Abstract
Background
Chronic tinnitus is a commonly occurring symptom of the auditory system. Epidemiological studies assume a lifetime prevalence in men and women of 3.5% for chronic tinnitus requiring treatment. Almost 25% of all Germans have experienced at least one episode of tinnitus. No causal therapy is yet available, but numerous treatment strategies are being pursued. Rigorous scientific assessment of these procedures is essential.
Methods
For this exhaustive revision of the German clinical practice guideline, the literature in the medical databases PubMed and Cochrane Library, including existing guidelines from various countries, was systematically searched using keywords on the topic of chronic tinnitus. On the basis of the revised guideline, a separate guideline was written in language accessible to patients.
Results
Chronic tinnitus is often associated with hearing loss, but the mental distress caused by the ear noise is another crucial element. Apart from expert counseling, the recommended treatment comprises psychotherapeutic interventions, particularly cognitive behavioral therapy (with effect sizes of 0.54 to 0.91 for reduction of the tinnitus-related distress), and measures to improve the hearing. There is insufficient evidence regarding the effects of drug treatment, sound and music therapy, and neuromodulation (magnetic stimulation or electrostimulation).
Conclusion
Alongside thorough and sound diagnosis and counseling, the principal treatment options for chronic tinnitus are specific cognitive behavioral therapy and expert psychotherapeutic interventions on an individual or group basis. Future—preferably interdisciplinary—research should evaluate the long-term effects of the treatment options, with particular attention to psychosomatic comorbidity.
Tinnitus is a very frequent symptom of impaired auditory processing. According to epidemiological studies in Europe and the USA, around a quarter of all people have experienced at least one episode. Around 10 to 15% of persons are affected by tinnitus over an extended period. Women and men are affected almost equally, and the prevalence increases at advanced age (> 65 years). The main risk factors are noise exposure, hearing loss, and mental stressors. However, only 3 to 5% are deemed to require treatment. Of these, half are seriously affected, impairing their ability to conduct and organize their lives (1, 2, e1, e2). The actual distress (3) arises essentially from comorbidities (Box 1, Box 2), but also from the degree of hearing loss (4– 6).
BOX 1. Typical comorbidities in chronic tinnitus.
1. Psychological/psychosomatic/psychiatric comorbidities
-
1.1. Mood disorders (frequency 37%*)
Dysthymia (ICD-10: F34.1)
Depressive episode (ICD-10: F32.0, F32.1, F.32.2, F32.3)
Recurrent depressive episodes (ICD-10: F33.0, F33.1, F33.2, F33.3)
-
1.2. Anxiety disorders (frequency 32%*)
Phobic disorders (ICD-10: F40)
e.g., specific phobia (ICD-10: F40.2)
Anxiety disorders (ICD-10: F41)
e.g., generalized anxiety disorder (ICD-10: F41.1)
Anxiety and depressive disorder, mixed (ICD-10: F41.2)
-
1.3. Reactions to severe stress and adjustment disorders
Acute reaction to burdening (ICD-10: F43.0)
Posttraumatic stress disorder (ICD-10: F43.1)
Adjustment disorder (ICD-10: F43.2)
-
1.4. Somatoform disorders (frequency 27%*)
Somatization disorder (ICD-10: F45.0)
Hypochondriacal disorder (ICD-10: F45.2)
Somatic stress disorder (bodily distress disorder, bodily distress syndrome) (ICD-11)
1.5. Psychological factors or behavioral factors associated with disorders or diseases classified elsewhere (ICD-10: F54) (frequency 4%*)
*Frequencies according to e3 and e4
BOX 2. Impairments resulting from tinnitus and comorbidities.
-
Impairment of the cognitive–emotional response system
Loss of concentration
Loss of control
Catastrophizing
Resignation
Dysfunctional thoughts
Impairment of life perspectives
Reduction of life coping skills
Loss of self-esteem
Helplessness
-
Impairment of the behavioral response system
Falling and staying asleep
Social withdrawal, isolation, avoidance behavior
Relationship disorder
-
Communication disorders
Accompanying hearing loss
Recruitment (loss of loudness adjustment in inner ear hearing loss)
Impairment of auditive perception, dysacusis
Hyperacusis
-
Impairment of the physiological response system
Myofascial dysbalance in the region of the cervical spine
Tension of the jaw and masticatory muscles, bruxism, craniomandibular dysfunction
Headache
Otalgia
Drowsiness
Vestibular disorder
The distress is measured using validated questionnaires such as the Tinnitus Questionnaire (TQ) or its short form (Mini-TQ) according to Goebel and Hiller (e5), the German-language Tinnitus Impairment Questionnaire according to Greimel (TBF12), or the Tinnitus Handicap Inventory (THI), or with the Tinnitus Functional Index (TFI). Treatment should be based on differential diagnostic considerations regarding the causative factors and concomitant symptoms. To date, however, no causal therapy able to ’’switch off“ tinnitus has been discovered (7).
At the same time, numerous procedures and drug treatments have been tested in consumer observational studies, some of them scientifically evaluated, and in case studies and randomized trials (RCT). The empirical evidence for many of these approaches is, however, weak (8). This is directly relevant for the updated German clinical practice guideline on chronic tinnitus (9) developed under the guidance of the German Society of Oto-Rhino-Laryngology, Head and Neck Surgery. The guideline provides physicians, therapists, and also patients with an overview of the scientific evidence regarding the diagnosis and treatment of chronic tinnitus, with particular reference to novel procedures that are currently in evaluation. Decision making in affected persons is supported by an additional patient-centered guideline intelligible to the lay person (10).
Methods
The methods for the development of the current guideline comply with the regulations of the Association of the Scientific Medical Societies in Germany (AWMF) and were based on a systematic literature search in PubMed and the Cochrane Library from 2014 to 31 December 2020. The starting point for the update was the guideline of 2014. Newly identified studies were added to the tables.
Based on an extensive literature search and the evidence tables derived therefrom, recommendations regarding mandatory and supplementary diagnostic procedures for chronic tinnitus were established and consensus was reached. Data on health benefits, adverse effects, and risks were systematically collected and were considered in the formulation of the recommendations (for a detailed description of methods see the eMethods).
Results
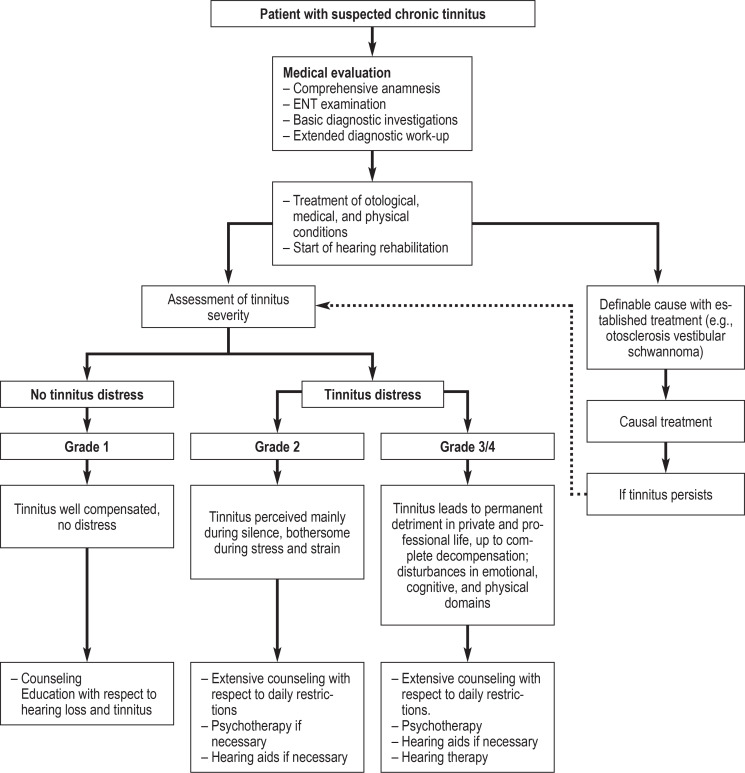
Based on a treatment algorithm established for the guideline (figure), the following sections evaluate the diagnostic procedures and therapeutic approaches and assess the evidence.
Figure.
Flowchart for treatment of chronic tinnitus
Diagnosis
In addition to otorhinolaryngological examination with otomicroscopy of the tympanum, the basic work-up includes complete audiometric assessment (sound and speech audiometry, measurement of impedance) and evaluation of the tinnitus. As an objective measure, brain-stem audiometry (BERA) is recommended for the exclusion of retrocochlear lesions such as the a very rare (1/100 000) vestibular schwannoma, for which tinnitus is almost always one of the first symptoms. Also recommended as an objective measure is the recording of otoacoustic emissions (TEOAE and/or DPOAE) to assess the functioning of the outer hair cells of the inner ear. This should be completed by basic examinations of the vestibular organ to detect spontaneous or provocation nystagmus and basic manual examinations of the masticatory apparatus and the cervical spine. Supplementary diagnostic procedures should be guided individually by the case history and the findings of the basic assessment. Tinnitus distress is measured by validated questionnaires (TQ, Mini-TQ, TBF12). In the most commonly used TQ (Mini-TQ), a score of 0–30 (0–7) represents a mild impairment, 31–46 (8– 12) a moderate impairment, 47–59 (13– 18) a severe impairment, and 60–84 (19– 24) the highest degree of impairment (e5).
Treatment
The guideline provides recommendations for the treatment of chronic tinnitus persisting for more than 3 months. For the treatment of acute tinnitus, particularly in association with or as a consequence of sudden hearing loss, the guideline on hearing loss (11) recommends systemic or intratympanic cortisone therapy.
Counseling and education
The starting point of every therapeutic intervention should be the counseling and education of the patient, based on comprehensive diagnostic assessment. The goal of tinnitus counseling is a psychoeducational explanation of the symptoms and the description of coping strategies to reduce fear and also to dampen excessive expectations of cure. Counseling provides the basis for the development of constructive habituation mechanisms and helps to avoid negative, self-reinforcing loops in the generation of tinnitus (12, 13). Particularly important is the message that effective therapeutic options do exist, even if the tinnitus cannot be directly “switched off.”. In many persons tinnitus disappears spontaneously without therapeutic intervention; however no studies exist and no precise percentages can be cited because a large number of such cases are not registered. Patients should, in particular, be advised of the self-help options (14).
Interventions for hearing loss
As tinnitus is associated with hardness of hearing in more than 90% of cases (8, e1), the use of devices in the treatment of hearing loss plays an important role and is therefore recommended. Regarding the efficacy of hearing aids for the treatment of tinnitus, the evidence strength of the studies published is only moderate or weak. This is mainly because only a small number of studies have been published investigating the efficacy of hearing aids specifically for the treatment of chronic tinnitus. Therefore, evidence cannot be reached even though clinical expertise suggests that hearing aids increase tinnitus suppression and habituation. In a large RCT, adjustment of hearing aids was found to be associated with amelioration of tinnitus by at least 20% in more than 70% of cases. Hearing aids were compared with devices combining hearing amplification and noise-generating functions (15). Similar results were found in a smaller study comparing high-compression hearing aids with normal hearing aids. Clinically relevant improvement was observed in 67 to 82% of patients, depending on the method employed (16). Good hearing aid provision requires intensive counseling and monitoring of patients, however, as shown by an American study of 133 hearing-impaired patients with tinnitus (17).
Better evidence exists for the treatment of severely hearing impaired and deaf tinnitus patients with a cochlear implant, even if the deafness is unilateral. However, the prevalence of such extensive hearing loss is, at 1.6%, much lower (e6). In a recent review (two RCTs and four prospective case–control studies with 136 patients overall), significant reduction of tinnitus suppression was achieved (average improvement of THI score 11.66 points, 95% confidence interval [17.65; 5.67]) (18). Renewed onset of tinnitus following implantation is possible in 0 to 10% of cases, but it is unclear whether this effect is attributable to the implantation or appears spontaneously. Generally, a large number of studies show a positive and also age-independent effect (e7, e8).
Hearing therapy, in which strategies are taught to distract attention away from the tinnitus sound, can support these effects, increase the acceptance of hearing aids and promote tinnitus habituation (19); however, this assessment is based on a single systematic review comprising 10 studies with just moderate (2a) evidence (20).
Noise generators (hearing aids that just emit a faint broadband noise) should not be recommended for tinnitus. A scoping review of 87 studies did not demonstrate efficacy (21).
Behavioral therapy and psychodynamic methods
Numerous studies show evidence for the efficacy of behavioral therapy interventions compared with both waiting-list control groups and active control groups for relief of tinnitus distress. Efficacy has been demonstrated for the various forms of behavioral therapy, with no significant differences between the forms of administration (e.g., face-to-face or online) and, to some degree, also for Internet-based behavioral therapy with no direct contact with the therapist. A Cochrane Review published in 2020 analyzed the results of 28 studies and found significant improvements in the THI score, with an average increase of 10.9 points. According to an older Cochrane Review (e9) the effect size lay between 0.54 and 0.91, according to the new review it was 0.56 (CI 0.30; 0.83). The reported improvement significantly surpasses the 7-point threshold value for a minimal clinically significant difference (22). The effect of psychodynamic interventions could be indirectly inferred because they frequently form part of multimodal treatment programs.
There are no indications for relevant side effects of (cognitive) behavioral therapy (CBT), but only some of the studies registered side effects systematically. There is no robust evidence for the long-term effects of more than 12 months of CBT because sufficient data are not available.
Psychodynamic and psychophysiologically oriented treatment methods with the goal of tinnitus habituation provide an important basis for the treatment of patients with chronic tinnitus, particularly if comorbidities that are evoked by tinnitus or reinforce tinnitus lead to significant distress. These treatment programs are administered on an outpatient or inpatient basis and are recommended with high evidence in the guideline. While the level of evidence for behavioral therapy is high, for psychodynamic methods—in the main depth psychology approaches—no randomized studies exist, and their effectiveness is at best indicated by catamnesis studies (e10). Prerequisites are the suitability of patients for such methods and their willingness to subscribe to the therapy and the underlying model. In the case of habituation as a consequence of a specific, cognitive learning process of the brain, the noise in the ear still exists but is perceived to a lesser degree or not at all in the absence of active focus on the tinnitus.
Tinnitus retraining therapy
Tinnitus retraining therapy (TRT) is a habituation technique intended to lessen the auditory, emotional, and autonomous impact of the tinnitus noise and thereby reduce the stress response to the tinnitus stimulus (23). After a detailed tinnitus history, distraction from the tinnitus is achieved by broadband noise delivered via a tinnitus device (noise generator) worn as a hearing-aid and non-standardized psychological counseling. While there is no evidence for short-term interventions, TRT can be considered for use as as a long-term intervention technique. An RCT showed significant improvement in the THI score after treatment for 12 months (e11). According to recent research the simultaneous prescription of noise generators can be dispensed with (24, 25).
Music and sound therapy
There is no evidence for music and sound therapies. Even tailor-made notched music training (TMNMT) should not be employed, because according to an RCT its effectiveness is no greater than that of placebo (26). This is also the case for acoustic (CR reset) neurostimulation, for which a review of eight studies with a total of 329 patients (one RCT, three non-controlled case–control studies) found no effect (27). Owing to the potentially harmful effect of tinnitus reinforcement and the high costs, there is a strongly negative recommendation for this method.
Drug treatment
There are no sufficient data on the effectiveness of drug treatment targeting tinnitus specifically, but there is evidence of potentially negative side effects. Based on systematic surveys and randomized studies, there is high evidence that betahistine (28), Ginkgo biloba extract (29), antidepressants, benzodiazepines, zinc, melatonin, cannabis, oxytocin, steroids, and gabapentin are not effective against chronic tinnitus and therefore cannot be recommended. This has to be distinguished from the drug treatment of frequent comorbidities of tinnitus such as anxiety disorders and depression. These comorbidities should be treated according to the available guidelines, which may include administration of drugs.
Dietary supplements
Dietary supplements such as vitamins, traditional Chinese–Korean herbal medicine, minerals, homeopathy, and lipoflavonoids should not be used in the treatment of tinnitus, because no proof of concept has been provided (30, 31).
Neuromodulation
The following so-called neuromodulation techniques seek to influence the neuronal excitability of the cortex, especially the auditory cortex, by direct, either magnetic or electric stimulation:
Repetitive transcranial magnetic stimulation (rTMS)
Transcranial (tDCS) and invasive electrostimulation
Bimodal acoustic and electric stimulation (vagus or trigeminus)
Low-level laser therapy
As the proof of concept for these methods is either contradictory (rTMS), or has not been demonstrated robustly, they should not be used. Most of the studies carried out are either not placebo-controlled or, if placebo-controlled, demonstrate non-effectiveness (32, 33). Some reviews are contradictory in their evaluation (34, e12, e13), while for bimodal vagus or trigeminus nerve stimulation no robust studies have yet been published (35, 36) and the existing studies are not placebo-controlled and afflicted by bias (37). Low-level laser therapy (formerly referred to as “soft laser”) has been available for many years, but there is no evidence of either safety or therapeutic effects in tinnitus. Controlled studies and meta-analyses are lacking (38, e14).
Manual medicine and physiotherapy
If modulation of tinnitus is detected during the initial basic investigation of the cervical spine and masticatory apparatus and the findings of supplementary manual medicine examination point to involvement of the cervical spine, temporomandibular joint function, and muscular trigger points or dysbalances, manual medicine and physiotherapy should be employed. The stated frequency of such causal involvement ranges very widely, however, from rare (8) to 30–40% (40), including vague, imprecise reports (e15). If the association is clear, physiotherapy, including exercises and trigger point treatments, can have positive effects on the severity of the tinnitus. However, reviews have described the methodological quality of the RCT they analyzed as poor (39, 40).
Conclusion
There is little or no evidence for many of the therapeutic approaches evaluated in the new German clinical practice guideline on chronic tinnitus, particularly for drug treatment and device-supported methods. Reasonable and effective treatment of tinnitus remains possible, however, and the new clinical practice guideline gives evidence-based recommendations:
The treatment of chronic tinnitus is based on a sound diagnostic work-up including assessment of audiological characteristics of the ear noise and the possible existence of hearing loss as well as psychosomatic comorbidities and other concomitant disorders. Comprehensive, anxiety-reducing counseling should be based on this assessment.
Hearing aids should be prescribed for the treatment of accompanying hearing loss. In the case of severe hearing loss or deafness, even if unilateral, a cochlear implant, should recommended whenever possible. There is also good evidence for this method regarding habituation.
The principal techniques available for further treatment, apart from counseling, are tinnitus-specific cognitive behavioral therapy and well-founded psychotherapeutic interventions—in individual or group settings, as a single treatment or multimodal. These therapeutic procedures ameliorate tinnitus distress, improve quality of life, and may also have a beneficial impact on comorbidities such as anxiety and depression.
If patients with severe decompensation due to tinnitus-induced helplessness or severe comorbidities (depression, anxiety) cannot be treated in an ambulatory setting, partially or wholly inpatient treatment can be recommended. Relevant information can be obtained from funding agencies or self-help groups. These treatments should be performed by qualified staff in a personalized, interdisciplinary, and multimodal manner in patients suffering from significant mental comorbidity.
Further systematic studies and reviews will be necessary to improve the implementation of severity-adjusted and, if indicated, multimodal diagnosis and care of patients suffering from tinnitus.
Supplementary Material
eMethods
The methods for the development of this guideline comply with the regulations of the Association of the Scientific Medical Societies in Germany (AWMF) according to the criteria of the German instrument for methodological assessment of guidelines (DELBI, version 2005/2006 + domain 8) Guidelines from various countries identified by a systematic search were consulted when formulating the consensus-based recommendations. The basis of the guideline was a systematic literature search in PubMed and the Cochrane Library from 2014 to the cut-off date, with the last update taking place on 31 December 2020. The consensus conferences took account of the latest references.
Assessment of the validity of the evidence underlying the recommendations is crucial for a clinical practice guideline. The starting point for the revision was the guideline published in 2014. The tables were supplemented with the newly identified studies. The participants in charge of the different sections then presented all studies in terms of the PICO questions and the probability of systematic risk of bias was evaluated. Overall, the search strategy (limited to publications in German or English) turned up 4396 records, of which 174 new studies (RCT) and 43 systematic reviews, including six Cochrane Reviews, were analyzed. Moreover, aspects of safety and extent of acceptance were taken into account. In addition, the reporting quality of all systematic reviews/meta-analyses (etable 1) was assessed on the basis of the PRISMA criteria (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) without a formalized process. The evidence level of each recommendation is oriented on the best evidence found. If a study was found to have a relevant risk of bias, it was downgraded by one level—in several cases, two levels—of evidence. Finally, in formulating the positive or negative recommendations it was necessary to differentiate between the evidence strength for “efficacy,” “weak efficacy,” and “no efficacy” of an intervention.
For the structured consensus process, a multidisciplinary authorized group of 20 professional societies and patients’ representatives was constituted according to the strictures of the AWMF (eBox and eTable 2). Several consensus conferences organized by the steering group took place; the last of them were held online, moderated by a representative of the AWMF.
The official representatives were requested to abstain from voting at the consensus conferences if they had any potential conflicts of interest; the latter are systematically laid out in the guideline.
Grading of the recommendations on diagnosis and treatment took place in accordance with the procedure for German national healthcare guidelines. Dissenting opinions were possible during the consensus process, but none were registered until the stage of final adoption (on three topics).
Based on the exhaustive literature search and the resulting evidence tables, recommendations for necessary and supplementary diagnostic procedures were formulated and agreed by consensus. In a nominal group procedure, positive and also negative recommendations for various treatment approaches were formulated in a structured consensus process and the strength of consensus was defined in each case. Data on health benefits, adverse effects, and risks (to the extent available) were also recorded systematically and considered when formulating the recommendations.
eBOX. Professional Societies.
German Society of Oto-Rhino-Laryngology, Head and Neck Surgery (leading)
German College of Psychosomatic Medicine (Deutsches Kollegium für Psychosomatische Medizin e.V., DKPM)
German Society of Psychosomatic Medicine and Medical Psychotherapy (Deutsche Gesellschaft für Psychosomatische Medizin und ärztliche Psychotherapie, DGPM)
German Study Center for ENT Medicine, Head and Neck Surgery (Deutsches Studienzentrum der HNO-Heilkunde, Kopfund Hals-Chirurgie, DSZ-HNO)
German Medical Society for Behavioral Therapy (Deutsche Ärztliche Gesellschaft für Verhaltenstherapie e.V., DÄVT)
German Society of Behavioral Medicine and Behavior Modification (Deutsche Gesellschaft für Verhaltensmedizin und Verhaltensmodifikation e.V., DGVM)
German Society for Psychiatry and Psychotherapy, Psychosomatics and Neurology e.V. (DGPPN)
German Psychological Society (DGPs)
German Society of Dental, Oral, and Maxillofacial Medicine (Deutsche Gesellschaft für Zahn-, Mundund Kieferheilkunde e.V., DGZMK) and
German Society of Functional Diagnosis and Treatment (Deutsche Gesellschaft für Funktionsdiagnostik und -therapie, DGFDT)
German Society of Phoniatrics and Pediatric Audiology (DGPP)
German Society of Physical and Rehabilitative Medicine (Deutsche Gesellschaft für Physikalische und Rehabilitative Medizin e.V., DGPRM)
German Society of Pediatrics and Adolescent Medicine (DGKJ)
German Society of Audiology (Deutsche Gesellschaft für Audiologie e.V., DGA)
Working Group of German-Speaking Audiologists, Neurootologists, and Otologists (Arbeitsgemeinschaft Deutschsprachiger Audiologen, Neurootologen und Otologen, ADANO)
German Professional Association of Oto-Rhino-Laryngologists (Deutscher Berufsverband der Hals-Nasen-Ohrenärzte e. V.)
German Tinnitus League (Deutsche Tinnitus-Liga e.V., DTL)
European Tinnitus Network (EUTINNET)
German Hearing Loss Union (Deutscher Schwerhörigenbund e.V., DSB)
German Cochlear Implant Society (DCIG)
eTable 1. Evidence table for the German clinical practice guideline on chronic tinnitus.
| Evidence-based recommendations*1 | Remarks | Evidence level*1 |
| Counseling should be recommended as the basis for treatment of chronic tinnitus. | Counseling should form the basis of treatment in every patient with chronic tinnitus. It comprises explanation of the findings after diagnostic tests described in the guideline have been carried out. Furthermore, counseling aims to avoid or take account of further/pre-existing comorbidities by supplying information about potential interventions to ameliorate the tinnitus-specific distress. | Moderate |
| Hearing aids should be recommended in chronic tinnitus and hearing loss. | Compensate of pre-existing hearing loss by means of hearing aids is a prerequirement for tinnitus habituation and may have a positive effect on the degree of tinnitus distress. | Moderate |
| Noise generators should not be recommended in chronic tinnitus. | Patients with hearing loss do not benefit additionally from the use of noise generators as well as hearing aids; no effect of noise generators alone in patients with normal hearing has been demonstrated. | Moderate |
| A cochlear implant (CI) should be recommended in tinnitus patients with severe hearing loss and deafness, including unilateral deafness (strong recommendation). | Use of a CI can achieve good suppression of tinnitus in patients with severe hearing loss and deafness, including unilateral deafness. | Moderate |
| Hearing training should be recommended in chronic tinnitus.*2 | Specific hearing therapy can promote tinnitus habituation by training and reinforcing inhibitory effects of hearing perception. | Moderate Low to weak efficacy |
| Behavioral therapy (in various forms) should be recommended in chronic tinnitus (strong recommendation). | Numerous studies have shown the efficacy of behavioral therapy interventions compared with both waiting-list and active control groups with regard to tinnitus distress. Efficacy has been demonstrated for different forms of behavioral therapy and also, to a limited extent, for Internet-based behavioral therapy. | High |
| Tinnitus retraining therapy (TRT) can be considered as a long-term treatment option in chronic tinnitus. Use of noise generators is not necessary (open recommendation). | The recommendation is restricted to long-term use (at least 12 months; then TRT is more effective than a tinnitus masker); hearing loss and hyperacusis must be taken into account; and particular attention must be paid to the counseling protocol. There is good evidence to show that using a noise generator yields no additional benefit. | High No evidence of efficacy in short-term use, weak evidence of efficacy in longer-term use |
| Music therapy is not required in chronic tinnitus (open recommendation). | Although music therapy techniques represent a reasonable approach with regard to training the hearing, no studies have yet demonstrated efficacy against chronic tinnitus. | High No evidence of efficacy |
| Tailor-made notched music therapy (TMNMT) should not be used in chronic tinnitus. | Music with the tinnitus frequency range “notched out” is available as a smartphone app or in connection with hearing aids. It is no more effective against tinnitus than normal unmodified music. There is evidence of potential for harm. | High No evidence of efficacy |
| Sound therapy should not be used. | Various types of stimulation have been proposed and tested: sounds, noises, auditory scenes, etc. Because of this plethora of methods no overall positive recommendation can be made. | Moderate No evidence of efficacy |
| Acoustic neuromodulation should not be used (strong recommendation). | There is insufficient evidence for the efficacy of acoustic neuromodulation according to the coordinated reset (CR) procedure. Regrading of the recommendation to strongly negative is due to the potential for harm and the high costs incurred by the patients. | High No evidence of efficacy |
| Drugs should not be used to treat chronic tinnitus(strong recommendation). | There are insufficient data on the efficacy of specific drug treatments for tinnitus; however, potentially significant adverse effects have been demonstrated. The negative recommendation has been upgraded owing to the potential risk to patients. This must be distinguished from drug treatment of frequent comorbidities of tinnitus such as anxiety disorders and depression. These concomitant diseases should be treated in accordance with the existing guidelines, including any appropriate medication. | Moderate to high, depending on type of preparationNo evidence of efficacy Evidence for non-recommendation: betahistine, ginkgo, antidepressants (high), benzodiazepines, zinc, melatonin, cannabis, oxytocin, steroids, and gabapentin (moderate) |
| Transcranial magnetic stimulation of the auditory cortex should not be used in chronic tinnitus. | Methods for transcranial magnetic stimulation of the auditory cortex have been intensively researched, mostly in studies with very small case numbers: recent meta-analyses come to contradictory conclusions as to whether the efficacy exceeds that of placebo. | High Inconsistent evidence of efficacy |
| Transcranial electrostimulation should not be used in chronic tinnitus. | There is evidence for the safety of transcranial electrostimulation but not for its efficacy in chronic tinnitus. | Moderate No evidence of efficacy |
| Transcutaneous or invasive vagus nerve stimulation, whether alone or in combination with acoustic stimulation, should not be used in chronic tinnitus. | Both transcutaneous and invasive cervically implanted vagus nerve stimulation can be used safely, but there is no evidence of efficacy against chronic tinnitus. | Moderate No evidence of efficacy |
| Bimodal acoustic and electrical stimulation should not be used in chronic tinnitus. | Bimodal acoustic and electrical stimulation is safe to use, but there is no robust evidence of efficacy. | Moderate Negative recommendation in view of existing conflicts of interest |
| Invasive electrostimulation of the brain should not be used in chronic tinnitus. | With regard to invasive treatments of tinnitus, there is no evidence either for their safety nor for therapeutic effects. The adverse effects may be severe, so the recommendation has been regraded to to strongly negative. | Moderate No evidence of efficacy |
| Transcutaneous electrical nerve stimulation (TENS) should not be used in chronic tinnitus. | There is only moderate evidence or none at all for the safety of TENS or for therapeutic effects against tinnitus. No controlled trials have been carried out. | Moderate No evidence of efficacy |
| Low-level laser treatment should not be used in chronic tinnitus. | There is no evidence either for the safety of low-level laser treatment methods or for therapeutic effects against tinnitus. No controlled trials have been carried out. | Moderate No evidence of efficacy |
| Manual medicine and physiotherapy should be offered in chronic tinnitus in the presence of modulation of the tinnitus by comorbid lesions of the cervical spine and the masticatory apparatus. | If modulation of tinnitus is determined in the course of basic assessment of the cervical spine and the masticatory apparatus and the findings of advanced manual medicine examination indicate involvement of the cervical spine, temporomandibular joint function, and muscular trigger points/imbalance, manual medicine and physiotherapy should be used.Manual medicine and physiotherapy have a positive effect on the severity of tinnitus and on cervical spine symptoms. A combination of physiotherapy and manual therapy along with patient education yields positive effects in patients with tinnitus and concomitant craniomandibular dysfunction. | High Recommendation downgraded owing to high risk of bias of the randomized clinical trials analyzed |
| Nutritional supplements should not be used in chronic tinnitus. | No evidence exists that nutritional supplements (e.g., vitamins, minerals, or phytotherapeutics) exert any effect on tinnitus, or that they differ from placebo treatments in respect of tinnitus reduction or adverse effects. | High No evidence of efficacy |
| (Electro)acupuncture should not be used in chronic tinnitus. | There is no evidence that acupuncture or electroacupuncture exhibits efficacy against tinnitus. There is moderate evidence that it can ameliorate comorbidities such as muscle tension or pain, with a possibly positive effect on the tinnitus. | High No evidence of efficacy |
| Patients with chronic tinnitus should be motivated to take up self-help options. | For many of those affected, self-help is an effective and supportive element of treatment. | Moderate |
*1 Simple recommendation (level B) unless otherwise indicated. The determinations of recommendation strength and evidence level are described in the methods report of the clinical practice guideline. The underlying evidence tables can be found in the long version.
*2 Dissenting opinion of the German Society for Psychiatry and Psychotherapy, Psychosomatics and Neurology (DGPPN): Hearing training can be considered in chronic tinnitus (open recommendation). Rationale: Owing to insufficient evidence, no recommendation can currently be made. Further research is required.
eTable 2. Collaborators.
| Mandated members | Address | Professional society |
| Prof. Dr. Birgit Mazurek Prof. Dr. Gerhard Hesse |
Charité-Universitätsmedizin Berlin, Tinnituszentrum, Charitéplatz 1, 10117 Berlin Tinnitus-Klinik am Krankenhaus Bad Arolsen, Große Allee 50, 34454 Bad Arolsen |
Coordinators, German Society of Oto-Rhino-Laryngology, Head and Neck Surgery (DGHNO-KHCH) |
| Prof. Dr. Claas Lahmann | Universitätsklinikum Freiburg, Klinik für Psychosomatische Medizin und Psychotherapie, Hauptstr. 8, 79104 Freiburg | German College of Psychosomatic Medicine (Deutsches Kollegium für Psychosomatische Medizin e.V., DKPM) |
| Prof. Dr. Christian Dobel | Friedrich-Schiller-Universität Jena, Experimentelle HNO-Heilkunde, HNO Klinik, Stoystr. 3, 07740 Jena | German Study Center for ENT Medicine, Head and Neck Surgery (Deutsches Studienzentrum der HNO-Heilkunde, Kopf- und Hals-Chirurgie, DSZ-HNO) |
| Prof. Dr. Berthold Langguth | Klinik für Psychiatrie u. Psychotherapie, Universität Regensburg, Universitätsstr. 84, 93053 Regensburg | German Society for Psychiatry and Psychotherapy, Psychosomatics and Neurology e. V. (DGPPN) |
| Prof. Dr. Ingrid Peroz | Charité-Universitätsmedizin Berlin, Abt. für Zahnärztliche Prothetik, Alterszahnmedizin und Funktionslehre, Aßmannshauser Str. 4–6, 14197 Berlin | German Society of Dental, Oral, and Maxillofacial Medicine (Deutsche Gesellschaft für Zahn-, Mund- und Kieferheilkunde e.V., DGZMK) and German Society of Functional Diagnosis and Treatment (Deutsche Gesellschaft für Funktionsdiagnostik und -therapie, DGFDT) |
| Prof. Dr. Wolfgang Delb | Deutsche Gesellschaft für Phoniatrie und Pädaudiologie e. V., Nikolaistr. 29, 37073 Göttingen | German Society of Phoniatrics and Pediatric Audiology (DGPP) |
| Prof. Dr. Gerhard Goebel | Medical Director (retired), Schön Klinik Roseneck, Tinnitus- und Hyperakusiszentrum im Neurozentrum Prien, Bernauerstr. 12, 83209 Prien am Chiemsee | German Medical Society for Behavioral Therapy (Deutsche Ärztliche Gesellschaft für Verhaltenstherapie e.V., DÄVT) |
| Dr. Anett Reißhauer | Charité-Universitätsmedizin, Arbeitsbereich Physikalische Medizin, Charitéplatz 1, 10117 Berlin | German Society of Physical and Rehabilitative Medicine (Deutsche Gesellschaft für Physikalische und Rehabilitative Medizin e.V., DGPRM) |
| Prof. Dr. Regina Trollmann | Universitäts-Kinderklinik Erlangen, Sozialpädiatrisches Zentrum, Neuropädiatrie und Epileptologie, Loschgestr. 15, 91054 Erlangen | German Society of Pediatrics and Adolescent Medicine (DGKJ) |
| Prof. Dr. Annette Limberger | Hochschule Aalen, Augenoptik und Hörakustik, Anton-Huber-Str. 23, 73430 Aalen | German Society of Audiology (Deutsche Gesellschaft für Audiologie e.V., DGA) |
| Prof. Dr. Thomas Zahnert | Universitätsklinik Carl Gustav Carus Klinik und Poliklinik für HNO-Heilkunde, Fetscherstr. 74, 01307 Dresden | Working Group of German-Speaking Audiologists, Neurootologists, and Otologists (Arbeitsgemeinschaft Deutschsprachiger Audiologen, Neurootologen und Otologen, ADANO) |
| PD. Dr. Jan Löhler | Deutscher Berufsverband der Hals-Nasen-Ohren-Ärzte e.V., Landesvorsitzender Schleswig-Holstein, Maienbeeck 1, 24576 Bad Bramstedt | German Professional Association of Oto-Rhino-Laryngologists (Deutscher Berufsverband der Hals-Nasen-Ohrenärzte e. V.) |
| Other participants | Function & professional society | Organization |
| Dr. Matthias Rudolph | Deutsche Tinnitus-Liga, Am Lohsiepen 18, 42369 Wuppertal | German Tinnitus League (Deutsche Tinnitus-Liga e.V., DTL) |
| Dr. Eberhard Biesinger | European Tinnitus Network (EUTINNET), Charitéplatz 1, 10117 Berlin | European Tinnitus Network (EUTINNET) |
| Dr. Harald Seidler | Deutscher Schwerhörigenbund e. V. (DSB), Breite Str. 3, 13187 Berlin | German Hearing Loss Union (Deutscher Schwerhörigenbund e.V., DSB) |
| Dr. Roland Zeh | Deutsche Cochlea Implant Gesellschaft e. V., Hauptstr. 43, 89250 Senden | German Cochlear Implant Society |
| Consultants and experts | Address | Professional society/organization |
| Prof. Dr. Ina B. Kopp Dr. Susanne Blödt |
AWMF-Institut für Medizinisches Wissensmanagement, c/o Philipps-Universität, Karl-von-Frisch-Str. 1, 35043 Marburg | Association of the Scientific Medical Societies in Germany (AWMF) |
| Dipl. Psych. Heribert Sattel | Klinikum rechts der Isar der Technischen Universität München, Klinik und Poliklinik für Psychosomatische Medizin und Psychotherapie, Langerstr. 3, 81675 München | |
| Dr. Volker Kratzsch | VAMED Rehaklinik Bad Grönenbach, Abteilung Hörbehinderung, Tinnitus und Schwindel-Erkrankungen, Sebastian-Kneipp-Allee 3–5, 87730 Bad Grönenbach | |
| Dr. Kurt Anschütz | Deutsche Stiftung Tinnitus & Hören Charité, Charitéplatz 1, 10117 Berlin | German Tinnitus and Hearing Foundation Charité (Deutsche Stiftung Tinnitus & Hören Charité) |
Acknowledgments
Clinical practice guidelines in the Deutsches Ärzteblatt, as in many other journals, are not subject to a peer review process, since clinical practice (S3 level) guidelines are texts which have already been evaluated, discussed, and broadly agreed upon multiple times by experts (peers).
Footnotes
Conflict of interest statement
Prof. Hesse is medical director and a co-partner of the Tinnitus Clinic at Bad Arolsen Hospital. He has received payment for legal opinions on the topic of tinnitus. He is the spokesman of the scientific advisory board of the German Tinnitus League (Deutsche Tinnitus-Liga), a board member of the Association of Central German Otorhinolaryngologists (Vereinigung mitteldeutscher HNO-Ärzte), a consultant to HNO Update, and a scientific advisor to the Tinnitus and Hearing Foundation Charité.
Prof. Mazurek has received support for research projects from terzo-Institut, Dr. Willmar Schwane GmbH & Co. KG, the Heinz and Heide Dürr Foundation, the Tinnitus and Hearing Foundation, Resaphene, and in connection with the EU projects UNITI, TIN-ACT, and TIGER. Travel costs and congress fees were taken over by Infecto Pharm, Dr. Willmar Schwane GmbH & Co. KG, MED-EL, the German Otorhinolaryngological Training Society (Deutsche Fortbildungsgesellschaft für HNO-Ärzte), and Geers. She is a board member of the German Tinnitus and Hearing Foundation (Deutsche Stiftung Tinnitus und Hören) and a member of the scientific advisory board of the German Tinnitus League (Deutsche Tinnitus-Liga). She has received third-party funding for projects in connection with the EU program HORIZON 2020.
The remaining authors declare that no conflict of interest exists.
References
- 1.Pilgramm M, Rychlik R, Lebisch H, Siedentop H, Goebel G, Kirchhoff D. Tinnitus in der Bundesrepublik Deutschland - eine repräsentative epidemiologische Studie. HNO aktuell. 1999;7:26–25. [Google Scholar]
- 2.McCormack A, Edmondson-Jones M, Somerset S, Hall D. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res. 2016;337:70–79. doi: 10.1016/j.heares.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 3.Biesinger E, Heiden C, Greimel V, Lendle T, Höing R, Albegger K. Strategien in der ambulanten Behandlung des Tinnitus. HNO. 1998;46 doi: 10.1007/s001060050215. 15769. [DOI] [PubMed] [Google Scholar]
- 4.Schecklmann M, Vielsmeier V, Steffens T, Landgrebe M, Langguth B, Kleinjung T. Relationship between audiometric slope and tinnitus pitch in tinnitus patients: insights into the mechanisms of tinnitus generation. PloS One. 2012;7 doi: 10.1371/journal.pone.0034878. e34878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zirke N, Seydel C, Szczepek A, Olze H, Haupt H, Mazurek B. Psychological comorbidity in patients with chronic tinnitus: analysis and comparison with chronic pain, asthma or atopic dermatitis patients. Qual Life Res. 2013;22:263–272. doi: 10.1007/s11136-012-0156-0. [DOI] [PubMed] [Google Scholar]
- 6.Cima RFF, van Breukelen G, Vlaeyen JWS. Tinnitus-related fear: mediating the effects of a cognitive behavioural specialised tinnitus treatment. Hear Res. 2018;358:86–97. doi: 10.1016/j.heares.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Mazurek B, Szczepek AJ, Brüggemann P. [Tinnitus - clinical symptoms and therapy] LRO. 2017;96:47–59. doi: 10.1055/s-0042-119419. [DOI] [PubMed] [Google Scholar]
- 8.Hesse G. Evidence and evidence gaps in tinnitus therapy. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2016;15 doi: 10.3205/cto000131. Doc04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.AWMF. Leitlinie Tinnitus. Leitlinien der Deutschen Gesellschaft für Hals-Nasen-Ohren-Heilkunde. Kopf- und Halschirurgie. 2021:1–108. Leitlinie 017/064: [Google Scholar]
- 10.AWMF. S3-Leitlinie Chronischer Tinnitus - Patientenleitlinie. 2021:1–9. 017/64. [Google Scholar]
- 11.AWMF. Leitlinie Hörsturz. Leitlinien der Dt Ges f Hals-Nasen-Ohren-Heilkunde. Kopf- und Halschirurgie. 2014:1–10. Leitlinie 017/010. [Google Scholar]
- 12.Hoare D, Kowalkowski V, Kang S, Hall D. Systematic review and meta-analyses of randomized controlled trials examining tinnitus management. Laryngoscope. 2011;121:1555–1564. doi: 10.1002/lary.21825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kreuzer PM, Vielsmeier V, Langguth B. Chronic tinnitus: an interdisciplinary challenge. Dtsch Arztebl Int. 2013;110:278–284. doi: 10.3238/arztebl.2013.0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kofahl C. Associations of collective self-help activity, health literacy and quality of life in patients with tinnitus. Patient Educ Couns. 2018;101:2170–2178. doi: 10.1016/j.pec.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Yakunina N, Lee WH, Ryu YJ, Nam EC. Tinnitus suppression effect of hearing aids in patients with high-frequency hearing loss: a randomized double-blind controlled trial. Otol Neurotol. 2019;40:865–871. doi: 10.1097/MAO.0000000000002315. [DOI] [PubMed] [Google Scholar]
- 16.Henry JA, McMillan G, Dann S, Bennett K, Griest S, Theodoroff S, et al. Tinnitus management: randomized controlled trial comparing extended-wear hearing aids, conventional hearing aids, and combination instruments. J Am Acad Audiol. 2017;28:546–561. doi: 10.3766/jaaa.16067. [DOI] [PubMed] [Google Scholar]
- 17.Kimball SH, Johnson CE, Baldwin J, Barton K, Mathews C, Danhauer JL. Hearing aids as a treatment for tinnitus patients with slight to mild sensorineural hearing loss. Semin Hear. 2018;39:123–134. doi: 10.1055/s-0038-1641739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borges ALF, Duarte P, Almeida RBS, Ledesma ALL, Azevedo YJ, Pereira LV, et al. Cochlear implant and tinnitus-a meta-analysis. Braz J Otorhinolaryngol. 2020;87:353–365. doi: 10.1016/j.bjorl.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hesse G, Schaaf H. Thieme. Stuttgart: 2012. Manual der Hörtherapie. [Google Scholar]
- 20.Hoare D, Stacey P, Hall D. The efficacy of auditory perceptual training for tinnitus: a systematic review. Ann Behav Med. 2010;40:313–324. doi: 10.1007/s12160-010-9213-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tutaj L, Hoare DJ, Sereda M. Combined amplification and sound generation for tinnitus: a scoping review. Ear hear. 2018;39:412–422. doi: 10.1097/AUD.0000000000000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fuller T, Cima R, Langguth B, Mazurek B, Vlaeyen JW, Hoare DJ. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev. 2020;1 doi: 10.1002/14651858.CD012614.pub2. CD012614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jastreboff PJ. 25 years of tinnitus retraining therapy. HNO. 2015;63:307–311. doi: 10.1007/s00106-014-2979-1. [DOI] [PubMed] [Google Scholar]
- 24.Bauer CA, Berry JL, Brozoski TJ. The effect of tinnitus retraining therapy on chronic tinnitus: a controlled trial. Laryngoscope Investig Otolaryngol. 2017;2:166–177. doi: 10.1002/lio2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scherer RW, Formby C Tinnitus Retraining Therapy Trial Research. Effect of tinnitus retraining therapy vs standard of care on tinnitus-related quality of life: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2019;145:597–608. doi: 10.1001/jamaoto.2019.0821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stein A, Wunderlich R, Lau P, Engell A, Wollbrink A, Shaykevich A, et al. Clinical trial on tonal tinnitus with tailor-made notched music training. BMC Neurol. 2016;16 doi: 10.1186/s12883-016-0558-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wegger M, Ovesen T, Larsen DG. Acoustic coordinated reset neuromodulation: a systematic review of a novel therapy for tinnitus. Front Neurol. 2017;8 doi: 10.3389/fneur.2017.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wegner I, Hall DA, Smit AL, McFerran D, Stegeman I. Betahistine for tinnitus. Cochrane Database Syst Rev. 2018;12 doi: 10.1002/14651858.CD013093.pub2. CD013093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hilton MP, Zimmermann EF, Hunt WT. Ginkgo biloba for tinnitus. Cochrane Database Syst Rev. 2013;3 doi: 10.1002/14651858.CD003852.pub3. CD003852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Posadzki P, Watson LK, Ernst E. Adverse effects of herbal medicines: an overview of systematic reviews. Clin Med (Lond) 2013;13:7–12. doi: 10.7861/clinmedicine.13-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hofmeister M. Do dietary factors significantly influence tinnitus? Aust J Gen Pract. 2019;48:153–157. doi: 10.31128/AJGP-07-18-4643. [DOI] [PubMed] [Google Scholar]
- 32.Landgrebe M, Hajak G, Wolf S, Padberg F, Klupp P, Fallgatter AJ, et al. 1-Hz rTMS in the treatment of tinnitus: a sham-controlled, randomized multicenter trial. Brain stimulation. 2017;10:1112–1120. doi: 10.1016/j.brs.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 33.Chen JJ, Zeng BS, Wu CN, Stubbs B, Carvalho AF, Brunoni AR, et al. Association of central noninvasive brain stimulation interventions with efficacy and safety in tinnitus management: a meta-analysis. Otolaryngol Head Neck Surg. 2020;1;146:801–809. doi: 10.1001/jamaoto.2020.1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lefebvre-Demers M, Doyon N, Fecteau S. Non-invasive neuromodulation for tinnitus: a meta-analysis and modeling studies. Brain Stimul. 2021;14:113–128. doi: 10.1016/j.brs.2020.11.014. [DOI] [PubMed] [Google Scholar]
- 35.Tyler R, Cacace A, Stocking C, Tarver B, Engineer N, Martin J, et al. Vagus nerve stimulation paired with tones for the treatment of tinnitus: a prospective randomized double-blind controlled pilot study in humans. Sci Rep. 2017;7 doi: 10.1038/s41598-017-12178-w. 11960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marks KL, Martel DT, Wu C, Basura GJ, Roberts LE, Schvartz-Leyzac KC, et al. Auditory-somatosensory bimodal stimulation desynchronizes brain circuitry to reduce tinnitus in guinea pigs and humans. Sci Transl Med. 2018;10 doi: 10.1126/scitranslmed.aal3175. 422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Conlon B, Langguth B, Hamilton C, Hughes S, Meade E, Connor CO, et al. Bimodal neuromodulation combining sound and tongue stimulation reduces tinnitus symptoms in a large randomized clinical study. Sci Transl Med. 2020;12 doi: 10.1126/scitranslmed.abb2830. 564. [DOI] [PubMed] [Google Scholar]
- 38.Choi JE, Lee MY, Chung PS, Jung JY. A preliminary study on the efficacy and safety of low level light therapy in the management of cochlear tinnitus: a single blind randomized clinical trial. Int Tinnitus J. 2019;23:52–57. doi: 10.5935/0946-5448.20190010. [DOI] [PubMed] [Google Scholar]
- 39.Michiels S, Van de Heyning P, Truijen S, Hallemans A, De Hertogh W. Does multi-modal cervical physical therapy improve tinnitus in patients with cervicogenic somatic tinnitus? Man Ther. 2016;26:125–131. doi: 10.1016/j.math.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 40.Kinne L, Bays LC, Fahlen KL, Owens JS. Somatic tinnitus and manual therapy: a systematic review. OJOR Online Jour ORL. 2019;1(2) [Google Scholar]
- E1.Biswas R, Hall DA. Prevalence, incidence, and risk factors for tinnitus. Curr Top Behav Neurosci. 2021;51:3–28. doi: 10.1007/7854_2020_154. [DOI] [PubMed] [Google Scholar]
- E2.Hesse G. Tinnitus II. ed. Stuttgart. Thieme. 2015 [Google Scholar]
- E3.Zirke N, Seydel C, Arsoy D, Klapp BF, Haupt H, Szczepek AJ, et al. Analysis of mental disorders in tinnitus patients performed with composite international diagnostic interview. Qual Life Res. 2013;22:2095–2104. doi: 10.1007/s11136-012-0338-9. [DOI] [PubMed] [Google Scholar]
- E4.Kratzsch V, Goebel G. Aktuelle Aspekte zu Tinnitus und Depression. HNO. 2018;66:188–197. doi: 10.1007/s00106-018-0477-6. [DOI] [PubMed] [Google Scholar]
- E5.Goebel G, Hiller W. Tinnitus-Fragebogen (TF) Ein Instrument zur Erfassung von Belastung und Schweregrad bei Tinnitus (siehe Anlage Tinnitus Fragebogen). Göttingen, Bern, Toronto, Seattle. Hogrefe Verlag für Psychologie. 1998 [Google Scholar]
- E6.Sohn W. Daten zur Prävalenz von Schwerhörigkeit. Deutscher Schwerhörigenbund DSB. Universität Witten-Herdecke. 2000 [Google Scholar]
- E7.Ramakers GG, van Zon A, Stegeman I, Grolman W. The effect of cochlear implantation on tinnitus in patients with bilateral hearing loss: a systematic review. Laryngoscope. 2015;125:2584–2592. doi: 10.1002/lary.25370. [DOI] [PubMed] [Google Scholar]
- E8.Olze H, Szczepek A, Haupt H, Zirke N, Graebel S, Mazurek B. The impact of cochlear implantation on tinnitus, stress and quality of life in postlingually deafened patients. Audiol Neurootol. 20121;7:2–11. doi: 10.1159/000323847. [DOI] [PubMed] [Google Scholar]
- E9.Martinez-Devesa P, Perera R, Theodoulou M, Waddell A. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev. 2010;9 doi: 10.1002/14651858.CD005233.pub3. CD005233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E10.Schaaf H, Weiß S, Hesse G. Catamnesis results of an inpatient neuro-otolog and psychosomatic tinnitus therapy 1-5 years after discharge. Eur Arch Otorhinolaryngol. 2017;274:701–710. doi: 10.1007/s00405-016-4316-7. [DOI] [PubMed] [Google Scholar]
- E11.Grewal R, Spielmann PM, Jones SE, Hussain SS. Clinical efficacy of tinnitus retraining therapy and cognitive behavioural therapy in the treatment of subjective tinnitus: a systematic review. J Laryngol Otol. 2014:1–6. doi: 10.1017/S0022215114002849. [DOI] [PubMed] [Google Scholar]
- E12.Dong C, Chen C, Wang T, Gao C, Wang Y, Guan X, et al. Low-frequency repetitive transcranial magnetic stimulation for the treatment of chronic tinnitus: a systematic review and meta-analysis of randomized controlled trials. Biomed Res Int. 2020 doi: 10.1155/2020/3141278. 3141278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E13.Liang Z, Yang H, Cheng G, Huang L, Zhang T, Jia H. Repetitive transcranial magnetic stimulation on chronic tinnitus: a systematic review and meta-analysis. BMC Psychiatry. 2020;20 doi: 10.1186/s12888-020-02947-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E14.Dehkordi MA, Einolghozati S, Ghasemi SM, Abolbashari S, Meshkat M, Behzad H. Effect of low-level laser therapy in the treatment of cochlear tinnitus: a double-blind, placebo-controlled study. Ear Nose Throat J. 2015;94:32–36. [PubMed] [Google Scholar]
- E15.Haider HF, Hoare DJ, Costa RFP, Potgieter I, Kikidis D, Lapira A, et al. Pathophysiology, diagnosis and treatment of somatosensory tinnitus: a scoping review. Front Neurosci. 2017;11 doi: 10.3389/fnins.2017.00207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
The methods for the development of this guideline comply with the regulations of the Association of the Scientific Medical Societies in Germany (AWMF) according to the criteria of the German instrument for methodological assessment of guidelines (DELBI, version 2005/2006 + domain 8) Guidelines from various countries identified by a systematic search were consulted when formulating the consensus-based recommendations. The basis of the guideline was a systematic literature search in PubMed and the Cochrane Library from 2014 to the cut-off date, with the last update taking place on 31 December 2020. The consensus conferences took account of the latest references.
Assessment of the validity of the evidence underlying the recommendations is crucial for a clinical practice guideline. The starting point for the revision was the guideline published in 2014. The tables were supplemented with the newly identified studies. The participants in charge of the different sections then presented all studies in terms of the PICO questions and the probability of systematic risk of bias was evaluated. Overall, the search strategy (limited to publications in German or English) turned up 4396 records, of which 174 new studies (RCT) and 43 systematic reviews, including six Cochrane Reviews, were analyzed. Moreover, aspects of safety and extent of acceptance were taken into account. In addition, the reporting quality of all systematic reviews/meta-analyses (etable 1) was assessed on the basis of the PRISMA criteria (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) without a formalized process. The evidence level of each recommendation is oriented on the best evidence found. If a study was found to have a relevant risk of bias, it was downgraded by one level—in several cases, two levels—of evidence. Finally, in formulating the positive or negative recommendations it was necessary to differentiate between the evidence strength for “efficacy,” “weak efficacy,” and “no efficacy” of an intervention.
For the structured consensus process, a multidisciplinary authorized group of 20 professional societies and patients’ representatives was constituted according to the strictures of the AWMF (eBox and eTable 2). Several consensus conferences organized by the steering group took place; the last of them were held online, moderated by a representative of the AWMF.
The official representatives were requested to abstain from voting at the consensus conferences if they had any potential conflicts of interest; the latter are systematically laid out in the guideline.
Grading of the recommendations on diagnosis and treatment took place in accordance with the procedure for German national healthcare guidelines. Dissenting opinions were possible during the consensus process, but none were registered until the stage of final adoption (on three topics).
Based on the exhaustive literature search and the resulting evidence tables, recommendations for necessary and supplementary diagnostic procedures were formulated and agreed by consensus. In a nominal group procedure, positive and also negative recommendations for various treatment approaches were formulated in a structured consensus process and the strength of consensus was defined in each case. Data on health benefits, adverse effects, and risks (to the extent available) were also recorded systematically and considered when formulating the recommendations.