Abstract
Background
Intensive care unit (ICU)–ward patient transfers are inherently high risk, and clinician miscommunication has been linked to adverse events and negative outcomes. Despite these risks, few educational tools exist to improve resident handoff communication at ICU–ward transfer.
Objective
We used human-centered design (HCD) methods to cocreate a novel electronic health record ICU–ward transfer tool alongside Internal Medicine residents at three academic hospitals.
Methods
We conducted HCD workshops at each hospital, performing process mapping, brainstorming, and rapid prototyping. We performed thematic analysis on verbatim-transcribed workshop audio recordings to inform development and adaptation of the final resident prototype into the ICU-PAUSE tool.
Results
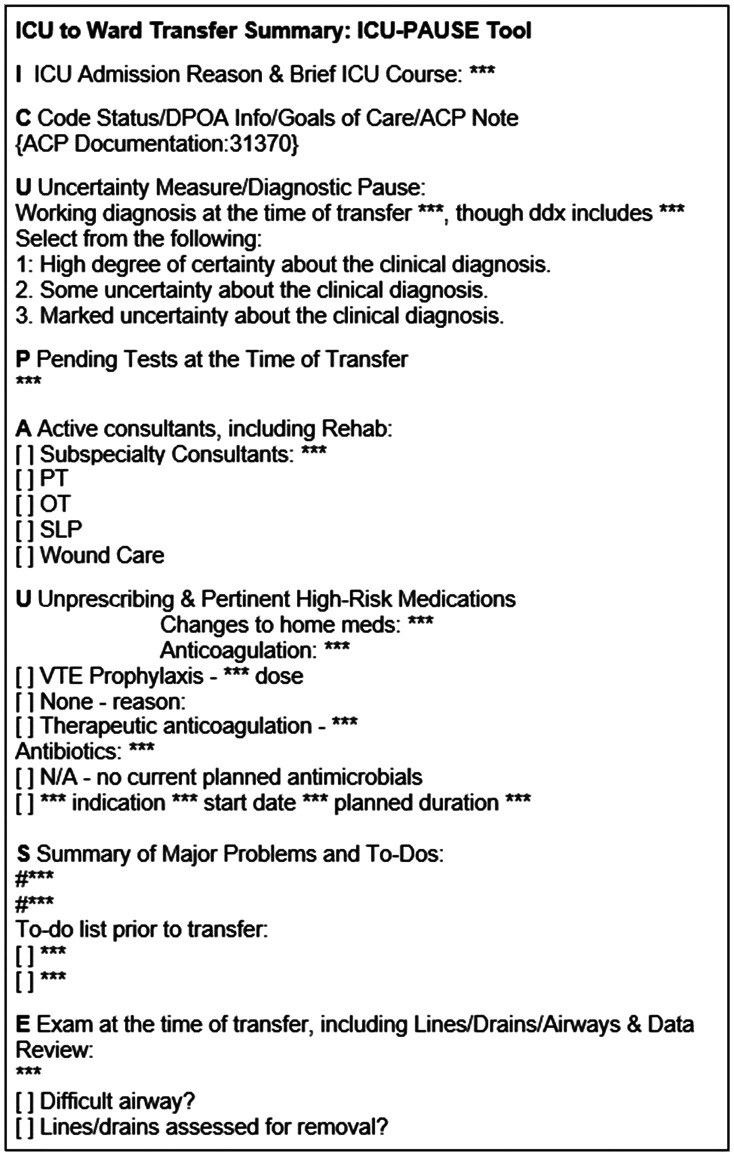
ICU-PAUSE focuses on reasons for ICU admission and problem-based ICU course (I); Code status, goals of care, and family contacts (C); a diagnostic pause acknowledging Uncertainty (U); Pending tests (P); Active consultants (A); high-risk medications, including medications to be Unprescribed (U); Summary of problems and to-dos (S); and a current physical Exam (E).
Conclusion
We used HCD to cocreate a novel, more user-friendly electronic ICU–ward transfer tool, ICU-PAUSE, alongside Internal Medicine trainees. Future steps will involve formal usability testing, evidence-driven implementation, and clinical evaluation of ICU-PAUSE across multiple hospitals.
Keywords: transitions of care, handoffs, quality-improvement education, human-centered design, qualitative research methods
Patients transferring from the intensive care unit (ICU) to the hospital wards are vulnerable because of patient complexity, clinical uncertainty, and nonintersecting communication between physicians and nurses (1). For day–night shift handoffs, structured communication with the IPASS framework, which has been used at many residency training programs, reduces medical errors and adverse events in the hospital (2). However, no analogous structures exist for ICU–ward transitions, and the IPASS framework does not readily translate to this transition of care.
ICU–ward transitions are managed heterogeneously across health systems (1), which may affect hospital quality and safety (3). Interventions to improve handoff communication must be designed with local context and educational objectives in mind if they are to be accepted, successfully implemented, and sustained (4). This imperative is especially important for electronic health record (EHR) interventions, for which the user experience depends on regulatory, organizational, and vendor priorities rather than those of users, particularly when users are residents who are frequently rotating on and off service (5).
Clinician transfer notes are an important element of high-quality handoffs. Recently, an expert panel deemed more than 60 items essential for ICU–ward handoff communication (6), a number that risks increasing documentation burdens and cognitive load. However, this panel did not address form, length, consistency, or other elements of a high-quality transfer note. Potentially, a more flexible process for developing a handoff tool could yield a more acceptable product, particularly for trainees, where documentation may serve as a communication tool to other clinicians and as a method for synthesizing clinical reasoning. Furthermore, because resident physicians both “give” and “receive” these handoffs, they bring important knowledge and insight to this problem from several perspectives.
The objective of this study was to allow front-line resident physicians to improve the ICU-to-ward transition process by generating a novel trainee-centered EHR-embedded tool for structured ICU–ward handoffs, using human-centered design (HCD) methods.
Methods
Theory
The project’s approach was grounded in HCD, an iterative approach to problem solving in which stakeholders are involved in all steps, from problem identification through prototype testing and evaluation (7, 8). We selected these methods to obtain detailed trainee input in the process of cocreating an EHR tool rather than the traditional top-down method of tool deployment. Our focus group guide (see Appendix E1 in the online supplement) was cognitively pretested to avoid bias and leading questions. We also tried to achieve principles of mixed-methods integration (9) by incorporating input from focus groups with principles gleaned from our prior work in the handoff literature to come up with prototypes of the tool.
Research Team Characteristics
Coinvestigators P.G.L., J.C.R., and L.S. served as faculty champions at their respective geographically diverse academic medical centers. All three had connections with the Internal Medicine residencies to enable buy-in from stakeholders. P.G.L. and L.S. have formal HCD training. L.S. and P.G.L. have formal qualitative research methods training through master’s degrees.
Timeline, Recruitment, and Participant Selection and Engagement
Between July 2019 and July 2020, we invited Internal Medicine residents (post-graduate year [PGY]-2s and PGY-3s who had already rotated in ICUs) at the University of California San Francisco, the University of Chicago, and Washington University in St. Louis to focus groups to reimagine the ICU-to-ward transition. Because resident physicians are the proximate clinicians for essentially all patients transferring from the medical ICUs at our hospitals, we restricted these sessions to residents.
Ethical Considerations
Workshops were voluntary and did not involve individual participation incentives. The institutional review boards of all three hospitals determined this study to be exempt. We presented preliminary results from this project at the 2020 American Thoracic Society International Conference (10).
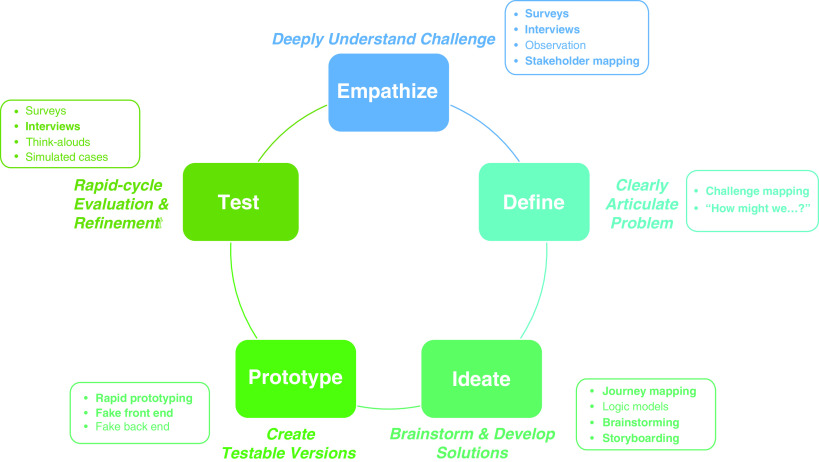
HCD
We anchored our methodology in HCD (8, 9), which is a process that aims to make interventions accessible to users and beneficiaries, and thereby effective, by longitudinally connecting user needs and preferences to creation and testing. HCD is a structured process that takes users through certain predefined steps: empathy, problem identification, ideation, prototyping, and testing.
Empathy, Problem Identification, and Ideation
Each site conducted an initial 120-minute workshop to introduce HCD and engage trainees in early HCD steps. Asking broadly, “How might we improve patient transitions from the ICU to the ward?” we facilitated several HCD activities through the key steps: journey/process mapping (empathy), brainstorming (problem identification), and prototype mapping (ideation), in which participants converged on ideas for prototyping. Each activity lasted approximately 30 minutes, including periods for silent reflection and note taking followed by small group discussions and large group readouts. Artifacts collected included brainstorming using Post-it notes as well as storyboards for the in-person sessions.
Rapid Prototyping, Evaluation, and Revision
Each site subsequently conducted additional 120-minute design workshops (two per site, six workshops total) via videoconference in light of the coronavirus disease (COVID-19) pandemic (11). Subsequent workshops included a subset of participants from the first session at each site, as well as participants who had not previously participated, to maximize the number of potential perspectives and avoid “groupthink.” We used trainee feedback to iteratively modify the prototypes in a subsequent workshop in a convergent manner toward an ideal future state. Residents examined and gave iterative feedback on two different versions of the EHR tool using A/B testing (a standardized comparison between two versions of a product, commonly used in software design, with different versions presented first or second randomly) (12) as part of a Microsoft PowerPoint slide deck and a virtual whiteboard.
Finally, we discussed final versions of the tool with local ICU leadership and synthesized content into the ICU-PAUSE tool.
Data Acquisition and Qualitative Analysis
With participants’ consent, we continuously audio-recorded all sessions and transcribed recordings verbatim. Two investigators (L.S. and B.G.) independently coded transcripts using both a theory-driven (inductive) and a data-driven approach within Dedoose software, reconciling disparate codes via discussion (13). We performed thematic content analysis following Standards for Reporting Qualitative Research (14). Using themes from the residents’ focus groups, we used their responses of components of an ideal handoff tool to create prototypes of the ICU-PAUSE handoff tool and then iteratively modified these prototypes in a subsequent resident workshop.
Qualitative analysts included a medical education researcher with experience in qualitative research in health professions education (L.S.) and a medical student researcher with experience in qualitative analysis (B.G.). We first categorized focus group content into domains that aligned with ideas for an ideal handoff tool. We later used these domains to create a priori codes for in-depth coding of all focus group transcripts. During coding, the two primary analysts coded each focus group independently and met to reconcile coding differences and reach consensus.
A graphical depiction of methods is summarized in Figure 1.
Figure 1.
Human-centered design phases, objectives, and example methods. Bold font indicates specific methods used for the current project. Stakeholder mapping visualizes all potential stakeholders and beneficiaries of a project and their relationships to the intervention. Challenge mapping uses insights from prior fieldwork to partition a large problem into discrete addressable subproblems and areas of potential solutions. “How might we…?” questions reframe barriers into opportunities for creative problem solving. Journey mapping visualizes each stakeholder’s external and internal interactions with a problem such that opportunities for innovation can be identified. Brainstorming involves formal exercises to generate and exchange new ideas. Storyboarding involves roughly visualizing potential innovations or solutions chronologically. Rapid prototyping involves iterative, generally low-fidelity, creation and revision of solutions developed during the ideation phase. Fake front and back ends involve creation of either user-facing (e.g., interactive screen which mirrors, but is not connected to, the her, such that user behavior can be safely observed) or developer-facing (e.g., isolated development mode to test secure login) scenarios.
Results
We engaged 4–10 stakeholders per session. Trainees identified three main themes around the role, content, and workflows related to an ideal ICU–ward handoff tool: 1) views of how a handoff tool can best serve the needs of ICU and wards teams; 2) expectations that the ICU–ward handoff must strike an appropriate balance between thoroughness and usability; and 3) realizations that design and implementation must consider user experience and best practices.
Under these themes, trainees identified specific attributes of an ideal handoff tool (Table 1), which coalesced around three goals: 1) the tool should synthesize key information and communicate the ICU team’s clinical reasoning; 2) the new tool should be integrated within a customizable EHR note template, minimizing clicks and redundancy; and 3) the tool should be a standardized outline to reduce errors of omission in handoff processes. Repeatedly, trainees described the importance of current and accurate information within handoff notes, while highlighting the difference between receiver uncertainty due to poor information transfer and uncertainty due to ongoing workups and inconclusive testing. Contrastingly, residents described a “trust but verify” mindset, through which handoff receivers cross-reference new information against their own history taking and review of records.
Table 1.
Residents’ desired elements for an intensive care unit–ward handoff tool
| Themes | Subthemes | Representative Quotations |
|---|---|---|
| Synthesizing information and communicating clinicians' reasoning | Clear description of patient course | “There are hopefully no mysteries.” |
| Prioritization of problems and tasks | “If I were receiving a patient, the to-dos and the pending stuff is more important to me than the tubes/lines/drains.” | |
| Action items and pending studies | “I like the prompts for the categories for the pending tests. That’s definitely something that can get lost.” | |
| Explicit contingency planning and anticipatory guidance | “I feel like there’s something that's missing that’s saying contingency plans, like oh, heads up, this patient is different from others and when those things happen, you should do this.” | |
| ACP | “If the ICU team has an ACP note, to point to it and make sure that it’s updated before transition prevents a lot of duplication of records.” | |
| Medications | “I always liked the ‘changes to home meds’ part...long-time home meds get held and then that’s forgotten on the floor and then it comes to discharge on the floor and you are like, why were we holding this in the first place?” | |
| Visualization (graphical timeline) | “I think this timeline would also be helpful not just for when you’re signing out to the primary team on the floor, but as coming back from when you're switching from days to nights or nights to days. Oftentimes you come in to patients that have been there for 24–48 h. So, I feel like this would be a concise way for you to quickly grasp what has really happened to that patient in kind of a snapshot view instead of clicking through Epic and looking through all the notes and trying to piece it together that way.” | |
| Illness severity during ICU stay | “What was their max dose of pressor and when were they on it? That can be really challenging to figure out if they've had an extended ICU stay. It’s also very clinically relevant on the floor to know how sick they got.” | |
| Vital contact information | “Right now what we have is the main person that we’ve been updating every day, since we do have to update families over the phone, and they can’t be there.” | |
| Customizable electronic health record integration to minimize clicks | Customizable | “If you could have a master document where you could customize what was where then, so things were pulled in but only used if you really wanted them, and certain sections could be expanded if you were using it for rounding or for team communication and then collapsed or minimized if you didn’t think they were essential…. Being able to drag, resize, and collapse could help it be more multifunctional.” |
| Multifunctionality | “I feel like the more functions a document serves, you use it for day-to-day handoffs between providers and for sign-out, etc., and for rounds, the more likely it is to be, to maintain in a way that is useful.” | |
| Reliability of information | “The less clunky it is, the easier it is to use… the more likely information is to be accurate.” | |
| Autopopulates text | “Do you think that this auto-importing loses some of the analysis and synthesis of being a physician and writing this yourself? I think some of the autoimporting is at risk of losing some of the credibility that you have of physically typing it.” | |
| Expandable for details | “It should expand and collapse based on what you put inside it.” | |
| Standardization to reduce errors of omission | Standardizing content to save time | “I think if we’re going to ask people to write summaries, which I think we should, a lot of the rest of this stuff you have listed here should be as dropdown or as auto-populated as possible, just for time’s sake. That's a lot of work for a transfer note.” |
| Explicit communication about family updates | “In terms of workflow, there should be...the ICU team, if they’re primary, should be calling the families and saying, just like we're updating every day, and saying, ‘today they’re transferring out of the ICU. You will receive a call from a different team.’ So there's no break in the communication.” | |
| Standardized information visible to all stakeholders | “I really like this as a way to short circuit that…. It’s just a nice way to get everyone on the same page before they leave.” | |
| Oversight from senior team members | “Maybe it’s something that the more experienced person on the team will be the person to be in charge of it every day and make sure it’s updated. So the senior, if they're supervising two interns, that will be maybe part of their job on a shift is just to run through those handovers and make sure they're up to date, and that unnecessary information has been removed and that they’re relatively streamlined.” |
Definition of abbreviations: ACP = advanced care planning; ICU = intensive care unit.
Based on residents’ prototypes, we converged upon the ICU-PAUSE tool (Figure 2) for ICU–ward transfer summaries. ICU-PAUSE focuses on reasons for ICU admission and problem-based ICU course (I); Code status, care goals, and family contacts (C); a diagnostic pause to acknowledge and document clinical Uncertainty (U); Pending tests (P); Active consultants (A); high-risk medications including medications to be Unprescribed (U); a Summary of major problems and outstanding action items (S); and an accurate, current physical Examination (E).
Figure 2.
Proposed ICU-PAUSE electronic tool. ACP = advanced care planning; ddx = differential diagnosis; DPOA = designated power of attorney; ICU = intensive care unit; N/A = not applicable; OT = occupational therapy; PT = physical therapy; SLP = speech and language pathology; VTE = venous thromboembolism.
Notably absent from this transfer note template are elements such as patient allergies, isolation status, and location. Although residents agreed these elements remain important for safe and effective patient care, they overwhelmingly desired to avoid including this information in the template because of its prominence elsewhere in the EHR. For example, one participant said “The less clunky it is, the easier it is to use. The more likely information is to be accurate.” Another participant noted, “If I were receiving a patient, the to-dos and the pending stuff is more important to me than the tubes/lines/drains.”
Discussion
We used HCD methods to develop a novel electronic health record tool to improve ICU–ward handoffs alongside residents at three academic medical centers. By working to empathize with handoff senders and receivers, we documented facilitators and barriers to successfully transitioning patients from the ICU to the wards, identified important priorities for a new handoff note tool, and developed and updated prototype tools until converging upon ICU-PAUSE.
Our work is innovative in several important ways. First, although clinical note templates may improve documentation outcomes (15), descriptions of template design methods and procedures are sparse. In one study, experienced reviewers judged notes using a redesigned template to be less accurate and less useful than prior-state notes, despite resident perceptions of improved organization and visual appeal (16). Notably, these redesigned notes were informed mainly via external resources (research and a national organization position statement), rather than specific needs of users and other stakeholders.
By contrast, HCD may improve accessibility, and thereby effectiveness, of an intervention by anchoring the creation process in the user and beneficiary needs and preferences at all steps. These benefits are particularly salient for tools to support EHR notes and tools, which are frequently both over- and underdesigned at the same time (17, 18) and are often designed with minimal or no end-user input (5).
Second, this same potential benefit applies specifically to ICU–ward transfers, which are relatively understudied compared with other in-hospital care transitions despite their inherently high risk. Recently, de Grood and colleagues described a modified Delphi process by which an expert panel listed essential ICU–ward handoff items (6). Although thorough, this list might increase documentation burdens on the composer, information overload for the receiver, or both. Furthermore, the list describes content alone but does not address the order, depth, consistency, or other elements of a high-quality transfer note. Given the emphasis our participants placed on balancing thoroughness with brevity, organization, and clarity, we speculate that our approach may yield a more acceptable product.
Third, although HCD methods are becoming more frequently used in applied clinical informatics, they remain underused overall. In the era of COVID-19, we discovered that HCD methodology was easily adaptable, with modest modifications allowing us to continue our original curricular intervention (11). To preserve the fidelity of the design process, we continued to adhere to the HCD methodology while adapting to the virtual environment, thus rapidly prototyping and cocreating the sessions digitally. HCD’s flexible methodology allowed us to meet residents’ needs even through our COVID-19–driven pivot to virtual prototyping.
Finally, we deliberately included a “diagnostic pause” moment within this tool, as well as in its name, to highlight the importance of diagnostic uncertainty (18). In focus groups, residents highlighted the importance of accurate handoff and highlighted uncertainty due to information transfer: residents and patient safety experts alike note that care transitions represent natural moments for explicit acknowledgment and discussion of diagnostic uncertainty to decrease the risk of poor information transfer and avoid premature closure.
Strengths and Limitations
Beyond these important innovations, our study has several strengths. First, conducting design sessions at multiple geographically diverse hospitals may improve generalizability. Despite the marked differences in handoff processes across our institutions (1), there was convergence of opinion by residents in focus groups across institutions, suggesting that this intervention may be generalizable to other academic medical centers. By including both PGY2 and PGY3 residents, we sought perspectives across a continuum of experience and comfort constructing and reviewing ICU–ward handoff notes. Finally, we applied rigorous standards to our qualitative methods, in keeping with current guidelines.
Limitations include the small number of self-selected residents and our restriction to Internal Medicine trainees, both of which could hinder generalizability. Further work must include important perspectives from other stakeholders such as faculty, advanced practice providers, nurses, and patients and families.
Moreover, we have not yet evaluated implementation data or outcome data regarding the use of the tool in academic medical centers by internal medicine trainees. Further research will be needed to implement and evaluate the use of this tool at academic and community medical centers. Further research could also evaluate the use of this tool for written handoff as part of a bundle of interventions including both oral and written components.
Conclusions
We used HCD to cocreate a novel, user-friendly ICU–ward transfer tool, ICU-PAUSE, alongside Internal Medicine trainees. Future steps will involve formal usability testing, evidence-driven implementation, and clinical evaluation of ICU-PAUSE across multiple hospitals.
Supplementary Material
Footnotes
Supported by the American Thoracic Society, CHEST, and APCCMPD (L.S.); NHLBI-KL2 TR002346 (P.G.L.); and a Big Ideas award from the Institute for Informatics at Washington University in St. Louis, the Healthcare Innovation Lab at Washington University in St. Louis, and BJC HealthCare.
Author Contributions: L.S., J.C.R., B.G., M.T., and P.G.L. made substantial contributions to the conception or design of the work or the acquisition, analysis, or interpretation of data for the work; drafted the work or revised it critically for important intellectual content; provided final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
This article has a data supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Santhosh L, Lyons PG, Rojas JC, Ciesielski TM, Beach S, Farnan JM, et al. Characterising ICU-ward handoffs at three academic medical centres: process and perceptions. BMJ Qual Saf . 2019;28:627–634. doi: 10.1136/bmjqs-2018-008328. [DOI] [PubMed] [Google Scholar]
- 2. Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD, et al. I-PASS Study Group Changes in medical errors after implementation of a handoff program. N Engl J Med . 2014;371:1803–1812. doi: 10.1056/NEJMsa1405556. [DOI] [PubMed] [Google Scholar]
- 3. Landrigan CP, Rahman SA, Sullivan JP, Vittinghoff E, Barger LK, Sanderson AL, et al. ROSTERS Study Group Effect on patient safety of a resident physician schedule without 24-hour shifts. N Engl J Med . 2020;382:2514–2523. doi: 10.1056/NEJMoa1900669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Urquhart R, Kendell C, Cornelissen E, Powell BJ, Madden LL, Kissmann G, et al. Identifying factors influencing sustainability of innovations in cancer survivorship care: a qualitative study. BMJ Open . 2021;11:e042503. doi: 10.1136/bmjopen-2020-042503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tutty MA, Carlasare LE, Lloyd S, Sinsky CA. The complex case of EHRs: examining the factors impacting the EHR user experience. J Am Med Inform Assoc . 2019;26:673–677. doi: 10.1093/jamia/ocz021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de Grood C, Job McIntosh C, Boyd JM, Zjadewicz K, Parsons Leigh J, Stelfox HT, ICU Transfer Summary Consensus Panel Identifying essential elements to include in intensive care unit to hospital ward transfer summaries: a consensus methodology. J Crit Care . 2019;49:27–32. doi: 10.1016/j.jcrc.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 7. Lyon AR, Brewer SK, Areán PA. Leveraging human-centered design to implement modern psychological science: return on an early investment. Am Psychol . 2020;75:1067–1079. doi: 10.1037/amp0000652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stanford d.school 2019https://dschool.stanford.edu/resources.
- 9. Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res . 2013;48:2134–2156. doi: 10.1111/1475-6773.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rojas JC, Lyons PG, Garcia BM, Thomashow MA, Santhosh L. Design thinking to create user-centered intensive care unit-ward handoffs at three academic hospitals [abstract] Am J Respir Crit Care Med . 2020;201:A1401. [Google Scholar]
- 11. Santhosh L, Rojas JC, Lyons PG. Zooming into focus groups: strategies for qualitative research in the era of social distancing. ATS Scholar . 2021;2:176–184. doi: 10.34197/ats-scholar.2020-0127PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kohavi R, Tang D, Xu Y. Trustworthy online controlled experiments: a practical guide to A/B testing. New York: Cambridge University Press; 2020. [Google Scholar]
- 13.Tolley EE, Ulin PR, Mack N, Robinson ET, Succop SM. Qualitative methods in public health: a field guide for applied research. San Francisco: John Wiley & Sons; 2016. [Google Scholar]
- 14. O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med . 2014;89:1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 15. Kahn D, Stewart E, Duncan M, Lee E, Simon W, Lee C, et al. A prescription for note bloat: an effective progress note template. J Hosp Med . 2018;13:378–382. doi: 10.12788/jhm.2898. [DOI] [PubMed] [Google Scholar]
- 16. Epstein JA, Cofrancesco J, Jr, Beach MC, Bertram A, Hedian HF, Mixter S, et al. Effect of outpatient note templates on note quality: NOTE (Notation Optimization through Template Engineering) randomized clinical trial. J Gen Intern Med . 2021;36:580–584. doi: 10.1007/s11606-020-06188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duan Y, Narendray NC.2015. pp. 34–39.
- 18. Kassirer JP. Our stubborn quest for diagnostic certainty. N Engl J Med . 1989;321:1272–1273. doi: 10.1056/NEJM198911023211820. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.