeda; and served on an advisory board for the Johnson & Johnson Services Inc. Lake Nona Life Project. Kessler is a co-owner of DataStat, Inc., a market research firm that carries out healthcare research. The remaining authors have no disclosures.
Footnotes
Ethical standards: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Anderson L, Campbell-Sills L, Ursano RJ, Kessler RC, Sun X, Heeringa SG, … Stein MB (2019). Prospective associations of perceived unit cohesion with postdeployment mental health outcomes. Depression and Anxiety, 36, 511–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armistead-Jehle P, Johnston SL, Wade NG, & Ecklund CJ (2011). Posttraumatic stress in U.S. Marines: The role of unit cohesion and combat exposure. Journal of Counseling and Development, 89, 81–88. [Google Scholar]
- Bates DM, Mächler M, Bolker B, & Walker S (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67, 1–48. [Google Scholar]
- Bliese PD, Adler AB, & Castro CA (2011). Research-based preventive mental health care strategies in the military. In ,Adler AB, Bliese PD, & Castro CA (Eds.), Deployment Psychology: Evidence-Based Strategies to Promote Mental Health in the Military (pp. 103–124). Washington, DC: American Psychological Association. [Google Scholar]
- Bliese PD, Maltarich MA, & Hendricks JL (2018). Back to basics with mixed-effects models: Nine take-away points. Journal of Business and Psychology, 33, 1–23. [Google Scholar]
- Breslau J, Setodji CM, & Vaughan CA (2016). Is cohesion within military units associated with post-deployment behavioral and mental health outcomes? Journal of Affective Disorders, 198, 102–107. [DOI] [PubMed] [Google Scholar]
- Brooks SK, & Greenberg N (2018). Non-deployment factors affecting psychological wellbeing in military personnel: Literature review. Journal of Mental Health, 27, 80–90. [DOI] [PubMed] [Google Scholar]
- Browne T, Iversen A, Hull L, Workman L, Barker C, Horn O, … Fear NT (2008). How do experiences in Iraq affect alcohol use among male UK armed forces personnel? Occupational and Environmental Medicine, 65, 628–633. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Griffith JE, Pace BT, Hinkson K, Bryan AO, Clemans TA, & Imel ZE (2015). Combat exposure and risk for suicidal thoughts and behaviors among military personnel and veterans: A systematic review and meta-analysis. Suicide and Life Threatening Behavior, 45, 633–649. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Ursano RJ, Kessler RC, Sun X, Heeringa SG, Nock MK, … Stein MB (2018). Prospective risk factors for post-deployment heavy drinking and alcohol or substance use disorder among US Army soldiers. Psychological Medicine, 48, 1624–1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho JP, & Hopko DR Behavioral theory of depression: reinforcement as a mediating variable between avoidance and depression. Journal of Behavior Therapy and Experimental Psychiatry, 42, 154–162. [DOI] [PubMed] [Google Scholar]
- Griffith J (2015). Cross (unit)-level effects of cohesion on relationships of suicide thoughts to combat exposure, postdeployment stressors, and postdeployment social support. Behavioral Medicine, 41, 98–106. [DOI] [PubMed] [Google Scholar]
- Hines LA, Sundin J, Rona RJ, Wessely S, & Fear NT (2014). Posttraumatic stress disorder post Iraq and Afghanistan: Prevalence among military subgroups. Canadian Journal of Psychiatry, 59, 468–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, & Milliken CS (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association, 295, 1023–1032. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, & Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351, 13–22. [DOI] [PubMed] [Google Scholar]
- Hofmann DA, & Gavin MB (1998). Centering decisions in hierarchical linear models: Implications for research in organizations. Journal of Management, 24, 623–641. [Google Scholar]
- Hom MA, Stanley IH, Schneider ME, & Joiner TE Jr. (2017). A systematic review of help-seeking and mental health service utilization among military service members. Clinical Psychology Review, 53, 59–78. [DOI] [PubMed] [Google Scholar]
- Joint Mental Health Advisory Team 7 (J-MHAT 7) (2011). Joint Mental Health Advisory Team 7 (J-MHAT 7) Report. Retrieved from: https://armymedicine.health.mil/Reports
- Jones N, Seddon R, Fear NT, McAllister P, Wessely S, & Greenberg N (2012). Leadership, cohesion, morale, and the mental health of UK Armed Forces in Afghanistan. Psychiatry, 75, 49–59. [DOI] [PubMed] [Google Scholar]
- Kanesarajah J, Waller M, Zheng WY, & Dobson AJ (2016). Unit cohesion, traumatic exposure and mental health of military personnel. Occupational Medicine, 66, 308–15. [DOI] [PubMed] [Google Scholar]
- Keane TM, Marshall AD, & Taft CT (2006). Posttraumatic stress disorder: Etiology, epidemiology, and treatment outcome. Annual Review of Clinical Psychology, 2, 161–97. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Colpe LJ, Fullerton CS, Gebler N, Naifeh JA, Nock MK, … Heeringa SG (2013). Design of the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). International Journal of Methods in Psychiatric Research, 22, 267–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Stein MB, Petukhova MV, Bliese P, Bossarte RM, Bromet EJ, … Army STARRS Collaborators (2017). Predicting suicides after outpatient mental health visits in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Molecular Psychiatry, 22, 544–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, & Ustun TB (2004). The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research, 13, 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, & Samper RE (2006). Deployment Risk and Resilience Inventory: A collection of measures for studying deployment related experiences of military personnel and veterans. Military Psychology, 18, 89–120. [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Kleiman EM, Nestor BA, & Cheek SM (2015). The hopelessness theory of depression: A quarter century in review. Clinical Psychology, 22, 345–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz JC, & Weissman MM (2004). Interpersonal psychotherapy: principles and applications. World Psychiatry, 3, 136–139. [PMC free article] [PubMed] [Google Scholar]
- Marroquin B (2011). Interpersonal emotion regulation as a mechanism of social support in depression. Clinical Psychology Review, 31, 1276–1290. [DOI] [PubMed] [Google Scholar]
- Mental Health Advisory Team (MHAT) 6 (2009). Mental Health Advisory Team (MHAT) 6 Operation Enduring Freedom 2009 Report. Retrieved from: https://armymedicine.health.mil/Reports.
- Mitchell MM, Gallaway MS, Millikan AM, & Bell M (2012). Interaction of combat exposure and unit cohesion in predicting suicide-related ideation among post-deployment soldiers. Suicide and Life Threatening Behavior, 42, 486–494. [DOI] [PubMed] [Google Scholar]
- Nock MK, Deming CA, Fullerton CS, Gilman SE, Goldenberg M, Kessler RC, … Ursano RJ (2013). Suicide among soldiers: a review of psychosocial risk and protective factors. Psychiatry, 76, 97–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panzarella C, Alloy LB & Whitehouse WG (2006). Expanded hopelessness theory of depression: On the mechanisms by which social support protects against depression. Cognitive Therapy and Research, 30, 307–333. [Google Scholar]
- Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Rivers AJ, Morgan CA, & Southwick SM (2010). Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom: The role of resilience, unit support, and postdeployment social support. Journal of Affective Disorders, 120, 188–192. [DOI] [PubMed] [Google Scholar]
- Pinheiro J, Bates D, DebRoy S, Sarkar D, & R Core Team (2019). nlme: Linear and nonlinear mixed effects models. R package version 3.1-141 [Computer software]. [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, … Mann JJ (2011). The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. American Journal of Psychiatry, 168, 1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods. Sage: Thousand Oaks, CA. [Google Scholar]
- Shaver JM, (2019). Interpreting interactions in linear fixed-effect regression models: When fixed-effect estimates are no longer within-effects. Strategy Science, 4, 25–40. [Google Scholar]
- Smith TC, Ryan MA, Wingard DL, Slymen DJ, Sallis JF, Kritz-Silverstein D, & The Millennium Cohort Study (2008). New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: Prospective population based US military cohort study. BMJ, 336, 366–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ursano RJ, Colpe LJ, Heeringa SG, Kessler RC, Schoenbaum M, Stein MB, & Army STARRS Collaborators (2014). The Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Psychiatry, 77, 107–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ursano RJ, Kessler RC, Naifeh JA, Herberman Mash H, Fullerton CS, Aliaga PA, … Stein MB (2018). Associations of time-related deployment variables with risk of suicide attempt among soldiers: Results From the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). JAMA Psychiatry, 75, 596–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, & Vasterling JJ (2008). Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment, 15, 391–403. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, & Keane T (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the annual convention of the International Society for Traumatic Stress Studies: San Antonio, TX. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


